Abstracts
Objective
Investigate binge eating (BE) prevalence in women according to the obesity degree and assess the associated factors.
Methods
Cross-sectional study with female adults presenting body mass index (BMI) ≥ 35 kg/m2. The analyzed variables were: sociodemographics, health status, obesity history, lifestyle, eating behavior and obesity degree. In order to analyse BE it was used the Binge Eating Scale (BES), which is considered positive when BES ≥ 18 points. Prevalence and prevalence ratios (PR) were calculated with confidence intervals (CI) of 95%. Multivariate analysis was carried out using Poisson regression.
Results
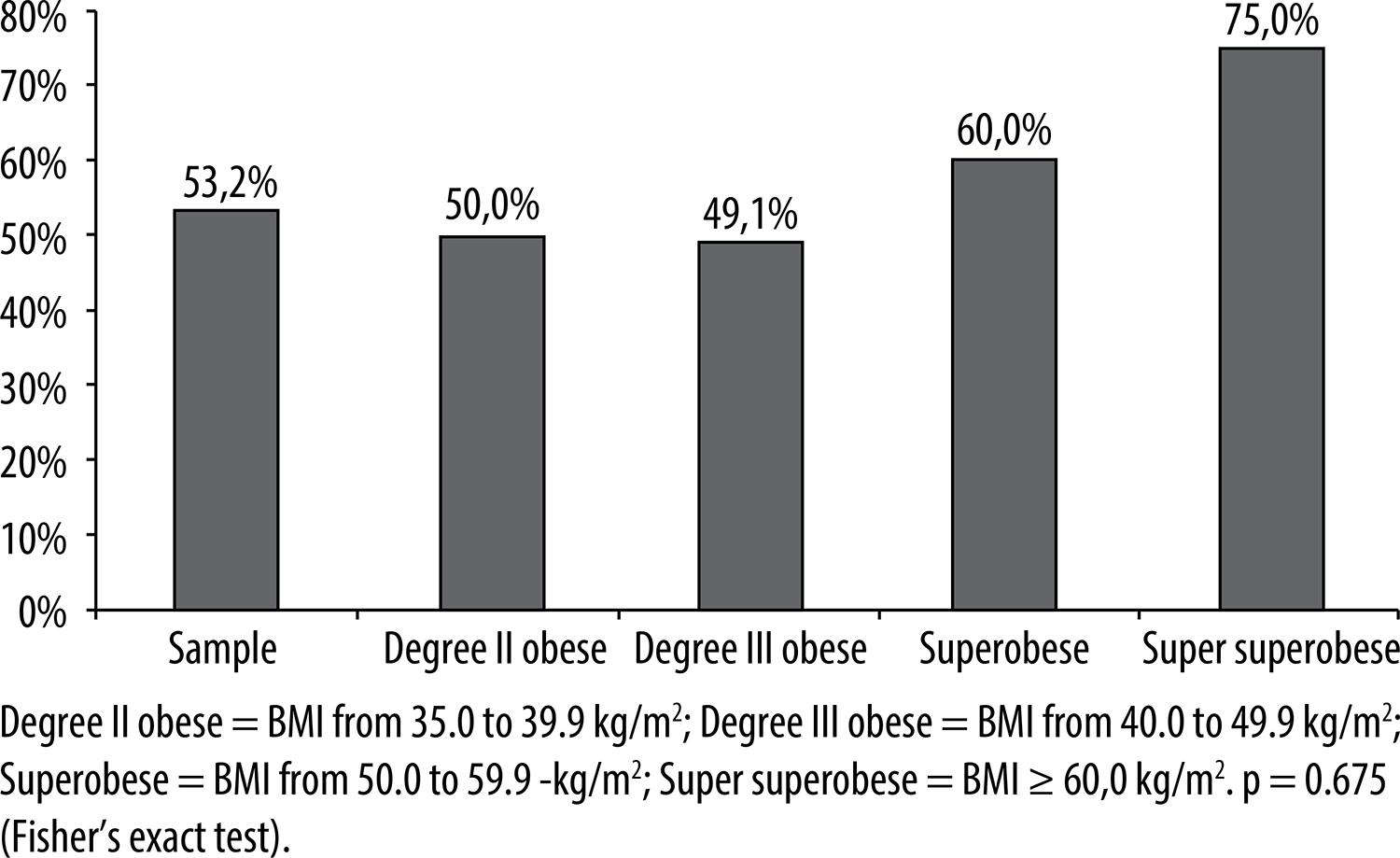
BE prevalence was 53.2%, and the prevalence in super superobese women (BMI ≥ 60 kg/m2) was 75%. After multivariate analysis, associations were observed between the age group 40-49 years old (PR = 2.0; 95% CI = 1.2-3.4) and the “snacking habit” (PR = 1.9; 95% CI = 1.2-2.9).
