| Declaration of potential conflict of interests of authors/collaborators of the Brazilian Guidelines of Hypertension – 2020 | |||||||
|---|---|---|---|---|---|---|---|
| If, within the last 3 years, the author/collaborator of the guideline: | |||||||
| Names of guideline collaborators | Participated in clinical and/or experimental studies sponsored by pharmaceutical or equipment companies related to this statement | Spoke at events or activities sponsored by industry related to this statement | Was (is) a member of a board of advisors or a board of directors of a pharmaceutical or equipment industry | Participated in normative committees of scientific research sponsored by industry | Received personal or institutional funding from industry | Wrote scientific papers in journals sponsored by industry | Owns stocks in industry |
| Alexandre Alessi | No | No | No | No | No | No | No |
| Alexandre Jorge Gomes de Lucena | No | No | No | No | No | No | No |
| Alvaro Avezum | No | No | No | No | No | No | No |
| Ana Luiza Lima Sousa | No | No | No | No | No | No | No |
| Andréa Araujo Brandão | No | Abbott, Daiichi Sankyo, EMS, Libbs, Novartis, Medley, Merck, Servier | No | No | Servier | Abbott, Daiichi Sankyo, EMS, Libbs, Novartis, Medley, Merck, Servier | No |
| Andrea Pio-Abreu | No | No | No | No | No | No | No |
| Andrei Carvalho Sposito | No | No | No | No | No | No | No |
| Angela Maria Geraldo Pierin | No | No | No | No | No | No | No |
| Annelise Machado Gomes de Paiva | No | No | No | No | No | No | No |
| Antonio Carlos de Souza Spinelli | No | Merck, Torrent, Boerhinger, Sandoz | No | No | EMS, Aché, Torrent | No | No |
| Armando da Rocha Nogueira | No | No | No | No | No | No | No |
| Audes Diógenes de Magalhães Feitosa | No | EMS, Servier, Sandoz, Merck, Medtronic e Omron | Omron | No | No | EMS, Servier e Omron | No |
| Bruna Eibel | No | No | No | No | No | No | No |
| Carlos Alberto Machado | No | No | Biolab, Omron | No | No | No | No |
| Carlos Eduardo Poli-de-Figueiredo | No | No | No | Fresenius | Centro de Pesquisa Clínico da PUCRS, Baxter, Fresenius, Alexion, AstraZeneca. | No | No |
| Celso Amodeo | No | Novartis, NovoNordisk, EMS, ACHE | Montecorp Farmasa | No | No | ACHE, Montecorp Farmasa | No |
| Cibele Isaac Saad Rodrigues | No | No | No | No | No | No | No |
| Cláudia Lúcia de Moraes Forjaz | No | No | No | No | No | No | No |
| Claudia Regina de Oliveira Zanini | No | No | No | No | No | No | No |
| Cristiane Bueno de Souza | No | No | No | No | No | No | No |
| Decio Mion Junior | No | Zodiac | No | No | No | Zodiac | No |
| Dilma do Socorro Moraes de Souza | No | No | No | No | No | No | No |
| Eduardo Augusto Fernandes Nilson | No | No | No | No | No | No | No |
| Eduardo Costa Duarte Barbosa | No | Servier, EMS | No | No | No | No | No |
| Elisa Franco de Assis Costa | No | No | No | No | Abbot Nutrition, Nestlé Health Sciences, Aché, Sandoz, Nutricia | Abboot Nutrition | No |
| Elizabete Viana de Freitas | No | No | No | No | No | No | No |
| Elizabeth da Rosa Duarte | No | No | No | No | Sim, Ache, Bayer, Novartis, Torrent, Servier. | No | No |
| Elizabeth Silaid Muxfeldt | No | No | No | No | No | No | No |
| Emilton Lima Júnior | No | Servier, Novo Nordisk, Bayer, Biolab, Amgem | No | Servier | No | No | No |
| Erika Maria Gonçalves Campana | No | No | No | No | Servier | Servier | No |
| Evandro José Cesarino | No | No | No | No | No | No | No |
| Fábio Argenta | No | No | No | No | Novartis, Bayer, Torrent, Lilly, Boehringer | No | No |
| Fernanda Marciano Consolim-Colombo | No | Merck, Ache, Daiichi | No | No | Não | No | No |
| Fernanda Spadotto Baptista | No | No | No | No | Não | No | No |
| Fernando Antonio de Almeida | No | No | No | No | Não | No | No |
| Fernando Nobre | No | Libbs, Cristália | No | No | Libbs, Novartis, Servier, Baldacci | Daichi Sankio, Libbs, Novartis, Biolab, Servier, Baldacci | No |
| Flávio Antonio de Oliveira Borelli | No | No | No | No | No | No | No |
| Flávio Danni Fuchs | No | No | No | No | No | No | No |
| Frida Liane Plavnik | No | No | No | No | No | No | No |
| Gil Fernando Salles | No | No | No | No | No | No | No |
| Gilson Soares Feitosa | No | No | No | No | No | No | No |
| Giovanio Vieira da Silva | No | Ache | No | No | No | Ache | No |
| Grazia Guerra | No | No | No | No | No | No | No |
| Heitor Moreno Júnior | No | No | No | No | No | No | No |
| Helius Carlos Finimundi | No | No | No | No | No | No | No |
| Isabel Cristina Britto Guimarães | No | No | No | No | No | No | No |
| Isabela de Carlos Back | No | No | No | No | No | No | No |
| João Bosco de Oliveira Filho | No | No | No | No | Novartis, Bristol, AztraZeneca | No | No |
| João Roberto Gemelli | No | No | No | No | Boeringher, Libbs | No | Boeringher, Libbs |
| José Fernando Vilela-Martin | No | No | No | No | No | No | No |
| Jose Geraldo Mill | No | No | No | No | No | No | No |
| José Marcio Ribeiro | No | No | No | No | No | No | No |
| Juan Carlos Yugar-Toledo | No | No | No | No | No | No | No |
| Leda A. Daud Lotaif | No | No | No | No | No | No | No |
| Lilian Soares da Costa | No | No | No | No | No | No | No |
| Lucélia Batista Neves Cunha Magalhães | No | No | No | No | No | No | No |
| Luciano Ferreira Drager | No | Aché, Biolab, Boehringer, Merck | ResMed | No | No | Aché, Biolab, Merck | No |
| Luis Cuadrado Martin | No | No | No | No | No | No | No |
| Luiz Aparecido Bortolotto | No | Servier, Novonordisk | No | No | No | No | No |
| Luiz César Nazário Scala | No | No | No | No | No | No | No |
| Madson Q. Almeida | No | No | No | No | No | No | No |
| Marcia Maria Godoy Gowdak | No | No | No | No | No | No | No |
| Marcia Regina Simas Torres Klein | No | No | No | No | No | No | No |
| Marco Antônio Mota-Gomes | Omron, Beliva | No | Omron, Libbs | No | No | Omron, Libbs | No |
| Marcus Vinícius Bolívar Malachias | No | Libbs, Biolab | No | No | No | Libbs. Biolab | No |
| Maria Cristina Caetano Kuschnir | No | No | No | No | No | No | No |
| Maria Eliane Campos Magalhães | No | No | No | No | No | No | No |
| Maria Eliete Pinheiro | No | No | No | No | No | No | No |
| Mario Fritsch Toros Neves | No | Servier | No | No | No | No | No |
| Mario Henrique Elesbão de Borba | No | EMS | No | No | No | No | No |
| Nelson Dinamarco Ludovico | No | Não | No | No | No | No | No |
| Osni Moreira Filho | No | Biolab, Servier | No | No | No | No | No |
| Oswaldo Passarelli Júnior | No | No | No | No | No | No | No |
| Otávio Rizzi Coelho | No | Daichi-Sankyo, Boehringer | No | Daichi-Sankyo, BAYER, Novo-Nordisk | No | Sanofi, Takeda, AstraZeneca, Daichi-Sankyo, Bayer | No |
| Paulo César Brandão Veiga Jardim | No | Servier, Libbs, EMS | No | No | No | Servier, Libbs | No |
| Priscila Valverde Vitorino | No | No | No | No | No | No | No |
| Renault Mattos Ribeiro Júnior | No | Daiichi Sankyo | No | No | No | No | No |
| Roberto Dischinger Miranda | No | EMS, Boehringher | No | No | No | EMS, Sanofi, Servier | No |
| Roberto Esporcatte | No | EMS | No | No | No | No | No |
| Roberto Franco | No | No | No | No | No | No | No |
| Rodrigo Pedrosa | No | No | No | No | No | No | No |
| Rogerio Andrade Mulinari | No | No | No | No | No | No | No |
| Rogério Baumgratz de Paula | No | No | No | No | No | No | No |
| Rogerio Toshiro Passos Okawa | No | No | No | No | No | No | No |
| Ronaldo Fernandes Rosa | No | No | No | No | No | No | No |
| Rui Manuel dos Santos Póvoa | No | No | No | No | No | No | No |
| Sandra Fuchs | No | No | No | No | No | No | No |
| Sandra Lia do Amaral | No | No | No | No | No | No | No |
| Sebastião R. Ferreira-Filho | No | No | No | No | No | No | No |
| Sergio Emanuel Kaiser | Engage, Alecardio, RED-HF, Odissey-Outcomes, SELECT | Amgen, Novo Nordisk, Novartis, astrazeneca, Momenta Farma, Daiichi-Sankyo, Pfizer, Baldacci | No | No | No | Novartis, Momenta Farma, Farmasa, EMS | No |
| Thiago de Souza Veiga Jardim | No | AstraZeneca, Torrent, Meck, Bayer | No | No | No | No | No |
| Vanildo Guimarães | No | Boehringer, Novartis, Sandoz | No | No | No | No | No |
| Vera H. Koch | No | No | No | No | No | No | No |
| Weimar Kunz Sebba Barroso de Souza | Ministério da Saúde, Sociedade Europeia de Hipertensão Arterial, Artery Society, EMS | EMS, Libbs, Sandoz, Servier, Cardios, Omron | Omron | No | EMS, Servier | EMS, Servier, Omron | No |
| Wille Oigman | No | No | No | No | No | No | No |
| Wilson Nadruz | No | No | No | No | No | No | No |
List of Abbreviations
| ABI | ankle-brachial index | GBD | global burden diseases |
|---|---|---|---|
| ABPM | ambulatory blood pressure monitoring | GH | growth hormone |
| AC | arm circumference | GRS | global risk score |
| ACEI | angiotensin-converting enzyme inhibitor | GST | gait speed test |
| ADL | activity of daily living | HBP | high blood pressure |
| AE | adverse event | HBPM | home blood pressure monitoring |
| AF | atrial fibrillation | HC | hypertensive crisis |
| Aix | augmentation index | HDL | high-density lipoprotein |
| AMI | acute myocardial infarction | HE | hypertensive emergency |
| APA | aldosterone-producing adenomas | HELPP | hemolysis, elevated liver enzymes, low platelets |
| APE | acute pulmonary edema | HF | heart failure |
| ARB | angiotensin II AT1 receptor blocker | HFpEF | heart failure with preserved ejection fraction |
| ASA | acetylsalicylic acid | HFrEF | heart failure with reduced ejection fraction |
| BB | beta-blockers | HPLC | high-performance liquid chromatography |
| BE | blinding effect | HR | heart rate |
| BMI | body mass index | hs-TnT | high-sensitivity troponin T |
| BP | blood pressure | HT | hypertension |
| CAD | coronary artery disease | HTPC | hypertensive pseudocrisis |
| CCB | calcium channel blocker | HU | hypertensive urgency |
| cfPWV | carotid-femoral pulse wave velocity | ICU | intensive care unit |
| CGA | comprehensive geriatric assessment | IGF-1 | insulin-like growth factor-1 |
| CHW | community health worker | IV | intravenous |
| CKD | chronic kidney disease | LE | level of evidence |
| CO | cardiac output | LLs | lower limbs |
| CRP | C-reactive protein | LR | level of recommendation |
| CT | computed tomography | LSC | lifestyle change |
| CV | cardiovascular | MH | masked hypertension |
| CVD | cerebrovascular disease | MNR | magnetic nuclear resonance |
| CVD | cardiovascular disease | MOD | multi-organ damage |
| CVRF | cardiovascular risk factor | MS | metabolic syndrome |
| DALYs | disability-adjusted life years | NB | newborn |
| DBP | diastolic blood pressure | NCD | noncommunicable disease |
| DIU | diuretics | NE | norepinephrine |
| DM | diabetes mellitus | NIHSS | National Institute of Health Stroke Scale |
| EF | ejection fraction | NO | nitric oxide |
| eGFR | estimated glomerular filtration rate | NOO- | peroxynitrite |
| eNOS | endothelial nitric oxide synthase | NPT | nonpharmacological treatment |
| EOD | end-organ damage | NT-proBNP | N-terminal pro b-type natriuretic peptide |
| FMD | fibromuscular dysplasia | NTG | nitroglycerin |
| FMD | flow-mediated dilation | OH | orthostatic hypotension |
| OSA | obstructive sleep apnea | RHT | resistant hypertension |
| PE | pre-eclampsia | RVH | renovascular hypertension |
| PEF | preserved ejection fraction | SBP | systolic blood pressure |
| PHEO | pheochromocytoma | SHT | sustained hypertension |
| PNS | Brazilian National Health Survey | SMBP | self-measured blood pressure |
| PNS | parasympathetic nervous system | SNP | sodium nitroprusside |
| POAD | peripheral occlusive atherosclerotic disease | SNS | sympathetic nervous system |
| PPH | postprandial hypotension | SUS | Brazilian Unified Health System |
| PRA | plasma renin activity | T4 | thyroxine |
| PVR | peripheral vascular resistance | TG | triglycerides |
| PWV | pulse wave velocity | TNT | true normotension |
| R/S | religiosity and spirituality | TSH | thyroid-stimulating hormone |
| RAAS | renin-angiotensin-aldosterone system | UAOBPM | unobserved automated office blood pressure measurement |
| RAS | renal artery stenosis | UN | United Nations |
| RCT | randomized controlled trial | WCE | white-coat effect |
| REF | reduced ejection fraction | WCH | white coat hypertension |
| RF | risk factors | WHO | World Health Organization |
| RfHT | refractory hypertension | YLL | years of life lost |
Content
1. Definition, Epidemiology, and Primary Prevention 528
1.1 Definition of Hypertension 528
1.2. Impact of Hypertension on Cardiovascular Diseases 528
1.3. Risk Factors for Hypertension 528
1.3.1. Genetics 528
1.3.2. Age 528
1.3.3. Sex 528
1.3.4. Race/Ethnicity 528
1.3.5. Overweight/Obesity 528
1.3.6. Sodium and Potassium Intake 528
1.3.7. Sedentary lifestyle 529
1.3.8. Alcohol 529
1.3.9. Socioeconomic Factors 529
1.3.10. Other Risk Factors for High BP 529
1.3.11. Obstructive Sleep Apnea (OSA) 529
1.3.12. Global Epidemiological Data 529
1.4. Prevalence of Hypertension in Brazil 529
1.5. Primary Prevention 530
1.5.1. Introduction 530
1.5.2. Weight Control (LR: I; LEE: A) 530
1.5.3. Healthy Diet (LR: I; LE: A) 530
1.5.4. Sodium (LR: I; LE: A) 530
1.5.5. Potassium (LR: I; LE: A) 530
1.5.6. Physical Activity (LR: I; LE: A) 530
1.5.7. Alcohol (LR: IIA; LE: B) 531
1.5.8. Psychosocial Factors (LR: IIb; LE: B) 531
1.5.9. Dietary Supplements (LR: I to III; LE: A and B) 531
1.5.10. Smoking (LR: I; LE: A) 531
1.5.11. Spirituality (LR: I; LE: B) 531
1.6. Strategies for the Implementation of Preventive Measures 531
2. Blood Pressure and Vascular Damage 535
2.1. Introduction 535
2.2. Blood Pressure, Clinical Outcomes, and Cardiovascular Damage 535
2.3. Blood Pressure, Inflammation, and Endothelial Dysfunction 536
2.4. Blood Pressure and Arterial Stiffness 536
2.4.1. Ankle-Brachial Index (ABI) 536
2.4.2. Pulse Wave Velocity (PWV) 537
2.4.3. Central Blood Pressure 537
3. Diagnosis and Classification 540
3.1. Introduction 540
3.2. Blood pressure measurement at the physician's office 540
3.3. Classification 540
3.4. Out-of-Office Blood Pressure Measurement 541
3.5. White-Coat Effect (WCE) and Masking Effect (ME) 541
3.6. White Coat Hypertension (WCH) and Masked Hypertension (MH) 541
3.7. Uncontrolled Masked and White Coat Hypertension 541
3.8. Diagnosis and Follow-Up Recommendations 541
3.9. Central Aortic Pressure 542
3.10. Genetics and Hypertension 542
4. Clinical and Complementary Assessment 548
4.1. Clinical History 548
4.2. Clinical Assessment 548
4.2.1. History-Taking 548
4.3. Physical Examination 548
4.3.1. Basic Laboratory Investigation, Assessment of Subclinical and Clinical End-Organ Damage 548
5. Cardiovascular Risk Stratification 552
5.1. Introduction 552
5.2. Additional Risk Stratification (Associated Conditions) 552
5.2.1. End-Organ Damage 553
5.2.2. Presence of Cardiovascular and Renal Disease 553
5.3. Assessment of Global Cardiovascular Risk 553
5.4. Challenges of Cardiovascular Risk Assessment in Hypertension 553
6. Therapeutic Decision and Targets 556
6.1. Introduction 556
6.2. Low- or Moderate-Risk Hypertensive Patients 556
6.3. High-Risk Hypertensive Patients 556
6.4. Hypertensive Patients with Coronary Disease 556
6.5. Hypertensive Patients with History of Stroke 556
6.6. Hypertensive Heart Failure Patients 557
6.7. Hypertensive Patients with Chronic Kidney Disease (CKD) 557
6.8. Diabetic Hypertensive Patients 557
6.9. Older Hypertensive Patients 557
7. Multidisciplinary Team 559
7.1. The Importance of a Multidisciplinary Approach to Hypertension Control 7.2. Team Composition and Work 559
7.2.1. Medical Professional: Specific Actions 559
7.2.2. Nursing Professional: Specific Actions 559
7.2.2.1. Nursing-Specific Actions in Primary Care 559
7.2.3. Nutrition Professional: Specific Actions 560
7.2.3.1. Dietetic Consultation 560
7.2.3.2. Collective Actions by Nutritionists 560
7.2.4. Physical Education Professional: Specific Actions 560
7.2.4.1. Collective Actions by Physical Education and Physical Therapy Professionals 560
7.3. Multidisciplinary Team Actions 561
8. Nonpharmacological Treatment 562
8.1. Introduction 562
8.2. Smoking 562
8.3. Dietary Patterns 562
8.4. Sodium Intake 563
8.5. Potassium 563
8.6. Dairy Products 563
8.7. Chocolate and Cocoa Products 563
8.8. Coffee and Caffeinated Products 563
8.9. Vitamin D 563
8.10. Supplements and Substitutes 564
8.11. Weight Loss 564
8.12. Alcohol Consumption 564
8.13. Physical Activity and Physical Exercise 564
8.14. Slow Breathing 565
8.15. Stress Control 565
8.16. Religiosity and Spirituality 565
9. Pharmacological Treatment 568
9.1. Treatment Objectives 568
9.2. General Principles of Pharmacological Treatment 568
9.3. Therapy Regimens 568
9.3.1. Monotherapy 568
9.3.2. Drug Combinations 568
9.4. General Characteristics of Different Classes of Antihypertensive Medications 569
9.4.1. Diuretics (DIUs) 569
9.4.1.1. Adverse Effects of Diuretics 569
9.4.2. Calcium Channel Blockers (CCBs) 569
9.4.2.1. Adverse Effects of Calcium Channel Blockers 570
9.4.3. Angiotensin-Converting Enzyme Inhibitors (ACEIs) 570
9.4.3.1. Adverse Effects of Angiotensin-Converting Enzyme Inhibitors 9.4.4. Angiotensin II AT1 Receptor Blockers (ARBs) 570
9.4.4.1. Adverse Effects of Angiotensin II AT1 Receptor Blockers 570
9.4.5. Beta-Blockers (BBs) 570
9.4.5.1. Adverse Effects of Beta-Blockers 571
9.4.6. Centrally Acting Sympatholytics 571
9.4.6.1. Adverse Effects of Centrally Acting Sympatholytics 571
9.4.7. Alpha-blockers 571
9.4.7.1. Adverse Effects of Alpha-Blockers 571
9.4.8. Direct-Acting Vasodilators 571
9.4.8.1. Adverse Effects of Direct-Acting Vasodilators 571
9.4.9. Direct Renin Inhibitors 571
9.4.9.1. Adverse Effects of Direct Renin Inhibitors 572
9.5. Antihypertensive Drug Combinations 572
10. Hypertension and Associated Clinical Conditions 578
10.1. Diabetes Mellitus (DM) 578
10.1.1. Treatment Objectives 578
10.2. Metabolic Syndrome (MS) 578
10.3. Coronary Artery Disease (CAD) 578
10.4. Hypertension in Chronic Kidney Disease (CKD) 578
10.4.1. Patient in Conservative Treatment: Goals and Treatment 578
10.4.2. Patients in Renal Replacement Therapy (RRT): Goals and Treatment 579
10.5. Heart Failure (HF) 579
10.6. Hemorrhagic Stroke and Ischemic Stroke 580
10.6.1. Hemorrhagic Stroke 580
10.6.2. Ischemic Stroke 580
11. Hypertension in Pregnancy 581
11.1. Epidemiology 581
11.2. Classification of Hypertension in Pregnancy 581
11.3. Concept and Diagnostic Criteria 581
11.4. Prediction and prevention of pre-eclampsia 581
11.5. Nonpharmacological treatment 582
11.6. Expectant management 582
11.7. Pharmacological treatment 582
11.8 Future Cardiovascular Risk 583
12. Hypertension in Children and Adolescents 586
12.1. Epidemiological Context and Importance of Hypertension in Pediatrics 586 12.2. Definition and Etiology 586
12.3. Diagnostic 586
12.3.1. BP Measurement Methods 586
12.4. History-Taking 587
12.5. Physical Examination 587
12.7. Ambulatory Blood Pressure Monitoring (ABPM) 587
12.8. Therapeutic Aspects 587
12.9. Nonpharmacological Therapy 587
12.10. Pharmacological Therapy 587
12.11. Follow-up of Children and Adolescents with HT 588
12.12. Hypertensive Crisis 588
13. Hypertensive Crisis 596
13.1. Definition 596
13.2. Classification 596
13.3. Major Epidemiological, Pathophysiological, and Prognostic Aspects 596
13.3.1. Epidemiology 596
13.3.2. Pathophysiology 596
13.3.3. Prognosis 596
13.4. Complementary Clinical and Laboratory Investigation 597
13.5. General Treatment of Hypertensive Crisis 597
13.6. Hypertensive Emergencies in Special Situations 597
13.6.1. Hypertensive Encephalopathy 597
13.7. Stroke 597
13.7.1. Ischemic Stroke 597
13.7.2. Hemorrhagic Stroke 598
13.7.3. Acute Coronary Syndromes 598
13.7.4. Acute Pulmonary Edema (APE) 598
13.7.4.1. Acute Aortic Dissection 598
13.7.5. Pre-eclampsia/Eclampsia 598
13.7.6. HE from Illicit Drug Use 598
13.7.7. Accelerated/Malignant Hypertension 598
13.7.8. Hypertension with Multi-Organ Damage 599
14. Hypertension in Older Adults 602
14.1. Introduction 602
14.2. Physiopathological Mechanisms 602
14.3. Diagnosis and Therapeutic Decision 603
14.4. Treatment 603
14.4.1. Nonpharmacological Treatment 603
14.4.2. Pharmacological Treatment 603
14.5. Special Situations 604
14.5.1. Functional Status and Frailty: Assessment and Implications 604
14.5.2. Cognitive Decline and Dementia 604
14.5.3. Polypharmacy and Adherence 604
14.5.4. Deintensification and Deprescription 605
14.5.5. Orthostatic and Postprandial Hypotension 605
15. Secondary Hypertension 606
15.1. Introduction 606
15.2. Nonendocrine Causes 606
15.2.1. Chronic Kidney Disease (CKD) 606
15.2.2. Renovascular Hypertension (RVH) 606
15.3. Fibromuscular Dysplasia 607
15.3.1. Coarctation of the Aorta 607
15.3.2. Obstructive Sleep Apnea (OSA) 607
15.3.2.1. Concept and Epidemiology 607
15.3.2.2. Clinical Presentation and Screening of OSA in Hypertension 608
15.3.2.3. Impact of Treatment of OSA on BP 608
15.3.2.4. Antihypertensive Treatment in Hypertensive Patients with OSA 608
15.4. Endocrine Causes 608
15.4.1. Primary Hyperaldosteronism (PH) 608
15.4.2. Pheochromocytoma 609
15.4.3. Hypothyroidism 609
15.4.4. Hyperthyroidism 609
15.4.5. Primary Hyperparathyroidism 609
15.4.6. Cushing's Syndrome 610
15.4.7. Obesity 610 15.4.8. Acromegaly 610 15.5. Pharmacological Causes, Hormones, and Exogenous Substances 610
16. Resistant and Refractory Hypertension 618 16.1. Definition and Classification 618 16.2. Epidemiology of Resistant Hypertension 618 16.3. Pathophysiology 618 16.4. Diagnostic Investigation 618 16.5. Treatment 618 16.5.1. Nonpharmacological Treatment 618 16.5.2. Pharmacological Treatment 619 16.5.3. New Treatments 619
17. Adherence to Antihypertensive Treatment 622
17.1. Introduction 622
17.2. Concept and Adherence 622
17.3. Treatment Adherence Assessment Methods 622
17.4. Factors Interfering in Adherence to Treatment 623
17.5. Strategies to promote adherence to antihypertensive treatment 623
17.6. Conclusion 623
18. Perspectives 625
18.1. Introduction 625
18.2. Definition, Epidemiology, and Primary Prevention 625
18.3. Blood Pressure and Vascular Damage 625
18.4. Cardiac Biomarkers 625
18.5. Diagnosis and Classification 625
18.6. Complementary Assessment and Cardiovascular Risk Stratification 626
18.7. Goals and Treatment 626
Reference 628
1. Definition, Epidemiology, and Primary Prevention
1.1. Definition of Hypertension
Hypertension (HT) is a chronic noncommunicable disease (NCD) defined by blood pressure levels for which the benefits of treatment (nonpharmacological and/or pharmacological) outweigh the risks. HT is a multifactorial condition, depending on genetic/epigenetic, environmental, and social factors ( Figure 1.1 ), characterized by persistent high blood pressure (BP), ie, systolic blood pressure (SBP) equal to or greater than 140 mm Hg and diastolic blood pressure (DBP) equal to or greater than 90 mm Hg, measured using the appropriate technique, on at least two different occasions, in the absence of antihypertensive medication. When possible, it is advised that these measurements be validated by assessing BP outside the physician's office using ambulatory blood pressure monitoring (ABPM), home blood pressure monitoring (HBPM), or self-measured blood pressure (SMBP) (see Chapter 3).
– Schematic description of major determinants of blood pressure and hypertension and their interactions n adults. Genetic/epigenetic, environmental, and social determinants interact to increase the BP of hypertensive patients and in the general population. ↑increased; ↓decreased.
– Percentage of deaths from hypertension, acute myocardial infarction, stroke, and chronic renal failure (Brazil, 2000).
1.2. Impact of Hypertension on Cardiovascular Diseases
As an often asymptomatic condition, BP usually progresses to structural and/or functional change to end organs, such as the heart, brain, kidneys, and blood vessels. It is the primary modifiable risk factor, independently, linearly, and continuously associated, for cardiovascular disease (CVD), chronic kidney disease (CVD), and early death. It is associated with metabolic risk factors for cardiocirculatory and renal diseases, such as dyslipidemia, abdominal obesity, glucose intolerance, and diabetes mellitus (DM). 11. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017; 317(2):165-82.
2. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65.
3. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
In addition, it has a significant impact on socioeconomic and medical costs due to fatal and nonfatal complications to end organs, such as: heart: coronary artery disease (CAD), heart failure (HF), atrial fibrillation (AF), and sudden death; brain: stroke, ischemic stroke, hemorrhagic stroke, and dementia; kidneys; CKD that may require dialysis therapy; and arterial system: peripheral occlusive atherosclerotic disease (POAD). 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
1.3. Risk Factors for Hypertension
1.3.1. Genetics
Genetic factors may influence BP levels from 30 to 50%. 77. Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61. However, due to wide genetic diversity, the gene variants we have studied thus far and Brazilian miscigenation, uniform data for this factor have yet to be identified. Further details about the genetic component of HT can be found in Chapter 3.
1.3.2. Age
SBP becomes a more significant problem with age, the result of the progressive hardening and decreased compliance of the great arteries. Approximately 65 percent of people age 60 or older have HT, and we should take into consideration Brazil's ongoing epidemiological transition, with an even greater number of older adults (age ≥ 60) in the coming decades leading to a substantial increase in the prevalence of HT and its complications. 77. Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61.,88. Singh GM, Danaei G, Pelizzari PM, Lin JK, Cowan MJ, Stevens GA, et al. The age associations of blood pressure, cholesterol, and glucose: analysis of health examination surveys from international populations. Circulation. 2012;125(18): 2204-11.
1.3.3. Sex
Among younger cohorts, BP is higher in men, but rises faster by decade in women. Therefore, in their sixth decades, women's BP is usually higher than men's, as is the prevalence of HT. For both sexes, the frequency of HT rises with age, reaching 61.5% and 68.0% for men and women age 65 or older, respectively. 77. Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61.
1.3.4. Race/Ethnicity
Race and ethnicity are important risk factors for HT, but socioeconomic status and lifestyle seem to be more relevant for the differing prevalence of HT than race and ethnicity themselves. 77. Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61.,88. Singh GM, Danaei G, Pelizzari PM, Lin JK, Cowan MJ, Stevens GA, et al. The age associations of blood pressure, cholesterol, and glucose: analysis of health examination surveys from international populations. Circulation. 2012;125(18): 2204-11. The Vigitel 2018 data show that, in Brazil, there was no significant differences between blacks and whites regarding the prevalence of HT (24.9% versus 24.2%). 99. Brazil. Ministério da Saúde. Vigitel Brazil, 2016: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília;2016.
1.3.5. Overweight/Obesity
There seems to be a direct, continuous, and almost linear relationship between overweight/obesity and BP levels. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269. Despite decades of unequivocal evidence that waist circumference (CC) provides both independent and additive information to body mass index (BMI) for predicting morbidity and risk of death, this parameter is not routinely measured in clinical practice. It is recommended that health professionals be trained to properly perform this simple measurement and consider it as an important “vital sign” in clinical practice. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
1.3.6. Sodium and Potassium Intake
High sodium intake has been shown to be a risk factor for high BP and consequently for the greater prevalence of HT. The literature shows that sodium intake is associated with CVD and stroke when mean intake is greater than 2 g of sodium, equivalent to 5 g of table salt. 1010. Mente A, O’Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392(10146):496–506. Sodium excretion studies show that, for those with high sodium intake, SBP was 4,5-6.0 mm Hg higher, and DBP 2.3-2.5 mm Hg higher, than for those at recommended sodium intake levels. 1111. Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, et al. Intersalt revisited: further analyses of 24 hours sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312(7041):1249-53.
It should also be stressed that excess sodium intake is one of the main modifiable risk factors for preventing and controlling HT and CVD, and that the Brazilian Unified Health System (SUS) spent USD 102 million in 2013 alone on hospitalizations attributable to excess sodium intake. 1212. Mill JG, Malta DC, Machado ÍE, Pate A, Pereira CA, Jaime PC, et al. Estimativa do consumo de sal pela população Brazileira: resultado da Pesquisa Nacional de Saúde 2013. Rev Bras Epidemiol [Internet]. 2019;22(suppl 2):E190009. [Citado em 2020 Mar 10]. Disponível em: http://www.scielo.br/pdf/rbepid/v22s2/1980-5497-rbepid-22-s2-e190009-supl-2.pdf .
http://www.scielo.br/pdf/rbepid/v22s2/19...
Conversely, increased sodium intake reduces blood pressure levels. It is worth highlighting that the effects of potassium supplementation seems to be greater for those with high sodium intake and for black people. Mean salt intake in Brazil is 9.3 g/day (9.63 g/day for men and 9.08 g/day for women), while potassium intake is 2.7 g/day for men and 2.1 g/day for women. 1212. Mill JG, Malta DC, Machado ÍE, Pate A, Pereira CA, Jaime PC, et al. Estimativa do consumo de sal pela população Brazileira: resultado da Pesquisa Nacional de Saúde 2013. Rev Bras Epidemiol [Internet]. 2019;22(suppl 2):E190009. [Citado em 2020 Mar 10]. Disponível em: http://www.scielo.br/pdf/rbepid/v22s2/1980-5497-rbepid-22-s2-e190009-supl-2.pdf .
http://www.scielo.br/pdf/rbepid/v22s2/19...
,1313. Araujo MC, Bezerra IN, Barbosa F dos S, Junger WL, Yokoo EM, Pereira RA, et al. Consumo de macronutrientes e ingestão inadequada de micronutrientes em adultos. Rev Saude Publica [Internet]. 2013;47(Supl.1):1775–895. [Acesso em 10 de mar 2020]. Disponível em: http://dx.doi.org/10.1590/S0034-89102013000700004 .
http://dx.doi.org/10.1590/S0034-89102013...
1.3.7. Sedentary lifestyle
There is a direct association between a sedentary lifestyle, high BP, and HT. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269. It should be noted that, globally in 2018, the rate of lack of physical activity (less than 150 minutes of physical activity per week or 75 minutes of vigorous physical activity per week) was 27.5%, with greater prevalence among women (31.7%) than men (23.4%). 1414. Guthold R, Stevens, GA, Riley, LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health. 2018;6(10):e1077-e1086.
In Brazil, the 2019 Vigitel phone survey found that 44.8% of adults did not perform sufficient levels of physical activity, and rates were worse for women (52.2%) than for men (36,1%). 99. Brazil. Ministério da Saúde. Vigitel Brazil, 2016: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília;2016.
1.3.8. Alcohol
The impact of alcohol intake has been investigated in various epidemiological studies. There is greater prevalence of HT or high blood pressure levels for those taking six or more doses per day, equivalent to 30 g of alcohol/day = 1 bottle of beer (5% alcohol, 600 mL); = 2 glasses of wine (12% alcohol, 250 mL); = 1 dose (42% alcohol, 60 mL) of distilled beverages (whiskey, vodka, spirits). That threshold should be cut in half for low-weight men and for women. 1515. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120.,1616. Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: the Atherosclerosis Risk in Communities Study. Hypertension. 2001;37(5):1242–50.
1.3.9. Socioeconomic Factors
Socioeconomic factors include lower educational levels, inadequate living conditions, and low family income as significant risk factors for HT. 1717. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.,1818. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55.
1.3.10. Other Risk Factors for High BP
In addition to the classic factors listed above, it is important to stress that some medications, often acquired without prescription, have the potential to promote high BP or make it harder to control, as do illicit drugs. The subject will be discussed in more detail in Chapter 15. These include monoamine oxidase inhibitors and sympathomimetic, such as decongestants (phenylephrine), tricyclic antidepressants (imipramine and others), thyroid hormones, oral contraceptives, nonsteroidal anti-inflammatory drugs, carbenoxolone and liquorice, glucocorticoids, cyclosporine, erythropoietin, and illicit drugs (cocaine, cannabis, amphetamine and 3,4-methylenedioxymethamphetamine (MDMA)). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,1919. Plavnik FL. Hipertensão arterial induzida por drogas: como detectar e tratar. Rev Bras Hipertens. 2002; 9:185-91.
1.3.11. Obstructive Sleep Apnea (OSA)
There is clear evidence behind the relation between OSA and HT and increased risk of resistant HT (see also Chapter 15). Mild, moderate, and severe OSA has a dose-response relationship with HT. There is a stronger association for Caucasian and male patients with OSA. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,2020. Ahmad M, Makati D, Akbar S. Review of and Updates on Hypertension in Obstructive Sleep Apnea. Int J Hypertens. 2017; 2017:1848375. https://doi.org/10.1155/2017/1848375 .
https://doi.org/10.1155/2017/1848375...
1.3.12. Global Epidemiological Data
CVD are the main cause of death, hospitalization, and outpatient medical visits worldwide, including developing countries such as Brazil. 2121. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980- 2016: a systematic analysis for the Global Burden of Disease Study . Lancet. 2017;390(10100):1151-210. In 2017, complete and revised data from Datasus showed a total of 1 312 663 deaths, 27.3% of which from CVD. 2222. 2017. Lancet. 2016;390:1151–210. Causes of Death 2008 [online database]. Geneva, World Health Organization. [Cited in 2020 Mar 10] Available from: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf
http://www.who.int/healthinfo/global_bur...
HT was associated with 45% of cardiac deaths (CAD and HF), 51.0% of deaths from cerebrovascular disease (CVD), and a small percentage of deaths directly related to HT (13.0%). It should be stressed that HT kills more by causing end-organ damage 2323. Brazil. Ministério da Saúde. DATASUS/MS/SVS/CGIAE - Sistema de Informações sobre Mortalidade SIM. [Acesso em 19 de abr 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID 10-Capitulos I00-I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def .
http://tabnet.datasus.gov.br/cgi/tabcgi....
( Figure 1.2 ).
In 2017, data from Global Burden of Disease (GBD) indicated that CVD accounted for 28.8% of total deaths from noncommunicable diseases (NCD). The GBD study found that there were almost 18 million deaths from CV causes in 2017 (31.8% of total deaths), accounting for 20.6% of total years of life lost (YLL) and 14,7% total DALYs (disability-adjusted life years, ie, years of healthy life lost). 1818. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55.,2121. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980- 2016: a systematic analysis for the Global Burden of Disease Study . Lancet. 2017;390(10100):1151-210.
Also according to GBD, SBP increase was found to be the main risk factor, responsible for 10.4 million deaths and 218 million DALYs. 2121. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980- 2016: a systematic analysis for the Global Burden of Disease Study . Lancet. 2017;390(10100):1151-210. It also accounts for approximately 40.0% of deaths of DM patients, 14.0% of maternal and fetal mortality during pregnancy, and 14.7% of total DALYs from CKD. 2424. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PFA. WHO analysis of causes of maternal death: a systematic review. Lancet.2006;367(9516):1066-74.
25. Udani S, Lazich I, Bakris GL. Epidemiology of hypertensive kidney disease. Nat Rev Nephrol. 2011;7(1):11-21.-2626. Brazil. Ministério da Saúde. DATASUS. Sistema de Informações Hospitalares do SUS(SIH/SUS). {Internet} Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/nruf.def/2008-2018/ CID 10-Capitulos I00 I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def . Acessado em 19/03/2020.
http://tabnet.datasus.gov.br/cgi/tabcgi....
Globally, in 2010, HT prevalence (≥140/90 mm Hg and/or use of antihypertensive medication) was 31.0%, higher for men (31.9%) than for women (30.1%). 1717. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.,1818. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55.
