Cardiovascular Diseases/prevention & control; Risk Factors; Socioeconomic Factors; Primary Prevention; Health Promotion; Cardiovascular Diseases/guidelines
Introduction
Brazil currently faces a major health challenge: the pandemic scenario of cardiovascular morbidity and mortality. According to Brazilian Health Ministry data, 326,000 deaths due to cardiovascular diseases (CVD) occurred in 2010, corresponding to approximately 1,000 deaths/day, 200,000 deaths due exclusively to ischemic heart and cerebrovascular diseases, reflecting a gloomy scenario far from the minimally acceptable control.
This current scenario can be attributed to many reasons, such as the insufficiency and inadequacy of public health policies for CVD prevention, leading to the well-known lack of infrastructure in primary health care, hindering the fight against preventable affections, mainly in the neediest areas.
In addition, it is worth mentioning the well-known sociocultural factors, such as the excessive consumption of high-caloric foods in association with physical inactivity, and, consequently, the development of obesity and diabetes, and excessive salt intake. Those factors contribute to the development of arterial hypertension, being decisive to the high prevalence of CVD and no opportunity to provide instructions on lifestyle changes.
The medical societies, in partnership with governments and universities, have endeavored to elaborate valuable documents containing strategic plans of CVD prevention and fight. However, simple and objective guidelines, which can be easily accessed and managed by health care personnel, are required to implement that which has been long discussed by specialists and scientists, although with modest results.
For the first time, guidelines and consensus documents, most of which already published in several other guidelines of specialties, have been gathered in a single document to provide the clinician with easy access to the recommendations for primary and secondary CVD prevention. For that, the Brazilian Society of Cardiology (SBC) has gathered specialized physicians with large experience in preventive actions to elaborate the present document.
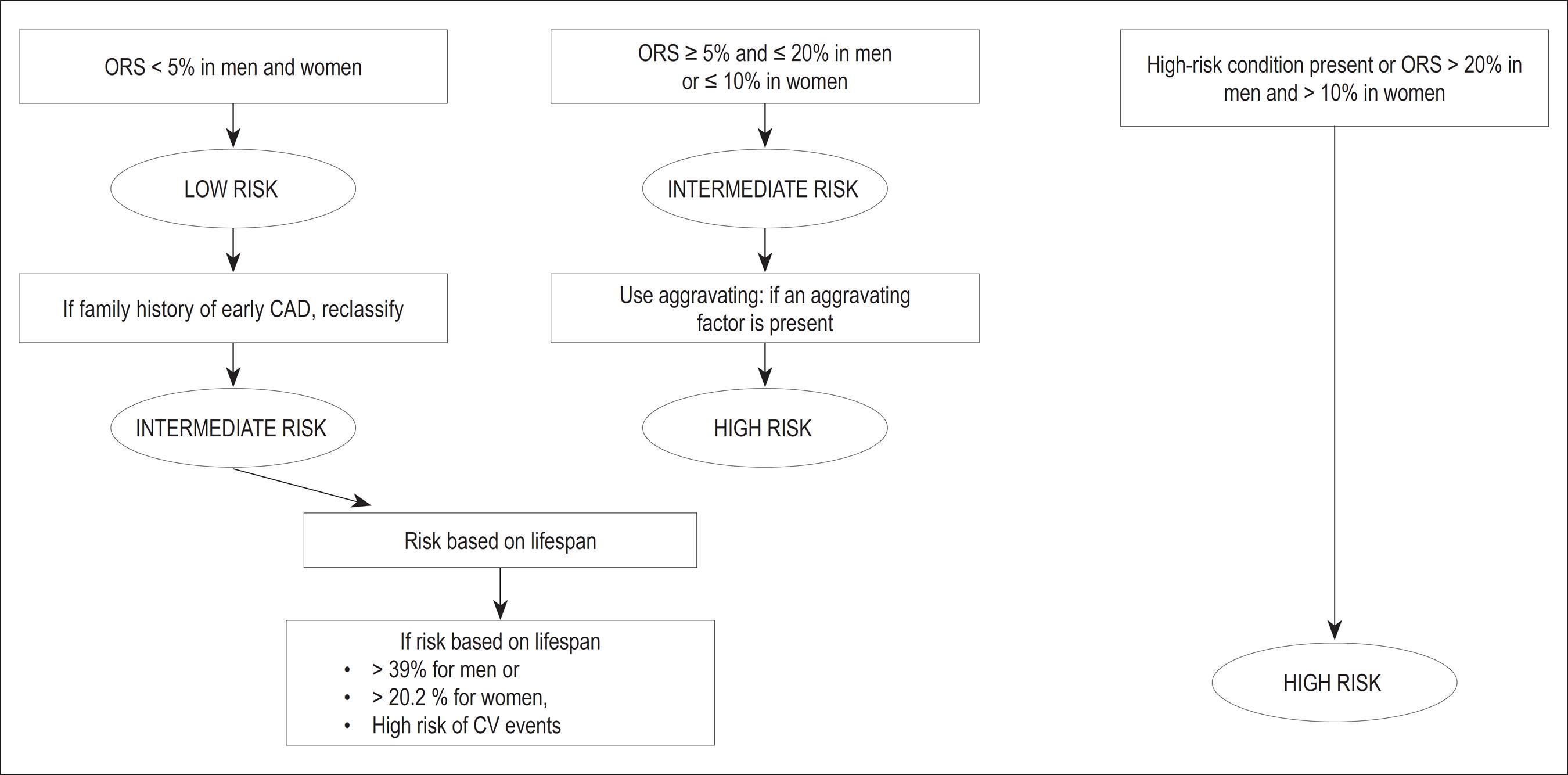
