Abstracts
BACKGROUND: Left bundle-branch block (LBBB) and the presence of systolic dysfunction are the major indications for cardiac resynchronization therapy (CRT). Mechanical ventricular dyssynchrony on echocardiography can help identify patients responsive to CRT. Left bundle-branch block can have different morphologic patterns. OBJECTIVE: To compare the prevalence of mechanical dyssynchrony in different patterns of LBBB in patients with left systolic dysfunction. METHODS: This study assessed 48 patients with ejection fraction (EF) < 40% and LBBB consecutively referred for dyssynchrony analysis. Conventional echocardiography and mechanical dyssynchrony analysis were performed, interventricular and intraventricular, with ten known methods, using M mode, Doppler and tissue Doppler imaging, isolated or combined. The LBBB morphology was categorized according to left electrical axis deviation in the frontal plane and QRS duration > 150 ms. RESULTS: The patients' mean age was 60 ± 11 years, 24 were males, and mean EF was 29% ± 7%. Thirty-two had QRS > 150 ms, and22, an electrical axis between -30º and +90º. Interventricular dyssynchrony was identified in 73% of the patients, while intraventricular dyssynchrony, in 37%-98%. Patients with QRS > 150 ms had larger left atrium and ventricle, and lower EF (p < 0.05). Left electrical axis deviation associated with worse diastolic function and greater atrial diameter. Interventricular and intraventricular mechanical dyssynchrony (ten methods) was similar in the different LBBB patterns (p = ns). CONCLUSION: In the two different electrocardiographic patterns of LBBB analyzed, no difference regarding the presence of mechanical dyssynchrony was observed.
Bundle-Branch Block; Ventricular Dysfunction; Cardiac Resynchronization Therapy; Stroke Volume
FUNDAMENTOS: O bloqueio do ramo esquerdo (BRE) e a presença de disfunção sistólica são as principais indicações de terapia de ressincronização cardíaca (TRC). A dissincronia ventricular mecânica pela ecocardiografia pode ajudar a identificar pacientes responsivos à TRC. O BRE pode mostrar diferentes padrões em sua morfologia. OBJETIVO: Comparar a prevalência de dissincronia mecânica em diferentes padrões de BRE em pacientes com disfunção sistólica esquerda. MÉTODOS: Analisaram-se 48 pacientes com fração de ejeção (FE) < 40% e BRE referidos consecutivamente para análise de dissincronia. Foram realizados ecocardiograma convencional e análise da dissincronia mecânica, interventricular e intraventricular, por 10 conhecidos métodos, usando modo M, Doppler e Doppler tecidual, sozinhos ou combinados. A morfologia do BRE foi categorizada pelo desvio esquerdo do eixo no plano frontal e duração de QRS > 150 ms. RESULTADOS: Eram 24 homens, com idade 60 ± 11 anos e FEVE de 29 ± 7%. Trinta e dois apresentavam QRS > 150 ms, e 22, ECG eixo entre -30º e +90º. A dissincronia interventricular foi identificada em 73% dos pacientes e a intraventricular em valores entre 37-98%. Portadores de QRS > 150 ms apresentaram maiores dimensões do átrio e ventrículo esquerdos, e menor FE (p < 0,05), e o desvio esquerdo do eixo associou-se a pior função diastólica e maior diâmetro atrial. A presença de dissincronia mecânica interventricular e intraventricular (10 métodos) foi semelhante entre os diferentes padrões de BRE (p = ns). CONCLUSÃO: Nos dois diferentes padrões eletrocardiográficos de BRE analisados, não foram observadas diferenças em relação à presença de dissincronia mecânica.
Bloqueio de Ramo; Disfunção Ventricular; Terapia de Ressincronização Cardíaca; Volume Sistólico
Instituto Dante Pazzanese de Cardiologia, São Paulo, SP - Brazil
Mailing Address
ABSTRACT
BACKGROUND: Left bundle-branch block (LBBB) and the presence of systolic dysfunction are the major indications for cardiac resynchronization therapy (CRT). Mechanical ventricular dyssynchrony on echocardiography can help identify patients responsive to CRT. Left bundle-branch block can have different morphologic patterns.
OBJECTIVE: To compare the prevalence of mechanical dyssynchrony in different patterns of LBBB in patients with left systolic dysfunction.