Conclusion
The prevalence of BE in severe obese women was high. Association with the “snacking habit” can be a BE marker that should be monitored in the severely obese individuals that fit this profile.
Obesity; women; eating behavior
Objetivo
Investigar a prevalência de compulsão alimentar periódica (CAP) em mulheres conforme grau de obesidade e avaliar os fatores associados.
Métodos
Estudo transversal realizado com adultas e índice de massa corporal (IMC) ≥ 35 kg/m2. Variáveis analisadas: sociodemográficas, condições de saúde, história de obesidade, estilo de vida, comportamento alimentar e grau de obesidade. Para análise da CAP, foi utilizada Escala de Compulsão Alimentar Periódica, sendo CAP aquelas com ≥ 18 pontos. Calcularam-se prevalência e razões de prevalências, com intervalos de confiança de 95%. Realizou análise multivariada pela regressão de Poisson.
Resultados
A prevalência de CAP foi de 53,2%, sendo a prevalência em super superobesas (IMC ≥ 60 kg/m2) de 75%. Após análise multivariada, foram associadas idade de 40 a 49 anos (RP = 2,0; IC 95% = 1,2-3,4) e “hábito de beliscar” (RP = 1,9; IC 95% = 1,2-2,9).
Conclusão
A prevalência de CAP em obesas graves foi elevada. A associação com “hábito de beliscar” pode ser um marcador de CAP, devendo ser monitorado em obesas graves com esse perfil.
Obesidade; mulheres; comportamento alimentar
INTRODUCTION
Obesity is considered a serious public health problem that affects approximately 500 million adults worldwide11 Kral JG, Kava RA, Caalano PM, Moore BJ. Severe obesity: the neglected epidemic. Obes Facts. 2012;5(1):254-69.. This illness afflicts different age groups, all social levels, both genders and its prevalence has been increasing significantly in recent decades22 WHO – World Health Organization. Obesity and overweight. Media centre, Fact sheet; 2012; 311. [citado em 25 Nov. 2012]. Disponível em: <http://www.who.int/mediacentre/factsheets/fs311/en/index.html>.
http://www.who.int/mediacentre/factsheet...
. In Brazil, 49% of the adult population are overweight and 14.8% are obese, according to the Family Budget Survey (FBS) 2008-200933 IBGE – Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares 2008/2009. Brasília, DF; 2009. [citado em 5 Abr. 2011]. Disponível em: <http://www.ibge.gov.br/home/presidencia/noticias/noticia_visualiza.php?id_noticia=1699&id_pagina=1>.
http://www.ibge.gov.br/home/presidencia/...
. Besides, severe obesity incidence has increased and it represents between 0.5 and 1% of the adult Brazilian population44 Santos LM, Oliveira LV, Perters LR, Conde WL. Trends in morbid obesity and in bariatric surgeries covered by the Brazilian public health system. Obes Surg. 2010;20(7):943-8..
Due the fact that obesity is a chronic disease with multifactorial etiology22 WHO – World Health Organization. Obesity and overweight. Media centre, Fact sheet; 2012; 311. [citado em 25 Nov. 2012]. Disponível em: <http://www.who.int/mediacentre/factsheets/fs311/en/index.html>.
http://www.who.int/mediacentre/factsheet...
; obese individuals present emotional alterations that can be classified either as determining factors or as a consequence of obesity55 Oliveira VM, Linardi RC, Azevedo AP. Cirurgia bariátrica – aspectos psicológicos e psiquiátricos. Rev Psiq Clín. 2004;31(4):199-201.. Obese individuals can show psychological suffering related to social discrimination, self-image depreciation, insecurity, and a general feeling of failure related to weight loss. Women are more exposed to media and western society demands for a beauty ideal, related to slenderness, which can generate emotional stress66 Bernardi F, Cichelero C, Vitolo MR. Comportamento de restrição alimentar e obesidade. Rev Nutr. 2005;18(1):85-93.
,
77 Pivetta LA, Gonçalves-Silva RMV. Compulsão alimentar e fatores associados em adolescentes de Cuiabá, Mato Grosso, Brasil. Cad. Saude Publica. 2010;26(2):337-46..