A study on worldwide trends in blood pressure from 1975 to 2015 assessing 19.1 million adults found that, in 2015, there was an estimated 1.13 billion adults with HT (597 million men and 529 million women), suggesting a 90% increase in the number of people with HT, especially in low- and medium-income countries. 1717. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.,1818. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55. The study found that HT prevalence decreased in high-income countries and some medium-income ones, but increased or held steady in lower-income nations. The factors implicated in that increase are likely population aging and greater exposure to other risk factors, such as high sodium and low potassium intake, in addition to sedentary lifestyles. 1717. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.,1818. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55.
1.4. Prevalence of Hypertension in Brazil
Countrywide prevalence data tend to vary according to the methodology and sample chosen. According to the 2013 Brazilian National Health Survey, 21.4% (95% CI 20.8-22.0) of Brazilian adults self-report HT, while BP readings and the use of antihypertensive medications indicate that the share of adults with BP at or above 140/90 mm Hg is approximately 32.3% (95% CI 31.7-33.0). HT prevalence was found to be higher among men and, as expected, to increase with age regardless of other parameters, reaching 71.7% for individuals age 70 and older ( Table 1.1 and Figure 1.3 ). 2727. Malta DC, Gonçalves RPF, Machado IE, Freitas MIF, Azeredo C, Szwarcwald CL et al. Prevalência da hipertensão arterial segundo diferentes critérios diagnósticos. Pesquisa Nacional de Saúde. Rev Bras Epidemiol. 2018; 21(sup 1): E180021.
In 2017, there was a total of 1 312 663 deaths, 27.3% of which from CVD, accounting for 22.6% of all early deaths in Brazil (ages 30 to 69). In one ten-year period (2008 through 2017), it is estimated that 667 184 could be attributed to HT in Brazil. 2121. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980- 2016: a systematic analysis for the Global Burden of Disease Study . Lancet. 2017;390(10100):1151-210.
22. 2017. Lancet. 2016;390:1151–210. Causes of Death 2008 [online database]. Geneva, World Health Organization. [Cited in 2020 Mar 10] Available from: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf
http://www.who.int/healthinfo/global_bur...
-2323. Brazil. Ministério da Saúde. DATASUS/MS/SVS/CGIAE - Sistema de Informações sobre Mortalidade SIM. [Acesso em 19 de abr 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID 10-Capitulos I00-I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def .
http://tabnet.datasus.gov.br/cgi/tabcgi....
In the death rate per 100 000 inhabitants from 2000 to 2018, we can see a slight uptick in AMI and a jump in direct HT, with 25% and 128% increases, respectively. 2323. Brazil. Ministério da Saúde. DATASUS/MS/SVS/CGIAE - Sistema de Informações sobre Mortalidade SIM. [Acesso em 19 de abr 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID 10-Capitulos I00-I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def .
http://tabnet.datasus.gov.br/cgi/tabcgi....
As for morbidity, we can see the population-adjusted hospitalization trend has been stable over the last ten years (Datasus Hospitalization System) both for all causes and for CVD ( Figure 1.3 ). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,2323. Brazil. Ministério da Saúde. DATASUS/MS/SVS/CGIAE - Sistema de Informações sobre Mortalidade SIM. [Acesso em 19 de abr 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID 10-Capitulos I00-I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def .
http://tabnet.datasus.gov.br/cgi/tabcgi....
More of the Brazilian health system's costs can be attributed to HT than to obesity and DM. In 2018, it is estimated that SUS spent USD 523.7 million in hospitalizations, outpatient procedures, and medications. 2828. Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Custos atribuíveis à obesidade, hipertensão e diabetes no Sistema Único de Saúde em 2018. Rev Panam Salud Publica. 2020;44:e32.
Over the last decade, CVD associated with HT account for 77% of the Brazilian Unified Health System's (SUS) hospitalization costs from CAD, and they increased 32% from 2010 to 2019 in Brazilian reais, from R$ 1.6 billion to R$ 2.2 billion over the same period. 2828. Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Custos atribuíveis à obesidade, hipertensão e diabetes no Sistema Único de Saúde em 2018. Rev Panam Salud Publica. 2020;44:e32.,2929. EAF, Silva EN, Jaime PC. Developing and applying a costing tool for hypertension and related cardiovascular disease: attributable costs to salt/sodium consumption. J Clin Hypertens. 2020;22(4):642-8.
1.5. Primary Prevention
1.5.1. Introduction
HT is highly prevalent and a major risk factor for CVD and kidney disease, combining genetic, environmental, and social determinants. It is easily diagnosable and effectively treatable by a diverse and highly efficiency therapeutic arsenal with few adverse effects. Even so, globally, the fact that it is an often asymptomatic disease means adherence to care is difficult and it remains mostly uncontrolled worldwide.
That equation makes treatment extremely challenging, and prevention remains the best option from a cost-benefit perspective. An adequate approach to risk factors for HT should be a major point of focus for SUS (the Brazilian Unified Health System). Several aspects of that issue deserve further consideration. Many are interwoven or ad to nonpharmacological treatment ( Chart 1.1 ), detailed in Chapter 8. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,3030. Dickey RA, Janick JJ. Lifestyle modifications in the prevention and treatment of hypertension. Endocr Pract. 2001; 7 (5):392-9.,3131. Perumareddi P. Prevention of hypertension related to cardiovascular disease. Prim Care. 2019;46(1):27-39.
1.5.2. Weight Control (LR: I; LEE: A)
Overall and central obesity are associated with increased risk of HT. On the other hand, weight loss promoted lower BP both for normotensive and for hypertensive individuals. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269. Being “as lean as possible” within the normal BMI range may be the best suggestion for primary prevention of HT. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,3232. Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension (Review) Exp Ther Med. 2016;12(4):2395-9.
33. Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2.3 million participants. Obes Rev. 2018;19(5):654-67.
34. Zhao Y, Qin P, Sun H, Liu Y, Liu D, Zhou Q, et al. Metabolically healthy general and abdominal obesity are associated with increased risk of hypertension. Br J Nutr. 2020;123(5):583-91.
35. Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-87.-3636. Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, et al. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database Syst Rev. 2016;Mar 2;3:CD008274.
1.5.3. Healthy Diet (LR: I; LE: A)
Several diets have been proposed for HT prevention which also favor hypertension control and contribute to health as a whole. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. One major proposal to that end is the DASH diet and its variants (low fat, Mediterranean, vegetarian/vegan, Nordic, low carbohydrate content, etc.). The benefits are even greater when combined with lower sodium intake. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
38. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: A systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59 (16): 2674-87.
39. Pergola G, D’Alessandro A. Influence of Mediterranean Diet on Blood Pressure. Nutrients. 2018;10 (1700):1-6.-4040. Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33(4):388-93.
Every report on the subject recommends eating healthy amounts of fruits, greens, vegetables, cereal, milk, and dairy products, as well as lowering salt and fat intake. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
38. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: A systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59 (16): 2674-87.
39. Pergola G, D’Alessandro A. Influence of Mediterranean Diet on Blood Pressure. Nutrients. 2018;10 (1700):1-6.
40. Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33(4):388-93.-4141. Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium Intake and Hypertension. Nutrients. 2019;11(9):1970. A meta-analysis compared varieties of these diets with the standard diet and found a greater decrease in SBP (-9.73 to -2.32 mm Hg) and DBP (-4.85 to -1.27 mm Hg) in the proper diet group. 3939. Pergola G, D’Alessandro A. Influence of Mediterranean Diet on Blood Pressure. Nutrients. 2018;10 (1700):1-6. Socioeconomic and cultural aspects have to be taken into account to ensure adherence to a given kind of dietary recommendation. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
1.5.4. Sodium (LR: I; LE: A)
Excess sodium intake is one of the main modifiable risk factors for preventing and controlling HT and CVD. 2929. EAF, Silva EN, Jaime PC. Developing and applying a costing tool for hypertension and related cardiovascular disease: attributable costs to salt/sodium consumption. J Clin Hypertens. 2020;22(4):642-8. Sodium restriction has been shown to lower BP in several studies. A meta-analysis found that a 1.75 g decrease in daily sodium intake (4.4 g of salt/day) is associated with a mean decrease of 4.2 and 2.1 mm Hg in SBP and DBP, respectively. The BP decrease from sodium restriction is greater in blacks, older adults, diabetic patients, and individuals suffering from metabolic syndrome (MS) and CKD. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
In the general population, individuals are recommended to restrict their sodium intake to approximately 2 g/day (equivalent to about 5 g of salt per day). 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269. Effectively lowering salt intake is not easy, and low-salt foods are often underappreciated. Patients should be advised to take care with how much salt they add to their food and not to eat high-salt items (industrialized and processed foods). 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
Decreasing Brazilian salt intake remains a high public health priority, but requires combined efforts from the food industry, all levels of government, and the public in general, since 80% of salt comes from processed foods. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,1010. Mente A, O’Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392(10146):496–506.,1212. Mill JG, Malta DC, Machado ÍE, Pate A, Pereira CA, Jaime PC, et al. Estimativa do consumo de sal pela população Brazileira: resultado da Pesquisa Nacional de Saúde 2013. Rev Bras Epidemiol [Internet]. 2019;22(suppl 2):E190009. [Citado em 2020 Mar 10]. Disponível em: http://www.scielo.br/pdf/rbepid/v22s2/1980-5497-rbepid-22-s2-e190009-supl-2.pdf .
http://www.scielo.br/pdf/rbepid/v22s2/19...
,4040. Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33(4):388-93. Adequate intake of fruits and vegetables leverages the beneficial effects of a low-sodium diet on BP. Salt substitutes with potassium chloride and less sodium chloride (30 to 50%) are useful to help lower sodium intake and increase potassium intake, despite their restrictions. 4242. Jafarnejad S, Mirzaei H, Clark CCT, Taghizadeh M, Ebrahimzadeh. The hypotensive effect of salt substitutes in stage 2 hypertension: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20(98):1-15.
1.5.5. Potassium (LR: I; LE: A)
The relationship between potassium supplementation and lowering HT is relatively well understood. 4343. Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. J Am Med Assoc. 1997;277(20):1624–32. Potassium supplementation represents a safe alternative, with no major adverse effects and modest but significant impact on BP, and can be recommended to help prevent the onset of HT. 4343. Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. J Am Med Assoc. 1997;277(20):1624–32.
44. Stone MS, Martyn L, Weaver CM. Potassium Intake, Bioavailability, Hypertension, and Glucose Control. Nutrients. 2016;8(444):1-13.
45. Filippini T, Violi F, D’Amico R, Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int J Cardiol. 2017. 230:127-35.
46. Poorolajal J, Zeraati F, Soltanian AR, Sheikh V, Hooshmand E, Maleki A. Oral potassium supplementation for management of essencial hypertension: A meta–analysis of randomized controlled trials. Plos One. 2017;12(4):1- 6.-4747. Caligiuri SPB, Pierce GN. A review of the relative efficacy of dietary, nutritional supplements, lifestyle, and drug therapies in the management of hypertension. Crit Rev Food Sci Nutr. 2017;57(16):3508-27. Adequate potassium intake, on the order of 90 to 120 mEq/day, may lead to a 5.3 mm Hg decrease in SBP and a 3.1 mm Hg decrease in DBP. 4545. Filippini T, Violi F, D’Amico R, Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int J Cardiol. 2017. 230:127-35. Its intake can increase by opting for sodium-poor and potassium-rich foods, such as beans, peas, dark leafy greens, bananas, melons, carrots, beets, dried fruit, tomatoes, potatoes, and oranges. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
1.5.6. Physical Activity (LR: I; LE: A)
A sedentary lifestyle is one of the ten most important risk factors for global mortality, causing approximately 3.2 million deaths per year. 4848. World Health Organization. (WHO). Global status report on noncommunicable diseases.Geneva; 2014. ISBN 978 92 4 156485 4.,4949. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990– 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859): 2224−60.
A meta-analysis of 93 papers and 5223 individuals showed that aerobic, dynamic resistance and isometric resistance training lower SBP and DBP at rest by 3.5/2.5, 1.8/3.2 and 10.9/6.2 mm Hg, respectively, in the general population. 5050. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473.
51. Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(3):327-34.-5252. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39(2):88-94.
All adults should be advised to practice at least 150 min/week of moderate physical activity or 75 min/week of vigorous activity. Aerobic exercises (walking, running, bicycling, or swimming) may be practiced for 30 minutes 5 to 7 times per week. Resistance training two to three days per week is also recommended. 5050. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473.,5252. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39(2):88-94. For additional benefits, in healthy adults, a gradual increase in physical activity to 300 minutes per week of moderate-intensity physical activity or 150 minutes per week of vigorous physical activity, or an equivalent combination of the two, ideally with supervised daily physical exercise. 5555. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Eur Heart J. 2016;37(29):2315-81.
1.5.7. Alcohol (LR: IIA; LE: B)
Alcohol consumption is estimated to account for approximately 10 to 30% of HT cases and approximately 6% of all-cause mortality worldwide. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,1515. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120.,5656. MacMahon S. Alcohol consumption and hypertension. Hypertension. 1987;9(2):111-21.
57. Lang T, Cambien F, Richard JL, Bingham A. Mortality in cerebrovascular diseases and alcoholism in France. Presse Med. 1987;16(28):1351-4.
58. Fuchs FD, Chambless LE, Folsom AR, Eigenbrodt ML, Duncan BB, Gilbert A, et al. Association between alcoholic beverage consumption and incidence of coronary heart disease in whites and blacks: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2004;160(5):466-74.-5959. World Health Organization.(WHO). Global status report on alcohol and health. Geneva; 2014. Among drinkers, intake should not exceed 30 g of alcohol/day, ie, 1 bottle of beer (5% alcohol, 600 mL), two glasses of wine (12% alcohol, 250 mL), or one 1 dose (42% alcohol, 60 mL) of distilled beverages (whiskey, vodka, spirits). That threshold should be cut in half for low-weight men, women, the overweight, and/or those with high triglycerides. Teetotalers should not be encouraged to drink. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,1515. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120.
1.5.8. Psychosocial Factors (LR: IIb; LE: B)
There is a wide variety of techniques used to control emotional stress and contribute to HT prevention, but there is still a dearth of robust studies on the subject. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,6060. Johnson HM. Anxiety and Hypertension: Is There a Link? A Literature Review of the Comorbidity Relationship Between Anxiety and Hypertension. Curr Hypertens Rep. 2019;21(9):66. Practicing emotional stress control can help CV reactivity, BP itself, and BP variability. 6161. Dalmazo AL, Fetter C, Goldmeier S, Irigoyen MC, Pelanda LC, Barbosa ECD, et al. Stress and Food Consumption Relationship in Hypertensive Patients. Arq Bras Cardiol. 2019;113(3):374-80.
62. Denollet J, Gidron Y, Vrints CJ, Conraads VM. Anger, suppressed anger, and risk of adverse events in patients with coronary artery disease. Am J Cardiol. 2010;105(11):1555-60.-6363. Bai Z, Chang J, Chen C, Li P, Yang K, Chi I. Investigating the effect of transcendental meditation on blood pressure: a systematic review and meta-analysis. J Hum Hypertens. 2015;29(11):653-62.
1.5.9. Dietary Supplements (LR: I to III; LE: A and B)
The effects of dietary supplements on lowering BP are usually small and heterogeneous. 5858. Fuchs FD, Chambless LE, Folsom AR, Eigenbrodt ML, Duncan BB, Gilbert A, et al. Association between alcoholic beverage consumption and incidence of coronary heart disease in whites and blacks: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2004;160(5):466-74.
59. World Health Organization.(WHO). Global status report on alcohol and health. Geneva; 2014.
60. Johnson HM. Anxiety and Hypertension: Is There a Link? A Literature Review of the Comorbidity Relationship Between Anxiety and Hypertension. Curr Hypertens Rep. 2019;21(9):66.
61. Dalmazo AL, Fetter C, Goldmeier S, Irigoyen MC, Pelanda LC, Barbosa ECD, et al. Stress and Food Consumption Relationship in Hypertensive Patients. Arq Bras Cardiol. 2019;113(3):374-80.
62. Denollet J, Gidron Y, Vrints CJ, Conraads VM. Anger, suppressed anger, and risk of adverse events in patients with coronary artery disease. Am J Cardiol. 2010;105(11):1555-60.
63. Bai Z, Chang J, Chen C, Li P, Yang K, Chi I. Investigating the effect of transcendental meditation on blood pressure: a systematic review and meta-analysis. J Hum Hypertens. 2015;29(11):653-62.
64. Tankeu AT, Agbor VN, Noubiap JJ. Calcium supplementation and cardiovascular risk: A rising concern. J Clin Hypertens. 2017;19(6):640-6.
65. Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. 2018;380(1):33-44.
66. Amoh-Mensah K, Ankomah SE, KariKari AK, Arthur JA. Prevention of Hypertension: A critical review of the Health benefits of Salt, Garlic, Fish oil, Chocolate and Vitamin D. Int J Med Sci Tech. 2017;7(7):38-46.
67. Paula TP, Kramer CK, Viana LV, Azevedo MJ. Effects of individual micronutrients on blood pressure in patients with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2017;7(40751): 1-12.-6868. Gröber U, Schimidt J, Kisters K. Magnesium in Prevention and Therapy. Nutrients. 2015; 7: 8199-226. There is evidence that the following supplements can help lower BP to a small degree: vitamin C, food-derived bioactive peptides, garlic, dietary fiber, flaxseed, dark chocolate (cocoa), soy, organic nitrates, and Omega-3 fatty acids. 3838. Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: A systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59 (16): 2674-87.,4747. Caligiuri SPB, Pierce GN. A review of the relative efficacy of dietary, nutritional supplements, lifestyle, and drug therapies in the management of hypertension. Crit Rev Food Sci Nutr. 2017;57(16):3508-27.,6969. Padwal R, Hackam D, Khan N, Tobe S. Primary prevention of CVD: modification of diet in people with hypertension. BMJ Clin Evid. 2016 Jan; 2016:pii:0214. Magnesium supplements, multivitamins, tea, and coenzyme Q10 have not been shown to lead to significant decreases in BP. 6464. Tankeu AT, Agbor VN, Noubiap JJ. Calcium supplementation and cardiovascular risk: A rising concern. J Clin Hypertens. 2017;19(6):640-6.,6565. Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. 2018;380(1):33-44.,7070. Flowers N, Hartley L, Todkill D, Stranges S, Rees K. Co-enzyme Q10 supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;(12):CD010405.
1.5.10. Smoking (LR: I; LE: A)
Regardless of its impact on BP, tackling this issue is critical, since smoking is the only completely avoidable risk factor for cardiovascular disease and death, and fighting it is paramount. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,7171. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2014.
72. World Health Organization. (WHO). Report on the global tobacco epidemic. Geneva; 2017.
73. Center for Disease Control and Prevention. How Tobacco Smoke Causes Disease: The Biology and Behavioural Basis for Smoking-attributable Disease. A Report of the Surgeon General;2010.
74. Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-centuryhazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-50.-7575. Khoramdad M, Vahedian-azimi A, Karimi L, Rahimi-Bashar F, Amini H, Sahebkar A. Association between passive smoking and cardiovascular disease: A systematic review and meta-analysis. IUBMB Life. 2020;72(4):677-86. From a prevention standpoint, the WHO recommends the following strategies for tobacco control: prevent the young from trying cigarettes, since the odds of becoming addicted for those who try are over 50%; and enforce the country's tobacco legislation, particularly the prohibition of marketing tobacco products to minors, in addition to other activities directed at this age group. 7272. World Health Organization. (WHO). Report on the global tobacco epidemic. Geneva; 2017. Chemical and psychological addiction makes the fight against smoking hard, but the benefits of cessation for CV mortality are apparent in the short run. 7171. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2014.,7373. Center for Disease Control and Prevention. How Tobacco Smoke Causes Disease: The Biology and Behavioural Basis for Smoking-attributable Disease. A Report of the Surgeon General;2010.
74. Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-centuryhazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-50.-7575. Khoramdad M, Vahedian-azimi A, Karimi L, Rahimi-Bashar F, Amini H, Sahebkar A. Association between passive smoking and cardiovascular disease: A systematic review and meta-analysis. IUBMB Life. 2020;72(4):677-86.
Rigor in fighting and controlling tobacco use, continuous guidance and unconditional psycho-emotional support for smokers, and occasionally prescribing medication have been shown to be the most effective approach. 7373. Center for Disease Control and Prevention. How Tobacco Smoke Causes Disease: The Biology and Behavioural Basis for Smoking-attributable Disease. A Report of the Surgeon General;2010. It is also important to protect individuals against exposure to secondhand smoking, which also implies greater risk. 7474. Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-centuryhazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-50.
1.5.11. Spirituality (LR: I; LE: B)
There is growing evidence that spirituality (S), a concept transcending religiosity (R), signifying a set of moral, emotional, behavioral, and attitudinal values toward the world, provides benefits in terms of CV risk, mortality, and, in particular, blood pressure control. 7676. VanderWeele TJ, Balboni TA, Koh HK, Health and Spirituality. JAMA. 2017;318(6):519-20.
The Black Women’s Health Study showed that women who coped with stressful situations through spirituality and religiosity had lower risk of developing HT over a 10-year follow-up period (incidence ratio = 0.87; 95% CI 0.75-1.00), and the association was stronger for those reporting higher levels of stress. The survey also found that R/S situations helped modulate and smooth out the challenges of daily life and brought benefits in terms of BP control. 7777. Cozier YC, Yu J, Wise LA, VanderWeele TJ, Balboni TA, Argentieri MA, et al. Religious and Spiritual Coping and Risk of Incident Hypertension in the Black Women’s Health Study. Ann Behav Med. 2018;52(12):989-98.
1.6. Strategies for the Implementation of Preventive Measures
Lifestyle changes (LSCs) are hard to implement, and society as a whole should work together to support that effort. It is important to establish and support ongoing health education programs directed at K-12 and vocational school students, staff, corporations, and the community. Using the media to raise awareness is an important strategy; periodic focused campaigns (City, State and/or National Hypertension and Prevention Day—Federal Law 10.439 from April 30, 2002, HT Week, the International Society of Hypertension's May Measurement Month, etc.); and additional actions: incorporating HT prevention, detection, and control to primary health care programs, including children and adolescents, and particularly in school health programs; deploying multidisciplinary care programs; strengthening government norms to lower the saturated fat and sodium content of industrialized foods; enhancing nutrition fact labels; and using efficient health indicators to monitor HT prevention and control actions and their results. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
4. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
5. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.-66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
| Key Takeaways |
|---|
| The numbers defining hypertension are arbitrary, but represent values for which the benefits of treatment (nonpharmacological and/or pharmacological) outweigh the risks. |
| HT is a multifactorial condition (genetics, environment, life habits and socioeconomic factors). |
| HT is a major risk factor for cardiovascular and kidney diseases. |
| HT is highly prevalent, easily diagnosed and can be properly treated, but low adherence means it is hard to control. |
| HT prevention is cost-effective and also the best way to decrease cardiovascular morbidity and mortality. |
2. Blood Pressure and Vascular Damage
2.1. Introduction
High blood pressure (BP) values are traditionally associated with risk for ischemic heart disease, stroke, chronic kidney disease (CKD), and early death. A classic meta-analysis of 61 prospective studies, tracking 12.7 million persons-year and a record of 56 000 deaths from coronary artery disease (CAD) or stroke, produced solid observational evidence. 7878. Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13. That meta-analysis showed that the risk begins with BP values as low as 115 mm Hg for systolic BP (SBP) or 75 mm Hg for diastolic BP (DBP), doubling for every 20 mm Hg increase in SBP or 10 mm Hg increase in DBP. Despite observational evidence, these findings have not been integrated with the definition of hypertension (HT) diagnosis, which has remained at 140/90 mm Hg for many years.
Thus, patients are still classified as hypertensive with BP levels above 140/90 mm Hg, and individuals with SBP from 120 to 139 mm Hg and DBP from 80 to 89 mm Hg are classified as having normal BP or as prehypertensives, but these have higher cardiovascular risk in comparison with their peers with normal or optimum BP levels. The impact of prehypertension (systolic BP 130-139 mm Hg, diastolic BP 85-89 mm Hg) on vascular risk was described in 2001 by Vasan et al., 7979. Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med.2001;345(8):1291-7. who analyzed 6859 participants in the Framingham Heart Study. In that study, the authors found an increase in absolute risk for cardiovascular (CV) events. Several other studies have since been published, and their analysis included lower risk patients (systolic BP 120-139, diastolic BP 80-89 mm Hg), such as the Hisayama study, by Fukuhara et al., 8080. Fukuhara M, Arima H, Ninomiya T, Hata J, Yonemoto K, Doi Y, et al. Impact of lower range of prehypertension events in a general population: the Hysayama Study. J Hypertens. 2012;30(5):893-900. which also found increased risk for CV disease.
Several other studies have been published since the early work by Vasan et al., which has led to a meta-analysis by Han et al. 8181. Han M, Li Q, Liu L, Zhang D, Ren Y, Zhao Y, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens. 2019; 37(12):2325-32. in 2019, which analyzed 47 studies and a total population of 491 666 individuals. In that meta-analysis, after controlling for multiple CV risk factors, prehypertension increased the total risk of disease by 40%, including that 12.09% of CV disease, 13.26% of coronary diseases, 24;60% of myocardial infarctions (MIs), and 19.15% of strokes could have been prevented if prehypertension was effectively controlled.
That leads to the conclusion that prehypertensive individuals, even if not considered actually hypertensives, should be better assessed and stratified. Noninvasive complementary examinations can evaluate the impact of BP on vessels and analyze early vascular damage both in hypertensive and prehypertensive patients, 8282. Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness A Scientific Statement from the American Heart Association. Hypertension. 2015; 66(3):698-722. such as flow-mediated dilation (FMD), which checks endothelial function, and pulse wave velocity (PWV) and ankle-brachial index (ABI), which check the medial layer. The goal of this chapter is to show the impact of increased BP on CV risk, on endothelial dysfunction (damage to the vascular endothelial layer) and arterial stiffness (damage to the vascular medial layer) before HT is diagnosed.
2.2. Blood Pressure, Clinical Outcomes, and Cardiovascular Damage
In the meta-analysis by Law et al., 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665. lowering SBP by 10 mm Hg in randomized controlled trials led to AMI and stroke prevention at the same rate estimated by observational studies for the same BP increase. The same was true for a more recent meta-analysis. 8484. Bundy JD, Li C, Stuchlik P, Bu X, Bu X, Kelly TN, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017; 2(7):775–81. In this study, the relative risk reduction for CV events in trials where participants were treated to achieve SBP targets from 120 to 124 mm Hg, compared to over 160 mm Hg, was 64%, close to the 75% risk reduction for an estimated 40 mm Hg decrease in SBP from the Prospective Studies Collaboration meta-analysis. 7878. Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13. Other meta-analyses have converged for these findings, and the largest included 600 000 participants from clinical trials. 8585. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67. The SPRINT clinical trial added more evidence to the studies discussed above. 8686. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16. The incidence of CVD decreased by 25% in patients randomized for a SBP < 120 mm Hg (intensive treatment), compared to those randomized for a target BP level below 140 mm Hg. There was a 43% decrease in CVD mortality and a 27% decrease in all-cause mortality. A similar benefit was found for participants 75 or older over the baseline, including frail individuals 8787. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24):2673–82. (LR: I LE: A).
More recently, several cohort studies with large sample sizes have come out showing that increased BP creates similar risks for other CV outcomes as those found for CAD and stroke. These include heart failure (HF), with and without preserved ejection fraction (EF), 8888. Ho JE, Enserro D, Brouwers FP, Kizer JR, Shah SJ, Psaty BM, et al. Predicting heart failure with preserved and reduced ejection fraction: The International Collaboration on Heart Failure Subtypes. Circ Heart Fail. 2016;9(6):pii:003026. atrial fibrillation, 8989. Emdin CA, Anderson SG, Salimi-Khorshidi G, Woodward M, MacMahon S, Dwyer T, et al. Usual blood pressure, atrial fibrillation and vascular risk: evidence from 4.3 million adults. Int J Epidemiol. 2017; 46(1):162-2. valvular heart disease, 9090. Rahimi K, Mohseni H, Kiran A, Tran J, Nazarzadeh M, Rahimian F, et al. Elevated blood pressure and risk of aortic valve disease: a cohort analysis of 5.4 million UK adults. Eur Heart J. 2018;39:3596-603.,9191. Rahimi K, Mohseni H, Otto CM, Conrad N, Tran J, Nazarzadeh M, et al. Elevated blood pressure and risk of mitral regurgitation: A longitudinal cohort study of 5.5 million United Kingdom adults. PLoS Med. 2017; 14(10):e1002404. peripheral arterial disease, 9292. Emdin CA, Anderson SG, Callender T, Conrad N, Salimi-Khorshidi G, Mohseni H, et al. Usual blood pressure, peripheral arterial disease, and vascular risk: cohort study of 4.2 million adults. BMJ. 2015;351:h4865. chronic kidney disease (CKD), 9393. Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005; 165(8):923-8.,9494. Kanno A, Kikuya M, Ohkubo T, Hashimoto T, Satoh M, Hirose T, et al. Pre-hypertension as a significant predictor of chronic kidney disease in a general population: the Ohasama Study. Nephrol. Dial Transplant. 2012; 27(8):3218-23. dementia, 9595. Emdin CA, Rothwell PM, Salimi-Khorshidi G, Kiran A, Conrad N, Callender T, et al. Blood pressure and risk of vascular dementia: evidence from a primary care registry and a cohort study of transient ischemic attack and stroke. Stroke. 2016; 47(6):1429-35.,9696. Walker KA, Sharrett R, Wu A, Schneider AL, Alber M, Lutsey PL, et al. Association of midlife to late-life blood pressure patterns with incident dementia. JAMA. 2019; 322(6):535-45. and Alzheimer's disease. 9797. Joas E, Bäckman K, Gustafson D, Ostling S, Waern M, Guo X, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 2012; 59(4):796-801. Diabetes mellitus, 9898. Emdin CA, Anderson SG, Woodward M, Rahimi K. Usual blood pressure and risk of new-onset diabetes evidence from 4.1 million adults and a meta-analysis of prospective studies. J Am Coll Cardiol. 2015; 66(14):1552–62. erectile dysfunction, 9999. Ning L, Yang L. Hypetension might be a risk factor for erectile dysfunction: a meta-analysis. Andrologia. 2017; 49(4) doi.org/10.1111/and.12644 and age-related macular degeneration 100100. Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010 Dec 13;10:31. 10:31. are likely consequences of sustained high BP. In general, these consequences are externalized after many years of exposure to high blood pressure levels, usually to values previously not associated with CV risk. 101101. Fuchs FD. Essentials of hypertension. Cham, Switzerland, Springer; 2018. Doi:.org/10.1007/978-3-319-632728
https://doi.org/10.1007/978-3-319-632728...
The consequences of high BP can be classified by onset as early or late and comprise most CVD ( Chart 2.1 ). Recently, authors have theorized that CVD is predominantly caused by the rightward shift of the BP distribution curve on a global scale. 102102. Fuchs FD, Whelton PK. High Blood Pressure and Cardiovascular Disease. Hypertension. 2020;75(2):285-92.
There is little experimental evidence showing the long-term prevention of high BP. Running clinical trials to show the effectiveness of interventions in the early stages of high BP and, consequently, in decreasing outcomes is a major challenge, since it would require long intervention periods. Despite this limitation, the SPRINT-Mind trials showed that the strategy of lowering SBP to below 120 mm Hg was associated with the decreased incidence of mild cognitive impairment and dementia 103103. Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, et al - SPRINT Research Group. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA. 2019;321(6):553-61. as well as Alzheimer's markers in magnetic resonance imaging. 104104. Nasrallah IM, Pajewski NM, Auchus AP, Chelune G, Cheung AK, Cleveland ML, et al - SPRINT Research Group. Association of intensive versus standard blood pressure control with cerebral write matter lesions. JAMA 2019;322(6):524-34.
In addition to increased risk of clinical outcomes from high BP, there was also evidence of preclinical vascular and cardiac damage from BP readings lower than those traditionally used to diagnose HT. Cardiac consequences have also been found from mildly elevated blood pressure levels, categorized as prehypertension. 105105. Markus MR, Stritzke J, Lieb W, Mayer B, Luchner A, Döring A, et al. Implications of persistent prehypertension for ageing-related changes in left ventricular geometry and function: the MONICA/KORA Augsburg study. J Hypertens. 2008; 26(10):2040–9.,106106. Santos AB, Gupta DK, Bello NA, Gori M, Claggett B, Fuchs FD, et al. Prehypertension is associated with abnormalities of cardiac structure and function in the atherosclerosis risk in communities Study. Am J Hypertens. 2016; 29(5):568–74. The PREVER trial found that, in these cases, lowering BP leads to smaller ECG-estimated ventricular mass, 107107. Fuchs SC, Poli-de-Figueiredo Carlos E, Figueiredo-Neto JA, Scala LC, Whelton PK, Mosele F, et al. Effectiveness of chlorthalidone plus amiloride for the prevention of hypertension: the PREVER-Prevention randomized clinical trial. J Am Heart Assoc. 2016;5(12):e004248. as well as an almost 50% decrease in HT.
Risk estimates for increased incidence for the diseases listed in Chart 2.1 have increased significantly in recent years as lower BP values were included in mathematical models. The most conservative attribute 49% of infarctions and 62% of strokes to BP above 115/75 mm Hg. 108108. World Health Organization. (WHO) The world health report 2002 - Reducing Risks, Promoting Healthy Life (Internet). Geneva; 2002.
Many justifications have been offered to explain centenarians' life spans. Curiously, even reports that found late onset of HT and CV events for these individuals 109109. Andersen SL, Sebastiani P, Dworkis DA, Feldman L, Perls TT. Health span approximates life span among many supercentenarians: compression of morbidity at the approximate limit of life span. J Gerontol A Biol Sci Med Sci. 2012; 67(4):395–405. did not attribute a causal relationship between those conditions. Considering the discussion above, it is natural to conclude that vascular aging is not inexorable. 102102. Fuchs FD, Whelton PK. High Blood Pressure and Cardiovascular Disease. Hypertension. 2020;75(2):285-92. Therefore, it can be deduced that the key for very long life spans probably consists of maintaining BP at actually normal values. More recently, the 14-year follow-up of participants in the MESA (Multi-Ethinic Study of Atherosclerosis) study 110110. Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, et al. Association of Normal Systolic Blood Pressure Level with Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiol.2020:5(9):1011-8. with no other CV risk factors found that SBP above 100 mmGg increased the risk of CV events threefold compared to participants with SBP between 90 and 99 mm Hg.
The evidence available allow us to hypothesize that, in the future, reference values for a HT diagnosis, as well as therapeutic targets, may be changed and brought closer to levels we now consider normal or optimum BP. More solid and robust evidence is still needed before that change can occur, however.
2.3. Blood Pressure, Inflammation, and Endothelial Dysfunction
HT and its complications are mediated by various mechanisms sharing one common trait, ie, endothelial dysfunction, characterized by the low availability of nitric oxide (NO) and the consequent local imbalance between arteriole relaxing and contracting factors. 111111. Kanel WB, Larson M. Long Term epidemiologic prediction of coronary disease. The Framingham Experience. Cardiology. 1993; 82(2-3):137-52. Endothelial dysfunction is a consequence of the imbalance between endothelial NO synthase (eNOS) or the transformation of NO into the free radical peroxynitrite (NOO-). 112112. Konukoglu D, Uzun H. Endothelial Dysfunction and Hypertension. Adv Exp Med Biol. 2017; 956:511-40. In that case, vasodilation mediated by several peptides, including bradykinin and angiotensin 1-7, is impaired, leading to increased peripheral vascular resistance and alterations in endothelial permeability. The onset of a chronic inflammatory state in HT patients via the increased production of proinflammatory cytokines (eg, leukocyte adhesion molecules such as endothelin-1 and angiotensin II) decreases eNOS expression, 113113. Bautista LE, Lopez-Jaramillo P, Vera LM, Casas JP, Otero AP, Guaracao AI. Is C-reactive protein an independent risk factor for essential hypertension? J Hypertens. 2001; 19(5):857-61.
114. Boos CJ, Lip GY. Is hypertension an inflammatory process? Curr Pharm Des. 2006; 12(13):1623-35.-115115. Grundy SM. Inflammation, hypertension, and the metabolic syndrome. JAMA. 2003; 290(22):3000-2. while increased oxidative stress accelerates NO degradation. Reduced local NO availability increases smooth vascular muscle tone, induces smooth muscle cell proliferation in the medial layer, and increases endothelial permeability, facilitating the passage of low-density lipoprotein (LDL-c) into the subendothelial space, which seems to be the initial event behind the onset of atherosclerosis. Thus, endothelial dysfunction would be at the root of two chronic diseases that usually go together, ie, HT and atherosclerosis. Therefore, identifying the degree of endothelial dysfunction might be an important step in assessing the clinical course of HT. At the biochemical level, ultrasensitive C-reactive protein (CRP) seems to be the most adequate clinically available marker to assess endothelial dysfunction.
Currently, the most widely used technique for analyzing endothelial function in vivo in clinical settings is brachial artery FMD, 116116. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39(2):257-65.
117. Thijssen DHJ, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. 2011; 300(1):2-12.
118. Thijssen DHJ, Bruno RM, van Mil ACCM, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019; 40(30):2534-47.-119119. Moens AL. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest. 2005; 127(6):2254-63. a noninvasive ultrasound method correlated with coronary endothelial function 120120. Celermajer DS, KE Sorensen, VM Gooch, DJ Spiegelhalter, OI Miller, ID Sullivan, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340(8828):1111-5.,121121. Takase B, A Uehata, T Akima, T Nagai, T Nishioka, A Hamabe, et al. Endothelium-dependent flow-mediated vasodilation in coronary and brachial arteries in suspected coronary artery disease. Am J Cardiol. 1998; 82(12):1535-9. and an independent predictor of CV disease. 121121. Takase B, A Uehata, T Akima, T Nagai, T Nishioka, A Hamabe, et al. Endothelium-dependent flow-mediated vasodilation in coronary and brachial arteries in suspected coronary artery disease. Am J Cardiol. 1998; 82(12):1535-9.,123123. Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010; 26(6):631-40. However, its availability is limited. Endothelium-dependent dilation is a consequence of brachial artery relaxation in response to increased shear stress and local release of NO. 119119. Moens AL. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest. 2005; 127(6):2254-63. The association between FMD and CV prognosis is that it reflects the bioavailability of NO. 124124. Green D, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-Mediated Dilation and Cardiovascular Event Prediction: Does Nitric Oxide Matter? Hypertension. 2011; 57(3):363-9. FMD may improve the predictive power of risk calculations based on traditional risk factors, including for young hypertensive patients. 119119. Moens AL. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest. 2005; 127(6):2254-63.,123123. Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010; 26(6):631-40. Antihypertensive medications that increase the bioavailability of NO and statins may be an interesting option for clinical management 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,125125. Soloviev MA. Correction of endothelial dysfunction in patients with arterial hypertension. Bull Exp Biol Med. 2011; 151(2):183-5. in order to maintain or preserve endothelial function for both asymptomatic patients and those with established CAD.
