Abstract
Staphylococcus lugdunensis is a rare virulent coagulase-negative staphylococcus (CoNS) that behaves similarly to Staphylococcus aureus in causing deep abscesses, skin and soft tissue infections, and central nervous system infections. Additionally, there can be certain blood stream infections including sepsis, septic shock, toxic shock syndrome, and endocarditis complicated by embolic events. Reports of septic arthritis of a native joint associated with this organism have been infrequent, justifying the presentation and discussion of this case.
Keywords:
S. Lugdunensis; Native joint infection; Staphylococcal species joint infection
INTRODUCTION
Staphylococcus lugdunensis is a virulent coagulase-negative staphylococcus (CoNS) that behaves similarly to Staphylococcus aureus, and it has been associated with rare cases of osteomyelitis of the vertebra, prosthetic implants, and endocarditis. Routine microbiological laboratory analyses may misidentify S. lugdunensis, since the colony morphology often resembles that of S. aureus, which leads to the underreporting of this infection. More recent and improved identification methods have determined an incidence of 53 infections per 100,000 inhabitants per year, in contrast to previous estimates of 5 infections per 100,000 inhabitants per year11. Herchline TE, Ayers LW. Occurrence of Staphylococcus lugdunensis in consecutive clinical cultures and relationship of isolation to infection. J Clin Microbiol. 1999;29(3):419-21.. S. lugdunensis can be aggressive and virulent, highlighting the importance for the correct identification of this organism.
CASE REPORT
A 62-year-old African-American male on a methadone program for ten years, with a medical history of prior intravenous (IV) heroin use, hepatitis C treated five years ago with sustained viral response, hypertension, and latent tuberculosis (status post-treatment after 14 years) came to the emergency department (ED) with complaints of worsening right hip pain over the past eight weeks. Pain was 9/10 in intensity, dull to sharp in nature, localized on the anterior aspect of the right hip, radiating to the lower leg, and worsening with minimal leg flexion and internal rotation. Pain was associated with subjective chills and weight loss. Six weeks ago, the patient was admitted to another facility for similar complaints, was found to have methicillin resistant Staphylococcus aureus (MRSA) bacteremia with septic arthritis of the same hip, diagnosed after right hip joint aspiration and cultures. Patient had then received treatment with IV vancomycin for six weeks.