METHODS: This study assessed 48 patients with ejection fraction (EF) < 40% and LBBB consecutively referred for dyssynchrony analysis. Conventional echocardiography and mechanical dyssynchrony analysis were performed, interventricular and intraventricular, with ten known methods, using M mode, Doppler and tissue Doppler imaging, isolated or combined. The LBBB morphology was categorized according to left electrical axis deviation in the frontal plane and QRS duration > 150 ms.
RESULTS: The patients' mean age was 60 ± 11 years, 24 were males, and mean EF was 29% ± 7%. Thirty-two had QRS > 150 ms, and 22, an electrical axis between -30º and +90º. Interventricular dyssynchrony was identified in 73% of the patients, while intraventricular dyssynchrony, in 37%-98%. Patients with QRS > 150 ms had larger left atrium and ventricle, and lower EF (p < 0.05). Left electrical axis deviation associated with worse diastolic function and greater atrial diameter. Interventricular and intraventricular mechanical dyssynchrony (ten methods) was similar in the different LBBB patterns (p = ns).
CONCLUSION: In the two different electrocardiographic patterns of LBBB analyzed, no difference regarding the presence of mechanical dyssynchrony was observed.
Keywords: Bundle-Branch Block; Ventricular Dysfunction; Cardiac Resynchronization Therapy; Stroke Volume.
Introduction
Heart failure, a clinical syndrome resulting from structural and/or functional cardiac dysfunction, is known to be the end stage of several cardiopathies. Electrocardiographic alterations, such as left bundle-branch block (LBBB), are common findings in patients with heart failure, mainly in the presence of systolic dysfunction1,2.
Currently, there are several treatment options for heart failure. One efficient alternative is cardiac resynchronization therapy3 (CRT). The indication for implantation of a resynchronizing pacemaker is based on clinical and electrocardiographic criteria, and echocardiographic data. On the electrocardiogram, QRS complex enlargement, as observed in LBBB, is the most frequent indication for that treatment4-6. However, treatment failure has been reported in approximately 30% of the cases in several series3.
In addition to the already known classic information, such as left ventricular dimension and ejection fraction, echocardiography allows the analysis of interventricular and intraventricular synchronism, which is the focus of CRT. Different methods, using several echocardiographic techniques, have been used to detect and stratify dyssynchrony7,8, enabling predicting those who will have good results with a certain treatment.
Left bundle-branch block can have different characteristics related to higher morbidity and mortality9,10. The relationship between different characteristics of LBBB and dyssynchrony assessed on echocardiography is yet to be established, which might contribute to the lack of success of that therapy.
Objectives
This study aimed at comparing conventional echocardiographic findings and those of ventricular synchrony related to different LBBB morphologies in patients with left ventricular systolic dysfunction.
Methods
This study was approved by the Committee on Ethics and Research of the Instituto Dante Pazzanese de Cardiologia.
Study population
This study assessed individuals followed up on an outpatient basis for heart failure treatment, who were referred to the echocardiography section with systolic dysfunction characterized by ejection fraction below 40%, according to the Simpson's method. All patients had sinus rhythm and LBBB11. Patients with the following characteristics were excluded: under the age of 18 years; wearing a pacemaker; and those who had undergone previous valvular surgery or had any degree of aortic valvulopathy. The clinical data concerning functional class, history and medications used were also assessed.
Electrocardiogram
Twelve-lead electrocardiography was performed. The PR intervals and QRS complexes were measured, and the frontal axis characteristics were assessed. The patients were classified into two groups according to the presence of QRS interval > 150 ms or left electrical axis deviation in the frontal plane, i.e. , frontal axis values < -30º.
Echocardiogram
Echocardiogram was performed on a Vivid7® device (GE Vingmed, System VII, Horton, Norway). The images were acquired as digital clips. Then, linear and two-dimensional measures were taken according to the American Society of Echocardiography guidelines, using a mean of three consecutive cycles on a EchoPAC PC work station, version 6.0.1® (GE Vingmed Ultrasound). Diastolic function was also characterized according to the American Society of Echocardiography guidelines, and mitral valve regurgitation was quantified12,13.
