Development: Department of Hypertension (DH) of the Brazilian Society of Cardiology
Norms and Guidelines Council (2020-2021): Brivaldo Markman Filho, Antonio Carlos Sobral Sousa, Aurora Felice Castro Issa, Bruno Ramos Nascimento, Harry Correa Filho, Marcelo Luiz Campos Vieira
Norms and Guidelines Coordinator (2020-2021): Brivaldo Markman Filho
Content
1. Definition and Epidemiology 580
1.1. Definition/New Concepts 580
1.2. Control of Hypertension in Brazil and Worldwide 580
1.3. Incidence and Prevalence of Resistant Hypertension 580
1.4. Factors Related to Resistant Hypertension 580
2. Prognostic Aspects 581
2.1. Introduction 581
2.2. Office Blood Pressure and Ambulatory Blood Pressure Monitoring 581
2.3. Target-Organ Damage 581
2.3.1. Central Arterial Pressure and Arterial Stiffening 581
2.3.2. Left Ventricular Hypertrophy 581
2.3.3. Albuminuria 581
2.3.4. Inflammatory Biomarkers 581
3. Flowchart of Assessment of Resistant Hypertension 581
3.1. Flowchart of the Diagnostic Approach in Resistant Hypertension 581
4. Blood Pressure Measurement 582
4.1. Office Blood Pressure in Resistant Hypertension 582
4.2. Ambulatory Blood Pressure Monitoring in Resistant Hypertension 582
4.3. Home Blood Pressure Monitoring and Blood Pressure Self-Measurement 583
4.4. Measurement of Central Arterial Pressure 583
5. Target-Organ Damage 583
5.1. Introduction 583
5.2. Vascular Changes 583
5.3. Cerebral Changes 583
5.4. Cardiac Changes 583
5.5. Renal Changes 584
6. Phenotype of the Patient with Resistant Hypertension 584
6.1. Introduction 584
6.2. Phenotype of the Patient with Resistant Hypertension 584
6.3. Phenotype of Controlled and Uncontrolled Resistant Hypertension 585
6.3.1. Pathophysiological Aspects 585
6.3.2. Clinical Differences 585
6.3.3. Prognosis 585
6.4. Phenotype of the Patient with Refractory Hypertension 586
7. Secondary Causes of Resistant Hypertension 586
7.1. Introduction 586
7.2. Secondary Hypertension due to Non-Endocrine Causes 586
7.2.1. Obstructive Sleep Apnea 586
7.2.2. Renal Parenchymal Disease 586
7.2.3. Renal Artery Stenosis 586
7.3. Secondary Hypertension due to Endocrine Causes 586
7.3.1. Primary Hyperaldosteronism 586
7.3.2. Pheochromocytoma 587
7.3.3. Hypothyroidism and Hyperthyroidism 587
8. Non-Pharmacological Treatment 587
8.1. Weight Loss 587
8.2. Salt Restriction 588
8.3. Alcohol Intake 588
8.4. Physical Activity 589
9. Pharmacological Treatment of Resistant Hypertension 589
10. New Treatments of Resistant Hypertension 589
10.1. Introduction 589
10.2. Direct Carotid Sinus Stimulation 589
10.3. Renal Sympathetic Denervation 590
10.4. Use of Continuous Positive Airway Pressure 590
10.5. Arteriovenous Fistula 591
References 591
1. Definition and Epidemiology
Coordinator: Heitor Moreno Júnior.
Authors: Juan Carlos Yugar-Toledo, Heitor Moreno Júnior, Miguel Gus, Guido Bernardo Aranha Rosito, and Luiz César Nazário Scala.
1.1. Definition/New Concepts
Resistant hypertension (RHTN) is defined as blood pressure (BP) persistently above the recommended target values despite the use of three antihypertensive agents of different classes, including one blocker of the renin-angiotensin system (angiotensin-converting enzyme inhibitor [ACEI] or angiotensin receptor blocker [ARB]), one long-acting calcium channel blocker (CCB), and one long-acting thiazide diuretic (TZD) at maximum recommended and tolerated doses, administered with appropriate frequency and doses and with proven adherence.
Other drugs may be added if the above ones fail (aldosterone antagonists, beta-blockers, and α-methyldopa). Experts disagree on issues related to dose/potency, although the main discussion occurs around the use of chlorthalidone or hydrochlorothiazide as the main TZD.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.
The definition above includes a subgroup of patients with RHTN whose BP is controlled with four or more antihypertensive medications, known as controlled RHTN (C-RHTN).22. Modolo R, de Faria AP, Almeida A, Moreno H. Resistant or refractory hypertension: are they different? Curr Hypertens Rep. 2014;16(10):485.,33. Modolo R, de Faria AP, Sabbatini AR, Moreno H. Resistant hypertension revisited: definition and true prevalence. J Hypertens. 2014;32(7):1546. A proposal to classify the disease into C-RHTN and uncontrolled RHTN (UC-RHTN),44. Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, et al. Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens. 2011;25(9):532-8. including refractory RHTN (Ref-RHTN), an extreme UC-RHTN phenotype involving use of five or more antihypertensive agents,55. Dudenbostel T, Siddiqui M, Oparil S, Calhoun DA. Refractory Hypertension: A Novel Phenotype of Antihypertensive Treatment Failure. Hypertension. 2016;67(6):1085-92. has gained space in the literature.66. Moreno H, Jr, Coca A. Resistant and refractory hypertension: reflections on pathophysiology and terminology. Blood Press. 2012;21(4):209-10.,77. Yugar-Toledo JC, Brunelli V, Vilela-Martin JF, Fattori A, Moreno H. Controlled Versus Uncontrolled Resistant Hypertension: Are They in the Same Bag? Curr Hypertens Rep. 2018;20(3):1-6.
Thus, UC-RHTN is defined by BP levels that remain above the desired level (140/90 mmHg) despite the concomitant use of four or more antihypertensive agents of different classes and a fourth drug, which is generally a mineralocorticoid receptor antagonist or a central sympathetic inhibitor (Chart 1).
1.2. Control of Hypertension in Brazil and Worldwide
An analysis of 135 population studies with 1 million individuals indicated that 31.1% of the adult population is hypertensive (95% CI; 30 to 32%), with an estimated rate of 28.5 and 31.5% in countries with the highest and lowest socioeconomic status, respectively. BP control varies according to socioeconomic status, reaching 28.4% in more developed countries and only 7.7% in those with a lower degree of development.88. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441-50. In Brazil, the control rate varied from 10.4 to 35.2% in populations studied in three regions of the country.99. Scala LC, Magalhães LB, Machado A. Epidemiologia da hipertensão arterial sistêmica. In: Sociedade Brasileira de Cardiologia. Livro texto da SBC. 2a ed. São Paulo:Manole;2015. São Paulo; 2015. p. 780-5.
A study conducted in 291 centers in all five Brazilian regions including 2,810 patients evaluated the control rates of hypertension according to risk profile and target BP. For patients with lower risk and target levels < 140/90 mmHg, the control rate was 61.7%, while for those with high risk and target levels < 130/80 mmHg, the corresponding value was 41.8%.1010. Nobre F, Ribeiro AB, Mion D Jr. [Control of arterial pressure in patients undergoing anti-hypertensive treatment in Brazil: Controlar Brazil]. Arq Bras Cardiol. 2010;94(5):663-70.
1.3. Incidence and Prevalence of Resistant Hypertension
The prevalence of RHTN among individuals with hypertension is estimated at 10 to 20% worldwide, resulting in approximately 200 million individuals with RHTN.1111. Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28(3):355-61. This variability is mainly due to differences in RHTN criteria and characteristics of the studied populations.
The National Health and Nutrition Examination Survey (NHANES) reported a prevalence of RHTN of about 9% in individuals with hypertension, corresponding to 12.8% of the individuals using antihypertensive agents in the US.1212. Bangalore S, Davis BR, Cushman WC, Pressel SL, Muntner PM, Calhoun DA, et al. Treatment-Resistant Hypertension and Outcomes Based on Randomized Treatment Group in ALLHAT. Am J Med. 2017;130(4):439-48 e9.
Still, the actual prevalence of RHTN is unknown. A meta-analysis by Achelrod et al.1111. Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28(3):355-61. evaluating populations of individuals with treated hypertension found a prevalence of 13.72% (95% CI; 11.19 to 16.24%), according to 20 observational studies, and 16.32% (95% CI; 10.68 to 21.95%), according to four randomized controlled trials.1111. Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28(3):355-61. In Brazil, a multicenter study (ReHOT) including ambulatory BP monitoring (ABPM) showed a prevalence of RHTN of 11.7%.1313. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.
Daugherty et al.1414. Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125(13):1635-42. analyzed the incidence of RHTN in 205,750 patients with hypertension who initiated antihypertensive treatment between 2002 and 2006. The authors found a rate of 1.9% at 1.5 years of follow-up (0.7 per 100 patients per year), leading to a 1.47 higher cardiovascular (CV) risk at 3.8 years.1414. Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125(13):1635-42.
1.4. Factors Related to Resistant Hypertension
RHTN is more prevalent in elderly, obese, and African descent individuals, as well as in patients with left ventricular hypertrophy (LVH), diabetes mellitus, chronic nephropathy, metabolic syndrome, increased alcohol and/or salt intake, and sedentary lifestyle.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.,1515. Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52(22):1749-57.
16. Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88(10):1099-107.-1717. Cai A, Calhoun DA. Resistant Hypertension: An Update of Experimental and Clinical Findings. Hypertension. 2017;70(1):5-9. Aspects related to RHTN include the following: 1) diagnostic factors – inadequate BP measurement technique, white-coat effect;11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.,1515. Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52(22):1749-57. 2) causal factors – increased salt sensitivity, volume expansion due to excessive salt intake or chronic kidney disease (CKD), use of nonsteroidal antiinflammatory drugs, anabolic steroids, oral contraceptives, sympathomimetic agents (nasal decongestants, appetite suppressants, cocaine), chemotherapeutic agents, antidepressants, erythropoietin, immunosuppressants, alcohol;11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.,1515. Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52(22):1749-57. 3) secondary causes of hypertension, including primary hyperaldosteronism, obstructive sleep apnea (OSA), CKD, renal artery stenosis, thyroid diseases;1515. Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52(22):1749-57. 4) therapeutic factors – medications that are either inappropriate or are used in insufficient doses, medical inertia, low adherence.1616. Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88(10):1099-107.,1717. Cai A, Calhoun DA. Resistant Hypertension: An Update of Experimental and Clinical Findings. Hypertension. 2017;70(1):5-9. Both systolic and diastolic hypertension may be resistant, the former being more prevalent.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.
2. Prognostic Aspects
Coordinator: Elizabeth Silaid Muxfeldt.
Authors: Alexandre Alessi, Andrea Araújo Brandão, Osni Moreira Filho, and Elizabeth Silaid Muxfeldt.
2.1. Introduction
RHTN is associated with high CV morbidity and mortality, increasing the risk of CV events by 47% in patients affected by this condition when compared with individuals with incident hypertension.1414. Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125(13):1635-42.
2.2. Office Blood Pressure and Ambulatory Blood Pressure Monitoring
True RHTN, diagnosed by ABPM, is associated with twice the CV risk compared with RHTN due to a white-coat effect.1818. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78. Overall, the average BP measurements obtained in all three ABPM periods are strong predictors of CV risk, while office BP has shown no prognostic value.1818. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.,1919. Salles GF, Cardoso CR, Muxfeldt ES. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med. 2008;168(21):2340-6. Longitudinal studies have highlighted high BP during sleep and the absence of nocturnal dipping as important predictors of CV risk.1818. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.
19. Salles GF, Cardoso CR, Muxfeldt ES. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med. 2008;168(21):2340-6.-2020. Muxfeldt ES, Cardoso CR, Salles GF. Prognostic value of nocturnal blood pressure reduction in resistant hypertension. Arch Intern Med. 2009;169(9):874-80. Prognostic importance of the nighttime BP pattern has also been shown in meta-analyses.2121. Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32(12):2332-40; discussion 40.
2.3. Target-Organ Damage
2.3.1. Central Arterial Pressure and Arterial Stiffening
Pulse wave velocity (PWV) has an independent predictive value in several subgroups of patients with hypertension.2222. Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236-41. Reduced arterial relaxation and elasticity have been observed in patients with RHTN compared with individuals with well-controlled hypertension, being a marker of prognosis and response to antihypertensive therapy.2323. Chung CM, Cheng HW, Chang JJ, Lin YS, Hsiao JF, Chang ST, et al. Relationship between resistant hypertension and arterial stiffness assessed by brachial-ankle pulse wave velocity in the older patient. Clin Interv Aging. 2014 Sep 5;9:1495-502. In hypertensive patients, PWV provides additive value when incorporated into CV risk scores.2424. Brandao AA, Amodeo C, Alcantara C, Barbosa E, Nobre F, Pinto F, et al. I Luso-Brazilian Positioning on Central Arterial Pressure. Arq Bras Cardiol. 2017;108(2):100-8.
2.3.2. Left Ventricular Hypertrophy
The electrocardiographic diagnosis of LVH has emerged as a predictor of risk for coronary disease (Cornell index) and cerebrovascular disease (Sokolow-Lyon index), and the regression of both indices reduces the risk of CV events by 35 and 40%, respectively.2525. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic impact of baseline and serial changes in electrocardiographic left ventricular hypertrophy in resistant hypertension. Am Heart J. 2010;159(5):833-40.
2.3.3. Albuminuria
Both baseline and serial changes in albuminuria have prognostic implications in RHTN. In a large prospective cohort of 531 patients with RHTN, the occurrence of moderately increased albuminuria (MIA) at baseline was an independent predictor of composite events and all-cause mortality.2626. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis. 2011;216(1):199-204. A later analysis by the same group, this time including 1,048 patients, showed that MIA increased by 40% the risk of fatal and nonfatal CV events and all-cause mortality.2727. da Costa PM, Cortez AF, de Souza F, Mares GS, Dos Santos BDM, Muxfeldt ES. Prognostic impact of baseline urinary albumin excretion rate in patients with resistant hypertension: a prospective cohort study. J Hum Hypertens. 2018;32(2):139-49.
During follow-up, the persistence of MIA at 2 years was a risk factor for CV events, while persistent normoalbuminuria emerged as a protective factor.2626. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis. 2011;216(1):199-204. Another cohort of 143 patients with RHTN assessed at baseline and after 6 years of follow-up showed that the development or persistence of MIA was associated with an increased risk of CV events. In contrast, the persistence of normoalbuminuria or regression of MIA was associated with a lower risk of major events.2828. Oliveras A, Armario P, Sierra C, Arroyo JA, Hernandez-del-Rey R, Vazquez S, et al. Urinary albumin excretion at follow-up predicts cardiovascular outcomes in subjects with resistant hypertension. Am J Hypertens. 2013;26(9):1148-54.