Chapter 1 presents the cardiovascular risk stratification for atherosclerosis prevention and treatment. In this chapter, the authors discuss questions such as acute coronary event as the first manifestation of atherosclerotic disease in at least half of the individuals with that complication. Thus, the identification of predisposed asymptomatic individuals is crucial to the effective prevention with correct definition of therapeutic goals, especially the criteria to identify high-risk patients (Table 1). The authors discuss the so-called risk scores, through which the overall risk is calculated, enabling the clinician to quantify and qualify the patients' individual risk, for both women (Tables 2 and 3) and men (Tables 4 and 5). The combination of those different scores allow the clinician to better estimate the risk, stratifying it gradually: presence of significant atherosclerotic disease or its equivalents; calculation of risk score; aggravating factors (Chart 1) and risk stratification based on lifespan. The authors propose a simplified algorithm for cardiovascular risk stratification, which is exemplified in Figure 1. The recommendations listed as class I and level of evidence A are few, because the other recommendations still require more comprehensive studies with long-term follow-up (Table 6).
Algoritmo de estratificação do risco cardiovascular. ERG: estratificação do risco global; DAC: doença arterial coronariana; CV: cardiovascular; RTV: risco por tempo de vida
Classification of recommendation and level of evidence for risk stratification in cardiovascular prevention
Chapter 2 approaches tobacco smoking, the major avoidable risk factor. It is known that 50% of the deaths of smokers, most of which caused by CVD, could be prevented with smoking cessation. In this chapter, the authors discuss preventive measures for tobacco use. Data from the Surveillance of Risk Factors and Protection Against Chronic Diseases via Telephone Inquiry (VIGITEL, in Portuguese), disclosed on April 2012, revealed advances in tobacco use control in Brazil, with 14.8% of smokers older than 18 years. They also approached the primordial prevention of tobacco use, enumerating factors that contribute to smoking initiation and proposing practical strategies for its combat. In addition, the authors discuss techniques to treat the psychological dependence of smokers with general and specific behavioral approaches. Furthermore, this chapter presents instruments to help to assess and understand the patient's profile by using universally accepted scales, such as Prochaska and Di Clemente's and Fagerström's. Finally, the authors approach, in a practical way, pharmacological treatment strategies of tobacco use, such as nicotine replacement with bupropion and varenicline, in addition to second-line drugs (nortriptyline), with their possible associations. Table 7 summarizes the classification of recommendation and level of evidence of those strategies.
