Abstract
Background:
Physical examination and B-type natriuretic peptide (BNP) have been used to estimate hemodynamics and tailor therapy of acute decompensated heart failure (ADHF) patients. However, correlation between these parameters and left ventricular filling pressures is controversial.
Objective:
This study was designed to evaluate the diagnostic accuracy of physical examination, chest radiography (CR) and BNP in estimating left atrial pressure (LAP) as assessed by tissue Doppler echocardiogram.
Methods:
Patients admitted with ADHF were prospectively assessed. Diagnostic characteristics of physical signs of heart failure, CR and BNP in predicting elevation (> 15 mm Hg) of LAP, alone or combined, were calculated. Spearman test was used to analyze the correlation between non-normal distribution variables. The level of significance was 5%.
Results:
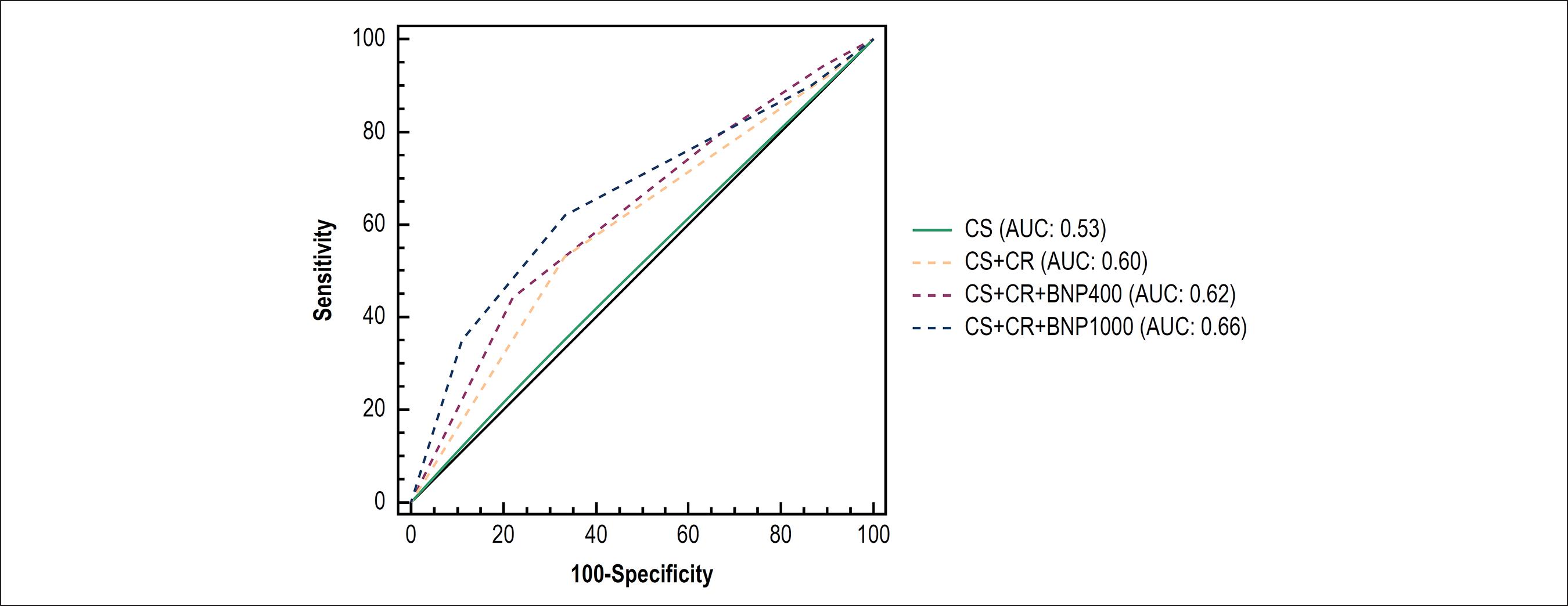
Forty-three patients were included, with mean age of 69.9 ± 11.1years, left ventricular ejection fraction of 25 ± 8.0%, and BNP of 1057 ± 1024.21 pg/mL. Individually, all clinical, CR or BNP parameters had a poor performance in predicting LAP ≥ 15 mm Hg. A clinical score of congestion had the poorest performance [area under the receiver operating characteristic curve (AUC) 0.53], followed by clinical score + CR (AUC 0.60), clinical score + CR + BNP > 400 pg/mL (AUC 0.62), and clinical score + CR + BNP > 1000 pg/mL (AUC 0.66).
Conclusion:
Physical examination, CR and BNP had a poor performance in predicting a LAP ≥ 15 mm Hg. Using these parameters alone or in combination may lead to inaccurate estimation of hemodynamics.
Keywords:
Heart Failure; Natriuretic Peptide, Brain; Hemodynamics; Ventricular Function, Left; Echocardiography, Doppler
Resumo
Fundamento:
Exame físico e peptídeo natriurético do tipo B (BNP) foram usados para estimar a hemodinâmica e adequar a terapia de pacientes com insuficiência cardíaca aguda descompensada (ICAD). Entretanto, correlação entre esses parâmetros e a pressão de enchimento do ventrículo esquerdo é controversa.
Objetivo:
Avaliar a acurácia diagnóstica do exame físico, da radiografia de tórax (RT) e do BNP para estimar a pressão atrial esquerda (PAE) avaliada pelo ecodopplercardiograma tecidual.
Métodos:
Pacientes admitidos com ICAD foram avaliados prospectivamente. As características diagnósticas dos sinais físicos de insuficiência cardíaca, RT e BNP para predizer elevação da PAE (> 15 mmHg), isolados ou combinados, foram calculadas. Teste de Spearman foi usado para analisar a correlação entre variáveis de distribuição não normal. O nível de significância foi 5%.
Resultados:
Este estudo incluiu 43 pacientes com idade média de 69,9 ± 11,1 anos, fração de ejeção ventricular esquerda de 25 ± 8.0%, e BNP de 1057 ± 1024,21 pg/mL. Individualmente, todos os parâmetros clínicos, RT e BNP apresentaram fraco desempenho para predizer PAE ≥ 15 mmHg. O escore clínico de congestão teve o pior desempenho [área sob a curva receiver operating characteristic (AUC) 0,53], seguindo-se escore clínico + RT (AUC 0,60), escore clínico + RT + BNP > 400 pg/mL (AUC 0,62) e escore clínico + RT + BNP > 1000 pg/mL (AUC 0,66).