2.3.4. Inflammatory Biomarkers
Elevated C-reactive protein is an independent predictor of coronary and cerebrovascular disease, and a more important marker in patients with RHTN who are younger, obese, and have uncontrolled ABPM and a non-dipping pattern (absent or attenuated nocturnal decline).2929. Cortez AF, Muxfeldt ES, Cardoso CR, Salles GF. Prognostic Value of C-Reactive Protein in Resistant Hypertension. Am J Hypertens. 2016;29(8):992-1000.
3. Flowchart of Assessment of Resistant Hypertension
Coordinator: Audes Diógenes de Magalhães Feitosa.
Authors: Oswaldo Passarelli Júnior, Dilma do Socorro Moraes de Souza, and Audes Diógenes de Magalhães Feitosa.
3.1. Flowchart of the Diagnostic Approach in Resistant Hypertension
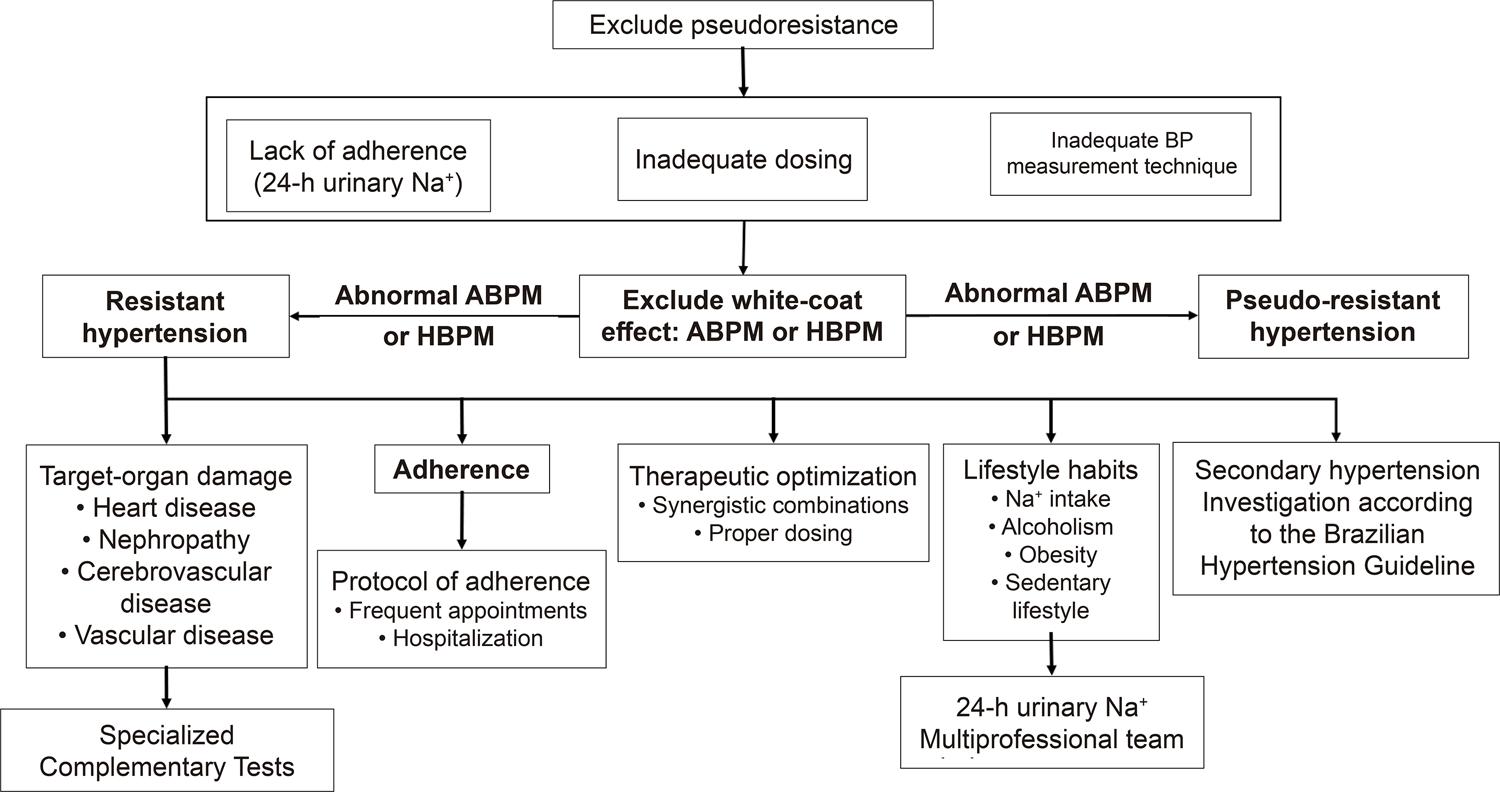
On clinical suspicion of RHTN, diagnostic confirmation is required, and the first step in the investigation is the exclusion of causes of pseudoresistance, such as lack of treatment adherence (pharmacological and non-pharmacological), inadequate dosing, improper BP measurement technique, and white-coat effect11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19. (Figure 1). Lack of BP control should be confirmed by ABPM and home blood pressure monitoring (HBPM).3030. de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57(5):898-902.
31. White WB. Ambulatory blood pressure monitoring as an investigative tool for characterizing resistant hypertension and its rational treatment. J Clin Hypertens (Greenwich). 2007;9(1 Suppl 1):25-30.-3232. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-104.
– Flowchart of the evaluation of resistant hypertension. ABPM: ambulatory blood pressure monitoring; HBPM: home blood pressure monitoring; Na+: sodium; BP: blood pressure.
Once pseudoresistance is excluded, the occurrence of RHTN is confirmed and a diagnostic investigation should be initiated with specific tests, according to recommendations of hypertension guidelines regarding the involvement of target-organ damage (TOD) and secondary hypertension.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,3434. Mancia G, Fagard R. Guidelines for the management of hypertension and target organ damage: reply. J Hypertens. 2013; 31(12):2464-5. The occurrence of associated comorbidities should be evaluated with specialized tests according to clinical suspicion.
Out-of-office BP measurement is fundamental since such readings are usually higher than those measured at home, reflecting the frequent occurrence of the white-coat effect in this population. Treatment adherence is always challenging, especially in public centers.
Patient-related problems that may occur include rejection to the excessive number of medications in complex dosing (excessive doses and tablets), medication side effects, sociocultural issues and lack of knowledge of the natural history of the disease, as well as other problems related to the physician, including poor doctor-patient relationship, non-synergistic dosing or wrong doses and omission or lack of knowledge in the investigation of treatable secondary causes. A potential problem related to health care services is difficulty in access to physicians, medications, and complementary tests.
All these factors hinder the adherence to pharmacological and non-pharmacological treatment and must, therefore, be verified and circumvented.
Salt intake should always be verified, if possible with a 24-hour urinary sodium measurement, as intake is often excessive due to the consumption of processed foods and lack of knowledge by the patients about excessive salt intake.
Treatment should be optimized, preferably with the same physician and for a minimum of 6 months to strengthen the doctor-patient relationship. Added to that are regular recommendations regarding healthy lifestyle habits and continuous verification of treatment adherence, with synergistic dosing schedules and appropriate medication adjustments, respecting the occurrence of comorbidities indicating or contraindicating certain antihypertensive drug classes.
4. Blood Pressure Measurement
Coordinator: Celso Amodeo.
Authors: Weimar Kunz Sebba Barroso, Marco Antônio Mota Gomes, Annelise Machado Gomes de Paiva, and Eduardo Costa Duarte Barbosa.
4.1. Office Blood Pressure in Resistant Hypertension
Although not diagnostic of RHTN, office BP should be verified, and the measurement procedure should follow the guidelines of the 7th Brazilian Guideline of Arterial Hypertension.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6. The BP can be measured with a manual, semiautomatic, or automatic sphygmomanometer. Several measurements are recommended, with the patient sitting in a calm and comfortable environment to improve reproducibility and bring the values obtained in the office close to those obtained on ABPM during daytime.
Consideration must be given to the occurrence of the white-coat effect, a phenomenon involving two situations. The first is a white-coat hypertension, in which BP is elevated in isolated office measurements but normal during ABPM or HBPM. The second is a white-coat effect, which is characterized by increased office BP in relation to the mean BP during daytime in the ABPM or the weekly average HBPM, without changing the diagnosis of hypertension or normotension.3535. Nobre FMJ, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 2018;110(5 Supl.1):1-29.
These two situations can lead to a false diagnosis of RHTN, resulting in unnecessary test requests and medication use. White-coat hypertension may be referred to as a cause of pseudo-resistant hypertension.3636. Silva GV, Mion D. Papel da MAPA e da MRPA na avaliação de pacientes com hipertensão de difícil controle. Rev Bras Hipertens. 2008;15(1):17-20.
4.2. Ambulatory Blood Pressure Monitoring in Resistant Hypertension
This test is necessary to rule out the hypothesis of white-coat hypertension, which falsely suggests RHTN.3737. Muxfeldt ES, Bloch KV, Nogueira AR, Salles GF. Twenty-four hour ambulatory blood pressure monitoring pattern of resistant hypertension. Blood Press Monit. 2003;8(5):181-5. The diagnosis is confirmed when the mean BP during daytime and over 24 hours is below 135/85 mmHg and 130/80 mmHg, respectively. Compared with casual BP measurements, the values obtained are more strongly related to the risks arising from hypertension, especially during ABPM evaluation, when an absence or attenuation of the BP reduction during sleep is identified, along with an increase in the difference between systolic and diastolic BP.3737. Muxfeldt ES, Bloch KV, Nogueira AR, Salles GF. Twenty-four hour ambulatory blood pressure monitoring pattern of resistant hypertension. Blood Press Monit. 2003;8(5):181-5.Chart 2 presents the main applicability in hypertension of the ABPM, a fundamental test in RHTN evaluation, diagnosis, and follow-up.
4.3. Home Blood Pressure Monitoring and Blood Pressure Self-Measurement
Home BP measurements are more accurate than casual BP measurements and offer a better prediction of risk for CV outcomes, contributing to greater adherence to drug treatment.3535. Nobre FMJ, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 2018;110(5 Supl.1):1-29.,3838. Souza WKS, Jardim PCB, Porto LB, Araújo FA, Sousa ALL, Salgado CM. Comparação e correlação entre automedida, medida casual e monitorização ambulatorial da pressão arterial. Arq Bras Cardiol. 2011;97(2):148-55.,3939. Breaux-Shropshire TL, Judd E, Vucovich LA, Shropshire TS, Singh S. Does home blood pressure monitoring improve patient outcomes? A systematic review comparing home and ambulatory blood pressure monitoring on blood pressure control and patient outcomes. Integr Blood Press Control. 2015;8:43-9. In this context, HBPM and BP self-measurement (BPSM) are viable and effective alternatives for proper diagnosis and improved adherence.4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,4141. Souza WKS, Jardim PCB, Brito LP, Araújo FA, Sousa ALL. Automedida da pressão arterial para o controle das cifras tensionais e para a adesão ao tratamento. Arq Bras Cardiol. 2012;98:(2)167-74.
4.4. Measurement of Central Arterial Pressure
Arterial stiffness is recognized as an important prognostic index and potential therapeutic target in patients with hypertension. As a result, central systolic blood pressure (cSBP) and PWV have been recently investigated in a population of patients with RHTN.4242. Vamsi V, Golub A, Mija P, Fekete P, Findri F, Prkacin I. Central blood pressure and pulse wave velocity in patients with resistant hypertension. Signa Vitae. 2018;14(Suppl 1):28-30. The mean age of the population was 58.7 ± 15.3 years, and 65% (n = 53) were women. Brachial and central blood pressures were elevated in all patients. Additionally, the PWV value was higher than the reference value for age, and the difference was statistically higher for PWV in women.
Another study2323. Chung CM, Cheng HW, Chang JJ, Lin YS, Hsiao JF, Chang ST, et al. Relationship between resistant hypertension and arterial stiffness assessed by brachial-ankle pulse wave velocity in the older patient. Clin Interv Aging. 2014 Sep 5;9:1495-502. analyzing associations between RHTN and arterial stiffness has shown that patients with RHTN have increased vascular stiffness compared with patients with well-controlled hypertension. PWV increased with arterial stiffness and correlated with BP levels, justifying the need for adequate BP control.
5. Target-Organ Damage
Coordinator: Roberto Dischinger Miranda.
Authors: José Fernando Vilela-Martin, Juan Carlos Yugar-Toledo, Wilson Nadruz Júnior, and Cibele Isaac Saad Rodrigues.
5.1. Introduction
Both C-RHTN and UC-RHTN are associated with a higher prevalence of TOD and higher CV risk and mortality compared with controlled hypertension.4343. Cuspidi C, Macca G, Sampieri L, Michev I, Salerno M, Fusi V, et al. High prevalence of cardiac and extracardiac target organ damage in refractory hypertension. J Hypertens. 2001;19(11):2063-70.
44. de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30(6):1211-6.-4545. Sim JJ, Bhandari SK, Shi J, Reynolds K, Calhoun DA, Kalantar-Zadeh K, et al. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and nonresistant hypertension. Kidney Int. 2015;88(3):622-32. Therefore, the investigation of TOD in RHTN is fundamental to complement the risk stratification and establish the prognosis.4444. de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30(6):1211-6.
5.2. Vascular Changes
Patients with RHTN present structural and functional vascular changes resulting not only from uncontrolled hypertension but also from early vascular aging. This is a complex process involving biochemical, enzymatic, and cellular changes that modify the function and structure of the artery, culminating in early and progressive degeneration of the arterial health.4343. Cuspidi C, Macca G, Sampieri L, Michev I, Salerno M, Fusi V, et al. High prevalence of cardiac and extracardiac target organ damage in refractory hypertension. J Hypertens. 2001;19(11):2063-70.
44. de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30(6):1211-6.
45. Sim JJ, Bhandari SK, Shi J, Reynolds K, Calhoun DA, Kalantar-Zadeh K, et al. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and nonresistant hypertension. Kidney Int. 2015;88(3):622-32.
46. Nilsson PM. Hemodynamic Aging as the Consequence of Structural Changes Associated with Early Vascular Aging (EVA). Aging Dis. 2014;5(2):109-13.-4747. Papakatsika S, Stabouli S, Antza C, Kotsis V. Early Vascular Aging: A New Target for Hypertension Treatment. Curr Pharm Des. 2016;22(1):122-6.
Pathophysiological mechanisms include increased oxidative stress, endothelial dysfunction, vascular remodeling, smooth muscle cell hypertrophy, increased arterial stiffness due to changes in collagen/elastin distribution, vascular inflammation, and increased expression of inflammatory mediators and matrix repair metalloproteinases, in addition to increased advanced glycation end-products and parietal calcification.4848. Barbaro NR, de Araujo TM, Tanus-Santos JE, Anhe GF, Fontana V, Moreno H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed Res Int. 2015;2015:631594.,4949. Barbaro NR, Fontana V, Modolo R, De Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Pressure.2015;24(1):7-13.