On arrival to the ED, the patient was hemodynamically stable. The patient was in mild distress due to the pain. There was tenderness to palpation on the right hip with no visible erythema, and significant limited range of motion for the right leg. Laboratory findings on admission are provided in Table 1. Other laboratory studies and serological markers for septic arthritis were unremarkable.
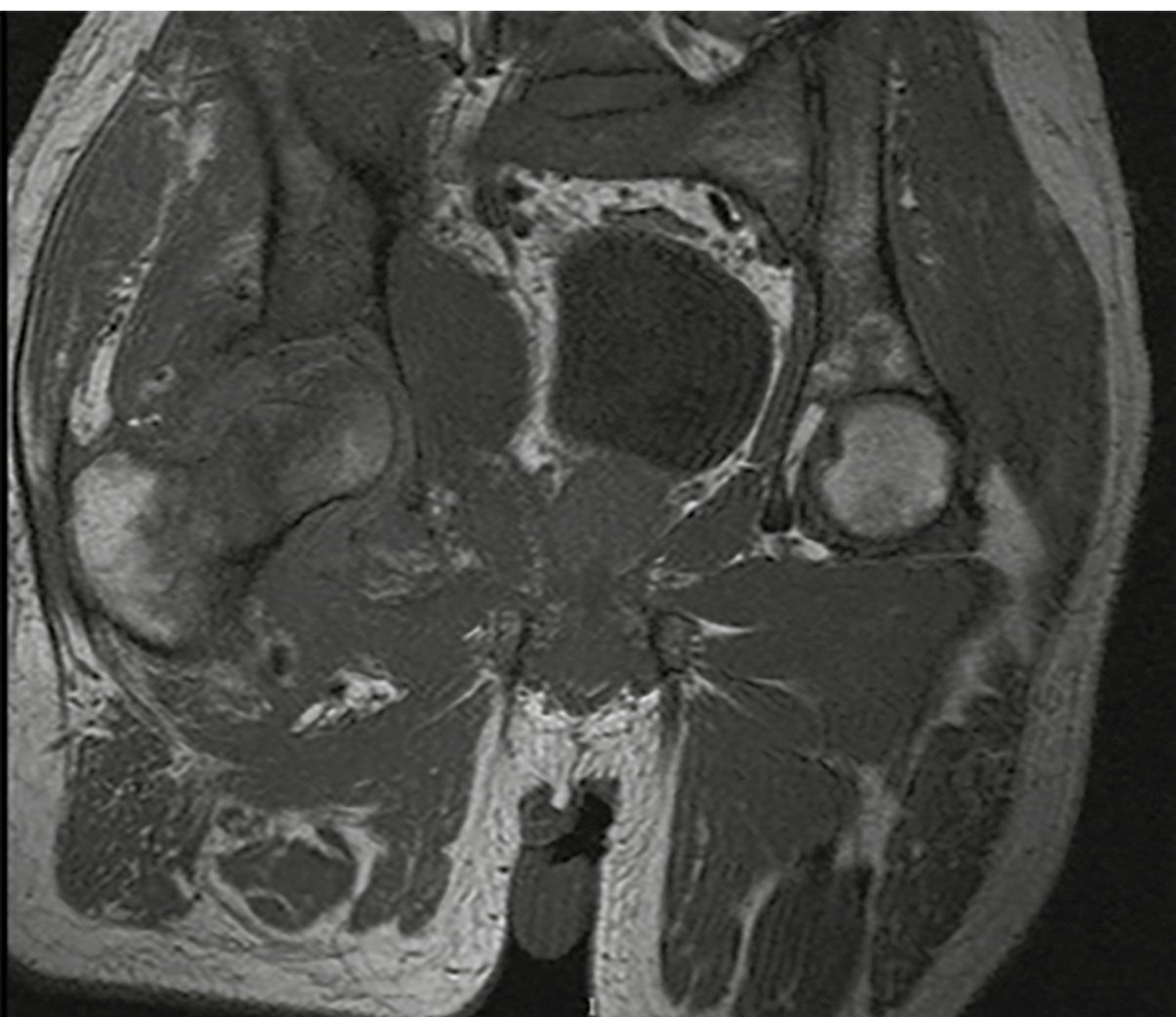
A computer tomography (CT) scan of the pelvis without contrast showed erosive changes within the acetabulum with poor cortical definition superiorly as well as erosive changes within the right femoral head and neck. There was fluid within the joint space, and thickening of the obturator internus muscle and soft tissues of the right hip. Magnetic resonance imaging with contrast showed findings suggestive of infectious arthritis (Figure 1). Initially, the patient received one dose of empiric IV vancomycin and piperacillin/tazobactam.
Prominent bony destruction involving the right femoral head and acetabulum with extensive synovitis. There is also severe periarticular soft tissue edema and ill-defined fluid.
The patient was evaluated by the orthopedics team and underwent joint aspiration by Interventional Radiology. During the procedure, the joint space and anterior soft tissues were irrigated with 5mL of normal saline, and the irrigated fluid was sent for culture and sensitivity. Empiric broad-spectrum antibiotics were restarted, and then later narrowed to IV nafcillin after Staphylococcus lugdunensis was identified in the aerobic cultures from the joint aspirate. Subsequently, blood cultures throughout the course remained negative. Bone biopsy showed a fragment of viable mature bone with fibrotic intertrabecular tissue with acute and chronic inflammation and a focal osteolytic interface. The patient was discharged to a short-term rehabilitation facility for six weeks of IV antibiotic therapy.