Conclusão:
Exame físico, RT e BNP tiveram desempenho fraco para predizer PAE ≥15 mmHg. O uso desses parâmetros isoladamente ou em combinação pode levar a estimativa imprecisa do perfil hemodinâmico. (Arq Bras Cardiol. 2018; 110(3):270-277)
Palavras-chave:
Insuficiência Cardíaca; Peptídeo Natriurético Encefálico; Hemodinâmica; Função Ventricular Esquerda; Ecocardiografia Doppler
Introduction
Clinical evaluation of patients with acute decompensated heart failure (ADHF) based only on physical examination has proved to be inadequate for both assessment of left ventricular (LV) function (systolic versus diastolic dysfunction)11 Thomas JT, Kelly RF, Thomas SJ, Stamos TD, Albasha K, Parrilo JE, et al. Utility of history, physical examination, electrocardiogram, and chest radiograph for differentiating normal from decreased systolic function in patients with heart failure. Am J Med. 2002; 112(6):437-45. doi: https://doi.org/10.1016/S0002-9343(02)01048-3.
https://doi.org/10.1016/S0002-9343(02)01...
,22 Vinch CS, Aurigemma GP, Hill JC, Gaasch WH, Volturo G, Tighe DA, et al. Usefulness of clinical variables, echocardiography, and levels of brain natriuretic peptide and norepinephrine to distinguish systolic and diastolic causes of acute heart failure. Am J Cardiol. 2003;91(9):1140-3. doi: https://doi.org/10.1016/S0002-9149(03)00170-X.
https://doi.org/10.1016/S0002-9149(03)00...
and estimation of patient’s hemodynamic status.33 Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989;261(6):884-8. doi: 10.1001/jama.1989.03420060100040.
https://doi.org/10.1001/jama.1989.034200...
Precise determination of LV filling pressures is critical to the proper treatment of patients with ADHF, since congestion is the main determinant of symptoms, hospitalization, and prognosis.44 Goldsmith SR, Brandimarte F, Gheorghiade M. Congestion as a therapeutic target in acute heart failure syndromes. Prog Cardiovasc Dis. 2010;52(5):383-92. doi: 10.1016/j.pcad.2009.11.005.
https://doi.org/10.1016/j.pcad.2009.11.0...
5 Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-7. doi: 10.1056/NEJMoa020233.
https://doi.org/10.1056/NEJMoa020233....
6 Logeart D, Thabut G, Jourdain P, Chavelas C, Beyne P, Beauvais F, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43(4):635-41. doi: https://doi.org/10.1016/j.jacc.2003.09.044.
https://doi.org/10.1016/j.jacc.2003.09.0...
-77 Rohde LE, Beck da Silva L, Goldraich L, Grazziotin TC, Palombini DV, Polanczyk CA, et al. Reliability and prognostic value of traditional signs and symptoms in outpatients with congestive heart failure. Can J Cardiol. 2004;20(7):697-702. PMID: 15197422. Additional assessment using both invasive88 Almeida Júnior GL, Esporcatte R, Rangel FO, Rocha RM, Gouvêa e Silva Gde M, Tura BR, et al. [Therapy of advanced heart failure adapted to hemodynamic objectives acquired by invasive hemodynamic monitoring]. Arq Bras Cardiol. 2005;85(4):247-53. doi: htpp://dx.doi.org/10.1590/S0066-782X2005001700004.
htpp://dx.doi.org/10.1590/S0066-782X2005...
and noninvasive tools may be useful, as it adds important information potentially contributing to tailored management.
Echocardiography has proven its usefulness in assessing the hemodynamic status of patients with ADHF, especially after the advent of new techniques, such as tissue Doppler imaging.99 Nagueh SF, Sun H, Kopelen HA, Middleton KJ, Khoury DS. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol. 2001;37(1):278-85. doi: https://doi.org/10.1016/S0735-1097(00)01056-1.
https://doi.org/10.1016/S0735-1097(00)01...
The so-called “hemodynamic echocardiogram” may help physicians to detect congestion.1010 Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures. A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102(15):1788-94. doi: https://doi.org/10.1161/01.CIR.102.15.1788.
https://doi.org/10.1161/01.CIR.102.15.17...
Several studies have shown that echocardiographic-derived hemodynamic parameters correlate significantly with those obtained by right heart catheterization.1111 Dini FL, Traversi E, Franchini M, Micheli G, Cobelli F, Pozzoli M. Contrast-enhanced Doppler hemodynamics for noninvasive assessment of patients with chronic heart failure and left ventricular systolic dysfunction. J Am Soc Echocardiogr. 2003;16(2):124-31. doi: 10.1067/mje.2003.8.
https://doi.org/10.1067/mje.2003.8....
Elevated levels of B-type natriuretic peptide (BNP) reflect increased LV filling pressures, secondary to myocyte stretch, due to volume or pressure overload.1212 Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, Lenert L, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol. 2001;37(2):379-85. doi: https://doi.org/10.1016/S0735-1097(00)01156-6.
https://doi.org/10.1016/S0735-1097(00)01...
,1313 Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998;135(5 Pt 1):825-32. PMID: 9588412. Whether the association of BNP values adds diagnostic accuracy to the standard clinical assessment in estimating patient’s hemodynamic status remains unknown. In this study we tested the hypothesis that BNP values add diagnostic accuracy to physical examination in detecting congestion in patients with ADHF, using echocardiogram-derived hemodynamic assessment as a reference method for comparison.
Methods
Sample studied
A prospective convenience sample of patients admitted to the emergency department or coronary care unit of three hospitals (one university-affiliated and two tertiary hospitals) due to ADHF was studied. The study was conducted according to the Declaration of Helsinki standards for human research. Institutional review boards approved the research protocol, and all participants provided written informed consent before enrollment.
Inclusion criteria
Patients with ADHF due to LV systolic dysfunction, with LV ejection fraction (LVEF) <40% by Simpson's method, New York Heart Association (NYHA) functional class III or IV on admission and sinus rhythm were included within 24 hours of emergency care.
Exclusion criteria
The exclusion criteria were as follows: ADHF due to acute coronary syndrome; echocardiographic window precluding adequate analysis of hemodynamic parameters; primary valve disease; mechanical prosthetic valve; single mitral flow pattern; and presence of cardiac pacing.
Physical examination
The following physical findings were evaluated: jugular venous distension; hepatojugular reflux; hepatomegaly; ascites; lower extremity edema; third heart sound (S3); pulmonary rales; arterial blood pressure; and proportional pulse pressure. Patients were examined in a quiet emergency or critical care room. The jugular venous distension was evaluated with the patient sitting upright and the presence of a visible internal jugular vein above the clavicle was considered elevated. The hepatojugular reflux was tested in patients with no visible jugular vein, applying a firm right abdominal pressure. The liver was examined with the patient in recumbent position. Hepatomegaly was considered when the liver had more than 10cm of length, considering percussion technique initiating on the third intercostal space, along the midclavicular line. Liver palpation was the method of choice to assess the lower margin of the liver if it was palpable in the abdomen.