The molecular mechanisms of vascular aging include genetic alterations in segments involved in DNA protection and repair5050. Camici GG, Savarese G, Akhmedov A, Luscher TF. Molecular mechanism of endothelial and vascular aging: implications for cardiovascular disease. Eur Heart J. 2015;36(48):3392-403. and mitochondrial metabolic activity.5151. Harvey A, Montezano AC, Touyz RM. Vascular biology of ageing-Implications in hypertension. J Mol Cell Cardiol. 2015 Jun;83:112-21.
In the microcirculation, endothelial dysfunction promotes vasoconstriction, eutrophic remodeling (increased media/lumen [M/L] ratio without external changes), decreased vasodilatory reserve and vascular rarefaction, the latter evaluated by in vivo capillaroscopy,5252. Rizzoni D, Agabiti Rosei C, De Ciuceis C, Semeraro F, Rizzoni M, Docchio F. New Methods to Study the Microcirculation. Am J Hypertens. 2018;31(3):265-73. gluteus biopsy, or yet, measurement of the M/L ratio with laser Doppler flowmetry of retinal arteries5353. Lehmann MV, Schmieder RE. Remodeling of retinal small arteries in hypertension. Am J Hypertens. 2011;24(12):1267-73. and optical videomicroscopy. In large arteries, parietal remodeling leads to increased arterial stiffness.4949. Barbaro NR, Fontana V, Modolo R, De Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Pressure.2015;24(1):7-13.,5454. Cecelja M, Chowienczyk P. Molecular Mechanisms of Arterial Stiffening. Pulse (Basel). 2016;4(1):43-8.
55. Mikael LR, Paiva AMG, Gomes MM, Sousa ALL, Jardim P, Vitorino PVO, et al. Vascular Aging and Arterial Stiffness. Arq Bras Cardiol. 2017;109(3):253-8.-5656. Mozos I, Malainer C, Horbanczuk J, Gug C, Stoian D, Luca CT, et al. Inflammatory Markers for Arterial Stiffness in Cardiovascular Diseases. Front Immunol. 2017;8:1058.
Arterial stiffness is estimated by carotid-femoral PWV (c-f PWV) and calculation of the augmentation index (AIx) by applanation tonometry.5757. Balduino Mendes AB, Giollo-Junior LT, de Andrade DO, Gregorio ML, Yugar-Toledo JC, Vilela-Martin JF. How to Investigate the Vascular Changes in Resistant Hypertension. Curr Hypertens Rev. 2016;12(2):139-47.,5858. Virdis A. Arterial Stiffness and Vascular Aging: From Pathophysiology to Treatment, with a Look at the Future. High Blood Press Cardiovasc Prev. 2018;25(2):135-6. These changes in arterial stiffness hemodynamic parameters and cellular biomarkers are associated with increased morbidity and mortality.5959. Joly L. Arterial stiffness and cognitive function. Geriatr Psychol Neuropsychiatr Vieil. 2017;15(1):83-8.,6060. Hughes TM, Wagenknecht LE, Craft S, Mintz A, Heiss G, Palta P, et al. Arterial stiffness and dementia pathology: Atherosclerosis Risk in Communities (ARIC)-PET Study. Neurology. 2018;90(14):e1248-e56.
The macrovascular involvement is further characterized by carotid, cerebral, coronary, and peripheral atherosclerotic diseases.6161. Muntner P, Davis BR, Cushman WC, Bangalore S, Calhoun DA, Pressel SL, et al. Treatment-resistant hypertension and the incidence of cardiovascular disease and end-stage renal disease: results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2014;64(5):1012-21.,6262. Lotufo PA, Pereira AC, Vasconcellos PS, Santos IS, Mill JG, Bensenor IM. Resistant Hypertension: Risk Factors, Subclinical Atherosclerosis, and Comorbidities Among Adults—The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Hypertens. 2015;17(1):74-80.
5.3. Cerebral Changes
The cerebrovascular involvement in RHTN is subtle and insidious. Microscopic white matter lesions begin early and may progress irreversibly, leading to cognitive impairment and progression to vascular dementia.6363. Iadecola C. Hypertension and Dementia. Hypertension. 2014;64(1):3-5.,6464. Laurent S, Boutouyrie P. The structural factor of hypertension: large and small artery alterations. Circ Res. 2015;116(6):1007-21.
Patients with RHTN have a higher risk of cerebral infarction and transient cerebral ischemia, a fact that has been pointed out by the Kaiser Permanente1616. Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88(10):1099-107. and REGARDS studies,6565. Howard VJ, Tanner RM, Anderson A, Irvin MR, Calhoun DA, Lackland DT, et al. Apparent Treatment-resistant Hypertension Among Individuals with History of Stroke or Transient Ischemic Attack. Am J Med. 2015;128(7):707-14.e2. which showed risk increases of 17 and 14%, respectively. Atherosclerosis of the carotid and small cerebral vessels is responsible for ischemic and thromboembolic phenomena. Retinal artery occlusion is a marker of small vessel injury and has been associated with an increased risk of cerebral events.6666. Hong J-H, Sohn S-I, Kwak J, Yoo J, Ahn SJ, Woo SJ, et al. Retinal artery occlusion and associated recurrent vascular risk with underlying etiologies. PLoS One. 2017;12(6):e0177663.
Uncontrolled hypertension is the leading cause of hemorrhagic stroke. Patients with RHTN have microangiopathy (Charcot-Bouchard aneurysms), which affect the penetrating arteries in the brain and cause intraparenchymal hemorrhage.6767. Hong D, Stradling D, Dastur CK, Akbari Y, Groysman L, Al-Khoury L, et al. Resistant Hypertension after Hypertensive Intracerebral Hemorrhage Is Associated with More Medical Interventions and Longer Hospital Stays without Affecting Outcome. Front Neurol. 2017;8:184.
Changes in large artery stiffness are also associated with increased occurrence of microvascular changes and a greater predisposition to cerebrovascular events.6868. Chen Y, Shen F, Liu J, Yang GY. Arterial stiffness and stroke: de-stiffening strategy, a therapeutic target for stroke. Stroke Vasc Neurol. 2017;2(2):65-72.
5.4. Cardiac Changes
Several cardiac changes may be observed in patients with RHTN, including LVH, left ventricular diastolic dysfunction (LVDD), and myocardial ischemia.6969. Cuspidi C, Vaccarella A, Negri F, Sala C. Resistant hypertension and left ventricular hypertrophy: an overview. J Am Soc Hypertens. 2010;4(6):319-24. LVH is an independent predictor of heart failure, coronary artery disease (CAD), arrhythmias, and stroke.7070. Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29(1):1-6.
In Brazil, the prevalence of LVH assessed by echocardiography in patients with RHTN ranges from 68 to 87%,7171. Muxfeldt ES, Salles GF. Pulse pressure or dipping pattern: which one is a better cardiovascular risk marker in resistant hypertension? J Hypertens. 2008;26(5):878-84.,7272. Modolo R, de Faria AP, Paganelli MO, Sabbatini AR, Barbaro NR, Nascimento BB, et al. Predictors of silent myocardial ischemia in resistant hypertensive patients. Am J Hypertens. 2015;28(2):200-7. with concentric LVH being the most common geometric pattern in these individuals.7272. Modolo R, de Faria AP, Paganelli MO, Sabbatini AR, Barbaro NR, Nascimento BB, et al. Predictors of silent myocardial ischemia in resistant hypertensive patients. Am J Hypertens. 2015;28(2):200-7.,7373. Muxfeldt ES, de Souza F, Margallo VS, Salles GF. Cardiovascular and renal complications in patients with resistant hypertension. Curr Hypertens Rep. 2014;16(9):471.
LVDD predisposes to cardiovascular events and heart failure, regardless of cardiac mass and BP levels.7474. Nadruz W, Shah AM, Solomon SD. Diastolic Dysfunction and Hypertension. Med Clin North Am. 2017;101(1):7-17. The exact prevalence of LVDD in patients with RHTN is uncertain, but the strong association between this condition and LVH7474. Nadruz W, Shah AM, Solomon SD. Diastolic Dysfunction and Hypertension. Med Clin North Am. 2017;101(1):7-17. suggests that LVDD is very frequent in this population. About one third of the patients with RHTN are diagnosed with CAD.7171. Muxfeldt ES, Salles GF. Pulse pressure or dipping pattern: which one is a better cardiovascular risk marker in resistant hypertension? J Hypertens. 2008;26(5):878-84. However, even in the absence of overt CAD, up to 28% of the patients with RHTN have myocardial ischemia,7272. Modolo R, de Faria AP, Paganelli MO, Sabbatini AR, Barbaro NR, Nascimento BB, et al. Predictors of silent myocardial ischemia in resistant hypertensive patients. Am J Hypertens. 2015;28(2):200-7. which may result from decreased coronary reserve and increased myocardial oxygen consumption, particularly in patients with LVH, and increased arterial stiffness.7070. Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29(1):1-6.,7474. Nadruz W, Shah AM, Solomon SD. Diastolic Dysfunction and Hypertension. Med Clin North Am. 2017;101(1):7-17.
5.5. Renal Changes
The association between RHTN and CKD is well established and may be causal or consequential. The anatomopathological substrate is hypertensive nephrosclerosis, resulting from hemodynamic abnormalities (glomerular hyperfiltration and hypertrophy), culminating in glomerulosclerosis. Nephrosclerosis (erroneously termed “benign”) is characterized by arteriosclerosis and arteriolosclerosis, hyalinosis, tubulointerstitial lesions, global glomerulosclerosis, and focal segmental glomerulosclerosis.
Known risk factors for CKD progression include age > 50 years, male sex, genetic predisposition, family history, African descent, hypertension duration and stage, low socioeconomic status, intensity of albuminuria, degree of renal dysfunction, dyslipidemia, obesity, diabetes, lifestyle habits (diet with excessive salt and/or protein, smoking), and use of nephrotoxic substances, among others.7575. Rodrigues CIS CR, Almeida FA. Hipertensao arterial resistente. In: Moura LRR, Alves MAR, Santos DR, Pecoits Filho R. Tratado de Nefrologia. São Paulo: Atheneu; 2018. Albuminuria and reduced estimated glomerular filtration rate (eGFR) identify patients at high CV and renal risks, and the reduction in albuminuria may be a therapeutic objective in RHTN.2626. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis. 2011;216(1):199-204.
27. da Costa PM, Cortez AF, de Souza F, Mares GS, Dos Santos BDM, Muxfeldt ES. Prognostic impact of baseline urinary albumin excretion rate in patients with resistant hypertension: a prospective cohort study. J Hum Hypertens. 2018;32(2):139-49.-2828. Oliveras A, Armario P, Sierra C, Arroyo JA, Hernandez-del-Rey R, Vazquez S, et al. Urinary albumin excretion at follow-up predicts cardiovascular outcomes in subjects with resistant hypertension. Am J Hypertens. 2013;26(9):1148-54.
Recommended tests for evaluation and follow-up of renal damage include urinalysis, serum creatinine for eGFR calculation using the equations MDRD or CKD-EPI, available at http://ckdepi.org/equations/gfr-calculator/, renal and urinary tract ultrasonography, and calculation of the albuminuria or urinary protein/creatinine ratio for CKD staging7575. Rodrigues CIS CR, Almeida FA. Hipertensao arterial resistente. In: Moura LRR, Alves MAR, Santos DR, Pecoits Filho R. Tratado de Nefrologia. São Paulo: Atheneu; 2018. (Figure 2).
– Prognosis of chronic kidney disease according to degrees of albuminuria and decline in estimated GFR.76 Green: low risk; yellow: moderate risk; orange: high risk; red: very high risk.
6. Phenotype of the Patient with Resistant Hypertension
Coordinator: Luciano Ferreira Drager.
Authors: Heitor Moreno Júnior, Juan Carlos Yugar-Toledo, and Luiz Aparecido Bortolotto.
6.1. Introduction
This section describes initially the characteristics that distinguish patients with RHTN from those with non-resistant hypertension. Subsequently, it discusses the differences between patients with C-RHTN and UC-RHTN, and finally, addresses the approach to the extreme phenotype of the RHTN patients, i.e., patients with refractory hypertension.
6.2. Phenotype of the Patient with Resistant Hypertension
Patients with RHTN often present some characteristics that distinguish them from those with non-resistant hypertension, including older age, obesity, a profile of increased salt intake, CKD, diabetes, presence of TODs such as LVH, female sex, and african descent.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19. The Brazilian multicenter study ReHOT has shown that diabetes, prior stroke, and BP at study entry ≥ 180/110 mmHg (hypertension stage 3) were independent predictors of true resistance.1313. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. While some of these characteristics are intuitive, others, including the female sex, still lack well-defined rationales in predicting RHTN.
6.3. Phenotype of Controlled and Uncontrolled Resistant Hypertension
6.3.1. Pathophysiological Aspects
C-RHTN shows greater dependence on volume status than UC-RHTN, due to critical persistence of water retention, increased sodium sensitivity, hyperaldosteronism, and renal dysfunction. Additionally, these individuals present increased plasma volume expansion measured by thoracic bioimpedance,7777. Taler SJ, Textor SC, Augustine JE. Resistant hypertension: comparing hemodynamic management to specialist care. Hypertension. 2002;39(5):982-8. higher plasma and urinary aldosterone concentrations, suppression of renin activity,7878. Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168(11):1159-64. high plasma aldosterone/renin ratio (ARR), and increased levels of atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP).7979. Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54(3):475-81.
80. Agarwal R. Resistant hypertension and the neglected antihypertensive: sodium restriction. Nephrol Dial Transplant. 2012;27(11):4041-5.
81. Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.
82. Calhoun DA. Refractory and Resistant Hypertension: Antihypertensive Treatment Failure versus Treatment Resistance. Korean Circ J. 2016;46(5):593-600.-8383. Eirin A, Textor SC, Lerman LO. Emerging concepts for patients with treatment-resistant hypertension. Trends Cardiovasc Med. 2016;26(8):700-6. This relationship between increased volume and pressure is the pathophysiological basis demonstrated in several studies8181. Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.,8484. Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004;22(11):2217-26.,8585. Laragh JH, Sealey JE. The Plasma Renin Test Reveals the Contribution of Body Sodium-Volume Content (V) and Renin–Angiotensin (R) Vasoconstriction to Long-Term Blood Pressure. Am J Hypertens. 2011;24(11):1164-80. and justifies the use of diuretics in patients with C-RHTN.8686. Calhoun DA, Booth JN, 3rd, Oparil S, Irvin MR, Shimbo D, Lackland DT, et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63(3):451-8.,8787. Judd EK, Calhoun DA, Warnock DG. Pathophysiology and Treatment of Resistant Hypertension: The Role of Aldosterone and Amiloride-Sensitive Sodium Channels. Semin Nephrol. 2014;34(5):532-9.
