Abstracts
OBJECTIVE: To compare inpatient and outpatient care costs for pregnant/parturient women with diabetes and mild hyperglycemia. METHODS: A prospective observational quantitative study was conducted in the Perinatal Diabetes Center in the city of Botucatu, Southeastern Brazil, between 2007 and 2008. Direct and indirect costs and disease-specific costs (medications and tests) were estimated. Thirty diet-treated pregnant women with diabetes were followed up on an outpatient basis, and 20 who required insulin therapy were hospitalized. RESULTS: The cost of diabetes disease (prenatal and delivery care) was US$ 3,311.84 for inpatients and US$ 1,366.04 for outpatients. CONCLUSIONS: Direct and indirect costs as well as total prenatal care cost were higher for diabetic inpatients while delivery care costs and delivery-postpartum hospitalization were similar. Prenatal and delivery-postpartum care costs were higher for these patients compared to those paid by Brazilian National Health System.
Pregnant Women; Hyperglycemia; Diabetes; Diabetes; Health Care Costs; Perinatal Care; Postpartum Period
OBJETIVO: Comparar costos de hospitalización y de atención por ambulatorio en gestantes/parturientas diabéticas y con hiperglicemia leve. MÉTODOS: Estudio observacional, prospectivo, cuantitativo descriptivo realizado en centro de diabetes perinatal en Botucatu, Sureste de Brasil, entre 2007 y 2008. Se estimaron los costos por absorción directos e indirectos disponibles en la institución y los costos específicos para la enfermedad (medicamentos y exámenes). Las 30 gestantes diabéticas tratadas con dieta fueron acompañadas en ambulatorio y 20 tratadas con dieta más insulina fueron hospitalizadas. RESULTADOS: El costo de la enfermedad diabetes (para asistencia prenatal y parto) fue de US$ 3,311.84 para las gestantes hospitalizadas y de US$ 1,366.04 para las acompañadas en ambulatorio. CONCLUSIONES: Los costos directos e indirectos y el costo total de la asistencia prenatal fueron más elevados en las gestantes diabéticas hospitalizadas mientras que los costos de la asistencia al parto y hospitalización para parto y puerperio fueron semejantes. Los costos de la asistencia prenatal como en el parto/puerperio fueron superiores a los valores pagados por el Sistema Único de Salud.
Gestantes; Hiperglicemia; Diabetes Gestacional; Costos de la Atención en Salud; Atención Perinatal; Periodo de Posparto
OBJETIVO: Comparar custos de hospitalização e de atenção ambulatorial em gestantes/parturientes diabéticas e com hiperglicemia leve. MÉTODOS: Estudo observacional, prospectivo, quantitativo descritivo realizado em centro de diabete perinatal em Botucatu, SP, entre 2007 e 2008. Foram estimados os custos por absorção diretos e indiretos disponíveis na instituição e os custos específicos para a doença (medicamentos e exames). As 30 gestantes diabéticas tratadas com dieta foram acompanhadas em ambulatório e 20 tratadas com dieta mais insulina foram hospitalizadas. RESULTADOS: O custo da doença diabete (para a assistência pré-natal e parto) foi de US$ 3,311.84 para as gestantes hospitalizadas e de US$ 1,366.04 para as acompanhadas em ambulatório. CONCLUSÕES: Os custos diretos e indiretos e o custo total da assistência pré-natal foram mais elevados nas gestantes diabéticas hospitalizadas enquanto os custos da assistência ao parto e hospitalização para parto e puerpério foram semelhantes. Os custos da assistência pré-natal como no parto/puerpério foram superiores aos valores pagos pelo Sistema Único de Saúde.
