Abstract
Basidiobolomycosis is an unusual fungal skin infection that rarely involves the gastrointestinal tract. This study reported a 5-year-old boy with gastrointestinal basidiobolomycosis that had been misdiagnosed as gastrointestinal lymphoma. He was treated by surgical resection and a combination of posaconazole and amphotericin B deoxycholate with an acceptable response and no recurrence.
Keywords:
Basidiobolomycosis; Lymphoma; Gastrointestinal
INTRODUCTION
Basidiobolomycosis (BM) is a rare infection caused by the fungus Basidiobolus ranarum (B. ranarum). BM is an environmental saprophyte found throughout the world and often infects immunocompetent patients. Patients with B. ranarum infection may present with subcutaneous, gastrointestinal, or systemic lesions11. Zabolinejad N, Naseri A, Davoudi Y, Joudi M, Aelami MH. Colonic basidiobolomycosis in a child: report of a culture-proven case. Int J Infect Dis. 2014;22:41-3.,22. Ejtehadi F, Anushiravani A, Bananzadeh A, Geramizadeh B. Gastrointestinal basidiobolomycosis accompanied by liver involvement: a case report. Iran Red Crescent Med J. 2014;16(9):e14109..
Diagnosis of gastrointestinal BM is difficult, and its clinical presentation is nonspecific, with no identifiable risk factors. An optimal treatment regimen for this uncommon infection has not yet been established. This study presents a boy with colonic BM involving the liver, masquerading as gastrointestinal lymphoma.
CASE REPORT
A 5-year-old boy, living in Bushehr province in the south of Iran, was referred to an oncology center affiliated with Shiraz University of Medical Sciences. He had a 2-month history of diffuse abdominal pain, non-bilious vomiting, poor appetite, weight loss, and a detectable mass on abdominal sonography. He had no fever, diarrhea, constipation, jaundice, or lower GI bleeding. He also had no recent history of travel abroad.
In his physical examination, he seemed ill and emaciated, his body temperature was 39°C, and his liver was tender on palpation 3cm inferior to the costal margin. His laboratory results are shown in Table 1.
Abdominopelvic CT (Computerized Tomography)scan showed multiple heterogeneous densities in the liver and a significantly thickened edematous intestinal wall with stratification of the ascending colon throughout the hepatic flexure, the adjacent part of the transverse colon, the cecum, and the terminal ileum. A mass measuring about 3.5 × 5cm infiltrated to the cecum and ascending colon as well as the terminal ileum, extending to the hepatic flexure in direct contact with the gallbladder. Multiple lymphadenopathies were detected. The mass was similar to Castleman's disease, lymphoma, or tuberculosis (Figure 1). Accordingly, gastrointestinal lymphoma was suspected.
A: Abdominal computed tomography scan shows multiple homogenous parenchymal densities in the liver. B: Plain abdominal radiogram, upright.
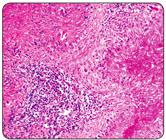
Colonoscopy with multiple biopsies was performed, revealing acute and chronic inflammation with numerous eosinophils and poorly shaped granulomas. The granulomas were surrounded with giant cells, morphologically consistent with fungal elements, and periodic acid-Schiff and Gomori-methenamine silver stains were both positive. These symptoms are indicative of BM (Figure 2).
Histopathology of surgically resected abdominal mass: hematoxylin and eosin stain (× 100), demonstrating granulomatosis inflammation with central necrosis and numerous eosinophils.
An exploratory laparotomy showed a mass connected to the anterior abdominal wall, involving the cecum, ileum, and ascending colon. En-bloc surgical resection of the mass was performed. At surgical resection, the mass involved the internal oblique and transversus abdominis muscle, and there was a small area of peritoneal ulceration, which was excised by a surrounding margin of healthy tissue. The specimen was sent for histopathological evaluation and culture, which revealed the presence of fungal hyphae with large width and thin walls, surrounded by eosinophils with multinucleated giant cells, lymphocytes, and histiocytes. A biopsy specimen from the omentum showed fat necrosis. Culture results of the mass indicated white to grey colonies with radiated folds that were consistent with gastrointestinal basidiobolomycosis. The results of other laboratory work for immunodeficiency such as the dihydrorhodamine (DHR) flow cytometric test, immunoglobulin and anti-tetanus antibody levels, and CH50 levels were in the normal range. HIV serology also was negative.
Treatment with amphotericin B (intravenous 1mg/kg/day for 2 months) and posaconazole (200mg by mouth four times per day) was started. The patient was followed closely by means of physical exams and abdominal computed tomography scans, which revealed no recurrence 6 months after starting therapy with posaconazole. Written informed consent was obtained from the parents.