Patients with chest radiography showing any sign of congestion were considered to be congested. The radiological evaluation was done through the posterior-anterior and left lateral chest radiography. In cases of inability to take chest radiography in posterior-anterior and lateral positions, an anterior-posterior position with the patient sitting in bed was performed. The chest radiography was performed immediately prior to the echocardiogram.
B-type natriuretic peptide assay
Simultaneously to echocardiography, blood sample was drawn for measurement of BNP. Samples were drawn in EDTA tubes and BNP was measured in whole blood, by immunofluorescence technique, using a commercially available kit (Triage ® BNP test of Biosite Inc., San Diego, CA, USA). All measurements were performed within 30 minutes of blood sampling. Patients with levels of BNP > 400 pg/mL were considered congested,1414 Goonewardena SN, Blair JE, Manuchehry A, Brennan JM, Keller M, Reeves R, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients refered for right heart catheterization. J Card Fail. 2010;16(1):69-75. doi: 10.1016/j.cardfail.2009.08.004.
https://doi.org/10.1016/j.cardfail.2009....
and with levels of BNP < 200 pg/mL were considered “dry”.1515 Villacorta H, Duarte A, Duarte NM, Carrano A, Mesquita ET, Dohmann HJ, et al. The role of B-type natriuretic peptide in the diagnosis of congestive heart failure in patients presenting to an emergency department with dyspnea. Arq Bras Cardiol. 2002;79(6):564-8. doi: http://dx.doi.org/10.1590/S0066-782X2002001500002.
http://dx.doi.org/10.1590/S0066-782X2002...
Echocardiogram evaluation
All patients were submitted to a transthoracic echocardiography with tissue Doppler imaging (GE Vivid 7, Wauwatosa, WI, USA) within a maximum of 30 minutes after completion of the physical exam. In each center, only one examiner (the most experienced) performed all echocardiographic evaluations. Echocardiographic measurements were performed in a blinded manner: the examiner was unaware of the physical findings. Images were obtained from patients in the left lateral and recumbent position, and measurements followed the recommendations of the American Society of Echocardiography.1616 Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440-63. doi: https://doi.org/10.1016/j.echo.2005.10.005
https://doi.org/10.1016/j.echo.2005.10.0...
All Doppler profiles were recorded in an apical 4-chamber view.
The estimated left atrial pressure (LAP) was calculated as follows: calculation of the E/E' ratio by measuring the intra-myocardial flow velocity with tissue Doppler. The early diastolic mitral annular velocity (E') was obtained by tissue Doppler in the LV lateral wall and in case of technical impossibility of obtaining the velocity in this wall, as in ischemic involvement, it was measured in the interventricular septum. At least three consecutive cardiac cycles were used and an average was used as the final result. This measurement, when combined with the trans-mitral flow obtained with pulsed Doppler in early diastole (E) results in the relationship E/E'. The LAP was then estimated by the formula: LAP: 1.24 x (E/E’) + 1.9. Indication of increased LV filling pressure was defined as LAP ≥ 15 mm Hg. Although patients with values below 15 mm Hg may have congestion, values ≥ 15 mm Hg have high specificity for increased LV filling pressure. Ejection fraction was evaluated through the Simpson’s method.
Statistical analysis
Descriptive statistics were expressed as frequency (%) for categorical variables. For continuous variables data are presented as means ± standard deviation for normally distributed data or median and interquartile range (IQR) for non-normally distributed data. Measures of diagnostic performance (sensitivity, specificity, accuracy, positive and negative predictive values) were used to evaluate the diagnostic utility of physical exam signs of heart failure and/or BNP in predicting LAP ≥ 15 mm Hg (defined as indication of increased LV filling pressure).
The Spearman test was used to analyze the correlation between non-normal distribution variables. The level of significance was 5%.
To determine the best cut-off value for BNP to estimate elevation in LAP, a receiver operating characteristic (ROC) curve was constructed. A clinical score (CS) was built by giving 1 point to each positive sign of decompensated heart failure (elevated jugular venous distension, hepatojugular reflux, hepatomegaly, pulmonary rales or edema). Patients with ≥ 2 points were considered with a positive CS, according to analysis of ROC curve. To evaluate the capacity of physical exam and noninvasive diagnostic tests for the prediction of elevated LAP (LAP ≥ 15 mm Hg), separate models were built using combination of CS, CS + chest radiography, CS + chest radiography + BNP > 400 pg/mL, and finally CS + chest radiography + BNP > 1000 pg/mL (based on optimal cut-off point of BNP). Each of these diagnostic tests was dichotomized and compared to determine the incremental predictive value. Statistical analyses were performed using SPSSÒ (SPSS Inc, Chicago, IL, USA).
Results
Patients characteristics
Forty-three patients were included in the study. Patients were predominantly male (75%), elderly (69.9 ± 11.1 years) and had ADHF of ischemic etiology (65%). The mean serum creatinine was 1.3 ± 0.4 mg/dL, and the mean BNP was 1057 pg/mL ± 1024 pg/mL. Table 1 shows clinical and demographic characteristics of patients. All patients were in NYHA functional class III (10.7%) or IV (89.3%), with a mean LVEF of 25% ± 8.0%.
Nine patients had LAP < 15 mm Hg as assessed by echocardiogram. The most frequent sign of decompensation was the presence of rales (27 patients), followed by S3 (19 patients), edema, hepatomegaly and hepatojugular reflux (12 patients each). Prevalence of all clinical signs is show in Table 2.
Accuracy of clinical signs to predict increased LV filling pressures
Elevated jugular venous pressure was the most specific (88%) clinical sign to predict LAP ≥ 15 mm Hg, and rales were the least specific (33%). Accuracy of each sign to predict LAP ≥ 15 mm Hg is shown in Table 3. Combining any two signs of congestion has the best accuracy to predict elevation in LAP, according to the ROC curve.