Gestantes; Hiperglicemia; Diabetes Gestacional; Custos de Cuidados de Saúde; Assistência Perinatal; Período Pós-Parto
Care cost for pregnant and parturient women with diabetes and mild hyperglycemia
Custo da assistência de gestantes e parturientes diabéticas e com hiperglicemia leve
Costo de la asistencia de gestantes y parturientas diabéticas y con hiperglicemia leve
Ana Claudia Molina CavassiniI; Silvana Andrea Molina LimaII; Iracema Mattos Paranhos CalderonIII; Marilza Vieira Cunha RudgeIII
IGraduate Program in Gynecology, Obstetrics and Mastology. Botucatu Medical School. Universidade Estadual Paulista Júlio de Mesquita Filho (Unesp). Botucatu, SP, Brazil
IIDepartment of Nursing. Botucatu Medical School. Unesp. Botucatu, SP, Brazil
IIIDepartment of Obstetrics and Gynecology. Botucatu Medical School. Unesp. Botucatu, SP, Brazil
Correspondence Correspondence: Ana Claudia Molina Cavassini Departamento de Ginecologia e Obstetrícia Faculdade de Medicina de Botucatu-Unesp Distrito de Rubião Junior, s/n 18618-000 Botucatu, SP, Brasil E-mail: acmolinacavassini@hotmail.com
ABSTRACT
OBJECTIVE: To compare inpatient and outpatient care costs for pregnant/parturient women with diabetes and mild hyperglycemia.
METHODS: A prospective observational quantitative study was conducted in the Perinatal Diabetes Center in the city of Botucatu, Southeastern Brazil, between 2007 and 2008. Direct and indirect costs and disease-specific costs (medications and tests) were estimated. Thirty diet-treated pregnant women with diabetes were followed up on an outpatient basis, and 20 who required insulin therapy were hospitalized.
RESULTS: The cost of diabetes disease (prenatal and delivery care) was US$ 3,311.84 for inpatients and US$ 1,366.04 for outpatients.
CONCLUSIONS: Direct and indirect costs as well as total prenatal care cost were higher for diabetic inpatients while delivery care costs and delivery-postpartum hospitalization were similar. Prenatal and delivery-postpartum care costs were higher for these patients compared to those paid by Brazilian National Health System.
Descriptors: Pregnant Women. Hyperglycemia. Diabetes, Gestational, economics. Health Care Costs. Perinatal Care, economics. Postpartum Period.
RESUMO
OBJETIVO: Comparar custos de hospitalização e de atenção ambulatorial em gestantes/parturientes diabéticas e com hiperglicemia leve.
MÉTODOS: Estudo observacional, prospectivo, quantitativo descritivo realizado em centro de diabete perinatal em Botucatu, SP, entre 2007 e 2008. Foram estimados os custos por absorção diretos e indiretos disponíveis na instituição e os custos específicos para a doença (medicamentos e exames). As 30 gestantes diabéticas tratadas com dieta foram acompanhadas em ambulatório e 20 tratadas com dieta mais insulina foram hospitalizadas.
RESULTADOS: O custo da doença diabete (para a assistência pré-natal e parto) foi de US$ 3,311.84 para as gestantes hospitalizadas e de US$ 1,366.04 para as acompanhadas em ambulatório.
CONCLUSÕES: Os custos diretos e indiretos e o custo total da assistência pré-natal foram mais elevados nas gestantes diabéticas hospitalizadas enquanto os custos da assistência ao parto e hospitalização para parto e puerpério foram semelhantes. Os custos da assistência pré-natal como no parto/puerpério foram superiores aos valores pagos pelo Sistema Único de Saúde.
Descritores: Gestantes. Hiperglicemia. Diabetes Gestacional, economia. Custos de Cuidados de Saúde. Assistência Perinatal, economia. Período Pós-Parto.
RESUMEN
OBJETIVO: Comparar costos de hospitalización y de atención por ambulatorio en gestantes/parturientas diabéticas y con hiperglicemia leve.
MÉTODOS: Estudio observacional, prospectivo, cuantitativo descriptivo realizado en centro de diabetes perinatal en Botucatu, Sureste de Brasil, entre 2007 y 2008. Se estimaron los costos por absorción directos e indirectos disponibles en la institución y los costos específicos para la enfermedad (medicamentos y exámenes). Las 30 gestantes diabéticas tratadas con dieta fueron acompañadas en ambulatorio y 20 tratadas con dieta más insulina fueron hospitalizadas.
RESULTADOS: El costo de la enfermedad diabetes (para asistencia prenatal y parto) fue de US$ 3,311.84 para las gestantes hospitalizadas y de US$ 1,366.04 para las acompañadas en ambulatorio.