Interventricular dyssynchrony was assessed as the difference between pre-ejection intervals, i.e. , from the beginning of the QRS complex to the beginning of the ventricular ejection into the aortic and pulmonary valves, using pulsed Doppler; interventricular dyssynchrony was considered to exist when that value exceeded 40 ms14,15. According to the literature, mechanical intraventricular dyssynchrony has been assessed by use of several methodologies, whose cutoff points have been described as markers of successful CRT. The analysis was performed according to the following criteria: 1) septal-to-posterior wall motion delay, in M mode, > 130 ms, as reported by Pitzalis et al16; 2) greater interval between maximum systolic motion of six left ventricular basal segments > 110 ms, measured on tissue Doppler, as demonstrated by Notabartolo et al17; 3) maximum systolic motion interval between the septum and lateral wall on tissue Doppler > 65 ms, as reported by Gorcsan et al18; 4) presence of positive criterion of the Saint Mary Hospital score, United Kingdom, as reported by Lane et al19; 5) positive criteria for the presence of dyssynchrony, as established by Cleland et al14, in the CARE-HF study; 6) standard deviation of the maximum motion times, measured on tissue Doppler maging, in 12 left ventricular segments > 32 ms, proposed by Yu et al7; 7) interval values > 60 ms of the onset of mitral ring systolic motion in four segments measured by use of tissue Doppler imaging, as reported by De Sutter et al20; 8) interval values > 100 ms of the end of mitral ring systolic motion in four segments measured on tissue Doppler imaging, as reported by Perez de Isla et al21, in the Spanish Ventricular Asynchrony Registry - RAVE; 9) interval between the maximum contraction of the anteroseptal and posterior segments > 130 ms measured by use of two-dimensional strain associated with the interval of the septal-to-lateral wall maximum systolic motion on tissue Doppler > 60 ms, as demonstrated by Gorcsan et al22
Statistical analysis
The quantitative variables were described as mean ± standard deviation, and the qualitative ones, as percentages. For comparing the different LBBB presentations, the following tests were used: Student t test; Wilcoxon test; chi-square test; and Fisher exact test. The JMP8.0® software (Institute Inc. , Carry, North Carolina) was used for calculation. The significance level of 5% was adopted.
Results
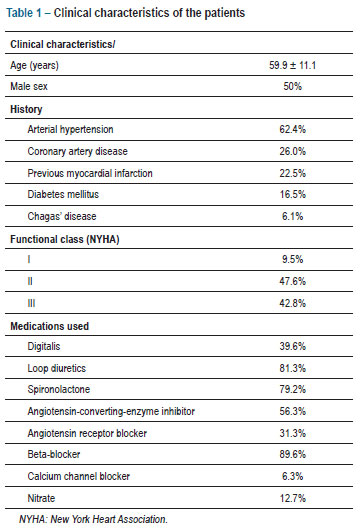
Table 1 shows the clinical characteristics of the 48 patients studied, with approximately 90% of them on beta-blockers and angiotensin-converting-enzyme inhibitors/angiotensin-receptor blockers. Table 2 shows their electrocardiographic findings. Table 3 shows their echocardiographic variables, with varied degrees of intraventricular dyssynchrony according to the criteria used.
When patients were compared according to their different LBBB morphologies, QRS duration > 150 ms and electrical axis in the frontal plane -30º did not relate to differences concerning sex, age, history, functional class or medication used, as shown in Tables 4 and 5.
Regarding echocardiographic findings, patients with QRS duration > 150 ms showed greater left ventricular linear dimensions and volumes, greater left atrial diameters and lower ejection fraction, as shown in Table 4.
Patients with left electrical axis deviation in the frontal plane, < -30º, showed greater left atrial diameters associated with higher grades of left ventricular diastolic dysfunction, and greater left ventricular diameter, as evidenced in Table 5.
The presence of interventricular and intraventricular dyssynchrony was similar in the two groups of LBBB (longer QRS interval duration and left electrical axis deviation in the frontal plane) (Tables 4 and 5).
Discussion
The different LBBB presentations assessed do not allow identifying a dyssynchrony pattern, and their prevalences did not differ in the different echocardiographic methodologies assessed.
However, the LBBB patterns relate to left ventricular morphologic and functional alterations, in which longer QRS complex durations associate with greater left ventricular dimensions, and the left electrical axis deviation on electrocardiogram relates to greater diastolic dysfunction and greater left atrial dimension.
Those findings are in accordance with the study by Das et al23, who have shown that left ventricular ejection fraction is more impaired when the QRS duration is increased in patients with LBBB, but it is not associated with left electrical axis deviation. However, according to Dhingra et al24, the higher incidence of events in patients with LBBB and left electrical axis deviation should be associated with greater diastolic dysfunction, which is known to relate to mortality25.
