Abstract
Introduction
The aim of this study was to establish the incidence rates of congenital syphilis in the South Region of Brazil from 2001 to 2009.
Methods
Temporal ecological and descriptive study based on the cases recorded by the System of Information of Notifiable Diseases.
Results
The incidence of congenital syphilis has been increasing in the South Region of Brazil since 2004; the highest incidence rates were in women who received prenatal care (113.5 new cases per 100,000 births, p<0.001), who were diagnosed with syphilis at pregnancy (69.8 new cases per 100,000 births, p=0.001), and whose partner did not undergo treatment for syphilis (53.1 new cases per 100,000 births, p=0.001).
Conclusions
The population of the present study mostly consisted of adult black women with low educational levels who attended prenatal care, who were diagnosed with syphilis during pregnancy, and whose partners were not treated for syphilis. Based on these results, actions are recommended to reduce the incidence of this disease, which is preventable by early diagnosis and appropriate treatment. The present was merely an ecological study; therefore, further investigations are necessary to elucidate the causes of these findings.
Congenital syphilis; Epidemiology; Incidence; Brazil
INTRODUCTION
Although syphilis is a fully preventable disease, it is still a relevant cause of death among newborn infants. Approximately 2.65 million stillbirths occur every year, 98% of which are in developing countries. Among live births, most syphilis-related deaths occur within the first week of life11. Mabey D, Peeling RW. Syphilis, still a major cause of infant mortality. Lancet Infect Dis 2011; 11:654-655..
Syphilis is a chronic systemic infectious disease caused by Treponema pallidum, a spirochete bacterium with sexual and vertical transmission resulting in the acquired and congenital forms of disease, respectively22. Avelleira JCR, Bottino G. Sífilis: diagnóstico, tratamento e controle. An Bras Dermatol 2006; 81:111-126.. Congenital syphilis occurs due to hematogenous spread of T. pallidum from an infected or inappropriately treated pregnant woman to the fetus33. Smeltzer SC, Bare BG. Tratado de enfermagem médico cirurgica. 10ª ed. Guanabara Koogan: Rio de Janeiro; 2005.. When mothers exhibit genital lesions at delivery, direct mother-to-child transmission of bacteria may occur. Untreated, the progression of syphilis is characterized by stages of active and latent disease and represents a public health concern in many developing countries44. Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Protocolo para prevenção da transmissão vertical do HIV e sífilis. Brasília: Ministério da Saúde; 2007..
Congenital syphilis exhibits variable behavior in different countries. Approximately one million pregnant women become infected every year, with 27/100,000 live births exhibiting congenital syphilis, 46/100,000 pregnancies ending in unintended abortion or perinatal death, and 2,700/100,000 live births being preterm or exhibiting low birth weight55. Walker DG, Walker GJ. Forgotten but not gone: the continuing scourge of congenital syphilis. Lancet Infect Dis 2002; 2:432-436.–77. Schmid G. Economic and programmatic aspects of congenital syphilis prevention. Bull World Health Organ 2004; 82:402-409.. According to the Pan American Health Organization the incidence of congenital syphilis in the Americas is approximately 1,200/100,000 live births88. Valderrama J, Zacarías F, Mazin R. Maternal syphilis and congenital syphilis in Latin America: big problem, simple solution. Rev Panam Salud Publica 2004; 16:211-217.. In the United States, the incidence was 8.8/100,000 live births in 200499. Centers for Disease Control and Prevention (CDC), Department of Health and Human Services. Sexually transmitted disease surveillance. Atlanta, GA: CDC; 2004.. The incidence of congenital syphilis has increased in Russia1010. Tikhonova L, Salakhov E, Southwick K, Shakarishvili A, Ryan C, Hillis S. Congenital syphilis in the Russian Federation: magnitude, determinants, and consequences. Sex Transm Infect 2003; 79:106-110.. In Brazil, an average of approximately 4,000 new cases of congenital syphilis are reported every year, corresponding to an incidence of 160/100,000 live births. Taking underreporting into consideration, 12,000 new cases are estimated to occur every year, increasing the incidence to 400/100,000 live births44. Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Protocolo para prevenção da transmissão vertical do HIV e sífilis. Brasília: Ministério da Saúde; 2007..
Congenital syphilis is a marker of the quality of mother-child care, as the risk of transplacental transmission is effectively reduced when diagnosis and clinical/therapeutic management are appropriate. Despite the low cost of treatment and the wide availability of simple preventive technologies, congenital syphilis is still a significant cause of child morbidity, morbidity, and perinatal death - especially related to the fetal component22. Avelleira JCR, Bottino G. Sífilis: diagnóstico, tratamento e controle. An Bras Dermatol 2006; 81:111-126.,33. Smeltzer SC, Bare BG. Tratado de enfermagem médico cirurgica. 10ª ed. Guanabara Koogan: Rio de Janeiro; 2005.. Therefore, the current annual incidence of disease has no justification, and interventions aimed at increasing the coverage of screening, treatment, and prevention of syphilis during pregnancy should be prioritized. For that purpose, the true extension and the particularities of the problem should be thoroughly investigated. The aim of the present study was to establish the incidence of congenital syphilis in the South Region of Brazil in the period from 2001 to 2009.