In contrast, patients with UC-RHTN often have sympathetic hyperactivity, evidenced by increased (24-hour) urinary metanephrines and resting heart rate, reduced 24-hour variability (spectral analysis), in addition to increased vascular stiffness (increased PWV).8888. Tsioufis C, Kordalis A, Flessas D, Anastasopoulos I, Tsiachris D, Papademetriou V, et al. Pathophysiology of resistant hypertension: the role of sympathetic nervous system. Int J Hypertens. 2011;2011:642416.,8989. Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA. Refractory Hypertension: Evidence of Heightened Sympathetic Activity as a Cause of Antihypertensive Treatment Failure. Hypertension. 2015;66(1):126-33. These markers of increased sympathetic activity, together with other factors linked to hyperaldosteronism,7878. Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168(11):1159-64.,9090. Mahmud A, Mahgoub M, Hall M, Feely J. Does aldosterone-to-renin ratio predict the antihypertensive effect of the aldosterone antagonist spironolactone? Am J Hypertens. 2005;18(12 Pt 1):1631-5.
91. Pimenta E, Calhoun DA. Resistant hypertension and aldosteronism. Curr Hypertens Rep. 2007;9(5):353-9.-9292. Wang C, Xiong B, Huang J. Efficacy and Safety of Spironolactone in Patients with Resistant Hypertension: A Meta-analysis of Randomised Controlled Trials. Heart Lung Circ. 2016;25(10):1021-30. are related to mechanisms that maintain high BP even with administration of four or more antihypertensive agents, characterizing UC-RHTN. Higher PWV values reflect exacerbated arterial stiffness,44. Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, et al. Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens. 2011;25(9):532-8. while elevated levels of cytokines, including tumor necrosis factor-alpha (TNF-α),4848. Barbaro NR, de Araujo TM, Tanus-Santos JE, Anhe GF, Fontana V, Moreno H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed Res Int. 2015;2015:631594.,5656. Mozos I, Malainer C, Horbanczuk J, Gug C, Stoian D, Luca CT, et al. Inflammatory Markers for Arterial Stiffness in Cardiovascular Diseases. Front Immunol. 2017;8:1058.,9393. Jain S, Khera R, Corrales-Medina VF, Townsend RR, Chirinos JA. "Inflammation and arterial stiffness in humans". Atherosclerosis. 2014;237(2):381-90. probably indicate vascular damage in patients with RHTN.4949. Barbaro NR, Fontana V, Modolo R, De Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Pressure.2015;24(1):7-13.
Other factors and mechanisms, such as age, obesity, OSA,44. Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, et al. Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens. 2011;25(9):532-8.,9494. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7.,9595. Florczak E, Prejbisz A, Szwench-Pietrasz E, Sliwinski P, Bielen P, Klisiewicz A, et al. Clinical characteristics of patients with resistant hypertension: the RESIST-POL study. J Hum Hypertens. 2013;27(11):678-85. African descent, adipokine deregulation,9696. de Faria AP, Modolo R, Fontana V, Moreno H. Adipokines: novel players in resistant hypertension. J Clin Hypertens (Greenwich). 2014;16(10):754-9. endothelial dysfunction, and increased activity of metalloproteinases-2, metalloproteinases-9 and adhesion molecules9797. Lacerda L, Faria AP, Fontana V, Moreno H, Sandrim V. Role of MMP-2 and MMP-9 in resistance to drug therapy in patients with resistant hypertension. Arq Bras Cardiol. 2015;105(2):168-75.
98. de Faria AP, Ritter AM, Sabbatini AR, Correa NB, Brunelli V, Modolo R, et al. Deregulation of Soluble Adhesion Molecules in Resistant Hypertension and Its Role in Cardiovascular Remodeling. Circ J. 2016;80(5):1196-201.-9999. Sabbatini AR, Barbaro NR, de Faria AP, Ritter AMV, Modolo R, Correa NB, et al. Matrix metalloproteinase-2 -735C/T polymorphism is associated with resistant hypertension in a specialized outpatient clinic in Brazil. Gene. 2017;620:23-9. are also involved in this process.
Genetic polymorphisms, especially those involving the renin-angiotensin-aldosterone system and the endothelial nitric oxide synthase (eNOS), have been correlated to RHTN100100. Lacchini R, Sabha M, Coeli FB, Favero FF, Yugar-Toledo J, Izidoro-Toledo TC, et al. T allele of -344 C/T polymorphism in aldosterone synthase gene is not associated with resistant hypertension. Hypertens Res. 2009;32(2):159-62.,101101. Yugar-Toledo JC, Martin JF, Krieger JE, Pereira AC, Demacq C, Coelho OR, et al. Gene variation in resistant hypertension: multilocus analysis of the angiotensin 1-converting enzyme, angiotensinogen, and endothelial nitric oxide synthase genes. DNA Cell Biol. 2011;30(8):555-64. (Figure 3). However, large studies conveniently characterized in individuals with the disease are needed to define the importance of genetics in this group of patients.
– Predominant pathophysiological mechanisms in controlled (C-RH) and uncontrolled (U-RH) resistant hypertension. Refractory hypertension (uncontrolled with five or more medications) is included in the U-RH group.
6.3.2. Clinical Differences
In 2011, Martins et al. published a comparative study in patients with C-RH and UC-RHTN44. Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, et al. Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens. 2011;25(9):532-8. specifically assessing biological factors contributing to resistance to antihypertensive agents. Body mass index (BMI), arterial stiffness (PWV), left ventricular mass index (LVMI), and plasma aldosterone concentration (PAC) were higher in the UC-RHTN group when compared with the C-RHTN group. Additionally, the authors demonstrated using multivariate analysis that PWV was dependent on age in both groups, although this influence was more pronounced in patients with UC-RHTN. They also showed that the UC-RHTN group had higher values of carotid intima-media thickness (cIMT) and PWV.102102. Figueiredo VN, Yugar-Toledo JC, Martins LC, Martins LB, de Faria AP, de Haro Moraes C, et al. Vascular stiffness and endothelial dysfunction: Correlations at different levels of blood pressure. Blood Press. 2012;21(1):31-8. Finally, the drop in nocturnal BP (dipping pattern) was less pronounced in the UC-RHTN group.103103. Quinaglia T, Martins LC, Figueiredo VN, Santos RC, Yugar-Toledo JC, Martin JF, et al. Non-dipping pattern relates to endothelial dysfunction in patients with uncontrolled resistant hypertension. J Hum Hypertens. 2011;25(11):656-64.
6.3.3. Prognosis
Pierdomenico et al.104104. Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18(11):1422-8. evaluated CV outcomes in subjects with C-RHTN and UC-RHTN. The occurrence of fatal and nonfatal CV events was investigated in 340 patients with C-RHtN (BP < 140/90 mmHg or daytime BP < 135/85 mmHg) and 130 patients with UC-RHTN (BP ≥ 140 or 90 mmHg and daytime BP > 135 or 85 mmHg). During follow-up (4.98 ± 2.9 years), the event rates per 100 patients/year were 0.87 and 4.1, respectively. These data also show that patients with UC-RHTN have a greater risk of CAD, stroke, arterial disease, congestive heart failure (CHF), kidney disease, and all-cause death compared with patients with C-RHTN.
6.4. Phenotype of the Patient with Refractory Hypertension
Refractory hypertension appears to be an extreme phenotype of patients with RHTN. Recently, phenotypic characterization has shown that these patients are younger than those with RHTN in general, are more commonly women, have a higher frequency of heart failure, and have particularly higher sympathetic activity than patients with RHTN.55. Dudenbostel T, Siddiqui M, Oparil S, Calhoun DA. Refractory Hypertension: A Novel Phenotype of Antihypertensive Treatment Failure. Hypertension. 2016;67(6):1085-92. These findings are important pillars for the pathophysiology of refractoriness, potentially constituting a therapeutic target for procedures such as renal denervation. Studies in this area are currently under development.
7. Secondary Causes of Resistant Hypertension
Coordinator: Fernanda Marciano Consolim-Colombo
Authors: Márcio Gonçalves de Sousa, Flávio Antonio de Oliveira Borelli, Cibele Isaac Saad Rodrigues, and Fernanda Marciano Consolim-Colombo.
7.1. Introduction
Secondary hypertension (SecHTN) is defined as increased BP due to an identifiable cause.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,105105. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54. Patients with RHTN should be investigated for the most prevalent causes of “non-endocrine” and “endocrine” SecHTN after exclusion of use of medications that may interfere with BP values: antiinflammatory drugs, glucocorticoids, nasal decongestants, appetite suppressants, antidepressants, immunosuppressants, erythropoietin, contraceptives, and illicit drugs.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,105105. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.
7.2. Secondary Hypertension due to Non-Endocrine Causes
7.2.1. Obstructive Sleep Apnea
Defined as a total or partial cessation of respiratory flow during sleep, this syndrome promotes oxyhemoglobin desaturation and microarousals during sleep. OSA is estimated to have a prevalence of 17%106106. Braam B, Taler SJ, Rahman M, Fillaus JA, Greco BA, Forman JP, et al. Recognition and Management of Resistant Hypertension. Clin J Am Soc Nephrol. 2017;12(3):524-35.among American adults and 30% among hypertensive individuals and may affect 60 to 80% of the patients with RHTN.9494. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. A recent meta-analysis107107. Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, et al. Association of obstructive sleep apnea with hypertension: A systematic review and meta-analysis. J Glob Health. 2018;8(1):010405. has concluded that the presence of OSA is related to a higher risk of RHTN.107107. Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, et al. Association of obstructive sleep apnea with hypertension: A systematic review and meta-analysis. J Glob Health. 2018;8(1):010405.
Activation of the sympathetic nervous system and humoral abnormalities are responsible for changes in vascular endothelial integrity, and their consequences in patients with OSA include increased BP, development of atherosclerotic disease, and cardiac arrhythmias, among others.108108. Drager LF, Bortolotto LA, Lorenzi MC, Figueiredo AC, Krieger EM, Lorenzi-Filho G. Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. 2005;172(5):613-8. Clinical suspicion can be verified with the Berlin questionnaire.109109. Senaratna CV, Perret JL, Matheson MC, Lodge CJ, Lowe AJ, Cassim R, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2017;36:116-24.
The diagnosis is established with polysomnography, which records apnea/hypopnea indices greater than five events/hour.
Treatment should include recommendations on sleep hygiene and weight loss, among others. For airway clearance, the use of equipment producing continuous positive airway pressure (CPAP) is the most recommended. However, the impact of this treatment on reducing BP values is still debatable.110110. Fava C, Dorigoni S, Dalle Vedove F, Danese E, Montagnana M, Guidi GC, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea a systematic review and meta-analysis. Chest. 2014;145(4):762-71.,111111. Guo J, Sun Y, Xue LJ, Huang ZY, Wang YS, Zhang L, et al. Effect of CPAP therapy on cardiovascular events and mortality in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath. 2016;20(3):965-74.
7.2.2. Renal Parenchymal Disease
Renal parenchymal disease (RPD) is one of the most prevalent causes of SecHTN. The diagnosis of this condition is relatively simple since the assessment of renal function is part of the routine approach in patients with hypertension. Patients on dialysis and renal transplant recipients have a high prevalence of hypertension, and CV events are responsible for high morbidity and mortality in this population.112112. Horl MP, Horl WH. Hemodialysis-associated hypertension: pathophysiology and therapy. Am J Kidney Dis. 2002;39(2):227-44.
The progression of renal dysfunction in patients with RPD is directly related to BP values, and target BP levels should be achieved to reduce CV morbidity and mortality. In patients with RPD and renal transplant recipients, ACEIs and angiotensin-II receptor blockers have been shown to offer renal protection additional to that obtained by BP reduction, and are, therefore, the preferred medications.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,105105. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.,113113. Wolley MJ, Stowasser M. Resistant Hypertension and Chronic Kidney Disease: a Dangerous Liaison. Curr Hypertens Rep. 2016;18(5):36.
7.2.3. Renal Artery Stenosis
Renovascular disease is a term used to define renal artery involvement by different pathologies, including atherosclerotic disease, fibromuscular dysplasia, and vasculitis, which can lead to arterial obstruction. Usually, no symptoms are associated with mild arterial obstruction. However, with obstructions affecting more than 70% of the artery, severe hypertension and even ischemic nephropathy may occur.
Renal artery stenosis (RAS) of atherosclerotic origin is present in 12.5% of the patients with RHTN older than 50 years of age.114114. van Jaarsveld BC, Krijnen P, Pieterman H, Derkx FH, Deinum J, Postma CT, et al. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med. 2000;342(14):1007-14. The diagnosis should always be determined, but the treatment of this condition is still much discussed in the literature.115115. Bavishi C, de Leeuw PW, Messerli FH. Atherosclerotic Renal Artery Stenosis and Hypertension: Pragmatism, Pitfalls, and Perspectives. Am J Med. 2016;129(6):635 e5- e14.,116116. Van der Niepen P, Rossignol P, Lengele JP, Berra E, Sarafidis P, Persu A. Renal Artery Stenosis in Patients with Resistant Hypertension: Stent It or Not? Curr Hypertens Rep. 2017;19(1):5. Adequate BP control and interruption of progressive renal function deterioration are the primary treatment goals in these patients. To achieve that, two therapeutic possibilities are available for this population: clinical and interventional (surgical or percutaneous, with or without stent implantation).
Interventions are recommended for patients with RHTN or accelerated hypertension with progressive loss of renal function, bilateral RAS or stenosis in a “single” kidney, or with severe complications (CHF and recurrent acute pulmonary edema).3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,115115. Bavishi C, de Leeuw PW, Messerli FH. Atherosclerotic Renal Artery Stenosis and Hypertension: Pragmatism, Pitfalls, and Perspectives. Am J Med. 2016;129(6):635 e5- e14.,116116. Van der Niepen P, Rossignol P, Lengele JP, Berra E, Sarafidis P, Persu A. Renal Artery Stenosis in Patients with Resistant Hypertension: Stent It or Not? Curr Hypertens Rep. 2017;19(1):5.
Other potential surgical indications include total renal artery obstruction, large arteriovenous fistulas, aortic lesion encompassing the renal arteries, and failure in clinical or endovascular treatment.117117. Mulherin JL, Jr., Edwards WH. Alternative methods of renal revascularization. Ann Surg. 1987;205(6):740-6.
7.3. Secondary Hypertension due to Endocrine Causes
7.3.1. Primary Hyperaldosteronism
Considered in the past to be a rare type of SecHTN (with a prevalence of about 1%), hyperaldosteronism is currently believed to occur in up to 22% of the cases in populations with RHTN.118118. Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.,119119. Kline GA, Prebtani APH, Leung AA, Schiffrin EL. Primary aldosteronism: a common cause of resistant hypertension. CMAJ. 2017;189(22):E773-E8.The most frequent cause of hyperaldosteronism is adrenal adenoma, while unilateral or bilateral hyperplasia is less frequently detected. Carcinomas (albeit infrequent) and genetic forms of the disease may also be responsible for the occurrence of hyperaldosteronism.
