Abstracts
BACKGROUND: Diet directly influences systemic arterial hypertension (SAH), which is one of the main risk factors for cardiovascular disease. OBJECTIVE: To associate hypertension with dietary factors in adults clinically selected for a change-of-lifestyle program. METHODS: Cross-sectional study comprising 335 individuals, aged between 44 and 65 years, clinically selected for a change-of-lifestyle program. We evaluated anthropometric data (BMI, %body fat and waist circumference), biochemical components (plasma glucose, triglycerides, total cholesterol, HDL-C and LDL-c) and diet, through the 24-hour recall method. The quality of the diet was assessed by the Healthy Eating Index. Blood pressure was measured according to the V Brazilian Guidelines on Hypertension and classified according to NCEP-ATPIII. Logistic regression was performed to determine the likelihood of changes in SBP and DBP according to dietary intake. The level of significance was set at p <0.05. RESULTS: There was a positive correlation between diastolic blood pressure and sugar and cholesterol intake, and a negative one with intake of fiber, portions of oil and fats and diet quality. Dietary variety with ≥ 8 food items showed a protective effect for alterations in systolic blood pressure, OR = 0.361 (0.148 to 0.878). CONCLUSION: A greater dietary variety had a protective effect on the systolic blood pressure.
Hypertension; blood pressure; diet, sodium-restricted; food quality
FUNDAMENTO: A dieta influencia diretamente a hipertensão arterial (HAS), que é um dos principais fatores de risco da doença cardiovascular. OBJETIVO: Associar a HAS com fatores dietéticos de adultos clinicamente selecionados para programa de mudança de estilo de vida. MÉTODOS: Estudo transversal composto por 335 indivíduos, com idade entre 44 e 65 anos, clinicamente selecionados para um programa de mudança de estilo de vida. Foram avaliados os dados antropométricos (IMC, % de gordura e circunferência abdominal), os componentes bioquímicos (concentrações plasmáticas de glicose, triglicerídeos, colesterol total, HDL-c e LDL-c) e a dieta, por meio do recordatório de 24 horas. A qualidade da dieta foi avaliada pelo Índice de Alimentação Saudável. A pressão arterial foi mensurada de acordo com a V Diretriz Brasileira de Hipertensão Arterial e classificada de acordo com o NCEP-ATPIII. A regressão logística foi realizada para determinar a probabilidade de alterações na PAS e PAD de acordo com a ingestão dietética. Adotou-se como significante o valor de p < 0,05. RESULTADOS: Observou-se correlação positiva da pressão arterial diastólica com o consumo de colesterol e açúcar; e negativa com a ingestão de fibras, porções de óleo e qualidade da dieta. A variedade da dieta ≥ 8 itens alimentares apresentou efeito protetor para alterações da pressão arterial sistólica; OR = 0,361 (0,148-0,878). CONCLUSÃO: A maior variedade da dieta ofereceu efeito protetor para alteração da pressão arterial sistólica.
Hipertensão; pressão arterial; dieta hipossódica; qualidade dos alimentos
Dietary variety is a protective factor for elevated systolic blood pressure
Erick Prado de Oliveira; Karina Fernandes de Camargo; Gabriela Kaiser Fullin Castanho; Marina Nicola; Kátia Cristina Portero-McLellan; Roberto Carlos Burini
Centro de Metabolismo em Exercício e Nutrição (CeMENutri) - Departamento de Saúde Pública - Faculdade de Medicina de Botucatu (UNESP); Departamento de Patologia - Faculdade de Medicina de Botucatu (UNESP), Botucatu, SP - Brasil
Mailing Address
ABSTRACT
BACKGROUND: Diet directly influences systemic arterial hypertension (SAH), which is one of the main risk factors for cardiovascular disease.
OBJECTIVE: To associate hypertension with dietary factors in adults clinically selected for a change-of-lifestyle program.
METHODS: Cross-sectional study comprising 335 individuals, aged between 44 and 65 years, clinically selected for a change-of-lifestyle program. We evaluated anthropometric data (BMI, %body fat and waist circumference), biochemical components (plasma glucose, triglycerides, total cholesterol, HDL-C and LDL-c) and diet, through the 24-hour recall method. The quality of the diet was assessed by the Healthy Eating Index. Blood pressure was measured according to the V Brazilian Guidelines on Hypertension and classified according to NCEP-ATPIII. Logistic regression was performed to determine the likelihood of changes in SBP and DBP according to dietary intake. The level of significance was set at p <0.05.