2.4. Blood Pressure and Arterial Stiffness
Assessments of vascular damage, a common finding in HT, are increasingly part of clinical practice. The damage involves microvascular alterations, atherosclerosis, increased arterial stiffness, and endothelial dysfunction. 126126. Persu A, De Plaen JF. Recent insights in the development of organ damage caused by hypertension. Acta Cardiologica. 2004; 59(4):369-81. There is probably a genetic component to arterial stiffness, 127127. Laurent S, Boutouyrie P, Lacolley P. Structural and Genetic Bases of Arterial Stiffness. Hypertension. 2005; 45(6):1050-5. but there are also two other important determinants: age and BP levels. 128128. Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, et al. Interaction Between Hypertension and Arterial Stiffness. An Expert Reappraisal. Hypertension. 2018; 72(4):796-805.
Age has greater impact on proximal (central) arteries, predominantly elastic, than on peripheral arteries, predominantly muscular. Central arteries grow stiffer with age, while muscular arteries change less. With age comes elastin fragmentation and generation and progressive accumulation of collagen, accompanied by calcium deposits in the medial layer of arteries, and consequently increased arterial stiffness. 128128. Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, et al. Interaction Between Hypertension and Arterial Stiffness. An Expert Reappraisal. Hypertension. 2018; 72(4):796-805.,129129. Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006; 27(21):2588–605.
Sustained BP increases trigger the onset of arterial medial hypertrophy, as it causes quantitative and qualitative alterations in the components of the arterial walls (elastin, collagen, and smooth muscle cells), leading to mechanical adaptations. 127127. Laurent S, Boutouyrie P, Lacolley P. Structural and Genetic Bases of Arterial Stiffness. Hypertension. 2005; 45(6):1050-5.,128128. Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, et al. Interaction Between Hypertension and Arterial Stiffness. An Expert Reappraisal. Hypertension. 2018; 72(4):796-805.,130130. Fridez P, Makino A, Kakoi D, Miyazaki H, Meister J, Hayashi K, et al. Adaptation of Conduit Artery Vascular Smooth Muscle Tone to Induced Hypertension. Ann Biomed Eng. 2002; 30(7):905–16. These findings have been described both for animal models 131131. Bardy N, Merval R, Benessiano J, Samuel JL, Tedgui A. Pressure and angiotensin-II synergistically induce aortic fibronectin expression in organ culture model of rabbit aorta. Circ Res. 1996; 79(1):70-8. and for in vitro studies and ex vivo organ cultures, 132132. Humphrey JD, Dufrense E, Schwartz MA. Mechanotransduction and extracellular matrix homeostasis. Nat Rev Mol Cell Biol. 2014;15(12):802-12.,133133. Liao D, Arnett DK, Tyroler HA, Riley WA, Chambless LE, Szklo M, et al. Arterial stiffness and the development of hypertension. Hypertension. 1999; 34(2): 201–6. where mechanosensitive cells respond to increased stress with extracellular matrix production. Therefore, HT accelerates vascular aging, a local mechanobiological response to increased induced stress from higher BP and, consequently, greater arterial stiffness (stiffness as a consequence). 128128. Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, et al. Interaction Between Hypertension and Arterial Stiffness. An Expert Reappraisal. Hypertension. 2018; 72(4):796-805.,134134. Humphrey JD, Harrison DG, Figueroa CA, Lacolley P, Laurent S. Central Artery Stiffness in Hypertension and Aging: A Problem with Cause and Consequence. Circ Res. 2016; 118(3):379–81.
However, several studies have found increased carotid or aortic stiffness in normotensive individuals, despite normal BP levels. 135135. Dernellis J, Panaretou M. Aortic stiffness is an independent predictor of progression to hypertension in nonhypertensive subjects. Hypertension. 2005; 45(3):426–31.
136. Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012; 308(9):875–81.
137. Weisbrod RM, Shiang T, Al Sayah L, Fry JL, Bajpai S, Reinhart-King CA, et al. Arterial stiffening precedes systolic hypertension in diet-induced obesity. Hypertension. 2013;62(6):1105-10.-138138. Van Gorp AW, van Ingen Schenau DS, Hoeks APG, Struijker Boudier HAJ, de Mey JGR, Reneman RS. In spontaneously hypertensive rats alterations in rat aortic wall properties precede development of hypertension. Am J Physiol. 2000;278(4):1241-7. Stiffer arteries create higher impedance for ventricular ejection, requiring higher blood pressure to keep blood flow constant. Thus, increased arterial stiffness may also lead to increased BP in the long run and, consequently, to CV risk. Studies have shown that arterial stiffness may precede HT, theorizing stiffness as a cause. Humphey et al. (2016) 134134. Humphrey JD, Harrison DG, Figueroa CA, Lacolley P, Laurent S. Central Artery Stiffness in Hypertension and Aging: A Problem with Cause and Consequence. Circ Res. 2016; 118(3):379–81. described the mechanism as neither cause nor consequence alone, but rather as both, ie, a positive feedback loop where stiffness leads to HT and HT leads to stiffness.
The impact of HT on the medial layer of arteries may be assessed using biomarkers capable of detecting damage and various levels of impairment, determining impact on mortality, predicting CV events, adding information to known risk factors, sufficiently stratifying risk to change therapeutic recommendations, and adding information to justify additional costs. 139139. Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífkova R, Cosentino F et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241(2):507-32. Biomarkers available for assessing arterial stiffness can be found in the following subsections.
2.4.1. Ankle-Brachial Index (ABI)
ABI is the ratio between systolic pressure in the ankle and the arm, 140140. Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. American Heart Association Council on Peripheral Vascular Disease. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012; 126(24):2890–909. considered a marker for arterial stiffness in patients without peripheral arterial disease. 141141. Rabkin SW, Him S, Sweeney C. Ankle-Brachial Index as an Indicator of Arterial Stiffness in Patients Without Peripheral Artery Disease. Angiology. 2012; 63(2):150-4. It may be measured using Doppler ultrasound or simply applying the oscillometric method, cheaper and more easily available, and readings obtained using both techniques are strongly correlated. 142142. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019; 42(9):1235–481. According to a 2008 meta-analysis, 143143. Fowkes FGR, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, et al. Ankle Brachial Index Combined with Framingham Risk Score to Predict Cardiovascular Events and Mortality: A Meta-Analysis. JAMA. 2008. 300(2):197-208. ABI ≤ 0.90 is associated with approximately twice the 10-year age-adjusted mortality, CV mortality, and higher rate of coronary events. Using ABI has led to the reclassification of CV risk categories and changing therapies for 19% of men and 36% of women. 143143. Fowkes FGR, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, et al. Ankle Brachial Index Combined with Framingham Risk Score to Predict Cardiovascular Events and Mortality: A Meta-Analysis. JAMA. 2008. 300(2):197-208. ABI as a predictor of cardiovascular risk is LR: IIa, LE: B.
| Level of recommendation | Level of evidence | |
|---|---|---|
| Blood pressure above 120 mm Hg increases vascular damage and cardiovascular risk | I | A |
| Use of serum markers to identify endothelial dysfunction | IIb | B |
| Use of brachial artery FMD (the gold standard technique for in vivo endothelial function analysis) in identification of endothelial dysfunction | IIb | B |
| Use of FMD for cardiovascular risk stratification | IIb | B |
| Arterial stiffness assessed with PWV is an independent predictor of cardiovascular risk, and its assessment, when possible, may make the risk stratification more accurate | IIa | A |
| ABI is an independent predictor of cardiovascular risk | IIa | B |
| Central blood pressure is an independent predictor of cardiovascular risk | IIa | B |
| Key Takeaways |
|---|
| Prehypertension increases cardiovascular risk. |
| Vascular damage is not found only in the hypertensive and may also be found in prehypertensives. |
| There are noninvasive tests to assess early vascular damage, but they are not always available. |
| Arterial stiffness analysis with PWV is an independent predictor of cardiovascular risk, and it may be assessed in clinical practice, when available. |
| Other methods, such as ABI and central blood pressure, may also be used to assess cardiovascular risk. FMD is more widely used in research settings. |
2.4.2. Pulse Wave Velocity (PWV)
PWV is considered the gold standard for arterial stiffness assessments due both to how easy it is to obtain and to the large body of evidence showing its association with CV disease regardless of traditional risk factors. 144144. Mattace-Raso FUS, Hofman A, Verwoert GC, Wittemana JCM, Wilkinson I, Cockcroft J, et al. Determinants of Pulse Wave Velocity in Healthy People and in the Presence of Cardiovascular Risk Factors: ‘Establishing Normal and Reference Values’. Eur Heart J. 2010; 31(19):2338–50.,145145. Boutouyrie P, Bruno RM. The Clinical Significance and Application of Vascular Stiffness Measurements. Am J Hypertens. 2019; 32(1):4-11.
Carotid-femoral PWV (cfPWV) is determined by dividing traveled distance by travel time (cfPWV = distance/time). The time may be measured directly in the same pulse wave or indirectly using an electrocardiogram. This noninvasive, robust and validated measure was standardized in an expert consensus document published by a European group in 2012. 146146. Van Bortel L, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Expert Consensus Document on the Measurement of Aortic Stiffness in Daily Practice Using Carotid-Femoral Pulse Wave Velocity. J Hypertens. 2012; 30(3):445-8.
Currently available validated methods include pulse tonometry 147147. Butlin M, Qasem A. Large Artery Stiffness Assessment Using SphygmoCor Technology. Pulse. 2016; 4(4):180–92.,148148. Weber T, M Ammer M, Rammer M, Adji A, O’Rourke MF, Siegfried Wassertheurer S, et al. Noninvasive determination of carotid–femoral pulse wave velocity depends critically on assessment of travel distance: a comparison with invasive measurement. Journal of Hypertension. 2009; 27(8):1624–30. and piezoelectric 149149. Stea F, Bozec E, Millasseau S, Khettab H, Boutouyrie P, Laurent S. Comparison of the Complior Analyse device with Sphygmocor and Complior SP for pulse wave velocity and central pressure assessment. J Hypertens. 2014; 32(4):873–80.,150150. Sztrymf B, Jacobs F, Chemla D, Richard C, Millasseau S. Validation of the new Complior sensor to record pressure signals non-invasively. J Clin Monit Comput. 2013; 27(6):613-9. and oscillometric mechanotransducers. 151151. Jones CR, Taylor K, Chowienczyk P, Poston L, Shennan AH. A validation of the Mobil O Graph (version 12) ambulatory blood pressure monitor. Blood Pressure Monitoring. 2000; 5(4):233–8.,152152. Hametner B, Wassertheurer S, Kropf J, Mayer C, Eber B, Weber T. Oscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood Press Monit. 2013; 18(3):173–6. In 2015, the American Heart Association published a position paper on standardizing the use of these devices to assess arterial stiffness. 8282. Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness A Scientific Statement from the American Heart Association. Hypertension. 2015; 66(3):698-722.
Increased arterial stiffness is predictive of outcomes. This was shown for cfPWV in hypertensive patients in the early 2000s 153153. Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001; 37(5): 1236-1241.,154154. Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002; 39(1): 10-5. and confirmed in several studies and two subsequent meta-analyses. 155155. Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 55(13):1318-27.,156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46. The first meta-analysis, from 2010, 155155. Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 55(13):1318-27. included 15877 patients from 17 trials, and showed that, risk-adjusted for age, sex, and risk factors, a 1 m/s increase in PWV led to a 14% increase in CV events, 15% in CV mortality, and 15% in all-cause mortality. In addition, a one standard deviation increase was associated to increases of 47%, 47%, and 42%, respectively. The second meta-analysis, published in 2014, 156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46. featuring 17635 patients from 16 trials, found that, for every one standard deviation increase in PWV, the risk increased 35% for CAD, 54% for stroke, and 45% for CVD.
As well as predicting outcomes, adding PWV to traditional CV risk factors helps with stratification. The first study to show improved risk stratification from adding PWV to other CV risk factors was performed on a population sample from the Framingham cohort. 157157. Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010; 121(4): 505-11. Later, the meta-analysis by Ben-Shlomo et al. (2014) 156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46. showed a 13% increase in risk prediction for individuals at intermediate risk when PWV was added.
Though PWV is relevant for event prediction and risk stratification, it is still little used in clinical practice. In 2019, a European group published a score 158158. Xaplanteris P, Vlachopoulos C, Protogerou AD, Aznaouridis K, Terentes-Printzios D, Argyris AA, et al. A clinical score for prediction of elevated aortic stiffness: derivation and validation in 3943 hypertensive patients. J Hypertens. 2019,37:339–4. based on clinical variables to prioritize individuals for PWV assessments. The score assesses easily available clinical variables and is known by the acronym SAGE: S ( systolic blood pressure ), A ( age ), G ( fasting plasma glucose ), and E ( estimated glomerular filtration rate ). PWV increases can be predicted accurately from that score. Therefore, we can prioritize arterial stiffness assessments for select hypertensive patients, improving its deployment in clinical practice.
The cutoff value for normal PWV, in most studies and guidelines, is under 10 m/s. However, due to the influence of age on arterial stiffness, current proposed reference values take into account the various age ranges and sex, as established by the European group in 2010 144144. Mattace-Raso FUS, Hofman A, Verwoert GC, Wittemana JCM, Wilkinson I, Cockcroft J, et al. Determinants of Pulse Wave Velocity in Healthy People and in the Presence of Cardiovascular Risk Factors: ‘Establishing Normal and Reference Values’. Eur Heart J. 2010; 31(19):2338–50. using tonometry, and more recently in a Brazilian study using oscillometric devices ( Table 2.1 ). 159159. Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP et al. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Jun 12.doi: 10.1038/s41440-020-0490 online ahead of print.
https://doi.org/10.1038/s41440-020-0490 ...
PWV as a predictor of cardiovascular risk is LR: IIa, LE: A.
– Reference values for central systolic pressure and pulse wave velocity in Brazilian and European populations with and without cardiovascular risk factors69,84,85
2.4.3. Central Blood Pressure
Central (aortic, carotid) blood pressure does not correspond to peripheral (brachial) blood pressure due to pulse amplification from the aorta to the periphery; the former is more relevant for CV pathogenesis than the latter. 160160. Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar M, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2013; 31:1865–71. Currently, central blood pressure can be easily measured by noninvasive methods using the same equipment utilized and validated for measuring PWV. 151151. Jones CR, Taylor K, Chowienczyk P, Poston L, Shennan AH. A validation of the Mobil O Graph (version 12) ambulatory blood pressure monitor. Blood Pressure Monitoring. 2000; 5(4):233–8.,161161. Ding FH, Fan WX, Zhang RY, Zhang Q, Li Y, Wang JG. Validation of the Noninvasive Assessment of Central Blood Pressure by the SphygmoCor and Omron Devices Against the Invasive Catheter Measurement. American Journal of Hypertension. 2011; 24(12):1306-1311.,162162. Pereira T, Maldonado J, Coutinho R, Cardoso E, Laranjeiro M, Andrade I, et al. Invasive validation of the Complior Analyse in the assessment of central artery pressure curves: a methodological study. Blood Press Monit. 2014; 19(5):280–7.
Central hemodynamic indices are independent predictors of future CV events and all-cause mortality according to the meta-analysis by Vlachoupoulos et al., which included 11 studies and a total of 5648 individuals with a mean follow-up period of 45 months. 160160. Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar M, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2013; 31:1865–71. Central blood pressure reference values were established by the European group in 2014 using tonometry, 163163. Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, on behalf of The Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure andi ts amplification in a general healthy population and according to cardiovascular risk factors. Eur Heart J.2014; 35(44):3122-3. and more recently in a Brazilian study with oscillometric devices ( Table 2.1 ). 159159. Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP et al. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Jun 12.doi: 10.1038/s41440-020-0490 online ahead of print.
https://doi.org/10.1038/s41440-020-0490 ...
Central blood pressure as a predictor of cardiovascular risk is LR: IIa LE: B.
3. Diagnosis and Classification
3.1. Introduction
The initial assessment of a patient with hypertension (HT) comprises diagnostic confirmation, suspicion, and identification of the secondary cause, and assessment of cardiovascular (CV) risks. End-organ damage (EOD) and associated diseases should also be investigated. The assessment comprises blood pressure (BP) measurement in and/or out of the office, using proper techniques and validated and well calibrated equipment, taking the patient's medical history (personal and family), physical examination, and clinical and laboratory investigation. All hypertensive patients should undergo general assessments, in addition to complementary assessments for specific groups. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
3.2. Blood Pressure Measurement at the Physician's Office
All medical assessments should include blood pressure measurements, whatever their specialty, and all other health care professionals should be properly trained in the process. Diagnosing HT and its phenotypes, as well as the management of the diagnosis, is the exclusive province of physicians.
Auscultatory or oscillometric sphygmomanometers are the preferred instruments for BP measurement. These devices should be validated according to standardized protocols and conditions, 165165. Stergiou GS, Alpert B, Mieke S, Asmar R, Atkins N, Eckert S, et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. J Hypertens. 2018;36(3):472-8. and their calibration checked annually (for oscillometric devices) or every six months (for auscultatory devices), or following Inmetro/Ipem recommendations. 166166. Brazil. Ministério do Desenvolvimento, Indústria e Comércio Exterior. Instituto Nacional de Metrologia, Qualidade e Tecnologia – Portaria n.46 de 22 de janeiro de 2016. Esfigmomanometros. [Internet] [Acesso em 25 fev 2020]. Disponível em: http://www.inmetro.gov.br/legislacao/rtac/pdf/RTAC002373.pdf .
http://www.inmetro.gov.br/legislacao/rta...
Initially, BP should be measured in both arms, preferably by simultaneous double arm measurement. If the difference between arms is > 15 mm Hg for SBP, there is increased CV risk, 167167. Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet 2012;379(9819):905–14. which may be connected to atheromatous vascular disease. All subsequent measurements should be performed on the arm with the highest BP values. If HT secondary to coarctation of the aorta is suspected, blood pressure should also be measured in the lower limbs, using properly sized cuffs for arm or thigh circumference ( Chart 3.1 ). 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
In older adults, diabetic patients, dysautonomia patients, or individuals taking antihypertensive medications, BP should also be measured 1 minute and 3 minutes after standing up (motionless). 168168. Saedon NI, Pin Tan M, Frith J. The Prevalence of Orthostatic Hypotension: A Systematic Review and Meta-Analysis. J Gerontol A Biol Sci Med Sci. 2020 Jan 1;75(1):117-22. Orthostatic hypotension is defined as a SBP decrease ≥ 20 mm Hg or a DBP decrease PAD ≥ 10 mm Hg within the 3rdminute standing up and is associated with higher risk of mortality and cardiovascular events. 169169. Fagard RH, De Cort P. Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. Hypertension 2010;56(1):56–61.
Charts 3.2 and 3.3 summarize the procedures and steps recommended for proper BP measurement. It should be stressed that improper BP measurements may lead to inaccurate classification, overestimating or underestimating the patient's true BP, and consequently to unnecessary treatment or lack of treatment for misassessed hypertensive patients. Given the simplicity of measuring BP by oscillometry, using a brachial oscillometric device may be preferable to auscultation when both techniques are available. 170170. Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, Zarnke KB. et al. Hypertension Canada’s 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults. Can J Cardiol. 2017;33(5):557-76. The differences between both techniques for measuring BP are highlighted in Chart 3.3 .
In the Systolic Blood Pressure Intervention Trial (SPRINT), 8686. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16. a new mode of measuring BP at the physician's office without an attending health care professional was used, known as unobserved automated office blood pressure measurement (UAOBPM). In this technique, after duly instructed, the patient measures their own blood pressure in a room set aside for that purpose. In SPRINT, participants followed a protocol where they waited in a quiet room for five minutes, then an automated device measured their BP three times, with one minute intervals, and recorded the readings. UAOBPM improves BP measurement reproducibility, and the white-coat effect may be significantly lowered or even eliminated. 171171. Myers MG. A short history of automated office blood pressure - 15 years to SPRINT. J Clin Hypertens (Greenwich) 2016;18:721–724.,172172. Parati G, Pomidossi G, Casadei ParatiR, Mancia G. Lack of alerting reactions to intermitent cuff inflations during noninvasive blood pressure monitoring. Hypertension 1985;7:597–601. In UAOBPM, readings are similar or lower than those obtained via ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring (HBPM). 173173. Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension 2010;55:195–200. However, one cannot forget that conventional office BP measurement is the basis for all currently available clinical and epidemiological data.
For obese individuals, optimum cuff size and shape to fit the patient's arm is critical. Proper cuff choice depends on both the circumference and the shape of the arm. 174174. Palatini P, Asmar R. Cuff challenges in blood pressure measurement. J Clin Hypertens. 2018; 20:1100–3 Longer and wider cuffs are required for measurements in these patients to avoid overestimating BP. The forearm approach should be considered valid and may be used in clinical settings for BP measurement when severe obesity makes measurement in the upper arm too challenging (arm circumference greater than 50 cm, for which there are no cuffs available). In these situations, the radial pulse should be auscultated, though there are limitations to that practice. 175175. Leblanc MÈ, Auclair A, Leclerc J, Bussières J, Agharazii M, Hould FS, et al. Blood pressure measurement in severely obese patients: validation of the forearm approach in different arm positions. Am J. Hypertens 2019;32(2):175–85,176176. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697-716. Cone-shaped, wide, short arms that do not fit large cuffs represent a particular challenge for BP measurement. The use of validated heart rate monitors should also be considered in these cases. 177177. Senarclens et al.Brachial or wrist blood pressure in obese patients:which is the best? Blood Pressure Monitoring 2008, 13:149–151.,178178. Irving G, Holden J, Stevens R, McManus RJ. Which cuff should I use? Indirect blood pressure measurement for the diagnosis of hypertension in patients with obesity: a diagnostic accuracy review. BMJ Open.2016;6:e012429. doi: 10.1136/bmjopen-2016-012429
3.3. Classification
The BP limits considered normal are arbitrary. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,179179. Fuchs FD, Scala LC, Vilela-Martin JF, de Mello, RB, Mosele, F, Whelton, PK, et al. Effectiveness of chlorthalidone/amiloride versus losartan in patients with stage I hypertension: results from the PREVER-treatment randomized trial. J Hypertens. 2016;34(4):798-806. The values used to classify BP in adults by using casual or office measurements are shown in Chart 3.4 . Individuals are considered hypertensives if SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg. When using office measurements, the hypertension diagnosis should always be validated with repeated readings, under ideal conditions, on at least two visits made days or weeks apart; or more assertively by using out-of-office measurements (ABPM or HBPM), except for patients already presenting with EOD or CV disease. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. Patient classification follows the office BP measure and the highest BP level, either systolic or diastolic.
Individuals with SBP ≥ 140 mm Hg and DBP < 90 mm Hg are classified as having isolated systolic HT, while SBP < 140 mm Hg and DBP ≥ 90 mm Hg is characteristic of isolated diastolic HT. Both isolated systolic HT and isolated diastolic HT have higher rates of white-coat HT (WCH). 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.
In the previous Brazilian guidelines, 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. what was then called normal BP is now known as optimum BP, while prehypertension is now divided into normal BP and prehypertension. Individuals with SBP from 130 to 139 and DBP from 85 to 89 mm Hg are now considered prehypertensive, since that population has shown a consistently higher risk of CV disease, coronary artery disease, and stroke than populations with BP between 120 and 129 or 80 and 84 mm Hg. They are also at greater risk of having masked hypertension (MH). 181181. Weber MA, Schiffrin EL, White WA, Mann S, Lindbolm LH, Venerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15.,182182. Egan BM, Stevens-Fabry S. Prehypertension-prevalence, health risks, and management strategies. Nat Rev Cardiol. 2015;12(5):289-300. Consequently, prehypertensive individuals should be monitored closely.
3.4. Out-of-Office Blood Pressure Measurement
Out-of-office BP may be measured using ABPM or HBPM, following its indications and restrictions. 183183. Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014;32(7):1359–66.
184. Stergiou GS, Parati G, Vlachopoulos C, Achimastos A, Andreadis E, Asmar R, et al. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: current status and future directions - Position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular variability. J Hypertens 2016;34(9):1665–77.
185. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure M. European Society of Hypertension position paper on ambulatory blood pressure monitoring. Hypertens 2013;31(9):1731–68.
186. Nobre F, Mion Jr. D, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 110(5Supl.1):1-29.-187187. Souza WK, Jardim PC, Porto LB, Araújo FA, Sousa AL, Salgado CM. Comparison and correlation between self-measured blood pressure, casual blood pressure measurement and ambulatory blood pressure monitoring. Arq Bras Cardiol. 2011;97(2):148-55. Out-of-office BP measurements should be encouraged. The major advantages and disadvantages of out-of-office BP measurement are summarized in Chart 3.5 , while its primary indications, as well as specific indications for HBPM, can be found in Chart 3.6 .
ABPM and HBPM should not be mistaken for self-measured blood pressure (SMBP), performed by patients themselves using automated devices, which do not follow any pre-established protocol. The measurements are made at random, at the patient's discretion or as requested by the physician. 188188. Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30(7):1289–99.
The COVID-19 pandemic has accelerated the development of telemedicine (televist, telecounseling, and telemonitoring), a change we believe to be irreversible. Currently, the Brazilian Unified Health System (SUS) already provides COVID-19 telecounseling, and supplementary health care services have already adopted it as well. Here, SMBP has the possibility of contributing to diagnosis, follow-up and treatment for hypertensive patients. To that end, this guideline recommends the use of high-quality oscillometric devices, ie, preferably brachial cuff-based devices that have been validated. Wrist blood pressure monitors should be discouraged, but where used, give preference to validated devices that include height and motion sensors. A minimum of seven measurements, performed during a 16- to 72-hour period, is recommended. Thus far, recommended normal values are the same as for HBPM, though specific studies and trials are still needed to compare BP values observed using each technique. 187187. Souza WK, Jardim PC, Porto LB, Araújo FA, Sousa AL, Salgado CM. Comparison and correlation between self-measured blood pressure, casual blood pressure measurement and ambulatory blood pressure monitoring. Arq Bras Cardiol. 2011;97(2):148-55.,189189. WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167-74.
The definition of hypertension by BP at the physician's office is shown on Chart 3.7 . Compared to office BP readings, HBPM values are usually low, and the diagnostic threshold for BP is ≥ 130/80 mm Hg (equivalent to office BP ≥ 140/90 mm Hg). 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,190190. Park JS, Rhee MY, Namgung J, Lee SY, Cho DK, Choi TY, et al. Comparison of Optimal Diagnostic Thresholds of Hypertension With Home Blood Pressure Monitoring and 24-Hour Ambulatory Blood Pressure Monitoring. Am J Hypertens. 2017 Nov 6;30(12):1170-6.
191. Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, et al. Outcome-Driven Thresholds for Home Blood Pressure Measurement: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 2012, 61(1), 27–34.-192192. D, Asayama K, Ohkubo T, Kikuya M, Kanno A, Hara A, et al. Stroke Risk in Treated Hypertension Based on Home Blood Pressure: the Ohasama Study. Am J Hypertens. 2010;23(5):508-14. HBPM offers more reproducible BP values and is more strongly related to EOD, particularly left ventricular hypertrophy, and to CV morbidity and mortality than office BP. 188188. Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30(7):1289–99.,193193. Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens 2012;30(3):449–56. There is also evidence that HBPM may offer a beneficial effect in terms of adherence to medication and BP control, 194194. McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, et al. Telemonitoring and selfmanagement in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010;376(9736):163–72.,195195. McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799–808. especially when combined with guidance and counseling. 196196. Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS One.2017;14:e1002389. Telemonitoring and smartphone applications may offer additional advantages for HBPM, 197197. Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens 2013;31(3):455–67; discussion 467–8.,198198. Parati G, Omboni S. Role of home blood pressure telemonitoring in hypertension management: an update. Blood Press Monit. 2010;15(6):285–95. such as BP measurement reminders and a convenient way to store and edit BP data in a digital report.
ABPM is a better predictor of CV risk and EOD than office BP. 199199. Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens. 2008;26(10):1919–27. In addition, 24-hour ambulatory BP means are better correlated with fatal or nonfatal events, 200200. Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348(24):2407–15.,201201. Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111(14):1777–83. such as fatal and nonfatal coronary events and strokes. 202202. ABC-H Investigators, Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32(12):2332–40; discussion 2340.
203. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51(1):55–61.
204. Parati G, Ochoa JE, Bilo G, Agarwal R, Covic A, Dekker FW, et al. Hypertension in chronic kidney disease part 2: role of ambulatory and home blood pressure monitoring for assessing alterations in blood pressure variability and blood pressure profiles. Hypertension. 2016;67(6):1102–10.-205205. Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162(3):192–204.
3.5. White-Coat Effect (WCE) and Masking Effect (ME)
The difference in BP between measurements taken at the physician's office and out of it is known as WCE or ME, when the values are positive or negative, respectively. Based on HBPM trials, differences equal to or higher than 15 mm Hg for SBP and/or 9 mm Hg for DBP indicate significant WCE, while differences equal to or lower than -1 mm Hg for SBP and/or DBP indicate significant ME. 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670. These scenarios do not change the diagnosis; ie, if the individual is normotensive, they remain normotensive, and if hypertensive, they remain hypertensive. However, it may be useful in identifying individuals at risk of significant BP differences at and out of the physician's office, which may contribute to better therapeutic management.
3.6. White Coat Hypertension (WCH) and Masked Hypertension (MH)
Several different phenotypes are possible for an HT diagnosis. True normotension (TNT) is defined as normal attended and unattended BP measurements, sustained HT (SHT) when both are abnormal, WCH when BP is high at the physician's office but normal outside it, and MH when BP is normal at the office, but high outside it. 206206. Mancia G, Zanchetti A. White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do next? J Hypertens. 1996;14(9):1049–52.,207207. Bobrie G, Clerson P, Menard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens. 2008;26(9):1715–25. Estimated prevalence rates in Brazil can be found in Figure 3.1 . 208208. Feitosa ADM, Mota-Gomes MA, Miranda RD, Barroso WS, Barbosa ECB, Pedrosa RP, et al. Impact of 2017 ACC/AHA hypertension guidelines on the prevalence of white-coat and masked hypertension: A home blood pressure monitoring study. J Clin Hypertens. 2018;20(12):1745-7.,209209. Paiva AMG, Gomes MICM, Campana EMG, Feitosa ADM, Sposito AC, Mota-Gomes MA, et al. Impact of hypertension phenotypes on the office and 24-h pulse wave velocity and augmentation index in individuals with or without antihypertensive medication use. Hypertens Res. 2019;42(12):1989-95.
– Population prevalence of hypertension according to various diagnostic criteria, in adults 18 or older, both genders, by age group (Brazil, 2013).
Though the prevalence varies between studies, WCH can be found in approximately 15 to 19% of individuals at the office and up to 30 to 40% of individuals with high BP at the office. It is more common among patients with stage 1 hypertension. 210210. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in whitecoat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25(11):2193-8.
211. Staessen JA, O’Brien ET, Amery AK, Atkins N, Baumgart P, De Cort P, et al. Ambulatory blood pressure in normotensive and hypertensive subjects: results from an international database. J Hypertens Suppl. 1994;12(7):S1-12.-212212. Barroso WKS, Feitosa ADM, Barbosa ECD, Miranda RD, Vitorino PVO, Brandão AA, et al Prevalence of Masked and White-Coat Hypertension in Pre-Hypertensive and Stage 1 Hypertensive patients with the use of TeleMRPA. Arq Bras Cardiol .2019;113(5):970-5.
The presence of EOD and the risk of CV events associated with WCH are lower than in SHT. 205205. Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162(3):192–204.,213213. Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35(4):677–88.,214214. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White-coat hypertension and cardiovascular events: a meta-analysis. J Hypertens. 2016;34(4):593–9. However, compared to TNT, WCH is associated with higher adrenergic activity, higher prevalence of metabolic risk factors, more frequent EOD and higher of developing diabetes mellitus, and progressing to SHT and left ventricular hypertrophy. 215215. Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52(6):1045–50.,216216. Rassi G, Seravalle G, Trevano FQ, Dell’oro R, Bolla G, Cuspidi C, Arenare F, Mancia G. Neurogenic abnormalities in masked hypertension. Hypertension 2007;50(3):537–42. In WCH, out-of-office BP values tend to be higher than in TNT, which might explain the increased long-term risk of CV events. 217217. Parati G, Omboni S, Staessen J, Thijs L, Fagard R, Ulian L, et al. Limitations of the difference between clinic and daytime blood pressure as a surrogate measure of the ‘white-coat’ effect. Syst-Eur investigators. J Hypertens. 1998;16(1):23–9.
218. Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J.2014;35(46):3304–12.
219. Mancia G. Clinical significance of white-coat hypertension. J Hypertens. 2016;34(4):623–6.
220. Mancia G. White-coat hypertension: growing evidence in favour of its adverse prognostic significance. J Hypertens. 2017;35(4):710–2.-221221. Mancia G, Grassi G. The heterogeneous nature of white-coat hypertension. J Am Coll Cardiol. 2016;68(19):2044–6.
Like WCH, the prevalence of MH may vary significantly across populations. However, overall, MH may be found in approximately 7 to 8% of individuals at the physician's office, and may total circa 15% of normotensives. 222222. Mancia G, Bombelli M, Cuspidi C, Facchetti R, Grassi G. Cardiovascular risk associated with white-coat hypertension: pro side of the argument. Hypertension. 2017;70(4):668–75.,223223. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219. Several factors can elevate out-of-office BP compared to office BP, such as being older, male, smoking, alcohol consumption, physical activity, exercise-induced hypertension, anxiety, stress, obesity, diabetes mellitus, chronic kidney disease, and family history of HT. MH is associated with dyslipidemia, dysglycemia , EOD, prehypertension, and adrenergic activity and increases the risk of progression to diabetes mellitus and SHT. 183183. Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014;32(7):1359–66.,185185. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure M. European Society of Hypertension position paper on ambulatory blood pressure monitoring. Hypertens 2013;31(9):1731–68.,198198. Parati G, Omboni S. Role of home blood pressure telemonitoring in hypertension management: an update. Blood Press Monit. 2010;15(6):285–95.,207207. Bobrie G, Clerson P, Menard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens. 2008;26(9):1715–25.,224224. Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24(1):52-8.
225. Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J, Staessen JA. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45(4):493–8.-226226. Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006;47(5):846–53. Meta-analyses of prospective studies report that the incidence of CV events is approximately twice as high in MH than in TNT, and comparable to that in HT. 210210. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in whitecoat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25(11):2193-8.,227227. Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291(11):1342–9.,228228. Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, et al. Response to masked hypertension in untreated and treated patients with diabetes mellitus: attractive but questionable interpretations and response to Is masked hypertension related to diabetes mellitus? Hypertension. 2013;62(4):e23–e25.
3.7. Uncontrolled Masked and White Coat Hypertension
WCH and MH were originally defined for people who were not being treated for HT. However, patients on antihypertensive medications may also have divergent BP behaviors in and out of the physician's office. The following terms are used for patients treated with antihypertensives: uncontrolled masked HT, when BP is controlled at the office, but high out of it; uncontrolled white-coat HT, when BP is high at the office, but normal out of it; uncontrolled sustained HT, when BP is high at and out of the office; and controlled HT, when BP is normal at and out of the office. 218218. Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J.2014;35(46):3304–12. Figure 3.2 shows the prevalence rates for these four phenotypes in Brazil. 213213. Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35(4):677–88.,214214. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White-coat hypertension and cardiovascular events: a meta-analysis. J Hypertens. 2016;34(4):593–9.
3.8. Diagnosis and Follow-Up Recommendations
HT is a habitually asymptomatic condition. Therefore, it should be assessed during doctor's visits and as part of structured population-based screening programs. In the latter, over 50% of HT patients did not known they had the disease. 229229. Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68.,230230. Lindholt JS, Sogaard R. Population screening and intervention for vascular disease in Danish men (VIVA): a randomised controlled trial. Lancet. 2017;390(10109):2256–65. BP should be measured at regular intervals, with frequency determined by BP classification ( Figure 3.3 ). Healthy individuals with optimum office BP (< 120/80 mm Hg) or normal BP (120-129/80-84 mm Hg) should have their BP measured at least one a year and during medical appointments. Patients suffering from prehypertension (130-139/85-89 mm Hg) should have their BP measured annually, or preferably more often than that, due to the high rates of progression to HT. In addition, if MH is suspected, ABPM or HBPM should be deployed to investigate the phenotype.
Since BP may be highly variable, a diagnosis of HT should not be based exclusively on BP values at a single visit, unless it is significantly elevated (stage 3 HT) or there is an established diagnosis of EOD or CV disease. For other patients, repeated BP measurements in subsequent visits to the physician's office should be used to verify persistent high BP as well as to stage the disease. The higher the stage, the more frequent the appointments should be and the shorter the interval between them. Therefore, stages 2 and 3 patients may require more frequent visits (days or weeks apart), while stage 1 patients may require visits after a few months, especially when there is no EOD and CV risk is low.
The guideline recommends the use of out-of-office BP measurements ( Figure 3.3 ) as an alternate strategy for repeated office BP measurements to confirm the HT diagnosis, as long as they are logistically and economically feasible. 231231. Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011 Jun 24;342:d3621. This approach may also generate relevant supplementary clinical information, such as detecting WCH and MH 213213. Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35(4):677–88.,214214. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White-coat hypertension and cardiovascular events: a meta-analysis. J Hypertens. 2016;34(4):593–9.,232232. Vinyoles E, Felip A, Pujol E, de la Sierra A, Dura R, del Rey RH, et al. Clinical characteristics of isolated clinic hypertension. J Hypertens, 2008;26(3):438–45. ( Chart 3.6 and Figure 3.3 ).
The exercise stress test is not recommended for the diagnostic assessment of HT due to several limitations, including lack of standardization in methods and definitions. Currently, there is no consensus about normal BP response to physical exercise.
3.9. Central Aortic Pressure
Several techniques have enabled the measurement of aortic BP (central BP) using algorithms based on brachial BP readings. 233233. Picone DS, Schultz MG, Otahal P, Aakhus S, Al-Jumaily AM, Black JA, et al. Accuracy of cuff-measured blood pressure: systematic reviews and meta-analyses. J Am Coll Cardiol. 2017;70(5):572–86.,159159. Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP et al. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Jun 12.doi: 10.1038/s41440-020-0490 online ahead of print.
https://doi.org/10.1038/s41440-020-0490 ...
Several studies show different reductions for central BP compared to brachial BP for select antihypertensive medications, and though central BP seems to be a better predictor of CV events than brachial BP, the added prognostic value of measuring central BP still requires more evidence. 160160. Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar M, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2013; 31:1865–71.,234234. Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–5.
Spurious HT (isolated systolic HT in young individuals with normal central BP) seems to be clearest case for use of central BP (when available) in clinical practice, making it the first indication for central BP measurement. It is found in a small fraction of young individuals, especially male athletes, but it remains unclear whether these patients are at lower CV risk than suggested by conventional BP measurements. 235235. Lurbe E, Redon J. Isolated systolic hypertension in young people is not spurious and should be treated: con side of the argument. Hypertension. 2016;68(2):276–80.
236. McEniery CM, Franklin SS, Cockcroft JR, Wilkinson IB. Isolated systolic hypertension in young people is not spurious and should be treated: pro side of the argument. Hypertension 2016;68(2):269–75.-237237. Miall WE, Oldham PD. The hereditary factor in arterial blood-pressure. BMJ. 1963 Jan;1(5323):75–80.
It should be stressed that the prognostic limitations of central BP are not applicable to other parameters associated with said measurements, such as pulse wave velocity (PWV) and augmentation index (AIx), which have well-established prognostic values. 238238. Snieder H, Hayward CS, Perks U, Kelly RP, Kelly PJ, Spector TD SO. Heritability of central systolic pressure augmentation: a twin study. Hypertension. 2000 Feb;35(2):574-9.