CONCLUSIONES: Los costos directos e indirectos y el costo total de la asistencia prenatal fueron más elevados en las gestantes diabéticas hospitalizadas mientras que los costos de la asistencia al parto y hospitalización para parto y puerperio fueron semejantes. Los costos de la asistencia prenatal como en el parto/puerperio fueron superiores a los valores pagados por el Sistema Único de Salud.
Descriptores: Gestantes. Hiperglicemia. Diabetes Gestacional, economía. Costos de la Atención en Salud. Atención Perinatal, economía. Periodo de Posparto.
INTRODUCTION
Pregnancies complicated by diabetes are associated with an increased risk of maternal and neonatal complications. The most serious maternal complication is the risk of developing type 2 diabetes within 10-12 years after birth.21 Perinatal complications include macrosomia and increased risk of birth trauma and intrapartum hypoxia/asphyxia, high C-section rates, delayed pulmonary maturation and consequent risk of respiratory distress syndrome, and metabolic disorders at birth including hypoglycemia, hypocalcemia and hypomagnesemia.19 All these conditions worsen neonatal prognosis and increase perinatal mortality. In addition, Rudge et al17 demonstrated that pregnant women with mild hyperglycemia (normal 100-g glucose tolerance test [GTT] and abnormal blood glucose profile) have perinatal outcomes comparable to those of diabetic women and should be treated following the same protocol.
Perinatal outcomes with either diabetes or mild hyperglycemia are directly associated to maternal metabolic control. Maternal hyperglycemia should be carefully controlled with either diet alone or diet plus insulin therapy so that effective blood glucose normalization can be achieved and adverse perinatal outcomes prevented. Newborns of pregnant women with inadequate blood glucose control (mean blood glucose >130 mg/dL in the third trimester) are reported to show macrosomia in 52.4%, fetal death in 14.3%, and malformations in 8.2%. Over the past decades, improved maternal and perinatal outcomes of diabetic pregnancies have been associated with maternal normal blood glucose levels.6 Strict blood glucose control requires either outpatient care or frequent short hospital stays.10,14 Treatment of diabetic pregnant women may be facilitated in tertiary care services12 by making hospitalization easier and offering specialized outpatient care, fetal well-being assessment, and delivery and neonatal care.
Financial and social advantages of outpatient management are numerous. However, repeated short hospital stays are helpful to pregnant women with pregestational diabetes who require insulin therapy from early pregnancy. During hospitalization, maternal blood glucose levels and the need to adjust insulin dosage are assessed. Careful insulin control in women with gestational diabetes can avoid maternal pancreatic beta-cell exhaustion9 and reduce the risk of future type 2 diabetes.19,21 Regarding the fetus, hyperinsulinization helps achieving the goals of the St. Vincent's Declaration with outcomes of diabetic pregnancy approximating those of non-diabetic pregnancy.16
Frequent hospitalizations can improve maternal and perinatal outcomes but they also increase hospital-related costs. This is a matter of concern for physicians, nurses and other health providers as hospital investments are guided by tools specifically designed for the analysis and control of these costs. The cost is the total sum paid by the hospital for personnel, provisions, facilities and equipment and can be a powerful management tool to evaluate the performance, revenue, and quality of services.1,4
Few studies on the costs of diabetic pregnancies have been conducted. One study assessed the costs of diabetes screening among women with history of gestational diabetes and undergoing a GTT every three years. They found significant cost reduction per case with early detection of diabetes.11 Other authors13 performed a cost analysis of treating pregnant women with diabetes with dietary advice, blood glucose monitoring and insulin therapy as needed compared with routine pregnancy care on both outpatient and inpatient settings. They showed that outpatient costs were US$ 67.43 in the intervention group and US$ 33.68 in the routine care group, whereas inpatient costs were US$ 612.55 and US$ 525.89, respectively. Another study22 showed that insulin therapy had a significant effect on gestational diabetes treatment cost, proving to be a very cost-effective strategy that can reduce additional costs for the treatment of perinatal complications.
This study aimed to compare inpatient and outpatient costs for pregnant/parturient women with diabetes or mild hyperglycemia.