DISCUSSION
Basidiobolomycosis is an unusual fungal infection with skin manifestation and rarely involves other systems. It is caused by B. ranarum, which infects immunocompromised patients and is an opportunistic pathogen in immunocompetent individuals22. Ejtehadi F, Anushiravani A, Bananzadeh A, Geramizadeh B. Gastrointestinal basidiobolomycosis accompanied by liver involvement: a case report. Iran Red Crescent Med J. 2014;16(9):e14109., such as the healthy, immunocompetent 5 year-old patient in the present case. Most similar cases with cutaneous involvement have been reported from tropical areas where the climate is warm and humid, such as Iran. In recent years, several cases of gastrointestinal BM in Iran have been reported33. Geramizadeh B, Foroughi R, Keshtkar-Jahromi M, Malek-Hosseini SA, Alborzi A. Gastrointestinal basidiobolomycosis, an emerging infection in the immunocompetent host: a report of 14 patients. J Med Microbiol. 2012;61(Pt 12):1770-4.
4. Geramizadeh B, Heidari M, Shekarkhar G. Gastrointestinal basidiobolomycosis, a rare and under-diagnosed fungal infection in immunocompetent hosts: a review article. Iran J Med Sci. 2015;40(2):90-7.
5. Seyedmousavi S, Guillot J, Tolooe A, Verweij PE, de Hoog GS. Neglected fungal zoonoses: hidden threats to man and animals. Clin Microbiol Infect. 2015;21(5):416-25.-66. Van den Berk GE, Noorduyn LA, van Ketel RJ, van Leeuwen J, Bemelman WA, Prins JM. A fatal pseudo-tumour: disseminated basidiobolomycosis. BMC Infect Dis. 2006;6:140..
It is unclear how the fungus is introduced into the host’s gastrointestinal tract, but it may occur through ingestion of contaminated soil, food, or exposure to animal feces44. Geramizadeh B, Heidari M, Shekarkhar G. Gastrointestinal basidiobolomycosis, a rare and under-diagnosed fungal infection in immunocompetent hosts: a review article. Iran J Med Sci. 2015;40(2):90-7.. Alternatively, it may be a zoonotic fungus77. Bittencourt AL, Andrade JA, Carvalho EM. Basidiobolomicose: Registro de um caso com aspectos incomuns. Rev Inst Med Trop Sao Paulo. 1987;29(6):381-4.,88. Pasha TM, Leighton JA, Smilack JD, Heppell J, Colby TV, Kaufman L. Basidiobolomycosis: an unusual fungal infection mimicking inflammatory bowel disease. Gastroenterology. 1997;112(1):250-4..
The clinical manifestations of gastrointestinal BM include abdominal pain, fever, vomiting, weight loss, and abdominal mass, which can be found during abdominal examination, by imaging, or during laparotomy, as it was in the current patient. The presence of an abdominal mass may be misdiagnosed as malignancy, especially Burkitt’s lymphoma or as an inflammatory process such as appendicular mass, inflammatory bowel disease, or other infectious diseases including intestinal tuberculosis, sarcoidosis, and amebiasis99. Mathew R, Kumaravel S, Kuruvilla S, Varghese RG, Shashikala MD, Srinivasan S, et al. Successful treatment of extensive basidiobolomycosis with oral itraconazole in a child. Int J Dermatol. 2005;44(7):572-5.. Lack of awareness or facilities to diagnose such a rare disease contributes to missing an early diagnosis and an increased risk of morbidity. Leukocytosis, marked eosinophilia, and an elevated erythrocyte sedimentation rate and C-reactive protein level were present in the current case, as well as in prior reports1010. Rabie ME, El Hakeem I, Al-Shraim M, Al Skini MS, Jamil S. Basidiobolomycosis of the colon masquerading as stenotic colon cancer. Case Rep Surg. 2011;(2011):Article ID 685460..
Although there have been some reports of clinical improvement with antifungal therapy alone, most patients with disseminated abdominal infection have received a combination of surgical and medical therapies. An optimal treatment regimen for this uncommon fungal infection has not yet been established. The best choice of antifungal agent is not clear, but itraconazole has been used with success in many reports99. Mathew R, Kumaravel S, Kuruvilla S, Varghese RG, Shashikala MD, Srinivasan S, et al. Successful treatment of extensive basidiobolomycosis with oral itraconazole in a child. Int J Dermatol. 2005;44(7):572-5.,1111. Al-Maani AS, Paul G, Jardani A, Nayar M, Al-Lawati F, Al-Baluishi S, et al. Gastrointestinal basidiobolomycosis: first case report from Oman and literature review. Sultan Qaboos Univ Med J. 2014; 14(2):e241-4.. A study regarding the use of antifungal agents showed that itraconazole has been used most frequently for BM (73%), followed by amphotericin (22%), ketoconazole (8%), and voriconazole (5%); in addition, potassium iodide and trimethoprim/sulfamethoxazole may also have some clinical efficacy1212. Rose SR, Lindsley MD, Hurst SF, Paddock CD, Damodaran T, Bennett J. Gastrointestinal basidiobolomycosis treated with posaconazole. Med Mycol Case Rep. 2012;2:11-4.. Generally, antifungal therapy is used for 8 months, and overall survival is estimated at 80%. Clinical failure has been described with amphotericin B11. Zabolinejad N, Naseri A, Davoudi Y, Joudi M, Aelami MH. Colonic basidiobolomycosis in a child: report of a culture-proven case. Int J Infect Dis. 2014;22:41-3.,1111. Al-Maani AS, Paul G, Jardani A, Nayar M, Al-Lawati F, Al-Baluishi S, et al. Gastrointestinal basidiobolomycosis: first case report from Oman and literature review. Sultan Qaboos Univ Med J. 2014; 14(2):e241-4.,1212. Rose SR, Lindsley MD, Hurst SF, Paddock CD, Damodaran T, Bennett J. Gastrointestinal basidiobolomycosis treated with posaconazole. Med Mycol Case Rep. 2012;2:11-4..