Bariatric surgery is a treatment option, widely used in severe obesity cases88 Sjöström L, Narbro K, Sjöström D, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Eng J Med. 2007;357(8):741-52. , 99 Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. Diretrizes brasileiras de obesidade 2009/2010. 3ª ed. Itapevi, SP: AC Farmacêutica; 2009.. Psychological disorders presence is commonly an exclusion criteria for bariatric surgery candidates; however, due to lack of consensus in the scientific literature, these are not considered as a formal counter indication for this procedure1010 Segal A, Fandiño, J. Indicações e contraindicações para realização das operações bariátricas. Rev Bras Psiquiatr. 2002;24(Supl III):68-72.. Nevertheless, psychological and psychiatric monitoring are recommended in the pre- and post-surgery periods, as bariatric surgery candidates usually demonstrate association with psychiatric disorders and the proper treatment will promote better prognostic after the surgery99 Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. Diretrizes brasileiras de obesidade 2009/2010. 3ª ed. Itapevi, SP: AC Farmacêutica; 2009. , 1010 Segal A, Fandiño, J. Indicações e contraindicações para realização das operações bariátricas. Rev Bras Psiquiatr. 2002;24(Supl III):68-72..
Due to the close relationship between binge eating (BE) and severe obesity, it is important to know the magnitude of this problem and its associated factors in obese patients that seek treatment, mainly because BE is a risk factor for comorbidities, such as: psychiatric disorders, and also hinders adherence to dietotherapic treatments1111 American Dietetic Association. Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders. J Am Diet Assoc. 2011;111(8):1236-41. , 1212 Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98-102.. This study aimed to investigate BE prevalence in women according to the obesity degree as well as to evaluate the associated factors.
METHODS
It was used a cross-sectional study carried out at the Severe Obesity Nutrition Ambulatory, at the Federal University of Goiás School Hospital (in Portuguese: Ambulatório de Nutrição em Obesidade Grave – ANOG). The invitation to participate of the research occurred sequentially to all patients that had appointments at ANOG; however inclusion in the research was not sequential. Some patients did not fulfill the eligibility criteria and some did not sign the informed consent form (ICF).
The inclusion criteria considered adult women (20-59 years old), who presented obesity degree II or superior, i.e., body mass index (BMI) ≥ 35 kg/m2, and sought nutritional treatment at ANOG and/or were bariatric surgery candidates. It was included in the research the women who fit the criteria above and accepted to be part of the study as well as signed the ICF. The exclusion criteria were: pregnant women; women who were breastfeeding; women with special needs; and post-bariatric surgery patients.
Data were collected between February, 2008 and June, 2012, during the first consultation. It was done through standardized pre-tested anamnesis application and anthropometric data collection by nutritionists or licensed nutrition academics. During consultation, the Binge Eating Scale (BES)1313 Freitas S, Lopes CS, Coutinho W, Appolinário JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215-20. was applied. At this moment patients chose the affirmatives that best described their feelings regarding eating behavior. In order to avoid comprehension difficulties, as most patients verified low schooling level, it was done a simple instrument reading for all patients, following the literature recommendation1313 Freitas S, Lopes CS, Coutinho W, Appolinário JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215-20..
BES is a translated and validated Likert scale for the Brazilian population, considered an investigative instrument that allows the evaluation of symptoms severity during binge eating episodes as well as tracking binge eating disorders (BED) occurrence in obese individuals during weight loss treatments1313 Freitas S, Lopes CS, Coutinho W, Appolinário JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215-20. , 1414 Palavras MA, Kaio GH, Mari JJ, Claudino AM. Uma revisão dos estudos latino-americanos sobre o transtorno da compulsão alimentar periódica. Rev Bras Psiquiatr. 2011;33(Supl 1):S81-94.. BES classifies BE severity degrees, categorized by the following scores: ≤ 17 points no BE, 18 to 26 points moderate BE, and score ≥ 27 severe BE1313 Freitas S, Lopes CS, Coutinho W, Appolinário JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215-20.. BE was the outcome variable in this study, defined as a BES score ≥ 18 points.
A multidisciplinary team accompanied the patients in this research, but it did not include a psychiatrist. Therefore, a BE-tracking instrument was selected in order to achieve the research goals and the individuals monitored with BE were forwarded to psychiatric follow-ups. The term BE is used to describe the feeding behaviour characterized by moments of extreme food ingestion in short periods of time, followed by a loss of control feeling by the individual, not followed by compensatory methods1414 Palavras MA, Kaio GH, Mari JJ, Claudino AM. Uma revisão dos estudos latino-americanos sobre o transtorno da compulsão alimentar periódica. Rev Bras Psiquiatr. 2011;33(Supl 1):S81-94. , 1515 Appolinario JC. Transtorno da compulsão alimentar periódica: uma entidade clínica emergente que responde ao tratamento farmacológico. Rev Bras Psiquiatr. 2004;26(2):75-6..
The studied variables included: sociodemographical data (age, marital status, schooling, and family income); health conditions (actual comorbidities and weight loss medication use); obesity clinical history (obesity onset, obesity in the family, and previous weight loss treatments); lifestyle (physical activities practice, use of tobacco or alcohol); eating behavior (number of meals per day, “snacking habit”, Binge Eating – BE), and anthropometric data (weight, height, and BMI).
