Abstracts
Infrapopliteal mycotic aneurysm resulting from endocarditis is rare, with only a few reported cases. We describe the case of a 28-year-old male patient who was suffering with pain and edema in the right leg. The ultrasound revealed an aneurysm of the right tibioperoneal trunk and a deep vein thrombosis (DVT). The patient was admitted and developed acute congestive heart failure, being diagnosed with possible endocarditis. A pseudo-aneurysm was revealed by arteriography. Aggressive antibiotic treatment was initiated, and open surgery confirmed a mycotic pseudo-aneurysm of the tibioperoneal trunk. To our knowledge, this is the 8th case reported of an infected aneurysm in this particular location.
Aneurysm; Infected; Tibial arteries; Endocarditis; Venous thrombosis; Review
Aneurisma micótico infra-poplíteo resultante de endocardite infecciosa é raro, com apenas alguns casos relatados. Descrevemos o caso de um paciente de 28 anos do sexo masculino que apresentou dor e edema na perna direita. A ultrassonografia demonstrou um aneurisma do tronco tíbio-fibular e trombose venosa profunda do membro inferior direito. O paciente foi internado e desenvolveu falência cardíaca aguda, sendo diagnosticado de endocardite bacteriana. Um pseudo-aneurisma foi evidenciado na arteriografia. Antibioticoterapia agressiva foi iniciada e cirurgia aberta confirmou um pseudo-aneurisma micótico do tronco tibio-fibular. Para o nosso conhecimento, este é o oitavo caso relatado de aneurisma infectado localizado especificamente nesta região.
CASE REPORT
Mycotic aneurysm of the tibioperoneal trunk: a first manifestation of an infected endocarditis
Aneurisma micótico de tronco tíbio-fibular: a primeira manifestação de uma endocardite infecciosa
Sergio Quilici BelczakI; Igor Rafael SincosII; Marcelo Passos TeivelisIII; Carlos Alberto Sian de OliveiraIII; Hélio FragosoIV; Ricardo AunV
IHCFMUSP, Doutor pela Faculdade de Medicina da Universidade de São Paulo, Docente da disciplina de Cirurgia Vascular da Faculdade São Camilo, Chefe do Serviço de Cirurgia Vascular do Hospital Geral de Carapicuiba
IIHCFMUSP, Docente da disciplina de Cirurgia Vascular da Faculdade São Camilo, Chefe do Serviço de Cirurgia Vascular do Hospital Geral de Carapicuiba
IIIHCFMUSP, Residente do Serviço de Cirurgia Vascular do Hospital das Clínicas da Universidade de São Paulo
IVHospital Geral de Carapicuíba, Chefe do Serviço de Cirurgia Geral do Hospital Geral de Carapicuíba
VHCFMUSP, Professor de Cirugia Vascular da Faculdade de Medicina da Universidade de São Paulo, Chefe do Serviço de Cirurgia Vascular e Endovascular do Prof. Dr. Ricardo Aun do Hospital Israelita Albert Einstein
Correspondence to Correspondence to: Sergio Quilici Belczak. E-mail: belczak@gmail.com
SUMMARY
Infrapopliteal mycotic aneurysm resulting from endocarditis is rare, with only a few reported cases. We describe the case of a 28-year-old male patient who was suffering with pain and edema in the right leg. The ultrasound revealed an aneurysm of the right tibioperoneal trunk and a deep vein thrombosis (DVT). The patient was admitted and developed acute congestive heart failure, being diagnosed with possible endocarditis. A pseudo-aneurysm was revealed by arteriography. Aggressive antibiotic treatment was initiated, and open surgery confirmed a mycotic pseudo-aneurysm of the tibioperoneal trunk. To our knowledge, this is the 8th case reported of an infected aneurysm in this particular location.
Keywords: Aneurysm; Infected; Tibial arteries; Endocarditis; Venous thrombosis; Review.
RESUMO
Aneurisma micótico infra-poplíteo resultante de endocardite infecciosa é raro, com apenas alguns casos relatados. Descrevemos o caso de um paciente de 28 anos do sexo masculino que apresentou dor e edema na perna direita. A ultrassonografia demonstrou um aneurisma do tronco tíbio-fibular e trombose venosa profunda do membro inferior direito. O paciente foi internado e desenvolveu falência cardíaca aguda, sendo diagnosticado de endocardite bacteriana. Um pseudo-aneurisma foi evidenciado na arteriografia. Antibioticoterapia agressiva foi iniciada e cirurgia aberta confirmou um pseudo-aneurisma micótico do tronco tibio-fibular. Para o nosso conhecimento, este é o oitavo caso relatado de aneurisma infectado localizado especificamente nesta região.