RESULTS: There was a positive correlation between diastolic blood pressure and sugar and cholesterol intake, and a negative one with intake of fiber, portions of oil and fats and diet quality. Dietary variety with ≥ 8 food items showed a protective effect for alterations in systolic blood pressure, OR = 0.361 (0.148 to 0.878).
CONCLUSION: A greater dietary variety had a protective effect on the systolic blood pressure.
Keywords: Hypertension; blood pressure; diet, sodium-restricted; food quality.
Introduction
Systemic arterial hypertension (SAH) is a major risk factor for cardiovascular mortality, being related to the increase of its incidence1,2. It has a greater influence on the risk of cardiovascular disease than smoking, hypercholesterolemia, hyperglycemia and obesity3.
According to population studies, the prevalence of hypertension in Brazil varies from 25.2% to 41.1%4-6, being more prevalent in women, especially after menopause7. The most recent Basic Data Indicators (BDI) survey shows that the prevalence of hypertension in the Brazilian population is 23.9% in adults, and when considered by gender, 21% of men and 26.3% of women have the disease8. SAH has high medical and socioeconomic costs arising mainly from its complications, such as cerebrovascular disease, coronary artery disease, heart failure, chronic renal failure and lower extremity vascular disease2.
Among the most important associated risk factors, some are considered not modifiable such as age, gender, ethnicity, socioeconomic factors and genetics. Among the modifiable ones, the inadequate lifestyle is related to higher prevalence of hypertension and reduced protection against the disease9. Therefore, a key component for the prevention and treatment of hypertension is the change in lifestyle, such as adopting a low-calorie diet, weight reduction, physical activity, decrease alcohol and/or salt intake2, which is the most effective and less costly way in terms of public health10.
The beneficial effects of a healthy diet (rich in fruits and vegetables, low on fat) on the behavior of blood pressure are well known11. Among the nutritional factors that are associated with high prevalence of hypertension are the high consumption of alcohol and sodium and excess weight. Recently, the consumption of potassium, calcium and magnesium has also been associated, which would attenuate the progressive increase in blood pressure with age12.
The Brazilian Society of Hypertension, in its guidelines, has started to recommend the DASH (Dietary Approaches to Stop Hypertension) diet in the non-pharmacological treatment of hypertension 2. The DASH diet emphasizes increased consumption of fruits, vegetables and low-fat dairy products, as well as whole grains, poultry, fish and nuts, and reduced consumption of fats, red meat, sweets and soft drinks. In a study carried out in patients with hypertension it has been observed that DASH substantially reduced blood pressure (systolic: 5.5 mmHg) in a period of two months, and, when combined with reduction in sodium intake, there was an additional decrease in blood pressure (systolic: 8.9 mm Hg)13.
To our knowledge, no national study has evaluated the influence of diet quality and consumption of servings of the food pyramid on hypertension and/or alterations in systolic (SBP) and diastolic blood pressure (DBP). Our group has shown the influence of diet on some risk factors for cardiovascular disease14-16; however, an association with hypertension has yet to be demonstrated. Accordingly, we intend to study the association of diet on hypertension in adults clinically selected for a change-of-lifestyle program.
Methods
Sample
A cross-sectional study was carried out in a subgroup of individuals referred to a change-of-lifestyle program, called "Move Pro-Health", in the city of Botucatu, state of São Paulo, Brazil, from 2004 to 2008. Individuals were voluntarily recruited for the study (convenience sample).
We evaluated 335 individuals, with or without systemic hypertension of both sexes (76.4% women), aged between 44 and 65, selected for the change-of-lifestyle program.
All subjects signed an informed consent form, which, together with the project, was approved by the Ethics in Research Committee (protocol # 3271-2009) from Faculdade de Medicina de Botucatu (FMB - UNESP).