DISCUSSION
The identification of S. lugdunensis is challenging; however, it can be differentiated from other CoNS by biochemical markers, specifically using the L-pyrrolidonyl arylamidase enzyme test and ornithine decarboxylase positivity test11. Herchline TE, Ayers LW. Occurrence of Staphylococcus lugdunensis in consecutive clinical cultures and relationship of isolation to infection. J Clin Microbiol. 1999;29(3):419-21.,22. Kragsbjerg P, Bomfim-Loogna J, Tornqvist E, Soderquist B. Development of antimicrobial resistance in Staphylococcus lugdunensis during treatment-report of a case of bacterial arthritis, vertebral osteomyelitis and infective endocarditis. Clin Microbiol Infect. 2000;6(1):496-9.. Most contemporary automated identification systems are able to correctly identify S. lugdunensis from other Staphylococcus species. However, S. lugdunensis is also able to protect itself from the immune system via the production of biofilm22. Kragsbjerg P, Bomfim-Loogna J, Tornqvist E, Soderquist B. Development of antimicrobial resistance in Staphylococcus lugdunensis during treatment-report of a case of bacterial arthritis, vertebral osteomyelitis and infective endocarditis. Clin Microbiol Infect. 2000;6(1):496-9.. Even though organisms are susceptible to an array of antimicrobials, infections can be very difficult to treat if they form and proliferate within a biofilm33. Hellbacher C, Törnqvist E, Söderquist B. Staphylococcus lugdunensis: clinical spectrum, antibiotic susceptibility, and phenotypic and genotypic patterns of 39 isolates. Clin Microbiol Infect . 2006;12(1):43-9.
4. Murdoch DR, Everts R, Chambers ST, Cowan IA. Vertebral osteomyelitis due to Staphylococcus lugdunensis. J Clin Microbiol . 1996;34(1), 993-4.-55. Babu E, Oropello J. Staphylococcus lugdunensis: the coagulase-negative staphylococcus you don’t want to ignore. Expert Rev Anti Infect Ther. 2011;9(10):901-7..
Most isolates of S. lugdunensis are sensitive to an array of antimicrobial therapy. However, there have been isolated case reports of resistance to commonly used empiric antibiotic therapy33. Hellbacher C, Törnqvist E, Söderquist B. Staphylococcus lugdunensis: clinical spectrum, antibiotic susceptibility, and phenotypic and genotypic patterns of 39 isolates. Clin Microbiol Infect . 2006;12(1):43-9.. No cases of vancomycin resistance have been mentioned so far. It remains unclear whether our patient developed vancomycin resistance or later had a co-infection/relapse with S. lugdunensis. It is noteworthy that susceptibility testing of a joint aspiration in our laboratory showed vancomycin sensitivity with a minimum inhibitory concentration of 1µg/mL.
Staphylococcus lugdunensis is an unusual cause of bone and joint infection. However the total number of patients with infection due to this organism may remain under-diagnosed because some clinical laboratories do not separate all isolates of CoNS in laboratory cultures and therefore may not fully identify isolates of S. lugdunensis66. Grupper M, Potasman I, Rosner I, Slobodin G, Rozenbaum M. Septic arthritis due to Staphylococcus lugdunensis in a native joint. Rheumatol Int. 2010;30(9):1231-3.,77. Liu C, Shen D, Guo J, Wang K, Wang H, Yan Z, et al. Clinical and microbiological characterization of Staphylococcus lugdunensis isolates obtained from clinical specimens in a hospital in China. BMC Microbiol. 2012;12(1):168-75.. Moreover, even physicians who are considering CoNS as a possible pathogen may not ask for further identification of a particular isolate of CoNS, and may therefore be unaware that the patient has a virulent S. lugdunensis as the true pathogen in a clinical infection, thereby undertreating the patient88. Weightman NC, Allerton KE, France J. Bone and prosthetic joint infection with Staphylococcus lugdunensis. J Infect. 2000;40(3):98-9.
9. Arias M, Tena D, Apellániz M, Asensio MP, Caballero P, Hernández C, et al. Skin and soft tissue infections caused by Staphylococcus lugdunensis: report of 20 cases. Scand J Infect Dis. 2010;42(11-12):879-84.