Aldosterone, through activation of mineralocorticoid receptors, is related to insulin resistance and endothelial dysfunction and, consequently, participates in the development of metabolic syndrome and CV and renal lesions associated with RHTN. Thus, mineralocorticoid receptor blockade improves endothelial dysfunction and contributes to a better response to RHTN and TOD therapies.118118. Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.,119119. Kline GA, Prebtani APH, Leung AA, Schiffrin EL. Primary aldosteronism: a common cause of resistant hypertension. CMAJ. 2017;189(22):E773-E8.
During the diagnostic evaluation, all patients with RHTN (not only those with hypokalemia) should be evaluated for the occurrence of hyperaldosteronism.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6. Screening should include the assessment of the plasma aldosterone concentration (PAC expressed in ng/dL) to plasma renin activity (PRA expressed in ng/mL/hr) called aldosterone/renin ratio (ARR). This method has excellent sensitivity but may yield false-positive results. Therefore, adoption of the minimum PAC and PRA values of 15 ng/dL and 0.5 ng/mL/h, respectively, are recommended. An ARR ≥ 100 establishes the diagnosis of hyperaldosteronism, while values < 20 to 30 indicate a low probability of the disease, and values in between detect “individuals potentially affected” by this condition.120120. Young JWF, Calhoun DA, Lenders JWM, Stowasser M, Textor SC. Screening for Endocrine Hypertension: An Endocrine Society Scientific Statement. Endocrine Rev. 2017;38(2):103-22. In the latter case, tests assessing the renin-aldosterone axis (saline infusion test, walking, use of diuretics) may be performed.
Tomography or magnetic resonance imaging is used for imaging identification of adrenal adenomas or hyperplasia. The absence of a visible tumor on tomography does not exclude the presence of a microadenoma, hence the importance of searching for excessive aldosterone production. Functional images, obtained by adrenal scintigraphy, may be useful in detecting adenomas and may differentiate them from nodular hyperplasia in up to 90% of the cases. Adrenal vein blood sampling can be used to confirm lateralization in aldosterone secretion and the presence of unilateral adenoma.120120. Young JWF, Calhoun DA, Lenders JWM, Stowasser M, Textor SC. Screening for Endocrine Hypertension: An Endocrine Society Scientific Statement. Endocrine Rev. 2017;38(2):103-22.,121121. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
In terms of treatment, unilateral resection usually corrects excessive aldosterone production and potassium loss in unilateral adenomas. The BP response to surgical treatment varies. Cases of hyperplasia benefit from aldosterone receptor blockade.121121. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
7.3.2. Pheochromocytoma
Pheochromocytoma is a rare neuroendocrine tumor that originates from chromaffin cells (cells producing catecholamines). The most common clinical manifestation of this condition is elevated BP, and the disease may arise from the adrenal medulla or extra-adrenal paraganglia (paragangliomas). Clinical exacerbation peaks between the third and fourth decades of life, but 10% of the cases arise in childhood.
These tumors may be sporadic or associated with genetic syndromes.122122. Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005;366(9486):665-75.,123123. Pillai S, Gopalan V, Smith RA, Lam AK. Updates on the genetics and the clinical impacts on phaeochromocytoma and paraganglioma in the new era. Crit Rev Oncol Hematol. 2016;100:190-208. They are usually unilateral; however, in familial syndromes, they may be bilateral, multiple, or extra-adrenal, and benign or malignant (5 to 26% of the cases). This etiology should be investigated in all patients presenting with RHTN and/or symptoms or signs suggestive of hyperadrenergic spells. Paroxysmal hypertension occurs in 30% of the cases, triggered by regular physical activity, exercises with increased intensity, surgical procedures, and use of certain substances such as tricyclic antidepressants, histamine, and opioids. Paroxysms may be accompanied by headache (60 to 90%), sweating (55 to 75%), and palpitations (50 to 70%). Symptoms of heart failure and electrocardiographic abnormalities may indicate myocarditis induced by catecholamine excess.
At diagnosis, measurement of metanephrines (catecholamine metabolites) in plasma and 24-hour urine has higher sensitivity and specificity than direct catecholamine measurement. When laboratory tests are not elucidative, clonidine suppression test may be performed (administration of clonidine 0.2 mg and measurement of catecholamines 1 hour before and 2 hours after the medication).
For a topographic diagnosis of the tumors and, eventually, the metastases, the recommended imaging methods are computed tomography and magnetic resonance imaging, both of which have sensitivity close to 100% for adrenal tumors. Whole-body 131 or 123 metaiodobenzylguanidine (MIBG) has sensitivity of 56 to 85% (malignant tumors) and high specificity. Octreoscan, bone mapping, and PET scan (with different markers) can be decisive when previous localization tests are negative or in the investigation of malignant disease.
Treatment is surgical. However, in preoperative or chronic medication therapy, alpha-blockers (prazosin, doxazosin, and dibenzyline) are initially used, combined or not with other agents such as beta-blockers (after effective alpha blockade), ACEIs, and CCBs. Control of BP levels and volume replacement are recommended before the surgical intervention.124124. Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth. 2017;31(4):1427-39. Sodium nitroprusside can be used in acute crises and during surgery.124124. Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth. 2017;31(4):1427-39.
7.3.3. Hypothyroidism and Hyperthyroidism
Hypertension may affect 40% of the patients with thyroid disorders, while correction of the glandular dysfunction usually results in BP control.125125. Saito I, Ito K, Saruta T. Hypothyroidism as a cause of hypertension. Hypertension. 1983;5(1):112-5. If BP levels remain high after correction of the hypothyroidism or hyperthyroidism, use of antihypertensive drugs is indicated.3232. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-104.,126126. Levey GS, Klein I. Catecholamine-thyroid hormone interactions and the cardiovascular manifestations of hyperthyroidism. Am J Med. 1990;88(6):642-6.
Causes of SecH in patients with RHTN are summarized in Table 1.
8. Non-Pharmacological Treatment
Coordinator: Sérgio Emanuel Kaiser.
Authors: Gil Fernando Salles, Maria de Fátima de Azevedo, and Lucélia Batista Neves Cunha Magalhães.
8.1. Weight Loss
Several mechanisms contribute to maintain high BP in obese patients with hypertension, including OSA, sympathetic hyperactivity, endothelial dysfunction, and modification of the intestinal microbiota – all these factors can promote an inflammatory phenotype and perpetuate a vicious cycle.130130. Cohen JB. Hypertension in Obesity and the Impact of Weight Loss. Curr Cardiol Rep. 2017;19(10):98. Patients with BMI ≥ 30 kg/m22. Modolo R, de Faria AP, Almeida A, Moreno H. Resistant or refractory hypertension: are they different? Curr Hypertens Rep. 2014;16(10):485. are 50% more likely to have uncontrolled BP than those with normal BMI (< 25 kg/m22. Modolo R, de Faria AP, Almeida A, Moreno H. Resistant or refractory hypertension: are they different? Curr Hypertens Rep. 2014;16(10):485.).131131. Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure : factors associated with lack of blood pressure control in the community. Hypertension. 2000;36(4):594-9. A BMI > 40 kg/m22. Modolo R, de Faria AP, Almeida A, Moreno H. Resistant or refractory hypertension: are they different? Curr Hypertens Rep. 2014;16(10):485. triples the chances of the requirement of multiple drugs for BP control.132132. Bramlage P, Pittrow D, Wittchen HU, Kirch W, Boehler S, Lehnert H, et al. Hypertension in overweight and obese primary care patients is highly prevalent and poorly controlled. Am J Hypertens. 2004;17(10):904-10.
A weight loss of 10 kg is associated with mean reductions of 6.0 mmHg in systolic BP and 4.0 mmHg in diastolic BP.133133. Aucott L, Poobalan A, Smith WC, Avenell A, Jung R, Broom J. Effects of weight loss in overweight/obese individuals and long-term hypertension outcomes: a systematic review. Hypertension. 2005;45(6):1035-41. Surprisingly, there is no consistent evidence on the effect of diet-induced weight loss in patients with RHTN, but this recommendation meets the common sense and the evidence available in other subgroups. There are also no data on the effect of bariatric surgery on BP in this subgroup. A recent randomized trial showed a reduction of at least 30% in the number of antihypertensive drugs in 84% of operated patients, compared with 12.4% in the clinically treated group.134134. Schiavon CA, Bersch-Ferreira AC, Santucci EV, Oliveira JD, Torreglosa CR, Bueno PT, et al. Effects of Bariatric Surgery in Obese Patients With Hypertension: The GATEWAY Randomized Trial (Gastric Bypass to Treat Obese Patients With Steady Hypertension). Circulation. 2018;137(11):1132-42.
8.2. Salt Restriction
Control of salt intake is especially effective in the elderly, in individuals of African descent, and in those with decreased glomerular filtration.135135. Edwards DG, Farquhar WB. Vascular effects of dietary salt. Curr Opin Nephrol Hypertens. 2015;24(1):8-13. These situations restrict the ability of water and sodium excretion by the kidneys, and BP becomes more dependent on volume variations. Not surprisingly, sodium sensitivity and volume overload account for the primary pathophysiological mechanism in most cases of RHTN.136136. White WB, Turner JR, Sica DA, Bisognano JD, Calhoun DA, Townsend RR, et al. Detection, evaluation, and treatment of severe and resistant hypertension. In: Congress of American Society of Hypertension Interactive (forum) Bethesda, MD, October 10th 2013. Proceedings. J Am Soc Hypertens. 2014;8(10):743-57. A systematic review and meta-analysis involving 34 studies with 3,230 participants on the effect of long-term reduction in sodium intake revealed a decrease in systolic BP of 5.8 mmHg (2.5 to 9.2; p = 0.001) associated with a decrease in urinary sodium excretion of up to 100 mmol in 24 h, which corresponds to a reduction in salt intake of approximately 6 g/day.137137. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. In patients with RHTN, a low-sodium diet with 2.5 g of salt daily reduced BP by up to 23.0/9.0 mmHg, clearly demonstrating the efficacy of this measure, despite the possibility of compromising the long-term adherence to such markedly restricted salt consumption.7979. Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54(3):475-81.
8.3. Alcohol Intake
Due to the direct relationship between the amount of alcohol consumed and BP levels, excessive alcohol consumption contributes significantly to hinder BP control.138138. Wildman RP, Gu D, Muntner P, Huang G, Chen J, Duan X, et al. Alcohol intake and hypertension subtypes in Chinese men. J Hypertens. 2005;23(4):737-43.After all, daily consumption of more than two drinks (about 24 g/day) is associated with increased BP levels.139139. Sarwar MS, Islam MS, Al Baker SM, Hasnat A. Resistant hypertension: underlying causes and treatment. Drug Res (Stuttg). 2013;63(5):217-23. A recent meta-analysis of 36 studies with 2865 participants revealed that a 50% reduction in daily alcohol intake among consumers of six or more drinks (72 g) led to a decrease of 5.50 mmHg in systolic BP (95% CI; 6.70 to 4.30) and 3.97 mmHg in diastolic BP (95% CI; 4.70 to 3.25).140140. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Publ Health. 2017;2(2):e108-e20. No studies have been published on patients with RHTN; however, based on available information, daily alcohol consumption is recommended to be restricted to less than two standard drinks (about 24 g) or even interrupted.
8.4. Physical Activity
Despite having been evaluated only in small groups of patients with RHTN, physical activity is probably as much – or even more – beneficial in these individuals compared with those with non-resistant hypertension.4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,141141. Ribeiro F, Costa R, Mesquita-Bastos J. Exercise training in the management of patients with resistant hypertension. World J Cardiol. 2015;7(2):47-51. Regular aerobic exercise decreases office and ambulatory BP in patients with RHTN142142. Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. 2012;60(3):653-8.
143. Guimaraes GV, de Barros Cruz LG, Fernandes-Silva MM, Dorea EL, Bocchi EA. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: a randomized controlled trial (HEx trial). Int J Cardiol. 2014;172(2):434-41.
144. Santos LP, Moraes RS, Vieira PJ, Ash GI, Waclawovsky G, Pescatello LS, et al. Effects of aerobic exercise intensity on ambulatory blood pressure and vascular responses in resistant hypertension: a crossover trial. J Hypertens. 2016;34(7):1317-24.-145145. Kruk PJ, Nowicki M. Effect of the physical activity program on the treatment of resistant hypertension in primary care. Prim Health Care Res Dev. 2018; 22:1-9. and attenuates the characteristic neurohumoral activation.146146. Cruz LG, Bocchi EA, Grassi G, Guimaraes GV. Neurohumoral and Endothelial Responses to Heated Water-Based Exercise in Resistant Hypertensive Patients. Circ J. 2017;81(3):339-45. Despite the lack of studies on resistance exercise in this subgroup, it is assumed that there is at least an advantage similar to that observed in patients with non-resistant hypertension.147147. Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950-8. Furthermore, the improved cardiorespiratory capacity obtained with physical activity appears to reduce mortality in patients with RHTN.148148. Narayan P, Doumas M, Kumar A, Faselis CJ, Myers JN, Pittaras A, et al. Impact of Cardiorespiratory Fitness on Mortality in Black Male Veterans With Resistant Systemic Hypertension. Am J Cardiol. 2017;120(9):1568-71. Therefore, this category of patients should be encouraged to perform regular physical activity of moderate intensity under proper supervision. In patients with very high BP (systolic BP ≥ 180 mmHg or diastolic BP ≥ 110 mmHg), physical activity should be delayed until the optimization of pharmacological treatment promotes BP reduction.4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,141141. Ribeiro F, Costa R, Mesquita-Bastos J. Exercise training in the management of patients with resistant hypertension. World J Cardiol. 2015;7(2):47-51.
9. Pharmacological Treatment of Resistant Hypertension
Coordinator: Rui Manoel dos Santos Póvoa.
Authors: Marcus Vinícius Bolívar Malachias, Armando da Rocha Nogueira, and Paulo César Brandão Veiga Jardim.
The objective of pharmacological treatment in RHTN is to identify the causes of lack of control and find the best combination of drugs, aiming at achieving the target BP with few adverse effects and greater adherence.
In general, triple treatment optimization is attempted with preferred drugs, namely, ACEIs or ARBs, dihydropyridine CCBs, and TZDs.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,149149. Povoa R, Barroso WS, Brandao AA, Jardim PC, Barroso O, Passarelli O, Jr., et al. I brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
Because they are better tolerated, ACEIs or ARBs must be increased to maximum doses in RHTN. Long-acting, higher potency TZDs, such as chlorthalidone instead of hydrochlorothiazide, should be used at appropriate doses for volume control, from 12.5 to 50 mg in a single dose in the morning.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.,3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,150150. Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. Indapamide is a second TZD option in RHTN.150150. Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115.Furosemide should be used in cases of CKD with a eGFR of 30 mL/min or less.11. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.,3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6. In RHTN, CCB should preferably be taken at night to alternate the peaks of action of the antihypertensive drugs.4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.
