Abstracts
Rhinocerebral zygomycosis is the most frequent form of fungal infection caused by members of the Zygomycetes class. A fatal case of rhinocerebral zygomycosis caused by Rhizopus (oryzae) arrhizus with histopathological and mycological diagnosis is reported in a diabetic patient.
Zygomicosis; Diabetes mellitus; Tuberculosis
Zigomicose rinocerebral é a forma mais frequente das infecções fúngicas causadas por membros da classe Zygomicetes. É relatado um caso fatal de zigomicose rinocerebral por Rhizopus (oryzae) arrhizus com diagnóstico histopatológico e micológico, em paciente diabética.
Zigomicose; Diabetes mellitus; Tuberculose
CASE REPORT RELATO DE CASO
Rhinocerebral zygomycosis in a diabetic patient
Zigomicose rinocerebral em paciente diabética
Mirella Alves da CunhaI; Andréia Ferreira NeryI; Francisco Pignataro LimaII; José Diniz JuniorIII; José Maciel NetoIV; Nicácia Barbosa CaladoI; Kleber Giovanni LuzI; Eveline Pipolo MilanI
IHospital Giselda Trigueiro, Departamento de Infectologia, Universidade Federal do Rio Grande do Norte, Natal, RN
IIDepartamento de Patologia, Universidade Federal do Rio Grande do Norte, Natal, RN
IIIDepartamento de Medicina Integrada, Universidade Federal do Rio Grande do Norte, Natal, RN
IVHospital Universitário Onofre Lopes, Universidade Federal do Rio Grande do Norte, Natal, RN
Address to Address to: Dra Eveline Pipolo Milan Av. Alm. Alexandrino de Alencar 1384/500 59015-350 Natal, RN, Brasil Tel: 55 84 3201-5747; 55 84 9402-7404 e-mail: evepipolo@gmail.com
ABSTRACT
Rhinocerebral zygomycosis is the most frequent form of fungal infection caused by members of the Zygomycetes class. A fatal case of rhinocerebral zygomycosis caused by Rhizopus (oryzae) arrhizus with histopathological and mycological diagnosis is reported in a diabetic patient.
Keywords: Zygomicosis. Diabetes mellitus. Tuberculosis.
RESUMO
Zigomicose rinocerebral é a forma mais frequente das infecções fúngicas causadas por membros da classe Zygomicetes. É relatado um caso fatal de zigomicose rinocerebral por Rhizopus (oryzae) arrhizus com diagnóstico histopatológico e micológico, em paciente diabética.
Palavras-chaves: Zigomicose. Diabetes mellitus. Tuberculose.
INTRODUCTION
Zygomycosis is a term used for a variety of fungal infections caused by members of the Zygomycetes class1. The genus Rhizopus accounts for a large proportion of cases of the order Mucorales, while Rhizopus (oryzae) arrhizus is the main species identified worldwide2,3. The most frequent form of infection is rhinocerebral, which manifests in the nasal mucosa and paranasal sinuses and may spread to the orbit through the ethmoid, maxillary sinuses or tear ducts, reaching the brain through the orbital vessels4.
The infection may be gastrointestinal, pulmonary, cardiac, rhinomaxillary, rhinocerebral-orbital or disseminated4,5. It is most common in immunocompromised individuals, patients with uncontrolled diabetes mellitus, hematological malignancy, advanced renal disease or with a transplanted kidney6. It generally occurs through inhalation of spores or, less frequently, percutaneously3,7. Rapid fungal invasion of tissue may occur as well as vascular invasion, with consequent ischemia and necrosis7. Healthy individuals seem to have strong natural immunity against zygomycosis and cutaneous-mucosal barrier integrity is the main line of defense against spores2,3.
The aim of this report is to present a case of rhinocerebral zygomycosis in a female diabetic patient.
CASE REPORT
The patient (SVN 27 years-old) was admitted to Giselda Trigueiro Hospital in May 2008 suffering from headaches for 21 days, associated with edema in the right hemiface, pain, with no phlogistic signs and accompanied by rhinorrhea and otorrhea. She had initiated treatment for pulmonary tuberculosis six months ealier, but had only completed four months. She was unaware of any history of diabetes mellitus, but this was confirmed during her hospital stay, showing a permanent state of glycemic decompensation.
A simple chest x-ray showed dense, fibrotic trabeculae in the upper lobe of the left lung, associated with round, radiolucent images, suggesting bubbles. A voluminous radiotransparent lesion was observed at the left lung base, possibly corresponding to the large bubble or even pneumothorax. A final diagnosis of sequelae from a specific process in the left lung was established.
Treatment was initiated with ceftriaxone, oxacillin, clindamycin and dexamethasone. Magnetic resonance of the face showed signs of subcutaneous cell tissue invasion and associated cutaneous thickening. Invasion and extension to the homolateral nasal cavity was also observed, filling it and covering the anterior portion of the zygomatic arch. An irregular uptake of the contrast medium was observed in the meninges and adjacent to the right temporal lobe, suggesting extension of the lesion to the central nervous system (SNC), with the formation of meningitis and cerebritis (Figure 1).
Extensive secretion drainage was performed, resulting in temporary clinical improvement. Sudden onset left hemiparesis developed three days after surgery.