METHODS
The present investigation was a temporal ecological and descriptive study that was approved by the human research ethics committee of the institution where it was conducted (protocol 281/2011). We used Chapter I of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), which includes congenital syphilis (A50).
The study population comprised all cases of congenital syphilis in the
South Region of Brazil (i.e., States of Paraná, Santa Catarina, and Rio
Grande do Sul) that were reported to the System of Information of Notifiable
Diseases (Sistema de Informação de Agravos de
Notificação - SINAN) from 2001 to 2009, available
through the Department of Informatics of the Unified Health System
(Departamento de Informática do Sistema Único de
Saúde - DATASUS). The data on births were collected from the
System of Information on Live Births (Sistema de Informações sobre
Nascidos Vivos - SINASC).1111. Ministério da Saúde; Sistema de Informações sobre
Nascidos Vivos-Notas técnicas [Internet]. Brasília: MS; 2012
[Cited 2012 March 10]. Available at: http://tabnet. datasus.
gov. br/cgi/sinasc/nvdescr.Htm/
http://tabnet...
Historical series were elaborated from 2001 to 2009 because
notified cases of congenital syphilis were available for that period through
SINAN.
The following variables were assessed: ethnicity, gender, area of residence, maternal educational level, maternal age range, children's age range, prenatal care attendance, final diagnosis, diagnosis at pregnancy, and treatment of partners.
The following ethnic categories were used: white, black, Asian, brown-skinned, and Indian. Gender was categorized as male or female. The notified cases were stratified according to urban or rural area of residence.
The educational level was stratified based on the number of years of formal school attendance, as follows: none, one to three years, four to seven years, eight to 11 years, and 12 or more years. As a function of the differences in the categories used by SINAN before and after 2006, the following groupings were considered for analysis in the present study: individuals with no education together with the illiterate; the category one to three years of education included all individuals who attended elementary school but did not complete grade four; the category four to seven years of education included individuals who completed elementary school grade four and those who attended grades five to eight, having completed an elementary education or not; the category eight to 11 years of education included individuals who either partially attended or completed secondary education; and category 12 or more years of education included individuals who either partially attended or completed a higher education.
The following child age-range categories were included in SINAN: up to six days old, seven to 27 days old, 28 days to less than one year old, one year old (12 to 23 months), two to four years old, and five to 12 years old. Because the incidence of disease cases among children older than six days was low, the variable age was dichotomized as up to six days old and more than six days old.
The variable maternal age was stratified as follows: 15 to 19 years old, 20 to 24 years old, 30 to 34 years old, 35 to 39 years old, 40 to 44 years old, and 45 to 49 years old. Only data for the period from 2001 to 2006 were available through SINAN. For the purpose of comparison with other studies, this variable was also stratified as less than 30 and greater than 30 years old.
The variable prenatal care attendance was categorized as follows: yes (attended prenatal care) and no (did not attend prenatal care). However, because prenatal care attendance is stratified in SINASC as a function of the number of visits made, we chose to define non-attendance as having made zero to six visits, and attendance was defined as having made seven or more visits.
Relative to the variable final diagnosis, congenital syphilis was classified as recent, late, syphilis-related stillbirths/abortions. The variable diagnosis at pregnancy was categorized as yes (mothers who were diagnosed with syphilis during pregnancy) and no (mothers who were not diagnosed with syphilis during pregnancy). As a function of differences in the categories used by SINAN before and after 2006, the following classifications were considered for analysis in the present study: the category yes included all women who were diagnosed with syphilis during pregnancy or at birth/curettage, and the category no included all women who were diagnosed with syphilis after delivery and those who were never diagnosed with syphilis. The variable treatment of partner was categorized as yes or no. It is noteworthy that the data for this variable were only available for years 2007 to 2009.
The absolute and relative frequencies of the data corresponding to all the variables were calculated. The raw incidence rate was calculated by dividing the number of recorded cases by the number of live births correlated with the selected variable at the same place and period, multiplied by 100,000. The standardized proportional incidence ratio was calculated for the variables ethnicity, gender, maternal age range, maternal educational level, and prenatal care attendance because these data were made available by SINAN and SINASC in DATASUS.
Data tabulation and access to SINAN were performed using the software TabNet, which is available for online access at DATASUS, and TabWin version 3.6 (Datasus, Brasília, Distrito Federal, Brazil). Both the indicators and descriptive statistical analysis were developed using Microsoft Excel 2007 and the Statistical Package for the Social Sciences - SPSS (IBM company, Armonk, New York, United States), version 17. The significance level was established as α=0.05 with a 95% confidence interval (CI).
The normality of the distribution of quantitative data was assessed by the Shapiro-Wilk test. One-way analysis of variance (ANOVA) followed by Tukey's post-hoc test was used to compare the means calculated for the variables ethnicity, maternal education level, area of residence, maternal age range, and final diagnosis. Student's t-test for independent samples was used to compare the means calculated for the variables gender, (dichotomized) maternal age range, (dichotomized) children's age range, prenatal care attendance, diagnosis at pregnancy, and treatment of partners.
RESULTS
From 2001 to 2009, 3,240 cases of congenital syphilis were reported in the South Region of Brazil, which corresponded to an average incidence of 94.0±28.4 cases per 100,000 live births. The characteristics of the investigated population are described in Table 1.