Classification of recommendation and level of evidence for the treatment of smoking in cardiovascular prevention
Chapter 3 discusses the real benefits of primary and secondary CVD prevention, with evident confirmation of diet, supplements and vitamins, aiming at helping the clinician to guide the community in choosing and consuming those products. In addition to supplements, omega-3 fatty acids, vitamins B, C, D and E, folates, alpha-linolenic acids and carotenoids were assessed (Tables 8).
Summary of the recommendations for not using vitamin supplements to prevent cardiovascular disease (CVD) and recommendations for the consumption of products rich in omega-3 fatty acids
Chapter 4 approaches obesity, overweight and nutrition transition, as well as the consequences for cardiovascular morbidity and mortality of their association with arterial hypertension, dyslipidemias, type 2 diabetes, osteoarthritides and cancer. Tables 9 and 10 list the classification of recommendation and levels of evidence for primary and secondary prevention.
Summary of the recommendations for obesity and overweight in cardiovascular disease primary prevention
Summary of the recommendations for obesity and overweight in cardiovascular disease secondary prevention
Chapter 5 summarizes the recommendations for systemic arterial hypertension (SAH), emphasizing its importance for the development of several pathologies, such as coronary artery disease, heart failure, cerebrovascular disease and chronic kidney disease. Table 11 shows the routine initial assessment of hypertensive patients, and Table 12, its complementary assessment. Therapeutic decision should consider the patient's additional risk. Table 13 shows nonpharmacological measures, which are listed according to their recommendation class and level of evidence. Figure 2 shows the algorithm of pharmacological treatment based on the patients' hypertension stages. Monotherapy can be initiated with any drug class, but SAH control is only achieved in one-third of the cases with that strategy. Chart 2 shows the goals to be met according to patients' characteristics.
Algoritmo do tratamento da hipertensão arterial segundo a VI Diretrizes Brasileiras de Hipertensão Arterial
Chapter 6 was aimed at discussing dyslipidemias, in an attempt to, after stratifying the individual risk, establish the therapeutic goals according to the overall risk level (low, intermediate or high). Specific goals are listed for high- and intermediate-risk patients. Patients at low cardiovascular risk should have their goals individualized at their clinician's discretion and according to lipid reference values. Table 14 presents strategies for lifestyle changes. Table 15 lists the pharmacological alternatives based on their recommendation class and level of evidence.
Recommendations for the nonpharmacological treatment of dyslipidemia in cardiovascular prevention
Chapter 7 discusses diabetes, emphasizing its high prevalence in the adult population, up to 13.5% in some municipalities, which could represent a current population of 17 million individuals with diabetes. Those numbers are increasing due to factors such as population growth and aging, and increasing urbanization, sedentary lifestyle and obesity. This important chapter discusses essential measures for prevention, such as lifestyle changes (Table 16).
Dietary and physical activity interventions in diabetes mellitus (DM) to prevent cardiovascular disease
Chapter 8 provides a review on metabolic syndrome. There are several versions of the metabolic syndrome definition, and this guideline adopted the joint position paper of several international organizations on the topic. The authors discuss the epidemiological aspects of its prevalence, approaching different population groups, and aspects related to cardiovascular and metabolic risks, in addition to metabolic syndrome risk factors. Table 17 shows the recommendation class and level of evidence of interventions in metabolic syndrome.
Chapter 9 discusses the role played by physical activity, physical exercise and sports in CVD prevention. Physically active individuals tend to be healthier and have better quality of life and longer life expectancy. Table 18 lists the recommended physical exercise levels. In addition, the risks of physical activity are approached, as well as the basic principles for exercise prescription and strategies to encourage referral, implementation and adherence.