Patients were questioned about: age in full years, which was then categorized in 20-29 years old, 30-39 years old, 40-49 years old, 50-59 years old; marital status (with partner/without partner), schooling years, which was then categorized in less than 9 years and ≥ 9 years; and family income calculated by minimum wage (MW)* * In 2012 the minimum wage in Brazil was R$ 622.00. . It was categorized as < 1 MW/ 1 to 2 MW/ > 2 MW. Current comorbidities presence (yes/no) and weight loss medication use were confirmed by medical prescriptions for continuous or mandatory medication and/or medical records. Regarding weight loss medication, anorexigen and psychiatric medications were considered, and to this second variable were included anxyolitics and antidepressives (yes/no).
Other variables studied included: obesity onset (childhood/adolescence/post-gestation/adulthood); obesity in family (yes/no); previous weight loss treatment (self-initiated or with a health professional help); physical activity practice (regular, irregular or none). In this category were considered as regular at least 150 minutes per week of moderate-intense aerobic activity1616 World Health Organization. Global recommendations on physical activity for health. Geneva: WHO; 2010.; use of tobacco (yes/no) for which ex-smokers were counted as smokers; alcoholic beverages consumption (yes/no); number of meals per day (< 4/≥ 4 meals/day) and if “snacking” was a habit. For the “snacking habit”, the question asked was: “Do you have the habit of eating any food or drinking beverages, with the exception of water, in an unplanned manner and outside established periods for main meals and snacks? If yes, do you consider this a regular habit, as part of your routine at least once a day?” (yes/no)1717 Drummond S, Crombie N, Kirk T. A critique of the effects of snacking on body weight status. Eur J Clin Nutr. 1996;50(12):779-83..
The anthropometric variables evaluated were weight and height and later it was calculated the BMI. Platform-type mechanical scales, with a maximum capacity of 300 kg and 100 g precision, were used to determine weight. Height measurement was carried by using a stadiometer, coupled to the scales, with a 0.1 cm precision.
Before weight measurements, the scales were calibrated, and then the surveyee was positioned in the center of the scale, in a firm position, barefoot and with the minimum amount of clothes possible, with arms parallel to the body. Weight measurements were verified in the front of the scale1717 Drummond S, Crombie N, Kirk T. A critique of the effects of snacking on body weight status. Eur J Clin Nutr. 1996;50(12):779-83.. It is important to highlight that the examiners participated of preliminary training. They were qualified to correctly carry out the anthropometric evaluation procedure in order to guarantee higher data reliability.
To classify obesity it was used the criteria from the World Health Organization (WHO) as well as from the Brazilian Association of Obesity Study and Metabolic Syndrome (in Portuguese: Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica – Abeso). It was considered a BMI between 35 and 39.9 kg/m2 obesity degree II and ≥ 40.0 kg/m2 as degree III99 Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. Diretrizes brasileiras de obesidade 2009/2010. 3ª ed. Itapevi, SP: AC Farmacêutica; 2009. , 1818 Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics; 1988.. It was also considered the criteria defined by the American Society for Metabolic and Bariatric Surgery (ASMBS), which considers superobesity if the BMI is between 50 and 59.9 kg/m2 and super superobesity if the BMI is ≥ 60 kg/m2 1919 World Health Organization. Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: World Health Organization; 2000. p. 256. WHO Obesity Technical Report Series, n. 284..
Database structure was built using the Epi-info software, version 3.5.3. Data were typed in double entries and only after data validation entry the statistical analysis was carried out using the Stata software, version 8.0.
Because this research is part of a wider study2121 Rodrigues APS, Silveira EA. Correlação e associação de renda e escolaridade com condições de saúde e nutrição em obesos graves. Ciênc Saúde Coletiva. 2015;20(1):165-74., the number of patients for the study was calculated a posteriori through the Epi-Info 6.0 software. It was selected the cross-sectional studies option and the Statcalc tool. The parameters utilized were: 80% power, confidence level 95%. Exposition variables considered were “snacking habit” with a 40% prevalence in non-exposed and 1:1 ratio (one exposed to one non-exposed) and weight loss medication use with a 50% prevalence among non-exposed and 1:5 ratio (1 exposed to 5 non-exposed). As a result, it would be necessary 90 patients to analyze the association between medicine and 92 patients to analyse “snacking habit”. Thereby the sample size considered was enough to carry out the research.
Statistical analysis included BE prevalence and prevalence ratios measurement (PR), with corresponding 95% confidence intervals (CI 95%). Pearsons’s Chi-Square Test or Fisher’s Exact Test were used to verify the association between BE and the studied variables. Variables that presented p < 0.20 in bivariate analysis were selected for multivariate analysis through a Poisson regression, with 5% significance level.