The average incidence by state was 57.1±10.7 cases per 100,000 live births in Paraná, 33.7±16.7 cases per 100,000 live births in Santa Catarina, and 170.2±70.1 cases per 100,000 live births in Rio Grande do Sul. A significant difference was found in the incidence of congenital syphilis among these three states, being highest in Rio Grande do Sul (p<0.001), with a peak in 2008 (290.1 cases per 100,000 live births) and a decrease of 6.4% in 2009. Although the results appear indicative of an association, the average incidences in Paraná and Santa Catarina were not significantly different (p= 0.478). Paraná exhibited two peaks of incidence, one in 2003 (64.2 cases per 100,000 live births) and the other in 2008 (70.2 cases per 100,000 live births), an 8.3% increase. In Santa Catarina, the peak incidence was in 2004 (52.6 cases per 100,000 live births) and the minimum incidence in 2002 (11.7 cases per 100,000 live births). Regarding the South Region of Brazil as a whole, the peak incidence of congenital syphilis occurred in 2008 (143.5 cases per 100,000 live births), with a progressive increase of 11.8% from 2004 to 2008, followed by a slight decrease of 4.87% in 2009.
A statistically significant association was found between the incidence of congenital syphilis and the area of residence. The incidence of congenital syphilis was higher in urban areas compared with rural areas (p<0.001). In urban areas, the highest number of cases was reported in 2008 (480 cases, 16.1%). In rural areas, the highest incidence (17.1%, 19 cases) was in 2008.
The Figure 1 shows that a statistically significant association (p=0.010) was found between ethnicity and the incidence of congenital syphilis: it was higher among blacks (450.9±320.1 cases per 100,000 live births) compared with whites (61.0±28.3 cases per 100,000 live births). No other significant association was found as a function of ethnicity. The peak incidence of congenital syphilis among blacks occurred in 2009 (1,003.6 cases per 100,000 live births), and the minimum occurred in 2004 (175.0 cases per 100,000 live births). The highest number of cases among whites was recorded in 2008 (102.5 cases per 100,000 live births), and the lowest occurred in 2001 (13.0 cases per 100,000 live births). The peak incidence of congenital syphilis among Asians, brown-skinned individuals, and Indians occurred in 2008 (1,304.4 cases per 100,000 live births), 2009 (252.6 cases per 100,000 live births), and 2007 (316.8 cases per 100,000 live births), respectively. The lowest number of cases among brown-skinned individuals was recorded in 2001 (54.3 cases per 100,000 live births), whereas no cases were recorded among Asians in 2001, 2007, and 2009 or among Indians in 2001, 2002, and 2004.
The average incidence of syphilis-related stillbirths/abortions (2.2±1.6 cases per 100,000 live births) was significantly lower (p<0.001) compared with the record of recent congenital syphilis cases (83.8±24.7 cases per 100,000 live births). The latter, in turn, was significantly higher (p<0.001) compared with the average incidence of late congenital syphilis (0.8±0.8 cases per 100,000 live births). No significant difference was found between the average incidence of late congenital syphilis and syphilis-related stillbirths/abortions (p=0.978). The incidence of recent congenital syphilis exhibited a 35.8% increase from 2001 to 2003, followed by a decrease of 16.2% in 2004 and a new increase of 66.5% from 2005 to 2009.
No significant difference (p=0.572) was found in the average incidence of congenital syphilis between males (86.5±28.2 cases per 100,000 live births) and females (93.6±23.7 cases per 100,000 live births).
A statistically significant association (p<0.001) was found with the variable age: the incidence of congenital syphilis was higher among infants up to six days old (87.6±28.5 cases per 100,000 live births) compared with older children (1.3±1.4 cases per 100,000 live births).
Although the results related to the variable maternal age seemed suggestive of a difference, it was not statistically significant (p=0.427). However, analysis of the dichotomized variable revealed a significantly greater incidence (p=0.021) of congenital syphilis among mothers older than 30 years (109.4±67.1 cases per 100,000 live births) compared with younger mothers (72.2±12.9 cases per 100,000 live births).
The average incidence of congenital syphilis was significantly higher (p<0.001) among the mothers with one to three years of education (245.2±177.3 cases per 100,000 live births) compared with those with eight to 11 years (39.1±13.0 cases per 100,000 live births) and 12 or more years of education (8.2±4.3 cases per 100,000 live births). Although these results seemed suggestive of a difference in the average incidence rates between the mothers with one to three and those with four to seven years of education, the difference was not statistically significant (p=0.109). The average incidence of congenital syphilis was also higher among the illiterate mothers (339.4±118.8 cases per 100,000 live births) compared with those with four to seven years of education (123.8±83.5 cases per 100,000 live births, p=0.001), eight to 11 years (39.1±13.0 cases per 100,000 live births, p<0.001), and 12 or more years (8.2±4.3 cases per 100,000 live births, p<0.001). Although the results seemed suggestive of a difference in the average incidence rates between the illiterate mothers and the ones with one to three years of education (245.2±177.3 cases per 100,000 live births), the difference was not statistically significant (p=0.310). In the mothers with one to three years of education, the incidence of congenital syphilis decreased by 74.2% from 2001 to 2004, then increased 112.4% from 2004 to 2005 and 312.8% from 2007 to 2009.