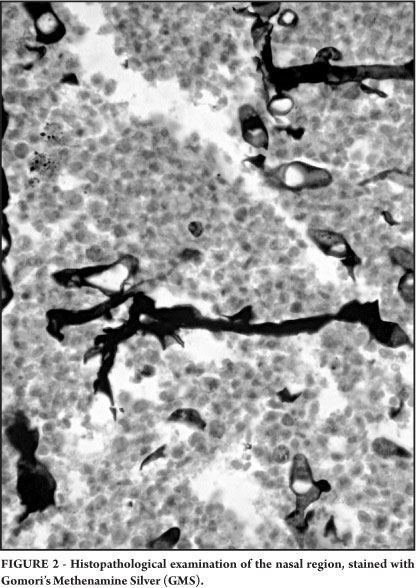
Histopathological examination of the nasal region using both routine staining, hematoxylin eosin, and spatial staining, Gomori Methenamine Silver (GMS) and Periodic Acid- Schiff (PAS), for fungus, revealed wide irregular non-septate hyphae, with frequent branches at right angles invading the mucosa, and extensive necrotic areas (Figure 2). The material was cultured in Sabouraud dextrose Agar medium at 25ºC. After 4 days, the growth of white aerial mycelium with cottony texture was observed, subsequently becoming covered with black dots. Micromorphology showed hyphae that were non-septate and unbranched sporangiophores arising opposite the rhizoids. Each sporangiophore sustained a round sporangium, full of spores that had a flat base (Figure 3). The fungus was diagnosed as Rhizopus (oryzae) arrhizus.
The patient was admitted to the ICU 18 days after hospital admission exhibiting a reduced level of consciousness. Amphotericin B was administered immediately, but the patient died 4 days later.
DISCUSSION
The rhinocerebral form of zygomycosis is the most frequently reported in diabetic patients8. In the case discussed here, the patient presented with a permanent hypoglycemic condition, resulting from the clinical decomposition of diabetes mellitus. She was at the end of treatment for pulmonary tuberculosis, with no signs of clinical respiratory improvement. Considering the likely cellular dysfunction of macrophages and neutrophils inherent in diabetic individuals and the greater possibility of invasive disease in immunosuppressed individuals2, it can be hypothesized that the etiologic agent of the initial pulmonary disease was the zygomycete, which, in light of her diabetes-related depressed immune system, spread to the CNS.
It should also be emphasized that the relation between tuberculosis and pulmonary tuberculosis remains unclear. Fungal infection may occur in cavities resulting from microbacterial invasion. Patel et al reported a recent case of concurrent zygomycosis and pulmonary tuberculosis in an elderly cardiopathic individual with a history of smoking, but with no other immunodepressive factors9.
With respect to the clinical manifestations of cerebral zygomycosis, Sundaram et al reported headaches, fever, unilateral facial edema, visual disorders and loss of vision as the most frequent symptoms5. Although the patient in question showed a compatible clinical picture, it is also symptomatic of other diseases. Diagnosing invasive zygomycosis is particularly difficult, since it is based on histopathological examination showing fungal invasion of the tissues3. Furthermore, clinical suspicion depends on imaging examinations, such as computerized axial tomography and magnetic resonance, which are useful for demonstrating compromised bones and paranasal sinus compromise, in addition to showing the extension of the lesion1.
At admission, she exhibited extensive tissue destruction and necrosis, indicating that the disease had been contracted approximately one month earlier. Difficulties inherent to the public health service delayed magnetic resonance and surgical intervention. Histopathological and culture results were available only three days before death, at which time amphotericin B was administered.
The prognosis of rhinocerebral zygomycosis is cautious and depends on several factors, such as the infection site, rapid diagnosis and severity of immunodepression1. Since its course is invariably fatal, early diagnosis is essential7.
It must be emphasized that both diagnostic difficulties and delayed surgical treatment in conjunction with early antifungal administration were factors that directly influenced the fatal outcome in this patient. Additionally, the lack of well designed studies that describe the natural evolution of zygomycosis with simultaneous compromise of the lungs, facial sinuses and CNS and that discuss its correlation with pulmonary tuberculosis, also contributed to the death of this patient.
Received in 18/08/2010
Accepted in 17/11/2010
- 1. Islam MN, Cohen DM, Celestina LJ, Ojha J, Claudio R, Bhattacharyya IB. Rhinocerebral zygomycosis: an increasingly frequent challenge: update and favorable outcomes in two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104:28-34.
- 2. Brown J. Zygomycosis: An emerging fungal infection. Am J Health Syst Pharm 2005; 62:2593-2596.
- 3. Torres-Narbona M, Guinea J, Muñoz P, Bouza E. Zigomicetos y zigomicosis en la era de las nuevas terapias antifúngicas. Rev Esp Quimioter 2007; 20:375-386.
- 4. Romano C, Miracco C, Massai L, Piane R, Alessandrini C, Petrini C, et al. Case Report. Fatal rhinocerebral zygomycosis due to Rhizopus oryzae. Mycoses 2002; 45:45-49.
- 5. Sundaram C , Mahadevan A, Laxmi V, Yasha TC, Santosh V, Murthy JMK, et al. Cerebral zygomycosis. Mycoses 2005; 48:396-407.
- 6. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in Human Disease. Clin Microbiol Rev 2000; 13:236-301.
- 7. Del Palacio A, Ramos MJ, Pérez A, Arribi A, Amondarain I, Alonso S, et al. Zigomicosis A propósito de cinco casos. Rev Iberoam Micol 1999; 16:50-56.
- 8. Lanternier F, Lortholary O. Zygomycosis and diabetes mellitus. Clin Microbiol Infect 2009; 15 (suppl 5):21-25.
- 9. Patel T, Clifton IJ, Kastelik JA, Peckham DG. Concurrent pulmonary zygomycosis and Mycobacterium tuberculosis infection: a case report. J Med Case Reports 2007; 17: 1-3.
Publication Dates
-
Publication in this collection
13 June 2011 -
Date of issue
Apr 2011
History
-
Received
18 Aug 2010 -
Accepted
17 Nov 2010