METHODS
This prospective study included all pregnant women with clinical/gestational diabetes or mild hyperglycemia who attended prenatal care at a tertiary perinatal diabetes center in the municipality of Botucatu, southeastern Brazil, in 2007. The study groups comprised diabetic outpatients - women with gestational diabetes mellitus (GDM) and mild hyperglycemia treated with diet alone on an outpatient basis (N = 30); and diabetic inpatients - women with pregestational diabetes taking insulin throughout pregnancy and women with mild hyperglycemia or GDM who, at some point during pregnancy, required insulin therapy in addition to diet (N = 20). The control group consisted of pregnant teenagers (aged 14 to 18 years) who attended prenatal care in an obstetric outpatient clinic of a tertiary hospital in the city of Botucatu in 2007 and showed no concurrent medical or obstetric conditions (N = 18). Pregnant teenagers with no concurrent medical or obstetric conditions were chosen as controls as they are closer to normal pregnant women, considering that this hospital provides care to high-risk pregnant women including pregnant teenagers.
According to the center's protocol, pregnant women with mild hyperglycemia or GDM treated with diet alone were followed up on an outpatient basis; women with pregestational diabetes (all treated with diet plus insulin therapy) and those who required diet plus insulin therapy to control hyperglycemia received in-hospital care for one day (24 hours) on a fortnightly basis until 28 weeks of gestation, and on a weekly basis from week 28 up to delivery. Deliveries took place in 2007 and 2008, when the cost of delivery care was assessed.
Direct, indirect and total costs were prospectively estimated for all pregnant/parturient women in all groups. The difference between the control group and the diabetic and/or hyperglycemic groups was the additional cost attributable to diabetes.
Inclusion criteria were diabetic pregnancy, prenatal care at the study tertiary hospital, no associated conditions, delivery at the study site, prenatal care starting in 2007. Subjects in the control group were pregnant teenagers who had no concurrent medical or obstetric conditions and gave birth at the tertiary hospital.
Pregnant women with diabetes who developed medical problems during pregnancy that could incur excess costs were excluded.
Patients were assessed by a high-risk obstetric team consisting of obstetric specialists, residents, nutritionists and neonatologists. Gestational diabetes screening was positive when fasting blood glucose >90 mg/dL was associated with a risk factor. The diagnosis was established based on a 100-g GTT and blood glucose profile (GP) evaluation. The cutoffs used were those proposed by Carpenter & Coustan3 for GTT, and Gilmer et al8 for blood glucose profile. Patients with abnormal GTT plus normal GP were diagnosed with gestational diabetes while those with normal GTT plus abnormal GP were diagnosed with mild hyperglycemia15 and treated with diet alone as outpatients. Women with abnormal GTT plus abnormal GP, as well as those with pregestational diabetes were hospitalized for one day (24 hours) on a fortnight basis until 28 weeks of gestation, and on a weekly basis from week 28 until delivery, and were treated with diet plus insulin therapy for blood glucose control.2,18 Thus, there were studied two groups: diabetic inpatients and diabetic outpatients.
Pregnant teenagers in the control group were followed up by a team of obstetricians, neonatologists and medical residents following the center's protocol, which is in accordance with the Brazilian Ministry of Health guidelines.ª a Ministério da Saúde (BR). Assistência Pré-Natal: manual técnico. Brasília (DF): Centro de Documentação do MS; 2000. Available from: http://bvsms.saude.gov.br/bvs/publicacoes/cd04_11.pdf In both study groups, pregnancy resolution was determined by a set of maternal and fetal risk factors including suboptimum blood glucose control, poor treatment compliance, fetal macrosomia, abnormal fetal biophysical profile and adverse obstetric history. In general, women with gestational diabetes and those with mild hyperglycemia underwent labor induction after 39 weeks of pregnancy. For subjects with pregestational diabetes, labor induction or pregnancy resolution occurred at most after 37 weeks of gestation whereas among control pregnant teenagers spontaneous onset of labor was awaited up to 10 days after their due date. Newborns received care from the team of neonatologists and, depending on their birth status and gestational age, they were followed up in the rooming-in unit, neonatal intermediate care nursery (NIN) or neonatal intensive care unit (NICU).
Data were collected longitudinally from hospital records for each patient from her first visit or hospital admission to postpartum examination. These data included information on medical and obstetric history, laboratory tests and imaging scans, medications prescribed, and supplies used. Based on the type and amount of these products and services, unit costs were determined according to prices used in public bids. Medications and supplies used during delivery were grouped into kits, namely C-section kit and vaginal delivery kit.