Chapter 10 discusses psychosocial factors in CVD prevention. Beginning with the definition of the concept, the chapter discusses the psychosocial conditions frequently associated with cardiovascular risk, such as low socioeconomic status, lack of social support, stress at work place and family life, depression, anxiety, hostility and type D personality. In addition, it assesses the recommendation class and level of evidence of approaching the psychosocial factors in primary prevention (Table 19) and for adherence (Table 20) by using cognitive-behavioral methods and indicating the 'ten strategic steps' to improve counseling for behavioral changes. Interventions on depression, anxiety and distress are also proposed as potential tools for adherence to preventive strategies (Chart 3), which can also be improved with the simple measures.
Classification of recommendation and level of evidence in approaching psychosocial factors in primary prevention
Classification of recommendation and level of evidence of adherence to strategy in cardiovascular prevention, lifestyle and medication
Chapter 11 approaches dyslipidemia, obesity and SAH in childhood and adolescence. Brazilian population studies have shown a 10%-35% prevalence of dyslipidemia in children and adolescents. Table 21 shows the reference values for lipids and lipoproteins in those age groups.
Table 22 shows the classification of SAH for children and adolescents. Changes in lifestyle are the initial therapeutic recommendation for primary SAH in children and adolescents. Pharmacological treatment is indicated for individuals with symptomatic hypertension, secondary hypertension, SAH target-organ lesion, types 1 and 2 diabetes mellitus, and persistent SAH despite the adoption of nonpharmacological measures, a situation in which such measures are an adjunct to the pharmacological treatment.
The diagnosis of obesity or overweight in children is clinical, and should be established via history and physical exam, followed by comparison of anthropometric data with population parameters, by using curves of body mass index (BMI) for age. Prevention comprises adequate nutrition during pregnancy, breastfeeding encouragement, identification of familial risk factors, careful child's growth and development follow-up, habit changes, especially the adoption of a healthy diet and global increase in physical activity. It is important to involve the child's entire family, parents, teachers and health care professionals, in addition to count on a multidisciplinary team.
The systematic analysis of studies on the effectiveness of interventions to promote physical activity in the pediatric age group (more particularly adolescents) has shown better results when the actions associate school, family and community, and when the educational actions involve environmental and health policies.
Table 23 shows the recommendations and their levels of evidence to prevent CVD in children and adolescents.
Classification of recommendation and level of evidence for the presence of cardiovascular diseases (CVD) in children and adolescents
Chapter 12 discusses topics related to legislation and prevention of CVD risk factors. The authors approach specific sanitary laws, discussing their effective role in health promotion and prevention, by creating healthy environments, in addition to emphasizing the importance of surveillance, prevention, health care, rehabilitation and health promotion
Chapter 13 discusses specific aspects of prevention of CVD associated with autoimmune diseases, influenza, chronic kidney disease, obstructive arterial disease, socioeconomic factors, obstructive sleep apnea, erectile dysfunction and periodontitis (Table 24).
We provide the medical class with a guideline that gathers, in one single publication, compiled and updated essential prevention topics to be used as a reference in CVD prevention.
-
Author contributionsConception and design of the research: Simão AF, Précoma DB, Andrade JP, Correa Filho H, Saraiva JFK, Oliveira GMM; Acquisition of data: Simão AF, Précoma DB, Correa Filho H, Oliveira GMM; Analysis and interpretation of the data: Simão AF, Correa Filho H, Saraiva JFK, Oliveira GMM; Writing of the manuscript: Simão AF, Précoma DB, Correa Filho H, Saraiva JFK, Oliveira GMM; Critical revision of the manuscript for intellectual content: Simão AF, Précoma DB, Andrade JP, Correa Filho H, Saraiva JFK, Oliveira GMM; Revision of the manuscript: Oliveira GMM.
-
Sources of FundingThere were no external funding sources for this study.
-
Study AssociationThis study is not associated with any thesis or dissertation work.
-
*
To access the complete document with references requested access the link: http://publicacoes.cardiol.br/consenso/2013/Diretriz_Prevencao_Cardiovascular.aspIntroduction
Publication Dates
-
Publication in this collection
May 2014
History
-
Received
29 Jan 2014 -
Reviewed
30 Jan 2014 -
Accepted
30 Jan 2014