Abstract
INTRODUCTION:
Chikungunya fever is a condition resulting from infection by chikungunya virus (CHIKV), an Aedes sp.-transmitted virus. This disease has been diagnosed in thousands of cases in the Americas, particularly in Brazil, in recent years, and there is an ongoing epidemic of chikungunya fever in Brazil that began in 2014. Clinical diagnosis is difficult; only a few cases have been confirmed by laboratory tests due to the low number of specific, efficient tests available for virus or antibody detection. Here, we aimed to evaluate different polymerase chain reaction (PCR) approaches for detection of CHIKV genetic material.
METHODS:
Specific primers and probes within the viral capsid gene region were designed for this work. To evaluate the analytic sensitivity of detection, human sera were spiked with serial dilutions of the viral stock. Several PCR protocols were performed to investigate the sensitivity of CHIKV RNA detection in serum dilutions ranging from 106 to 1 PFU equivalents.
RESULTS:
The technique showing the greatest sensitivity was a real-time PCR assay using specific probes that could detect the genetic material of the virus at all dilutions, followed by conventional PCR. Digital PCR showed low sensitivity and was much more expensive than other technologies. Digital PCR should be used for specific purposes other than clinical diagnosis.
CONCLUSIONS:
Although quantitative PCR using probes was more expensive than the use of intercalating dyes or conventional PCR, it had the highest sensitivity out of all tested PCR approaches.
Keywords:
Chikungunya vírus; Alphavirus; Digital polymerase chain reaction; Arboviruses quantitative polymerase chain reaction
INTRODUCTION
Chikungunya fever is a mosquito-borne viral disease transmitted by Aedes sp., particularly Aedes aegypti and A. albopictus11. Enserink M. Infectious diseases. Massive outbreak draws fresh attention to little-known virus.Science. 2006;311(5764):1085., and is found mostly in tropical countries, although the origin of the disease is thought to be Africa. The first occurrence of chikungunya fever occurred in 1952-1953 in Tanzania, after viral isolation from a febrile patient22. AbuBakar S, Sam IC, Wong PF, MatRahim N, Hooi PS, Roslan N.. Reemergence of endemic Chikungunya, Malaysia. Emerg Infect Diseases. 2007;13(1):147-9.. Chikungunya virus (CHIKV) is a spherical enveloped virus with icosahedral symmetry, a diameter of about 60-70nm, and a positive, single-stranded ribonucleic acid (RNA) genome of approximately 12,000 nucleotides33. Kuhn RJ. Togaviridae. In: Knipe DM, Howlwey Fields Virology. 6th edition. Philadelphia: Lippincott Williams & Wilkins; 2013. p. 629-650.. The genome is composed of two open read frames that encode a nonstructural polyprotein, which is cleaved into four nonstructural proteins (nsP1-4), and a structural polyprotein, which is cleaved into five structural proteins (C, E3, E2, 6K, and E1)44. Khan AH, Morita K, Parquet MC, Hasebe F, Mathenge EGM, Igarashi A. Complete nucleotide sequence of chikungunya virus and evidence for an internal polyadenylation site. J Gen Virol. 2002;83(Pt 12):3075-84..
The clinical manifestations of chikungunya fever include high fever, skin rash, myalgia and severe joint pain and can persist for years after infection55. Morrison TE. Reemergence of chikungunya virus. J Virol. 2014;88(20):11644-7.. There are no efficient antiviral therapies for CHIKV infection, and treatment aims to manage symptoms, e.g., analgesics and rehydration. No commercial vaccines are available, and vector control is still the only effective approach to prevent the spread of the disease66. Sam IC, AbuBakar S. Chikungunya virus infection. Med J Malaysia 2006;61(2):264-9..
Most CHIKV diagnostics are performed based on clinical outcomes; however, it can be difficult to differentiate CHIKV infection from other arboviruses, since the symptoms are very similar. Laboratory tests are critical for distinguishing this infection from other acute febrile illnesses, and viral isolation can be performed for detection of CHIKV. Unfortunately, these methods are time-consuming and cannot be performed in all laboratories. Reverse transcription polymerase chain reaction (RT-PCR) during the acute phase of infection and detection of immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies against CHIKV (by enzyme-linked immunosorbent assay, immunofluorescent tests, or neutralization assays) are also used, but only for small-scale analyses77. Mohan A, Kiran DNH, Manohar IC, Kumar DP. Epidemiology, clinical manifestations, and diagnosis of Chikungunya fever: lessons learned from the re-emerging epidemic. Indian J Dermatol. 2010;55(1):54-63..