In addition, costs for personnel, telephone services, water supply, sewage services, power supply, general administration and cleaning services for outpatient units, maternity unit and obstetric delivery rooms were determined using the hospital's full costing system. The full costing method allowed to estimating mean cost per visit (annual cost of the outpatient unit divided by the number of visits per year); per day of hospital stay (annual cost of the maternity unit divided by the number of hospital stays per year); and per delivery either cesarean section or vaginal (annual cost of the obstetric delivery rooms divided by the number of deliveries per year).
The costs obtained from hospital records as well as those determined by the full costing method were categorizes as direct and indirect costs. Direct costs were those related to medications, laboratory tests, imaging scans, supplies and personnel. Indirect costs were those related to water supply, sewage services, power supply, telephone services, general administration and cleaning services.
Both direct and indirect costs were expressed in dollar values for the year 2009 (US$ 1.00 = R$ 1.97).
First, the costs per mother were calculated. Then, mean and standard deviations were estimated for each group of pregnant women.
In order to calculate the cost of diabetes during pregnancy, the costs of prenatal care (visits and/or hospital stays during pregnancy), delivery and postpartum care (hospitalization) were estimated using the formulae as shown below, which were previously defined for this study:
Prenatal, delivery and postpartum care cost in the three groups were compared by applying the Kruskal-Wallis test for independent samples following the Shapiro-Wilk test to check the probability distribution of the study variables. The significance level was set at 5% (p<0.05) for all tests.
The study was approved by the Research Ethics Committee of Botucatu Medical School, Universidade Estadual Paulista Julio de Mesquita Filho (number 493/2007).
RESULTS
Table 1 shows mean and total direct and indirect costs of prenatal care for pregnant inpatients and outpatients with diabetes or mild hyperglycemia and pregnant teenagers. Direct and indirect prenatal care costs were US$ 187.84 per diabetic inpatient, US$ 53.43 per diabetic outpatient and US$ 46.51 per teenager. Considering the number of prenatal visits per patient, total prenatal care cost was US$ 2,160.18 per diabetic inpatient, US$ 341.95 per diabetic outpatient and US$ 381.40 per teenager. Both total and unit costs of prenatal care were significantly higher among diabetic inpatients than diabetic outpatients and teenagers.
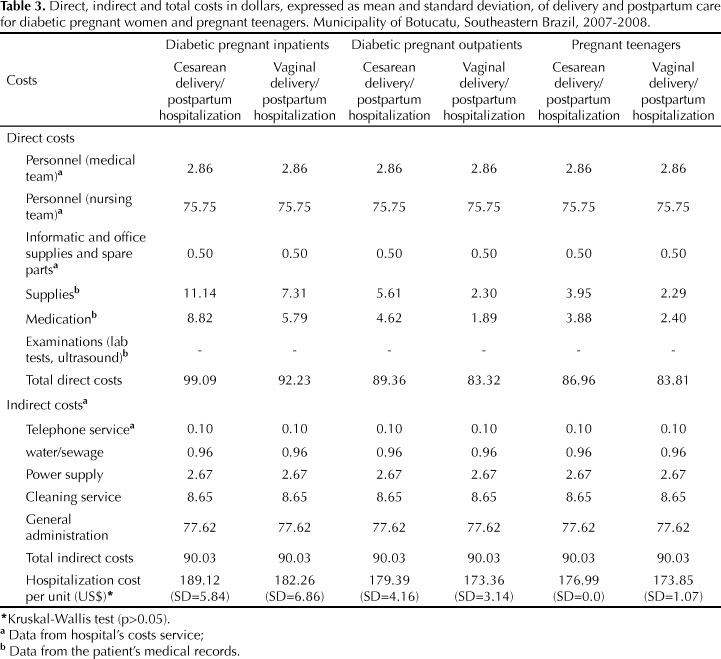
Direct and indirect as well as mean and total delivery costs (cesarean or vaginal) in all three groups are shown in Table 2. Considering that full costing is the method used for cost estimation, direct and indirect costs of cesarean and vaginal deliveries were the same except for supplies and medications, which varied according to delivery mode. Thus, the costs of cesarean and vaginal deliveries as estimated by the full costing method are similar.