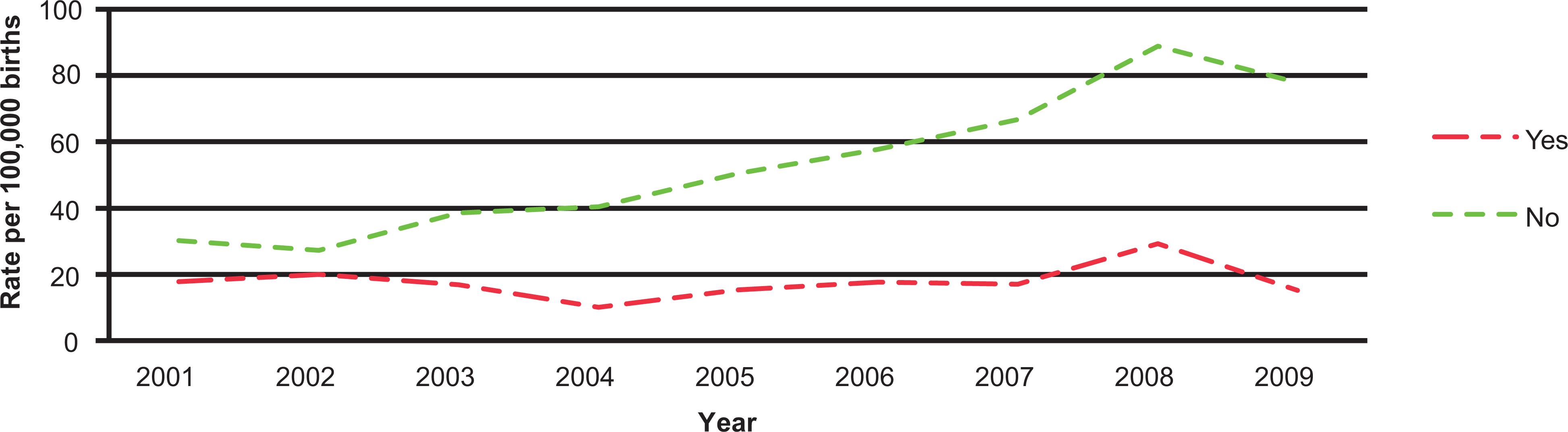
The average incidence of congenital syphilis exhibited a significant difference (p<0.001) between the women who attended prenatal care and those who did not, being higher in the former (113.4±24.1 cases per 100,000 live births) compared with the latter (44.3±31.6 cases per 100,000 live births) (Figure 2). Among the women who attended prenatal care, the incidence of congenital syphilis increased by 12% from 2001 to 2003, followed by a decrease of 31.9% from 2003 to 2004, an increase of 53.1% from 2005 to 2008, and another decrease of 9.7% from 2008 to 2009. Among the women who did not attend prenatal care, the incidence of congenital syphilis exhibited two rises, one from 2001 to 2003 (82.7%) and the other from 2006 to 2009 (164.2%), whereas the period from 2004 to 2005 exhibited a fall of 23.8% relative to 2003.
The Figure 3 shows the average incidence of congenital syphilis was significantly higher (p=0.001) among the cases with diagnosis during pregnancy (69.7±30.7 cases per 100,000 live births) compared with those not diagnosed during pregnancy (17.6±6.6 cases per 100,000 live births). The peak incidence of congenital syphilis in the women diagnosed during pregnancy occurred in 2008 (123.8 cases per 100,000 live births), and the minimum occurred in 2004 (42.0 cases per 100,000 live births). With respect to the cases without diagnosis at pregnancy, the peak incidence was recorded in 2006 (30.3 cases per 100,000 live births), and the minimum was recorded in 2007 (8.5 cases per 100,000 live births).
A statistically significant association (p=0.001) was found between the incidence of congenital syphilis and the variable treatment of partner (Figure 4). The average incidence of the disease was higher among the cases in which the mother's partner was not treated for syphilis (53.1±21.4 cases per 100,000 live births). In that population of women, the average incidence of syphilis increased by 225% from 2002 to 2008, followed by a decrease of 12.4% from 2008 to 2009. In the population of women whose partners were appropriately treated for syphilis (17.7±5.1 cases per 100,000 live births), the incidence rates varied during the investigated period, with a peak in 2008 (29.3 cases per 100,000 live births).
DISCUSSION
The aim of the present study was to investigate the incidence of congenital syphilis in the South Region of Brazil from 2001 to 2009. The incidence averaged 94 new cases per 100,000 births and progressively increase from 2004 onwards. Our findings corroborate the results of an ecological study conducted by the Inter-Agency Network for Health Information for the period from 1998 to 2005, which found a 81.9% increase in the average incidence of the disease from 1999 to 20051212. Rede Interagencial de Informação para a Saúde. Organização Pan-Americana da Saúde. Indicadores básicos para a saúde no Brasil: conceitos e aplicações. Brasília: Organização Pan-Americana da Saúde; 2008..