3.10. Genetics and Hypertension
Primary hypertension is a multifactorial, but with a strong genetic component. Family and twin studies have shown 30 to 50% heritability levels. 239239. Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50(10): 1412–25.,240240. Raina R, Krishnappa V, Das A, Amin H, Radhakrishnan Y, Nair NR et al. Overview of Monogenic or Mendelian Forms of Hypertension. Front Pediatr. 2019 Jul 01 ;7:263. Most of the genetic risk is polygenic, ie, it comes from the contribution of hundreds of DNA variants that, taken together and after interacting with the environment, increase the risk of developing a hypertensive phenotype. A recent study of over 1 million patients showed that DNA variations in over 900 genes are associated with BP control, explaining approximately 27% of the heritability of BP control. 240240. Raina R, Krishnappa V, Das A, Amin H, Radhakrishnan Y, Nair NR et al. Overview of Monogenic or Mendelian Forms of Hypertension. Front Pediatr. 2019 Jul 01 ;7:263. The study paves the way for the use of gene panels to assess HT risk, which might help guide preventive efforts.
In contrast with primary HT, various forms of secondary HT are caused by heritable single-gene mutations (monogenic HT), such as familial hyperaldosteronism, Liddle's syndrome, congenital adrenal hyperplasia, and hereditary pheochromocytoma and paraganglioma ( Chart 3.8 ). 240240. Raina R, Krishnappa V, Das A, Amin H, Radhakrishnan Y, Nair NR et al. Overview of Monogenic or Mendelian Forms of Hypertension. Front Pediatr. 2019 Jul 01 ;7:263.,241241. Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol. 2015;11(2):101–11. These causes should be investigated in patients suspected of secondary HT. Genetic diagnoses need to take into consideration proper treatment as well as allow genetic counseling for families and early screening for asymptomatic family members.
| Recommendation | LR | LE |
|---|---|---|
| BP should be classified as optimum, normal, prehypertension or stages 1 to 3, depending on BP measurement at the physician's office. | I | C |
| HT screening programs are recommended. All adults (≥ 18 years old) should have their BP measured at the physician's office, have their values recorded in their files, and be made aware of their BP. 160160. Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar M, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2013; 31:1865–71.,234234. Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–5. | I | B |
| Given the simplicity of measuring BP by oscillometry, using an automated brachial oscillometric device may be preferable to auscultation when both techniques are available. | I | C |
| Annual BP measurement is indicated if the office BP is < 140/90 mm Hg. | I | C |
| It is recommended that BP be measured in both arms, at least on the first visit, since differences in SBP greater than 15 mm Hg across arms might suggest atheromatous disease and is associated with increased CV risk. 167167. Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet 2012;379(9819):905–14. | I | A |
| If a difference in BP < 15mm Hg is found, it is recommended that all subsequent BP readings use the arms with the highest BP value. | I | C |
| It is recommended that the HT diagnosis be based on repeated office BP measurements, on multiple visits, except for stage 3 HT and especially for high-risk patients. Three BP measurements should be taken at each appointment, at 1 to 2 minute intervals; additional measurements should only be performed if the first two readings differ by > 10 mm Hg. The patient's BP is the mean of the last two BP readings. | I | C |
| It is recommended that the HT diagnosis be based on out-of-office BP measurements using ABPM and/or HBPM, as long as these measurement techniques are feasible (logistically and economically). | I | C |
| Out-of-office BP (ie, ABPM or HBPM) is specifically recommended for various clinical indications, such as identifying WCH and MH, quantifying treatment effects and identifying possible causes of side effects (eg, symptomatic hypotension). 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,170170. Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, Zarnke KB. et al. Hypertension Canada’s 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults. Can J Cardiol. 2017;33(5):557-76.,180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. 01,209 | I | A |
| Pulse pressure, BP variability and central BP may be considered, but are currently little used in routine clinical practice. They may provide useful additional information in certain circumstances and stand as valuable research instruments. | IIb | C |
| Genetic testing should be considered in specialized centers for patients suspected of rare monogenic causes of secondary HT or for those with pheochromocytoma. 240240. Raina R, Krishnappa V, Das A, Amin H, Radhakrishnan Y, Nair NR et al. Overview of Monogenic or Mendelian Forms of Hypertension. Front Pediatr. 2019 Jul 01 ;7:263. 241. Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol. 2015;11(2):101–11.-242242. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-42. |
IIa | B |
| Routine genetic testing for hypertensive patients is not recommended. | III | C |
| Key Takeaways |
|---|
| BP should be classified as optimum, normal, prehypertension or stages 1 to 3, depending on office BP. |
| HT screening programs are recommended. All adults (≥ 18 years old) should have their BP measured at the physician's office, have their values recorded in their files, and be made aware of their BP. |
| Annual BP measurement is indicated if the office BP is < 140/90 mm Hg. |
| It is recommended that the HT diagnosis be based on repeated office BP measurements, on multiple visits, or on out-of-office BP measured by ABPM and/or HBPM when either or both are feasible. |
| Out-of-office BP (ie, ABPM or HBPM) is specifically recommended for various clinical indications, such as identifying WCH and MH, quantifying treatment effects and identifying possible causes of side effects (eg, symptomatic anemia hypotension). |
4. Clinical and Complementary Assessment
4.1. Clinical History
The clinical assessment of hypertensive patients should follow the traditional methodology, consisting of taking their hypertensive patient, physical examination, and laboratory tests. Chart 4.1 summarizes the objectives. Following every step of the process will enable physicians to correctly diagnose hypertension (HT) and stratify cardiovascular and renal risks, contributing to a more adequate therapeutic strategy.
4.2. Clinical Assessment
4.2.1. History-Taking
A full patient history should be taken, including mandatory questions about timing of diagnosis and prior antihypertensive treatments (medications and dosage). In addition, symptoms indicating the progress of hypertension, especially the presence of end-organ damage (EOD), should be investigated. It is also important to establish the patient's personal history and to build a timeline to better understand their clinical condition.
Family histories should also be taken to corroborate a diagnosis of primary HT 243243. Murabito JM, Nam BH, D’Agostino RB Sr, Lloyd-Jones DM, O’Donnell CJ, Wilson PW. Accuracy of offspring reports of parenteral cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. 2004;140(6):434-40. (LR: I; LE: B). During the appointment, the patient should be asked, among others, about the presence of specific cardiovascular disease (CVD) and kidney disease risk factors, 244244. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr. J, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-52.
245. Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321-9.-246246. Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159(10):1104-9. comorbidities and biopsychosocial, cultural, and socioeconomic aspects. 244244. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr. J, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-52.,245245. Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321-9.,247247. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation. 2014;130(19):1692-9. Assessing the use of other nonantihypertensive medications, whether legal or illegal drugs, that might interfere with BP (Chapter 9) is critical, as is investigating the patient's clinical history for signs suggesting secondary causes of HT, as detailed in Chapter 15.
4.3. Physical Examination
A detailed physical examination should be performed, with proper and repeated BP and heart rate (HR) measurements, as described in Chapter 3, as well as the search for signs of EOD and findings that might suggest secondary causes of HT.
Anthropometric data, such as weight, height, as well as body mass index (BMI) calculation, 248248. Obesity Classification – World Obesity Federation. [Cited in 2020 Jan 12].Avaliable from: https://www.worldobesity.org/about/about-obesity/obesity-classification?_ga=2.27200504.476223329.1582981112-571126236.1582981112
https://www.worldobesity.org/about/about...
and abdominal circumference (AC) , 248248. Obesity Classification – World Obesity Federation. [Cited in 2020 Jan 12].Avaliable from: https://www.worldobesity.org/about/about-obesity/obesity-classification?_ga=2.27200504.476223329.1582981112-571126236.1582981112
https://www.worldobesity.org/about/about...
have normal reference values defined by the World Obesity Federation (available online at https://www.worldobesity.org/ . The assessment should include palpation and auscultation of the heart, carotid arteries, and pulses. Measuring the ankle-brachial index (ABI) is also encouraged, as is fundoscopy. 249249. Carter SA. Indirect systolic pressures and pulses waves in arterial occlusive disease of the lower extremities. Circulation. 1968;37(4):624-37.,250250. Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Health Study (CHS) Collaborative Reserch Group. Circulation. 1993;88(3):837-45. To calculate ABI, divide brachial systolic blood pressure (SBP) by ankle SBP for both the left and the right side. The normal arm/ankle SBP ratio is higher than 0.90. Mild obstruction is characterized by ABI from 0.71 to 0.90; moderate, from 0.41 to 0.70; and severe, from 0.00 to 0.40 (LR: IIa, LE: B). It is an important tool for diagnosing peripheral occlusive atherosclerotic disease and to determine the prognosis for cardiovascular events. 250250. Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Health Study (CHS) Collaborative Reserch Group. Circulation. 1993;88(3):837-45.
In some cases, measuring central blood pressure (CBP) in order to detect isolated systolic hypertension in young individuals (spurious hypertension of youth) may be recommended, since, unlike brachial artery readings, CBP is not high in these situations (LR: IIa, LE: B) (Chapter 3). 251251. Rourke MF, Adji A. Guidelines on guidelines: focus on isolated systolic hypertension in youth. J Hypertens. 2013;31(4):649–54.,252252. Brandão AA, Amodeo C, Alcantara C, Barbosa E, Nobre F, Pinto F, et al. I Posicionamento Luso-Brazileiro de Pressão Arterial Central. Arq Bras Cardiol. 2017;108(2):100-8. Chart 4.2 shows a summary of the physical examination.
4.3.1. Basic Laboratory Investigation, Assessment of Subclinical and Clinical End-Organ Damage
The goal of complementary assessment is to detect subclinical or clinical end-organ damage to better stratify cardiovascular (CV) risk. To stratify global CV risk, in addition to classical risk factors ( Chart 4.3 ), other, recently-identified risk factors should also be considered, although not all have been incorporated into clinical scores. 253253. Mancia G, Narkiewiczk, Redon J, Zanchetti A, Bohm M, Christiaens T et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: theTask Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357.,254254. D’Agostino Sr RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WBl. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6): 743–53. Important elements in this investigations include altered glycemia or glycated hemoglobin, abdominal obesity (metabolic syndrome), pulse pressure > 65 mm Hg in older adults, history of pre-eclampsia/eclampsia, and family history of HT (for borderline hypertensive patients). 254254. D’Agostino Sr RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WBl. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6): 743–53.
Changes in pulse wave velocity (PWV), when available, are indicative of EOD, and may reclassify intermediate CV risk patients as high-risk (LR: IIa, LE: A) (Chapter 2). 156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46. Basic laboratory assessment ( Chart 4.4 and 4.5 ) should be part of the initial routine for all hypertensive patients. 253253. Mancia G, Narkiewiczk, Redon J, Zanchetti A, Bohm M, Christiaens T et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: theTask Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357. The recommended tests are serum potassium, uric acid, creatinine, glycemia, and lipid profile, as well as urinalysis and an electrocardiogram for possible left ventricular hypertrophy.
To assess renal function, one should obtain the estimated glomerular filtration rate using the Modification of Diet in Renal Diseases (MDRD) 255255. Levey AS, Bosch JP, Lewis JB, Greene LT, Rogers N, Roth D. A more accurate accurate method to estimate GFR from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461-70. formula or, preferably, the Chronic Kidney Diseases Epidemiology Collaboration (CKD-EPI) 256256. . A New Equation to Estimate Glomerular Filtration Rate. Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI). Ann Intern Med. 2009;150(9):604-12. formula, available at http://mdrd.com/.
Figure 4.1 shows the estimated glomerular filtration rate (eGFR) accompanied by staging (stages 1 through 5) and prognosis for chronic kidney disease and considering albuminuria levels, according to the Kidney Diseases Improving Global Outcomes (KDIGO) guidelines. 257257. Levey AS, Eckardt K-U, Dorman NM, Christiansen SL, Hoorn EJ, Ingelfinger JR, et al. Nomenclature for kidney function and disease: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Inter. 2020 97(6):1117–29.,258258. KDIGO CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013, 3(1):1-150. The colors indicate renal prognosis and management. Green means low risk and good prognosis; yellow, intermediate risk, patient should be monitored; orange, high risk, poor prognosis, mandatory referral to specialist; red, very high risk, poor prognosis, mandatory referral to specialist.
In terms of renal assessment:
It is recommended that the clinical laboratory make the creatinine test results available along with the eGFR results (LR: I, LE: B);
Creatinine clearance results (24 h urine) are not recommended, except for significant changes in muscle mass (amputation), body surface at the extremities and clinical instability (LR: I, LE: B);
It is recommended that the urine protein to albumin ratio be analyzed, in order of importance: urine albumin to creatinine ratio (ACR), urine protein to creatinine ratio (PCR), protein urine test strips with automated or manual reading. It is recommended that clinical laboratories report ACR and PCR for all urine samples and not just their concentrations (LR: I, LE: B).
| Key Takeaways |
|---|
| A full medical history and physical examination should always include proper BP measurement, analysis of anthropometric parameters and investigation of signs and symptoms of end-organ impairment and secondary causes of hypertension. |
| In hypertensive patients, it is important to investigate comorbidities (diabetes mellitus, dyslipidemia, and kidney and thyroid disease, among others) to improve CV risk stratification and treatment. |
| The routine supplementary tests recommended in this guideline are basic, easily available and easy to interpret, low-cost and mandatory for all patients, at least in their first visit and once a year. Other tests are required for indicated populations. |
| Investigating end-organ damage, both clinical and subclinical, is essential for fuller therapeutic guidance. |
5. Cardiovascular Risk Stratification
5.1. Introduction
There is a widely established causal, linear, and continuous relation between increased blood pressure (BP) and risk of cardiovascular disease (CVD) for both sexes, all ages, and all ethnic groups. 8585. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67. BP interacts synergically with other CVD risk factors (RFs), and its pro-atherogenic effect is proportional to the number and intensity of these additional factors. 7878. Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13.,273273. NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389 (10064):37-55. CVD is a multifactorial condition, dependent on synergic interactions in the whole causal system responsible for its development. In addition, modest increases in several RFs may trigger greater increases in cardiovascular (CV) risk than sharp increases in a single RF. 273273. NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389 (10064):37-55.,274274. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global Burden of hypertension: analysis of worldwide data. Lancet. 2005 Jan 15-21; 365(9455):217-23. Therefore, quantifying risk for hypertensive patients, ie, the probability of a given individual developing CVD during a given period, is an essential part of the process and can help guide preventive and treatment strategies. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
It should be stressed that the impact of hypertension (HT) control is proportional to the absolute individual risk and to the global estimated risk. 276276. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H and Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-47.
277. Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(1):56-64.-278278. Blood Pressure Lowering Treatment Trialists C. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-8. It is noteworthy that the concept of residual risk represents the magnitude of the risk remaining after traditional risk factors are under control. 279279. Matsura Y, Kanter JE, Bornfeldt KE. Highlighting Residual Atherosclerotic Cardiovascular Disease. Arterioscler Thromb Vasc Biol. 2019;39(1):e1-e9. Partial RF control and/or late onset of effective therapeutic measures may be key elements for residual CV risk in hypertensive patients. Despite the lack of tools for the identification of residual risk, it is clear that early and accurate RF control is essential. 279279. Matsura Y, Kanter JE, Bornfeldt KE. Highlighting Residual Atherosclerotic Cardiovascular Disease. Arterioscler Thromb Vasc Biol. 2019;39(1):e1-e9. Thus, a comprehensive approach to all RFs is fully justified. To that end, when identified, hypertensive patients should be told about risk factors potentially subject to change in order to improve the efficacy of both pharmacological and nonpharmacological measures. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
CV risk should not be estimated intuitively or by simply adding up the RFs observed, but rather through the application of methods that take into consideration its complex and multifactorial nature. 44. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232. The process should be based on equations or algorithms, 44. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.,280280. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.,281281. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk 2020. Eur Heart J. 2020;41(1):111-88. instruments that estimate risk based on multivariate regression models based on population-level studies and are recommended by multiple guidelines worldwide. 44. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.,280280. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.,281281. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk 2020. Eur Heart J. 2020;41(1):111-88. Even experienced physicians make mistakes in over 50% of cases when estimating risk without the aid of equations or algorithms. 282282. Sposito AC, Ramires JA, Jukema JW, Molina JC, da Silva PM, Ghadanfar MM, Wilson PW. Physicians’ attitudes and adherence to use of risk scores for primary prevention of cardiovascular disease: cross-sectional survey in three world regions. Curr Med Res Opin. 2009;25(5):1171-8.
However, one cannot forget the lack of Brazilian population data for these risk estimate models, making them less accurate for assessing CV in Brazil. In other words, international scores may underestimate risk by failing to consider the most prevalent or relevant RFs in Brazil. To mitigate that limitation and prevent the underdiagnosis of high-risk patients, this guideline recommends the identification of other markers, known as risk-modifying factors, to reassess risk in individuals classified as being at moderate risk (see details below).
CV risk classification depends on BP levels, associated CVRFs, presence of end-organ damage (EOD), structural and/or functional damage from HT to vessels, heart, brain, kidneys, and retina, and/or presence of established CVD or kidney disease. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. Different scoring systems have been developed and applied to classify hypertensives as low, moderate and high CV risk patients. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. However, new biomarkers, precursors, and predictors still seem necessary to improve risk prediction and lower the difference between calculated risk and event rates, especially in individuals classified as being at moderate risk. 283283. Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkin et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association, Circulation. 2009;119(7):2408-16.
284. Cooney MT, Dudina AL, Graham IM. Value and Limitations of Existing Scores for the Assessment of Cardiovascular Risk A Review for Clinicians. J Am Coll Cardiol. 2009;54(14):1209-27.-285285. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014; 383(9932):1899–911. Adding relative versus lifetime risk assessment tools risk advancement periods throughout the life cycle, especially for assessing young individuals at low absolute risk but high relative risk of CVD, as well as in older adults, for whom risk estimates are still challenging due to rapid changes in life expectancy and function in latter years. 285285. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014; 383(9932):1899–911.
5.2. Additional Risk Stratification (Associated Conditions)
Several factors known to, by themselves, determine or accelerate the onset of CVD, regardless of BP values, can coexist or add to each other in most hypertensive patients. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.,286286. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364(9438):937-52.
287. Wang OJ, Wang Y, Chen J, Krumholz HM. Recent Trends in Hospitalization for Acute Myocardial Infarction. Am J Cardiol. 2012; 109(11):1589–93.-288288. Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583-612. Associated conditions, whether from their prevalence in the general population or the strength of their association with CV events, should be identified in hypertensive patients by their clinical history, physical examination, and complementary testing. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. Therefore, the examination should look for: a) coexisting RFs in HT ( Chart 5.1 ); b) EOD ( Chart 5.2 ); c) presence of established kidney disease and CVD.
Identifying these conditions is important both to develop an estimate of the risk to which the hypertensive patient is exposed in their current stage and to make sure that controllable RFs will be targeted by adequate therapeutic interventions, as intensive as their degree of risk requires. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. The most prevalent and most easily identifiable RFs should be prioritized, as well as those for which there is solid evidence of association with CV risk ( Chart 5.1 ).
The factors listed in Chart 5.1 need to be taken into accounting when estimating CV risk, in accordance with current diagnostic criteria. Age is linearly correlated with HT and risk of CV complications, such as myocardial infarction (AMI) and stroke, and that linearity is more evident for strokes. For AMI, the level of association rises sharply with sex, beginning at age 55 for men and 65 for women. 287287. Wang OJ, Wang Y, Chen J, Krumholz HM. Recent Trends in Hospitalization for Acute Myocardial Infarction. Am J Cardiol. 2012; 109(11):1589–93. Smoking, quantified by pack-year load, secondhand smoking and other forms of tobacco use, such as cigars, pipes, and vapes, are considered central elements for CV risk. Dyslipidemia is characterized by increased low-density lipoprotein (LDL) or the atherogenic lipoprotein profile obtained by subtracting high-density lipoprotein (HDL) from total cholesterol, ie, non-HDL cholesterol. HDL cholesterol levels are still indicated for risk estimates and has separate thresholds for men and women. High triglycerides (TG) are also characteristic of dyslipidemia, particularly when associated with decreased HDL cholesterol or at levels above 500 mg/dL; in this case, there is indication for specific treatment and pancreatitis should be considered. The criteria for diagnosing diabetes mellitus are fasting plasma glucose > 126 mg/dL; glycated hemoglobin > 6.5%, measured by high-performance liquid chromatography (HPLC); or glucose > 200mg/dL 2 h after oral glucose overload in oral glucose tolerance test or random blood glucose. Obesity should be considered when body mass index (BMI) is > 30kg/m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. or when abdominal circumference (AC) is > 80 cm in women or > 94 cm in men of European or African descent or > 90 cm in men of Asian descent. 289289. International Diabetes Federation. IDF Consensus Worldwide Definition of the Metabolic Syndrome. 2006. [Cited in 2020 Mar 10]. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html .
https://www.idf.org/e-library/consensus-...
5.2.1. End-Organ Damage
Risk estimates for hypertensive patients should be supplemented with the investigation of EOD, which is frequent, often underdiagnosed, and usually not included in risk stratification scores. They cause additional increases in CV risk, especially when coexisting in a single individual 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,66. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.,77. Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61. ( Chart 5.2 ).
5.2.2. Presence of Cardiovascular and Renal Disease
The presence of documented cerebrovascular and renal disease determines the increased risk of CV events in hypertensive patients. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.,290290. Perrone-Filardi P, Coca A, Galderisi M, Paolillo S, Alpendurada F, de Simone G, et al. Noninvasive cardiovascular imaging for evaluating subclinical target organ damage in hypertensive patients: a consensus article from the European Association of Cardiovascular Imaging, the European Society of Cardiology Council on Hypertension and the European Society of Hypertension. J Hypertens. 2017; 35(9):1727–41.
291. PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358(9287):1033-41.-292292. Manning LS, Mistri AK, Potter J, Rothwell PM, Robinson TG. Short-term blood pressure variability in acute stroke: post hoc analysis of the controlling hypertension and hypotension immediately post stroke and continue or stop post-stroke antihypertensives collaborative study trials. Stroke. 2015; 46(6):1518-24. Cerebrovascular disease should be considered in case of ischemic stroke, brain hemorrhage, or transient ischemic attack. Coronary artery disease includes angina, AMI, silent myocardial ischemia, myocardial revascularization surgery, or prior coronary interventions. Heart failure (HF) with preserved ejection fraction (pEF) or reduced ejection fraction (rEF) should also be considered in manifested cardiovascular disease, 8686. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. as well as atrial fibrillation (AF). 293293. Grundvold I, Skretteberg PT, Liestol K, Erikssen G, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: a 35-year follow-up study. Hypertension. 2012; 59(2):198–204. Likewise, symptomatic peripheral occlusive atherosclerotic disease (POAD) 294294. Singer DR, Kite A. Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg. 2008;35(6):701–8. and aortic disease related with aneurysms, hematomas, or ulcerations represent cardiovascular manifestations with major impact on global CV risk. Because of its close association with CV risk, stage 4 or higher chronic kidney disease should be considered an indicator of high risk, identified by estimated glomerular filtration rate (eGFR) < 30 mL/min/1.73m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. , urine albumin/creatinine ratio in an isolated sample (> 300 mg/g creatinine); and urine protein/creatinine in an isolated sample (> 300 mg/g creatinine). Finally, retinopathy attributable to the hypertensive process, such as hemorrhages, exudates, and papilledema, also indicates high risk. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
Chart 5.3 shows the main reasons for performing risk estimates, taking into consideration, in addition to blood pressure levels, the presence of coexisting cardiovascular risk factors, EOD, and kidney and/or cardiovascular disease. These include establishing a reasonably accurate prognostic estimate and distinguishing cases requiring more intensive therapeutic regimens. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
Chart 5.4 is especially important for risk stratification for hypertensive patients. It is worth considering that the RFs mentioned above are only those with established epidemiological value, easily obtainable in most clinical settings, and with proven prognostic value. It helps us understand how the progression of risks associated with the presence of different BP levels and presence of RFs, EOD, or cardiovascular and/or kidney disease impact middle-aged individuals.
In moderate-risk patients, tests are recommended when feasible and available, but never in an overgeneralized process, to identify subclinical EOD markers in order to make risk estimates more accurate. 8282. Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness A Scientific Statement from the American Heart Association. Hypertension. 2015; 66(3):698-722.,295295. Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Petersen C et al. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010; 31(7):883-91.,296296. Orlova IA, Nuraliev EY, Yarovaya EB, Ageev FT. Prognostic value of changes in arterial stiffness in men with coronary artery disease. Vasc Health Risk Manag. 2010; 6:1015–21. Echocardiograms to assess LVH, which also record ventricular function parameters, and left ventricular mass index (LVMI) are important (LR: IIa, LE: B), as is albuminuria, preferably in the urine albumin/creatinine ratio, and ABI calculation (LR: IIa, LE: B). Vascular biomarkers added more recently to clinical practice, such as carotid-femoral pulse wave velocity (cfPWV), may also contribute for the reclassification of CV risk for these individuals (LR: IIa, LE: A), 296296. Orlova IA, Nuraliev EY, Yarovaya EB, Ageev FT. Prognostic value of changes in arterial stiffness in men with coronary artery disease. Vasc Health Risk Manag. 2010; 6:1015–21.,297297. Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension. 2009; 54(6):1328–36. as well as establish a worse prognosis for patients with established CV disease. 139139. Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífkova R, Cosentino F et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241(2):507-32.,298298. Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63. This aspect is particularly important for young individuals, who have lower relative risk and for whom there is the opportunity to prevent irreversible structural and functional damage to the arterial walls.
Other conditions are also known to influence or change CV risk for hypertensive patients classified as at moderate risk, but have lower discriminative power. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. Its identification is not recommended for the identification of high-risk patients or for those without any of the coexisting risk factors discussed above ( Chart 5.5 ).
5.3. Assessment of Global Cardiovascular Risk
Global CV risk stratification is not specific for hypertensive patients, and its objective is to determine the risk of a given individual ages 30 to 74 to develop CVD in general over the next 10 years. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,44. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.,280280. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.,281281. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk 2020. Eur Heart J. 2020;41(1):111-88.,299299. Bertoluci MC, Moreira RO, Faludi A, Izar MC, Schaan BD, Valerio CM et al. Brazilian guidelines on prevention of cardiovascular disease in patients with diabetes: a position statement from the Brazilian Diabetes Society (SBD), the Brazilian Cardiology Society (SBC) and the Brazilian Endocrinology and Metabolism Society (SBEM). Diabetol Metab Syndr. 2017; 9:53. It should be stressed that the relative impact of HT is one of the highest for any CVRFs, and therefore used in all global risk estimate equations. In addition, CV risk cannot be effectively mitigated without taking into consideration all the elements that determine the clinical course of hypertensive patients. A quick and practical way of calculating global CV risk is to use the Cardiovascular Risk Stratification Calculator recommended and provided by the SBC Atherosclerosis Department on its website, available for Android and iOS devices. 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
5.4. Challenges of Cardiovascular Risk Assessment in Hypertension
Several clinical conditions can impact CV risk stratification for hypertensive patients, and age is one of the most important. In the short run, while older patients have higher absolute risk, the young have lower absolute risk even when they have an unfavorable risk profile. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. In the long run or for their lifetime risk, the influence of age on CV risk flips, and longevity loss becomes highest for those who had RFs when young.
Another limitation is the duration of exposure to the disease or RF. Scoring instruments that use binary (yes or no) choices for clinical conditions such as DM and smoking to assess cardiovascular risk do not take into consideration the duration of these conditions. Therefore, patients with longer exposure times have higher CV risk compared to individuals exposed to the same factors for shorter periods. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. This means that incorporating new instruments to assess relative versus lifetime risk and periods of risk increase seem to be necessary, especially for young adults with low absolute risk but high relative risk for CVD. 280280. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.,299299. Bertoluci MC, Moreira RO, Faludi A, Izar MC, Schaan BD, Valerio CM et al. Brazilian guidelines on prevention of cardiovascular disease in patients with diabetes: a position statement from the Brazilian Diabetes Society (SBD), the Brazilian Cardiology Society (SBC) and the Brazilian Endocrinology and Metabolism Society (SBEM). Diabetol Metab Syndr. 2017; 9:53. The concepts of “vascular age” and “cardiometabolic age” can be helpful in that strategy. 300300. Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, and assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2015; 31(5): 549-68.,301301. British Cardiac Society; British Hypertension Society; Diabetes UK; HEART UK; Primary Care Cardiovascular Society; Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005; 91 Suppl 5:v1-52. 6.
The influence of the duration of antihypertensive treatment can also impact the risk estimate. In hypertensive patient who have recently started treatment, blood pressure before onset of treatment should be considered, while in patients who have been in treatment for longer periods, current blood pressure readings should be used. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
The timing and value of BP readings to be considered in CV risk stratification and different HT phenotypes should also be taken into account. Therefore, out-of-office BP measurements are increasingly encouraged. Home measurements, ambulatory blood pressure monitoring (ABPM), and home blood pressure monitoring (HBPM) have led to important complementary information, though office BP readings are still the reference for diagnosis and to assess treatment efficacy. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,302302. Sánchez RA, Boggia J, Peñaherrera E, Barroso WS, Barbosa E, Villar R, et al. Ambulatory blood pressure monitoring over 24 h: A Latin American Society of Hypertension position paper-accessibility, clinical use and cost effectiveness of ABPM in Latin America in year 2020. J Clin Hypertens. 2020; 22(4): 527–43. To that end, the recommendation for ABPM has been widened to include confirming the diagnosis of HT, considering the higher correlation of ABPM readings with EOD and cardiovascular morbidity and mortality compared to casual BP measurements. 303303. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, et al; European Society of Hypertension Working Group on Blood Pressure Monitoring. J Hypertens. 2013 Sep; 31(9):1731-68. Likewise, different HT patterns, such as masked hypertension, isolated systolic hypertension, and absence of nighttime dipping, or even increased BP during sleep, also seem to lead to different degrees of cardiovascular risk. 304304. Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018; 378(16):1509–20.,305305. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011; 57(1):3–10. Thus, these limitations should be taken into consideration when customizing CV risk estimates for hypertensive patients in clinical practice.
| Key Takeaways |
|---|
| Over 50% of hypertensive patients have additional CVRFs. |
| The presence of one or more additional CVRFs increases the risk of coronary, cerebrovascular, renal, and peripheral artery disease in hypertensive patients. |
| Identifying additional RFs should be part of diagnostic assessments of hypertensive patients, especially when there is family history of CVD. |
| CV risk should be estimated for all hypertensive patients using a simple scoring system, based on BP levels and the presence of additional RFs and comorbidities ( Chart 5.1 ). |
| CV risk can be estimated practically and reliably by identifying RFs, such as age > 65, sex (men > women), heart rate (> 80 bpm), increased body weight, diabetes mellitus, high LDL-c, family history of CVD, family history of SHT, smoking, and psychosocial and/or socioeconomic factors; for EOD: presence of LVH, moderate to severe CKD (eGFR < 60 mL/min/1.73m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. ) or other assessment confirming presence of EOD and prior diseases: CAD, HF, stroke, POAD, AF, and stage 3 or higher CKD. |
6. Therapeutic Decision and Targets
6.1. Introduction
One of the specific goals of treatment for hypertensive patients is to achieve blood pressure control by hitting a previously established blood-pressure (BP) target. That target should be defined on an individual basis, and always take into account age and presence of cardiovascular disease (CVD) or risk factors (RFs). In general, BP decreases should target BP levels below 140/90 mm Hg, but not lower than 120/70 mm Hg (LR: I, LE: A). In younger individuals without RFs, lower targets, with values below 130/80 mm Hg, are achievable.
6.2. Low- or Moderate-Risk Hypertensive Patients
Cardiovascular (CV) risk estimates are extremely important in hypertensive patients, as they determine possible differences in BP targets. Hypertensive patients with few additional FR should be assessed from two perspectives: hypertensives with significantly high blood pressure levels without other RFs (stage 2 hypertension: moderate risk) and those with smaller BP increases (stage 1 hypertension: low risk).
The benefits of treating hypertensive patients without other associated CV risk factors with significantly high BP readings (> 160 mm Hg) are well established and have long been systematically recommended by Brazilian and international guidelines. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. On the other hand, there is too little scientific evidence from randomized trials justifying treatment for stage 1 hypertensive patients with low CV risk. The reason is that the large number of participants and long follow-up period required mean that a controlled randomized trial with participants with those characteristics would be infeasible. Therefore, meta-analyses of individual data from participants in randomized trials with stage 1 hypertensive patients with no prior CVD can help us determine the best course of action. 306306. Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012 Aug15;(8):CD006742.
307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.-308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36. One such study found that treating low-risk hypertensive patients did not lead to a decrease in coronary artery disease (CAD) outcomes, CV events, or CV mortality in a four- to five-year follow-up period. 306306. Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012 Aug15;(8):CD006742. There was, however, a trend of low stroke and total mortality rates, with both decreases clearly achieved as follow-up times grew longer or as more patients were added to the studies. A second meta-analyses, including approximately 9 000 participants from five randomized trials, found that lowering systolic blood pressure (SBP) by 7 mm Hg with pharmacological treatment led to a 34% decrease in composite outcomes (CAD and stroke) and a 19% decrease in all-cause mortality. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95. A third study found lower CV disease and mortality when the initial BP was equal to or higher than 140/90 mm Hg, and the same result was not found for lower initial values. 308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36. All these outcomes are supported by a subgroup analysis from the Heart Outcomes Prevention Evaluation (HOPE)-3 trial. In that study, even if stage 1 hypertensive patients were classified as having intermediate CV risk, antihypertensive treatment with a 6 mm Hg mean decrease in SBP led to a 27% decrease in major CV events. 309309. Lonn EM, Bosch J, López-Jaramillo P, Zhu J, Liu L, Pais P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–20. Based on this date, pharmacological treatment can be initiated for stage 1 hypertensive patient with low cardiovascular risk, combined with nonpharmacological treatment (LR: I, LE: A).
In terms of blood-pressure targets for low CV risk hypertensive patients, there is also too little specific data from randomized trials. A recent meta-analysis and data from a large observational study suggest that blood-pressure targets below 140/90 mm Hg should be set and achieved for these patients, with larger decreases in CV outcomes attained from SBP readings between 120 and 130mm Hg. 8585. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67.,310310. Lee CJ, Ryu J, Kim HC, Ryu DR, Ihm SH, Kim YJ, et al. Clinical benefit of treatment of stage-1, low-risk hypertension Korean national health insurance database analysis. Hypertension. 2018;72(6):1285–93. Therefore, for these patients, targets below 140/90 mm Hg are recommended, and closer to 120/80 mm Hg, if tolerated ( Chart 6.1 ) (LR: I, LE: B).
6.3. High-Risk Hypertensive Patients
In general, hypertensive patients with three or more RFs, diabetic patients, those with end-organ damage (EOD), CV disease, or kidney disease are considered to be at high risk. In clinical practice, the most frequent examples of individuals with high CV risk are hypertensive patients with CAD, prior history of stroke, heart failure and chronic renal failure (CRF), and HT associated with diabetes mellitus (DM). These comorbidities are discussed in Chapter 10 ( Associated Clinical Conditions ), but the targets for each of these clinical situations are discussed below. Keep in mind that high risk depends not only on RFs and EOD, but also on HT staging, as shown in Chart 5.4 , and a patient may have RF or EOD but also have stage 3 HT ( Chart 6.1 ).
6.4. Hypertensive Patients with Coronary Disease
HT is an important independent RF for the onset of myocardial ischemia. Before age 50, diastolic BP (DBP) is the main predictor for CAD risk, while SBP is more important after age 60. 311311. Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging?: The Framingham Heart Study. Circulation. 2001;103(9):1245–9. In older populations, DBP is inversely related with CAD risk, and pulse pressure becomes a stronger predictor of CAD. 311311. Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging?: The Framingham Heart Study. Circulation. 2001;103(9):1245–9. In a meta-analysis including nearly 1 million adults, fatal CAD was correlated with BP levels equal to and higher than 115/75 mm Hg for all ages. 7878. Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13. In that case, antihypertensive treatment for CAD patients should result in BP < 130/80 mm Hg, but no lower than 120/70 mm Hg. In patients with evidence of myocardial ischemia, DBP should be cautiously lowered to 70 mm Hg, especially in diabetic patients and in the very old. 312312. Mahtta D, Elgendy IY, Pepine CJ. Optimal medical treatment of hypertension in patients with coronary artery disease. Expert Rev Cardiovasc. 2018;16(11):815-23. Lowering SBP in older patients with CAD and high pulse pressure requires great care, since they may lead to very low DBP values and trigger myocardial ischemia. 313313. Rosendorff C, Lackland DT, Allison M, Aronow WS, Black HR, Blumenthal RS, et al. Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Am Coll Cardiol. 2015;65(18):1998–2038.
6.5. Hypertensive Patients with History of Stroke
HT is the most important RF for ischemic and hemorrhagic stroke and is directly related to blood pressure levels. In younger individuals with no history of established CV or renal disease, keeping BP within the normal or optimum range, targeting a BP level of 120/80 mm Hg, may be the most effective for of primary prevention for cerebrovascular disease. For those with one or more prior strokes, the most adequate target for secondary prevention should be assessed according to type of stroke and post-event time (Table 10.2). In chronic cases of secondary prevention, keeping SBP from 120 to 130 mm Hg is recommended (LR: I, LE: A). 314314. Yannoutsos A, Dreyfuss CT, Safar ME, Blacher J. Optimal blood pressure target in stroke prevention. Curr Opin Neurol. 2017;30(1):8-14. For older adults or those with associated coronary disease, a relatively common scenario, the J-curve phenomenon should be taken into consideration when BP falls below 120/70 mm Hg, with higher risk of CV events and mortality. 315315. Béjot Y. Targeting blood pressure for stroke prevention: current evidence and unanswered questions. J Neurol. 2019; doi: 10.1007/s00415-019-09443-5. Online ahead of print.
6.6. Hypertensive Heart Failure Patients
Hypertension is considered a risk factor for both forms of heart failure, ie, with reduced ejection fraction and with preserved ejection fraction. Adequate treatment for HT lowers the incidence of HF. No clinical trials specifically for the HF population have compared different treatment goals. Therefore, recommendations are extrapolated from the evidence from other high-risk populations, for which lowering BP has been shown to be most protective against CV events, though with potentially increased side effects. In patients already suffering from HF with reduced ejection fraction, blood pressure control decreases mortality and readmission rates for cardiac decompensation. The proper target for this population is < 130/80 mm Hg, but taking care to keep it above 120/70 mm Hg. 316316. Pinho-Gomes AC, Rahimi K. Management of blood pressure in heart failure. Heart. 2019;105(8):589-95. In patients with preserved ejection fraction, the best form of treatment remains uncertain, so the recommended treatment strategy is similar to that for patients with reduced ejection fraction. 317317. Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018;3(4):288–97.,318318. Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018 Jul 15;263:69-74.