Johnson and coworkers analyzed several commercially available tests to diagnose CHIKV infections during both the acute and convalescent phases. According to the authors, the Center for Disease Control and Prevention (CDC) evaluated serological kits for anti-CHIKV antibodies in patient serum and showed that only 20% (2/10) kits showed acceptable results. Moreover, for viral RNA detection by real-time reverse transcription polymerase chain reaction (RT-PCR), the sensitivity of the tests is variable, and detection ranges from less than 100 to 5.3 copies88. Johnson BW, Russell BJ, Goodman CH. 2016. Laboratory Diagnosis of Chikungunya Virus Infections and Commercial Sources for Diagnostic Assays. J Infect Dis. 2016;214(suppl 5):S471-S474..
In Brazil, the first cases of autochthonous CHIKV infection were reported in late 2013 in the northern and northeastern part of the country, where the climate and the presence of Aedes aegypti permitted epidemic state99. Nunes MRT, Faria NR, de Vasconcelos JM, Golding N, Kraemer MUG, de Oliveira LF, et al. Emergence and potential for spread of Chikungunya virus in Brazil. BMC Medicine. 2015;13:102.. According to the Brazilian Ministry of Health, from 2014 until March 2017, there were more than 330,000 suspected cases of autochthonous CHIKV transmission1010. Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico. Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a Semana Epidemiológica 10. Brasília: Ministério da Saúde; 2017. volume 48, nº 10, p. 1-10. [Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2017/marco/31/Monitoramento-dos-casos-de-dengue-febre-de-chikungunya-e-febre-pelo-virus-Zika-10-%202017.pdf.
http://portalarquivos.saude.gov.br/image...
, although few were confirmed by laboratory tests and most were characterized based on clinical-epidemiological evidence.
Thus, because of the scarcity of precise, specific tests to confirm CHIKV infection, we conducted the present study to analyze different PCR approaches for detection of the genetic material of CHIKV in spiked serum samples. Additionally, we evaluated the sensitivity of the assays and performed a cost-benefit analysis for each protocol.
METHODS
Virus isolation and titration
The CHIKV strain BzH1 used in this study was sequenced, and the sequence was deposited in the National Center for Biotechnology Information (NCBI) database under GenBank accession number KT581023. Viral stock was produced in VERO cells. After infecting the cell monolayer and verifying the cytopathic effect (2-3 days), the supernatant was collected and subjected to ultracentrifugation (2h at 110,000 × g, 4ºC) to concentrate viral stock. Virus stocks were titrated by plaque assays in VERO cells, and virus titers are presented as plaque-forming units (PFU)/mL.
Design of the primers and probe
After alignment of the whole-genome sequences of CHIKV available on NCBI, primers and a probe were designed within the capsid gene region, amplifying an 89-bp region. Primer sensitivity was evaluated by quantitative polymerase chain reaction (qPCR) using a plasmid that was previously cloned as a template. The sequences of the primers and probe and the optimal concentration are described in Table 1.
Virus dilution
A 10-fold serial dilution of CHIKV was spiked in the serum of a healthy donor (PCR, IgM, and IgM-negative for alphaviruses and flaviviruses) at 106-1 PFU equivalents/dilution.
RNA extraction and cDNA synthesis
RNA from all dilutions was extracted with a kit specific for viral RNA (QiaAmp Viral RNA Mini Kit; Qiagen, Valencia, CA, USA) according to the manufacturer’s protocol. A sample of only serum was also extracted as a negative control. cDNA was synthesized with a high-capacity reverse transcriptase (High-Capacity cDNA Reverse Transcriptase; Thermo Fisher, Massachusetts, USA).
PCR approaches
One microliter of cDNA was used in all different PCR approaches in order to equalize the amount of genetic material. The final volume was set to 15μL for all techniques. Conventional PCR was performed using TopTaq Master mix (Qiagen) in a Veriti Thermocycler. Real-time PCR using SYBR Green (Quantifast SYBR Qiagen), EVA Green (Biotium), or probes (Quantitect Virus; Qiagen) were performed in a RealPlex 4 Thermocycler (Eppendorf). Supplies from Applied Biosystems (Foster City, CA, USA) were used to perform digital polymerase chain reaction (dPCR) experiments (Quantstudio 3D 20K chip and Master mix), including equipment (Chip Loader, Proflex Thermal Cycler, and Quantstudio 3D reader). The annealing temperature for all protocols was 61°C, and the extension temperature was 72°C (even for optimized DNA polymerases).
