Abstracts
Tuberculosis (TB) is a current public health problem, remaining the most common worldwide cause of mortality from infectious disease. Recent studies indicate that genitourinary TB is the third most common form of extra-pulmonary disease. The diagnosis of renal TB can be hypothesized in a non-specific bacterial cystitis associated with a therapeutic failure or a urinalysis with a persistent leukocyturia in the absence of bacteriuria. We report on the case of a 33-year-old man who presented on admission end stage renal disease (ESRD) secondary to renal TB and a past history of pulmonary TB with important radiologic findings. The diagnosis was based on clinical findings despite all cultures being negative. Empiric treatment with tuberculostatic drugs was started and the patient became stable. He was discharged with no symptom, but without renal function recovery. He is on maintenance hemodialysis three times a week. TB is an important cause of kidney disease and can lead to irreversible renal function loss.
Renal tuberculosis; Tuberculosis; Obstructive uropathy; Extra-pulmonary tuberculosis; End-stage kidney disease
A tuberculose (TB) é um problema atual de saúde pública, persistindo como a causa mais comum de óbito por doenças infecciosas. Estudos recentes indicam que a TB genitourinária é a terceira forma mais comum de doença extra-pulmonar. O diagnóstico da TB renal pode ser suspeito na presença de cistite bacteriana não-específica associada a falha terapêutica ou com exame de urina apresentando leucocitúria persistente na ausência de bacteriúria. Relatamos o caso de um paciente de 33 anos, sexo masculino, que apresentou na admissão insuficiência renal crônica terminal secundária à TB renal, que tinha história prévia de TB pulmonar, com importantes achados radiológicos. O diagnóstico foi baseado nos achados clínicos apesar de todas as culturas terem sido negativas. Tratamento empírico com drogas tuberculostáticas foi iniciado e o paciente evoluiu estável. Foi de alta assintomático, mas sem recuperação da função renal. Ele encontra-se em hemodiálise três vezes por semana. A TB é uma causa importante de doença renal e pode levar à perda irreversível da função renal.
CASE REPORT
Review of genitourinary tuberculosis with focus on end-stage renal disease
Revisão acerca da tuberculose genitourinária com foco na insuficiência renal crônica terminal
Neiberg A. LimaI; Carol C. VasconcelosII; Pedro Henrique O. FilgueiraIII; Meissa KretzmannIII; Ticiano A. S. SindeauxIII; Beni Feitosa NetoI; Geraldo B. Silva JuniorIII,IV; Elizabeth F. DaherI,III
IDivision of Nephrology, Hospital Geral de Fortaleza, Fortaleza, Ceará, Brazil
IIDivision of Radiology, UDI, Teresina, Piauí, Brazil
IIIDepartment of Internal Medicine, School of Medicine, Federal University of Ceará, Fortaleza, Ceará, Brazil
IVSchool of Medicine, Health Sciences Center, University of Fortaleza, Fortaleza, Ceará, Brazil
Correspondence to Correspondence to: Elizabeth De Francesco Daher Rua Vicente Linhares 1198, 60270-135 Fortaleza, CE, Brasil. E-mail: ef.daher@uol.com.br, geraldobezerrajr@yahoo.com.br
ABSTRACT
Tuberculosis (TB) is a current public health problem, remaining the most common worldwide cause of mortality from infectious disease. Recent studies indicate that genitourinary TB is the third most common form of extra-pulmonary disease. The diagnosis of renal TB can be hypothesized in a non-specific bacterial cystitis associated with a therapeutic failure or a urinalysis with a persistent leukocyturia in the absence of bacteriuria. We report on the case of a 33-year-old man who presented on admission end stage renal disease (ESRD) secondary to renal TB and a past history of pulmonary TB with important radiologic findings. The diagnosis was based on clinical findings despite all cultures being negative. Empiric treatment with tuberculostatic drugs was started and the patient became stable. He was discharged with no symptom, but without renal function recovery. He is on maintenance hemodialysis three times a week. TB is an important cause of kidney disease and can lead to irreversible renal function loss.
Keywords: Renal tuberculosis; Tuberculosis; Obstructive uropathy; Extra-pulmonary tuberculosis; End-stage kidney disease.