Biochemical Assessment
To perform the biochemical analyses, subjects underwent blood collection after an overnight fast (8-12 hours), via standard venipuncture procedure. Blood was analyzed for glucose, triglycerides (TG), total cholesterol (TC) and HDL cholesterol (HDL-C) measurements, quantified in serum by the dry-chemistry method (Sistema Vitros, Johnson & Johnson), while the concentrations of LDL cholesterol (LDL-C) was estimated using Friedewald formula17 [LDL-C = TC - (HDL-C + TG / 5]). The classification of normal values followed those established by NCEP-ATPIII18.
Anthropometric Assessment
The anthropometric assessment consisted of measurements of body weight and height, according to the procedures described by Heyward and Stolarczyk19, with subsequent calculation of Body Mass Index (BMI). BMI was classified according to the World Health Organization20.
The Abdominal Circumference (AC) was measured using an inextensible, inelastic, measuring tape and the measurement was performed at midpoint between the lower margin of the last palpable rib and the iliac crest18.
The calculation of body composition, body fat percentage (BF%) and Fat Free Mass (FFM) was carried out by bioelectrical impedance (BIA) in a BiodynamicsÒ device (model 450, USA). Based on the resistance in ohms obtained by BIA and the calculation of BMI, the equation of Segal et al. was applied to obtain the fat-free mass21. Based on the values of FFM, we estimated the Absolute Fat Mass (AFM) by subtracting the body weight minus FFM and calculating the % BF.
Dietary Intake Assessment
Dietary intake was assessed by nutritional history with the 24-hour recall method. The recall was applied from Tuesday to Friday and the data related to the weekend were not collected. Dietary data were in household measures and were converted to grams and milliliters to enable chemical analysis of food consumption. Culinary preparations made with more than one food group had their ingredients distinguished and classified in their respective groups, a procedure that follows the adapted Brazilian Food Pyramid Guide recommendations22.
Subsequently, the data were processed using the nutritional analysis software NutWin (2002), release 1.523. The quality of the diet was assessed by the Healthy Eating Index (HEI)24, based on Adapted Brazilian Food Pyramid22.
HEI is a dietary analysis method used to determine the individual's quality of diet. We considered the eight food groups of the food pyramid, the percentage of total fat, saturated fat, amount of dietary cholesterol and dietary variety for the score. The variety of diet was defined as the amount of different food items present in the diet.
Clinical assessment of blood pressure
We evaluated the systolic and diastolic blood pressure of subjects in the sitting position, according to the procedures described by the VI Brazilian Guidelines on Arterial Hypertension2, with cuffs of adequate size for arm circumference, respecting the width / length ratio of 1:2, the width on the rubber cuff that must correspond to 40% of arm circumference, and its length, of at least 80%. The time interval between blood pressure measurements was 1-2 minutes. The subjects were diagnosed as having hypertension according to "The Adult Treatment Panel III of the National Cholesterol Education Program" (NCEP-ATP III)18.
Statistical Analysis
The tests were performed using SAS software release 9.1 and STATISTICA 6.0. Data were presented as mean ± SD. For comparison of individuals with or without hypertension, the t test was used for continuous variables.. Normality of the sample was tested through the Shapiro-Wilk test. Pearson's partial correlation was used to correlate the dietary variables with systolic and diastolic blood pressure, adjusted for sex, age, total caloric intake (TCI), and BMI. A linear regression analysis was performed with 95% confidence interval (95%CI) to observe the odds ratio of the studied individuals to present hypertension and alterations in SBP and DBP according to dietary intake. Data were adjusted for sex, age, BMI, and TCI. The results were discussed based on the significance level of p <0.05.
Results
It was observed that individuals with hypertension had higher BMI, %BF and WC. There was no significant difference between groups when dietary parameters were assessed. Regarding the biochemical data, the group of hypertensive patients had higher plasma concentrations of fasting glucose, total cholesterol, LDL-C and triglycerides when compared to the nonhypertensive group (Table 1).