RESULTS
Ninety-seven female patients were invited to participate of the study. Three of them refused to participate, so the final sample had 94 patients. Patients presented an average age 37.7 ± 10.4 years, average weight 119.2 ± 17.3 kg, average height 1.59 ± 0.1 m, and average BMI 47.4 ± 6.6 kg/m2. This way, 10.6% (n = 10) were classified as obese individuals degree II, 58.5% (n = 55) classified as obese individuals degree III, 26.6% (n = 25) as superobese, and 4.3% (n = 4) as super superobese.
Binge eating prevalence was 53.2% (n = 50). From those 28.7% (n = 27) were classified as moderate BE and 24.5% (n = 23) as severe BE. When analyzing BE prevalence according to obesity degrees, it was observed a higher BE occurrence in super superobese (75.0%). Although it was not found significant association between BE and obesity degrees (p = 0.675) (Figure 1).
Binge Eating (BE) prevalence in severe obese women according to obesity degree, at the Severe Obesity Nutrition Ambulatory, Federal University of Goiás School Hospital (ANOG/HC/UFG), 2008-2012 (n = 94).
The majority of patients (69.9%) were either married or in a consensual relationship, 51.6% had at least 9 years of schooling, and 43.9% achieved a family income between 1 and 2 minimum wages (Table 1).
Binge Eating (BE) prevalence and brute prevalence ratio according to the following variables: sociodemographical data, obesity clinical history and eating behavior in women at the Severe Obesity Nutrition Ambulatory, Federal University of Goiás School Hospital (ANOG/HC/UFG), 2008-2012 (n = 94)
The highest BE prevalence was verified in women between 40 and 49 years old (76.2%), with less than 9 years of schooling (60.0%), family income between one and two minimum wages per month (60.0%), obesity onset in their adolescence (60.0%), that had undergone through previous weight loss self-treatment (62.5%), who eat four or more meals per day (62.0%), and that present “snacking habit” (64.4%). This last variable was the only one that showed significant association (p = 0.020) (Table 2).
The current comorbidity that presented highest BE prevalence was dyslipidemia (69.2%). Regarding weight loss medication use, BE frequency in those making use of psychiatric medication was higher in relation to the use of anorexigens. Only one patient reported the use of anxiolytics, but did not present BE. BE was more frequent in sedentary women or in those practicing irregular physical activity (55.8%), in non-smokers (54.4%), and those who did not consume alcohol (55.0%), but no significant association was observed (Table 2).
Current comorbidity that showed more BE prevalence was dyslipidemia (69.2%). About weight loss medication, BE frequency in those women who used psychiatric medication was bigger when compared to women who used anorexigen medication. Only one patient mentioned using anxiolytics, but did not present BE. BE was more frequent in women that practiced physical activity in an irregular way or were sedentary (55.8%), in those who were non-smokers (54.5%) and those who did not use alcoholic beverages (55.0%). However, it was not noticed significant association (Table 2).
The variables included in multivariate analysis were: age (p = 0.082), number of meals per day (p = 0.018), “snacking habit” (p = 0.020), and dyslipidemia (p = 0.185). Association with BE was maintained only in the age group of 40-49 years old, with BE prevalence twice as higher in relation to the age group of 30-39 years old, as well as with the “snacking habit” with a BE prevalence 1.9 times higher regarding those that did not present this behavior (Table 3).
DISCUSSION
This study detected a high BE prevalence (53.2%) in women suffering from severe obesity, who sought nutritional treatment at ANOG and part of them were bariatric surgery candidates. High BE prevalence in severe obese individuals was also observed in a study encompassing patients of both genders, in pre-operatory bariatric surgery conditions, with 44% prevalence2222 Jones-Corneille LR, Wadden TA, Sarwer DB, Faulconbridge LF, Fabricatore AN, Stack RM, et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical Interviews. Obes Surg. 2012;22(3):389-97. and in a research including women in pre-operatory bariatric surgery treatment, with 77.3% prevalence2323 Müller A, Claes L, Mitchell JE, Fischer J, Horbach T, Zwaan M. Binge eating and temperament in morbidly obese prebariatric surgery patients. Eur Eat Disord Rev. 2012;20(1):e91-5..
A research that used the same instrument to track BE in obese patients waiting for bariatric surgery observed a 56.7% BE prevalence. From those, 25.4% were considered moderate BE and 31.3% were considered severe BE2424 Petribu K, Ribeiro ES, Oliveira FMF, Braz CIA, Gomes MLM, Araújo DE, et al. Transtorno da compulsão alimentar periódica em uma população de obesos mórbidos candidatos a cirurgia bariátrica do hospital universitário Oswaldo Cruz, em Recife – PE. Arq Bras. Endocrinol Metab. 2006;50(5):901-8.. Such a high occurrence of BE was found as well in obese individuals who did not seek weight loss treatment66 Bernardi F, Cichelero C, Vitolo MR. Comportamento de restrição alimentar e obesidade. Rev Nutr. 2005;18(1):85-93. and among college female students, who did not seek weight loss programs, with 54.5% BE prevalence in those overweight and obese2525 Vitolo MR, Bortolini GA, Horta RL. Prevalência de compulsão alimentar entre universitárias de diferentes áreas de estudo. Rev Psiquiatr Rio Gd Sul. 2006;28(1):20-6..