6.7. Hypertensive Patients with Chronic Kidney Disease (CKD)
Most CKD patients have high BP, which increases the risk of CV diseases, CKD, and death. The Systolic Blood Pressure Intervention Trial (SPRINT) study concluded that systolic BP < 120 mm Hg lowered the risk of CV disease and mortality for nondiabetic adults with high CV risk, many of whom have CKD. However, it could not halt the progression of CKD. 319319. Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, et al. Effects of intensive BP control in CKD. J Am Soc Nephrol. 2017;28(9):2812–23. Notoriously, in that study, BP was measured using automated devices, frequently unattended, which usually results in lower readings than office BP measurements. 320320. Filipovsky J, Seidlerova J, Kratochvil Z, Karnosova P, Hronova M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 2016;25(4):228–34.,321321. Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67(5):808–12. The absolute decrease in risk may be greater for patients with albuminuria due to the strong association between albuminuria and kidney and CV disease, but the effects of intensive decreases in BP on the risk of CVD seem to be similar by albuminuria level. 322322. Heerspink HJ, Ninomiya T, Perkovic V, Woodward M, Zoungas S, Cass A, et al. ADVANCE Collaborative Group: Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Eur Heart J. 2010;31(23):2888–96.,323323. Ku E, Gassman J, Appel LJ, Smogorzewski M, Sarnak MJ, Glidden DV, et al. BP control and long-term risk of ESRD and mortality. J Am Soc Nephrol. 2017;28(2):671–7. Current evidence indicates a BP target of < 130/80 mm Hg for CKD patients, regardless of DM. 275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.,324324. Chang AR, Appel LJ. Target Blood Pressure for Cardiovascular Disease Prevention in Patients with CKD. Clin J Am Soc Nephrol. 2018; 13(10):1572–4.,325325. Chang AR, Lóser M, Malhotra R, Appel LJ. Blood pressure goals in patients with CKD: A review of evidence and guidelines. Clin J Am Soc Nephrol. 2019;14(1):161-9. In patients with end-stage CKD, the benefits of intensive BP control are uncertain due to their short duration and to hemodynamic effects possibly leading to greater decreases in glomerular filtration rate (GFR). Regardless of targets, BP decreases in CKD patients always requires attention to proper BP measurements and monitoring adverse events, especially electrolyte abnormalities and decreases in GFR. 325325. Chang AR, Lóser M, Malhotra R, Appel LJ. Blood pressure goals in patients with CKD: A review of evidence and guidelines. Clin J Am Soc Nephrol. 2019;14(1):161-9.
6.8. Diabetic Hypertensive Patients
In hypertensive DM patients, morbidity and mortality prevention comes from glycemic control, BP normalization, and lowering other CV risk factors. 326326. American Diabetes Association. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S111–34. Keeping BP under control is keep for renal protection in diabetic individuals, as it lowers albuminuria, in addition to its importance in lowering the risk of stroke and left ventricular hypertrophy (LVH). 327327. Toklu B, Bangalore S. Blood pressure lowering in patients with type 2 diabetes improves cardiovascular events including mortality, but more intensive lowering to systolic blood pressure less than 130 mm Hg is associated with further reduction in stroke and albuminuria without further reduction in cardiac events. Evid Based Med. 2015;20(5):183–4.,328328. Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC, et al. Effect of Intensive Blood Pressure Lowering on Left Ventricular Hypertrophy in Patients With Diabetes Mellitus: Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial. Hypertension. 2015;66(6):1123–9. Evidence from randomized controlled trials, meta-analyses and observational studies with hypertensive diabetes patients shows that lowering SBP to 130-139 mm Hg, with values closer to the lower bound of 130 mm Hg, effectively protects against CV and renal complications. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,329329. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: Systematic review and meta-analyses. BMJ. 2016;24:352 i717. DBP may be lowered to 70-79 mm Hg without compromising individual protection and safety. On the other hand, there is no conclusive data indicating that lowering SBP to < 130 mm Hg leads to higher CV and renal protection. SBP values < 120 mm Hg should be avoided. Therefore, for diabetic patients, the recommended target is < 130/80 mm Hg (LR: IIa, LE: B).
Achieving a lower SBP target implies the need for a larger number of antihypertensive medications, increasing the risk of severe adverse effects. 330330. Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85. In practice, ideal BP targets can vary across diabetic hypertensive patients by age and presence of EOD. For instance, there is no data available for recent-onset diabetes patients with no complications and, therefore, relatively low CV and renal risks. In these cases, very low blood pressure levels may be more easily tolerated and result in greater medium- and long-term benefits. Overall, BP control is harder for patients with diabetes than for patients without diabetes. In addition, diabetic hypertensive patients often have satisfactory office BP levels, but high ABPM or HBPM readings, characterizing masked hypertension. This reinforces the need for out-of-office BP measurement in order to better assess BP control in diabetic hypertensive patients. 331331. De Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: A position statement by the American diabetes association. Diabetes Care. 2017;40(9):1273–84.
6.9. Older Hypertensive Patients
The complexities of older hypertensive patients are discussed in Chapter 14. BP targets for older populations should consider functional status, frailty and comorbidities in addition to chronological age (≥ 60 in low-income countries and ≥ 65 in all others, according to most international associations). 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,275275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57. Therefore, the therapeutic goal should balance the potential benefits and harm from BP targets.
In most clinical trials that show the benefit of treating BP in older patients, the SBP target ranged from 140 to 150 mm Hg, with greater decreases in deaths and CV events. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,332332. Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mmHg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499-503. In the HYVET trial, which included active and nonfrail patients over 80 years old, in addition to lowering SBP < 150 mm Hg (mean: 144 mm Hg), there were significant decreases in mortality, fatal strokes, and HF. 333333. Beckett N, Peters R, Leonetti G, et al, HYVET Study Group. Subgroup and per-protocol analyses from the Hypertension in the Very Elderly Trial. J Hypertens 2014;32(7):1478–87. In a meta-analysis and systematic review of nine studies, the authors found robust evidence that decreases < 150/90 mm Hg lower mortality and fewer strokes and cardiac events in older adults. 334334. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: A systematic review and meta-analysis. Ann Intern Med. 2017;166(6):419–29. However, recent clinical trials have found evidence for benefits from lower BP targets for older patients. 8787. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24):2673–82.,335335. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93. In the SPRINT trial subgroup consisting of individuals over age 75, 8787. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24):2673–82. the intensive treatment group that achieved a mean target BP level of 124/62 mm Hg had significant decreases in CV events and HF as well as all-cause mortality compared to the group with a less intensive target, for which the average BP level achieved was 135/67 mm Hg. That study suggests that more intensive treatment may be beneficial even for frailer older adults, but the incidence of falls was higher, as was the incidence of impaired kidney function, in the more intensive blood pressure control group. Another relevant data point from the SPRINT trial is that BP measurements were unsupervised, and these readings tend to be lower than those obtained with conventional methods. Therefore, the target achieved is equivalent to BP values from 130 to 139 mm Hg when compared to readings from previous studies. 321321. Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67(5):808–12. In another meta-analysis, Bavish et al. 335335. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93. showed that more aggressive BP control for patients ≥ 65 years old led to greater decreases in CV events, but it has several methodological restrictions and found greater rates of renal failure in the more intensive control group.
Overall, recommended targets for Brazilian patients ≥ 60 years old is to achieve levels matching their global condition (healthy or frail), as shown in both Chart 6.2 and Chapter 14. In older adults, targets should be treated individually, taking into account patients' quality of life, risk of falls, frailty, independence, and presence of comorbidities.
| Key Takeaways |
|---|
| In low to moderate CV risk hypertensive patients, the treatment goal is to achieve values below 140/90 mm Hg. |
| In hypertensives with CAD, the therapeutic target is to have BP < 130/80 mm Hg, but diastolic BP should be kept above 70 mm Hg. |
| For hypertensive patients with HF or who have had a stroke, antihypertensive treatment should be titrated until achieving the target of BP < 130/80 mm Hg, but the presence of CAD and advanced age, both common in that scenario, limits the ability to lower BP down to 120/70 mm Hg. |
| In hypertensive patients with CKD, the treatment goal is BP < 130/80 mm Hg, but always monitoring patients for adverse events, especially impaired kidney function and electrolyte abnormalities. |
| Hypertension treatment in diabetic patients should try to keep BP levels < 130/80 mm Hg, but avoid sharp decreases in BP to levels below 120/70 mm Hg. |
7. Multidisciplinary Team
7.1. The Importance of a Multidisciplinary Approach to Hypertension Control
Uncontrolled hypertension (HT) remains a widely prevalent cardiovascular risk factor (CVRF) in Brazil and throughout the world. Various Brazilian and international studies have consistently shown the superiority of blood pressure (BP) control using a multidisciplinary team approach when compared to conventional treatment, including higher quality care, higher adherence and therapeutic success rates, fewer CVRFs, and lower CV morbidity and mortality. 336336. Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47(1): 100-2.
337. Weinstein E, Rucker LM. Team-based care to improve control of hypertension in an inner city practice. Healthc (Amst). 2016; 4(1):52-6.
338. Mansoor SM, Krass I, Aslani P. Multiprofessional interventions to improve patient adherence to cardiovascular medications. J Cardiovasc Pharmacol Ther. 2013; 18(1)19-30.
339. Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009; 169(19): 1748-55.
340. Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006; 44(7): 646-57.-341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9. Shared patient care and decision-making are associated with lower costs and better results in HT treatment. 342342. David G, Gunnarsson C, Saynisch PA, Chawla R, Nigam S.. Do patient-centered medical homes reduce emergency department visits? Health Serv Res. 2015; 50(2):418-39.,343343. Jacob V, Chattopadhyay SK, Thota AB, et al. Economics of Team-based Care in Controlling Blood Pressure: A Community Guide Systematic Review. Am J Prev Med 2015; 49(5): 772-83.
Different objectives require different strategies, including patient-centered care, integration between multiple professionals, shared goals and targets, and collaborative decision-making with patient participation. 344344. Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45. A Brazilian retrospective longitudinal study with the goal of evaluating the effect of multidisciplinary care in hypertensive patients age 80 and older (n = 71), treated by a specialized service for an average of 15.2 years, found lower BP values, increased BP control rates and treatment optimization. 345345. Jardim LM, Jardim TV, Souza WK, Barroso de Souza WKS, Pimenta CD, Sousa AL, et al. Multiprofessional Treatment of High Blood Pressure in Very Elderly Patients. Arq Bras Cardiol. 2017; 108(1): 53-9.
A systematic review of 80 U.S. studies from 1980 to 2012 showed the efficacy of team-based care. There was a 12% increase in BP control rates, with median systolic BP (SBP) decrease of -5.4 mm Hg and median diastolic BP (DBP) decrease of -1.8 mm Hg, especially when the team included nurses and pharmacists. These results were found in various multidisciplinary setups and for various American population groups. 346346. Proia KK, Thota AB, Njie GJ, Finnie R, Hopkins D, Mukhtar Q, et al. Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014; 47(1):86-99.
A multidisciplinary team is established through actions that integrate the contributions from all of its members. The spatial element is not the single determinant of this unit; more important is the practice of developing joint actions, where each discipline acts as an independent agent in its own realm, but always acknowledging and collaborating with the actions of other team members.
Multidisciplinary work has been used successfully in primary 347347. Kuhmmer R, Lazzaretti RK, Guterres CM, Raimundo FV, Leite LE, Delabary TS, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):456. , secondary, 336336. Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47(1): 100-2. and tertiary 341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9. health care settings. The high complexity of professional activities may drive them away from joint efforts. On the other hand, it is in health promotion and in the level of primary care that we find the greatest potential for integration and where team performance is most effectively embodied. Teamwork has advantages such as encouraging patients to reproduce knowledge and attitudes, favoring research activities in care, and providing opportunities for growth for team members and, consequently, for the institutions themselves. 337337. Weinstein E, Rucker LM. Team-based care to improve control of hypertension in an inner city practice. Healthc (Amst). 2016; 4(1):52-6.,343343. Jacob V, Chattopadhyay SK, Thota AB, et al. Economics of Team-based Care in Controlling Blood Pressure: A Community Guide Systematic Review. Am J Prev Med 2015; 49(5): 772-83.,348348. Strumpf E, Ammi M, Diop M, Laniel JF, Tousignant P. The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J Health Econ. 2017;55:76-94.
349. Norouzi Z, Jafarnejad F, Khadivzadeh T, Esmaily H, Headjazi A. Comparison of the effect of standardized patient-based training with team-based learning on the knowledge of midwifery students in providing services to victims of rape. J Educ Health Promot. 2019;8:267.-350350. Kravetz JD, Walsh RF. Team-Based Hypertension Management to Improve Blood Pressure Control. J Prim Care Community Health 2016;7(4):272-5.
Deploying a multidisciplinary approach requires organizational change at the health care system level, also important in home care settings. 336336. Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47(1): 100-2. A multidisciplinary approach to HT has level of recommendation I and level of evidence A ( Chart 7.1 ). 351351. Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001; 21(3):221-32. Therefore, health care becomes a fundamentally collective and complex form of work, requiring interdisciplinarity and multidisciplinarity. 341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.,347347. Kuhmmer R, Lazzaretti RK, Guterres CM, Raimundo FV, Leite LE, Delabary TS, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):456.,352352. Overwyk KJ, Dehmer SP, Roy K, Maciosek MV, Hong Y, Baker-Goering MM, et al. Modeling the Health and Budgetary Impacts of a Team-based Hypertension Care Intervention That Includes Pharmacists. Med Care. 2019;57(11):882-9. Some duties and responsibilities are shared by all team members, others are specific to each role (LR: I, LE: A).
7.2. Team Composition and Work
7.2.1. Medical Professional: Specific Actions
General practitioners are involved in primary care, while cardiologists, nephrologists, and hypertension specialists are present at the other levels. The activities specific to physicians are as follows: 341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.
-
• Medical visit (detailed in Chapter 4).
-
• Responsible for diagnosis, risk stratification, and prescription of pharmacological and nonpharmacological therapy.
-
• Clinical assessment of patients at least twice a year.
-
• Referral and counter-referral within the health care system.
In addition to physicians, professionals from various health care disciplines (nurses, pharmacists, social workers, nutritionists, physical education professionals, physical therapists, educators, psychologists) have established multidisciplinary teams to provide care for hypertensive patients for several decades in developed countries. 353353. Tagliacozzo DM, Luskin DB, Lashof JC, Ima K. Nurse intervention and patient behavior: an experimental study. Am J Public Health. 1974; 64(6): 596-603.,354354. Dickey FF, Mattar ME, Chudzik GM. Pharmacist counsling increases drug regimen compliance. Hospitals. 1975; 49(9): 85-6, 88.
7.2.2. Nursing Professional: Specific Actions
The activities specific to nurses are as follows:
-
• Performing patient intake, identifying alongside users the various obstacles and barriers in their daily lives, and encouraging the coping process.
-
• Enabling people to increase their control over factors impacting self-care, improving their health. Advanced communication skills, behavior change techniques, patient education, and counseling skills are key elements to improve and enhance health care systems, necessary to help patients with chronic conditions. 355355. Brazil.Ministério da Saúde. Política Nacional de Educação Permanente em Saúde: o que se tem produzido para o seu fortalecimento. Brasília; 2018. The Brazilian Ministry of Health stresses that developing actions focused on health promotion and prevention of noncommunicable disease (NCD), especially HT and diabetes mellitus (DM), is an enormous challenge. 356356. Brazil.Ministério da Saúde. Síntese de evidências para políticas de saúde: adesão ao tratamento medicamentoso por pacientes portadores de doenças crônicas. Brazilia; 2018.
-
• Encouraging self-care.
-
• Planning strategies to promote and assess patient adherence to prescribed behaviors using educational, motivational, cognitive and technological approaches. 344344. Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45.,357357. Marquez Contreras E, Marquez Rivero S, Rodriguez Garcia E, Ramos LLG, Vilas JCP, Suarez AB, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167-73.
358. Hallberg I, Ranerup A, Bengtsson U, et al. Experiences, expectations and challenges of an interactive mobile phone-based system to support self-management of hypertension: patients’ and professionals’ perspectives. Patient Prefer Adherence. 2018 Mar 28;12:467-76.
359. Hallberg I, Ranerup A, Bengstsson U, Kjellgren K. Supporting the self-management of hypertension: Patients’ experiences of using a mobile phone-based system. J Hum Hypertens. 2016; 30(2):141-6.
360. Schoenthaler A, de la Calle F, Pitaro M, Lum A, Chaplin W, Mogavero J, et al. A Systems-Level Approach to Improving Medication Adherence in Hypertensive Latinos: a Randomized Control Trial. J Gen Intern Med. 2020; 35(1): 182-9. 2019/10/19. DOI: 10.1007/s11606-019-05419-3.-361361. Schoenthaler A, De La Calle F, Barrios-Barrios M, Garcia A, Pitaro M, Lum A, et al. A practice-based randomized controlled trial to improve medication adherence among Latinos with hypertension: study protocol for a randomized controlled trial. Trials. 2015;16:290. -
• Promoting educational health-literacy initiatives for users. 344344. Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45.,362362. Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: A randomized controlled trial. Patient Educ Couns. 2020; 103: 336-42.
-
• Home visits to reinforce medication use and help manage care and/or technologies to promote proper use, such as helping users establish medication intake habits and routines. 363363. Serene Olin S, Kutash K, Pollock M, et al. Developing quality indicators for family support services in community team-based mental health care. Adm Policy Ment Health. 2014; 41: 7-20.,364364. Ranerup A and Hallberg I. Actors and intentions in the development process of a mobile phone platform for self-management of hypertension. Inform Health Soc Care 2015; 40: 299-318.
7.2.2.1. Nursing-Specific Actions in Primary Care
Teams working in basic care should try to follow the principle of “person-centered care,” in which individuals are the main agents of personalized care. Professionals should help users develop the knowledge, aptitudes, competences and trust needed to more effectively manage and make informed decisions about their own health. Management plans are designed for people, according to their needs and their possibilities to pursue a full and independent lifestyle. To that end, the Ministry of Health published Ordinance 2.436, dated September 21, 2017, 365365. Brazil.Ministério da Saúde. Política Nacional de Atenção Básica. Portaria no 2.436, de 21 de setembro de 2017. Brasília;2017. establishing guidelines for the actions and activities of nursing staff, such as:
-
• Providing health care services to the individuals and families serve by the team and, when indicated or required, at homes and/or other community spaces (schools, associations, etc.) at every step of patients' life cycles.
-
• Performing nursing visits and procedures, requesting supplementary tests and prescribing medication in accordance with protocol, clinical and therapeutic guidelines and other technical standards, as established by federal, state, municipal or Federal District managers, in accordance with legislation and regulations.
-
• Performing and/or supervising patient intake with qualified listening and risk classification, following established procedures.
-
• Performing risk stratification and developing a care plan for individuals with chronic conditions in their territory alongside other team members.
-
• Performing group activities and referring users to other services, when necessary, following the flow rules established by the local health care network.
-
• Planning, managing and assessing the actions of nursing technicians and assistants, community health workers (CHW), and endemic disease control agents together with other team members. 365365. Brazil.Ministério da Saúde. Política Nacional de Atenção Básica. Portaria no 2.436, de 21 de setembro de 2017. Brasília;2017.
-
• Supervising the actions of nursing technicians/assistants and CHW.
-
• Implementing and updating routines, protocols, and flows connected to their area of expertise at their primary health care unit.
-
• Performing other duties under their purview in accordance with legislation.
7.2.3. Nutrition Professional: Specific Actions
A recent meta-analysis 366366. Riegel GR, Ribeiro PAB, Rodrigues MP, et al.Efficacy of nutritional recommendations given by registered dietitians compared to other healthcare providers in reducing arterial blood pressure: Systematic review and meta-analysis. Clin Nutr. 2018; 37(2): 522-31. showed that nutritional counseling is more effective in lowering BP when provided by a multidisciplinary team including a nutritionist. In primary care, dietetic consultations were found to be the most effective in improving diet quality. 367367. Mitchell LJ, Ball LE, Ross LJ, et al. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J Acad Nutr Diet. 2017; 117(1): 1941-62.
7.2.3.1. Dietetic Consultation 367,368
Visits to nutritionists should include the following items:
-
• Nutritional history with an assessment of eating routine, number of meals, meal times, types and quantity of food, and frequency of cardioprotective foods.
-
• Anthropometric assessment: height, weight, and abdominal circumference measurement and body mass index calculation.
-
• Prescribe and guide diet based on medical diagnosis and laboratory examinations.
-
• Monitor diet changes and anthropometric evolution.
-
• Take part in actions involving the population.
7.2.3.2. Collective Actions by Nutritionists
The following actions are recommended:
-
• Nutritional guidance should center of impactful changes in BP reduction: weight loss, 369369. Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association Between Obesity and Cardiovascular Outcomes: A Systematic Review and Meta-analysis of Mendelian Randomization Studies. JAMA Netw Open. 2018; 1(7): e183788.,370370. Dwivedi AK, Dubey P, Cistola DP. Association Between Obesity and Cardiovascular Outcomes: Updated Evidence from Meta-analysis Studies. Curr Cardiol Rep.2020; 22(4):25. increased intake of fruits and vegetables, 371371. Zhao CN, Meng X, Li Ya, Li S, Tang GY, Li HB. Fruits for Prevention and Treatment of Cardiovascular Diseases. Nutrients. 2017; 9(6):598.
372. Mellendick K, Shanahan L, Wideman L, calkins S, Keane S, Lovelady C. et al. Diets Rich in Fruits and Vegetables Are Associated with Lower Cardiovascular Disease Risk in Adolescents. Nutrients. 2018; 10(2):136.-373373. Alissa EM. Ferns GA. Dietary fruits and vegetables and cardiovascular diseases risk. Crit Rev Food Sci Nutr. 2017; 57(9):1950-62. and lower sodium intake. 374374. Aminde LN, Cobiac LJ, Veerman JL. Potential impact of a modest reduction in salt intake on blood pressure, cardiovascular disease burden and premature mortality: a modelling study. Open Heart. 2019; 6(1): e000943.,375375. He FJ, Tan M, Ma Y, et al. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020; 75: 632-47. -
• Currently, the use of free technological resources in nutrition represent an important large-scale information resource and should be encouraged. 376376. Graham GN, Ostrowski M, Sabina AB. Population health-based approaches to utilizing digital technology: a strategy for equity. J Public Health Policy 2016; 37(Suppl 2): 154-66.,377377. Grahame JA. Digital Note-Taking: Discussion of Evidence and Best Practices. J Physician Assist Educ. 2016; 27(1): 47-50.
7.2.4. Physical Education Professional: Specific Actions
Sedentary behavior (time sitting, watching TV or at the cellphone or computer) and physical inactivity (physical activity habits below recommended levels) represent a major public health issue, as they increase treatment costs and lower life expectancy. 378378. Zhao R, Bu W, Chen Y, Chen X. The Dose-Response Associations of Sedentary Time with Chronic Diseases and the Risk for All-Cause Mortality Affected by Different Health Status: A Systematic Review and Meta-Analysis. J Nutr Health Aging. 2020; 24(1): 63-70.
379. Ozemek C, Lavie CJ. Rognmo O. Global physical activity levels - Need for intervention. Prog Cardiovasc Dis. 2019; 62(2): 102-7.-380380. de Rezende LF, Rabacow FM, Viscondi JY, Luiz O, Matsudo V. Effect of physical inactivity on major noncommunicable diseases and life expectancy in Brazil. J Phys Act Health. 2015; 12(3): 299-306. Physical education professionals have the task of applying the recommendations found in Chapter 8 to minimize these behaviors. To that end, the professional should:
-
• Recommend less sedentary behavior in adult and adolescent populations.
-
• Encourage meeting minimum physical activity (PA) recommendations for the whole population through the collective actions detailed below. Practicing these activities contributes to lowering cardiovascular mortality even in case of sedentary behavior. 381381. Ekelund U, Brown WJ, Steene-Johannessen J, Wang M, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019; 53(14): 886-94.
-
• Plan, teach and supervise physical exercise (PE) programs, in person or at a distance, individually or in groups, matching local networks and the specific characteristics of each individual. Professionals should make use of technological resources (cellphones, Internet, video games, videos, etc.) to encourage participation, monitor the frequency and intensity of exercises, and teach individuals how to increase their daily regular physical activity levels;
-
• Perform pre-participation assessments, indicate prior medical evaluation for recommended cases, and perform regular reassessments to verify the effectiveness of physical activity practices and adjust them as they evolve.
7.2.4.1. Collective Actions by Physical Education and Physical Therapy Professionals
-
• Within multidisciplinary teams, developing community-based PA should be encouraged, through patients and representatives from the community and civil society organizations, given that leisure activities improve quality of life for the community.382
-
• As team members, physical education professionals should use positive results to show that treating and preventing HT depends on a combination of decreasing sedentary behavior and increasing physical activity with other factors, such as a healthy diet, weight loss, less stress, decreased salt and alcohol intake, smoking cessation, etc. In addition, adherence to pharmacological treatment and frequent BP readings should be encouraged in order to help control the disease.
-
• The strategy of establishing Leagues and Associations of people who suffer from HT helps increase patients' adherence to treatment, and these professionals could join the health care teams working alongside these institutions.
-
• One-off activities, such as Hypertension Prevention Campaigns and Fight Against Hypertension Campaigns, are important and efficient strategies to help patients learn about their health. Physical education and physical therapy professionals have an important role in this setting.
7.3. Multidisciplinary Team Actions
At the primary and secondary care level, in addition to physicians, the multidisciplinary teams can include nurses, nursing technician/assistants, nutritionists, psychologists, social workers, physical education professionals, physical therapists, pharmacists, music therapists, managerial staff, and community health workers, though not all role are required before the team can act. 383383. Balamurugan A, Adolph S, Faramawi M, George M. Community Team-Based Care for Hypertension Management: A Public-Private Partnership in Rural Arkansas. J Ark Med Soc. 2017; 113(7):150-4.,384384. Sidney S. Team-Based Care: A Step in the Right Direction for Hypertension Control. Am J Prev Med. 2015; 49(5): e81-e82.
According to the National Primary Care Policy (Ordinance 2.436, dated September 21, 2017), defines, in Article 2, that “primary care is the set of individual, familial and collective actions that involve the promotion, prevention, protection, diagnosis, treatment, rehabilitation, damage reduction, palliative care, and surveillance, based on practices of comprehensive care and qualified management, performed by a multidisciplinary team and directed toward the population of a given territory over which the teams assume responsibility.” 365365. Brazil.Ministério da Saúde. Política Nacional de Atenção Básica. Portaria no 2.436, de 21 de setembro de 2017. Brasília;2017.
Role overlaps can be minimized by establishing clear rules and working on group harmony. Keep in mind that the education and attitude changes are slow process, and that standardized, clear, objective and balanced communication is critical to achieve one's goals. 343343. Jacob V, Chattopadhyay SK, Thota AB, et al. Economics of Team-based Care in Controlling Blood Pressure: A Community Guide Systematic Review. Am J Prev Med 2015; 49(5): 772-83. Team members should work within the boundaries of their specific roles and education, as determined by guidelines and their respective boards. The individual actions of other team members should also be acknowledged. 347347. Kuhmmer R, Lazzaretti RK, Guterres CM, Raimundo FV, Leite LE, Delabary TS, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):456.,384384. Sidney S. Team-Based Care: A Step in the Right Direction for Hypertension Control. Am J Prev Med. 2015; 49(5): e81-e82.
Multidisciplinary teams have been used to treat hypertensive patients in developed countries for several decades. 341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.,348348. Strumpf E, Ammi M, Diop M, Laniel JF, Tousignant P. The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J Health Econ. 2017;55:76-94.,350350. Kravetz JD, Walsh RF. Team-Based Hypertension Management to Improve Blood Pressure Control. J Prim Care Community Health 2016;7(4):272-5.,385385. Santschi V, Wuerzner G, Chiolero A, Brurnand B. Team-based care for improving hypertension management among outpatients (TBC-HTA): study protocol for a pragmatic randomized controlled trial. BMC Cardiovasc Disord.2017; 17(1): 39. Educational and therapeutic actions may involve groups of patients, family members and the community as a whole, and the methods deployed should always take into consideration the specificities of local and regional societies and cultures. Modern approaches may involve social media and distance education techniques. 338338. Mansoor SM, Krass I, Aslani P. Multiprofessional interventions to improve patient adherence to cardiovascular medications. J Cardiovasc Pharmacol Ther. 2013; 18(1)19-30.,351351. Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001; 21(3):221-32.,357357. Marquez Contreras E, Marquez Rivero S, Rodriguez Garcia E, Ramos LLG, Vilas JCP, Suarez AB, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167-73.,362362. Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: A randomized controlled trial. Patient Educ Couns. 2020; 103: 336-42.,386386. Al-Rubaey MG, Shwaish MI. Impact of hypertension education on treatment compliance among hypertensive patients in Baghdad 2017. J Pak Med Assoc .2019; 69(Suppl 3): S9-S12.,387387. Chen Y, Li X, Jing G, Pan B, Long B, Zhi Tong B, et al. Health education interventions for older adults with hypertension: A systematic review and meta-analysis. Public Health Nurs. 2020 ;37(3): 461-9. Examples of the work of patient-centered multidisciplinary teams, with evidence of better BP control, can be found in Chart 7.1 .
In a recent analysis on the future of HT, Dzau & Balatbat 388388. Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7. state that, to this day, care delivery for hypertensive patients is fragmented, service providers are not aligned, and the information is siloed, and that better health care coordination and integration across different care settings and providers is needed. They also claim that, in the future, controlling or preventing HT will depend on the successful convergence of advances in digital, biotechnological, and biomedical sciences, with a special role for multidisciplinary work. 388388. Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7.
| Key Takeaways |
|---|
| In primary care for hypertensive patients, physicians are responsible for diagnosis, risk stratification, and pharmacological and nonpharmacological therapeutic management, at least twice a year. |
| At the population level, the most important guidelines are to keep body weight within the reference range, increase intake of fruits and vegetables, and lower sodium intake. |
| In multidisciplinary teams, physical education professionals should recommend decreased sedentary behavior and encourage individuals to meet minimum physical activity requirements in order to acquire healthy habits and improve quality of life for the community. |
| Nursing care should be person-centered, making basic information more accessible and understandable and aiding individual and collective self-care decision-making through nursing visits, home visits, and educational group activities. |
| Strategies for patient-centered multidisciplinary teams, with evidence of better BP control, should be deployed by multidisciplinary teams themselves. |
8. Nonpharmacological Treatment
8.1. Introduction
High blood pressure (BP), smoking, obesity, unhealthy diets, and insufficient physical activity are established cardiovascular risk factors (CVRFs) and the target of interventions for hypertension (HT) control. In recent years, unconventional therapies have been investigated, involving the adoption of slow breathing, music therapy, and spirituality. In this chapter on nonpharmacological treatment (NPT), we discuss the evidence behind recommendations for smoking, eating habits, sodium, potassium, dairy, chocolate and cocoa products, vitamin D, supplements and substitutes, weight loss, alcohol consumption, physical activity and exercise, slow breathing, stress control, and spirituality and religiosity.
8.2. Smoking
Smoking remains one of the most important CVRFs, and in addition to cigarettes, the use of cigars, cigarillos, pipes, hookahs and vapes remains particularly high in certain countries and is associated with increased CV risk 400400. Yan R, Li W, Yin L, Wang Y, Bo J; PURE-China Investigators. Cardiovascular Diseases and Risk-Factor Burden in Urban and Rural Communities in High-, Middle-, and Low-Income Regions of China: A Large Community-Based Epidemiological Study. J Am Heart Assoc. 2017;6(2):e004445. (LR: I, LE: A). In Brazil, smoking has trended downward in the last 15 years, but the decrease has not been uniformly distributed 401401. Malta DC, Silva AGD, Machado ÍE, Sá ACMGN, Santos FMD, Prates EJS, Cristo EB. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J Bras Pneumol. 2019;45(5):e20180384. (LR: IIa, LE: B). Smoking has considerable potential to cause damage, such as accelerating atherothrombotic processes and temporarily increasing BP. On average, tobacco use increases BP by 5 to 10 mm Hg, 402402. Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Smith N, et al. Screening for High Blood Pressure in Adults: A Systematic Evidence Review for the U.S. Rockville MD:Agency Research and Quality;2014. [Evidence Synthesis No. 121. AHRQ / Publication No. 13-05194-EF-1. ] but there are no studies showing the beneficial effects of smoking cessation on HT control. Regardless, cessation should be emphasized due to the risk of CV disease and neoplasia. 403403. Bhatnagar A, Maziak W, Eissenberg T, Ward KD, Thurston G, King BA, et al. Water Pipe (Hookah) Smoking and Cardiovascular Disease Risk: A Scientific Statement from the American Heart Association. Circulation. 2019;139(19):e917-36. Medications for smoking cessation (such as sustained-release bupropion, varenicline, nicotine gum, drops, nasal spray, and patches) are effective in helping smokers quit 404404. Leone FT, Zhang Y, Evers-Casey S, Evins AE, Eakin MN, Fathi J, et al. Initiating Pharmacologic Treatment in Tobacco-Dependent Adults. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5-e31. (LR: IIa, LE: B).
8.3. Dietary Patterns
Healthy eating patterns are associated with lower BP. The DASH (Dietary Approaches to Stop Hypertension) diet is capable of lowering BP, with the effect attributed to the increase in fruit, vegetable, low-fat dairy and whole-grain intake, as well moderate consumption of nuts and lower fat, candy, sugary beverages, and red meat. The hypotensive effect is due more to the dietary pattern ( Chart 8.1 ) than to its individual components—high sodium, calcium, magnesium and fiber content, with lower levels of cholesterol and total and saturated fat 405405. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.,406406. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH–Sodium Collaborative. Research Group. N Engl J Med. 2001;344:3–10. (LR: I, LE: A). The association between the DASH diet with sodium restriction 406406. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH–Sodium Collaborative. Research Group. N Engl J Med. 2001;344:3–10. has resulted in a decrease in systolic BP (SBP) of 11.5 mm Hg for hypertensive individuals and 7.1 mm Hg for normotensives compared to a high-sodium diet. Meta-analyses of randomized controlled trials confirm the BP reduction effect 406406. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH–Sodium Collaborative. Research Group. N Engl J Med. 2001;344:3–10.,407407. Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2020;11(5):1150-60. (LR: I, LE: A). Some studies suggest that adherence to the DASH diet is associated with lower risk of stroke 408408. Larsson SC, Wallin A, Wolk A. Dietary Approaches to Stop Hypertension diet and incidence of stroke: results from 2 prospective cohorts. Stroke. 2016;47(4):986-90.,409409. Mertens E, Markey O, Geleijnse JM, Lovegrove JA, Gibens DI. Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: evidence from the Caerphilly Prospective Study. Eur J Nutr. 2018;57(3):1245-58. (LR: IIa, LE: B), cardiovascular mortality 410410. Soltani S, Arablou T, Jayedi A, Salehi-Abargouei A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutr J. 2020;19(1):37. (LR: I, LE: A) and kidney disease 411411. Mozaffari H, Ajabshir S, Alizadeh S. Dietary Approaches to Stop Hypertension and risk of chronic kidney disease: A systematic review and meta-analysis of observational studies. Clin Nutr. 2020;39(7):2035-44. (LR: I, LE: A).
Like DASH, the Mediterranean diet is rich in fruits, vegetables, and whole grains and low in red meat. It has a high fat content due to the large amounts of olive oil (source of monounsaturated fatty acids) and includes the consumption of fish and nuts, as well moderate intake of red wine 412412. Martínez-González MA, Gea A, Ruiz-Canela M. The mediterranean diet and cardiovascular health. Circ Res. 2019;124(5):779-98. (LR: IIa, LE: B). The diet decreases the risk of cardiovascular issues 413413. Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72(1):30-43.,414414. Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173-91. (LR: IIa, LE: A), but its effects on blood pressure are modest 414414. Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173-91.
415. Nissensohn M, Román-Viñas B, Sánchez-Villegas A, Piscopo S, Serra-Majem L. The effect of the mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutr Educ Behav. 2016;48(1):42-53.
416. Jennings A, Berendsen AM, de Groot LCPGM, Feskens EJM, Brzozowska A, Sicinska E, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults. Hypertension. 2019;73(3):578-86.-417417. Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64(1):69-76. (LR: IIa, LE: B).
8.4. Sodium Intake
Worldwide habitual sodium intake is estimated at 4 g/day 418418. Fuchs SF. Estudo PREVER: Mudanças de Estilo de Vida. Porto Alegre: Engenho de Idéias; 2011. 47 p. (LR: IIa, LE: B), while the recommended intake for hypertensive individuals and for the general population is 2 g/day 419419. Powles J, Gahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intake in 1990 and 2010: a systematic analysis of 24h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733. (LR: I, LE: A). Not to depend on individual adherence to sodium restriction, which decreases in the long run, governments are now working with the food industry to lower sodium content in their products. Epidemiological data show that sodium intake is directly associated with high BP, and randomized controlled trials have shown the hypotensive effect of sodium restriction. The proof of concept is based on the dose-response curve, showing that even a small decrease in sodium intake can have an effect, stronger in hypertensive individuals, blacks and older adults 420420. World Health Organization. WHO. Guideline: Sodium intake for adults and children. Geneva;2012. (LR: I, LE: A). Restricting sodium intake to about 1800 mg/day is associated with a 5.4 mm Hg decrease in SBP for hypertensive individuals 421421. Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trial. BMJ. 2020 Feb 24; 368:m315. (LR: I, LE: A). Examples of sodium-rich foods include processed meats (ham, bologna, sausages, salami), bacon, dried meat, chicken nuggets; canned food (tomato extract, corn, peas), cheese (yellow cheese: Parmesan, provolone, prato), ready-made seasonings (Arisco, Sazon, soy sauce [shoyu], Worcestershire sauce, ketchup, mustard, mayo, concentrated extracts, meat tenderizers, and instant soup) and industrialized snacks (potato chips, French fries, and other snacks). 422422. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on bloodpressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ; 2013;346:f1325. One part of salt restriction diets is to read the nutrition facts labels on all foods and choose those lower on salt (sodium chloride) and other sources of sodium, giving preference to fresh, frozen or “no salt added” canned vegetables, and to use herbs, spices, and saltless mixes to cook and season food. One should cook rice, pasta, and cereals without salt and choose items with low sodium content, deprecating frozen foods, pizza, ready-made mixes, canned soups and creams, and salad dressings. Whenever possible, wash off canned foods, such as tuna, to lower sodium intake. Some forms of salt (pink Himalayan salt and sea salt, among others) have the same sodium chloride content as table salt and rock salt.
8.5. Potassium
High-sodium diets are usually low on potassium, associated with higher incidence of HT. Several randomized controlled trials in population clusters have tested replacing sodium chloride table salt with low-sodium, high-potassium salt products, and led to decreases in BP 423423. Bernabe-Ortiz A, Sal Y Rosas VG, Ponce-Lucero V, Cárdenas MK, Carrillo-Larco RM, Diez-Canseco F, et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26(3):374-8.
424. Marklund M, Singh G, Greer R, Cudhea F, Matsushita K, Micha R, Brady T, et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: modelling study. BMJ. 2020;369:m824.
425. Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015; 33(8):1509-20.