RESUMO
A tuberculose (TB) é um problema atual de saúde pública, persistindo como a causa mais comum de óbito por doenças infecciosas. Estudos recentes indicam que a TB genitourinária é a terceira forma mais comum de doença extra-pulmonar. O diagnóstico da TB renal pode ser suspeito na presença de cistite bacteriana não-específica associada a falha terapêutica ou com exame de urina apresentando leucocitúria persistente na ausência de bacteriúria. Relatamos o caso de um paciente de 33 anos, sexo masculino, que apresentou na admissão insuficiência renal crônica terminal secundária à TB renal, que tinha história prévia de TB pulmonar, com importantes achados radiológicos. O diagnóstico foi baseado nos achados clínicos apesar de todas as culturas terem sido negativas. Tratamento empírico com drogas tuberculostáticas foi iniciado e o paciente evoluiu estável. Foi de alta assintomático, mas sem recuperação da função renal. Ele encontra-se em hemodiálise três vezes por semana. A TB é uma causa importante de doença renal e pode levar à perda irreversível da função renal.
INTRODUCTION
Tuberculosis (TB) is a current public health problem, remaining the most common worldwide cause of mortality from infectious disease, with an estimated global incidence of 8 to 10 million/year7,9,10,16,22.
The difficulty in diagnosing extra-pulmonary tuberculosis can be attributed to the poor access of disseminated lesions, the fact of patients being usually paucibacillary (very often causing a negative smear), histopathologic findings are not pathognomonic (granulomatous reaction can be found in other diseases) and there are lower rates of bacteriological positivity (only in a quarter of the cases)14. The diagnosis of renal TB can be hypothesized in the setting of non-specific bacterial cystitis associated with a therapeutic failure or a urinalysis with a persistent leukocyturia and absence of bacteriuria1,7,14,18.
Most extra-pulmonary forms of TB are seen in organs without optimum conditions for bacterial growth, generally with an insidious onset and a chronic evolution14. Recent studies indicate that genitourinary TB is the third most common form of extra-pulmonary disease after peripheral lymphadenopathy7,10,21.
The occurrence of extra-pulmonary TB is not common in HIV-negative patients, and the development of end-stage kidney disease caused by TB is even less common, being rarely reported in medical literature5,7,17. Following the patient's consent, we report on the case of a young man with a past history of pulmonary TB treated for six months with rifampicin, isoniazid and pyrazinamide (RIP), who presented on admission ESRD secondary to renal TB.
CASE REPORT
A 33-year-old man was admitted to the emergency room with symptoms of fatigue, anorexia, nausea, vomiting, progressive dyspnea at rest, orthopnea, paroxysmal nocturnal dyspnea and ascending edema of the legs initiated two months before the admission. He also had a history of mild to moderate chronic flank pain initiated three years before admission which radiated to lower quadrants of the abdomen, was intermittent, arising one to two times per month. His past history showed a diagnosis of pulmonary tuberculosis treated during a six month period two and a half years before admission, past habits of alcohol intake (one liter of distillated drinks per day) and tobacco (24 packets per year) and mild weight loss.
At physical examination he was pale (3+/4+), tachypneic, and had a blood pressure of 160 x 100 mmHg. He also had at auscultation a pancardiac systolic murmur (2+/6+), diffuse crackles in both hemithorax and edema of the legs (3+/4+). Complementary exams showed negative serologies (Anti-HBc, HBsAg, anti-HCV, VDRL and anti-HIV); hemoglobin 4.6g/dL; hematocrit 14.5%; white blood count 1140/mm3; platelets 261000/mm3; BUN 273 mg/dL; creatinine 13.6 mg/dL; bicarbonate 21 mEq/L (ref. 24-26 mEq/L); sodium 138 mEq/L (ref. 135‑145 mEq/L); potassium 5.5 mEq/L (ref. 3.5-5.0 mEq/L); total calcium 7.1 mg/dL (ref. 8.4-9.5 mg/dL); phosphorus 11.4 mEq/L (ref. 2.5-4.5 mEq/L) and PTH 1715 pg/mL (ref. 150-300 pg/mL). He also presented oliguria (400 mL/24h) and hemodialysis was immediately initiated. Anemia was considered as consequence of chronic kidney disease. The investigation for ferropenic and other anemias were negative. Treatment began with blood transfusion and erythropoietin.