Although not all patients meet the criteria proposed by the last guidelines for implantation of resynchronizing pacemakers5, those indications have been modified, and most patients studied constitute a group candidate for CRT, including patients with ejection fraction < 40%5,26. Findings might indicate lack of relationship between longer QRS intervals in LBBB and the response to that type of treatment27, because the prevalence of mechanical dyssynchrony is similar regardless of the echocardiographic method used.
Despite the limitations of using echocardiography as the method for selecting candidates for pacemaker implantation with evidenced capacity of resynchronization on the PROSPECT study28, most of the methods used proved to distinguish patients who would benefit from that therapy. Single center studies have reported several echocardiographic methods that evidenced a better response to that therapy.
Sweeney et al29 have shown that the conventional electrocardiographic report in patients with LBBB, such as QRS duration and the presence of left electrical axis deviation, are not enough to predict individuals who will have echocardiographic improvement after cardiac resynchronization by use of pacemaker. However, electrocardiographic evidence of longer left ventricular activation time and smaller scar volume characterizes the group of patients with a better response to the resynchronizer. Such measures were not assessed in the present study, and the study by Sweeney et al29 has not compared those electrocardiographic findings with the echocardiographic assessment of mechanical synchrony. That relationship can be tested in a further study.
Conclusion
In the two different electrocardiographic patterns of LBBB analyzed with ten echocardiographic methods, no difference regarding the presence of mechanical dyssynchrony was observed. They can, however, be associated with known risk patterns, such as a reduced ejection fraction and greater diastolic dysfunction grades.
Author contributions
Conception and design of the research: Barretto RBM, Piegas LS, Moreira DA, França FF; Acquisition of data: Barretto RBM, Melo Neto JF, Resende TU; Analysis and interpretation of the data: Barretto RBM, Piegas LS, Assef JE, Melo Neto JF, Resende TU, Moreira DA, França FF; Statistical analysis and Obtaining funding: Barretto RBM; Writing of the manuscript: Barretto RBM, Piegas LS, Assef JE; Critical revision of the manuscript for intellectual content: Barretto RBM, Assef JE, LeBihan DC, Meneghelo RS, Sousa AGMR.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of doctoral submitted by Rodrigo Bellio de Mattos Barretto, from Universidade de São Paulo.
References
- 1. Aaronson KD, Schwartz JS, Chen TM, Wong KL, Goin JE, Mancini DM. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997;95(12):2660-7.
- 2. Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, Ordin DL, et al. Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol. 2003;41(2):217-23.
- 3. McAlister FA, Ezekowitz J, Hooton N, Vandermeer B, Spooner C, Dryden DM, et al. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA. 2007;297(22):2502-14.
- 4. Martinelli Filho M, Zimerman LI, Lorga AM, Vasconcelos JTM, Rassi A Jr. Diretrizes brasileiras de dispositivos cardíacos eletrônicos implantáveis (DCEI). Arq Bras Cardiol. 2007;89(6):e-210-38.
- 5. Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA 3rd, et al; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Heart Rhythm Society. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. [corrected]. Circulation. 2012;126(14):1784-800. Erratum in Circulation. 2013;127(3):e357-9
- 6. Vardas PE, Auricchio A, Blanc JJ, Daubert JC, Drexler H, Ector H, et al; European Society of Cardiology; European Heart Rhythm Association. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28(18):2256-95.
- 7. Yu CM, Abraham WT, Bax J, Chung E, Fedewa M, Ghio S, et al; PROSPECT Investigators. Predictors of response to cardiac resynchronization therapy (PROSPECT) - study design. Am Heart J. 2005;149(4):600-5.
- 8. Yu CM, Bax JJ, Gorcsan J 3rd Critical appraisal of methods to assess mechanical dyssynchrony. Curr Opin Cardiol. 2009;24(1):18-28.
- 9. Iuliano S, Fisher SG, Karasik PE, Fletcher RD, Singh SN; Department of Veterans Affairs Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure. QRS duration and mortality in patients with congestive heart failure. Am Heart J. 2002;143(6):1085-91.
- 10. Wang NC, Maggioni AP, Konstam MA, Zannad F, Krasa HB, Burnett JC Jr, et al; Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators. Clinical implications of QRS duration in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction. JAMA. 2008;299(22):2656-66.
- 11. Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: Part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council On Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53(11):982-91.
- 12. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10(2):165-93.