Accuracy of chest radiography and BNP to predict increased LV filling pressures
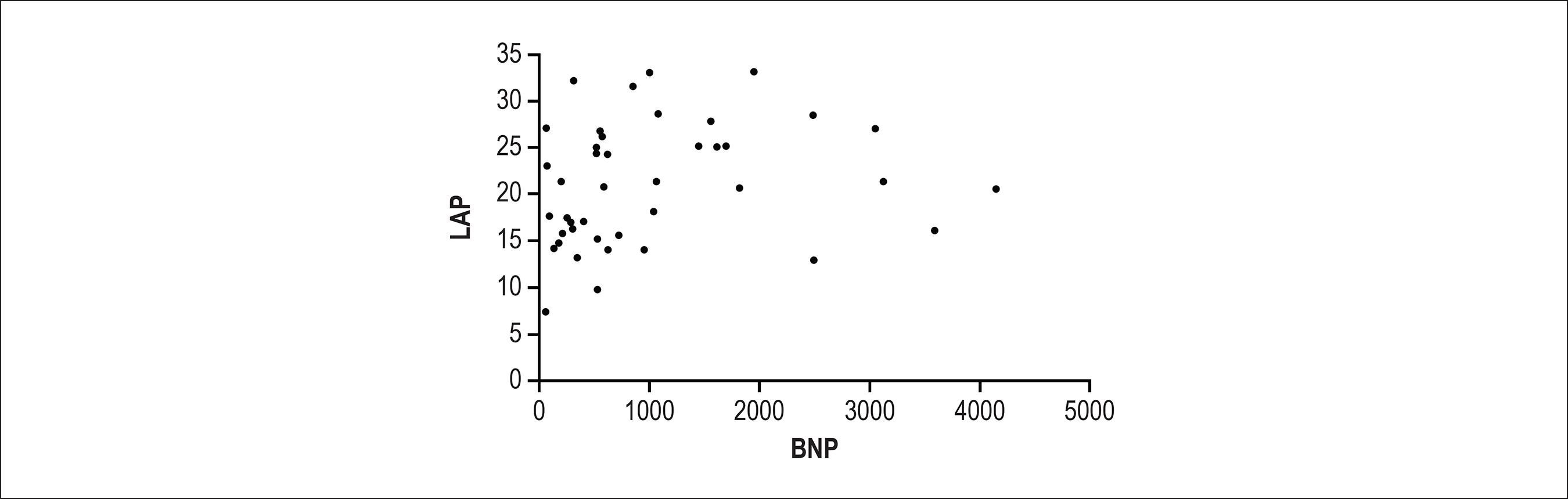
Levels of BNP > 400 pg/mL had a suboptimal diagnostic capability to estimate congestion. Figure 1 illustrates the poor correlation between BNP and echocardiographically assessed LAP.
Correlation between left atrial pressure (LAP) and B-type natriuretic peptide (BNP). r = 0.3 (p = 0.046).
In fact, chest radiography showed a slightly better accuracy than BNP levels to predict congestion. Table 4 shows the performance of these variables to predict LAP ≥ 15 mm Hg. We constructed a ROC curve to estimate the best cut-off point of BNP to predict elevation of LA filling pressure. Levels of BNP > 1000 pg/mL showed a specificity of 88% and a positive predictive value of 93% to predict congestion, but this cut-off loses sensitivity (44% vs 73%) and accuracy (53% vs 67%) when compared with a value > 400 pg/mL (Table 4).
Diagnostic characteristics of the B-type natriuretic peptide (BNP) and chest radiography to predict left atrial pressure ≥ 15 mm Hg
Combinations of clinical signs, chest radiography and BNP to predict increased LV filling pressures
Table 5 depicts the diagnostic characteristics of the CS alone, CS plus chest radiography and these two plus BNP > 400 pg/mL to predict LAP ≥15 mm Hg. Incremental accuracy was observed when progressively combining these parameters. The three parameters combined achieved a sensitivity of 91% and a positive predictive value of 81% to detect a LAP ≥ 15 mm Hg.
Diagnostic characteristics of clinical score, chest radiograph (CR), B-type natriuretic peptide (BNP) and all combined to predict left atrial pressure ≥ 15 mm Hg
Diagnostic performances of combined clinical tools
Accuracy of CS and its combinations with chest radiography and BNP with cut-off values of 400 pg/mL or 1000 pg/mL are illustrated in Figure 2. Combinations of CS with chest radiography (AUC 0.60) and BNP > 400 pg/mL (AUC 0.62) did not improve the ability to discriminate between low or high LAP. Combination with levels of BNP > 1000 pg/mL improved only modestly (AUC 0.66).
Receiver operator characteristics curves for estimating left atrial pressure ≥ 15 mm Hg. Estimates were based on dichotomized variables. CS: clinical score; CR: chest radiography; BNP: B-type natriuretic peptide.
Discussion
In this study, we have assessed the diagnostic accuracy of heart failure clinical signs to predict elevation of cardiac filling pressures as derived from echocardiogram-based parameters. Additionally, we have combined information from clinical signs and chest radiography regarding congestion and finally added the BNP value in order to augment the diagnostic accuracy in assessing congestion. This strategy reflects a “real world” practice to clinically evaluate the hemodynamics of ADHF patients, and we compared this clinical approach with objective measurements of hemodynamics derived from tissue Doppler echocardiogram. We have shown that a CS of congestion, chest radiography and BNP, alone or in combination do not accurately predict elevation of LAP.
Clinical findings in ADHF
Jugular venous pressure
The jugular venous pressure is the most important and probably the only physical examination sign that is relatively accurate in estimating ventricular filling pressures.1717 Butman SM, Ewy GA, Standen JR, Kern KB, Hahn E. Bedside cardiovascular examination in patients with severe chronic heart failure: importance of rest or inducible jugular venous distension. J Am Coll Cardiol. 1993;22(4):968-74. https://doi.org/10.1016/0735-1097(93)90405-P.
https://doi.org/10.1016/0735-1097(93)904...
In a study with 35 patients in a critical care unit, the jugular venous pressure was accurate in estimating low or high filling pressures.1818 Vinayak AG, Levitt J, Gehlbach B, Pohlman AS, Hall JB, Kress JP. Usefulness of the External Jugular Vein Examination in Detecting Abnormal Central Venous Pressure in Critically Ill Patients. Arch Intern Med. 2006;166(19):2132-37. doi: 10.1001/archinte.166.19.2132.
https://doi.org/10.1001/archinte.166.19....
In another study, after evaluating a thousand patients referred for cardiac transplantation, the authors observed that estimated right atrial pressure below or above 10 was concordant with a pulmonary capillary wedge pressure (PCWP) below or above 22 mm Hg in 79% of patients.1919 Drazner MH, Hamilton MA, Fonarow G, Creaser J, Flavell C, Stevenson LW. Relationship between right and left-sided filling pressures in 1000 patients with advanced heart failure. J Heart Lung Transplant. 1999;18(11):1126-32. doi: https://doi.org/10.1016/S1053-2498(99)00070-4.
https://doi.org/10.1016/S1053-2498(99)00...
Other studies also have shown prognostic information about elevated jugular venous pressure in patients with heart failure. Its presence was associated with adverse outcome, including progression of heart failure, even after adjustment for other prognostic factors.2020 Drazner MH, Rame JE, Stevenson LW, Dries DL. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001;345(8):574-81. doi: 10.1056/NEJMoa010641.
https://doi.org/10.1056/NEJMoa010641....