INTRODUCTION
Sir William Osler introduced the term mycotic aneurysm in 188512 in his lecture on endocarditis. Infected aneurysms can develop from hematogenous spread of infectious microemboli into the vasa vasorum of a normal-caliber artery (which is the usual definition of mycotic aneurysm), infection of a pre-existing intimal defect by circulating infectious agent (infected arteritis), infection of a pre-existing true aneurysm, contiguous involvement of the vessel from an adjacent source of infection, or direct infectious inoculation of the vessel wall11.
Although the term mycotic (which, by definition, refers to fungus) is widely used for infected aneurysms of embolic origin, most cases are due to bacteria, mainly Streptococcus spp, Salmonella spp and Staphylococcus aureus2.
After the widespread use of antibiotics for bacterial endocarditis and the replacement of infected heart valves, mycotic aneurysms caused by septic emboli have become rarer. In decreasing frequency, the aorta, peripheral arteries, cerebral arteries and visceral arteries are the most affected sites7.
The most frequently involved peripheral vessel is the femoral artery, and the majority of the emboli lodge in the bifurcation of the common femoral artery. Lodging in the infrapopliteal arteries is very rare, with few cases reported. We report here a case of mycotic aneurysm of the right tibioperoneal trunk in a patient who suffered from bacterial endocarditis.
CASE REPORT
The patient was a 28-year-old male who was referred to our institution with a suspected diagnosis of deep vein thrombosis (DVT), presenting a 15-day history of pain and swelling of the right leg. There were no complaints of fever or any other symptom suggesting endocarditis.
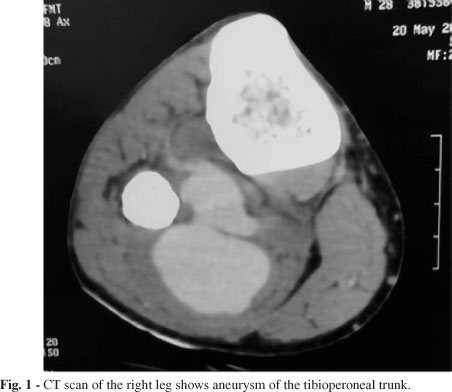
The positive findings in physical examination were a diastolic murmur, edema in the right leg and a pulsatile mass in the right calf. The patient had no history of intravenous drug abuse or dental treatment, although he presented teeth in poor conditions. Duplex scan of the right inferior limb was performed, confirming DVT in popliteal vein, and revealed a 3.2 centimeter measuring aneurysm in the tibioperoneal trunk. The origins of the peroneal and posterior tibial originated from the aneurysm. Anticoagulation was initiated because of the DVT. CT scan of the right leg confirmed the huge aneurysm in the tibioperoneal trunk (Fig. 1).
On the third day after the admission, the patient developed tachycardia and dyspnea. Differential diagnoses were pulmonary embolism (PE) and heart failure from valve disease. An echocardiogram was performed, and revealed vegetations and severe dysfunction on the aortic valve, without signs of pulmonary hypertension. With this data, PE was considered less likely, and aortic valve insufficiency and endocarditis were considered as main diagnoses. Four blood culture samples were taken, but turned out to be negative. The patient met the modified Duke criteria8 for possible endocarditis.
The patient was transferred to the intensive care unit for clinical stabilization and aggressive treatment with Penicillin, Oxacylin and Gentamycin. After ten days, he recovered from the congestive heart failure and left the ICU, asymptomatic.
Under stable clinical conditions, investigation of the aneurysm proceeded. Arteriography of the right inferior limb revealed the pseudoaneurysm of the right tibioperoneal trunk (Fig. 2).
Open surgery was performed. There was a huge hematoma and venous compression of the popliteal vein by the aneurysm was present. The infragenicular popliteal artery was exposed, as were the anterior and posterior tibial arteries. The pseudoaneurysm was opened, exposing a great amount of thrombi (Fig. 3). Bacteriological culture of the thrombotic material was performed, but was negative.
The ipsilateral, reversed greater saphenous veingraft was placed from the tibioperoneal trunk, just below the origin of the anterior tibial artery, to the posterior tibial artery (Fig. 4). The peroneal artery was ligated. At postoperative evaluation, distal pulses of the right inferior limb were palpable and with good amplitude. The patient had an uneventful recovery and continued under antibiotic therapy for six weeks.
DISCUSSION
In the post-antibiotic and heart surgery era, infectious aneurysms from endocarditis became rare. There has been a growing number of cases of infected aneurysms, but this reflects more "local" origin infections - such as those associated with trauma or vascular access for medical reasons - than embolic events per se. Intra-venous drug users are at risk for both endocarditis and local (near injection sites) causes for infected aneurysms/pseudoaneurysms.
Regarding our case report, in which native heart valve was damaged, the embolic origin is unequivocal. Once vasa vasorum are infected, local ischemia occurs on the wall of the vessel, and its weakness leads to the (pseudo-)aneurysm.