- 13. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al; American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16(7):777-802.
- 14. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352(15):1539-49.
- 15. Leclercq C, Kass DA. Retiming the failing heart: principles and current clinical status of cardiac resynchronization. J Am Coll Cardiol. 2002;39(2):194-201.
- 16. Pitzalis MV, Iacoviello M, Romito R, Massari F, Rizzon B, Luzzi G, et al. Cardiac resynchronization therapy tailored by echocardiographic evaluation of ventricular asynchrony. J Am Coll Cardiol. 2002;40(9):1615-22.
- 17. Notabartolo D, Merlino JD, Smith AL, DeLurgio DB, Vera FV, Easley KA, et al. Usefulness of the peak velocity difference by tissue Doppler imaging technique as an effective predictor of response to cardiac resynchronization therapy. Am J Cardiol. 2004;94(6):817-20.
- 18. Gorcsan J 3rd, Kanzaki H, Bazaz R, Dohi K, Schwartzman D. Usefulness of echocardiographic tissue synchronization imaging to predict acute response to cardiac resynchronization therapy. Am J Cardiol. 2004;93(9):1178-81.
- 19. Lane RE, Chow AW, Chin D, Mayet J. Selection and optimisation of biventricular pacing: the role of echocardiography. Heart. 2004;90 Suppl 6:vi10-6.
- 20. De Sutter J, Van de Veire NR, Muyldermans L, De Backer T, Hoffer E, Vaerenberg M, et al; Working Group of Echocardiography and Cardiac Doppler of the Belgian Society of Cardiology. Prevalence of mechanical dyssynchrony in patients with heart failure and preserved left ventricular function (a report from the Belgian multicenter registry on dyssynchrony). Am J Cardiol. 2005;96(11):1543-8.
- 21. Perez de Isla L, Florit J, Garcia-Fernandez MA, Evangelista A, Zamorano J. Prevalence of echocardiographically detected ventricular asynchrony in patients with left ventricular systolic dysfunction. J Am Soc Echocardiogr. 2005;18(8):850-9.
- 22. Gorcsan J 3rd, Tanabe M, Bleeker GB, Suffoletto MS, Thomas NC, Saba S, et al. Combined longitudinal and radial dyssynchrony predicts ventricular response after resynchronization therapy. J Am Coll Cardiol. 2007;50(15):1476-83.
- 23. Das MK, Cheriparambil K, Bedi A, Kassotis J, Reddy CV, Makan M, et al. Prolonged QRS duration (QRS >170 ms) and left axis deviation in the presence of left bundle branch block: a marker of poor left ventricular systolic function? Am Heart J. 2001;142(5):756-9.
- 24. Dhingra RC, Amat-Y-Leon F, Wyndham C, Sridhar SS, Wu D, Rosen KM. Significance of left axis deviation in patients with chronic left bundle branch block. Am J Cardiol. 1978;42(4):551-6.
- 25. Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194-202.
- 26. Linde C, Abraham WT, Gold MR, St John Sutton M, Ghio S, Daubert C; REVERSE (REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction) Study Group. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J Am Coll Cardiol. 2008;52(23):1834-43.
- 27. Mollema SA, Bleeker GB, van der Wall EE, Schalij MJ, Bax JJ. Usefulness of QRS duration to predict response to cardiac resynchronization therapy in patients with end-stage heart failure. Am J Cardiol. 2007;100(11):1665-70.
- 28. Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, et al. Results of the predictors of response to CRT (PROSPECT) trial. Circulation. 2008;117(20):2608-16.
- 29. Sweeney MO, van Bommel RJ, Schalij MJ, Borleffs CJ, Hellkamp AS, Bax JJ. Analysis of ventricular activation using surface electrocardiography to predict left ventricular reverse volumetric remodeling during cardiac resynchronization therapy. Circulation. 2010;121(5):626-34.
- 30. Yu CM, Zhang Q, Fung JW, Chan HC, Chan YS, Yip GW, et al. A novel tool to assess systolic asynchrony and identify responders of cardiac resynchronization therapy by tissue synchronization imaging. J Am Coll Cardiol. 2005;45(5):677-84.
Mechanical dyssynchrony is similar in different patterns of left bundle-branch block
Publication Dates
-
Publication in this collection
24 Sept 2013 -
Date of issue
Nov 2013
History
-
Received
06 Nov 2012 -
Accepted
26 June 2013 -
Reviewed
19 June 2013