426. China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007; 25(10):2011-8.
427. Zhou B, Wang HL, Wang WL, Wu XM, Fu LY, Shi JP. Long-term effects of salt substitution on blood pressure in a rural north Chinese population. J Hum Hypertens. 2013; 27(7):427-33.-428428. Peng Y-G, Li W, Wen X-X, Li Y, Hu J-H, Zhao L-C. Effects of salt substitutes on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(6):1448-54. (LR: I, LE: A). The magnitude of the effect on blood pressure varies with dietary sodium intake and the extent of its replacement by alternative sources of food in the population. A prior meta-analysis 428428. Peng Y-G, Li W, Wen X-X, Li Y, Hu J-H, Zhao L-C. Effects of salt substitutes on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(6):1448-54. (LR: I, LE: A) confirmed the effect of sodium replacement for younger and older adults in the short and long term, though the hypotensive effect seems to be more pronounced for hypertensive individuals, with a mean difference of -8.87 mm Hg (95% CI: -11.19 to -6.55) in SBP and -4.04 mm Hg (95% CI: -5.70 to -2.39) in diastolic BP (DBP) over the control group 4242. Jafarnejad S, Mirzaei H, Clark CCT, Taghizadeh M, Ebrahimzadeh. The hypotensive effect of salt substitutes in stage 2 hypertension: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20(98):1-15. (LR: I, LE: A). A meta-analysis of sodium restriction interventions found that, in six high-quality studies, ranging from two months to three years, salt substitutes (potassium chloride replacing sodium chloride from 25 to 50%) significant lowered SBP (-5.7 mm Hg; 95% CI -8.5 to -2.8) and DBP (-2.0 mm Hg; 95% CI -3.5 to -0.4) in China 429429. Jin A, Xie W, Wu Y. Effect of salt reduction interventions in lowering blood pressure in Chinese populations: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2020;10(2):e032941. (LR: I, LE: A). Potassium-rich foods include apricot, avocado, melon, skim milk, leafy greens, fish (flounder and tuna), beans, orange, peas, prune, spinach, tomato, and raisins.
8.6. Dairy Products
Dairy consists of a heterogeneous food group, and its impact on health should be assessed in terms of all of its components. Though rich in saturated fatty acids (in whole milk), they may contain potentially beneficial elements, such as whey protein, phospholips from the fat globule membrane, calcium, magnesium, potassium, probiotics, and vitamins K1and K2430430. Thorning TK, Bertram HC, Bonjour JP, de Groot L, Dupont D, Feeney R, et al. Whole dairy matrix or single nutrients in assessment of health effects: current evidence and knowledge gaps. Am J Clin Nutr. 2017;105(5):1033-45.,431431. Mozaffarian D, Wu JHY. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ Res. 2018;122(2):369-84. (LR: IIa, LE: B). Cohort studies suggest dairy consumption is inversely associated with CV risk disease 432432. Dehghan M, Mente A, Rangarajan S, Sheridan P, Mohan V, Igbal R, et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2018;392(10161):2288-97,433433. Buendia JR, Li Y, Hu FB, Cabral HJ, Bradlee ML, Quatromoni PA, et al. Regular yougurt intake and risk of cardiovascular disease among hypertensive adults. Am J Hypertens. 2018;31(5):557-65. (LR: IIa, LE: B). Some randomized controlled trials suggest a modest hypotensive effect, especially for nonfat dairy product 434434. Machin DR, Park W, Alkatan M, Mouton M, Tanaka H. Hypotensive effects of solitary addition of conventional nonfat dairy products to the routine diet: a randomized controlled trial. Am J Clin Nutr. 2014;100(1):80-7.,435435. Rietsema S, Eelderink C, Joustra ML, van Vliet IMY, van Londen M, Corpeleijn E, et al. Effect of high compared with low dairy intake on blood pressure in overweight middle-aged adults: results of a randomized crossover intervention study. Am J Clin Nutr. 2019;110(2):340-8. (LR: IIa, LE: A) and milk proteins 436436. Hidayat K, Du HZ, Yang J, Chen GC, Zhang Z, Lin ZN, Qin LQ. Effects of milk proteins on blood pressure: a meta-analysis of randomized control trials. Hypertens Res. 2017;40(3):264-70. (LR: IIa, LE: B). Keep in mind that dietary guidelines recommend the consumption of low-fat dairy products 437437. Brazil.Ministério da Saúde. Guia Alimentar Para a População Brazileira. 2ª ed. Brasília; 2014.,438438. Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. U.S. Department of Agriculture, Agricultural Research Service, Washington(DC);2015. (LR: IIa, LE: B).
8.7. Chocolate and Cocoa Products
A meta-analysis of ten randomized controlled trials (n = 297) found a 4.5 mm Hg decrease (95% CI: 3.3 to 5.9) and a 2.5 mm Hg decrease (95% CI: 1.2 to 3.9) in systolic and diastolic blood pressure, respectively, from increase consumption of cocoa products. The studies were very heterogeneous and the interventions, diverse 439439. Desch S, Schmidt J, Kobler D, Sonnabend M, Eitel I, Sareban M, et al. Effect of cocoa products on blood pressure: systematic review and meta-analysis. Am J Hypertens. 2010;23(1):97-103. (LR: IIa, LE: A). A recent meta-analysis found similar but weaker results 440440. Ried K, Fakler P, Stocks NP, and Cochrane Hypertension Group National Institute of Integrative Medicine. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. 2017 Apr 25;4(4):CD008893. (LR: IIa, LE: A). Two aspects deserve attention, though the more recent meta-analysis had more studies. One was that heterogeneity persisted across trials with variable amounts of flavonoids. The second is that increased intake of chocolate or cocoa products adds calories to the diet, which must then be set off by some degree of dietary restriction.
8.8. Coffee and Caffeinated Products
In addition to caffeine ( Chart 8.2 ), coffee is also rich in bioactive compounds, such as polyphenols, especially chlorogenic acids, magnesium, and potassium, which may favor lower BP. 441441. Mesas AE, Leon-Munoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr. 2011;94(4):1113-26. Caffeine can cause sharp increases in BP for over three hours, but regular consumption leads to tolerance. 442442. van Dam RM, Hu FB, Willett WC. Coffee, caffeine, and health. N Engl J Med. 2020; 383(4):369-78. Long-term coffee intake has not been associated with higher incidence rates of HT. 443443. D´Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose-response meta-analysis of prospective studies. Eur J Nutr. 2019; 58(1):271-80. On the contrary, meta-analyses of cohort studies show that coffee intake is associated with a mild decrease in hypertension risk 443443. D´Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose-response meta-analysis of prospective studies. Eur J Nutr. 2019; 58(1):271-80.,444444. Grosso G, Micek A, Godos J, Pajak A, Sciacca S, Bes-Rastrollo M, Galvano F, Martinez-Gonzalez MA. Long-Term Coffee Consumption Is Associated with Decreased Incidence of New-Onset Hypertension: A Dose-Response Meta-Analysis. Nutrients. 2017;9(8):890. (LR: IIb, LE: B). In the absence of robust experimental evidence, it is recommended that coffee intake should not exceed low to moderate amounts (≤ 200 mg of caffeine) (LR: IIa, LE: B).
8.9. Vitamin D
Despite some observational studies suggesting vitamin D deficiency being associated with higher blood pressure or higher incidence rates of hypertension 445445. Ke L, Mason RS, Mpofu E, Vingren JL, Li Y, Graubard BI, et al. Hypertension and other cardiovascular risk factors are associated with vitamin D deficiency in an urban Chinese population: a short report. J Steroid Biochem Mol Biol. 2017;173:286-91.,446446. Zhang D, Cheng C, Wang Y, Sun H, Yu S, Xue Y, et al. Effect of vitamin D on blood pressure and hypertension in the general population: an update meta-analysis of cohort studies and randomized controlled trials. Prev Chronic Dis. 2020;17:E03. (LR: IIb, LE: A), studies on vitamin D supplementation have found inconsistent results 447447. Pilz S, Gaksch M, Kienreich K, Grubler M, Verheyen N, Fahrleitner-Pammer A, et al. Effects of vitamin D on blood pressure and cardiovascular risk factors: a randomized controlled trial. Hypertension. 2015;65(6):1195-201.
448. Arora P, Song Y, Dusek J, Plotnikoff G, Sabatine MS, Cheng S, et al. Vitamin D therapy in individuals with prehypertension or hypertension: the DAYLIGHT trial. Circulation. 2015;131(3):254-62.-449449. Shu L, Huang K. Effect of vitamin D supplementation on blood pressure parameters in patients with vitamin D deficiency: a systematic review and meta-analysis. J Am Soc Hypertens. 2018;12(7):488-96. (LR: IIb, LE: A). Therefore, the role of vitamin D in blood pressure control is still unclear.
8.10. Supplements and Substitutes
In addition to lowering sodium intake from processed foods, other alternatives enable us to minimize the harmful effects from sodium consumption and, at the same time, enjoy the beneficial effects of potassium. In a randomized controlled trial, Chinese participants with prior cardiovascular disease or SBP above 160 mm Hg were selected at random to receive a combination of 65% sodium chloride, 25% potassium chloride, and 10% magnesium sulfate or 100%-sodium chloride table salt. The intervention resulted in a mean decrease of 3.7 mm Hg (1.6 to 5.9) in systolic pressure, with maximum effect in 12 months, a 5.4 mm Hg (2.3 to 8.5) decrease 426426. China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007; 25(10):2011-8. (LR: IIa, LE: B). A randomized controlled trial with hypertensive individuals and their families found similar but weaker results after 36 months 2828. Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Custos atribuíveis à obesidade, hipertensão e diabetes no Sistema Único de Saúde em 2018. Rev Panam Salud Publica. 2020;44:e32. (LR: I, LE: A).
Though calcium supplementation may have a mild effect on preventing hypertension 450450. Cormick G, Ciapponi A, Cafferata ML, Belizán JM. Calcium Supplementation for Prevention of Primary Hypertension. Cochrane Database Syst Rev.2015;(6):CD010037. (LR: IIa, LE: B), its role in treatment has not yet been established. A meta-analysis of 12 randomized controlled trials found the use of multivitamin and multimineral supplements lowered BP in individuals suffering from chronic diseases. In a subgroup consisting of 58 hypertensive individuals, the analysis found a 7.98 mm Hg (14.95 to 1.02) decrease in SBP, but negligible significance for its impact on DBP 451451. Li K, Liu C, Kuang X, Deng Q, Zhao F, Li D. Effects of Multivitamin and Multimineral Supplementation on Blood Pressure: A Meta-Analysis of 12 Randomized Controlled Trials. Nutrients. 2018;10(8):1018. (LR: IIa, LE: B).
8.11. Weight Loss
The hypertensive effect of weight gain is well known. The relationship between BP and obesity rates is practically linear. Excess body fat, especially visceral fat, is a major risk factor for increased BP, which may be responsible for 65 to 75% of cases of HT. 452452. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol. 2019;15(6):367-85. Weight loss lowers BP even without reaching the desired weight. In a meta-analysis of 25 studies, losing 5.1 kg in weight led to a mean decrease of 4.4 mm Hg in SBP and 3.6 mm Hg in DBP 453453. Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42(5):878–84. (LR: I, LE: A). For overweight and obese individuals, weight loss is always an essential recommendation in HT treatment. Body fat assessments should not limit themselves to body mass index (BMI), but rather include central adiposity parameters, such as waist circumference (WC). Ideally, individuals should attain and maintain a healthy body weight, defined as BMI (kg/m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. ) < 25 in adults (LR: I, LE: A) and, according to the Brazilian Ministry of Health, from 22 to < 27 in older adults, as well as WC (cm) < 90 for men and < 80 for women. Evidence from a meta-analysis including participants from four continents shows that, for every 5-unit increases in BMI above > 25, the risk of early death increases approximately 31%, as does the 49% risk of cardiovascular mortality 454454. Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86. (LR: IIa, LE: B).
8.12. Alcohol Consumption
There is a linear relationship between alcohol consumption and BP, and alcohol abuse is linked to higher rates of HT. A recent meta-analysis, including 36 randomized controlled trials and 2865 participants, found that, for up to two drinks a day, lowering alcohol intake was not associated with significant decreases in BP. However, for individuals who took more than two drinks a day, lowering alcohol intake was associated with a greater decrease in BP, approximately 5.5 mm Hg (6.70 to 4.30) in SBP and 3.97 (4.70 to 3.25) in DBP. The decrease was more pronounced for those who drank six or more drinks a day and lowered their intake by approximately 50% 1515. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120. (LR: IIa, LE: B). Among drinkers, intake should not exceed 30 g of alcohol/day, ie, 1 bottle of beer (5% alcohol, 600 mL), two glasses of wine (12% alcohol, 250 mL), or one 1 dose (42% alcohol, 60 mL) of distilled beverages (whiskey, vodka, spirits). That threshold should be cut in half for low-weight men, women, the overweight, and/or those with high triglycerides. Teetotalers should not be encouraged to drink alcohol. 1515. Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120.
8.13. Physical Activity and Physical Exercise
Physical activity (PA) refers to any body motion that increases energy expenditure above consumption at rest, such as walking, working, housework, and leisure activities. Physical exercise (PE), in turn, refers to structured, organized, and purposeful PA, with goals like improving health and/or fitness. 455455. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126-31. Sedentary behavior is spent in low energy expenditure activities (≤ 1.5 MET), such as those performed sitting, reclining, or lying down (watching TV, sitting at the computer, playing video games, or working). 456456. US Department of Health and Human Services. Physical Activity Guidelines for Americans 2018. [Cited in 2020 Apr 12] Available at: https://health.gov/sites/default/files/201909/Physical_Activity_Guidelines_2nd_edition.pdf .
https://health.gov/sites/default/files/2...
Decreasing sedentary time, even for small periods, lowers the mortality risk 457457. Ekelund U, Steene-Johannessen J, Brown WJ. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonized meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-10. (LR: IIb, LE: B).
Regular physical exercise lowers the incidence of HT. 458458. Liu X, Zhang D, Liu Y, Sun X, Han C, Wang B, et al. Dose-response associations between physical activity and incident hypertension: a systematic review and meta-analysis of cohort studies. Hypertension. 2017; 69(5):813-20. In addition, hypertensives who follow PA health recommendations show a 27 to 50% decrease in mortality risk, but lower levels of PA also produce benefits 5353. Leitzmann MF, Park Y, Blair A, Ballard-Barbash R, Mouw T, Hollenbeck AR, et al. Physical activity recommendations and decreased risk of mortality. Arch Intern Med. 2007;167(22):2453-60. (LR: I, LE: A). In HT treatment, additional benefits may be obtained from structure PE, with aerobic training supplemented by resistance training. Aerobic training has a proven effect in lowering office and ambulatory BP, while dynamic resistance training and isometric handgrip resistance training lower office BP, but there is no evidence that it lowers ambulatory BP. 459459. Cao L, Li X, Yan P, Wang X, Li M, Li R, et al. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J Clin Hypertens. 2019;21(7):868-76.
Chart 8.3 shows the magnitude of the effect of that training (LR: I, LE: A). 459459. Cao L, Li X, Yan P, Wang X, Li M, Li R, et al. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J Clin Hypertens. 2019;21(7):868-76.
460. MacDonald HV, Johnson BT, Huedo-Medina TB, Livingston J, Forsyth KC, Kraemer WJ, et al. Dynamic Resistance Training as Stand- Alone Antihypertensive Lifestyle Therapy: A Meta-Analysis. J Am Heart Assoc. 2016;5(10): e003231.-461461. Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57(1-2):154-60.
Other forms of training, such as aquatic exercise, 462462. Igarashi Y, Nogami Y. The effects of regular aquatic exercise on blood pressure: a meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2018;25(2):190-9. yoga, 463463. Cramer H, Langhorst J, Dobos G, Lauche R. Yoga for metabolic syndrome: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23(18):1982-93. tai chi, 464464. Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, et al. Tai Chi for Essential Hypertension: a Systematic Review of Randomized Controlled Trials. Curr Hypertens Rep. 2020;22(3):25. and high-intensity interval training , 465465. Costa EC, Hay JL, Kehler DS, Boreskie KF, Arora RC, Umpierre D, et al. Effects of High-Intensity Interval Training Versus Moderate- Intensity Continuous Training on Blood Pressure in Adults with Pre- to Established Hypertension: a Systematic Review and Meta-Analysis of Randomized Trials. Sports Med. 2018;48(9):2127-42. among others, also seem to lower office BP for hypertensive patients. However, there is no documented evidence on their effects on ambulatory blood pressure nor on their potential risks, so they are still not recommended. Chart 8.4 lists physical activity and physical exercise recommendations.
Light to moderate PA and PE may be prescribed to for individuals without heart, cerebrovascular, or renal disease without prior medical assessment. If symptoms appear during PA or PE, it should be interrupted and the individual should seek medical help. Hypertensive individuals with comorbidities, who are symptomatic or who intend to participate in high-intensity or competitive activities should undergo a prior medical evaluation. 466466. Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, Pescatello LS. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473-9. The exercise stress test is recommended to evaluate physical fitness and to prescribe physical exercise, 467467. Meneguelo RS et al. III Diretrizes da Sociedade Brazileira de Cardiologia sobre Teste Ergométrico. Arq Bras Cardiol. 2010;95(5, supl.1):1-26. enabling an assessment of BP response to physical effort and check for coronary disease in symptomatic individuals or those with multiple risk factors. Training sessions should be canceled if BP is above 160/105 mm Hg; measuring BP during aerobic training is recommended for hypertensive individuals who exhibit hyper-reactivity, and the intensity of the physical activity should be lowered if BP is above 180/105 mm Hg (LR: IIa, LE: C).
8.14. Slow Breathing
Slow or guided breathing requires respiratory rate reduction to 6-10 breaths/minute for 15-20 minutes/day to promote casual BP reduction. Randomized controlled trials on device guided breathing (Resperate device®), analyzed in a previous meta-analysis, found no significant decrease in BP after excluding five studies involving industry participation. 468468. Mahtani KR, Nunan D, Heneghan CJ. Device-guided breathing exercises in the control of human blood pressure: systematic review and meta-analysis. J Hypertens. 2012; 30(5):852-60. A recent meta-analysis, combining six voluntary slow breathing exercise trials compared to natural breathing, found a 6.36 mm Hg decrease in SBP (95% CI: 10.32 to 2.39) and a 6.39 mm Hg decrease in DBP (95% CI: 7.30 to 5.49) in DBP compared to control group participants in randomized controlled trials lasting up to six months. 469469. Zou Y, Zhao X, Hou YY, Liu T, Wu Q, Huang YH, et al. Meta-Analysis of Effects of Voluntary Slow Breathing Exercises for Control of Heart Rate and Blood Pressure in Patients with Cardiovascular Diseases. Am J Cardiol. 2017;120(1):148–53. Existing evidence shows that, in the short run, voluntary slow breathing exercises can lower SBP and DBP in HT patients with CV disease (LR: IIa, LE: A). In a clinical trial with a small number of participants, slow breathing was shown to lower blood pressure at rest for individuals with isolated HT, in addition to responses to static and dynamic exercises 470470. Ubolsakka-Jones C, Tongdee P, Jones DA. The effects of slow loaded breathing training on exercise blood pressure in isolated systolic hypertension. Physiother Res Int. 2019;24(4):e1785. (LR: IIb, LE: B).
The association between listening to music and deep breathing, in comparison with listening to music only, did not result in statistically significant BP reductions. Participants from both treatment groups achieved clinically significant BP reductions 471471. Kow FP, Adlina B, Sivasangari S, Punithavathi N, Ng KK, Ang AH, et al. The impact of music guided deep breathing exercise on blood pressure control - A participant blinded randomised controlled study. Med J Malaysia. 2018;73(4):233–8. (LR: IIb, LE: B).
8.15. Stress Control
Overall, no robust evidence on the efficacy of techniques used in stress management has been found, including behavioral therapies, transcendental meditation (LR: IIb, LE: B), other meditation techniques (LR: III, LE: C), yoga (LR: III, LE: C), relaxation therapies (LR: III, LE: C), and biofeedback approaches (LR: IIb, LE: B). There is more evidence for guided slow breathing than there is available for acupuncture (LR: III, LE B). Clinical indications show only a trend towards lowering BP, whether used separately or in combination 472472. Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61(6):1360-83. (LR: IIa, LE: B). In two meta-analyses, music therapy was associated with a significant reduction in SBP, 473473. Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews. 2013,12:CD006577.,474474. Do Amaral MAS, Neto MG, de Queiroz JG, Martins-Filho PRS, Saquetto M B, Carvalho VO. Effect of music therapy on blood pressure of individuals with hypertension: A systematic review and Meta-analysis. Int J Cardiol. 2016;214:461–4. while in a third only its tendency to lower BP was observed 475475. Kühlmann AYR, Etnel JRG, Roos-Hesselink JW, Jeekel J, Bogers AJJC, Takkenberg JJM. Systematic review and meta-analysis of music interventions in hypertension treatment: a quest for answers. BMC Cardiovasc Disord. 2016;16:69. (LR: IIb; LE: A).
Meditation can be seen as the experience of emptying one's mind and making it devoid of thought; the practice of focusing one's concentration on a single object until becoming aware of that object; contemplating a single aspect of reality; or developing a given mental or even behavioral quality. 476476. Maynard BR, Solis MR, Miller VL, Brendel KE. Mindfulness-based interventions for improving cognition, academic achievement, behavior, and socioemotional functioning of primary and secondary school students. Campbell Systematic Reviews; 2017 https://doi.org/10.4073/CSR.2017.5
https://doi.org/10.4073/CSR.2017.5...
,477477. Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation Programs for Psychological Stress and Well-being A Systematic Review and Meta-analysis. JAMA Intern Med. 2014;174(3):357-68. A systematic review showed that transcendental meditation led to a 4 mm Hg decrease in SBP and a 2 mm Hg decrease in DBP 478478. Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of systematic reviews and meta-analyses. Complement Ther Med. 2017;34:26-34.83. (LR: IIb, LE: B). However, the mechanisms through which meditation lowers BP are not fully understood, and others have criticized these studies for methodological limitations. 479479. GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, et al; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Hypertension. Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart Assoc. 2017;6(10):e002218.
8.16. Religiosity and Spirituality
Spirituality is associated with physical, psychological and social aspects, enabling a more holistic view of human beings and placing them at the center of attention and of treatment 480480. Steinhauser KE, Fitchett G, Handzo GF, Johnson KS, Koenig HG, Pargament KI, et al. State of the Science of Spirituality and Palliative Care Research Part I: Definitions, Measurement, and Outcomes. J Pain Symptom Manag. 2017;54(3):428-40. (LR: IIb, LE: C). It may be considered a set of moral, mental and emotional values that guide thoughts, behaviors, and attitudes 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,481481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28. (LR: I, LE: B). Religion, in turn, is understood as an organized system of beliefs, practices, and symbols with the purpose of bringing its adherents closer to the transcendental or the divine 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,481481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28. (LR: I, LE: B).
Studies suggest there is an association between religiosity and spirituality (R/S) and all-cause mortality, cancer, and CV mortality, as well as quality of life 482482. Chida Y, Steptoe A, Powell LH. Religiosity/Spirituality and Mortality A Systematic Quantitative Review. Psychother Psychosom. 2009;78(2):81–90.
483. Li S, Stampfer MJ, Williams DR, VanderWeele TJ. Association of Religious Service Attendance With Mortality Among Women. JAMA Intern Med 2016;176(6):777-85.
484. VanderWeele TJ, Yu J, Cozier YC, Wise L, Argentieri MA, Rosenberg L, et al. Attendance at Religious Services, Prayer, Religious Coping, and Religious/Spiritual Identity as Predictors of All-Cause Mortality in the Black Women’s Health Study. Am J Epidemiol. 2017;185(7):515-22.-485485. Abu HO, Ulbricht C, Ding E, Allison JJ, Salmoirago-Blotcher E, Goldberg RJ, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res. 2018;27(11):2777-97. (LR: I, LE: B). The relevant mechanisms involve favorable changes in lifestyle and CVRFs, such as lower levels of serum glucose, cholesterol, fibrinogen, cortisol, and inflammatory cytokines 481481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28.,486486. Shattuck EC, Muehlenbein MP. Religiosity/Spirituality and Physiological Markers of Health. J Relig Health. 2020;59(2):1035-54. (LR: I, LE: B).
Given the multidimensional aspects of R/S and the characteristics of study populations, observational studies that assess the association between BP and/or HT risk have found heterogeneous results, but most suggest beneficial effects. 7777. Cozier YC, Yu J, Wise LA, VanderWeele TJ, Balboni TA, Argentieri MA, et al. Religious and Spiritual Coping and Risk of Incident Hypertension in the Black Women’s Health Study. Ann Behav Med. 2018;52(12):989-98.,481481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28.,487487. Spence ND, Farvid MS, Warner ET, et al. Religious Service Attendance, Religious Coping, and Risk of Hypertension in Women Participating in the Nurses’ Health Study II. Am J Epidemiol. 2020;189(3):193-203.,488488. Holt-Lunstad J, Steffen PR, Sandberg J, Jensen B. Understanding the connection between spiritual well-being and physical health: an examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. J Behav Med. 2011;34(6):477-88. In the SWAN (Study of Women’s Health Across the Nation) study, with over 1600 middle-aged women as participants, daily spiritual practices were not found to be protective for SBP or HT. 489489. Fitchett G, Powell LH. Daily spiritual experiences, systolic blood pressure, and hypertension among midlife women in SWAN. Ann Behav Med. 2009;37(3):257-67. In the Chicago Community Adult Health Study, frequency of religious attendance was not associated with HT, while the habit of prayer had a positive association. Spirituality was connected to diastolic HT, while the meaning of forgiveness was associated with lower DBP and lower probability of HT. 490490. Buck AC, Williams DR, Musick MA, Sternthal MJ. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Soc Sci Med. 2009;68(2):314-22. In a different study, more frequent religious attendance was associated with lower DBP, but not lower SBP 491491. Suh H, Hill TD, Koenig HG. Religious Attendance and Biological Risk: A National Longitudinal Study of Older Adults. J Relig Health. 2019;58(4):1188-202. (LR: IIa, LE: B).
A recent review found that elements of R/S may interfere positively in adherence to pharmacological treatment, but other studies have found opposite or mixed effects, especially for severe and chronic diseases 492492. Badanta-Romero B, de Diego-Cordero R, Rivilla-García E. Influence of Religious and Spiritual Elements on Adherence to Pharmacological Treatment. J Relig Health. 2018;57(5):1905-17. (LR: IIa, LE: C). Health care professionals should learn to identify patient demands and expectations, provide adequate support, and overcome conflicts. Open-ended questions or semistructured surveys can be useful to that end 33. Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.,493493. Oliveira JA, Anderson MI, Lucchetti G, Pires EV, Gonçalves LM. Approaching Spirituality Using the Patient-Centered Clinical Method. J Relig Health. 2019;58(1):109-18. (LR: I, LE: B). Despite the fact that evidence from observational studies correlate R/S and HT, few clinical trials have assessed the effects of interventions in this area, especially for severe CV diseases, chronic diseases or palliative care 481481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28.,494494. Balboni TA, Fitchett G, Handzo GF, et al. State of the Science of Spirituality and Palliative Care Research Part II: Screening, Assessment, and Interventions. J Pain Symptom Manage. 2017;54(3):441-53. (LR: IIb, LE: B).
| Key Takeaways |
|---|
| Hypertensive individuals should be assessed in terms of smoking habits, and smoking cessation should be pursued, with the help of medications if needed, since it increases CV risk. |
| Diets like DASH, which increase fruit, vegetable, low-fat dairy, and whole-grain intake as well fostering moderate consumption of nuts and lower fat, candy, sugary beverages, and red meat consumption, should be prescribed |
| Daily sodium intake should be restricted to 2 g/day, with sodium chloride replaced by potassium chloride where there are no restrictions. |
| Body weight should be controlled to maintain BMI < 25 kg/m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. . |
| Individuals should perform at least 150 minutes of moderate physical activity per week Decreasing sedentary behavior should be encouraged, with individuals standing for 5 minutes for every 30 minutes spent sitting down. |
9. Pharmacological Treatment
9.1. Treatment Objectives
Cardiovascular (CV) protection is the primary objective of antihypertensive treatment. Lower blood pressure (BP) is the first goal, while the greater objective is to reduce the CV outcomes and mortality linked to hypertension (HT). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45. Meta-analyses of randomized clinical trials studying hypertensive patients show that decreasing systolic BP by 10 mm Hg and diastolic BP by 5 mm Hg with medications is accompanied by a significant decrease in relative risk for major outcomes: 37% for risk of stroke, 22% for coronary artery disease (CAD), 46% for heart failure (HF), 20% for CV mortality, and 12% for all-cause mortality. 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,8585. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.,496496. Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-598.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35. The higher the CV risk, the greater the benefits, but there are benefits even for patients with small BP elevations and low to moderate CV risk. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.,496496. Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-598.
It should be stressed that these findings come mostly from clinical trials involving high CV risk hypertensives age 50 and older, and follow-up is rarely longer than five years. Therefore, the befits for young individuals, for low- to moderate-risk individuals, and from longer treatment periods are extrapolated from the scientific evidence available. 498498. Sytkowski PA, D’Agostino RB, Belanger AJ, Kannel WB. Secular trends in long-term sustained hypertension, long-term treatment, and cardiovascular mortality. The Framingham Heart Study 1950 to 1990. Circulation. 1996;93(4): 697–703. In particular, for this patient group, we infer that assessing the impact of antihypertensive medications in protecting end-organs may be a useful indirect indicator for treatment effectiveness, especially reduction of left ventricular mass 499499. Bang CN, Devereux RB, Okin PM. Regression of electrocardiographic left ventricular hypertrophy or strain is associated with lower incidence of cardiovascular morbidity and mortality in hypertensive patients independent of blood pressure reduction - A LIFE review. J Electrocardiol. 2014;47(5):630–35.,500500. Fagard RH, Celis H, Thijs L, Wouters S. Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studies. Hypertension. 2009;54(5):1084–91. and albuminuria. 501501. Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45(2):198–202. Thus, adequate treatment for individuals below the age of 50 is strongly recommended.
9.2. General Principles of Pharmacological Treatment
Most hypertensive patients require medications in addition to lifestyle changes in order to achieve their blood-pressure targets. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.,502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23. Chart 9.1 shows the recommended treatment onset for lifestyle interventions and pharmacological treatment according to blood pressure, age, and cardiovascular risk.
– Onset of treatment with lifestyle interventions and pharmacological treatment according to blood pressure, age, and cardiovascular risk
The five main classes of antihypertensive medication—diuretics (DIUs), calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), and beta-blockers (BBs)—have shown to significantly lower BP compared to placebos, as well as produce significant decreases in fatal and nonfatal CV outcomes, and this benefit is fundamentally linked to the BP decrease. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,308308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35. BBs are useful in specific clinical conditions: post-acute myocardial infarction (AMI), chest angina, HF with reduced ejection fraction (HFrEF), heart rate (HR) control, and women of childbearing age. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45. Other classes, such as alpha-blockers, centrally acting sympatholytics, aldosterone antagonists and direct vasodilators, have not been as widely studied in clinical trials, are associated with higher rates of adverse events, and should only be used when BP control has not been achieved with combinations based on the primary medication classes mentioned above. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
The desirable features of antihypertensive medications are that they:
-
• Have shown the ability to reduce CV morbidity and mortality;
-
• Be effective orally;
-
• Be well tolerated;
-
• Preferably be administered in a single daily dose;
-
• Able of being used in association;
-
• Have quality control in its production.
-
Additional recommendations are:
-
• Use for at least four weeks, before any change, except for special situations;
-
• Do not use compound medications, which are not subject to pharmacokinetic control and pharmacovigilance;
-
• Patients are instructed about the importance of continuous use of antihypertensive medication, the occasional need for dose adjustments and switching or combination of drugs, and the occasional onset of adverse effects;
-
• There is no sufficient evidence for recommending routine nocturnal administration of antihypertensive medications, except under special conditions.
9.3. Therapy Regimens
Pharmacological treatment may start as monotherapy or as drug combinations. It should be emphasized that the use of drug combinations is the preferred strategy for most hypertensive patients ( Figure 9.1 ).
9.3.1. Monotherapy
Monotherapy can be the initial antihypertensive strategy for stage 1 HT patients at low CV risk 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45. , with BP 130-139/85-89 mm Hg at high CV risk 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95. or older adults and/or frail individuals 44. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232. ( Figure 9.1 ). For these patient profiles, the desired BP decrease is small and should be achieved gradually in order to prevent adverse events. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
Treatment should be individualized, and the initial choice of medication should be based on the general desirable characteristics of the antihypertensive medications described previously, on individuals particularities, on the presence of associated diseases and end-organ damage (EOD), and on socioeconomic conditions. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.
The preferred classes of antihypertensive medication 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45. for BP control in the initial monotherapy are as follows:
-
• Thiazide and thiazide-like diuretics; 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
-
• CCBs; 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
-
• ACEIs; 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
-
• ARBs. 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
BBs may be considered as the initial drug in certain situations, 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,497497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35. as described above, and are more frequently used in combination with other medications. Dosages may be adjusted in order to achieve recommended blood-pressure targets.
9.3.2. Drug Combinations
Drug combination are the preferred therapeutic strategy for most hypertensive patients, regardless of HT staging and associated CV risk 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
505. Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42-50.
506. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.-507507. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427. ( Figure 9.1 ). Treatment should begin with a combination of two medications with different mechanisms of actions, except for the association of thiazide DIUs and potassium-sparing DIUs. If the blood-pressure target is not reached, adjusting doses and/or adding a third drug are indicated. Next, more medications are added until the BP control is achieved. 502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.-504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
The rationale for drug combinations is based on the incremental antihypertensive effect when working on different physiopathological mechanisms by synergistic actions and by inhibiting the activation of counter-regulatory mechanisms. 502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.,503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10. In addition, drug combinations have the potential of decreasing the rate of side effects due to the lower dose of each combined medication or the ability of one drug to antagonize the adverse effects of another. 502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.,503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10. Higher adherence to treatment and decreased therapeutic inertia are important benefits. Fixed-dose and single-pill combinations are preferable, as they are associated with higher adherence to treatment and, consequently, to better clinical results. 502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.,503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
The onset of fixed-dose drug combination treatment is associate with decreased risk of CV outcomes compared to the traditional onset of treatment with monotherapy, faster achievement of blood-pressure targets, protection of end-organs, and long-term CV outcomes. 502502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
505. Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42-50.
506. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.-507507. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427.
9.4. General Characteristics of Different Classes of Antihypertensive Medications
Chart 9.2 lists the antihypertensive medications available in Brazil, divided by therapeutic class.
9.4.1. Diuretics (DIUs)
The mechanisms of antihypertensive action of DIUs are initially related to their natriuretic effects, with a decrease in the circulating volume and extracellular volume. After 4-6 weeks, circulating volume normalizes and a reduction in peripheral vascular resistance (PVR) occurs. Diuretics lower BP and CV morbidity and mortality. 508508. Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997;277(9):739-45.
509. . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP-Cooperative Research Group. JAMA. 1991;265(24):3255-64.-510510. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcome in high-risk hypertensive patients to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;228(23):2981-97. Their antihypertensive effect is not directly related to their doses, but side effects are associated with dose and potency of diuretic action. Thiazide (hydrochlorothiazide) or thiazide-like (chlorthalidone and indapamide) DIUs at low doses should be preferred, because they are milder and longer-acting. Loop DIUs (furosemide and bumetanide) should be reserved for clinical conditions featuring sodium and fluid retention, such as renal failure (creatinine > 2.0 mg/dL or estimated glomerular filtration rate ≤ 30 mL/min/1.73m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. ) and edema (HF or nephritic syndrome). Potassium-sparing DIUs (spironolactone and amiloride) are usually associated with a thiazide or loop DIU. Spironolactone is habitually used as the fourth medication in drug combinations for patients with resistant and refractory HT. This aspect is discussed in further detail in the chapter 16 to those more severe forms of HT.
Chlorthalidone has higher diuretic potency than hydrochlorothiazide, compared at proper doses, and its longer half-life made it the preferential DIU for resistant or refractory HT, since sodium and fluid retention is an important mechanism in resistance to treatment. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96. The indication of chlorthalidone as the preferred DIU because it promotes a higher decrease in CV events is controversial, as a meta-analysis and observational studies with large numbers of participants were not in agreement. 495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.,511511. Dhalla IA, Gomes T, Yao Z, Nagge J, Persaud N, Hellings C, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158(6):447-55.,512512. Hripcsak G, Suchard MA, Shea S, Chen R, You SC, Pratt N, et al. Comparison of Cardiovascular and Safety Outcomes of Chlorthalidone vs Hydrochlorothiazide to Treat Hypertension. JAMA Intern Med. 2020;180(4):542–51. On the other hand, as expected from the more intense diuretic effect, these studies have found greater rates of adverse effects for chlorthalidone, particularly hydroelectrolytic and metabolic disorders. Indapamide, a thiazide-like, which has been growing in use in recent years, like chlorthalidone, has greater potency and longer-acting diuretic effect; like previous medications, it has proven antihypertensive effect, decreases CV events and has a positive metabolic profile. 513513. Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-Head Comparisons of Hydrochlorothiazide With Indapamide and Chlorthalidone. Antihypertensive and Metabolic Effects. Hypertension 2015; 65(5):1041–6. Thus, there is no definitive data behind the preference for chlorthalidone in antihypertensive treatment for individuals with normal renal function, but it may be used when a larger diuretic effect is desirable, especially in resistant HT, as it is more potent than hydrochlorothiazide.
9.4.1.1. Adverse Effects of Diuretics
Major adverse effects of diuretics are weakness, cramps, hypovolemia, and erectile dysfunction. Hypopotassemia is the most common metabolic effect, often accompanied by hypomagnesemia, which can induce ventricular arrhythmias, mainly extrasystole. Hypopotassemia also leads to insulin secretion, increasing glucose intolerance, and the risk of developing type 2 diabetes mellitus. Uric acid increase is an almost universal effect of DIUs, and may trigger gout crises in predisposed individuals.
The use of low doses of DIUs decreases the risk of adverse effects without hindering their antihypertensive efficacy, especially when associated with other drug classes. Spironolactone may cause gynecomastia and hyperpotassemia, and the latter is the most frequent electrolyte disorder in patients with impaired renal function. There are reports that indapamide may have a better metabolic profile than hydrochlorothiazide. 513513. Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-Head Comparisons of Hydrochlorothiazide With Indapamide and Chlorthalidone. Antihypertensive and Metabolic Effects. Hypertension 2015; 65(5):1041–6.
9.4.2. Calcium Channel Blockers (CCBs)
This medication class blocks the calcium channels in smooth muscle cell membranes in the arterioles, lowers calcium availability inside cells to impair muscle contraction, and consequently decreases peripheral vascular resistance by vasodilation. 514514. Elliott WJ, Ram CV. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13(9):687-9.,515515. Messerli FH. Calcium antagonists in hypertension: from hemodynamics to outcomes. Am J Hypertens. 2002;15(7 Pt 2):94S-7S.
CCBs can be divided into two basic forms: dihydropyridines and nondihydropyridines. Dihydropyridines (amlodipine, nifedipine, felodipine, manidipine, levamlodipine, lercanidipine, lacidipine) are predominant vasodilators, with minimum interference in HR and systolic function, and therefore are more often used as antihypertensive agents.
Nondihydropyridines, such as diphenylalkylamines (verapamil) and benzothiazepines (diltiazem), have a lower vasodilating effect, and act on the heart musculature and the cardiac conduction system. Thus, they lower HR, have an antiarrhythmic effect and can depress systolic function, primarily in patients already suffering from myocardial dysfunction, and should be avoided in individuals with that condition.
Long-acting CCBs should be preferred to prevent unwanted oscillations in HR and BP. They are effective antihypertensive medications that reduce CV morbidity and mortality. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,515515. Messerli FH. Calcium antagonists in hypertension: from hemodynamics to outcomes. Am J Hypertens. 2002;15(7 Pt 2):94S-7S.