Although the initial hypothesis that BE prevalence would increase along with the obesity degree, the increase observed was not statistically significant, even though it reached 75% among the super superobeses. Several studies have found elevated BE prevalence in obese individuals, although the association with obesity degrees was not assessed66 Bernardi F, Cichelero C, Vitolo MR. Comportamento de restrição alimentar e obesidade. Rev Nutr. 2005;18(1):85-93. , 2525 Vitolo MR, Bortolini GA, Horta RL. Prevalência de compulsão alimentar entre universitárias de diferentes áreas de estudo. Rev Psiquiatr Rio Gd Sul. 2006;28(1):20-6. , 2626 França GV, Gigante DP, Olinto MT. Binge eating in adults: prevalence and association with obesity, poor self-rated health status and body dissatisfaction. Public Health Nutr. 2014;17(4):932-8. in the same manner as this study. Only one prospective study in Brazil, evaluated 28 adults who suffered from overweight or obesity, found a higher BE occurrence associated with a higher degree of obesity2727 Mosca LN, Costa LRLG, Ramos CFC, Asano LMT, Ferreira AD. Compulsão alimentar periódica de pacientes em tratamento para redução de peso. J Health Sci Inst. 2010;28(1):59-63.. In the current study, there was no association between BE and obesity degrees, which could be due to the patients profile. All patients were severely obese with an average BMI of 47.4 ± 6.6 kg/m2, 58.5% presented obesity degree III and 26.6% presented superobesity. Also, the women showed very specific characteristics, such as low education levels (48.4% attended school for less than 9 years), and low family income (43.9% reported income between 1 and 2 minimum wages).
In a population-based transversal-type study carried out with 2097 adults, a BE prevalence of 7.9% was verified, being more prevalent in women (9.6%) and among younger individuals, between 20 and 29 years old (11.0%), with a decreasing trend as age advances2626 França GV, Gigante DP, Olinto MT. Binge eating in adults: prevalence and association with obesity, poor self-rated health status and body dissatisfaction. Public Health Nutr. 2014;17(4):932-8.. Another study evaluated 2855 adults and elderlies who often visited shopping malls in five Brazilian cities observed a higher BE prevalence in the female gender (13.0%), and in younger women, between 18 and 40 years old (17.5%)2828 Siqueira KS, Appolinário JC, Sichieri R. Relationship between binge-eating episodes and self-perception of body weight in a nonclinical sample of five Brazilian cities. Rev Bras Psiquiatr. 2005;27(4):290-4.. Regarding age, the findings mentioned above do not match with this study findings, as the age group presenting higher BE prevalence was 40 to 49 years of age (76.2%), with a BE risk twice as higher regarding women in the age group 30-39 years old. The age group 20-29 years old was not associated with BE. These findings might have occurred due to different characteristics of the study sample, revealing that in women suffering from severe obesity the association with age does not follow the same trend of general female population. The association verified between BE and the age group 40-49 years old raises the hypothesis of a relationship with menopause, as the age group is concomitant to this process. Women in menopause show a higher prevalence of anxiety2929 Polisseni AF, Araújo DAC, Polisseni F, Mourão Junior CA, Polisseni J, Fernandes ES, et al. Depressão e ansiedade em mulheres climatéricas: fatores associados. Rev Bras Ginecol Obstet. 2009;31(1):28-34., which could cause the beginning of eating disorders.
The “snacking habit” is a frequent eating pattern in obese patients submitted to surgical techniques with gastric restrictions1212 Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98-102.. Especially after the first six months post-operatory, this behaviour is observed as it is impossible for patients to eat excessive amounts of food, and then they usually develop a “snacking behavior”1212 Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98-102.. This habit is a factor that prevents adherence to dietotherapic treatment and presents as consequences unsatisfactory weight loss and difficulty in maintaining weight loss1212 Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98-102.. Research carried out with post-operatory bariatric surgery patients have found the prevalence of “snacking habit” between 37.0%3030 Marchesini SD. Acompanhamento psicológico tardio em pacientes submetidos à cirurgia bariátrica. ABCD Arq Bras Cir Dig. 2010;23(2):108-13. and 44.0%3131 Elkins G, Whitfield P, Marcus J, Symmonds R, Rodriguez J, Cook T. Noncompliance with behavioral recommendations following bariatric surgery. Obes Surg. 2005;15(4):546-51.. However, the few existing research that assessed this behaviour in severely obese individuals within the pre-operatory period found prevalence between 26.4%3232 Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity. 2008;16(3):615-22. and 19.5%3333 Burgmer R, Grigutsch K, Zipfel S, Wolf AM, Zwaan M, Husemann B, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg. 2005;15(5):684-91..