Intolerance to CCBs due to side effects is often one of the causes of treatment resistance. In such cases, lipophilic CCBs (manidipine, lercanidipine, manidipine) or levamlodipine, at low doses, may be attempted or, in selected cases, a non-dihydropyridine CCB such as diltiazem and verapamil.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6. If a CCB cannot be used, introduction of a beta-blocker may be considered, preferably one with vasodilatory action, such as nebivolol or carvedilol.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,151151. Salles GF, Cardoso CR, Fonseca LL, Fiszman R, Muxfeldt ES. Prognostic significance of baseline heart rate and its interaction with beta-blocker use in resistant hypertension: a cohort study. Am J Hypertens. 2013;26(2):218-26. Beta-blockers may also be considered in association with one or more preferred antihypertensive drugs – ACEI or ARB, TZD, CCB – in special conditions such as heart failure, CAD, and increased basal heart rate, among others.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,150150. Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115.,151151. Salles GF, Cardoso CR, Fonseca LL, Fiszman R, Muxfeldt ES. Prognostic significance of baseline heart rate and its interaction with beta-blocker use in resistant hypertension: a cohort study. Am J Hypertens. 2013;26(2):218-26.
Failure to reach the target BP with triple therapy requires the use of a fourth drug, which current preferred option is spironolactone, 25 to 50 mg daily.1313. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,152152. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059-68.
153. Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159-66.-154154. Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, et al. The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies. Am J Hypertens. 2015;28(11):1376-85. In cases of intolerance to spironolactone, which main adverse effect is gynecomastia in men, 12.5 mg daily may be attempted. As eplerenone is not available in our country, if intolerance to spironolactone persists even at low doses, replacement with a central sympatholytic agent should be considered, preferably clonidine, between 0.100 and 0.200 mg twice daily,152152. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059-68. or a potassium-sparing diuretic, preferably amiloride (only available sparingly in our country in compounded formulations), from 10 to 20 mg;155155. Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabetes Endocrinol. 2018;6(6):464-75. or a beta-blocker, preferably with vasodilatory action, if not yet used;4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85. or an alpha-blocker, preferably doxazosin 1 to 16 mg in one (nighttime) or two daily doses.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.,4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,155155. Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabetes Endocrinol. 2018;6(6):464-75.
All these antihypertensive agents may be used in combination when necessary for BP control.3333. Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6. When no control is obtained with the addition of the fourth drug or combinations of the following options, a direct vasodilator must be used, preferably hydralazine, at doses between 50 and 150 mg administered twice or thrice daily.4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.Due to frequent adverse effects, the vasodilator minoxidil should be reserved for situations of extreme resistance when all previous alternatives fail4040. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.,150150. Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. (Figure 4).
– Flowchart of RH treatment. CCB: calcium channel blocker; ARB: angiotensin receptor blocker; HR: heart rate; ACEI: angiotensin-converting enzyme inhibitor; CKD: chronic kidney disease; BP: blood pressure.
In RHTN treatment, attention must be given to possible adverse effects of each drug used, along with their possible interactions.
10. New Treatments of Resistant Hypertension
Coordinator: Luiz Aparecido Bortolotto.
Authors: Luiz Aparecido Bortolotto, Luciano Ferreira Drager, and Thiago de Souza Veiga Jardim
10.1. Introduction
In recent years, new types of interventional treatment have been evaluated in patients with RHTN, including:
10.2. Direct Carotid Sinus Stimulation
Stimulation of carotid baroreceptors increases their activity and, consequently, reduces sympathetic flow, resulting in decreased BP.156156. van Kleef MEAM, Bates MC, Spiering W. Endovascular Baroreflex Amplification for Resistant Hypertension. Curr Hypertens Report. 2018;20(5):46. Interventions promoting this stimulation have been used to treat patients with RHTN lacking response to clinical treatment.156156. van Kleef MEAM, Bates MC, Spiering W. Endovascular Baroreflex Amplification for Resistant Hypertension. Curr Hypertens Report. 2018;20(5):46.
157. Bisognano JD, Bakris G, Nadim MK, Sanchez L, Kroon AA, Schafer J, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58(7):765-73.
158. Heusser K, Tank J, Brinkmann J, Menne J, Kaufeld J, Linnenweber-Held S, et al. Acute Response to Unilateral Unipolar Electrical Carotid Sinus Stimulation in Patients with Resistant Arterial Hypertension. Hypertension. 2016;67(3):585-91.-159159. Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-9. Baroreflex activation therapy (BAT) is a surgical procedure in which electrodes are surgically implanted on the external portion of the carotid sinus unilaterally or bilaterally.157157. Bisognano JD, Bakris G, Nadim MK, Sanchez L, Kroon AA, Schafer J, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58(7):765-73.,159159. Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-9. BAT has shown significant reductions in BP persisting for up to 3 years in randomized controlled trials.157157. Bisognano JD, Bakris G, Nadim MK, Sanchez L, Kroon AA, Schafer J, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58(7):765-73.,159159. Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-9. However, this procedure is invasive and expensive and is associated with side effects, limiting its indication in clinical practice.156156. van Kleef MEAM, Bates MC, Spiering W. Endovascular Baroreflex Amplification for Resistant Hypertension. Curr Hypertens Report. 2018;20(5):46.,159159. Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-9. Another form of stimulation is the amplification of the endovascular baroreflex (implantation of an expandable device within the carotid artery), which has shown promising results with greater safety in controlling BP in RHTN.156156. van Kleef MEAM, Bates MC, Spiering W. Endovascular Baroreflex Amplification for Resistant Hypertension. Curr Hypertens Report. 2018;20(5):46. These procedures are not available in Brazil.
10.3. Renal Sympathetic Denervation
Renal sympathetic denervation (RSD) by ablation catheter reduces renal efferent activity and, consequently, increases renal blood flow and decreases activation of the renin-angiotensin-aldosterone system, water retention, and renal afferent activity, which through brain signaling, decreases sympathetic action on heart and vessels.160160. Schmieder RE, Mahfoud F, Azizi M, Pathak A, Dimitriadis K, Kroon AA, et al. European Society of Hypertension position paper on renal denervation. J Hypertens. 2018;391(10137):2335-45.
Data from uncontrolled studies have shown reductions of up to 30 mmHg in office systolic BP in patients with RHTN, without complications related to the procedure.161161. Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circ Res. 2015;116(6):1074-95. However, the SYMPLICITY HTN-3 trial,162162. Bakris GL, Townsend RR, Flack JM, Brar S, Cohen SA, D'Agostino R, et al. 12-month blood pressure results of catheter-based renal artery denervation for resistant hypertension: the SYMPLICITY HTN-3 trial. J Am Coll Cardiol. 2015;65(13):1314-21. a randomized sham-controlled study, showed no significantly superior effect of BP reduction after 6 months from RSD. A meta-analysis of 11 controlled studies comparing RSD with optimized pharmacological treatment or sham procedure in patients with RHTN showed that RSD was not superior in reducing BP, with heterogeneity of responses in the studies, mainly due to lack of a sham control in most publications and heterogeneity in assessment of treatment adherence.163163. Pappaccogli M, Covella M, Berra E, Fulcheri C, Di Monaco S, Perlo E, et al. Effectiveness of Renal Denervation in Resistant Hypertension: A Meta-Analysis of 11 Controlled Studies. High Blood Press Cardiovasc Prev. 2018;25(2):167-76.
The development of new circumferential catheters with distal renal artery applications may promote a more complete RSD, and their effects on BP reduction have been demonstrated in patients with untreated hypertension.164164. Morganti A, Mancia G. Resistant hypertension: Renal denervation or intensified medical treatment? Eur J Intern Med. 2018;50:6-11.
The 2018 European Society of Hypertension position paper does not recommend RSD for treatment of hypertension in general but includes a recommendation of this procedure in the context of controlled clinical studies with sham procedures and optimized therapy for safety and efficacy assessment in populations with a large number of individuals.160160. Schmieder RE, Mahfoud F, Azizi M, Pathak A, Dimitriadis K, Kroon AA, et al. European Society of Hypertension position paper on renal denervation. J Hypertens. 2018;391(10137):2335-45.
Based on this evidence, RSD is currently an alternative only for patients with UC-RHTN with optimized pharmacological treatment and proven therapeutic adherence or with important drug-related adverse effects, to be always performed at referral centers trained for the procedure.164164. Morganti A, Mancia G. Resistant hypertension: Renal denervation or intensified medical treatment? Eur J Intern Med. 2018;50:6-11.
10.4. Use of Continuous Positive Airway Pressure
OSA is a clinical condition affecting more than half of the patients with RHTN9494. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. and is mainly treated with CPAP, an air compressor that applies continuous positive pressure to the patient’s airway. To date, seven randomized trials have analyzed the effect of treatment of OSA with CPAP in patients with RHTN.165165. Lozano L, Tovar JL, Sampol G, Romero O, Jurado MJ, Segarra A, et al. Continuous positive airway pressure treatment in sleep apnea patients with resistant hypertension: a randomized, controlled trial. J Hypertens. 2010 ;28(10):2161-8.
166. Pedrosa RP, Drager LF, de Paula LKG, Amaro ACS, Bortolotto LA, Lorenzi-Filho G. Effects of OSA treatment on BP in patients with resistant hypertension: a randomized trial. Chest. 2013;144(5):1487-94.
167. Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, Diaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407-15.
168. de Oliveira AC, Martinez D, Massierer D, Gus M, Goncalves SC, Ghizzoni F, et al. The antihypertensive effect of positive airway pressure on resistant hypertension of patients with obstructive sleep apnea: a randomized, double-blind, clinical trial. Am J Respir Crit Care Med. 2014;190(3):345-7.
169. Muxfeldt ES, Margallo V, Costa LM, Guimaraes G, Cavalcante AH, Azevedo JC, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension. 2015;65(4):736-42.
170. Litvin AY, Sukmarova ZN, Elfimova EM, Aksenova AV, Galitsin PV, Rogoza AN, et al. Effects of CPAP on "vascular" risk factors in patients with obstructive sleep apnea and arterial hypertension. Vasc Health Risk Manag. 2013;9:229-35.-171171. Joyeux-Faure M, Baguet JP, Barone-Rochette G, Faure P, Sosner P, Mounier-Vehier C, et al. Continuous Positive Airway Pressure Reduces Night-Time Blood Pressure and Heart Rate in Patients With Obstructive Sleep Apnea and Resistant Hypertension: The RHOOSAS Randomized Controlled Trial. Front Neurol. 2018;9:318. Except for one of these studies,170170. Litvin AY, Sukmarova ZN, Elfimova EM, Aksenova AV, Galitsin PV, Rogoza AN, et al. Effects of CPAP on "vascular" risk factors in patients with obstructive sleep apnea and arterial hypertension. Vasc Health Risk Manag. 2013;9:229-35. the others found significant reductions in BP (5 mmHg on average; one study showed reductions ≥ 10 mmHg after CPAP use).169169. Muxfeldt ES, Margallo V, Costa LM, Guimaraes G, Cavalcante AH, Azevedo JC, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension. 2015;65(4):736-42.
However, the proportion of patients who achieved the target BP (< 140/90 mmHg) with CPAP was low, possibly due to poor CPAP adherence. In clinical practice, the BP response to CPAP varies, even in patients with good adherence. A recent study showed predictive biomarkers of better BP response to CPAP in patients with RHTN.172172. Sanchez-de-la-Torre M, Khalyfa A, Sanchez-de-la-Torre A, Martinez-Alonso M, Martinez-Garcia MA, Barcelo A, et al. Precision Medicine in Patients With Resistant Hypertension and Obstructive Sleep Apnea: Blood Pressure Response to Continuous Positive Airway Pressure Treatment. J Am Coll Cardiol. 2015;66(9):1023-32. Validation and large-scale application of these biomarkers could help select better those patients who benefit most from BP reduction.
10.5. Arteriovenous Fistula
The creation of an arteriovenous fistula (AVF) can decrease BP by reducing total peripheral resistance and blood volume and inducing baroreflex inhibition and release of natriuretic peptides.173173. Bertog SC, Sobotka NA, Sobotka PA, Lobo MD, Sievert K, Vaskelyte L, et al. Percutaneous Creation of a Central Iliac Arteriovenous Anastomosis for the Treatment of Arterial Hypertension. Curr Hypertens Rep. 2018;20(3):18. In a prospective randomized controlled trial, the creation of a central iliac AVF by an implantable device in 44 patients with RHTN led to significant reductions in 24-hour office and ambulatory systolic BP compared with pharmacological treatment.174174. Lobo MD, Sobotka PA, Stanton A, Cockcroft JR, Sulke N, Dolan E, et al. Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial. Lancet. 2015;385(9978):1634-41. However, there was a high rate of complications due to ipsilateral venous stenosis, requiring intervention in the AVF group.
Further studies with a greater number of patients and with a comparison of AVF versus sham procedure are being conducted to verify the benefits of AVF in RHTN.173173. Bertog SC, Sobotka NA, Sobotka PA, Lobo MD, Sievert K, Vaskelyte L, et al. Percutaneous Creation of a Central Iliac Arteriovenous Anastomosis for the Treatment of Arterial Hypertension. Curr Hypertens Rep. 2018;20(3):18.
Referências
-
1Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-19.
-
2Modolo R, de Faria AP, Almeida A, Moreno H. Resistant or refractory hypertension: are they different? Curr Hypertens Rep. 2014;16(10):485.
-
3Modolo R, de Faria AP, Sabbatini AR, Moreno H. Resistant hypertension revisited: definition and true prevalence. J Hypertens. 2014;32(7):1546.
-
4Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, Martin JF, et al. Characteristics of resistant hypertension: ageing, body mass index, hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hypertens. 2011;25(9):532-8.
-
5Dudenbostel T, Siddiqui M, Oparil S, Calhoun DA. Refractory Hypertension: A Novel Phenotype of Antihypertensive Treatment Failure. Hypertension. 2016;67(6):1085-92.
-
6Moreno H, Jr, Coca A. Resistant and refractory hypertension: reflections on pathophysiology and terminology. Blood Press. 2012;21(4):209-10.
-
7Yugar-Toledo JC, Brunelli V, Vilela-Martin JF, Fattori A, Moreno H. Controlled Versus Uncontrolled Resistant Hypertension: Are They in the Same Bag? Curr Hypertens Rep. 2018;20(3):1-6.
-
8Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441-50.
-
9Scala LC, Magalhães LB, Machado A. Epidemiologia da hipertensão arterial sistêmica. In: Sociedade Brasileira de Cardiologia. Livro texto da SBC. 2a ed. São Paulo:Manole;2015. São Paulo; 2015. p. 780-5.