Due to the small input volume required in dPCR, we decided to standardize all techniques using a fixed volume instead of the same concentration of genetic material; the volume used was close to the maximum required for the technique. Additionally, when working with patient samples, particularly large numbers of samples, the use of volume is easier and less laborious than fixing the concentration of genetic material. Sample to sample variation can still exist, however, because viral load fluctuation among samples is frequent.
PCR specificity for CHIKV detection
The new set of primers and probe was tested against other alphaviruses (Eastern Equine Encephalitis, Western Equine Encephalitis, Mucambo, Mayaro, Venezuelan Equine Encephalitis, and Aura viruses) and flaviviruses (Dengue viruses, serotypes 1, 2, 3 and 4; West Nile, Yellow Fever, Saint Louis encephalitis, and Zika viruses). RT-qPCR using probes and conventional PCR for all these viruses were performed as described above.
RESULTS
Virus titration and efficiency test
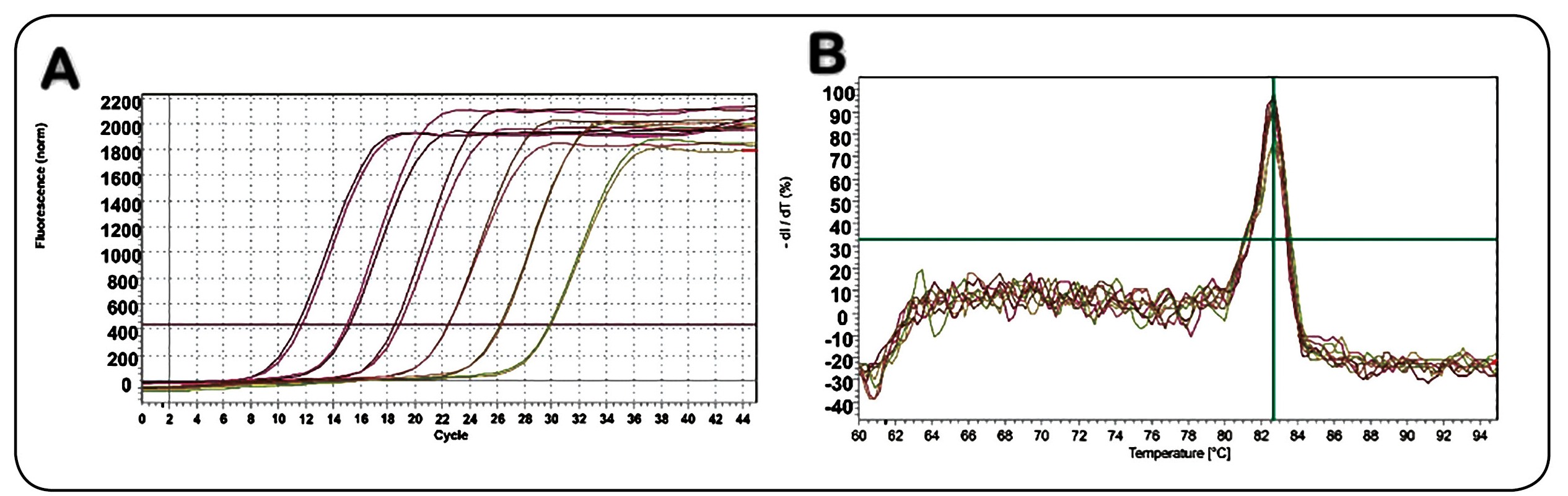
After centrifugation, the titer of CHIKV stock was 1 × 107 PFU/mL. The amplicon was cloned into a TA cloning vector (Topo TA Cloning Kit; Thermo Fisher, Massachusetts, USA), and serial 10-fold dilutions were made to optimize PCR parameters and to test the sensitivity of primers. The cloned plasmid was also used as a positive control. As shown in Figure 1A, the coefficient of determination (R2) for the plasmid standard curve was equal to 1, with an efficiency of 88%, indicating the great sensitivity of the designed primers. The negative control was not amplified under the cycling conditions optimized in this work, and the melting curve (Figure 1B), with only one peak at 82.7°C, supported the specificity of the primers.