The highest incidence in this study occurred in urban areas (p<0.001), as was also found in a nationwide temporal study conducted through the Family Health Strategy for the period from 2001 to 20081313. Araújo CL. Análise da situação da sífilis congênita e da sua relação com a cobertura da estratégia de saúde da família no Brasil (2001 a 2008) [Dissertatio]. [Brasília]: Universidade de Brasília; 2010.. These findings might indicate that the identification of cases occurs more comprehensively in urban areas compared with rural areas, as a function of the large regional distances in rural areas that cause many cases of syphilis occurring during pregnancy to go undiagnosed or unreported. Obviously, undetected cases will not be treated and nor will the women's partners; thus, one should systematically consider the possibility of treatment failure and of cases in pregnant women who do not attend prenatal care. This fact once again indicates the relevance of prenatal care in the eradication of congenital syphilis.
No significant difference was found in the incidence of congenital syphilis as a function of gender (p=0.572), which agrees with the results of a temporal study conducted in Portugal that assessed the period from 1993 to 2004 to identify risk factors for congenital syphilis1414. Jacinto S, Henriques M, Ferreira T, Carvalhosa G, Costa T, Valido AM. A sífilis congénita ainda existe! Análise retrospectiva de 12 anos de uma grande maternidade. Acta Pediatr Port 2007; 38: 65-68.. Congenital syphilis is a disease with vertical transmission and is influenced by the maternal disease stage and by the length of fetal exposure, but not by gender1515. Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Diretrizes para o controle de sífilis congênita: manual de bolso. Brasília: Ministério da Saúde, 2006..
The present study found a higher incidence of congenital syphilis among blacks compared with all other ethnicities (p=0.010). This finding corroborates the results of a case-control study conducted in Belo Horizonte, Minas Gerais, Brazil, from 2001 to 2008, which found a greater incidence of the disease among black and brown-skinned mothers (odds ratio [OR]: 2.1; 95% CI: 1.5-2.8) compared with all other ethnicities1616. Lima MG, Santos RF, Barbosa GJ, Ribeiro GS. Cien Saude Colet 2013; 18:499-506.. Despite the global initiative to eradicate congenital syphilis launched by the World Health Organization (WHO) in 2007, the situation showed little change five years later; thus, the results of some studies suggest that ethnicity is not necessarily associated with the incidence of disease, which instead appears to be associated with socio-demographic factors. In addition, appropriate prenatal care targeting the control of syphilis might reduce the incidence of syphilis-related stillbirths and perinatal deaths by 50%1717. Chen XS, Yin YP. Syphilis: still a major cause of infant mortality. Lancet Infect Dis 2012; 12:269-270..
In a temporal study that included 2,145 Brazilian puerperal women admitted to maternity hospitals for delivery or curettage from 1999 to 2000, non-white ethnicity was associated with a greater risk of not being diagnosed during pregnancy1818. Rodrigues CS, Guimarães MDC, Comini CC. Missed opportunities for congenital syphilis and HIV perinatal transmission prevention. Rev Saude Publica 2008; 42:851-858.. One case-control study conducted in Porto Alegre in 1998-2000 disclosed the relevance of certain socioeconomic characteristics (black ethnicity and low maternal educational level) as risk factors for congenital syphilis following adjustment for the variables representing access to prenatal care. Thus, although the fact that women under highly vulnerable conditions tend to attend few prenatal care visits is well established, this pattern might be due to factors that are not associated with prenatal care and that cause social inequalities to be associated with different risks of congenital syphilis1919. Puccini RF, Pedroso GC, Silva EMK, Araújo NS, Silva NN. Eqüidade na atenção pré-natal e ao parto em área da Região Metropolitana de São Paulo, 1996. Cad Saude Publica 2003; 19:35-45.. Such factors include the following: insufficient transportation resources to laboratories and healthcare centers; a lack of social support, particularly from the women's partners; and unsafe sex practices, which increase the risk for recurrent T. pallidum infections2020. Araújo CL, Shimizu HE, Sousa AI, Hamann EM. Incidence of congenital syphilis in Brazil and its relationship with the Family Health Strategy. Rev Saude Publica 2012; 46:479-486..
Our study found an inverse relationship between maternal educational level and the incidence of congenital syphilis. This finding agrees with the results of a temporal study conducted in Brazil targeting the period from 1999 to 2000, in which women with less than eight years of education and income equivalent to less than three times the minimum wage and single women were less likely to be screened for congenital syphilis and for infection with the human immunodeficiency virus (HIV) during pregnancy. These socio-demographic factors might denote greater vulnerability in the investigated population and represent markers of poor access to screening tests and healthcare services1818. Rodrigues CS, Guimarães MDC, Comini CC. Missed opportunities for congenital syphilis and HIV perinatal transmission prevention. Rev Saude Publica 2008; 42:851-858.. A cross-sectional study that included 702 pregnancies assisted at the General Hospital of University of Caxias do Sul, Brazil, from 2000 to 2001 found that the higher the maternal educational level, the earlier the onset of prenatal care and the larger the number of prenatal care visits attended2121. Trevisan MR, De Lorenzi DRS, Araújo NM, Ésber K. Perfil da assistência pré-natal entre usuárias do Sistema Único de Saúde em Caxias do Sul. Rev Bras Ginecol Obstet 2002; 24:293-299..