10. Karnani R, Myers JP. Bone and joint infections caused by Staphylococcus lugdunensis: report of 2 cases and review of the literature. Infect Dis Clin Pract. 2008;16(2):94-9.
11. Gill VJ, Selepak ST, Williams EC. Species identification and antibiotic susceptibilities of coagulase-negative staphylococci isolated from clinical specimens. J Clin Microbiol . 1983;18(6):1314-9.-1212. Bocher S, Tonning B, Skov RL, Prag J. Staphylococcus lugdunensis, a common cause of skin and soft tissue infections in the community. J Clin Microbiol . 2009;47(4):946-50..
In conclusion, the importance of correctly identifying S. lugdunensis is underscored. Isolation of S. lugdunensis is significant, and the organism should not be discarded as a contaminant without careful consideration. If the clinical situation does not correlate with CoNS, prompt identification to the species level should be performed.
Acknowledgments
We thank the patient described for allowing us to share his details.
REFERENCES
-
1Herchline TE, Ayers LW. Occurrence of Staphylococcus lugdunensis in consecutive clinical cultures and relationship of isolation to infection. J Clin Microbiol. 1999;29(3):419-21.
-
2Kragsbjerg P, Bomfim-Loogna J, Tornqvist E, Soderquist B. Development of antimicrobial resistance in Staphylococcus lugdunensis during treatment-report of a case of bacterial arthritis, vertebral osteomyelitis and infective endocarditis. Clin Microbiol Infect. 2000;6(1):496-9.
-
3Hellbacher C, Törnqvist E, Söderquist B. Staphylococcus lugdunensis: clinical spectrum, antibiotic susceptibility, and phenotypic and genotypic patterns of 39 isolates. Clin Microbiol Infect . 2006;12(1):43-9.
-
4Murdoch DR, Everts R, Chambers ST, Cowan IA. Vertebral osteomyelitis due to Staphylococcus lugdunensis J Clin Microbiol . 1996;34(1), 993-4.
-
5Babu E, Oropello J. Staphylococcus lugdunensis: the coagulase-negative staphylococcus you don’t want to ignore. Expert Rev Anti Infect Ther. 2011;9(10):901-7.
-
6Grupper M, Potasman I, Rosner I, Slobodin G, Rozenbaum M. Septic arthritis due to Staphylococcus lugdunensis in a native joint. Rheumatol Int. 2010;30(9):1231-3.
-
7Liu C, Shen D, Guo J, Wang K, Wang H, Yan Z, et al. Clinical and microbiological characterization of Staphylococcus lugdunensis isolates obtained from clinical specimens in a hospital in China. BMC Microbiol. 2012;12(1):168-75.
-
8Weightman NC, Allerton KE, France J. Bone and prosthetic joint infection with Staphylococcus lugdunensis J Infect. 2000;40(3):98-9.
-
9Arias M, Tena D, Apellániz M, Asensio MP, Caballero P, Hernández C, et al. Skin and soft tissue infections caused by Staphylococcus lugdunensis: report of 20 cases. Scand J Infect Dis. 2010;42(11-12):879-84.
-
10Karnani R, Myers JP. Bone and joint infections caused by Staphylococcus lugdunensis: report of 2 cases and review of the literature. Infect Dis Clin Pract. 2008;16(2):94-9.
-
11Gill VJ, Selepak ST, Williams EC. Species identification and antibiotic susceptibilities of coagulase-negative staphylococci isolated from clinical specimens. J Clin Microbiol . 1983;18(6):1314-9.
-
12Bocher S, Tonning B, Skov RL, Prag J. Staphylococcus lugdunensis, a common cause of skin and soft tissue infections in the community. J Clin Microbiol . 2009;47(4):946-50.
Publication Dates
-
Publication in this collection
Jul-Aug 2018
History
-
Received
19 May 2017 -
Accepted
04 May 2018