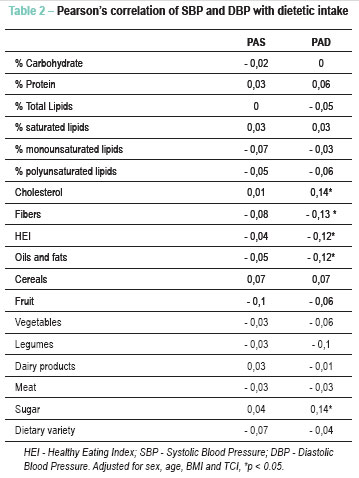
Table 2 shows Pearson's correlation between the food groups and the values of SBP and DBP. There was a positive correlation between DBP and the consumption of cholesterol and sugar, and a negative one with the consumption of fibers, servings of oil/fats and HEI.
According to Table 3, a dietary variety ≥ 8 food items showed a protective effect for alterations in SBP. There was no association between diet and hypertension and DBP.
To explain the inverse relationship between dietary variety and SBP, a correlation was performed between diet variety with all food components in order to characterize the consumption of individuals who had more varied diets. A positive correlation was observed between dietary variety with intake of vegetables (r = 0.34, p <0.05), fruit (r = 0.32, p <0.05), fibers (r = 0.22, p <0.05), dairy products (r = 0.20, p <0.05) and HEI (r = 0.20, p <0.05) and a negative one for legume consumption (r = -0.11; p <0.05), meats (r = -0.15, p <0.05) and cereals (r = -0.19, p <0.05). There was no significant correlation for intake of macronutrients, servings of oil/fats and sugar (data not shown).
Discussion
The main result of this study was that dietary variety (food items ≥ 8) offered a protective effect for alterations in SBP regardless of gender, age, BMI, and TCI. Furthermore, we observed a positive correlation between dietary variety and food sources of potassium, calcium and fibers (vegetables, fruit, dairy products) and a negative one with foods high in saturated fat, sodium and refined carbohydrates (meat and % of carbohydrate).
The consumption of potassium, calcium and magnesium has been associated with attenuation of the progressive increase in blood pressure levels12. Potassium is responsible for the reduction in intracellular sodium through the sodium-potassium pump and induces the decrease in blood pressure (BP) by increasing the natriuresis, reducing renin and norepinephrine and increasing prostaglandin secretion. Calcium helps regulate the heartbeat and reduces sodium levels when in high concentrations and magnesium inhibits the contraction of vascular smooth muscle and may play a role in regulating BP as a vasodilator25,26.
A study carried out recently in Japan investigated the associations of consumption of fruit, vegetables and their micronutrients with a reduced risk of SAH. The high consumption of fruit and vegetables was associated with a lower risk of developing hypertension, suggesting that the decrease in blood pressure was due to the presence of potassium and vitamin C in the foods27. A study with Australian adolescents showed that the consumption of fruit, vegetables, grains and fish was inversely associated with DBP28.
No direct effect of fruit and vegetable consumption was observed in our study, probably due to the fact that both hypertensive and nonhypertensive patients showed low consumption of this type food; moreover, there was no difference regarding the consumption of these food groups between the groups.
The consumption of fibers was negatively correlated with the decrease in BP, albeit weakly. This fact can also be explained by the low fiber consumption in both groups. It is known that individuals with high intake of dietary fiber may have significantly lower risk for developing coronary heart disease, infarction, hypertension, diabetes and obesity29,30.
We observed a positive correlation between sugar consumption and DBP. Inadequate consumption of this type of food is associated with increased insulin production, and may have a direct effect on the increase in renal reabsorption of sodium and thus, increase BP31. Moreover, insulin resistance and hyperinsulinemia may play a role in the pathogenesis of hypertension associated with obesity, due to the increase in inflammatory markers32,33. Hyperinsulinemia causes increased activity of the sympathetic nervous system and tubular reabsorption of sodium, actions that contribute to the increase in BP34-36.
Higher BMI, %BF and WC were observed among individuals with hypertension, which was expected37. Visceral fat can mediate the increase in blood pressure by reducing the natriuresis. The higher sodium retention would be caused by the activation of the renin-angiotensin system, activation of the sympathetic nervous system and also by changes in intrarenal hemodynamics, consequent to the compression of the renal medulla38. This shows the importance of adjusting the data for adiposity (BMI) when we analyze the influence of diet on hypertension, because then, these effects can be neutralized.