Urinalysis demonstrated urinary pH 6.0; leucocytes 1+; protein 4+; erythrocytes 3+; uncountable leucocitary casts and negative culture of the urine for pyogenic agents. Renal ultrasound showed a small right kidney (7.5 x 4.5 x 5.8 cm), left kidney with increased dimensions (12 x 5.8 x 5.8 cm), bilateral nephrolithiasis, left hydronephrosis with parenchyma reduction and a complex right cyst with peripheral calcifications.
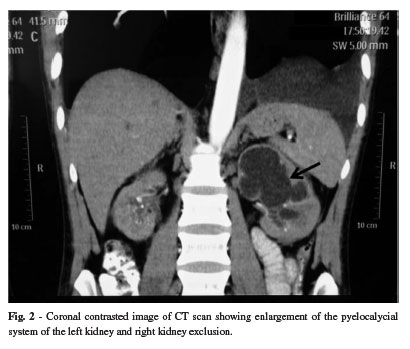
Once primary radiographic exams were altered, computed tomographies of the abdomen and thorax were performed (Figs. 1 and 2) which evidenced alterations compatible with tuberculosis. With the hypothesis of disseminated tuberculosis, cutaneous tuberculin test was performed (17 mm), ten samples of urine for mycobacteria culture, bronchoscopy with culture for Koch bacilli from the bronchoalveolar lavage and thoracocentesis with pleural biopsy were obtained. All mycobacterial cultures were negative.
During the follow-up, renal and pleural extra-pulmonary tuberculosis were considered as the main possible diagnosis for the case. The Light's criterion of the pleural fluid was compatible with exudate and Adenosine Deaminase of 50 U/L, and empiric treatment was initiated with tuberculostatic agents adjusted according to the Brazilian guidelines for TB. The patient became stable and was discharged with no symptom, but without renal function recovery. He is on maintenance hemodialysis three times a week.
DISCUSSION
During the initial primary pulmonary infection, the M. tuberculosis organisms multiply and evoke an inflammatory reaction. As there is still little host defense to the multiplication of the bacteria at this stage, rapid spreading occurs, through the lymphatics and blood stream. Within about four weeks, however, the rate of multiplication decreases as the host response develops and the dissemination ceases20. Genitourinary TB is usually caused by metastatic spread of organisms through the blood stream during the initial infection. Active disease results from the reactivation of the initial infection20.
In this case, the patient had bilateral renal involvement. Tuberculosis may involve the kidney as part of generalized disseminated infection or as localized genitourinary disease. The kidney is usually infected by the hematogenous spread of bacilli from the focus of infection in the lungs and/or bowel. Clinically, renal tuberculosis usually presents unilaterally, but post mortem studies showed that the disease was often bilateral. The healing process results in fibrous tissue and calcium salts being deposited, producing the classic calcified lesion20.
Our patient reported ejaculation with minimal volume, probably due to genital involvement, which is a possible occurrence in cases of disseminated tuberculosis. Genital tuberculosis in males most commonly involves the epididymis followed by the prostate. Tuberculous epididymitis probably is a result of blood-borne infection because it is often an isolated finding without urinary tract involvement. It is important to be aware that a high proportion of men with genital tuberculosis (50 - 75%) have radiologic abnormalities in the urinary tract, which did not happen in this case once the ultrasonography of the genital region was normal. The urinary tract of such patients with primary location of tuberculous infection on the epididymis should be investigated13.
He had a past history of pulmonary tuberculosis, which was treated over a six month period. The knowledge of tuberculosis infection early in life either as primary pulmonary manifestation or as an extra-pulmonary manifestation provides an important clue in a large number of cases. One has to be aware that the latency between pulmonary manifestation and genitourinary TB is enormous. In some cases, it could take more than 30 years before genitourinary TB becomes evident13.
The diagnosis was possible because the ADA pleural fluid and radiological injuries were compatible, despite cultures being negative. Also, the typical sterile pyuria was found and skin tests were strongly positive. The most common laboratory abnormalities are pyuria, albuminuria, and hematuria. Seventy five percent of patients have an abnormal chest roentgenogram on admission. Eighty eight percent of patients tested have positive skin tests and sixty three percent tested have abnormal excretory urography. Sixteen percent show renal calcification3.