But several factors limit its power in predicting filling pressures. There is not a universal method to estimate the jugular venous pressure. Controversy exists regarding the position (sitting upright or semirecumbent position of 30-45º), the jugular vein being used (internal x external), and the technique of measurement (vertically above clavicle, Louis angle or estimated right atrium position).2121 Leier CV, Chatterjee K. The physical examination in heart failure - part I. Congest Heart Fail. 2007;13(1):41-7. doi: 10.1111/j.1527-5299.2007.06409.x.
https://doi.org/10.1111/j.1527-5299.2007...
,2222 Leier CV, Young JB, Levine TB, Pina I, Armstrong PW, Fowler MB, et al. Nuggets, pearls, and vignettes of master heart failure clinicians. Part 2-the physical examination. Congest Heart Fail. 2001;7(6):297-308. doi: 10.1111/j.1527-5299.2001.01167.x.
https://doi.org/10.1111/j.1527-5299.2001...
In patients with heart failure with preserved systolic function, the jugular vein pressure is far less studied.2323 Drazner MH, Prasad A, Ayers C, Markham DW, Hastings J, Bhella PS, et al. The relationship of right- and left-sided filling pressures in patients with heart failure and a preserved ejection fraction. Circ Heart Fail. 2010;3(2):202-6. doi: 10.1161/CIRCHEARTFAILURE.108.876649. Erratum in: Circ Heart Fail. 2012;5(1):e17.
https://doi.org/10.1161/CIRCHEARTFAILURE...
,2424 Leier CV. Examining the jugular vein is never in vain. Circ Heart Fail. 2010;3(2):175-7. doi: 10.1161/CIRCHEARTFAILURE.110.944116.
https://doi.org/10.1161/CIRCHEARTFAILURE...
In accordance with these observations, we have also found that elevated jugular venous pressure had the best specificity (88%) of all physical findings for elevated LAP. Additionally, in patients with no elevated jugular venous pressure, but with a positive hepatojugular reflux, we were able to identify an elevated LAP in 10 out of 12 patients. However, as expected, the absence of elevated jugular venous pressure was not able to exclude elevated LAP.
Third heart sound
Collins et al.2525 Collins SP, Peacock WF, Lindsell CJ, Clopton P, Diercks DB, Hiestand B, et al. S3 detection as a diagnostic and prognostic aid in emergency department patients with acute dyspnea. Ann Emerg Med. 2009;53(6):748-57. doi: 10.1016/j.annemergmed.2008.12.029.
https://doi.org/10.1016/j.annemergmed.20...
have studied patients with dyspnea in the emergency department and found that S3 did not improve diagnostic accuracy for ADHF, with a sensitivity of only 14.6%. Moreover, in that study, a low diagnostic accuracy (58%) for the diagnosis of ADHF when utilizing all signs together was observed. In our study, S3 was present in less than half of patients and, when present, showed a positive predictive value of 79% for LAP > 15 mm Hg. When absent, an elevation of filling pressures could not be ruled out. In addition, S3 did not add any information regarding hemodynamic status. This is in accordance with other studies.33 Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989;261(6):884-8. doi: 10.1001/jama.1989.03420060100040.
https://doi.org/10.1001/jama.1989.034200...
,2626 Marcus GM, Gerber IL, McKeown BH, Vessey JC, Jordan MV, Huddleston M, et al. Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. JAMA. 2005;293(18):2238-44. doi:10.1001/jama.293.18.2238.
https://doi.org/10.1001/jama.293.18.2238...
Of note, in our study, all physical examinations were done by a heart failure specialist. In the setting of a less experienced professional, the accuracy of physical exam (particularly S3) can be low, since studies suggest poor agreement between medical interns or residents and phonocardiographic findings.2727 Marcus G, Vessey J, Jordan MV, Huddleston M, McCkeown B, Gerber IL, et al. Relationship between accurate auscultation of a clinically useful third heart sound and level of experience. Arch Intern Med. 2006;166(6):617-22. doi: 10.1001/archinte.166.6.617.
https://doi.org/10.1001/archinte.166.6.6...
On the other hand, reasonable agreement in S3 detection has been found among professionals of heart failure clinics.2828 Sauer J, Rabelo ER, Castro RA, Goldraich L, Rohde LE, Clausell N, et al. Nurse’s performance in classifying heart failure patients based on physical exam: comparison with cardiologist’s physical exam and levels of n-terminal pro-B-type natriuretic peptide. J Clin Nurs. 2010;19(23-24):3381-9. doi: 10.1111/j.1365-2702.2010.03403.x.
https://doi.org/10.1111/j.1365-2702.2010...
Levels of BNP
The strongest evidence for clinical use of BNP is to discriminate the cause of dyspnea in patients admitted in the emergency department2929 Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-7. doi: 10.1056/NEJMoa020233.
https://doi.org/10.1056/NEJMoa020233....
and to assess prognosis.3030 Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M; ADHERE Scientific Advisory Committee and Investigators. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;49(19):1943-50. doi: https://doi.org/10.1016/j.jacc.2007.02.037.
https://doi.org/10.1016/j.jacc.2007.02.0...
,3131 Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, et al; Rapid Emergency Department Heart Failure Outpatient Trial investigators. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44(6):1328-33. doi: https://doi.org/10.1016/j.jacc.2004.06.015.
https://doi.org/10.1016/j.jacc.2004.06.0...
For other BNP purposes, data are less clear. In the Escape Trial,3232 Drazner MH, Hellkamp AS, Leier CV, Shah MR, Miller LW, Russell SD, et al. Value of clinical assessment of hemodynamics in advanced heart failure: the ESCAPE Trial. Circ Heart Fail. 2008;1(3):170-7. doi: 10.1161/CIRCHEARTFAILURE.108.769778.
https://doi.org/10.1161/CIRCHEARTFAILURE...
the ROC curve for the performance of BNP in estimating an elevation in PCWP > 22 mm Hg showed a poor performance (AUC = 0.55). Another study with 40 critically ill patients utilizing invasive hemodynamic monitoring has shown a weak correlation between BNP and PCWP (r = 0.58).3333 Forfia PR, Watkins SP, Rame E, Stewart KJ, Shapiro EP. Relationship between B-type natriuretic peptides and pulmonary capillary wedge pressure in the intensive care unit. J Am Coll Cardiol. 2005;45(10):1667-71. doi: 10.1016/j.jacc.2005.01.046.
https://doi.org/10.1016/j.jacc.2005.01.0...
Our data were consistent with these studies, showing a weak correlation between BNP and LAP (r = 0.29). BNP was also tested for guiding treatment, because, theoretically, lowering BNP is a consequence of lowering filling pressures,3434 Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001;7(1):21-9. doi: 10.1054/jcaf.2001.23355.
https://doi.org/10.1054/jcaf.2001.23355....
but this strategy failed to show clinical benefit.3535 Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, Rickenbacher P, et al; TIME-CHF Investigators. BNP-guided VS symptom guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA. 2009;301(4):383-92. doi: 10.1001/jama.2009.2.
https://doi.org/10.1001/jama.2009.2....