-
10Nobre F, Ribeiro AB, Mion D Jr. [Control of arterial pressure in patients undergoing anti-hypertensive treatment in Brazil: Controlar Brazil]. Arq Bras Cardiol. 2010;94(5):663-70.
-
11Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28(3):355-61.
-
12Bangalore S, Davis BR, Cushman WC, Pressel SL, Muntner PM, Calhoun DA, et al. Treatment-Resistant Hypertension and Outcomes Based on Randomized Treatment Group in ALLHAT. Am J Med. 2017;130(4):439-48 e9.
-
13Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.
-
14Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125(13):1635-42.
-
15Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52(22):1749-57.
-
16Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88(10):1099-107.
-
17Cai A, Calhoun DA. Resistant Hypertension: An Update of Experimental and Clinical Findings. Hypertension. 2017;70(1):5-9.
-
18Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.
-
19Salles GF, Cardoso CR, Muxfeldt ES. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med. 2008;168(21):2340-6.
-
20Muxfeldt ES, Cardoso CR, Salles GF. Prognostic value of nocturnal blood pressure reduction in resistant hypertension. Arch Intern Med. 2009;169(9):874-80.
-
21Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32(12):2332-40; discussion 40.
-
22Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236-41.
-
23Chung CM, Cheng HW, Chang JJ, Lin YS, Hsiao JF, Chang ST, et al. Relationship between resistant hypertension and arterial stiffness assessed by brachial-ankle pulse wave velocity in the older patient. Clin Interv Aging. 2014 Sep 5;9:1495-502.
-
24Brandao AA, Amodeo C, Alcantara C, Barbosa E, Nobre F, Pinto F, et al. I Luso-Brazilian Positioning on Central Arterial Pressure. Arq Bras Cardiol. 2017;108(2):100-8.
-
25Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic impact of baseline and serial changes in electrocardiographic left ventricular hypertrophy in resistant hypertension. Am Heart J. 2010;159(5):833-40.
-
26Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis. 2011;216(1):199-204.
-
27da Costa PM, Cortez AF, de Souza F, Mares GS, Dos Santos BDM, Muxfeldt ES. Prognostic impact of baseline urinary albumin excretion rate in patients with resistant hypertension: a prospective cohort study. J Hum Hypertens. 2018;32(2):139-49.
-
28Oliveras A, Armario P, Sierra C, Arroyo JA, Hernandez-del-Rey R, Vazquez S, et al. Urinary albumin excretion at follow-up predicts cardiovascular outcomes in subjects with resistant hypertension. Am J Hypertens. 2013;26(9):1148-54.
-
29Cortez AF, Muxfeldt ES, Cardoso CR, Salles GF. Prognostic Value of C-Reactive Protein in Resistant Hypertension. Am J Hypertens. 2016;29(8):992-1000.
-
30de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57(5):898-902.
-
31White WB. Ambulatory blood pressure monitoring as an investigative tool for characterizing resistant hypertension and its rational treatment. J Clin Hypertens (Greenwich). 2007;9(1 Suppl 1):25-30.
-
32Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-104.
-
33Malachias M, Plavnik FL, Machado CA, Malta D, Scala LCN, Fuchs S. 7th Brazilian Guideline of Arterial Hypertension: Chapter 1 - Concept, Epidemiology and Primary Prevention. Arq Bras Cardiol. 2016;107(3 Suppl 3):1-6.
-
34Mancia G, Fagard R. Guidelines for the management of hypertension and target organ damage: reply. J Hypertens. 2013; 31(12):2464-5.
-
35Nobre FMJ, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 2018;110(5 Supl.1):1-29.
-
36Silva GV, Mion D. Papel da MAPA e da MRPA na avaliação de pacientes com hipertensão de difícil controle. Rev Bras Hipertens. 2008;15(1):17-20.
-
37Muxfeldt ES, Bloch KV, Nogueira AR, Salles GF. Twenty-four hour ambulatory blood pressure monitoring pattern of resistant hypertension. Blood Press Monit. 2003;8(5):181-5.
-
38Souza WKS, Jardim PCB, Porto LB, Araújo FA, Sousa ALL, Salgado CM. Comparação e correlação entre automedida, medida casual e monitorização ambulatorial da pressão arterial. Arq Bras Cardiol. 2011;97(2):148-55.
-
39Breaux-Shropshire TL, Judd E, Vucovich LA, Shropshire TS, Singh S. Does home blood pressure monitoring improve patient outcomes? A systematic review comparing home and ambulatory blood pressure monitoring on blood pressure control and patient outcomes. Integr Blood Press Control. 2015;8:43-9.
-
40Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.
-
41Souza WKS, Jardim PCB, Brito LP, Araújo FA, Sousa ALL. Automedida da pressão arterial para o controle das cifras tensionais e para a adesão ao tratamento. Arq Bras Cardiol. 2012;98:(2)167-74.
-
42Vamsi V, Golub A, Mija P, Fekete P, Findri F, Prkacin I. Central blood pressure and pulse wave velocity in patients with resistant hypertension. Signa Vitae. 2018;14(Suppl 1):28-30.
-
43Cuspidi C, Macca G, Sampieri L, Michev I, Salerno M, Fusi V, et al. High prevalence of cardiac and extracardiac target organ damage in refractory hypertension. J Hypertens. 2001;19(11):2063-70.
-
44de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30(6):1211-6.
-
45Sim JJ, Bhandari SK, Shi J, Reynolds K, Calhoun DA, Kalantar-Zadeh K, et al. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and nonresistant hypertension. Kidney Int. 2015;88(3):622-32.
-
46Nilsson PM. Hemodynamic Aging as the Consequence of Structural Changes Associated with Early Vascular Aging (EVA). Aging Dis. 2014;5(2):109-13.
-
47Papakatsika S, Stabouli S, Antza C, Kotsis V. Early Vascular Aging: A New Target for Hypertension Treatment. Curr Pharm Des. 2016;22(1):122-6.
-
48Barbaro NR, de Araujo TM, Tanus-Santos JE, Anhe GF, Fontana V, Moreno H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed Res Int. 2015;2015:631594.
-
49Barbaro NR, Fontana V, Modolo R, De Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Pressure.2015;24(1):7-13.
-
50Camici GG, Savarese G, Akhmedov A, Luscher TF. Molecular mechanism of endothelial and vascular aging: implications for cardiovascular disease. Eur Heart J. 2015;36(48):3392-403.
-
51Harvey A, Montezano AC, Touyz RM. Vascular biology of ageing-Implications in hypertension. J Mol Cell Cardiol. 2015 Jun;83:112-21.
-
52Rizzoni D, Agabiti Rosei C, De Ciuceis C, Semeraro F, Rizzoni M, Docchio F. New Methods to Study the Microcirculation. Am J Hypertens. 2018;31(3):265-73.
-
53Lehmann MV, Schmieder RE. Remodeling of retinal small arteries in hypertension. Am J Hypertens. 2011;24(12):1267-73.
-
54Cecelja M, Chowienczyk P. Molecular Mechanisms of Arterial Stiffening. Pulse (Basel). 2016;4(1):43-8.
-
55Mikael LR, Paiva AMG, Gomes MM, Sousa ALL, Jardim P, Vitorino PVO, et al. Vascular Aging and Arterial Stiffness. Arq Bras Cardiol. 2017;109(3):253-8.
-
56Mozos I, Malainer C, Horbanczuk J, Gug C, Stoian D, Luca CT, et al. Inflammatory Markers for Arterial Stiffness in Cardiovascular Diseases. Front Immunol. 2017;8:1058.
-
57Balduino Mendes AB, Giollo-Junior LT, de Andrade DO, Gregorio ML, Yugar-Toledo JC, Vilela-Martin JF. How to Investigate the Vascular Changes in Resistant Hypertension. Curr Hypertens Rev. 2016;12(2):139-47.
-
58Virdis A. Arterial Stiffness and Vascular Aging: From Pathophysiology to Treatment, with a Look at the Future. High Blood Press Cardiovasc Prev. 2018;25(2):135-6.
-
59Joly L. Arterial stiffness and cognitive function. Geriatr Psychol Neuropsychiatr Vieil. 2017;15(1):83-8.
-
60Hughes TM, Wagenknecht LE, Craft S, Mintz A, Heiss G, Palta P, et al. Arterial stiffness and dementia pathology: Atherosclerosis Risk in Communities (ARIC)-PET Study. Neurology. 2018;90(14):e1248-e56.
-
61Muntner P, Davis BR, Cushman WC, Bangalore S, Calhoun DA, Pressel SL, et al. Treatment-resistant hypertension and the incidence of cardiovascular disease and end-stage renal disease: results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2014;64(5):1012-21.
-
62Lotufo PA, Pereira AC, Vasconcellos PS, Santos IS, Mill JG, Bensenor IM. Resistant Hypertension: Risk Factors, Subclinical Atherosclerosis, and Comorbidities Among Adults—The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). J Clin Hypertens. 2015;17(1):74-80.
-
63Iadecola C. Hypertension and Dementia. Hypertension. 2014;64(1):3-5.
-
64Laurent S, Boutouyrie P. The structural factor of hypertension: large and small artery alterations. Circ Res. 2015;116(6):1007-21.
-
65Howard VJ, Tanner RM, Anderson A, Irvin MR, Calhoun DA, Lackland DT, et al. Apparent Treatment-resistant Hypertension Among Individuals with History of Stroke or Transient Ischemic Attack. Am J Med. 2015;128(7):707-14.e2.
-
66Hong J-H, Sohn S-I, Kwak J, Yoo J, Ahn SJ, Woo SJ, et al. Retinal artery occlusion and associated recurrent vascular risk with underlying etiologies. PLoS One. 2017;12(6):e0177663.
-
67Hong D, Stradling D, Dastur CK, Akbari Y, Groysman L, Al-Khoury L, et al. Resistant Hypertension after Hypertensive Intracerebral Hemorrhage Is Associated with More Medical Interventions and Longer Hospital Stays without Affecting Outcome. Front Neurol. 2017;8:184.
-
68Chen Y, Shen F, Liu J, Yang GY. Arterial stiffness and stroke: de-stiffening strategy, a therapeutic target for stroke. Stroke Vasc Neurol. 2017;2(2):65-72.
-
69Cuspidi C, Vaccarella A, Negri F, Sala C. Resistant hypertension and left ventricular hypertrophy: an overview. J Am Soc Hypertens. 2010;4(6):319-24.
-
70Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29(1):1-6.
-
71Muxfeldt ES, Salles GF. Pulse pressure or dipping pattern: which one is a better cardiovascular risk marker in resistant hypertension? J Hypertens. 2008;26(5):878-84.
-
72Modolo R, de Faria AP, Paganelli MO, Sabbatini AR, Barbaro NR, Nascimento BB, et al. Predictors of silent myocardial ischemia in resistant hypertensive patients. Am J Hypertens. 2015;28(2):200-7.
-
73Muxfeldt ES, de Souza F, Margallo VS, Salles GF. Cardiovascular and renal complications in patients with resistant hypertension. Curr Hypertens Rep. 2014;16(9):471.
-
74Nadruz W, Shah AM, Solomon SD. Diastolic Dysfunction and Hypertension. Med Clin North Am. 2017;101(1):7-17.
-
75Rodrigues CIS CR, Almeida FA. Hipertensao arterial resistente. In: Moura LRR, Alves MAR, Santos DR, Pecoits Filho R. Tratado de Nefrologia. São Paulo: Atheneu; 2018.
-
76Summary of Recommendation Statements. Kidney Int Suppl.2013;3(1):5-14.
-
77Taler SJ, Textor SC, Augustine JE. Resistant hypertension: comparing hemodynamic management to specialist care. Hypertension. 2002;39(5):982-8.
-
78Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168(11):1159-64.
-
79Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, et al. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54(3):475-81.
-
80Agarwal R. Resistant hypertension and the neglected antihypertensive: sodium restriction. Nephrol Dial Transplant. 2012;27(11):4041-5.
-
81Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.
-
82Calhoun DA. Refractory and Resistant Hypertension: Antihypertensive Treatment Failure versus Treatment Resistance. Korean Circ J. 2016;46(5):593-600.
-
83Eirin A, Textor SC, Lerman LO. Emerging concepts for patients with treatment-resistant hypertension. Trends Cardiovasc Med. 2016;26(8):700-6.
-
84Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004;22(11):2217-26.
-
85Laragh JH, Sealey JE. The Plasma Renin Test Reveals the Contribution of Body Sodium-Volume Content (V) and Renin–Angiotensin (R) Vasoconstriction to Long-Term Blood Pressure. Am J Hypertens. 2011;24(11):1164-80.
-
86Calhoun DA, Booth JN, 3rd, Oparil S, Irvin MR, Shimbo D, Lackland DT, et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63(3):451-8.
-
87Judd EK, Calhoun DA, Warnock DG. Pathophysiology and Treatment of Resistant Hypertension: The Role of Aldosterone and Amiloride-Sensitive Sodium Channels. Semin Nephrol. 2014;34(5):532-9.
-
88Tsioufis C, Kordalis A, Flessas D, Anastasopoulos I, Tsiachris D, Papademetriou V, et al. Pathophysiology of resistant hypertension: the role of sympathetic nervous system. Int J Hypertens. 2011;2011:642416.
-
89Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA. Refractory Hypertension: Evidence of Heightened Sympathetic Activity as a Cause of Antihypertensive Treatment Failure. Hypertension. 2015;66(1):126-33.
-
90Mahmud A, Mahgoub M, Hall M, Feely J. Does aldosterone-to-renin ratio predict the antihypertensive effect of the aldosterone antagonist spironolactone? Am J Hypertens. 2005;18(12 Pt 1):1631-5.
-
91Pimenta E, Calhoun DA. Resistant hypertension and aldosteronism. Curr Hypertens Rep. 2007;9(5):353-9.
-
92Wang C, Xiong B, Huang J. Efficacy and Safety of Spironolactone in Patients with Resistant Hypertension: A Meta-analysis of Randomised Controlled Trials. Heart Lung Circ. 2016;25(10):1021-30.
-
93Jain S, Khera R, Corrales-Medina VF, Townsend RR, Chirinos JA. "Inflammation and arterial stiffness in humans". Atherosclerosis. 2014;237(2):381-90.
-
94Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7.
-
95Florczak E, Prejbisz A, Szwench-Pietrasz E, Sliwinski P, Bielen P, Klisiewicz A, et al. Clinical characteristics of patients with resistant hypertension: the RESIST-POL study. J Hum Hypertens. 2013;27(11):678-85.
-
96de Faria AP, Modolo R, Fontana V, Moreno H. Adipokines: novel players in resistant hypertension. J Clin Hypertens (Greenwich). 2014;16(10):754-9.
-
97Lacerda L, Faria AP, Fontana V, Moreno H, Sandrim V. Role of MMP-2 and MMP-9 in resistance to drug therapy in patients with resistant hypertension. Arq Bras Cardiol. 2015;105(2):168-75.