Disproportionate concentrations of congenital syphilis among the offspring of women belonging to the most vulnerable groups (blacks, individuals with low educational levels, and individuals with low socioeconomic levels) have been identified not only in Brazil1818. Rodrigues CS, Guimarães MDC, Comini CC. Missed opportunities for congenital syphilis and HIV perinatal transmission prevention. Rev Saude Publica 2008; 42:851-858. but also in other countries, such as the United States2222. Revollo R, Tinajeros F, Hilari C, García SG, Zegarra L, Díaz-Olavarrieta C, et al. Maternal and congenital syphilis in four provinces in Bolivia. Salud Publica Mex 2007; 49:422-428.,2323. Gottlieb SL, Pope V, Sternberg MR, McQuillan GM, Beltrami JF, Berman SM, et al. Prevalence of syphilis serore activity in the United States: data from the National Health and Nutrition Examination Surveys (NHANES) 2001-2004. Sex Transm Dis 2008; 35:507-511.. These findings might suggest inequalities in access to preventive measures.
Regarding maternal age, our study revealed that the average incidence of congenital syphilis was higher among women older than 30 years compared with the younger women (p=0.021). This finding contrasts with the results of previous studies2424. Campos ALA, Araújo MAL, Melo SP, Gonçalves MLC. Epidemiologia da sífilis gestacional em Fortaleza, Ceará, Brasil: um agravo sem controle. Cad Saude Publica 2010; 26:1747-1755.. Although adolescence is generally considered a relevant risk factor for the acquisition of sexually transmitted diseases, including syphilis, this finding was not observed in the present study2525. Araujo EC, Costa KSG, Silva RS, Azevedo VNG, Lima FAS. Importância do pré-natal na prevenção da Sífilis Congênita. Rev Para Med 2006; 20:47-51..
The average incidence of congenital syphilis was higher among the women who attended prenatal care compared with those who did not (p<0.001). A cross-sectional study that assessed 2,145 Brazilian puerperal women admitted to maternity hospitals for delivery or curettage from 1999 and 2000 investigated missed opportunities for preventing congenital syphilis as a consequence of having had no testing. That study found that congenital syphilis had a prevalence of 41.2%, that 15% of the women with a missed prevention opportunity attended fewer than four prenatal care visits, and that late onset and early discontinuation of prenatal care attendance were more common among the unscreened women (42% and 16%, respectively)1818. Rodrigues CS, Guimarães MDC, Comini CC. Missed opportunities for congenital syphilis and HIV perinatal transmission prevention. Rev Saude Publica 2008; 42:851-858..
The higher incidence of congenital syphilis among the mothers who attended prenatal care compared with those who did not might be explained by the fact that establishing a diagnosis is no guarantee of receiving appropriate treatment. Several authors observed that a lack of prenatal care is most relevant among the factors associated with high prevalence rates of congenital syphilis. A cross-sectional study conducted in Fortaleza, Ceará, Brazil, from May to October 2008 found that, although most (85.2%) participants had access to prenatal care (5.8 visits on average), the prevalence of congenital syphilis was extremely high2626. Lorenzi DRS, Madi JM. Sífilis Congênita como indicador de assistência pré-natal. Rev Bras Ginecol Obstet 2001; 23:647-652.. Those findings further reinforce the notion that prenatal care should be assessed as a function of the number of medical visits and that the quality of care should also be taken into consideration2727. Walker GJ, Walker DG. Congenital syphilis: a continuing but neglected problem. Semin Fetal Neonatal Med 2007; 12:198-206..
In the present study, the incidence of congenital syphilis was higher among the women diagnosed with syphilis during pregnancy (p=0.001). In addition to a lack of or inadequate treatment, this finding might have been due to the healthcare providers' neglect to provide safe sex education (e.g., in the use of condoms) during or after treatment or to the women's lack of adherence to such advice, which would make them susceptible to reinfection following the end of appropriate treatment2828. Hawkes S, Matin N, Broutet N, Low N. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 2011; 11:684-691..
Consequently, the lack of partner treatment is a relevant indicator of the difficulties women face in receiving appropriate treatment (as recommended by the Health Ministry) and of the risk of reinfection experienced by women despite appropriate treatment during pregnancy. Notably, not all pregnant women have stable partners, and SINAN does not make this information available. Were all pregnant women screened and all those with positive results treated with benzathine penicillin before pregnancy week 28, the rate of syphilis-related stillbirths or neonatal deaths could be reduced. Considering the high cost of treating congenital syphilis and the fact that the cost of preventive intervention is one of the lowest among all collective health actions, it is easy to understand why the cost/benefit ratio of prevention is far more favorable than that of treatment. For instance, in Tanzania, the cost of screening is USD1.44 per woman, whereas the cost of treatment is USD20.00 per woman2727. Walker GJ, Walker DG. Congenital syphilis: a continuing but neglected problem. Semin Fetal Neonatal Med 2007; 12:198-206.. Therefore, screening women for syphilis is recommended in almost all countries, although it is not systematically performed, as our study reveals.