Taking into account the rates of cesarean and vaginal deliveries in each group, mean delivery cost was US$ 346.68 for diabetic inpatients, US$ 344.28 for diabetic outpatients and US$ 340.00 for teenagers. Using the full costing method, there was no significant difference in total and mean delivery costs among the groups studied.
Table 3 shows mean and total direct and indirect costs of delivery/postpartum hospitalization in all groups. The cost of cesarean delivery/postpartum hospitalization/day was US$ 189.12 per diabetic inpatient, US$ 179.39 per diabetic outpatient, and US$ 176.99 per pregnant teenager. Total cost of vaginal delivery/postpartum hospitalization/day was US$ 182.26 per diabetic inpatient, US$ 173.36 per diabetic outpatient, and US$ 173.85 per teenager. As the full costing method was used for estimation, no statistical difference was seen among these values.
For the institution, total pregnancy/cesarean delivery/postpartum cost was US$ 3,417.10 per diabetic inpatient, US$ 1,481.24 per diabetic outpatient, and U$ 1,439.26 per teenager, whereas total pregnancy/vaginal delivery/postpartum cost was US$ 3,066.23 per diabetic inpatient, US$ 1,289.24 per diabetic outpatient, and US$ 1,259.76 per teenager (Table 4).
Total prenatal care and total delivery/postpartum costs were significantly higher in the group of diabetic pregnant inpatients.
The mean total cost of pregnancy, delivery and postpartum care was 2.6-fold higher among diabetic pregnant inpatients than among pregnant teenagers, and 2.42-fold higher than among diabetic pregnant outpatients. No statistical difference was seen between outpatient and control groups.
The additional cost attributable to diabetes was US$ 2,042.10 among inpatients and US$ 96.30 among outpatients.
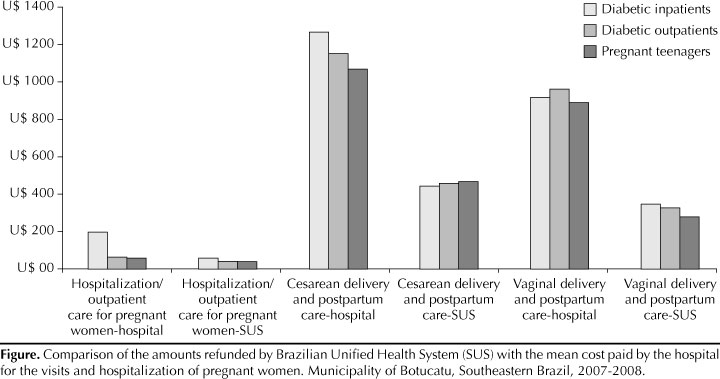
The Figure shows that the costs of both prenatal (hospitalization/visits during pregnancy) and delivery/postpartum care (cesarean and vaginal deliveries) were higher than the amounts reimbursed by the Brazilian Unified Health System (Sistema Único de Saúde - SUS).
DISCUSSION
Hospitalization was a major factor contributing to increasing costs of health care to diabetic pregnant women.
The mean cost of prenatal-delivery-postpartum care for diabetic pregnant women on an outpatient basis was 8% higher than that for pregnant teenagers. The slight difference seen among groups may be explained by the mean number of outpatient visits, 6.4 visits per diabetic woman and 8.2 per teenager during prenatal care. The small number of visits per diabetic woman in the outpatient group is explained by the fact that these women started receiving specific prenatal care after GDM was diagnosed around 24-28 weeks of gestation.2,19
The excess cost of care for diabetic pregnant women managed by hospitalization is due not only to hospitalization costs during pregnancy but also to a higher rate of cesareans in this group (70.0%). In fact, the costs of delivery and day of hospitalization for delivery and postpartum care were similar in all groups as they were estimated by the full costing method. However, there was a greater number of hospitalization days for cesarean (4.8) than for vaginal delivery (3.1).