A: Plasmid standard curve showing the sensitivity of the designed primers, using SYBR Green. B: Melting curve, with a unique peak temperature of 82.7°C.
PCR approaches
Conventional PCR was able to detect as low as 10 PFU equivalents per dilution (Figure 2). The best result was obtained with real-time PCR using specific probes, which amplified CHIKV genetic material at all dilutions.
Conventional PCR of CHIKV genetic material in spiked serum dilution. Lane 1: 100-bp ladder; Lane 2: negative control; Lanes 3-9: virus dilutions ranging from 106 to 1 copy. PCR: polymerase chain reaction; CHIKV: Chikungunya virus.
Digital PCR had the lowest sensitivity of all techniques. SYBR Green was slightly better than EVA Green. The results from all approaches are shown in Table 2.
A cost analysis per sample and the amount of time required from extraction through analysis are shown in Table 3.
PCR specificity for CHIKV
No amplification was found, either by the probe-based RT-qPCR or with conventional PCR, for all other alphaviruses and flaviviruses. Thus, the new set of proposed primers for molecular detection of CHIKV RNA was specific and could be used in regions in which several arboviral diseases coexisted.
DISCUSSION
CHIKV is an emergent pathogen that has caused many disease outbreaks in humans in southeast Asia, Indonesia, China, Polynesia, and South America1111. Rowland-Jones SL. Chikungunya: out of the tropical forests and heading our way. Trans R Soc Trop Med Hyg. 201;110(2):85-6.. In subtropical countries, such as Brazil, which harbor several viruses that can cause similar symptoms, e.g., dengue virus, CHIKV, Mayaro virus, yellow fever virus, and, more recently, Zika virus, obtaining an appropriate diagnosis is essential for effective treatment of the infection. CHIKV infection is usually diagnosed based on clinical criteria during an outbreak, and no specific, reliable laboratory tests for detection of CHIKV have been developed.
Viral isolation can be performed in cell lines and by intracerebral inoculation of newborn mice; however, these methods are time-consuming and laborious. Alternatively, molecular assays are available for CHIKV detection; however, they can be difficult to implement in some settings due to the lack of technology or high costs of tests. Conventional and real-time PCR have been used to amplify nsP1, nsP2, or even envelope protein genes (e.g., E3, E2, or E1)1212. de Morais Bronzoni RV, Baleotti FG, Ribeiro Nogueira RM, Nunes M, Moraes Figueiredo LT. Duplex reverse transcription-PCR followed by nested PCR assays for detection and identification of Brazilian alphaviruses and flaviviruses. J Clin Microbiol. 2005;43(2):696-702.,1414. Carletti F, Bordi L, Chiappini R, Ippolito G, Sciarrone MR, Capobianchi MR, et al. Rapid detection and quantification of Chikungunya virus by a one-step reverse transcription polymerase chain reaction real-time assay. Am J Trop Med Hyg. 2007;77(3):521-524.. Loop-mediated isothermal amplification has also been proposed; this method amplifies nucleic acid under isothermal conditions without the use of a thermal cycler and is a fast, specific, and cost-effective technique1515. Parida MM. Rapid and real-time detection technologies for emerging viruses of biomedical importance. J Biosciences 2008;33(4):617-28.. Overall, identification of a rapid, sensitive test during the acute phase of the disease is critical for improving treatment options and controlling the infection.
In this current work, we designed a set of primers and a probe to detect CHIKV infection with high precision and evaluated different PCR approaches in terms of sensitivity, cost-effectiveness, and time requirements. Conventional PCR showed great sensitivity and did not detect only the last dilution (1 PFU equivalent). Although this was also the least expensive technique and did not require expensive equipment, conventional PCR requires laborious post-PCR handling and electrophoresis, which can increase the total time of the analysis and requires the handling of ethidium bromide and exposure to ultraviolet light1616. Mackay IM, Arden KE, Nitsche A. Real-time PCR in virology. Nucleic Acids Res. 2002;30(6):1292-1305..