Results presented by this research are worrying, as 50% of severe obese patients presented “snacking habit” before undergoing bariatric surgery, which is a percentage higher than observed in other studies. This “snacking habit” could compromise weight loss both while preparing for the surgery as well as after the surgery. This study is, to the best of the authors’ knowledge and after systematic reviews, the only study that analyzes the association between BE and “snacking habit” in Brazilian women with severe obesity, candidates to bariatric surgery. The “snacking habit” affected 64.4% of those women with BE, and was significantly associated even after multivariate analysis. Thereby these findings are relevant and contribute to scientific knowledge in the field.
The primary hypothesis is that eating impulsivity can occur because of very restrictive diets and/or frustrations caused by unsuccessful and slow treatments. Satisfactory weight loss and its maintenance require a longer time than what is expected by the patient, which are factors that could also contribute for the occurrence of BE and “snacking habit”. This highlights the relevance of a multidisciplinary team in severe obesity treatment, with the participation of psychologists, psychiatrists and nutritionists, reinforcing the several questions involved in “snacking habit” and binge eating.
The fact that BES is a tracking instrument and not a diagnosis instrument could be cited as this research limitation; however this point was discussed in the methodology section. BES is an easy analysis and low cost questionnaire; it is also useful to analyze BE occurrence but not to diagnose BED. However, BES, as BE a tracking instrument in severely obese individuals is useful to clinical support as well as to nutritional treatment. It can also increase obese patients comprehension of their own situation and, therefore, optimize intervention strategies.
A high prevalence of binge eating was observed in severely obese women, with a statistically significant association with the age group 40-49 years old as well as with “snacking habit”. The association between BE and “snacking habit” is an important finding and can contribute to evaluation development, monitoring and treatment strategies for severely obese individuals. Research on BE and “snacking habit” must be part of severely obese individuals anamnesis, candidates or not for bariatric surgery, during pre- and post-operatory periods. The goal is to increase effectiveness in the pondered loss treatment, in the adoption of more healthy eating habits, and also when forwarding a patient to psychiatrist binge eating disorder diagnosis and treatment.
REFERENCES
-
1Kral JG, Kava RA, Caalano PM, Moore BJ. Severe obesity: the neglected epidemic. Obes Facts. 2012;5(1):254-69.
-
2WHO – World Health Organization. Obesity and overweight. Media centre, Fact sheet; 2012; 311. [citado em 25 Nov. 2012]. Disponível em: <http://www.who.int/mediacentre/factsheets/fs311/en/index.html>.
» http://www.who.int/mediacentre/factsheets/fs311/en/index.html> -
3IBGE – Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares 2008/2009. Brasília, DF; 2009. [citado em 5 Abr. 2011]. Disponível em: <http://www.ibge.gov.br/home/presidencia/noticias/noticia_visualiza.php?id_noticia=1699&id_pagina=1>.
» http://www.ibge.gov.br/home/presidencia/noticias/noticia_visualiza.php?id_noticia=1699&id_pagina=1> -
4Santos LM, Oliveira LV, Perters LR, Conde WL. Trends in morbid obesity and in bariatric surgeries covered by the Brazilian public health system. Obes Surg. 2010;20(7):943-8.
-
5Oliveira VM, Linardi RC, Azevedo AP. Cirurgia bariátrica – aspectos psicológicos e psiquiátricos. Rev Psiq Clín. 2004;31(4):199-201.
-
6Bernardi F, Cichelero C, Vitolo MR. Comportamento de restrição alimentar e obesidade. Rev Nutr. 2005;18(1):85-93.
-
7Pivetta LA, Gonçalves-Silva RMV. Compulsão alimentar e fatores associados em adolescentes de Cuiabá, Mato Grosso, Brasil. Cad. Saude Publica. 2010;26(2):337-46.
-
8Sjöström L, Narbro K, Sjöström D, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Eng J Med. 2007;357(8):741-52.
-
9Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabólica. Diretrizes brasileiras de obesidade 2009/2010. 3ª ed. Itapevi, SP: AC Farmacêutica; 2009.
-
10Segal A, Fandiño, J. Indicações e contraindicações para realização das operações bariátricas. Rev Bras Psiquiatr. 2002;24(Supl III):68-72.
-
11American Dietetic Association. Position of the American Dietetic Association: nutrition intervention in the treatment of anorexia nervosa, bulimia nervosa, and other eating disorders. J Am Diet Assoc. 2011;111(8):1236-41.