These data show the advantage of managing diabetic pregnancies in an outpatient setting, introducing and encouraging self-monitoring of blood glucose levels and blood glucose control with reflectance meters according to the literature recommendations from the 1980s.5,7,20
In our study the diabetes was managed according to its severity: women with gestational diabetes or mild hyperglycemia were treated with diet on an outpatient setting while those with pregestational diabetes, GDM or mild hyperglycemia receiving insulin therapy were frequently hospitalized during pregnancy. Given that maternal and perinatal outcomes of diabetes-complicated pregnancies among women treated as outpatients have been demonstrated to be similar to those seen among women treated as inpatients,6,14,22 a study comparing the costs of these different management protocols is needed to determine whether outpatient management is cost-effective in pregnant women with diabetes of varying degrees of severity treated with diet or insulin therapy.14,22
Outpatient management has been demonstrated to be as effective as hospitalization with regard to blood glucose control. In addition, it is particularly advantageous in terms of quality of life. It prevents psychological, mental and social stress of in-hospital care; prevents the disruption caused in the family by hospitalization, and allows pregnant women to continue working. Furthermore, home glucose monitoring reflects true ambient blood glucose control and allows patients to play an active role in their care. All these advantages are associated with a reduction in the costs of diabetes in pregnancy, but they should be interpreted with caution. The outcomes of outpatient care are similar to those observed with hospital management, but the former is more convenient for the patient and lowers treatment costs.14
The amount reimbursed by SUS is quite below the estimated cost incurred by the study hospital for both inpatient and outpatient care during pregnancy as well as through delivery and postpartum. The additional cost of this specialized care is covered by the university institution that runs the hospital. The difference between the amount paid by the institution and that reimbursed by SUS corresponds to the resources invested by the university in teaching, research, and community services.
Overall, the study analysis pointed to strategies that should be implemented at all levels: the hospital's Perinatal Diabetes Research Center should carried out a randomized prospective controlled study to compare the effectiveness of outpatient and hospitalization management in diabetic pregnant women regardless of disease severity; there should be a reduction of cesarean rates in diabetic women, as well as the number of days in hospital after birth, to lower costs; SUS should review health care costs and increase its budget for disease treatment.
In conclusion, diabetes in pregnancy increases medical care cost. The highest costs were associated with medical cases requiring hospital treatment. Direct and indirect costs as well as total cost of prenatal care were higher in diabetic inpatients; direct, indirect and total costs of delivery care (cesarean and vaginal) and delivery-postpartum hospitalization were similar in all groups. Thus, total costs of prenatal, delivery and postpartum care were significantly higher among diabetic pregnant inpatients. The additional cost attributable to diabetes was higher among inpatients than outpatients. The costs of prenatal and delivery/postpartum care of hospitalization and visits during pregnancy were higher than the amounts reimbursed by SUS.
Received: 8/3/2010
Approved: 9/25/2011
Paper based on the doctoral thesis by Cavassini ACM, presented to the Graduate Program in Gynecology, Obstetrics and Mastology of Botucatu Medical School, Unesp, Botucatu, São Paulo, in 2009.
The authors declare that there are no conflicts of interests.
- 1. Asevedo FMF, Koch HA. Avaliação dos custos para implantação de um serviço de mamografia. Radiol Bras 2004;37(2):101-5. DOI:10.1590/S0100-39842004000200007
- 2. Ayach W, Costa RAA, Calderon IMP, Rudge MVC. Comparison between 100-g glucose tolerance test and two other screening tests for gestacional diabetes: combined fasting glucose with risk factors and 50-g glucose tolerance test. Sao Paulo Med J 2006;124(1):4-9. DOI:10.1590/S1516-31802006000100002
- 3. Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 1982;144(7):768-73.
- 4. Castilho V, Fugulin FMT, Gaidzinski RR. Gerenciamento de custos nos serviços de enfermagem. In: Kurcgant P, coordenadora. Gerenciamento em enfermagem. Rio de Janeiro: Guanabara Koogan; 2005. p.171-83.
- 5. Cousins L. The California Diabetes and Pregnancy Program: a statewide collaborative program for the pre-conception and prenatal care of diabetic women. Baillieres Clin Obstet Gynecol1991;5(2):443-59.
- 6. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GDF, et al. Williams obstetrics. 20.ed. Norwalk: Appleton & Lange; 1997.
- 7. Dicker D, Feldberg D, Yeshaya A, Peleg D, Karp M, Goldman JA. Fetal surveillance in insulin-dependent diabetic pregnancy: predictive value of the biophysical profile. Am J Obstet Gynecol 1988;159(4):800-4.