The use of intercalating dyes and probes together with optimized polymerases for amplification of genetic material made real-time PCR a faster and more efficient technique and permitted the quantification of gene expression and/or viral load with no postamplification handling1616. Mackay IM, Arden KE, Nitsche A. Real-time PCR in virology. Nucleic Acids Res. 2002;30(6):1292-1305.. In our work, SYBR Green and EVA Green both showed average detection of the dilutions within 40 cycles of amplification. SYBR Green was slightly better than EVA Green, and the reaction cost was very similar. Additionally, there were no differences in the time requirements for assays using the two reagents. As nonspecific dyes, both techniques require melting curve analysis and optimization of the reagent and primer concentrations in order to avoid generating false-positive/-negative results. There was a slight difference in the temperature of the melting curve peak between SYBR Green and EVA Green, due to dye saturation (82.7 and 83.4°C, respectively).
The use of real-time pCR with DNA probes that anneal to the DNA target is the preferred method for diagnosing pathogens in clinical research because the fluorescent signal is only emitted during specific amplification of the target sequence1717. Yang S, Rothman RE. PCR-based diagnostics for infectious diseases: uses, limitations, and future applications in acute-care settings. Lancet Infect Dis. 2004;4(6):337-48.. Additionally, there is a decrease in the total execution time with this protocol compared with qPCR using intercalant dyes because no melting curve is necessary after the amplification steps. In our study, qPCR using hydrolytic probes showed the highest sensitivity, amplifying all sample dilutions. Besides being slightly more expensive than conventional PCR or those using intercalant dyes, this method was more reliable, practical, and precise than the other methods.
dPCR showed very low sensitivity to detect large amounts of PFU equivalents and may not be suitable for detection of infections with high viral loads. This recently developed technique uses an algorithmic analysis by Poisson distribution to precisely quantify the amount of DNA in a sample. Extensive optimization is required, and dPCR is also the most expensive technique tested in this study. However, dPCR is necessary for detection of small viral loads or rare mutation/genes, and dPCR permits high absolute quantification when compared with other techniques1818. Whale AS, Huggett JF, Cowen S, Speirs V, Shaw J, Ellison S, et al. Comparison of microfluidic digital PCR and conventional quantitative PCR for measuring copy number variation. Nucleic Acids Res . 2012;40(11):e82.. However, the limit of detection is usually 3-10 molecules/μL1919. White 3rd RA, Quake SR, Curr K. Digital PCR provides absolute quantitation of viral load for an occult RNA virus. J Virol Methods. 2012;179(1):45-50. due to the need for positive/negative wells inside the chip in order to apply the Poisson distribution.
The total time for performing the procedures did not differ much among the assays, and all assays were performed according to the manufacturers’ specifications for each kit. Some enzymes had different activation times and cycle conditions. The total time included extraction and reverse transcription, which were the same for all approaches.
Although PCR is more expensive than other techniques, such as virus isolation, it is also more reliable, and there is no need for a confirmation test. Our cost-effectiveness analysis did not include equipment or training of personnel, and costs can vary depending on the brand of reagents used. However, the overall benefit of PCR for detection of pathogens is enormous when compared with other techniques, and PCR represents a relatively quick and reliable diagnostic tool. qPCR using probes showed the best result among all protocols tested in this study, and although this technique is not always feasible, it can be a powerful tool to detect CHIKV infection during the acute phase of the disease.
In conclusion, in this study, we described an assay for molecular detection of CHIKV RNA with a new set of primers and a probe and compared this assay with several technical PCR approaches. Of all PCR protocols, real-time PCR using probes was the most sensitive technique and was specific for CHIKV when tested against other circulating arboviral diseases with similar symptoms.
Although some papers in the literature have stated that real-time PCR is more sensitive and, in most cases, more specific for several diseases, this was the first time that a comparison using all three PCR techniques, with very well standardized procedures, was performed for detection of CHIKV genetic material. The methodologies described herein, including the new set of primers, could help improve the diagnosis of CHIKV infection and differentiate CHIKV from other cocirculating arboviral diseases.
REFERENCES
-
1Enserink M. Infectious diseases. Massive outbreak draws fresh attention to little-known virus.Science. 2006;311(5764):1085.
-
2AbuBakar S, Sam IC, Wong PF, MatRahim N, Hooi PS, Roslan N.. Reemergence of endemic Chikungunya, Malaysia. Emerg Infect Diseases. 2007;13(1):147-9.