In the present study, we found that the incidence of congenital syphilis was higher among the infants aged up to six days compared with older children (p<0.001). These results agree with the findings reported by a retrospective study of 45 disease cases occurring from 2003 to 2005, based on the review of notification forms and clinical records. This study found that 91.1% of the cases were notified within five days of birth, whereas an active search of the serology results (venereal disease research laboratory test-VDRL) allowed for retrospective notification of four cases. The results indicated that no time was lost in the notification of cases, which might also account for the results of the present study2929. Donalísio MR, Freire JB, Mendes ET. Investigação da sífilis congênita na microrregião de Sumaré, estado de São Paulo, Brasil - desvelando a fragilidade do cuidado à mulher gestante e ao recém-nascido. Epidemiol Serv Saude 2007; 16:165-173..
The Health Ministry classifies congenital syphilis based on the moment when the diagnosis is established, as follows: early diagnosis is classified as occurring up to two years of age, and late diagnosis is classified as occurring after two years of age. Although two-thirds of cases are asymptomatic at birth44. Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Protocolo para prevenção da transmissão vertical do HIV e sífilis. Brasília: Ministério da Saúde; 2007., as established by a retrospective descriptive study conducted in the Sumaré micro-region of São Paulo, Brazil, targeting the period 2003-2005 (according to which 77.3% of the affected newborn infants were asymptomatic at birth)2929. Donalísio MR, Freire JB, Mendes ET. Investigação da sífilis congênita na microrregião de Sumaré, estado de São Paulo, Brasil - desvelando a fragilidade do cuidado à mulher gestante e ao recém-nascido. Epidemiol Serv Saude 2007; 16:165-173., early diagnosis is supported by several clinical findings from data, including prematurity, bone disease, blood disease, mucocutaneous manifestations, liver enlargement, spleen enlargement, and neurosyphilis44. Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Protocolo para prevenção da transmissão vertical do HIV e sífilis. Brasília: Ministério da Saúde; 2007.. In our study, early congenital syphilis was predominant (p<0.01). One analysis of congenital syphilis cases conducted at Santa Casa do Pará Maternity Hospital in 1996 found that 42.4% of newborns exhibited signs indicative of disease, among which prematurity (16.7%), liver enlargement (11.9%), and stillbirth (7.1%) were the most frequent3030. Araújo EC, Moura AFA, Ramos FLP, Holanda VGDA. Sífilis congênita: incidência em recém-nascidos. J Pediatr 1999; 75:119-125.. On these grounds, a predominance of cases classified as early congenital syphilis might denote high diagnostic efficacy.
The aforementioned study conducted in the Sumaré micro-region did not establish any mechanism to ensure the assessment of mothers after delivery or of the children who were infected after birth. The authors also found that the prenatal information recorded on the notification forms and in the clinical records, which might have contributed to the late diagnoses of congenital syphilis, was poor2929. Donalísio MR, Freire JB, Mendes ET. Investigação da sífilis congênita na microrregião de Sumaré, estado de São Paulo, Brasil - desvelando a fragilidade do cuidado à mulher gestante e ao recém-nascido. Epidemiol Serv Saude 2007; 16:165-173.. Therefore, one should pay attention to records because inappropriate follow-up of newborn infants might lead to underdiagnosing late congenital syphilis.
The population of the present study mostly comprised adult black mothers with low educational levels who attended prenatal care, who were diagnosed with syphilis during pregnancy, and whose partners had not been treated for syphilis.
Incomplete notification forms, underreporting, discrepancies in the data provided by SINAN and SINASC, and differences in the categories used by SINAN before and after 2006 represent some of the limitations of the present study.
Because the present investigation was merely an ecological study, further research is necessary to investigate the causes of these findings. In addition, the impact of social inequities (e.g., inadequate prenatal care attendance, low maternal educational levels, black ethnicity) on the incidence of congenital syphilis calls attention to the relevance of actions aimed at reducing inequity and, consequently, the incidence of congenital syphilis, which is preventable by early diagnosis and appropriate treatment3030. Araújo EC, Moura AFA, Ramos FLP, Holanda VGDA. Sífilis congênita: incidência em recém-nascidos. J Pediatr 1999; 75:119-125.. Moreover, hindrances to strategies for achieving appropriate prevention of mother-to-child transmission of syphilis deserve attention. Future studies might also approach the integration of the various types of healthcare services available for treating pregnant women, the surveillance and monitoring systems, the healthcare supply, human resources, and the lack of certain resources, such as diagnostic tests for congenital syphilis and related diseases.
REFERENCES
-
1Mabey D, Peeling RW. Syphilis, still a major cause of infant mortality. Lancet Infect Dis 2011; 11:654-655.
-
2Avelleira JCR, Bottino G. Sífilis: diagnóstico, tratamento e controle. An Bras Dermatol 2006; 81:111-126.
-
3Smeltzer SC, Bare BG. Tratado de enfermagem médico cirurgica. 10ª ed. Guanabara Koogan: Rio de Janeiro; 2005.
-
4Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Protocolo para prevenção da transmissão vertical do HIV e sífilis. Brasília: Ministério da Saúde; 2007.
-
5Walker DG, Walker GJ. Forgotten but not gone: the continuing scourge of congenital syphilis. Lancet Infect Dis 2002; 2:432-436.
-
6Finelli L, Berman SM, Koumans EH, Levine WC. Congenital syphilis. Bull World Health Organ 1998; 76 (suppl II):126-128.