The use of posaconazole in the present case had several potential advantages. For example, there was no need for dose adjustment in hepatic or renal insufficiency. Moreover, it was well tolerated with limited side effects, and its absorption was not inhibited by medications that affect gastric acidity1212. Rose SR, Lindsley MD, Hurst SF, Paddock CD, Damodaran T, Bennett J. Gastrointestinal basidiobolomycosis treated with posaconazole. Med Mycol Case Rep. 2012;2:11-4.. However, the limitations of using posaconazole include cost, the lack of an intravenous preparation for hospitalized patients, and the need for therapeutic monitoring due to variable absorption.
Gastrointestinal BM is an emerging disease in the south of Iran, so special attention should be given to patients exhibiting an abdominal mass with localized eosinophilia. Moreover, the present case demonstrates the importance of antifungal therapy. This study introduces posaconazole as an effective single agent treatment with minimum complications during a prolonged treatment plan.
REFERENCES
-
1Zabolinejad N, Naseri A, Davoudi Y, Joudi M, Aelami MH. Colonic basidiobolomycosis in a child: report of a culture-proven case. Int J Infect Dis. 2014;22:41-3.
-
2Ejtehadi F, Anushiravani A, Bananzadeh A, Geramizadeh B. Gastrointestinal basidiobolomycosis accompanied by liver involvement: a case report. Iran Red Crescent Med J. 2014;16(9):e14109.
-
3Geramizadeh B, Foroughi R, Keshtkar-Jahromi M, Malek-Hosseini SA, Alborzi A. Gastrointestinal basidiobolomycosis, an emerging infection in the immunocompetent host: a report of 14 patients. J Med Microbiol. 2012;61(Pt 12):1770-4.
-
4Geramizadeh B, Heidari M, Shekarkhar G. Gastrointestinal basidiobolomycosis, a rare and under-diagnosed fungal infection in immunocompetent hosts: a review article. Iran J Med Sci. 2015;40(2):90-7.
-
5Seyedmousavi S, Guillot J, Tolooe A, Verweij PE, de Hoog GS. Neglected fungal zoonoses: hidden threats to man and animals. Clin Microbiol Infect. 2015;21(5):416-25.
-
6Van den Berk GE, Noorduyn LA, van Ketel RJ, van Leeuwen J, Bemelman WA, Prins JM. A fatal pseudo-tumour: disseminated basidiobolomycosis. BMC Infect Dis. 2006;6:140.
-
7Bittencourt AL, Andrade JA, Carvalho EM. Basidiobolomicose: Registro de um caso com aspectos incomuns. Rev Inst Med Trop Sao Paulo. 1987;29(6):381-4.
-
8Pasha TM, Leighton JA, Smilack JD, Heppell J, Colby TV, Kaufman L. Basidiobolomycosis: an unusual fungal infection mimicking inflammatory bowel disease. Gastroenterology. 1997;112(1):250-4.
-
9Mathew R, Kumaravel S, Kuruvilla S, Varghese RG, Shashikala MD, Srinivasan S, et al. Successful treatment of extensive basidiobolomycosis with oral itraconazole in a child. Int J Dermatol. 2005;44(7):572-5.
-
10Rabie ME, El Hakeem I, Al-Shraim M, Al Skini MS, Jamil S. Basidiobolomycosis of the colon masquerading as stenotic colon cancer. Case Rep Surg. 2011;(2011):Article ID 685460.
-
11Al-Maani AS, Paul G, Jardani A, Nayar M, Al-Lawati F, Al-Baluishi S, et al. Gastrointestinal basidiobolomycosis: first case report from Oman and literature review. Sultan Qaboos Univ Med J. 2014; 14(2):e241-4.
-
12Rose SR, Lindsley MD, Hurst SF, Paddock CD, Damodaran T, Bennett J. Gastrointestinal basidiobolomycosis treated with posaconazole. Med Mycol Case Rep. 2012;2:11-4.
Publication Dates
-
Publication in this collection
Sep-Oct 2017
History
-
Received
14 Feb 2017 -
Accepted
20 June 2017