516. Elliott WJ, Bandari A. The role of calcium antagonists in stroke prevention. J Clin Hypertens (Greenwich). 2005;7(4 Suppl 1):5-8.-517517. Nathan S, Pepine CJ, Bakris GL. Calcium antagonists: effects on cardiorenal risk in hypertensive patients. Hypertension 2005;46(4):637-42. An outcome study has reaffirmed the efficacy, tolerability and safety of this drug class HT treatment in CAD patients, 518518. Rollins G. Calcium antagonist and beta blocker regimens found equally effective in hypertensive patients with coronary artery disease. Rep Med Guidel Outcomes Res. 2004;15(2):1, 5-6. making it an alternative to BBs when the latter cannot be used, or in combination for cases of refractory angina.
9.4.2.1. Adverse Effects of Calcium Channel Blockers
Ankle swelling is usually the most common side effect, resulting from the vasodilating action (more arterial than venous), which causes capillary transudation. Throbbing headaches and dizziness are common. Facial blushing is more common with fast-acting dihydropyridine CCBs. Hyperchromia of the distal third of the legs (ochre dermatitis) and gingival hypertrophy are two occasional adverse effects.
Adverse effects are usually dose-dependent, may cause intolerance to dihydropyridine CCBs and may result in resistance to treatment. In these cases, lipophilic CCBs (manidipine, lercanidipine, lacidipine) may be tested, or levamlodipine at low doses. Verapamil and diltiazem can worsen HF, as well as bradycardia and atrioventricular block. Verapamil has been found to cause constipation. 516516. Elliott WJ, Bandari A. The role of calcium antagonists in stroke prevention. J Clin Hypertens (Greenwich). 2005;7(4 Suppl 1):5-8.
9.4.3. Angiotensin-Converting Enzyme Inhibitors (ACEIs)
Angiotensin-converting enzyme inhibitors are effective antihypertensive drugs whose primary action is inhibiting angiotensin I converting enzyme, responsible for both transforming angiotensin I into angiotensin II (vasoconstrictor) and lowering bradykinin degradation (vasodilator). They are effective for HT treatment, lowering CV morbidity and mortality. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95. They have been shown to be useful in many other CV conditions, such as HFrEF and post-AMI anti-remodeling, and may have antiatherosclerotic properties. They also delay renal function decline in patients with diabetic nephropathy or kidney diseases of other etiologies, especially in case of albuminuria. 519519. Vejakama P, Thakkinstian A, Lertrattananon D, Ingsathit A, Ngarmukos C, Attia J. Reno-protective effects of renin-angiotensin system blockade in type 2 diabetic patients: a systematic review and network meta-analysis. Diabetologia 2012;55(3):566-78.
9.4.3.1. Adverse Effects of Angiotensin-Converting Enzyme Inhibitors
Usually well-tolerated by most hypertensive patients, its major side effect is dry coughs, affecting 5 to 20% of patients. Angioneurotic edema and skin rashes are rare. 520520. Baram M, Kommuri A, Sellers SA, Cohn JR. ACE inhibitor-induced angioedema. J Allergy Clin Immunol Pract. 2013;1(5):442-5. When administered to renal failure patients, it can initially worsen renal function, usually discretely, due to adjustments in intraglomerular hemodynamics (vasodilation of efferent arterioles and lower glomerular filtration pressure) resulting in higher plasma creatinine and urea rates. 521521. Ryan MJ, Tuttle KR. Elevations in serum creatinine with RAAS blockade: why isn’t it a sign of kidney injury? Curr Opin Nephrol Hypertens. 2008;17(5):443-9. However, the initial loss of renal function is a protective mechanism, since it prevents glomerular hyperfiltration and slows down the progression of chronic kidney disease. 522522. Maschio G, Alberti D, Janin G, Locatelli F, Mann JF, Motolese M, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med. 1996;334(15):939-45. In case of major loss of renal function (> 30%), the medication should be withdrawn and the possibility of bilateral renal artery stenosis or renal artery stenosis in solitary functioning kidney.
ACEIs and other renin-angiotensin-aldosterone system (RAAS) blockers may cause hyperpotassemia in patients with renal failure, especially diabetic patients, and are contraindicated during pregnancy due to the risk of fetal complicactions. 523523. Polifka JE. Is there an embryopathy associated with first-trimester exposure to angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists? A critical review of the evidence. Birth Defects Res A Clin Mol Teratol. 2012;94(8):576-98.,524524. Laube GF, Kemper MJ, Schubiger G, Neuhaus TJ. Angiotensin-converting enzyme inhibitor fetopathy: long-term outcome. Arch Dis Child Fetal Neonatal Ed. 2007;92(5):F402-3. Therefore, they should be carefully monitored when administered to adolescents and women of childbearing age.
9.4.4. Angiotensin II AT1 Receptor Blockers (ARBs)
ARBs antagonize angiotensin II action via the specific blockade of AT1 receptors, responsible for the primary effects of angiotensin II (vasoconstriction, cell proliferation and aldosterone release). In HT treatment, especially in populations at high CV risk or with comorbidities, they decrease CV and renal (diabetic nephropathy) morbidity and mortality 525525. Dahlof B, Devereux R, Kjeldsen S, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the losartan intervention or endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):995-1003.
526. Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):1004-10.
527. Julius S, Kejdelsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients in high cardiovascular risk treated with regimens based on valsartan and amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022-31.
528. Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, et al; CHARM Investigators and Committees. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM Overall programme. Lancet. 2003;362(9386):759-66.
529. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861-9.
530. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al; Collaborative Study Group. Renoprotective effect of the angiotensin receptor antagonist irbersartan in patients with nephropathy due to type 2 diabetes. N Eng J Med. 2001;345(12):851-60.-531531. Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. The effect of irbersartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345(12):870-8.
9.4.4.1. Adverse Effects of Angiotensin II AT1 Receptor Blockers
Adverse effects related to ARBs are not common, with exanthema observed in rare occasions. Like ACEIs, ARBs may promote an initial decrease in glomerular filtration via vasodilation of efferent arterioles, lowering glomerular filtration pressure, but the effect is nephroprotective in the long run. 529529. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861-9.
530. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al; Collaborative Study Group. Renoprotective effect of the angiotensin receptor antagonist irbersartan in patients with nephropathy due to type 2 diabetes. N Eng J Med. 2001;345(12):851-60.-531531. Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. The effect of irbersartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345(12):870-8. Similarly to ACEIs, ARBs may cause hypercalcemia, especially in the presence of renal failure, and are contraindicated during pregnancy, and the same care should be taken for women of childbearing age.
9.4.5. Beta-Blockers (BBs)
Beta-blockers have complex pharmacological actions. They promote an initial decrease in cardiac output and renin secretion, with readaptation of baroreceptors and decrease in catecholamines in nervous synapses. 532532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
,533533. López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al; Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62.
They can be divided into three categories, according to selectivity in adrenergic receptor binding: 1) nonselective: block both beta-1 adrenergic receptors, found mainly in the myocardium, and beta-2 receptors, found in smooth muscle, the lungs, blood vessels and other organs (propranolol, nadolol and pindolol, the latter displaying intrinsic sympathomimetic activity, acting as a partial adrenergic agonist and producing less bradycardia); 2) cardioselective: preferentially block beta-1 adrenergic receptors (atenolol, metoprolol, bisoprolol and nebivolol, which is the most cardioselective); and 3) vasodilator: manifests as peripheral alpha-1 adrenergic receptor antagonism (carvedilol) and nitric oxide production (nebivolol). 532532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
533. López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al; Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62.
534. Dulin B, Abraham WT. Pharmacology of carvedilol. Am J Cardiol. 2004;93(9A):3B-6B.-535535. Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269-77. Propranolol is useful to patients with essential tremor, mitral valve prolapse, hyperkinetic syndromes (hyperthyroidism and panic disorder), vascular headache, and portal hypertension. 532532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
,533533. López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al; Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62.
A meta-analysis 536536. Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366(9496):1545-1553. including over 130 thousand primary hypertension patients compared BBs to other classes of antihypertensive medications, placebos, and no treatment. It found that compared to other antihypertensive medications (DIUs, CCBs, ACEIs, ARBs), beta-blockers increase the risk of stroke by 16%. Compared to placebo or untreated patients, beta-blockers the lower risk of stroke, but only half as much as would be expected from observed blood pressure decreases. The meta-analysis 534534. Dulin B, Abraham WT. Pharmacology of carvedilol. Am J Cardiol. 2004;93(9A):3B-6B. also found that compared to other antihypertensive medications, atenolol increases the risk of stroke by 26% and overall mortality by 8%, both significant results. This is the main reason this guideline recommends BBs as an initial antihypertensive medication only in cases for which there is a specific indication.
9.4.5.1. Adverse Effects of Beta-Blockers
The adverse effects are bronchospasm, bradycardia, atrioventricular conduction disorders, peripheral vasoconstriction, insomnia, nightmares, depression, asthenia, and sexual dysfunction. BBs are contraindicated for patients with asthma, chronic obstructive pulmonary disease (COPD), and second- and third-degree atrioventricular block. They may lead to glucose intolerance, induce onset of diabetes mellitus, hypertriglyceridemia, high LDL-cholesterol, and low HDL-cholesterol. The impact on glucose metabolism is potentiated when combined with DIUs. Third-generation BBs (carvedilol and nebivolol) have neutral impact or may even improve the glucose and lipid metabolism, possibly because of their vasodilatory effect, with decrease in insulin resistance and improvement of glucose uptake by peripheral tissues. 532532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
,535535. Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269-77. Studies on nebivolol have also found less sexual dysfunction, possibly due to its effect on endothelial nitric oxide synthesis. 532532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
,535535. Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269-77.
9.4.6. Centrally Acting Sympatholytics
Centrally acting alpha-agonists stimulate the alpha-2 receptors involved in sympatho-inhibitory mechanisms. 537537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61. Their well-defined effects are as follows: a decrease in sympathetic activity and baroreceptor reflex, contributing to relative bradycardia and orthostatic hypotension; mild decrease in PVR and cardiac output; lower plasma renin levels; and fluid retention. Representatives of that group include methyldopa, clonidine, and the imidazoline receptor inhibitor rilmenidine. 538538. Atlas D, Diamant S, Zonnenschein R. Is the imidazoline site a unique receptor? A correlation with clonidine-displacing substance activity. Am J Hypertens. 1992;5(4 Pt 2):83S.,539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262. Clonidine also acts on presynaptic alpha-2 receptors, which prevent norepinephrine release. It accumulates in nerve endings and, when withdrawn suddenly, the uncontrolled release may cause an adrenergic crisis. 537537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61. Despite some central alpha-2 agonism, rilmenidine has greater affinity for subtype I imidazoline receptor binding sites, causing fewer undesirable effects than clonidine. 538538. Atlas D, Diamant S, Zonnenschein R. Is the imidazoline site a unique receptor? A correlation with clonidine-displacing substance activity. Am J Hypertens. 1992;5(4 Pt 2):83S.
This class of medication has no unwanted metabolic effects and do not interfere with peripheral resistance to insulin or to the lipid profile. Methyldopa is primarily indicated for HT during pregnancy, as it is used for short periods, there is a large body of experience with its use during this period, and it has a better safety profile for pregnant women and for fetuses. 537537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61.,539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262. Clonidine can be useful in HT associated with restless legs syndrome, 540540. Wagner ML, Walters AS, Coleman RG, Hening WA, Grasing K, Chokroverty S. Randomized double-blind, placebo-controlled study of clonidine in restless legs syndrome. Sleep. 1996;19(1):52-8. opioid withdrawal, 541541. Bond WS. Psychiatric indications for clonidine. J Clin Psychopharmacol. 1986;6(2):81-7. menopausal hot flashes, 542542. Pandya KJ, Raubertas RF, Flynn PJ, Hynes HE, Rosenbluth RJ, Kirshner JJ, et al. Oral clonidine in postmenopausal patients with breast cancer experiencing tamoxifen-induced hot flashes: a University of Rochester Cancer Center Community Clinical Oncology Program study. Ann Intern Med. 2000,132(10):788-93. diarrhea associated with diabetic neuropathy, 543543. Fedorak RN, Field M, Chang EB. Treatment of diabetic diarrhea with clonidine. Ann Intern Med. 1985;102(2):197-9. and sympathetic hyperactivity in patients with alcoholic cirrhosis. 544544. Esler M, Dudley F, Jennings G, Debinski H, Lambert G, Jones P, et al. Increased sympathetic nervous activity and the effects of its inhibition with clonidine in alcoholic cirrohosis. Ann Intern Med. 1992;116(6):446-55.
9.4.6.1. Adverse Effects of Centrally Acting Sympatholytics
Methyldopa can cause autoimmune reactions, such as fever, hemolytic anemia, galactorrhea, and liver dysfunction, which, in most cases, disappear with cessation of use. If an adverse reaction occurs, methyldopa can be replaced by another central alpha-agonist. 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
There is a risk of rebound effect from the discontinuation of clonidine, especially when combined with beta-blockers, and can be dangerous in the preoperative period. 537537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61. Gradual withdrawal over two to four weeks prevents the rebound effect. Medications in this class have adverse reactions due to their central action, such as drowsiness, sedation, dry mouth, fatigue, postural hypotension, and erectile dysfunction. 537537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61.,539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
9.4.7. Alpha-blockers
Alpha-blockers act as competitive antagonists of postsynaptic alpha-1 receptors, decreasing PVR without changes in cardiac output. 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262. They promote greater blood pressure decreases in standing position and in reflex tachycardia. Therefore, postural hypotension is common, often found after the first dose. The hypotensive effect is mild in monotherapy, the combined use being preferred. They have favorable and discrete action on the lipid and glucose metabolisms. 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262. Medications in this class used as antihypertensives include doxazosin, prazosin, and terazosin.
A beneficial adjunct action of alpha-1 blockers is the relaxation of the pelvic floor musculature, which helps patients with benign prostatic hyperplasia (BPH) empty their bladders. Therefore, alpha-blockers are also used in men with BPH, particularly doxazosin, tamsulosin, alfuzosin, and silodosin.
9.4.7.1. Adverse Effects of Alpha-Blockers
Alpha-blockers may cause symptomatic hypotension on the first dose. Tolerance is a frequent phenomenon, requiring increasing doses to maintain the antihypertensive effect (tachyphylaxis). Alpha-blockers may cause urinary incontinence in women. There is evidence that patients treated with doxazosin are at higher risk for HF. 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
9.4.8. Direct-Acting Vasodilators
The oral medications in this class are hydralazine and minoxidil. They act directly by relaxing arterial smooth muscles, leading to a PVR decrease. 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
9.4.8.1. Adverse Effects of Direct-Acting Vasodilators
The side effects of hydralazine are headache, flushing, reflex tachycardia, and lupus-like reaction (dose-dependent). 539539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262. In addition, it can cause anorexia, nausea, vomiting, and diarrhea. Vasodilators may cause sodium and fluid retention, with increased circulating volume and reflex tachycardia. A side effect of minoxidil is hirsutism, found in approximately 80% of the patients.
9.4.9. Direct Renin Inhibitors
Aliskiren, the only representative of this drug class commercially available, causes direct renin inhibition with consequent decrease in angiotensin II production. 545545. Müller DN, Derer W, Dechend R. Aliskiren-mode of action and preclinical data. J Mol Med. 2008;86(6):659-62. Other actions may contribute to BP lowering and tissue protection, such as the reduction in plasma renin activity, 545545. Müller DN, Derer W, Dechend R. Aliskiren-mode of action and preclinical data. J Mol Med. 2008;86(6):659-62. renin/prorenin receptor blockade, 546546. Danser AH. (Pro)renin receptors: are they biologically relevant? Curr Opin Nephrol Hypertens. 2009;18(1):74-8. and decrease in intracellular angiotensin II production. 547547. Singh VP, Le B, Khode R, Baker KM, Kumar R. Intracellular angiotensin II production in diabetic rats is correlated with cardiomyocyte apoptosis, oxidative stress, and cardiac fibrosis. Diabetes. 2008;57(12):3297-306. Erratum in: Diabetes. 2009;58(3):770.
Antihypertensive efficacy studies have confirmed its antihypertensive activity in monotherapy and in combination, at a similar level as other RAAS blockers and with the apparent additional benefit of lowering proteinuria in kidney disease patients. 548548. Musini VM, Fortin PM, Bassett K, Wright JM. Blood pressure lowering efficacy of renin inhibitors for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD007066.,549549. Heerspink HJL, Persson F, Brenner BM, Chaturvedi N, Brunel P, McMurray JJ, et al. Renal outcomes with aliskiren in patients with type 2 diabetes: a prespecified secondary analysis of the ALTITUDE randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(4):309-17. However, there is no evidence of its benefits on CV morbidity and mortality for hypertensive and prehypertensive patients. 550550. Bjerre HL, Christensen JB, Buus NH, Simonsen U, Su J. The role of aliskiren in the management of hypertension and major cardiovascular outcomes: a systematic review and meta-analysis. J Hum Hypertens. 2019;33(11):795-806.,551551. Zhang JT, Chen KP, Guan T, Zhang S. Effect of aliskiren on cardiovascular outcomes in patients with prehypertension: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2015;9:1963-71.
9.4.9.1. Adverse Effects of Direct Renin Inhibitors
They are well tolerated. Skin rashes, diarrhea (especially at high doses above 300 mg/day), creatine phosphokinase increases, and coughing may occur in less than 1% of patients. They are contraindicated during pregnancy for the same reasons as ACEIs and ARBs.
9.5. Antihypertensive drug combinations
Initial antihypertensive drug combination therapy seems to be associated with decreased risk of CV outcomes compared to the traditional onset of treatment with monotherapy. 552552. Gradman AH, Parisé H, Lefebvre P, Falvey H, Lafeuille MH, Duh MS. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension. 2013;61(2):309-18. Initial two-drug combinations, compared to sequential association promotes quicker control and may lower BP up to five times more, 506506. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300. with clear impact on EOD and long-term CV outcomes. A meta-analysis found that fixed-dose two-drug combinations improve adherence by 24% compared with a free-drug component regimen. 553553. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-Dose Combinations Improve Medication Compliance: A Meta-Analysis. Am J Med. 2007;120(8):713–9. However, few studies focus specifically on assessing drug combinations on CV outcomes.
The ACCOMPLISH study 554554. Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, et al. Benazepril plus Amlodipine or Hydrochlorothiazide for Hypertension in High-Risk Patients. N Engl J Med. 2008;359(23):2417–28. compared benazepril combined with hydrochlorothiazide and with amlodipine. The difference in systolic and diastolic BP between the two groups, though significant, was only 0.9/1.1 mm Hg lower in the amlodipine arm. There was a decrease in risk of primary outcomes, consisting of nonfatal AMI, stroke, hospitalization for unstable angina, myocardial revascularization surgery, and cardiopulmonary resuscitation, in favor of the benazepril-amlodipine group. The choice of hydrochlorothiazide in that study was criticized because its effect lasts less than 24 hours, unlike the longer-acting amlodipine. However, a different report found no significant differences in 24-hour BP across groups. 555555. Jamerson KA, Bakris GL, Weber MA. 24-Hour Ambulatory Blood Pressure in the ACCOMPLISH Trial. N Engl J Med. 2010;363(1):98–8. In patients with body mass index (BMI) > 30 kg/m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. , there were no differences in primary outcomes between the two groups. 556556. Weber MA, Jamerson K, Bakris GL, Weir MR, Zappe D, Zhang Y, et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the ACCOMPLISH randomised controlled trial. Lancet. 2013;381(9866):537–45. Another prespecified analysis found an addition decrease in kidney disease progressions from a benazepril-amlodipine combination. 557557. Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–81.
The ASCOT-BPLA study 558558. Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906. compared a strategy based on amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide. Approximately 78% of patients in each group used combination therapy for hypertension control. There were no differences in primary outcomes, consisting of nonfatal AMI and fatal CAD, but secondary outcomes, such as stroke, fatal coronary events, CV mortality, and all-cause mortality, were all significantly lower for the amlodipine group. De novo diabetes development rates were 30% higher for the group treated with BBs and thiazide. The CAFE sub-study 234234. Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–5. found a more significant decrease in central aortic pressure from an amlodipine-perindopril combination and attributed it, at least in part, to the greater decrease in secondary outcomes for the group.
In the multicenter VALUE trial, 527527. Julius S, Kejdelsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients in high cardiovascular risk treated with regimens based on valsartan and amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022-31. high CV risk patients received antihypertensive treatment based on valsartane or amlodipine. Approximately 25% of patients in both groups required the addition of 12 to 25 mg of hydrochlorothiazide for BP control. Despite the higher and earlier blood pressure decrease in the amlodipine group, the combined primary cardiac outcome at the end of four years was similar for both groups, as were the fatal AMI and all-cause mortality rates. There were fewer HF cases with valsartane and fewer nonfatal AMI and stroke cases with amlodipine.
In HOPE-3, 309309. Lonn EM, Bosch J, López-Jaramillo P, Zhu J, Liu L, Pais P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–20. directed primarily to studying the effects of medications in prehypertensive patients at intermediate CV risk, an initial strategy based on a fixed-dose combination of candesartan and hydrochlorothiazide led to a 27% decrease in the composite outcome risk of CV death, nonfatal AMI, and stroke in stage 1 hypertension individuals. However, no benefits have been found for prehypertensives.
The PROGRESS trial, 291291. PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358(9287):1033-41. which assessed patients with prior cerebrovascular disease; the ADVANCE trial, 559559. Patel A, ADVANCE Collaborative Group, MacMahon S, Chalmers J, Neal B, Woodward M, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9500):829–40. which studied individuals with type 2 diabetes; and HYVET, 560560. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of Hypertension in Patients 80 Years of Age or Older. N Engl J Med. 2008;358(18):1887–98. which studied patients 80 years of age or older, used an intervention based on perindopril and indapamide and showed the benefits of combining DIUs and ACEIs to lower issues such as stroke and vascular dysfunction; macro- and microvascular outcomes; and death, stroke, and HF, respectively.
Combining BBs and thiazides lowered CV outcomes when compared to a placebo in older trials, especially those involving older patients, 509509. . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP-Cooperative Research Group. JAMA. 1991;265(24):3255-64.,561561. Dahlöf B, Hansson L, Lindholm LH, Scherstén B, Ekbom T, Wester P-O. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281–5.,562562. Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751–6. but underperformed the combination of thiazides and losartan in the LIFE trial, 526526. Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):1004-10. where it provided less protection against stroke and favored glucose metabolic disorders. The use of fixed-dose combinations of thiazides with atenolol and other BBs should be restricted to specific indications for this class 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,495495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45. given the induction of potential metabolic disorders from DIUs, such as insulin resistance, hyperglycemia, hyperuricemia, and hypopotassemia.
The combination of dihydropyridine calcium channel blockers and thiazide diuretics may be especially useful for older adults with isolated systolic hypertension or in cases where the use of RAAS blockers are contraindicated or restricted due to their potential risks, such as in women of childbearing age.
The polygon in Figure 9.2 shows the preferred (connected by a green line), contraindicated (red line) and possible but less often studied (dotted line) combinations. 11. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017; 317(2):165-82. In stage 3 hypertension and resistant hypertension patients, the goal is to optimize the triple treatment with preferred medications—ACEIs or ARBs, dihydropyridine CCBs, and thiazide or thiazide-like DIUs. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96. A clinical trial assessed the fixed triple combination of amlodipine, valsartan, and hydrochlorothiazide, all available in Brazil, for stages 2 and 3 HT patients, and found mean decreases of 39.7 mm Hg in systolic BP and 24.7 mm Hg in diastolic BP, significantly higher than two-drug combinations involving the same medications. 563563. Calhoun DA, Lacourcière Y, Chiang YT, Glazer RD. Triple antihypertensive therapy with amlodipine, valsartan, and hydrochlorothiazide: a randomized clinical trial. Hypertension. 2009;54(1):32-9.
Failing to reach the blood-pressure target with triple therapy requires the use of a fourth drug, and the current preferred medication is spironolactone. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.
565. Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, et al. The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies. Am J Hypertens. 2015;28(11):1376–85.
566. Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159-66.-567567. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68. BBs, clonidine, 564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. and doxazosin 567567. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68. are options for 4thor 5thdrugs, and hydralazine 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. may also be added in cases of intolerance to any of the previous antihypertensive options and in resistant HT. 503503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96. In the PATHWAY 2 study, 567567. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68. amiloride use was shown to be as effective as spironolactone, providing an alternate treatment for resistant HT. However, the medication is not available from manufacturers in Brazil. The ReHOT study 564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. showed that the efficacy of clonidine is similar to that of spironolactone as the 4thmedication for resistant HT patients. However, in 24-hour ambulatory BP analysis, spironolactone outperformed clonidine.
Treatment combining two renin-angiotensin system blockers, such as an ACEI with an ARB or any of the two with renin inhibitors, is contraindicated, since they lead to an increase in adverse effects without decreasing CV outcomes. 568568. Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372(9638):547–53.-569569. Parving H-H, Brenner BM, McMurray JJV, de Zeeuw D, Haffner SM, Solomon SD, et al. Cardiorenal End Points in a Trial of Aliskiren for Type 2 Diabetes. N Engl J Med. 2012;367(23):2204–13.
Chart 9.3 lists the major clinical trials that used combinations of antihypertensive medications, while Chart 9.4 shows the primary levels of evidence and level of recommendation of pharmacological treatments. Figure 9.1 shows the usual steps of combining medications for HT control.
| Key Takeaways |
|---|
| The primary objectives of antihypertensive treatment are lowering blood pressure and the risk of CV outcomes and mortality associated with hypertension. |
| Pharmacological treatment should be combined with nonpharmacological measures, and the preferred antihypertensive classes for use in monotherapy or combination therapies are: thiazide or thiazide-like diuretics, CCBs, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and beta-blockers (with specific indications). |
| Combining medications is the first recommended strategy for moderate- to high-risk stage 1 hypertensive patients and stages 2 and 3 patients, preferably in a single pill. Monotherapy should be considered for low-risk stage 1 hypertensive patients and for oldest old and/or frail individuals. |
| Two-drug treatments should begin with an ACEI or ARB combined with a thiazide or thiazide-like DIU or a CCB. In nonobese high-risk patients, CCB combinations are preferred. |
| When two medications combined are unable to control BP, patients should be prescribed three drugs, usually an ACEI or ARB combined with a thiazide or thiazide-like DIU and a CCB; if needed, add spironolactone next. |
10. Hypertension And Associated Clinical Conditions
10.1. Diabetes Mellitus (DM)
Hypertension (HT) is a frequent finding in DM patients, especially type 2 diabetes. Evidence shows the benefits of lowering BP for this population, with subsequent lower rates of macro and microvascular events and lower mortality. These include lower rates of chronic kidney disease (CKD), 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,329329. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: Systematic review and meta-analyses. BMJ. 2016;24:352 i717. diabetic retinopathy, and albuminuria. 576576. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15. Current data show a major reduction in cardiovascular (CV) risk for DM patients, though it remains a high-prevalence illness and an important risk factor (RF) for cardiovascular disease (CVD). 577577. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics – 2018 update: a report from the American Heart Association. Circulation. 2018 Mar 20;137(12):e67-e492.,578578. Gaede P, Vedel P, Larsen N, Gunnar VH Jensen, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383-93. The relationship between DM and HT provides relevant data, such as the presence of HT in 40% of recently-diagnosed patients with type 2 DM 579579. . Hypertension in Diabetes Study (HDS): I. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertens. 1993;11(3):309-17. and that 50% of type DM patients become hypertensive before the onset of albuminuria. This population is at high CV risk, so assessing urinary albumin and creatinine excretion, fundus health, and dysautonomia should be part of the investigation. 580580. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. Erratum in: JAMA. 2014;311(17):1809.
10.1.1. Treatment Objectives
Randomized clinical trials show the benefits of antihypertensive treatment for this population, such as the lower incidence of stroke, coronary syndromes, and CKD when BP levels below 140/90 mm Hg are achieved. In a meta-analysis of 13 clinical trials involving DM patients, systolic blood pressure (PAS) between 131 and 135 mm Hg decreased all-cause mortality risk by 13%, while more intensive SBP control to ≤ 130 mm Hg was associated with a greater decrease in strokes. 581581. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810. A second meta-analysis found significant decreases in mortality from achieving a mean SBP of 138 mm Hg and a significant decrease in strokes with a mean of 122 mm Hg. 576576. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15. Therefore, BP control is important to lower the risk of micro and macrovascular complications and should be maintained if these benefits are to be sustained (LR: I, LE: A).
Rigorous nonpharmacological treatment is required for all diabetic hypertensive patients. Office BP ≥ 140/90 mm Hg indicates the need for pharmacological treatment. All medications used in lowering BP may be administered to diabetic patients. The evidence supports the preferential use of RAAS blockers, particularly for patients with end-organ damage (EOD). 526526. Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):1004-10.,582582. Niskanen L, Hedner T, Hansson L, Lanke J, Niklason A; CAPPP Study Group. Reduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/ beta-blocker-based treatment regimen: a sub analysis of the Captopril Prevention Project. Diabetes Care. 2001;24(12):2091-6.
583. Ostergren J, Poulter NR, Sever PS, Dahlof B, Wedel H, Beevers G, et al. ASCOT Investigators. The Anglo-Scandinavian Cardiac OutcomesTrial: blood pressure-lowering limb: effects in patients with type II diabetes. J Hypertens. 2008;26:2103-.11.-584584. Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, et al. ACCOMPLISH Investigators. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010;56(1):77-85. BP often requires combination therapy, and calcium channel blockers (CCBs) and/or diuretics (DIUs) are the recommended drug classes for combinations with RAAS inhibitors. 506506. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.,585585. Tocci G, Paneni F, Palano F, Sciarretta S, Ferrucci A, Kurtz T, et al. Angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers and diabetes: a meta-analysis of placebo-controlled clinical trials. Am J Hypertens. 2011;24(5):582-90. Combining two or more classes in a single galenic formulation should be considered, taking into account that adherence to treatment is paramount in this high-risk population.
10.2. Metabolic Syndrome (MS)
MS is characterized by a set of CV risk factors, including central obesity, high glycemia, and typical dyslipidemia (high triglycerides and low HDL-cholesterol levels) associated with increased BP. 586586. Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hipertension in the metabolic syndrome. Nutr J. 2008 Apr 17;7:10.
587. Alberti KG, Zimmet P, Shaw J. Metabolic Syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469-80.-588588. Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care. 2005;28(9):2322-5. These metabolic changes are found in 30 to 40% of HT patients, 589589. Kahn R, Buse J, Ferrannini E, Stern M. The metabolic Syndrome: Time for a critical appraisal: Joint statement from American Diabetes Association and European Association for the Study of Diabetes. Diabetes Care. 2005; 84 Supll 1):3-28. and the presence of high blood pressure (BP) in MS increases global CV risk by triggering mechanisms associated with prothrombotic and pro-inflammatory states. 590590. Gagliardi ART. Obesidade central, bases hormonais e moleculares da síndrome metabólica. Rev Soc Cardiol Estado de São Paulo. 2004;14(4):557-66. Therefore, investigating metabolic alterations from MS and central obesity is indispensable for HT patients. Lifestyle changes (LSCs) for weight loss, lower sodium intake, and controlling dysglycemia and dyslipidemia are recommended for all patients in these conditions. 591591. Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al.Prevention of type 2 diabetes mellitus by changes in life style among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344(18):1343–50. Pharmacological treatment should be initiated whenever BP ≥ 140/90 mm Hg, since there is no evidence of benefit in the use of antihypertensive agents for MS with normal BP levels. 592592. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-52. Erratum in: Circulation. 2005;112(17):e298. The choice of antihypertensive medications should prioritize therapeutic classes capable of improving insulin resistance, or at least not make it worse, such as angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II AT1receptor blockers (ARBs), and CCBs. DIUs and beta-blockers (BBs), except for direct-acting vasodilators, may be indicated as additional medications. 593593. Stears AJ, Woods SH, Watts MM, Burton TJ, Graggaber J, Mir FA, Brown MJ. A double-blind, placebo-controlled, crossover trial comparing the effects of amiloride and hydrochlorothiazide on glucose tolerance in patients with essential hypertension. Hypertension .2012; 59(5):934–42.
10.3. Coronary Artery Disease (CAD)
Robust epidemiological evidence connects HT to CAD. Data from the INTERHEART study show that 25% of infarctions (AMI) may be attributable to HT. 286286. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364(9438):937-52. A meta-analysis assessing the impact of BP found a mean decrease of 17% in CAD for every 10 mm Hg decrease in SBP. 8585. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67.
Treatment for HT associated with CAD, which includes post-AMI patients with chest angina and myocardial revascularization (MRV), should preferably comprise BBs, ACEIs, or ARBs, in addition to statins and acetylsalicylic acid. Beta-blockers are beneficial after AMI, especially within 2 years from the acute event. 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665. Similarly, ACEIs and ARBs tested on that condition have also proven beneficial. 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.,594594. Borghi C, Bacchelli S, Degli Esposti D, Bignamini A, Magnani B, Ambrosioni E. Effects of the administration of an angiotensin-converting enzyme inhibitor during the acute pHAe of myocardial infarction in patients with arterial hypertension. SMILE Study Investigators. Survival of Myocardial Infarction Long-term Evaluation. Am J Hypertens. 1999;12(7):665-72.,595595. Gustafsson F, Kober L, Torp-Pedersen C, Hildebrandt P, Ottesen MM, Sonne B, et al. Long-term prognosis after acute myocardial infarction in patients with a history of arterial hypertension. TRACE study group. Eur Heart J. 1998;19(4):588-94. In patients with chronic CAD and multiple risk factors, such as HT, ACEIs have been found to lower relevant clinical outcomes 596596. Arnold JM, Yusuf S, Young J. Prevention of heart failure in patients in the heart outcomes prevention evaluation (HOPE) study. Circulation. 2003;107(9):1284-90. (LE: I; LR: A).
Regarding BP target, it is worth considering the likelihood of the J-curve effect, found in different studies, 597597. Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006;144(12):884-93.
598. Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, et al. ONTARGET investigators. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27(7):1360-9.
599. Zanchetti A, Mancia G. Longing for clinical excellence: a critical outlook into the NICE recommendations on hypertension management--is nice always good? J Hypertens. 2012;30(4):660-8.-600600. Mancia G, Parati G, Bilo G, Gao P, Fagard R, Redon J, et al. Ambulatory blood pressure values in the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET). Hypertension. 2012;60(6):1400-6. in which the excessive BP decreases, mainly in diastolic blood pressure (DBP), can trigger CV events in patients with obstructive CAD. Thus, the goal is to achieve SBP < 130 mm Hg and DBP < 80 mm Hg (LR: IIa; LE: B), while levels below 120/70 mm Hg should be avoided. 601601. Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al., CLARIFY Investigators. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 2016;388(10056):2142–52. Additional medications, such as CCBs and thiazide diuretics, 181181. Weber MA, Schiffrin EL, White WA, Mann S, Lindbolm LH, Venerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15. may be administered to achieve those BP targets.
10.4. Hypertension in Chronic Kidney Disease (CKD)
10.4.1. Patient in Conservative Treatment: Goals and Treatment
In CKD, BP levels to be achieved remain undetermined, and the evidence depends on associated morbidities. 602602. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-43. Nondiabetic patients treated with strict targets (< 130/80 mm Hg) showed slower disease progression only in subgroups with proteinuria, and CV events could not be assessed 603603. Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. African American Study of Kidney Disease and Hypertension Study Group: Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: Results from the AASK trial. JAMA. 2002;288(19):2421-31.,604604. Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. Modification of Diet in Renal Disease Study Group: The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N Engl J Med.1994;330(13): 877-84. (LR: IIa; LE: A). On the other hand, a meta-analysis has found lower mortality with intensive treatment for HT. 605605. Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(10):1498-505. In diabetic patients, strict targets led to decreased albuminuria, improved retinopathy and fewer strokes, but no impact on other CV outcomes 581581. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810.,606606. Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P, et al. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. 2011;29(7):1253-69.,607607. Cushman WC, Evans GW, Byington RP, Goff, Jr DC, Grimm RH, Cutler JA, et. al. ACCORD Study Group: Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17): 1575-85. (LR: IIa; LE: A).
A study with 9361 nondiabetic patients, out of which 2646 had CKD, found a decrease in CV events in the order of 25% for the treatment group that sought SBP below 120 mm Hg. This suggests the probable benefits provided by this strategy in CV protection for CKD patients 8686. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16. (LR: I; LE: A).
In terms of pharmacological treatment, ACEIs or ARBs are indicated for hypertensive patients with or without albuminuria, and its use in combination therapy is proscribed 608608. Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, et al. VA NEPHRON-D Investigators. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 2013;369(20):1892-903. (LR: I; LE: A). Thiazide 8383. Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665. or loop diuretics, the latter for G4 and G5 CKD, and CCBs are effective, especially in combination with ACEIs or ARBs 609609. Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. ACCOMPLISH Trial Investigators. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomized controlled trial. Lancet. 2010;375(9721):1173-81. (LR: I; LE: A). BBs are indicated for CAD and associated heart failure (HF). 610610. Foody JM, Farrell MH, Krumholz HM. beta-blocker therapy in heart failure: Scientific review. JAMA 2002;287(7): 883–9. Mineralocorticoid receptor antagonists lower proteinuria, but may cause hyperpotassemia. Clinical trials of new antagonists in this class are in progress. 611611. Clinical Trial. Efficacy and Safety of Finerenone in Subjects with Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (NCT02540993). US: National Institutes of Health; 2020.
| This guideline recommends a BP target < 130/80 mm Hg for adults with HT and CKD, whether diabetic or not. Stricter targets may be sought in select cases, under strict vigilance and after patients have been informed of the risks. |
|---|
10.4.2. Patients in Renal Replacement Therapy (RRT): Goals and Treatment
Managing HT in patients undergoing dialysis treatment can be a challenge, especially due to the volume overload that increases BP variability, overestimating it pre-dialysis and overestimating it afterward. 612612. Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and post-dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. CJASN. May 2006;1(3):389-98. There is no evidence regarding optimum BP levels for dialysis patients, but the most often accepted values immediately before and after hemodialysis (HD) are ≤ 140/90 mm Hg and ≤130/80 mm Hg, respectively 613613. Silva GV, Barros S, Abensur H, Ortega KC, Mion Jr D. Cochrane Renal Group Prospective Trial Register: CRG060800146. Home blood pressure monitoring in monitoring in blood pressure control among hemodialysis patients: an open randomized clinical trial. Nephrol Dial Transplant. 2009; 24(12):3805-11.,614614. Georgianos PI, Agarwal R. Blood pressure and mortality in long-term hemodialysis-time to move forward. Am J Hypertens. 2017;30(3):211-22. (LR: IIa; LE: C). For these patients, there is a (paradoxical) U-shaped association between SBP measured at the dialysis unit and CVD risk, with values above 160 mm Hg or < 110 mm Hg implicated in increased mortality 614614. Georgianos PI, Agarwal R. Blood pressure and mortality in long-term hemodialysis-time to move forward. Am J Hypertens. 2017;30(3):211-22.,615615. Bansal N, McCulloch CE, Lin F, Alper A, Anderson AH, Cuevas M, et al. Blood pressure and risk of cardiovascular events in patients on chronic hemodialysis: the CRIC study (Chronic Renal Insufficiency Cohort). Hypertension. 2017;70(2):435-43. (LR: IIa; LE: B).