In contrast, in the recent PROTECT trial,3636 Januzzi Jr JL, Rehman SU, Mohammed AA, Bhardwaj A, Barajas L, Barajas J, et al. Use of amino-terminal Pro-B-Type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol. 2011;58(18):1881-9. doi: 10.1016/j.jacc.2011.03.072.
https://doi.org/10.1016/j.jacc.2011.03.0...
a similar strategy of guiding treatment according to amino-terminal-Pro-BNP levels against standard of care resulted in decreased incidence of events, improvement in quality of life and in cardiac remodeling. However, that trial was conducted in an outpatient setting, involving very few heart failure patients in more advanced functional classes.
In the present study, we used a cut-off point of 400 pg/mL for BNP as a marker of congestion, since this value was employed in previous studies.1414 Goonewardena SN, Blair JE, Manuchehry A, Brennan JM, Keller M, Reeves R, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients refered for right heart catheterization. J Card Fail. 2010;16(1):69-75. doi: 10.1016/j.cardfail.2009.08.004.
https://doi.org/10.1016/j.cardfail.2009....
,3535 Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, Rickenbacher P, et al; TIME-CHF Investigators. BNP-guided VS symptom guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA. 2009;301(4):383-92. doi: 10.1001/jama.2009.2.
https://doi.org/10.1001/jama.2009.2....
We have observed that BNP levels > 400 pg/mL had a poor prediction performance to identify elevation in LAP, similar to other physical findings or chest radiography performances when taken individually. No valuable information on filling pressures was observed when BNP levels were below 400 pg/mL. Using the AUC, we found that BNP levels of 1000 pg/mL had the best specificity to predict LAP ≥ 15 mm Hg. Therefore, we have also utilized this cut-off value in our subsequent combined analysis. Patients with moderate or severe renal impairment had higher BNP values, in our study the mean values of urea and creatinine were only slightly elevated and should not have influenced the results.
Although there is a time difference between the change in ventricular filling pressures and the corresponding change in BNP levels, this time lapse does not seem to have clinical significance. The half-life of BNP is short, about 20 minutes, and, in addition, the treatment-induced decrease in pulmonary capillary pressure leads to a rapid reduction in BNP levels (30 to 50 pg/mL/hour).
Combining tools to estimate congestion
In patients with intermediate BNP levels (100-500 pg/mL), adding the information about the presence of S3 increases the positive predictive value from 54% to 80%.3737 Collins SP, Lindsell CJ, Peacock WF, Hedger VD, Askew J, Eckert DC, et al. The combined utility of an S3 heart sound and B-type natriuretic peptide levels in emergency department patients with dyspnea. J Card Fail. 2006;12(4):286-92. doi: 10.1016/j.cardfail.2006.01.012.
https://doi.org/10.1016/j.cardfail.2006....
A recent study with 50 patients utilized a very similar strategy to our study, comparing a CS, BNP and a hand carried ultrasound in estimating elevation of ventricular filling pressures, but the gold standard in that study was right heart catheterization.1414 Goonewardena SN, Blair JE, Manuchehry A, Brennan JM, Keller M, Reeves R, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients refered for right heart catheterization. J Card Fail. 2010;16(1):69-75. doi: 10.1016/j.cardfail.2009.08.004.
https://doi.org/10.1016/j.cardfail.2009....
As in ours, that study used a cut-off value for BNP > 400 pg/mL and for PCWP ≥15 mm Hg as referencing parameters. The clinical symptom score had very little predictive utility for an elevated PCWP. Combining the information of jugular venous pressure, BNP and ultrasound, the best diagnostic characteristics for predicting elevated LV filling pressure was achieved (AUC 0.98). In our study, combining the findings of physical examination with chest radiography and BNP augmented progressively the sensitivity (64%, 82% and 91%, respectively) for detecting an elevated LAP, achieving a positive predictive value of 81%, although with a poor specificity. Still, combining these tools showed a modest power in predicting high filling pressures (AUC: 0.62). Thus, ours and the study by Goonewardena et al.1414 Goonewardena SN, Blair JE, Manuchehry A, Brennan JM, Keller M, Reeves R, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients refered for right heart catheterization. J Card Fail. 2010;16(1):69-75. doi: 10.1016/j.cardfail.2009.08.004.
https://doi.org/10.1016/j.cardfail.2009....
showed that clinical examination and BNP are not fully capable to precisely detect elevated filling pressures, and echocardiographically-derived hemodynamic assessment can reliably be incorporated into clinical practice of ADHF, avoiding the traditional invasive right heart catheterization method. The increasing utilization of hand carried ultrasound can be of great value in this area.
Study limitations
We have used the echocardiogram as the gold-standard method for defining filling pressures instead of right heart catheterization. Nonetheless, hemodynamic echocardiogram-derived parameters are well validated in the medical literature when correlated with invasive measurements.3838 Temporelli PL, Scapellato F, Eleuteri E, Imparato A, Giannuzzi P. Doppler echocardiography in advanced systolic heart failure, a noninvasive alternative to Swan-Ganz catheter. Circ Heart Fail. 2010;3(3):387-94. doi: 10.1161/CIRCHEARTFAILURE.108.809590.
https://doi.org/10.1161/CIRCHEARTFAILURE...
39 Nagueh SF, Bhatt R, Vivo RP, Krim SR, Sarvari SI, Russell K, et al. Echocardiographic evaluation of hemodynamics in patients with decompensated systolic heart failure. Circ Cardiovasc Imaging. 2011;4(3):220-7. doi: 10.1161/CIRCIMAGING.111.963496.
https://doi.org/10.1161/CIRCIMAGING.111....
-4040 Stein JH, Neumann A, Preston LM, Constanzo MR, Parrillo JE, Johnson MR, et al. Echocardiographic for hemodynamic assessment of patients with advanced heart failure and potential heart transplant recipients. J Am Coll Cardiol. 1997;30(7):1765-72. doi: https://doi.org/10.1016/S0735-1097(97)00384-7.
https://doi.org/10.1016/S0735-1097(97)00...
We primarily use the lateral annulus to measure E/e' ratio. Although the most recent recommendations suggest using the mean of the lateral and septal annulus values, this was mainly validated in normal subjects. The most recent 2016 guideline of the American Society of Echocardiography and the European Association of Cardiovascular Imaging recognizes that at times only the lateral e’ or septal e’ velocity is available, and it is clinically valid.
In addition, we did not follow patients during the hospitalization or in the post-discharge period to observe whether the initial hemodynamic profile was compatible with the clinical course.
Conclusions
In this study, we showed that in ADHF patients, clinical assessment alone or in conjunction with chest radiography and BNP may lead to inaccurate estimation of echocardiographically-derived hemodynamic profiling.