-
3Kuhn RJ. Togaviridae. In: Knipe DM, Howlwey Fields Virology. 6th edition. Philadelphia: Lippincott Williams & Wilkins; 2013. p. 629-650.
-
4Khan AH, Morita K, Parquet MC, Hasebe F, Mathenge EGM, Igarashi A. Complete nucleotide sequence of chikungunya virus and evidence for an internal polyadenylation site. J Gen Virol. 2002;83(Pt 12):3075-84.
-
5Morrison TE. Reemergence of chikungunya virus. J Virol. 2014;88(20):11644-7.
-
6Sam IC, AbuBakar S. Chikungunya virus infection. Med J Malaysia 2006;61(2):264-9.
-
7Mohan A, Kiran DNH, Manohar IC, Kumar DP. Epidemiology, clinical manifestations, and diagnosis of Chikungunya fever: lessons learned from the re-emerging epidemic. Indian J Dermatol. 2010;55(1):54-63.
-
8Johnson BW, Russell BJ, Goodman CH. 2016. Laboratory Diagnosis of Chikungunya Virus Infections and Commercial Sources for Diagnostic Assays. J Infect Dis. 2016;214(suppl 5):S471-S474.
-
9Nunes MRT, Faria NR, de Vasconcelos JM, Golding N, Kraemer MUG, de Oliveira LF, et al. Emergence and potential for spread of Chikungunya virus in Brazil. BMC Medicine. 2015;13:102.
-
10Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico. Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a Semana Epidemiológica 10. Brasília: Ministério da Saúde; 2017. volume 48, nº 10, p. 1-10. [Disponível em: http://portalarquivos.saude.gov.br/images/pdf/2017/marco/31/Monitoramento-dos-casos-de-dengue-febre-de-chikungunya-e-febre-pelo-virus-Zika-10-%202017.pdf.
» http://portalarquivos.saude.gov.br/images/pdf/2017/marco/31/Monitoramento-dos-casos-de-dengue-febre-de-chikungunya-e-febre-pelo-virus-Zika-10-%202017.pdf. -
11Rowland-Jones SL. Chikungunya: out of the tropical forests and heading our way. Trans R Soc Trop Med Hyg. 201;110(2):85-6.
-
12de Morais Bronzoni RV, Baleotti FG, Ribeiro Nogueira RM, Nunes M, Moraes Figueiredo LT. Duplex reverse transcription-PCR followed by nested PCR assays for detection and identification of Brazilian alphaviruses and flaviviruses. J Clin Microbiol. 2005;43(2):696-702.
-
13Pastorino B, Bessaud M, Grandadam M, Murri S, Tolou HJ, Peyrefitte CN. Development of a TaqMan RT-PCR assay without RNA extraction step for the detection and quantification of African Chikungunya viruses. J Virol Methods. 2005;124(1-2):65-71.
-
14Carletti F, Bordi L, Chiappini R, Ippolito G, Sciarrone MR, Capobianchi MR, et al. Rapid detection and quantification of Chikungunya virus by a one-step reverse transcription polymerase chain reaction real-time assay. Am J Trop Med Hyg. 2007;77(3):521-524.
-
15Parida MM. Rapid and real-time detection technologies for emerging viruses of biomedical importance. J Biosciences 2008;33(4):617-28.
-
16Mackay IM, Arden KE, Nitsche A. Real-time PCR in virology. Nucleic Acids Res. 2002;30(6):1292-1305.
-
17Yang S, Rothman RE. PCR-based diagnostics for infectious diseases: uses, limitations, and future applications in acute-care settings. Lancet Infect Dis. 2004;4(6):337-48.
-
18Whale AS, Huggett JF, Cowen S, Speirs V, Shaw J, Ellison S, et al. Comparison of microfluidic digital PCR and conventional quantitative PCR for measuring copy number variation. Nucleic Acids Res . 2012;40(11):e82.
-
19White 3rd RA, Quake SR, Curr K. Digital PCR provides absolute quantitation of viral load for an occult RNA virus. J Virol Methods. 2012;179(1):45-50.
-
Financial support:Fundação de Apoio ao Ensino, Pesquisa e Assistência do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto (FAEPA).
Publication Dates
-
Publication in this collection
Jul-Aug 2017
History
-
Received
30 Sept 2016 -
Accepted
30 June 2017