Our patient was referred because of suspected deep vein thrombosis (which he had). It was a case associated with DVT and the diagnosis of the aneurysm before any clinical manifestation related to endocarditis. It's the first case like that described in the literature.
The Doppler finding of the arterial aneurysm was not expected, and the patient had not previously noticed a pulsatile mass on his calf. It was an incidental finding, but later heart failure prompted medical staff to perform an echocardiogram. Despite negative blood cultures, the patient met the Duke's criteria for possible endocarditis (one major - positive echocardiogram findings, and one minor - vascular events).
We performed a PubMed/MedLine search and found seven case reports on tibioperoneal trunk infected aneurysms (Table 1).
The first infected aneurysm in this region was reported in 19921. That patient developed the aneurysm 18 months after the diagnosis of endocarditis.
Of the seven cases, only one5 was not related to endocarditis. It was a renal transplant recipient patient whose history was of sepsis after skin infection and concomitant leg pain. Investigation of the limb led to the diagnosis of an infra-popliteal infected aneurysm.
Of the six cases with endocarditis diagnosis, in five the infected aneurysm was diagnosed after the endocarditis. Only one3 was similar to ours: first the aneurysm was detected because of leg pain and edema, and further investigation with an echocardiogram and blood cultures diagnosed endocarditis.
Regarding interval from endocarditis diagnosis and aneurismal diagnostic: in two6,9 out of five cases, the infected aneurysm diagnosis was concomitant (or "brief after"), and the remainder three1,4,10 ranged from four weeks to 18 months.
As in two cases bilateral disease was described9,10, we can consider there were nine aneurysms of the tibioperoneal trunk (on a total of seven cases) reported to date.
In all cases reported, some kind of intervention took place, except for the right leg of a pediatric patient with a bilateral infection9 whose investigation diagnosed a thrombosed aneurysm on the right limb.
Endovascular treatment (with coil embolization) was performed in one case6. Ligation/closure of the aneurysm was undertaken on four cases3,4,5,10, without reconstruction, and arterial reconstruction with saphenous vein was performed on three cases1,6,9.
Considering a case like this one, we conclude that the diagnosis of endocarditis should be suspected in all patients with infected aneurysms. This could prevent further complications related to the endocarditis.
Received: 16 November 2011
Accepted: 30 March 2012
- 1. Akers DL Jr, Fowl RJ, Kempczinski RF. Mycotic aneurysm of the tibioperoneal trunk: case report and review of the literature. J Vasc Surg. 1992;16:71-4.
- 2. Brown SL, Busuttil RW, Baker JD, Machleder HI, Moore WS, Barker WF. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. J Vasc Surg. 1984;1:541-7.
- 3. Khasnis, A, Chick D, Havlichek D Jr. Mycotic aneurysm of the tibioperoneal trunk as a complication of aortic valve endocarditis due to lactobacillus case infection: case report and review of literature. Infect Dis Clin Pract. 2006;14:185-7.
- 4. Kreidy R, Hatem J. Mycotic aneurysm of the tibioperoneal trunk. An extremely rare localization with pseudo-phlebitis clinical presentation. J Med Liban. 2006;54:50-3.
- 5. Lacombe M. Mycotic aneurysm after kidney transplantation. Chirurgie. 1999;124:649-54.
- 6. Larena-Avellaneda A, Debus ES, Daum H, Kindel M, Gross-Fengels W, Imig H. Mycotic aneurysms affecting both lower legs of a patient with Candida endocarditisendovascular therapy and open vascular surgery. Ann Vasc Surg. 2004;18:130-3.
- 7. Lee WK, Mossop PJ, Little AF, Fitt GJ, Vrazas JI, Hoang JK, Hennessy OF. Infected (mycotic) aneurysms: spectrum of imaging appearances and management. Radiographics. 2008;28:1853-68.
- 8. Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633-8.
- 9. McKee MA, Ballard JL. Mycotic aneurysms of the tibioperoneal arteries. Ann Vasc Surg. 1999;13:188-90.
- 10. Murashita T, Yasuda K, Takigami T, Sakuma M, Matsui Y, Sasaki S, Shiiya N. Mycotic aneurysm of the bilateral tibioperoneal trunks associated with bacterial endocarditis: a case report. Int Angiol. 1997;16:176-9.
- 11. Nakata Y, Shionoya S, Kamiya K. Pathogenesis of mycotic aneurysm. Angiology. 1968;19:593-601.
- 12. Osler W. The Gulstonian lectures on malignant endocarditis. Br Med J. 1885;1:467-70.
Publication Dates
-
Publication in this collection
21 May 2012 -
Date of issue
June 2012
History
-
Received
16 Nov 2011 -
Accepted
30 Mar 2012