-
Sources of FundingThere were no external funding sources for this study.
-
Study AssociationThis article is part of the thesis of Doctoral submitted by Gustavo Luiz Gouvêa de Almeida Junior, from Universidade Federal do Rio Grande do Sul.
-
Ethics approval and consent to participateThis study was approved by the Ethics Committee of the Hospital Pró-Cardíaco under the protocol number 021/10 (CAAE:0021.1.346.001-10). All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013. Informed consent was obtained from all participants included in the study.
References
-
1Thomas JT, Kelly RF, Thomas SJ, Stamos TD, Albasha K, Parrilo JE, et al. Utility of history, physical examination, electrocardiogram, and chest radiograph for differentiating normal from decreased systolic function in patients with heart failure. Am J Med. 2002; 112(6):437-45. doi: https://doi.org/10.1016/S0002-9343(02)01048-3
» https://doi.org/10.1016/S0002-9343(02)01048-3 -
2Vinch CS, Aurigemma GP, Hill JC, Gaasch WH, Volturo G, Tighe DA, et al. Usefulness of clinical variables, echocardiography, and levels of brain natriuretic peptide and norepinephrine to distinguish systolic and diastolic causes of acute heart failure. Am J Cardiol. 2003;91(9):1140-3. doi: https://doi.org/10.1016/S0002-9149(03)00170-X
» https://doi.org/10.1016/S0002-9149(03)00170-X -
3Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989;261(6):884-8. doi: 10.1001/jama.1989.03420060100040.
» https://doi.org/10.1001/jama.1989.03420060100040. -
4Goldsmith SR, Brandimarte F, Gheorghiade M. Congestion as a therapeutic target in acute heart failure syndromes. Prog Cardiovasc Dis. 2010;52(5):383-92. doi: 10.1016/j.pcad.2009.11.005.
» https://doi.org/10.1016/j.pcad.2009.11.005. -
5Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-7. doi: 10.1056/NEJMoa020233.
» https://doi.org/10.1056/NEJMoa020233. -
6Logeart D, Thabut G, Jourdain P, Chavelas C, Beyne P, Beauvais F, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43(4):635-41. doi: https://doi.org/10.1016/j.jacc.2003.09.044.
» https://doi.org/10.1016/j.jacc.2003.09.044. -
7Rohde LE, Beck da Silva L, Goldraich L, Grazziotin TC, Palombini DV, Polanczyk CA, et al. Reliability and prognostic value of traditional signs and symptoms in outpatients with congestive heart failure. Can J Cardiol. 2004;20(7):697-702. PMID: 15197422.
-
8Almeida Júnior GL, Esporcatte R, Rangel FO, Rocha RM, Gouvêa e Silva Gde M, Tura BR, et al. [Therapy of advanced heart failure adapted to hemodynamic objectives acquired by invasive hemodynamic monitoring]. Arq Bras Cardiol. 2005;85(4):247-53. doi: htpp://dx.doi.org/10.1590/S0066-782X2005001700004.
» htpp://dx.doi.org/10.1590/S0066-782X2005001700004. -
9Nagueh SF, Sun H, Kopelen HA, Middleton KJ, Khoury DS. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol. 2001;37(1):278-85. doi: https://doi.org/10.1016/S0735-1097(00)01056-1.
» https://doi.org/10.1016/S0735-1097(00)01056-1. -
10Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures. A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102(15):1788-94. doi: https://doi.org/10.1161/01.CIR.102.15.1788.
» https://doi.org/10.1161/01.CIR.102.15.1788. -
11Dini FL, Traversi E, Franchini M, Micheli G, Cobelli F, Pozzoli M. Contrast-enhanced Doppler hemodynamics for noninvasive assessment of patients with chronic heart failure and left ventricular systolic dysfunction. J Am Soc Echocardiogr. 2003;16(2):124-31. doi: 10.1067/mje.2003.8.
» https://doi.org/10.1067/mje.2003.8. -
12Dao Q, Krishnaswamy P, Kazanegra R, Harrison A, Amirnovin R, Lenert L, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol. 2001;37(2):379-85. doi: https://doi.org/10.1016/S0735-1097(00)01156-6.
» https://doi.org/10.1016/S0735-1097(00)01156-6. -
13Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998;135(5 Pt 1):825-32. PMID: 9588412.
-
14Goonewardena SN, Blair JE, Manuchehry A, Brennan JM, Keller M, Reeves R, et al. Use of hand carried ultrasound, B-type natriuretic peptide, and clinical assessment in identifying abnormal left ventricular filling pressures in patients refered for right heart catheterization. J Card Fail. 2010;16(1):69-75. doi: 10.1016/j.cardfail.2009.08.004.
» https://doi.org/10.1016/j.cardfail.2009.08.004. -
15Villacorta H, Duarte A, Duarte NM, Carrano A, Mesquita ET, Dohmann HJ, et al. The role of B-type natriuretic peptide in the diagnosis of congestive heart failure in patients presenting to an emergency department with dyspnea. Arq Bras Cardiol. 2002;79(6):564-8. doi: http://dx.doi.org/10.1590/S0066-782X2002001500002.
» http://dx.doi.org/10.1590/S0066-782X2002001500002. -
16Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440-63. doi: https://doi.org/10.1016/j.echo.2005.10.005
» https://doi.org/10.1016/j.echo.2005.10.005 -
17Butman SM, Ewy GA, Standen JR, Kern KB, Hahn E. Bedside cardiovascular examination in patients with severe chronic heart failure: importance of rest or inducible jugular venous distension. J Am Coll Cardiol. 1993;22(4):968-74. https://doi.org/10.1016/0735-1097(93)90405-P
» https://doi.org/10.1016/0735-1097(93)90405-P -
18Vinayak AG, Levitt J, Gehlbach B, Pohlman AS, Hall JB, Kress JP. Usefulness of the External Jugular Vein Examination in Detecting Abnormal Central Venous Pressure in Critically Ill Patients. Arch Intern Med. 2006;166(19):2132-37. doi: 10.1001/archinte.166.19.2132.
» https://doi.org/10.1001/archinte.166.19.2132. -
19Drazner MH, Hamilton MA, Fonarow G, Creaser J, Flavell C, Stevenson LW. Relationship between right and left-sided filling pressures in 1000 patients with advanced heart failure. J Heart Lung Transplant. 1999;18(11):1126-32. doi: https://doi.org/10.1016/S1053-2498(99)00070-4.
» https://doi.org/10.1016/S1053-2498(99)00070-4. -
20Drazner MH, Rame JE, Stevenson LW, Dries DL. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001;345(8):574-81. doi: 10.1056/NEJMoa010641.
» https://doi.org/10.1056/NEJMoa010641. -
21Leier CV, Chatterjee K. The physical examination in heart failure - part I. Congest Heart Fail. 2007;13(1):41-7. doi: 10.1111/j.1527-5299.2007.06409.x.