-
12Saunders R. “Grazing”: a high-risk behavior. Obes Surg. 2004;14(1):98-102.
-
13Freitas S, Lopes CS, Coutinho W, Appolinário JC. Tradução e adaptação para o português da Escala de Compulsão Alimentar Periódica. Rev Bras Psiquiatr. 2001;23(4):215-20.
-
14Palavras MA, Kaio GH, Mari JJ, Claudino AM. Uma revisão dos estudos latino-americanos sobre o transtorno da compulsão alimentar periódica. Rev Bras Psiquiatr. 2011;33(Supl 1):S81-94.
-
15Appolinario JC. Transtorno da compulsão alimentar periódica: uma entidade clínica emergente que responde ao tratamento farmacológico. Rev Bras Psiquiatr. 2004;26(2):75-6.
-
16World Health Organization. Global recommendations on physical activity for health. Geneva: WHO; 2010.
-
17Drummond S, Crombie N, Kirk T. A critique of the effects of snacking on body weight status. Eur J Clin Nutr. 1996;50(12):779-83.
-
18Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics; 1988.
-
19World Health Organization. Obesity: preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva: World Health Organization; 2000. p. 256. WHO Obesity Technical Report Series, n. 284.
-
20American Association of Clinical Endocrinologists/The Obesity Society/American Society for Metabolic & Bariatric Surgery. Medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr Pract. 2008;14(Suppl 1).
-
21Rodrigues APS, Silveira EA. Correlação e associação de renda e escolaridade com condições de saúde e nutrição em obesos graves. Ciênc Saúde Coletiva. 2015;20(1):165-74.
-
22Jones-Corneille LR, Wadden TA, Sarwer DB, Faulconbridge LF, Fabricatore AN, Stack RM, et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical Interviews. Obes Surg. 2012;22(3):389-97.
-
23Müller A, Claes L, Mitchell JE, Fischer J, Horbach T, Zwaan M. Binge eating and temperament in morbidly obese prebariatric surgery patients. Eur Eat Disord Rev. 2012;20(1):e91-5.
-
24Petribu K, Ribeiro ES, Oliveira FMF, Braz CIA, Gomes MLM, Araújo DE, et al. Transtorno da compulsão alimentar periódica em uma população de obesos mórbidos candidatos a cirurgia bariátrica do hospital universitário Oswaldo Cruz, em Recife – PE. Arq Bras. Endocrinol Metab. 2006;50(5):901-8.
-
25Vitolo MR, Bortolini GA, Horta RL. Prevalência de compulsão alimentar entre universitárias de diferentes áreas de estudo. Rev Psiquiatr Rio Gd Sul. 2006;28(1):20-6.
-
26França GV, Gigante DP, Olinto MT. Binge eating in adults: prevalence and association with obesity, poor self-rated health status and body dissatisfaction. Public Health Nutr. 2014;17(4):932-8.
-
27Mosca LN, Costa LRLG, Ramos CFC, Asano LMT, Ferreira AD. Compulsão alimentar periódica de pacientes em tratamento para redução de peso. J Health Sci Inst. 2010;28(1):59-63.
-
28Siqueira KS, Appolinário JC, Sichieri R. Relationship between binge-eating episodes and self-perception of body weight in a nonclinical sample of five Brazilian cities. Rev Bras Psiquiatr. 2005;27(4):290-4.
-
29Polisseni AF, Araújo DAC, Polisseni F, Mourão Junior CA, Polisseni J, Fernandes ES, et al. Depressão e ansiedade em mulheres climatéricas: fatores associados. Rev Bras Ginecol Obstet. 2009;31(1):28-34.
-
30Marchesini SD. Acompanhamento psicológico tardio em pacientes submetidos à cirurgia bariátrica. ABCD Arq Bras Cir Dig. 2010;23(2):108-13.
-
31Elkins G, Whitfield P, Marcus J, Symmonds R, Rodriguez J, Cook T. Noncompliance with behavioral recommendations following bariatric surgery. Obes Surg. 2005;15(4):546-51.
-
32Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity. 2008;16(3):615-22.
-
33Burgmer R, Grigutsch K, Zipfel S, Wolf AM, Zwaan M, Husemann B, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg. 2005;15(5):684-91.
-
This study was approved by the Federal University of Goiás School Hospital Ethics Committee (in Portuguese: Comitê de Ética do Hospital das Clínicas da Universidade Federal de Goiás – CEP/HC/UFG).
-
*
In 2012 the minimum wage in Brazil was R$ 622.00.
Publication Dates
-
Publication in this collection
Apr-Jun 2015
History
-
Received
27 Oct 2014 -
Accepted
13 Apr 2015