It was observed that hypertensive individuals showed higher plasma glucose, glycemia, total cholesterol, triglycerides and LDL-C levels, which increases the risk of cardiovascular diseases30. According to Schaan et al39, individuals with some degree of abnormal glucose homeostasis had a higher prevalence of hypertension.
Study limitations
This was a cross-sectional study, and, therefore, the cause-effect mechanisms cannot be defined. Secondly, 24-hour recall was conducted in a single a day, which may not accurately reflect the habits of the evaluated individuals. Moreover, the consumption of sodium and alcohol was not evaluated, which may influence blood pressure.
Conclusion
The present study showed that the greater the dietary variety (eight or more different types of food) offered a protective effect for alterations in SBP. The other dietary variables studied were not significantly associated with BP.
References
- 1. Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review.
- 2. Sociedade Brasileira de Cardiologia / Sociedade Brasileira de Hipertensão / Sociedade Brasileira de Nefrologia. VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1 supl. 1):1-51.
- 3. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-52.
- 4. Cipullo JP, Martin JF, Ciorlia LA, Godoy MR, Cação JC, Loureiro AA, et al. Prevalência e fatores de risco para hipertensão em uma população urbana brasileira. Arq Bras Cardiol. 2010;94(4):519-26.
- 5. de Souza AR, Costa A, Nakamura D, Mocheti LN, Stevanato Filho PR, Ovando LA. Um estudo sobre hipertensão arterial sistêmica na cidade de Campo Grande, MS. Arq Bras Cardiol. 2007;88(4):441-6.
- 6. Castro RA, Moncau JE, Marcopito LF. Hypertension prevalence in the city of Formiga, MG (Brazil). Arq Bras Cardiol. 2007;88(3):334-9.
- 7. Barton M, Meyer MR. Postmenopausal hypertension: mechanisms and therapy. Hypertension. 2009;54(1):11-8.
- 8. Ministério da Saúde. Datasus. Pesquisa e indicadores de dados básicos do Brasil. [Acesso em 2011 maio 16]. Disponível em http://tabnet.datasus.gov.br/cgi/idb2009/matriz.htm
- 9. Greenlund KJ, Daviglus ML, Croft JB. Differences in healthy lifestyle characteristics between adults with prehypertension and normal blood pressure. J Hypertens. 2009;27(5):955-62.
- 10. Mensah GA, Bakris G. Treatment and control of high blood pressure in adults. Cardiol Clin. 2010;28(4):609-22.
- 11. Parikh A, Lipsitz SR, Natarajan S. Association between a DASH-like diet and mortality in adults with hypertension: findings from a population-based follow-up study. Am J Hypertens. 2009;22(4):409-16.
- 12. Molina MDCB, Cunha RS, Herkenhoff LF, Mill JG. Hipertensão arterial e consumo de sal em população urbana. Rev Saúde Pública. 2003;37(6):743-50.
- 13. Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am J Hypertens. 2007;20(3):225-32.
- 14. de Oliveira EP, Manda RM, Torezan GA, Corrente JE, Burini RC. Dietary, anthropometric, and biochemical determinants of plasma high-density lipoprotein-cholesterol in free-living adults. Cholesterol. 2011;2011:851750. Epub 2010 Dec 15.
- 15. Pimentel GD, Portero-McLellan KC, de Oliveira EP, Spada AP, Oshiiwa M, Zemdegs JC, et al. Long-term nutrition education reduces several risk factors for type 2 diabetes mellitus in Brazilians with impaired glucose tolerance. Nutr Res. 2010;30(3):186-90.
- 16. Takahashi MM, de Oliveira EP, Moreto F, Portero-McLellan KC, Burini RC. Association of dyslipidemia with intakes of fruit and vegetables and the body fat content of adults clinically selected for a lifestyle modification program. Arch Latinoam Nutr. 2010;60(2):148-54.
- 17. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499-502.
- 18. de Lemos AS, Wolfe ML, Long CJ, Sivapackianathan R, Rader DJ. Identification of genetic variants in endothelial lipase in persons with elevated high-density lipoprotein cholesterol. Circulation. 2002;106(11):1321-6.
- 19. Heyward VH, Stolarczyk LM. Avaliação da composição corporal aplicada. São Paulo: Manole; 2000.