» https://doi.org/10.1111/j.1527-5299.2007.06409.x. -
22Leier CV, Young JB, Levine TB, Pina I, Armstrong PW, Fowler MB, et al. Nuggets, pearls, and vignettes of master heart failure clinicians. Part 2-the physical examination. Congest Heart Fail. 2001;7(6):297-308. doi: 10.1111/j.1527-5299.2001.01167.x.
» https://doi.org/10.1111/j.1527-5299.2001.01167.x. -
23Drazner MH, Prasad A, Ayers C, Markham DW, Hastings J, Bhella PS, et al. The relationship of right- and left-sided filling pressures in patients with heart failure and a preserved ejection fraction. Circ Heart Fail. 2010;3(2):202-6. doi: 10.1161/CIRCHEARTFAILURE.108.876649. Erratum in: Circ Heart Fail. 2012;5(1):e17.
» https://doi.org/10.1161/CIRCHEARTFAILURE.108.876649 -
24Leier CV. Examining the jugular vein is never in vain. Circ Heart Fail. 2010;3(2):175-7. doi: 10.1161/CIRCHEARTFAILURE.110.944116.
» https://doi.org/10.1161/CIRCHEARTFAILURE.110.944116. -
25Collins SP, Peacock WF, Lindsell CJ, Clopton P, Diercks DB, Hiestand B, et al. S3 detection as a diagnostic and prognostic aid in emergency department patients with acute dyspnea. Ann Emerg Med. 2009;53(6):748-57. doi: 10.1016/j.annemergmed.2008.12.029.
» https://doi.org/10.1016/j.annemergmed.2008.12.029. -
26Marcus GM, Gerber IL, McKeown BH, Vessey JC, Jordan MV, Huddleston M, et al. Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. JAMA. 2005;293(18):2238-44. doi:10.1001/jama.293.18.2238.
» https://doi.org/10.1001/jama.293.18.2238 -
27Marcus G, Vessey J, Jordan MV, Huddleston M, McCkeown B, Gerber IL, et al. Relationship between accurate auscultation of a clinically useful third heart sound and level of experience. Arch Intern Med. 2006;166(6):617-22. doi: 10.1001/archinte.166.6.617.
» https://doi.org/10.1001/archinte.166.6.617. -
28Sauer J, Rabelo ER, Castro RA, Goldraich L, Rohde LE, Clausell N, et al. Nurse’s performance in classifying heart failure patients based on physical exam: comparison with cardiologist’s physical exam and levels of n-terminal pro-B-type natriuretic peptide. J Clin Nurs. 2010;19(23-24):3381-9. doi: 10.1111/j.1365-2702.2010.03403.x.
» https://doi.org/10.1111/j.1365-2702.2010.03403.x. -
29Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al; Breathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-7. doi: 10.1056/NEJMoa020233.
» https://doi.org/10.1056/NEJMoa020233. -
30Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M; ADHERE Scientific Advisory Committee and Investigators. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;49(19):1943-50. doi: https://doi.org/10.1016/j.jacc.2007.02.037.
» https://doi.org/10.1016/j.jacc.2007.02.037. -
31Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, et al; Rapid Emergency Department Heart Failure Outpatient Trial investigators. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44(6):1328-33. doi: https://doi.org/10.1016/j.jacc.2004.06.015.
» https://doi.org/10.1016/j.jacc.2004.06.015. -
32Drazner MH, Hellkamp AS, Leier CV, Shah MR, Miller LW, Russell SD, et al. Value of clinical assessment of hemodynamics in advanced heart failure: the ESCAPE Trial. Circ Heart Fail. 2008;1(3):170-7. doi: 10.1161/CIRCHEARTFAILURE.108.769778.
» https://doi.org/10.1161/CIRCHEARTFAILURE.108.769778. -
33Forfia PR, Watkins SP, Rame E, Stewart KJ, Shapiro EP. Relationship between B-type natriuretic peptides and pulmonary capillary wedge pressure in the intensive care unit. J Am Coll Cardiol. 2005;45(10):1667-71. doi: 10.1016/j.jacc.2005.01.046.
» https://doi.org/10.1016/j.jacc.2005.01.046. -
34Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001;7(1):21-9. doi: 10.1054/jcaf.2001.23355.
» https://doi.org/10.1054/jcaf.2001.23355. -
35Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, Rickenbacher P, et al; TIME-CHF Investigators. BNP-guided VS symptom guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA. 2009;301(4):383-92. doi: 10.1001/jama.2009.2.
» https://doi.org/10.1001/jama.2009.2. -
36Januzzi Jr JL, Rehman SU, Mohammed AA, Bhardwaj A, Barajas L, Barajas J, et al. Use of amino-terminal Pro-B-Type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. J Am Coll Cardiol. 2011;58(18):1881-9. doi: 10.1016/j.jacc.2011.03.072.
» https://doi.org/10.1016/j.jacc.2011.03.072. -
37Collins SP, Lindsell CJ, Peacock WF, Hedger VD, Askew J, Eckert DC, et al. The combined utility of an S3 heart sound and B-type natriuretic peptide levels in emergency department patients with dyspnea. J Card Fail. 2006;12(4):286-92. doi: 10.1016/j.cardfail.2006.01.012.
» https://doi.org/10.1016/j.cardfail.2006.01.012. -
38Temporelli PL, Scapellato F, Eleuteri E, Imparato A, Giannuzzi P. Doppler echocardiography in advanced systolic heart failure, a noninvasive alternative to Swan-Ganz catheter. Circ Heart Fail. 2010;3(3):387-94. doi: 10.1161/CIRCHEARTFAILURE.108.809590.
» https://doi.org/10.1161/CIRCHEARTFAILURE.108.809590. -
39Nagueh SF, Bhatt R, Vivo RP, Krim SR, Sarvari SI, Russell K, et al. Echocardiographic evaluation of hemodynamics in patients with decompensated systolic heart failure. Circ Cardiovasc Imaging. 2011;4(3):220-7. doi: 10.1161/CIRCIMAGING.111.963496.
» https://doi.org/10.1161/CIRCIMAGING.111.963496. -
40Stein JH, Neumann A, Preston LM, Constanzo MR, Parrillo JE, Johnson MR, et al. Echocardiographic for hemodynamic assessment of patients with advanced heart failure and potential heart transplant recipients. J Am Coll Cardiol. 1997;30(7):1765-72. doi: https://doi.org/10.1016/S0735-1097(97)00384-7.
» https://doi.org/10.1016/S0735-1097(97)00384-7.
Publication Dates
-
Publication in this collection
Mar 2018
History
-
Received
07 Aug 2017 -
Reviewed
09 Oct 2017 -
Accepted
18 Oct 2017