-
7Schmid G. Economic and programmatic aspects of congenital syphilis prevention. Bull World Health Organ 2004; 82:402-409.
-
8Valderrama J, Zacarías F, Mazin R. Maternal syphilis and congenital syphilis in Latin America: big problem, simple solution. Rev Panam Salud Publica 2004; 16:211-217.
-
9Centers for Disease Control and Prevention (CDC), Department of Health and Human Services. Sexually transmitted disease surveillance. Atlanta, GA: CDC; 2004.
-
10Tikhonova L, Salakhov E, Southwick K, Shakarishvili A, Ryan C, Hillis S. Congenital syphilis in the Russian Federation: magnitude, determinants, and consequences. Sex Transm Infect 2003; 79:106-110.
-
11Ministério da Saúde; Sistema de Informações sobre Nascidos Vivos-Notas técnicas [Internet]. Brasília: MS; 2012 [Cited 2012 March 10]. Available at: http://tabnet. datasus. gov. br/cgi/sinasc/nvdescr.Htm/
» http://tabnet -
12Rede Interagencial de Informação para a Saúde. Organização Pan-Americana da Saúde. Indicadores básicos para a saúde no Brasil: conceitos e aplicações. Brasília: Organização Pan-Americana da Saúde; 2008.
-
13Araújo CL. Análise da situação da sífilis congênita e da sua relação com a cobertura da estratégia de saúde da família no Brasil (2001 a 2008) [Dissertatio]. [Brasília]: Universidade de Brasília; 2010.
-
14Jacinto S, Henriques M, Ferreira T, Carvalhosa G, Costa T, Valido AM. A sífilis congénita ainda existe! Análise retrospectiva de 12 anos de uma grande maternidade. Acta Pediatr Port 2007; 38: 65-68.
-
15Ministério da Saúde, Secretaria de Vigilância em Saúde, Programa Nacional de DST e AIDS. Diretrizes para o controle de sífilis congênita: manual de bolso. Brasília: Ministério da Saúde, 2006.
-
16Lima MG, Santos RF, Barbosa GJ, Ribeiro GS. Cien Saude Colet 2013; 18:499-506.
-
17Chen XS, Yin YP. Syphilis: still a major cause of infant mortality. Lancet Infect Dis 2012; 12:269-270.
-
18Rodrigues CS, Guimarães MDC, Comini CC. Missed opportunities for congenital syphilis and HIV perinatal transmission prevention. Rev Saude Publica 2008; 42:851-858.
-
19Puccini RF, Pedroso GC, Silva EMK, Araújo NS, Silva NN. Eqüidade na atenção pré-natal e ao parto em área da Região Metropolitana de São Paulo, 1996. Cad Saude Publica 2003; 19:35-45.
-
20Araújo CL, Shimizu HE, Sousa AI, Hamann EM. Incidence of congenital syphilis in Brazil and its relationship with the Family Health Strategy. Rev Saude Publica 2012; 46:479-486.
-
21Trevisan MR, De Lorenzi DRS, Araújo NM, Ésber K. Perfil da assistência pré-natal entre usuárias do Sistema Único de Saúde em Caxias do Sul. Rev Bras Ginecol Obstet 2002; 24:293-299.
-
22Revollo R, Tinajeros F, Hilari C, García SG, Zegarra L, Díaz-Olavarrieta C, et al. Maternal and congenital syphilis in four provinces in Bolivia. Salud Publica Mex 2007; 49:422-428.
-
23Gottlieb SL, Pope V, Sternberg MR, McQuillan GM, Beltrami JF, Berman SM, et al. Prevalence of syphilis serore activity in the United States: data from the National Health and Nutrition Examination Surveys (NHANES) 2001-2004. Sex Transm Dis 2008; 35:507-511.
-
24Campos ALA, Araújo MAL, Melo SP, Gonçalves MLC. Epidemiologia da sífilis gestacional em Fortaleza, Ceará, Brasil: um agravo sem controle. Cad Saude Publica 2010; 26:1747-1755.
-
25Araujo EC, Costa KSG, Silva RS, Azevedo VNG, Lima FAS. Importância do pré-natal na prevenção da Sífilis Congênita. Rev Para Med 2006; 20:47-51.
-
26Lorenzi DRS, Madi JM. Sífilis Congênita como indicador de assistência pré-natal. Rev Bras Ginecol Obstet 2001; 23:647-652.
-
27Walker GJ, Walker DG. Congenital syphilis: a continuing but neglected problem. Semin Fetal Neonatal Med 2007; 12:198-206.
-
28Hawkes S, Matin N, Broutet N, Low N. Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 2011; 11:684-691.
-
29Donalísio MR, Freire JB, Mendes ET. Investigação da sífilis congênita na microrregião de Sumaré, estado de São Paulo, Brasil - desvelando a fragilidade do cuidado à mulher gestante e ao recém-nascido. Epidemiol Serv Saude 2007; 16:165-173.
-
30Araújo EC, Moura AFA, Ramos FLP, Holanda VGDA. Sífilis congênita: incidência em recém-nascidos. J Pediatr 1999; 75:119-125.
Publication Dates
-
Publication in this collection
Mar-Apr 2014
History
-
Received
24 Feb 2014 -
Accepted
14 Apr 2014