-
98de Faria AP, Ritter AM, Sabbatini AR, Correa NB, Brunelli V, Modolo R, et al. Deregulation of Soluble Adhesion Molecules in Resistant Hypertension and Its Role in Cardiovascular Remodeling. Circ J. 2016;80(5):1196-201.
-
99Sabbatini AR, Barbaro NR, de Faria AP, Ritter AMV, Modolo R, Correa NB, et al. Matrix metalloproteinase-2 -735C/T polymorphism is associated with resistant hypertension in a specialized outpatient clinic in Brazil. Gene. 2017;620:23-9.
-
100Lacchini R, Sabha M, Coeli FB, Favero FF, Yugar-Toledo J, Izidoro-Toledo TC, et al. T allele of -344 C/T polymorphism in aldosterone synthase gene is not associated with resistant hypertension. Hypertens Res. 2009;32(2):159-62.
-
101Yugar-Toledo JC, Martin JF, Krieger JE, Pereira AC, Demacq C, Coelho OR, et al. Gene variation in resistant hypertension: multilocus analysis of the angiotensin 1-converting enzyme, angiotensinogen, and endothelial nitric oxide synthase genes. DNA Cell Biol. 2011;30(8):555-64.
-
102Figueiredo VN, Yugar-Toledo JC, Martins LC, Martins LB, de Faria AP, de Haro Moraes C, et al. Vascular stiffness and endothelial dysfunction: Correlations at different levels of blood pressure. Blood Press. 2012;21(1):31-8.
-
103Quinaglia T, Martins LC, Figueiredo VN, Santos RC, Yugar-Toledo JC, Martin JF, et al. Non-dipping pattern relates to endothelial dysfunction in patients with uncontrolled resistant hypertension. J Hum Hypertens. 2011;25(11):656-64.
-
104Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18(11):1422-8.
-
105Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.
-
106Braam B, Taler SJ, Rahman M, Fillaus JA, Greco BA, Forman JP, et al. Recognition and Management of Resistant Hypertension. Clin J Am Soc Nephrol. 2017;12(3):524-35.
-
107Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, et al. Association of obstructive sleep apnea with hypertension: A systematic review and meta-analysis. J Glob Health. 2018;8(1):010405.
-
108Drager LF, Bortolotto LA, Lorenzi MC, Figueiredo AC, Krieger EM, Lorenzi-Filho G. Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. 2005;172(5):613-8.
-
109Senaratna CV, Perret JL, Matheson MC, Lodge CJ, Lowe AJ, Cassim R, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2017;36:116-24.
-
110Fava C, Dorigoni S, Dalle Vedove F, Danese E, Montagnana M, Guidi GC, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea a systematic review and meta-analysis. Chest. 2014;145(4):762-71.
-
111Guo J, Sun Y, Xue LJ, Huang ZY, Wang YS, Zhang L, et al. Effect of CPAP therapy on cardiovascular events and mortality in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath. 2016;20(3):965-74.
-
112Horl MP, Horl WH. Hemodialysis-associated hypertension: pathophysiology and therapy. Am J Kidney Dis. 2002;39(2):227-44.
-
113Wolley MJ, Stowasser M. Resistant Hypertension and Chronic Kidney Disease: a Dangerous Liaison. Curr Hypertens Rep. 2016;18(5):36.
-
114van Jaarsveld BC, Krijnen P, Pieterman H, Derkx FH, Deinum J, Postma CT, et al. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med. 2000;342(14):1007-14.
-
115Bavishi C, de Leeuw PW, Messerli FH. Atherosclerotic Renal Artery Stenosis and Hypertension: Pragmatism, Pitfalls, and Perspectives. Am J Med. 2016;129(6):635 e5- e14.
-
116Van der Niepen P, Rossignol P, Lengele JP, Berra E, Sarafidis P, Persu A. Renal Artery Stenosis in Patients with Resistant Hypertension: Stent It or Not? Curr Hypertens Rep. 2017;19(1):5.
-
117Mulherin JL, Jr., Edwards WH. Alternative methods of renal revascularization. Ann Surg. 1987;205(6):740-6.
-
118Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.
-
119Kline GA, Prebtani APH, Leung AA, Schiffrin EL. Primary aldosteronism: a common cause of resistant hypertension. CMAJ. 2017;189(22):E773-E8.
-
120Young JWF, Calhoun DA, Lenders JWM, Stowasser M, Textor SC. Screening for Endocrine Hypertension: An Endocrine Society Scientific Statement. Endocrine Rev. 2017;38(2):103-22.
-
121Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
-
122Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005;366(9486):665-75.
-
123Pillai S, Gopalan V, Smith RA, Lam AK. Updates on the genetics and the clinical impacts on phaeochromocytoma and paraganglioma in the new era. Crit Rev Oncol Hematol. 2016;100:190-208.
-
124Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth. 2017;31(4):1427-39.
-
125Saito I, Ito K, Saruta T. Hypothyroidism as a cause of hypertension. Hypertension. 1983;5(1):112-5.
-
126Levey GS, Klein I. Catecholamine-thyroid hormone interactions and the cardiovascular manifestations of hyperthyroidism. Am J Med. 1990;88(6):642-6.
-
127Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-42.
-
128Pappachan JM, Tun NN, Arunagirinathan G, Sodi R, Hanna FWF. Pheochromocytomas and Hypertension. Curr Hypertens Rep. 2018;20(1):3.
-
129Kenny D, Polson JW, Martin RP, Paton JF, Wolf AR. Hypertension and coarctation of the aorta: an inevitable consequence of developmental pathophysiology. Hypertens Res. 2011;34(5):543-7.
-
130Cohen JB. Hypertension in Obesity and the Impact of Weight Loss. Curr Cardiol Rep. 2017;19(10):98.
-
131Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure : factors associated with lack of blood pressure control in the community. Hypertension. 2000;36(4):594-9.
-
132Bramlage P, Pittrow D, Wittchen HU, Kirch W, Boehler S, Lehnert H, et al. Hypertension in overweight and obese primary care patients is highly prevalent and poorly controlled. Am J Hypertens. 2004;17(10):904-10.
-
133Aucott L, Poobalan A, Smith WC, Avenell A, Jung R, Broom J. Effects of weight loss in overweight/obese individuals and long-term hypertension outcomes: a systematic review. Hypertension. 2005;45(6):1035-41.
-
134Schiavon CA, Bersch-Ferreira AC, Santucci EV, Oliveira JD, Torreglosa CR, Bueno PT, et al. Effects of Bariatric Surgery in Obese Patients With Hypertension: The GATEWAY Randomized Trial (Gastric Bypass to Treat Obese Patients With Steady Hypertension). Circulation. 2018;137(11):1132-42.
-
135Edwards DG, Farquhar WB. Vascular effects of dietary salt. Curr Opin Nephrol Hypertens. 2015;24(1):8-13.
-
136White WB, Turner JR, Sica DA, Bisognano JD, Calhoun DA, Townsend RR, et al. Detection, evaluation, and treatment of severe and resistant hypertension. In: Congress of American Society of Hypertension Interactive (forum) Bethesda, MD, October 10th 2013. Proceedings. J Am Soc Hypertens. 2014;8(10):743-57.
-
137He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
-
138Wildman RP, Gu D, Muntner P, Huang G, Chen J, Duan X, et al. Alcohol intake and hypertension subtypes in Chinese men. J Hypertens. 2005;23(4):737-43.
-
139Sarwar MS, Islam MS, Al Baker SM, Hasnat A. Resistant hypertension: underlying causes and treatment. Drug Res (Stuttg). 2013;63(5):217-23.
-
140Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Publ Health. 2017;2(2):e108-e20.
-
141Ribeiro F, Costa R, Mesquita-Bastos J. Exercise training in the management of patients with resistant hypertension. World J Cardiol. 2015;7(2):47-51.
-
142Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W, Westhoff TH. Aerobic exercise reduces blood pressure in resistant hypertension. Hypertension. 2012;60(3):653-8.
-
143Guimaraes GV, de Barros Cruz LG, Fernandes-Silva MM, Dorea EL, Bocchi EA. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: a randomized controlled trial (HEx trial). Int J Cardiol. 2014;172(2):434-41.
-
144Santos LP, Moraes RS, Vieira PJ, Ash GI, Waclawovsky G, Pescatello LS, et al. Effects of aerobic exercise intensity on ambulatory blood pressure and vascular responses in resistant hypertension: a crossover trial. J Hypertens. 2016;34(7):1317-24.
-
145Kruk PJ, Nowicki M. Effect of the physical activity program on the treatment of resistant hypertension in primary care. Prim Health Care Res Dev. 2018; 22:1-9.
-
146Cruz LG, Bocchi EA, Grassi G, Guimaraes GV. Neurohumoral and Endothelial Responses to Heated Water-Based Exercise in Resistant Hypertensive Patients. Circ J. 2017;81(3):339-45.
-
147Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950-8.
-
148Narayan P, Doumas M, Kumar A, Faselis CJ, Myers JN, Pittaras A, et al. Impact of Cardiorespiratory Fitness on Mortality in Black Male Veterans With Resistant Systemic Hypertension. Am J Cardiol. 2017;120(9):1568-71.
-
149Povoa R, Barroso WS, Brandao AA, Jardim PC, Barroso O, Passarelli O, Jr., et al. I brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
-
150Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115.
-
151Salles GF, Cardoso CR, Fonseca LL, Fiszman R, Muxfeldt ES. Prognostic significance of baseline heart rate and its interaction with beta-blocker use in resistant hypertension: a cohort study. Am J Hypertens. 2013;26(2):218-26.
-
152Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059-68.
-
153Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159-66.
-
154Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, et al. The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies. Am J Hypertens. 2015;28(11):1376-85.
-
155Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet Diabetes Endocrinol. 2018;6(6):464-75.
-
156van Kleef MEAM, Bates MC, Spiering W. Endovascular Baroreflex Amplification for Resistant Hypertension. Curr Hypertens Report. 2018;20(5):46.
-
157Bisognano JD, Bakris G, Nadim MK, Sanchez L, Kroon AA, Schafer J, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58(7):765-73.
-
158Heusser K, Tank J, Brinkmann J, Menne J, Kaufeld J, Linnenweber-Held S, et al. Acute Response to Unilateral Unipolar Electrical Carotid Sinus Stimulation in Patients with Resistant Arterial Hypertension. Hypertension. 2016;67(3):585-91.
-
159Wallbach M, Lehnig LY, Schroer C, Luders S, Bohning E, Muller GA, et al. Effects of Baroreflex Activation Therapy on Ambulatory Blood Pressure in Patients With Resistant Hypertension. Hypertension. 2016;67(4):701-9.
-
160Schmieder RE, Mahfoud F, Azizi M, Pathak A, Dimitriadis K, Kroon AA, et al. European Society of Hypertension position paper on renal denervation. J Hypertens. 2018;391(10137):2335-45.
-
161Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circ Res. 2015;116(6):1074-95.
-
162Bakris GL, Townsend RR, Flack JM, Brar S, Cohen SA, D'Agostino R, et al. 12-month blood pressure results of catheter-based renal artery denervation for resistant hypertension: the SYMPLICITY HTN-3 trial. J Am Coll Cardiol. 2015;65(13):1314-21.
-
163Pappaccogli M, Covella M, Berra E, Fulcheri C, Di Monaco S, Perlo E, et al. Effectiveness of Renal Denervation in Resistant Hypertension: A Meta-Analysis of 11 Controlled Studies. High Blood Press Cardiovasc Prev. 2018;25(2):167-76.
-
164Morganti A, Mancia G. Resistant hypertension: Renal denervation or intensified medical treatment? Eur J Intern Med. 2018;50:6-11.
-
165Lozano L, Tovar JL, Sampol G, Romero O, Jurado MJ, Segarra A, et al. Continuous positive airway pressure treatment in sleep apnea patients with resistant hypertension: a randomized, controlled trial. J Hypertens. 2010 ;28(10):2161-8.
-
166Pedrosa RP, Drager LF, de Paula LKG, Amaro ACS, Bortolotto LA, Lorenzi-Filho G. Effects of OSA treatment on BP in patients with resistant hypertension: a randomized trial. Chest. 2013;144(5):1487-94.
-
167Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, Diaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407-15.
-
168de Oliveira AC, Martinez D, Massierer D, Gus M, Goncalves SC, Ghizzoni F, et al. The antihypertensive effect of positive airway pressure on resistant hypertension of patients with obstructive sleep apnea: a randomized, double-blind, clinical trial. Am J Respir Crit Care Med. 2014;190(3):345-7.
-
169Muxfeldt ES, Margallo V, Costa LM, Guimaraes G, Cavalcante AH, Azevedo JC, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension. 2015;65(4):736-42.
-
170Litvin AY, Sukmarova ZN, Elfimova EM, Aksenova AV, Galitsin PV, Rogoza AN, et al. Effects of CPAP on "vascular" risk factors in patients with obstructive sleep apnea and arterial hypertension. Vasc Health Risk Manag. 2013;9:229-35.
-
171Joyeux-Faure M, Baguet JP, Barone-Rochette G, Faure P, Sosner P, Mounier-Vehier C, et al. Continuous Positive Airway Pressure Reduces Night-Time Blood Pressure and Heart Rate in Patients With Obstructive Sleep Apnea and Resistant Hypertension: The RHOOSAS Randomized Controlled Trial. Front Neurol. 2018;9:318.
-
172Sanchez-de-la-Torre M, Khalyfa A, Sanchez-de-la-Torre A, Martinez-Alonso M, Martinez-Garcia MA, Barcelo A, et al. Precision Medicine in Patients With Resistant Hypertension and Obstructive Sleep Apnea: Blood Pressure Response to Continuous Positive Airway Pressure Treatment. J Am Coll Cardiol. 2015;66(9):1023-32.
-
173Bertog SC, Sobotka NA, Sobotka PA, Lobo MD, Sievert K, Vaskelyte L, et al. Percutaneous Creation of a Central Iliac Arteriovenous Anastomosis for the Treatment of Arterial Hypertension. Curr Hypertens Rep. 2018;20(3):18.
-
174Lobo MD, Sobotka PA, Stanton A, Cockcroft JR, Sulke N, Dolan E, et al. Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial. Lancet. 2015;385(9978):1634-41.
-
This statement should be cited as:Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES, et al. Brazilian Position Statement on Resistant Hypertension – 2020. Arq Bras Cardiol. 2020; 114(3):576-596
-
Note: These statements are for information purposes and are not to replace the clinical judgment of a physician, who must ultimately determine the appropriate treatment for each patient.
-
ErratumIn the figure 1 of the Portuguese version, where "hipertensão segundária" is mentioned, the correct is "Hipertensão arterial pseudorresistente". In the English version, where "abnormal" is mentioned, right side of the figure 1, the correct is "normal".
Publication Dates
-
Publication in this collection
06 Apr 2020 -
Date of issue
May-Jun 2020