-
20World Health Organization (WHO). The World Health Report 2002: reducing risks, promoting healthy lifestyles. Geneva; 2002.
- 21. Segal KR, Van Loan M, Fitzgerald PI, Hodgdon JA, Van Itallie TB. Lean body mass estimation by bioelectrical impedance analysis: a four-site cross-validation study. Am J Clin Nutr. 1988;47(1):7-14.
- 22. Philippi ST, Latterza AR, Cruz AT, Ribeiro LC. Adapted food pyramid: a guide for a right food choice. Rev Nutr. 1999;12(1):65-80.
- 23. Navab M, Ananthramaiah GM, Reddy ST, Van Lenten BJ, Ansell BJ, Hama S, et al. The double jeopardy of HDL. Ann Med. 2005;37(3):173-8.
- 24. Mota JF, Rinaldi AEM, Pereira AF, Maestá N, Scarpin MM, Burini RC. Adaptation of the healthy eating index to the food guide of the Brazilian population. Rev Nutr. 2008;21(5):545-52.
- 25. Franceschini SCC, Priore SE, Euclydes MP. Necessidades e recomendações de nutrientes. In: Cupari L. Guias de medicina ambulatorial e hospitalar. UNIFESP/ Escola Paulista de Medicina. 2ª ed. São Paulo: Manole; 2002. p. 3-26.
- 26. Davis MM, Jones DW. The role of lifestyle management in the overall treatment plan for prevention and management of hypertension. Semin Nephrol. 2002;35(2):35-43.
- 27. Utsugi MT, Ohkubo T, Kikuya M, Kurimoto A, Sato RI, Suzuki K, et al. Fruit and vegetable consumption and the risk of hypertension determined by self measurement of blood pressure at home: the Ohasama study. Hypertens Res. 2008;31(7):1435-43.
- 28. McNaughton SA, Ball K, Mishra GD, Crawford DA. Dietary patterns of adolescents and risk of obesity and hypertension. J Nutr. 2008;138(2):364-70.
- 29. Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, et al. Health benefits of dietary fiber. Nutr Rev. 2009;67(4):188-205.
- 30. Takahashi MM, de Oliveira EP, de Carvalho AL, Dantas LA, Burini FH, Portero-McLellan KC, et al. Metabolic syndrome and dietary components are associated with coronary artery disease risk score in free-living adults: a cross-sectional study. Diabetol Metab Syndr. 2011;3:7.
- 31. Carvalho MHC, Colaço AL, Fortes ZB. Citocinas, disfunção endotelial e resistência à insulina. Arq Bras Endocrinol Metab. 2006;50(2):304-12.
- 32. Orsatti FL, Nahas EA, Orsatti CL, de Oliveira EP, Nahas-Neto J, da Mota GR, et al. Muscle mass gain after resistance training is inversely correlated with trunk adiposity gain in postmenopausal women. J Strength Cond Res. 2011 Oct 7. [Epub ahead of print]
- 33. Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860-7.
- 34. DeFronzo RA, Ferrannini E. Insulin resistance. a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991;14(3):173-94.
- 35. Rosa EC, Zanella MT, Ribeiro AB, Junior OK. Obesidade visceral, hipertensão arterial e risco cárdio-renal: uma revisão. Arq Bras Endocrinol Metab. 2005;49(2):196-204.
- 36. Lopes HF. Hipertensão e inflamação: papel da obesidade. Rev Bras Hipertens. 2007;14(4):239-44.
- 37. Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128(2):81-8.
- 38. Manrique C, Lastra G, Gardner M, Sowers JR. The renin angiotensin aldosterone system in hypertension: roles of insulin resistance and oxidative stress. Med Clin North Am. 2009;93(3):569-82.
- 39. Schann BDA, Harzheim E, Gus I. Perfil de risco cardíaco no diabetes mellitus e na glicemia de jejum alterada. Rev Saúde Pública. 2004;38(4):529-36.
Publication Dates
-
Publication in this collection
15 Mar 2012 -
Date of issue
Apr 2012
History
-
Received
09 Aug 2011 -
Accepted
01 Dec 2011 -
Reviewed
09 Aug 2011