- 8. Gilmer MDG, Beard RW, Brooke FM, Oakley NW. Carbohydrate metabolism in pregnancy. Part I. Diurnal plasma glucose profile in normal and diabetic women. Br Med J 1975;3(5980):399-402.
- 9. Guyton AC, Hall JE. Tratado de fisiologia médica. 10. ed. Rio de Janeiro: Guanabara Koogan; 2002. cap.78, p.827-39.
- 10. Gyves MT, Rodman HM, Little AB, Fanaroff AA, Merkatz IR. A modern approach to management of pregnant diabetics: a two year analysis of perinatal outcomes. Am J Obstet Gynecol. 1977;128(6):606-16.
- 11. Kim C, Herman WH, Vijan S. Efficacy and cost of postpartum screening strategies for diabetes among women with histories of gestacional diabetes mellitus. Diabetes Care 2007;30(5):1102-6. DOI:10.2337/dc06-2237
- 12. Kitzmiller JL, Jovanovic L. Insulin therapy in pregnancy. In: Hod M, Jovanovic L, Di Renzo GC, Leiva A, Langer O, editors. Textbook of diabetes and pregnancy. London: Martin Dunitz; 2003. cap.27, p.359-78.
- 13. Moss JR, Crowther CA, Hiller JE, Willson KJ, Robinson JS; Australian Carbohydrate Intolerance Study in Pregnant Women Group. Costs and consequences of treatment for mild gestational diabetes mellitus: evaluation from the ACHOIS randomised trial. BMC Pregnancy Childbirth. 2007;7:27. DOI:10.1186/1471-2393-7-27
- 14. Nachum Z, Ben-Shlomo I, Weiner E, Ben-Ami M, Shalev E. Diabetes in pregnancy: efficacy and cost of hospitalization as compared with ambulatory management: a prospective controlled study. Isr Med Assoc J 2001;3(12):915-9.
- 15. Negrato CA, Jovanovic L, Tambascia MA, Calderon IMP, Geloneze B, Dias A, et al. Mild gestational hyperglycaemia as a risk factor for metabolic syndrome in pregnancy and adverse perinatal outcomes. Diabetes Metab Res Rev 2008;24(4):324-30. DOI:10.1002/dmrr.815
- 16. Pallardo F, Herranz L, Garcia-Ingelmo T, Grande C, Martin-Vaquero P, Janez M, et al. Early postpartum metabolic assessment in women with prior gestational diabetes. Diabetes Care 1999;22(7):1053-8.
- 17. Rudge MVC, Peraçoli JC, Berezowski AT, Calderon IMP, Brasil MAM. The oral glucose tolerance test is a poor predictor of hyperglycaemia during pregnancy. Braz J Med Biol Res 1990;23(11):1079-89.
- 18. Rudge MVC, Calderon IMP, Ramos MD, Suetake H, Peraçoli JC. Investigação diagnóstica do diabetes na gestação. Rev Bras Ginecol Obstet 1996;18(1):21-6.
- 19. Rudge MVC, Calderon IMP, Ramos MD, Brasil MAM, Rugolo LMSS, Bossolan G, et al. Hiperglicemia materna diária diagnosticada pelo perfil glicêmico: um problema de saúde pública materno e perinatal. Rev Bras Ginecol Obstet 2005;27(11):691-7. DOI:10.1590/S0100-72032005001100010
- 20. Schneider JM, Curet LB, Olson RW, Shay G. Ambulatory care of the pregnant diabetic. Obstet Gynecol 1980;56(2):144-9.
- 21. Silva MRG, Calderon IMP, Gonçalves LC, Aragon FF, Padovani CR, Pimenta WP. Ocorrência de diabetes melito em mulheres com hiperglicemia em gestação prévia. Rev Saude Publica 2003;37(3):345-50. DOI:10.1590/S0034-89102003000300013
- 22. Todorova K, Palaveev O, Petkova VB, Stefanova M, Dimitrova ZL. A pharmacoeconomical model for choice of a treatment for pregnant women with gestational diabetes. Acta Diabetol 2007;44(33):144-8. DOI:10.1007/s00592-007-0255-5
Correspondence:
Publication Dates
-
Publication in this collection
03 Feb 2012 -
Date of issue
Apr 2012
History
-
Received
08 Mar 2010 -
Accepted
25 Sept 2011