The diagnosis of genitourinary TB can be based on culture studies. At least three, but preferably five, consecutive early morning specimens of urine should be cultured on Lowenstein-Jensen medium to isolate M. tuberculosis23.
The diagnosis of TB on images of the urinary tract depends on the stage of the infection. Tubercular granulomas in the renal pyramids coalesce to form ulcers which discharge mycobacteria and pus in the urine. Untreated lesions enlarge and a tubercular abscess may form in the parenchyma. Later on, perinephric abscess is formed and the kidney is replaced by caseous material ("putty kidney") which may become calcified ("cement kidney") and nonfunctional leading to renal failure9.
Approximately 75% of renal tuberculosis involvement is unilateral, but in our patient we could find involvement in both kidneys24. The collecting system is the most common site of genitourinary TB. In the early stage of urinary TB, few calices are involved and only papillary necrosis or calyceal deformity is depicted on imaging studies. Fibrosis occurring after healing of acute inflammation results in multifocal strictures19.
The most characteristic imaging finding of urinary TB is uneven caliectasis. It is caused by the varying degree of fibrosis and obstruction at various sites. Our case did not show radiological features of papillary necrosis, but a thickening of the ureteral wall to the right, an important caliceal dilation and distortion mainly associated with a left cortical thinning (Figs. 1 and 2).
When the renal pelvis and ureter are affected by TB, hydronephrosis becomes severe. The involved segments show wall thickening and enhancement on CT and MRI. In patients with healed or chronic TB, calcifications may be noted. Renal calcifications are a common manifestation of TB at conventional radiography, occurring in 24% to 44% of patients. In our patient, we were able to see outlying calcifications in both kidneys as is quoted in the literature12. Extensive parenchymal calcification in a nonfunctioning, autonephrectomized kidney is characteristic of end-stage TB.
The differential diagnosis for the imaging appearance of renal tuberculosis includes chronic pyelonephritis, papillary necrosis, medullary sponge kidney, caliceal diverticulum, renal cell carcinoma, transitional cell carcinoma, and xanthogranulomatous pyelonephritis. The most valuable radiologic feature of genitourinary TB is the multiplicity of abnormal findings. Whenever a pattern of chronic renal inflammatory disease is recognized, particularly in the setting of periureteric or peripelvic fibrosis, tuberculosis must be considered9.
Cavitation, the hallmark of post-primary TB, affects about 50% of patients. The cavities typically have thick, irregular walls, which become smooth and thin with successful treatment. Cavities are usually multiple and occur within areas of consolidation. Resolution can result in emphysematous change or scarring. The minority of the cavities demonstrates air-fluid levels; however, these findings can indicate the presence of superinfection15.
If there is airway disease and, in particular, endobronchial spread of infection, tree-in-bud opacities may develop. These findings, which are usually visible in the lung periphery and resemble a branching tree with buds at the tips of the branches, are indicative of active tuberculosis. Lymphadenopathy and pneumothoraces are seen in only about 5% of patients15.
Airway involvement is characterized by bronchial stenosis, leading to lobar collapse or hyperinflation, obstructive pneumonia, and mucoid impaction. Bronchial stenosis is seen in 10% - 40% of patients with active TB15 and is best demonstrated with CT, which usually shows long segment narrowing with irregular wall thickening, luminal obstruction, and extrinsic compression4. It also results in tree-in-bud opacities and traction bronchiectasis, particularly of the upper lobes. Pleural effusions occur most often in primary TB but are seen in approximately 18% of post-primary cases and they are usually small.
High resolution tomographic findings of our patient demonstrated parenchymal bands, traction bronchiectasis with cavities in between, center-lobular emphysema, reduced volume of the upper lobes and extensive left pleural thickening. These findings are consistent with chronic TB and revealed no signs of exacerbation2.
The patient was managed with dialysis, therapy for heart failure and specific pharmacological treatment for TB. The chemotherapy regimen was instituted according to the Brazilian guidelines for the treatment of TB. He left the hospital with control of his symptoms to finish treatment during six months.
In summary, renal TB is an important cause of kidney disease, mainly in tropical areas of the globe, and can lead to end-stage renal disease if not diagnosed early and treated correctly.
Received: 04 July 2011
Accepted: 28 November 2011
- 1. Afiune JB. Tuberculose extrapulmonar. In: Veronesi R, Focaccia R, editores. Tratado de infectologia. 2. ed. Săo Paulo: Atheneu; 2002. p. 964-9.
- 2. Burrill J, Williams CJ, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis: a radiologic review. Radiographics. 2007;27:1255-73.
- 3. Christensen WI. Genitourinary tuberculosis: review of 102 cases. Medicine (Baltimore). 1974;53:377-90.
- 4. Curvo-Semedo L, Teixeira L, Caseiro-Alves F. Tuberculosis of the chest. Eur J Radiol. 2005;55:158-72.
- 5. Daher EF, Silva Júnior GB, Damasceno RT, Santos GM, Corsino GA, Silva SL, et al. End-stage renal disease due to delayed diagnosis of renal tuberculosis: a fatal case report. Braz J Infect Dis. 2007;11:169-71.
- 6. Davidson AJ, Hartman DS, Choyke PL, Wagner BJ. Parenchymal disease with normal size and contour. In: Davidson AJ, editor. Davidson's radiology of the kidney and genitourinary tract. 3rd ed. Philadelphia: Saunders; 1999. p. 327-58.
- 7. Eastwood JB, Corbishley CM, Grange JM. Tuberculosis and the kidney. J Am Soc Nephrol. 2001;12:1307-14.
- 8. Engin G, Acunas B, Acunas G, Tunaci M. Imaging of extrapulmonary tuberculosis. Radiographics. 2000;20:471-88.
- 9. Gibson MS, Puckett ML, Shelly ME. Renal tuberculosis. Radiographics. 2004;24:251-6.
- 10. Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005;72:1761-8.
- 11. Jung YY, Kim JK, Cho KS. Genitourinary tuberculosis: comprehensive cross-sectional imaging. AJR Am J Roentgenol. 2005;184:143-50.
- 12. Kollins SA, Hartman GW, Carr DT, Segura JW, Hattery RR. Roentgenographic findings in urinary tract tuberculosis: a 10 year review. Am J Roentgenol Radium Ther Nucl Med. 1974;121:487-99.
- 13. Lenk S, Schroeder J. Genitourinary tuberculosis. Curr Opin Urol. 2001;11: 93-8.
- 14. Lopes AJ, Capone D, Mogami R, Tessarollo B, Cunha DL, Capone RB, et al. Tuberculose extrapulmonar: aspectos clínicos e de imagem. Pulmăo RJ. 2006;15:253-61.
- 15. McAdams HP, Erasmus J, Winter JA. Radiologic manifestations of pulmonary tuberculosis. Radiol Clin North Am. 1995;33:655-78.
- 16. Muttarak M, Chiang Mai WN, Lojanapiwat B. Tuberculosis of the genitourinary tract: imaging features with pathological correlation. Singapore Med J. 2005;46:568-75.
- 17. Oliveira JL, Silva Junior GB, Daher EF. Tuberculosis-associated chronic kidney disease. Am J Trop Med Hyg. 2011;84:843-4.
- 18. Rose BD. Renal disease in tuberculosis. UpToDate, 2002. Available from: http://www.uptodate.com/contents/renal-disease-in-tuberculosis
- 19. Wang LJ, Wong YC, Chen CJ, Lim KE. CT features of genitourinary tuberculosis. J Comput Assist Tomogr. 1997;21:254-8.
- 20. Warren D, Johnson JR, Johnson CW, Lowe FC. Genitourinary tuberculosis. In: Walsh PC, editor. Campbell's Urology. 8th ed. Philadelphia: Saunders; 2002.
- 21. Wise GJ, Marella VK. Genitourinary manifestations of tuberculosis. Urol Clin North Am. 2003;30:111-21.
- 22. World Health Organization. Global tuberculosis control: WHO report 1998. Geneva, WHO; 1998.
- 23. World Health Organization. Treatment of tuberculosis: guidelines for national programmes. 3rd ed. Geneva: WHO; 2003.
- 24. Zissin R, Gayer G, Chowers M, Shapiro-Feinberg M, Kots E, Hertz M. Computerized tomography findings of abdominal tuberculosis: report of 19 cases. Isr Med Assoc J. 2001;3:414-18.
Publication Dates
-
Publication in this collection
23 Feb 2012 -
Date of issue
Feb 2012
History
-
Received
04 July 2011 -
Accepted
28 Nov 2011