In this population, home BP readings are more reproducible, provide relevant information for therapeutic decisions, and are better associated with BP control 613613. Silva GV, Barros S, Abensur H, Ortega KC, Mion Jr D. Cochrane Renal Group Prospective Trial Register: CRG060800146. Home blood pressure monitoring in monitoring in blood pressure control among hemodialysis patients: an open randomized clinical trial. Nephrol Dial Transplant. 2009; 24(12):3805-11. (LR: IIa; LE: B). Systolic means from home measurements are linearly associated with increased CV risk. 615615. Bansal N, McCulloch CE, Lin F, Alper A, Anderson AH, Cuevas M, et al. Blood pressure and risk of cardiovascular events in patients on chronic hemodialysis: the CRIC study (Chronic Renal Insufficiency Cohort). Hypertension. 2017;70(2):435-43.,616616. Georgianos PI, Agarwal R. Systolic and diastolic hypertension among patients on hemodialysis: Musings on volume overload, arterial stiffness, and erythropoietin. Semin Dial. 2019;32(6):507-12. In addition to hypervolemia, arterial stiffness is an important cause of systolic hypertension in stage 5D CKD patients. This specific phenotype reflects the acceleration of the atherosclerosis process and premature vascular aging in this population. 616616. Georgianos PI, Agarwal R. Systolic and diastolic hypertension among patients on hemodialysis: Musings on volume overload, arterial stiffness, and erythropoietin. Semin Dial. 2019;32(6):507-12. Other mechanisms, such as sleep apnea, 617617. Tada T, Kusano KF, Ogawa A, Iwasaki J, Sakuragi J, Kusano I, et al. The predictors of central and obstructive sleep apnoea in haemodialysis patients. Nephrol Dial Transplant 2007; 22:1190-7. sympathetic hyperactivity, 618618. Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG, et al. Hypertension in hemodialysis patients treated with atenolol or lisinopril: A randomized controlled trial. Nephrol Dial Transplant.2014;29(3):672-81. and erythropoietin use, should also be considered. 616616. Georgianos PI, Agarwal R. Systolic and diastolic hypertension among patients on hemodialysis: Musings on volume overload, arterial stiffness, and erythropoietin. Semin Dial. 2019;32(6):507-12.
HT treatment for patients undergoing dialysis treatment is only effective for 1/3 of individuals, and is even harder to achieve due to hemodynamic instability during sessions, which may cause intradialytic hypotension or hypertension, leading to poorer CV prognoses 619619. Kishnan N and Peixoto AJ. We hold antihypertensives prior to dialysis. Semin Dial. 2016 Jul;29(4):323-5. (LR: IIa; LE: B).
Treatment should start with measures focusing on achieving “dry weight,” such as salt and water restriction and ultrafiltration in dialysis 620620. Agarwal R and Sinha AD. Clinical pharmacology of antihypertensive therapy for the treatment of hypertension in chronic kidney disease. Clin J Am Soc of Nephrol 2019;14(5):757-64. (LR: IIa; LE: A). Regardless, approximately 60% of dialysis patients require three or more antihypertensives, in several combinations, to control HT 620620. Agarwal R and Sinha AD. Clinical pharmacology of antihypertensive therapy for the treatment of hypertension in chronic kidney disease. Clin J Am Soc of Nephrol 2019;14(5):757-64. (LR: IIa; LE: A). In this population, sympathetic nervous system (SNS) hyperactivity has a major role in the origins of HT and in CVD. Accordingly, beta blockade was superior to ACE inhibition in preventing CV morbidity and in BP control for patients with left ventricular hypertrophy (LVH) undergoing hemodialysis treatment. 618618. Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG, et al. Hypertension in hemodialysis patients treated with atenolol or lisinopril: A randomized controlled trial. Nephrol Dial Transplant.2014;29(3):672-81. In kidney transplant patients, CCBs and ARBs are the first option, since there is evidence that they prevent graft loss 621621. Cross NB, Webster AC, Masson P, O’ Connel PJ, Craig JC, et al. Antihypertensive treatment for kidney transplant recipients. Transplantation. 2009;88(1):7-18.,622622. Ibrahim HN, Jackson S, Connaire J, Matas A, Ney A, Najafian B, et al. Angiotensin II blockade in kidney transplant recipients. J Am Soc Nephrol. 2013;24(2):320-7. (LR: I; LE: A).
| This guideline suggests the individualization of treatment in RRT, considering comorbidities, pharmacokinetics, and the cardioprotective effect of medications. |
|---|
10.5. Heart Failure (HF)
HT has a key role in the pathophysiology of HF, leading to the onset of LVH and left ventricular diastolic and systolic dysfunction. 623623. Stokes J 3rd, Kannel WB, Wolf PA, D’Agostino RB, Cupples LA. Blood pressure as a risk factor for cardiovascular disease the framingham study-30 years of follow-up. Hypertension. 1989;13(5):I-13-I–18.
624. Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5(2):167–73.-625625. Goyal D, Macfadyen RJ, Watson RD, Lip GYH. Ambulatory blood pressure monitoring in heart failure: A systematic review. Eur J Heart Fail. 2005;7(2):149–56. It is the greatest RF for the disease, and usually precedes the clinical syndrome by several years. In HF with preserved ejection fraction (HFpEF), HT is even more frequent, and it is the most common RF, with prevalence rates of up to 90%. 626626. Pfeffer MA. Heart Failure and Hypertension Importance of Prevention Heart failure Randomized clinical trials Antihypertensive agents Prevention. 2017;101(1):19–28.
Early diagnosis of HT and adequate treatment can significantly lower the risk of developing HF, especially for older adults. Pharmacological strategies for BP control promote decreases of approximately 50% in HF incidence in adults, and a 64% decrease for those age 80 and older. 560560. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of Hypertension in Patients 80 Years of Age or Older. N Engl J Med. 2008;358(18):1887–98.,627627. Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J Am Coll Cardiol. 1996;27(5):1214–8.-628628. Tadic M, Cuspidi C, Frydas A, Grassi G. The role of arterial hypertension in development heart failure with preserved ejection fraction: just a risk factor or something more? Heart Fail Rev. 2018;23(5):631–9. The SPRINT trial, with a stronger SBP decrease target (< 120 mm Hg) for a high CV risk population, found a decrease of 27% in total mortality and 38% in progression to HF. 8686. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16.,629629. Kostis JB, Davis BR, Cutler J, Grimm RH, Berge KG, Cohen JD, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. J Am Med Assoc. 1997;278(3):212–6. The impact of antihypertensive treatment on preventing HF has been found for various classes of antihypertensive medication, such as BBs, DIUs, CCBs, and ACEIs. 630630. Thomopoulus C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment .6.Prevention of heart failure and new-onset heart failure–meta-analyses of randomized trials. J Hypertens. 2016;34(3):373-84.
BP targets in HF settings should be similar to those recommended for high CV risk individuals, ie, < 130/80 mm Hg. 631631. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology / American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017; 136(6):e137-e161. HT treatment in HF should consider its presentation, ie, whether with preserved ejection fraction (HFpEF) or reduced ejection fraction (HFrEF) ( Chart 10.1 ). The first therapeutic antihypertensive option for HFrEF should supplement medications promoting neurohormonal blockade, be dose-optimized, and have scientific evidence proving it reduces mortality. 632632. Rohde LEP, Montera MW, Bocchi EA, Clausell NO, Albuquerque DC, Rassi S, et al. Diretriz Brazileira de insuficiência cardíaca crônica e aguda. Arq Bras Cardiol. 2018;111(3):436–539. These medications are RAAS blockers, BBs, and aldosterone antagonists. The sacubitril/valsartane combination is a new treatment option impacting mortality reduction in HFrEF, but still with no evidence of benefits for HT. 633633. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371 (11): 993-1004.
If blood pressure levels remain high despite the neurohormonal blockade, they can also be combined with DIUs; vasodilator hydralazine-nitrate combination; or dihydropyridine CCBs. Nondihydropyridine CCBs, such as diltiazem and verapamil, and BBs are contraindicated. 631631. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology / American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017; 136(6):e137-e161.
Due to the strong association between HFpEF and HT, antihypertensive treatment is indicated for most patients. Diuretics should be used for BP control and for symptoms connected to hypervolemia, but randomized clinical trials have not found lower mortality rates for HFpEF patients. Despite the lack of evidence about the benefits of SNS and RAAS blockers to lower HFpEF mortality, these substances should still be used for blood pressure control. 634634. Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJV, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-preserved trial. Lancet. 2003;362(9386):777–81.
635. Forman D, Gaziano JM. Irbesartan in patients with heart failure and preserved ejection fraction. Curr Cardiovasc Risk Rep. 2009;3(5):311–2.
636. Cleland JGF, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27(19):2338–45.
637. Yamamoto K, Origasa H, Hori M. Effects of carvedilol on heart failure with preserved ejection fraction: The Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15(1):110–8.
638. Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.-639639. Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20. Other classes of antihypertensives may also be used.
The relationship between SBP levels and CV mortality follows a J-shaped curve, especially for HFrEF. 640640. Lee TT, Chen J, Cohen DJ, Tsao L. The association between blood pressure and mortality in patients with heart failure. Am Heart J. 2006;151(1):76-83.,641641. Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43(8):1439–44. Data from clinical trials such as Copernicus, DigTrial, Val-HeFT and PARADIGM-HF 318318. Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018 Jul 15;263:69-74.,642642. Rouleau JL, Roecker EB, Tendera M, Mohacsi P, Krum H, Katus HA, et al. Influence of pretreatment systolic blood pressure on the effect of carvedilol in patients with severe chronic heart failure: The Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) study. J Am Coll Cardiol. 2004;43(8):1423–9.
643. Anand IS, Rector TS, Kuskowski M, Thomas S, Holwerda NJ, Cohn JN. Effect of baseline and changes in systolic blood pressure over time on the effectiveness of valsartan in the Valsartan Heart FailureTrial. Circ Heart Fail. 2008;1(1):34-42-644644. Böhm M, Young R, Jhund PS, Solomon SD, Gong J, Lefkowitz MP, et al. Systolic blood pressure, cardiovascular outcomes and efficacy and safety of sacubitril/ valsartan (LCZ696) in patients with chronic heart failure and reduced ejection fraction: Results from PARADIGM-HF. Eur Heart J. 2017;38(15):1132-43. have verified the relationship between lower BP values and higher mortality rates.
In HFpEF, the association between BP levels and clinical outcomes remains controversial. 317317. Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018;3(4):288–97.,318318. Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018 Jul 15;263:69-74. In that patient group, BP levels should be kept within the 120-129/70-79 mm Hg target range.
10.6. Hemorrhagic Stroke and Ischemic Stroke
Ischemic and hemorrhagic stroke are the most frequent manifestations of the vascular damage caused by HT and are the leading cause of death and impairment for those patients. 292292. Manning LS, Mistri AK, Potter J, Rothwell PM, Robinson TG. Short-term blood pressure variability in acute stroke: post hoc analysis of the controlling hypertension and hypotension immediately post stroke and continue or stop post-stroke antihypertensives collaborative study trials. Stroke. 2015; 46(6):1518-24. Preventing all forms of stroke is possible by achieving BP target levels with adequate treatment (see Chapter 6) 291291. PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358(9287):1033-41.,645645. Rashid P. Leornardi-Bee J. Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34(11):2741-8.
646. PATS Collaborating Group. Poststroke antihypertensive treatment study: a preliminary result. Chin Med J (Engl). 1995;108(9):710-7.
647. Gueyffier F, Boissel JP, Boutitie F, Pocock S, Coope J, Cutler J, et al. Effect of antihypertensive treatment in patients having already suffered from stroke. Gathering the evidence. The INDANA (IN-dividual Data Analysis of Antihypertensive intervention trials) Project Collaborators. Stroke. 1997;28(12):2557-62.
648. Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32(11):1032-40.
649. Schrader J, Luders S, Kulschewski A, Hammersen F, Plate K, Berger J, et al; MOSES Study Group. Morbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES). Stroke. 2005;36(6):1218-26.
650. Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, et al; ProFESS Study Group. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med. 2008;359(12):1225-37.
651. White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, et al; SPS3 Investigators. Blood pressure after recent stroke: baseline findings from the secondary prevention of small subcortical strokes trial. Am J Hypertens. 2013;26(9):1114-22.-652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110. (LR: IIa; LE: B).
10.6.1. Hemorrhagic Stroke
High BP increases the likelihood of hematoma expansion, leading to worse prognosis and increased risk of death. 653653. Rodriguez-Luna D, Pineiro S, Rubiera M, Ribo M, Coscojuela P, Pagola J, et al. Impact of blood pressure changes and courseon hematoma growth in acute intracerebral hemorrhage. Eur J Neurol.2013;20(9):1277–83. Robust studies suggest that lowering BP (within 6 h) to values <140/90 mm Hg does not lower the rates of primary events, including mortality. 654654. Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al, INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355–65. Therefore, immediately lowering BP for hemorrhagic stroke cases is not recommended unless SBP levels are > 220 mm Hg.
10.6.2. Ischemic Stroke
The benefits of lowering BP for strokes are less clear, but should be considered for thrombolysis candidates, since, in their case, if BP > 180/105 mm Hg, there may be a greater risk of hemorrhaging. 655655. Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, et al. Relationship of blood pressure, antihypertensive therapy, and outcome inischemic stroke treated with intravenous thrombolysis: retrospective analysisfrom Safe Implementation of Thrombolysis in Stroke-International StrokeThrombolysis Register (SITS-ISTR). Stroke. 2009;40(7):2442–9.,656656. Wu W, Huo X, Zhao X, Liao X, Wang C, Pan Y, et al.Relationship between blood pressure and outcomes in acute ischemic strokepatients administered lytic medication in the TIMS-China Study. PLoS One.2016;11(2):e0144260. A meta-analysis suggests that lowering blood pressure in ischemic strokes may have a neutral effect on mortality. 657657. Lee M, Ovbiagele B, Hong KS, Wu YL, Lee JE, Rao NM, et al. Effect of blood pressure lowering in early ischemic stroke: meta-analysis. Stroke. 2015;46(7):1883-9.,658658. Zhao R, Liu FD, Wang S, Peng JL, Tao XX, Zheng B, et al. Blood pressure reduction in the acute phase of an ischemic stroke does not improve short- or longtermdependency or mortality: a meta-analysis of current literature. Medicine(Baltimore) 2015;94(23):e896.
Chart 10.2 , adapted from the ESC and ESH guidelines, 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. lists therapeutic targets and recommendations for acute stroke and cerebrovascular disease patients.
| Key Takeaways |
|---|
| BP control is important to lower the risk of micro and macrovascular complications and should be maintained if these benefits are to be sustained (LR: I, LE: A). Office BP ≥ 140/90 mm Hg indicates the need for pharmacological treatment preferably accompanied by LSCs and the use of RAAS blockers, while DIUs and CCBs may be added to achieve a blood-pressure target of <140/90 mm Hg. |
| Pharmacological treatment should be initiated for MS whenever BP ≥ 140/90 mm Hg, prioritizing the use of metabolically neutral antihypertensives or those that improve insulin sensitivity, such as ACEIs, ARBs, and CCBs. |
| In CKD patients, the BP target is <130/80 mm Hg, and may be stricter in select cases. In dialysis patients, achieving “dry weight” is key. Approximately 60% of dialysis patients require 3 or more antihypertensives, in several combinations, to control HT. For kidney transplant patients, CCBs and ARBs represent their first therapeutic option. |
| Immediately lowering BP for hemorrhagic stroke cases is not recommended unless SBP levels are ≥ 220 mm Hg; if so, use IV medications, with target SBP 180 mm Hg. |
| For HT and HF (PEF and REF) patients, the blood-pressure target should be <130/80 mm Hg. In HFrEF, blood pressure levels should be controlled with BBs, ARBs, and spironolactone, while all antihypertensives may be used for HFpEF. |
| Treatment for HT associated with CAD, which includes post-AMI patients with chest angina and myocardial revascularization (MRV), should preferably comprise beta-blockers, ACEIs, or ARBs, in addition to statins and acetylsalicylic acid, with a blood-pressure target of < 130/80 mm Hg. |
| J- or U-shaped curves are often seen in CAD patients, and levels below 120/70 mm Hg are to be avoided. In CKD, especially in dialysis patients, SBP levels above 160 mm Hg or <110 mm Hg have been implicated in increased mortality. |
11. Hypertension in Pregnancy
11.1 Epidemiology
Hypertensive disorders of pregnancy is one of the leading causes of maternal and perinatal mortality throughout the world. From 0.9 to 1.5% of pregnant women have chronic hypertension, and it is estimated that pre-eclampsia (PE) complicates 2 to 8% of pregnancies globally. 659659. Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and out-comes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206(2):134.e1–8.,660660. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–44. Those syndromes are causal factors associated with perinatal and maternal death, may permanently impair maternal health and may cause major issues from preterm birth associated with early indications for intervention (elective preterm birth). 660660. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–44. In Brazil, PE is the leading cause of provider-initiated preterm birth, 661661. Ramos JGL, Sass N, Costa SHM. Preeclampsia. Rev Bras Ginecol Obstet. 2017;39(9):496–512. and the estimated incidence rates are 1.5% for PE and 0.6% for eclampsia. 662662. Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):1–7. The prevalence of eclampsia in the more developed regions of Brazil is 0.2%, with an 0.8% mortality rate, 661661. Ramos JGL, Sass N, Costa SHM. Preeclampsia. Rev Bras Ginecol Obstet. 2017;39(9):496–512. while prevalence rates in less developed regions rise to 8.1%, with a corresponding mortality rate of 22.0%. 663663. Giordano JC, Parpinelli MA, Cecatti JG, Haddad SM, Costa ML, Surita FG, et al. The burden of eclampsia: results from a multicenter study on surveillance of severe maternal morbidity in Brazil. PLoS One. 2014;9(5):e97401.
11.2. Classification of Hypertension in Pregnancy
We recommend the definitions and classification put forth by the A merican College of Obstetricians and Gynecologists (ACOG), 664664. . American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019 Jan;133(1):e1-e25.,665665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50. which can be found in Chart 11.1 (LR: IIb, LE: B).
11.3. Concept and Diagnostic Criteria
Hypertension in pregnancy is defined as the presence of systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg, considering the fifth Korotkoff sound, confirmed by another measurement after a 4-hour interval. Ideally, the measurement should be taken with the patient sitting down or in left lateral decubitus position, with a properly sized cuff. The manual auscultatory method is the gold standard, since automated devices may underestimate blood pressure (BP), especially in severe pre-eclampsia. Ambulatory blood pressure monitoring (ABPM) is superior to BP measurements at the physician's office and home blood pressure monitoring (HBPM) for nonpregnant women. For pregnant women, it helps avoid unnecessary treatment for white coat hypertension (WCH) and is useful in managing high-risk gestational hypertension and in detecting masked hypertension. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. The role of ABPM and HBPM is still controversial in pregnancy. The International Society for the Study of Hypertension in Pregnancy (ISSHP) recommends the use of ABPM before the 20th gestational week and HBPM for follow-up. 666666. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291-310. The cutoff point for HT is ≥ 135/85 mm Hg for daytime ABPM and ≥ 130/80 mm Hg for HBPM (Chapter 3).
The definition and classification of hypertensive disorders in pregnancy can be found in Chart 11.1 .
11.4. Prediction and prevention of pre-eclampsia
Calcium supplementation (> 1 g/day) is not recommended for pregnant women with normal calcium intake 667667. Hofmey GJ, Lawrie TA, Atallah ÁN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014; 6:CD001059. (LR: III, LE: A), but is recommended for those with low calcium intake and at intermediate to high risk of pre-eclampsia 667667. Hofmey GJ, Lawrie TA, Atallah ÁN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014; 6:CD001059. (LR: I, LE: A).
Low doses of acetylsalicylic acid (ASA) (75- 150 mg/day) at the end of the first gestational trimester can be useful for primary prevention of pre-eclampsia in pregnant women at intermediate to high risk of pre-eclampsia 668668. . CLASP: a randomized trial of low-dose aspirin for the prevention and treatment of pre-eclampsia among 9364 pregnant women. CLASP (Collaborative Low dose Aspirin Study in Pregnancy) Collaborative Group. Lancet. 1994; 343(8898):619–29.
669. Duley L, Henderson-Damart DJ, Meher S, King JF. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database of Syst Rev.2004;(1): CD 004659.-670670. Rolnik DL, Wright D, Poon L, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk of preterm preeclampsia. N Engl J Med. 2017;377(7):613–22. (LR: I, LE: A). However, its use is not recommended in the absence of risk 669669. Duley L, Henderson-Damart DJ, Meher S, King JF. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database of Syst Rev.2004;(1): CD 004659. (LR: III, LE: A).
Pre-eclampsia prediction should preferentially be performed during the 1st semester using assessment methods that take into consideration maternal clinical history (risk factors) associated with Doppler ultrasound to check for flow resistance in the uterine arteries. There are also promising laboratory tests to assess angiogenesis, such as serum soluble endoglin, PIGF (placental endotelial growth factor), sFlt-1 (soluble fms-like tyrosine kinase receptor-1), and sFlt-1/PlGF ratio, but which are still not available in clinical practice. 666666. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291-310.
In patients at high risk for PE, the use of calcium for low-intake populations (< 600 mg/day), a dose of 1.0 to 2g/day effectively lowers the risk of PE. 667667. Hofmey GJ, Lawrie TA, Atallah ÁN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014; 6:CD001059.
Chart 11.2 summarizes the use of ASA at low doses (75-150 mg/day) for eclampsia prevention. It should be initiated preferably before the 16th week, with no increase in maternal or fetal complications, and is recommended by international guidelines such as NICE 2019, 671671. Hypertension in pregnancy: diagnosis and management NICE guideline Published: 25 June 2019.[Internet] [Cited in 2019 may 23] Available at: www.nice.org.uk/guidance/ng133 .
www.nice.org.uk/guidance/ng133...
the WHO's 672672. World Health Organization. WHO. Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia. Geneve: 2011. and that of the American College of Obstetricians and Gynecologists (ACOG). 664664. . American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019 Jan;133(1):e1-e25. A study 670670. Rolnik DL, Wright D, Poon L, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk of preterm preeclampsia. N Engl J Med. 2017;377(7):613–22. involving 1776 patients, comparing acetylsalicylic acid at 150 mg and a placebo, starting at 11 to 14 weeks, found a total event rate (PE) of 1.6% for the acetylsalicylic acid group and 4.3% for the placebo group (OR: 0.38, 95% CI 0.2 to 0.74, p = 0.004). This confirms the protective effect of acetylsalicylic acid for high-risk pregnant women.
In its 2019 report on screening and prevention, 673673. Poon LC, Shennan A, Hyett JA, Kapur A, Hadar E, Divakar H, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(Suppl 1):1-33. the International Federation of Gynecology and Obstetrics (FIGO) suggests the use of the Fetal Medicine Foundation risk calculator to determine when acetylsalicylic acid is indicated in pre-eclampsia prevention. This useful tool is available at https://fetalmedicine.org/research/assess/pre-eclampsia/first-trimester.
11.5. Nonpharmacological Treatment
For SBP persisting above 160 mm Hg for more than 15 minutes, nonpharmacological treatment alone should not be used (LR: III, LE: B). Relative rest at hospital or day hospital with monitoring is suggested for pre-eclampsia (LR: IIa, LE: B). Hospitalization is indicated for patients with severe gestational hypertension (LR: I, LE: B).
Nonpharmacological treatment alone should not be used to treat severe HT persisting for > 15 min 674674. American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180. to prevent irreversible neurological damage, since SBP values > 155 mm Hg, especially > 160 mm Hg, are detected immediately before a stroke. 675675. Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressure. Obstet Gynecol. 2005;105(2):246-54. Severe diastolic hypertension (> 105 or 110 mm Hg) does not develop before most strokes in pregnant women with severe pre-eclampsia. 676676. Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG . 2011;118 (Suppl 1):1-203.
A systematic review found no differences in outcomes between strict rest and relative rest for pregnant women with hypertension and proteinuria. 677677. Meher S, Abalos E, Carroli G. Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database Syst Rev. 2005;19(4):CD003514. Relative rest at hospital, as compared with routine house activity, reduces the risk of severe hypertension. Rest is not routinely indicated for gestational hypertension. 677677. Meher S, Abalos E, Carroli G. Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database Syst Rev. 2005;19(4):CD003514. Prenatal care units and hospital admissions have similar clinical outcomes for mothers and newborns, but women may prefer treatment at day hospitals. 678678. Dowswell T, Middleton P, Weeks A. Antenatal day care units versus hospital admission for women with complicated pregnancy. Cochrane Database of Syst Rev. 2009;(4):CD001803.
Although there is no indication for specific care during hospitalization, maternal and fetal monitoring is required. Blood pressure should be measured periodically, with daily weight and diuresis assessment, and patients should be instructed about warning signs. Laboratory tests (CBC with platelet count, liver enzymes, uric acid, creatinine and proteinuria) should be performed once to twice a week. Fetal follow-up comprises assessment of growth, movements, well-being and biophysical profile, as well as ultrasound.
11.6. Expectant Management
Expectant management is not recommended after 37 gestational weeks for women with gestational hypertension and prehypertension 679679. Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG. Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88. (LR: III, LE: B). Expectant management is suggested between the 34th and 37th gestational weeks for stable women, without clinical worsening or severe hypertension 680680. Broekhuijsen K, van Baaren GJ, van Pampus MG, Ganzevoort W, Sikkema JM, Woiski MD, et al. Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. Lancet. 2015;385(9986):2492-501. (LR: IIa, LE: B).
Premature delivery for patients with PE can be associated with decreased mortality. 681681. Ronsmans C, Campbell O. Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health. 2011;11(Suppl 3):S8. Optimum delivery time before the 32nd to 34th weeks poses a dilemma due to the uncertainty in the balance between maternal safety (end of pregnancy) and fetal maturity (expectant). 681681. Ronsmans C, Campbell O. Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health. 2011;11(Suppl 3):S8. After the 34th week, survival is high and baby and placenta delivery is effective in developed countries. 681681. Ronsmans C, Campbell O. Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health. 2011;11(Suppl 3):S8. Physicians tend to delay birth until the 37th week, if it is considered safe.
The HYPITAT study compared induction of labor versus expectant monitoring for severe hypertension or PE without signs of severity (at the time, called mild PE) after the 36th week. 679679. Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG. Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88. Women in the intervention group had a 29% lower risk of worse maternal outcomes, without affecting neonatal outcomes, suggesting that expectant treatment up to 37 weeks is not indicated. 679679. Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG. Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88. In the HYPTAT-II study, in nonsevere HT between the 34th and 37th gestational weeks, expectant management increased maternal risk as compared to immediate delivery, but decreased the occurrence of neonatal respiratory distress syndrome. 680680. Broekhuijsen K, van Baaren GJ, van Pampus MG, Ganzevoort W, Sikkema JM, Woiski MD, et al. Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. Lancet. 2015;385(9986):2492-501. Therefore, immediate delivery is not justified, and expectant monitoring should be considered until the clinical situation worsens. If labor inducing labor before the 34th week is indicated and both maternal and fetal clinical statuses allow a 48-hour wait to see if the situation resolves, corticosteroid use for fetal pulmonary maturation may be considered. 682682. Peraçoli JC, Borges VTM, Ramos JG, Cavalli RC, Costa SHAM, Oliveira LG, et al. Pre-eclampsia/Eclampsia. Rev Bras Ginecol Obstet. 2019;41(5):318-32.
11.7. Pharmacological Treatment
Urgent pharmacological treatment is indicated for severe hypertension 674674. American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180.,675675. Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressure. Obstet Gynecol. 2005;105(2):246-54. and in the presence of warning signs (LR: I, LE: B). There is no consensus BP value to indicate when pharmacological treatment should be initiated. Pharmacological treatment should be initiated when BP is above 150-160/100-110 mm Hg 665665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.,674674. American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180.,676676. Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG . 2011;118 (Suppl 1):1-203. with the goal of keeping it in the 120-160/80-100 mm Hg range (LR: IIb, LE: B).
The choice of the antihypertensive medication depends on the attending physician’s experience and familiarity with the drug chosen and its side effects 683683. Duley L, Henderson-Smart DJ, Meher S. Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev. 2006;(3):CD001449. (LR: IIb, LE: B). The use of ACEIs, ARBs, and direct renin inhibitors is contraindicated in pregnancy (LR: I; LE: B), and atenolol and prazosin should be avoided if possible 683683. Duley L, Henderson-Smart DJ, Meher S. Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev. 2006;(3):CD001449.,684684. Centers for disease control and prevention. Postmarketing surveillance for angiotensin-converting enzyme inhibitor use during the first trimester of pregnancy – United States, Canada and Israel, 1987-1995. JAMA. 1997; 277(15):1193-4. (LR: IIa, LE: B).
Magnesium sulfate is recommended for eclampsia prevention and treatment (LR: I, LE: B). To avoid maternal deaths, SBP > 150-160 mm Hg should indicate urgent treatment, 676676. Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG . 2011;118 (Suppl 1):1-203. in line with other Brazilian and international guidelines, which set the cutoff point at 160 mm Hg. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
When to initiate pharmacological treatment for pregnant hypertensives with BP below 160/110 mm Hg is still controversial, except for pregnant women with end-organ damage (EOD). Cochrane's systematic review 685685. Abalos E, Duley L, Steyn DW. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database of Syst Rev. 2014;6(2): CD002252. showed that treating mild to moderate HT does not significantly lower maternal, fetal, and newborn morbidity.
However, the CHIPS trial, 686686. Magee LA, von Dadelszen P, Rey E, Ross S, Asztalos E, Murphy KE, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372(5):407-17.,687687. Magee LA, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, et al. The CHIPS randomized controlled trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood pressure? Hypertension. 2016;68(5):1153-9. which assessed aggressive treatment (DBP up to 85 mm Hg) versusnonaggressive treatment (DBP up to 100 mm Hg) in a post-hoc analysis, found a major increase in severe hypertension and unfavorable fetal outcomes, such as miscarriages, ICU stays longer than 48 hours, preterm birth, and low weight. Thus, new studies are assessing whether to administer medication starting at 140/90 mm Hg. 665665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.
According to ACOG, the HT control target should be SBP > 120 and < 160 mm Hg, and DBP > 80 and < 110 mm Hg, since both hypertension and induced hypotension may harm placental perfusion and, consequently, fetal growth. The goal is to prevent the progression of EOD and cardiac and cerebrovascular complications, as well as obstetric and fetal complications. 665665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.
Pharmacological therapy should begin as monotherapy using first-line medications (methyldopa, long-acting nifedipine, or beta-blockers, except atenolol). If proper control is not achieved, combine it with another first-line medication or a second-line one (thiazide diuretic, clonidine, and hydralazine); avoid combining medications from the same pharmacological class. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are formally contraindicated in case of pregnancy due to the risk of fetal malformation, which may lead to intrauterine renal failure, as are mineralocorticoid receptor antagonists, due to hormonal blockade, and atenolol, due to the high risk of fetal growth restriction associated with its use. Diuretics should also be avoided for PE patients due to the possibility of increasing intravascular volume depletion. 665665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.,688688. Butalia S, Audibert F, Côté AM, Firoz T, Logan AG, Magee LA, et al. Hypertension Canada’s 2018. Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34(5):526-31. A study comparing the efficacy of labetalol, long-acting nifedipine and methyldopa for managing severe gestational hypertension suggests that all medication classes were viable options, but long-acting nifedipine was more effective than labetalol and methyldopa. 689689. Easterling T, Mundle S, Bracken H, Parvekar S, Mool S, Magee LA, et al. Oral antihypertensive regimens (nifedipine retard, labetalol, and methyldopa) for management of severe hypertension in pregnancy: an open-label, randomised controlled trial. Lancet 2019;394(10203):1011-21.
Hypertensive emergencies in pregnant women may be treated with oral nifedipine (10 mg) or with IV hydralazine. Currently, the trend is to prefer nifedipine 10 mg, which may be repeated in 10 to 20 mg orally every 20 to 30 minutes, and if patients are unresponsive after the third dose, 5 mg of IV hydralazine every 20 to 30 minutes up to a dose of 15 mg. 674674. American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180.
In exceptional situations, such as acute pulmonary edema and refractory severe hypertension, the use of sodium nitroprusside may be considered the preferential option for urgent BP control 690690. Sass N, Itamoto CH, Silva MP, Torloni MR, Atallah NA. Does sodium nitroprusside kill babies? A systematic review. Sao Paulo Med J. 2007;125:108-11. for a maximum of 4 hours due to the risk of fetal cyanide poisoning.
In postpartum hypertension for nonchronic hypertensive patients, HT usually resolves within the 1stweek (5 to 6 days), but the risk of complications such as stroke, acute pulmonary edema (APE), and renal failure remains during this period. There is also risk of eclampsia during this period, and 32 to 44% of women may have postpartum seizures. 691691. Townsend R, O’Brien P, Khalil A. Current best practice in the management of hypertensive disorders in pregnancy. Integr Blood Press Control. 2016:9,79-94.
Postpartum women may take all antihypertensive medications, and breastfeeding is the only limiting factor. Therefore, physicians should prioritize antihypertensives excreted in breast milk to a lesser extent.
Chart 11.3 lists the main antihypertensive medications available in Brazil in terms of breastfeeding. 692692. Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-[Internet] [Cited in 2019 May 12] . Available from: https://www.ncbi.nlm.nih.gov/books/NBK501922/ .
https://www.ncbi.nlm.nih.gov/books/NBK50...
693. Regit-Azgrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018; 39(34):3165–241.-694694. Halpern DG, Weinberg CR, Pinnelas R, Mehta-Lee S, Economy KE, Valente AM. Use of Medication for Cardiovascular Disease During Pregnancy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(4):457-76. Hypertensive crises in postpartum women may be treated in the conventional manner. A study comparing captopril and clonidine for HT control (SBP ≥ 180 mm Hg ad DBP ≥ 110 mm Hg) found no significant difference between the two, only a tendency for clonidine to perform better on the 3rdday postpartum. 695695. Noronha Neto C C, Maia SSB, Katz L, Coutinho IC, Souza AR, Amorim MM. Clonidine versus Captopril for Severe Postpartum Hypertension: A Randomized Controlled Trial. Plos One. 2017;12(1):e0168124. Both were considered safe and effective for treating hypertensive emergencies in postpartum women. 696696. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366(9499):1797–803.
11.8. Future Cardiovascular Risk
Hypertensive disorders of pregnancy are a marker of future risk (I: A), and a more careful and integrated approach should be adopted for these women in order to effectively prevent cardiovascular and kidney disease (LR: I, LE: C). Patients who develop any form of HT during pregnancy, especially with negative outcomes, such as preterm birth and early PE, experience a consistent increase in risk of future CVD and kidney disease. 696696. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366(9499):1797–803.
697. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
698. Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, et al. Long-Term Cardiovascular Risk in Women With Hypertension During Pregnancy. J Am Coll Cardiol. 2019;74(22):2743-54.-699699. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800-9. The risk of chronic hypertension is 3 to 4 times higher, while risk of stroke is 1.8 times higher. Likewise, the risk of coronary artery disease (CAD) doubles with age. 696696. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366(9499):1797–803.,697697. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
In a prospective study, 698698. Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, et al. Long-Term Cardiovascular Risk in Women With Hypertension During Pregnancy. J Am Coll Cardiol. 2019;74(22):2743-54. gestational HT was associated with greater incidence of CAD (HR: 1.8; 95% CI: 1.3 to 2.6; p < 0.001), HF (HR: 1.7; 95% CI: 1.04 to 2.60; p = 0.03), aortic stenosis (HR: 2.9; 95% CI: 1.5 to 5.4; p < 0.001), and mitral insufficiency (HR: 5.0; 95% CI: 1.5 to 17.1; p = 0.01), showing a 30% global CV risk increase. Norwegian data show that PE is associated with a 3- to 15-fold increase in risk of stage 5 CKD. 699699. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800-9. Hypertensive disorders of pregnancy are a marker of future risk, and a more careful and integrated approach should be adopted for these women in order to effectively prevent CVD and kidney disease.
| Key Takeaways | |
|---|---|
| Classification | Pre-eclampsia, chronic hypertension, overlapping pre-eclampsia, and gestational hypertension. |
| Prevention | Calcium and acetylsalicylic acid for high-risk patients. |
| Nonpharmacological treatment | Should not be used for persistent SBP above 160 mm Hg for more than 15 minutes. Relative rest at hospital with monitoring for pre-eclampsia. Hospitalization of pregnant patients with severe HT. |
| Expectant management | Expectant management is suggested between the 34th and 37th gestational weeks for stable women, without clinical worsening or severe hypertension. |
| Pharmacological treatment | Urgent pharmacological treatment is indicated for severe hypertension and in the presence of warning signs. Pharmacological treatment should be initiated when BP is above 150-160/100-110 mm Hg, with the goal of keeping it in the 120-160/80-100 mm Hg range. The choice of the antihypertensive medication depends on the attending physician’s experience and familiarity with the drug chosen and its side effects. Magnesium sulfate is recommended for eclampsia prevention and treatment. |
12. Hypertension in Children and Adolescents
12.1. Epidemiological Context and Importance of Hypertension in Pediatrics
The prevalence of high blood pressure (HBP) and hypertension (HT) in children and adolescents has increased in recent years. The current prevalence of HT in the pediatric age group ranges from 3% to 5%, while HBP is estimated at 10-15%. 700700. Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113(3 Pt 1):475-82.,701701. McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and prehypertension among adolescents. J Pediatr. 2007;150(6):640-4. In children ages 7 to 12, HBP and HT prevalence rates are 4.7% and 1.9% respectively, and both are more prevalent among the obese. 702702. Brian KK, Elena K, Margaret DC, Yachim O, David SF, Cynthia LO. Prevalence of and trends in dyslipidemia and blood pressure among us child and adolescents 1999-2012. Jama Pediatr. 2015: 169(3):272-9.
The Brazilian Study of Cardiovascular Risks in Adolescents (ERICA) evaluated 73399 Brazilian students ages 12 to 17. Total HBP prevalence in Brazil was 14.5%, and the highest rate was 29.3% for boys ages 15 to 17. The overall prevalence of HT was 9.6%, likewise highest among older children. The study found that 17.8% of prevalence rates for HT among adolescents is attributable to obesity. 703703. Bloch VK, Klein CH, Szklo M, Kuschnir MCC et al. Prevalências de hipertensão arterial e obesidade Brazileiros. Rev. Saúde Pública. 2016: 50(supl 1)1-13.
Pediatric HT is usually asymptomatic, but as many as 40% of hypertensive children have left ventricular hypertrophy (LVH) at their initial diagnosis. Though oligosymptomatic in childhood, LVH is a precursor to arrhythmias and HF in adults. 704704. Brady TM, Redwine KM, Flynn JT; American Society of Pediatric Nephrology. Screening blood pressure measurement in children: are we saving lives? Pediatr Nephrol. 2014;29(6):947-50. Pediatric HT is also associated with the development of other changes to end-organs, such as increased carotid intima-media thickness, lower arterial distensibility, and retinal arteriolar narrowing. Blood pressure measurements from the age of 3 onwards are recommended, at least annually. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
12.2. Definition and Etiology
In children and adolescents, the definitions of HBP and HT are related to the normal distribution curve for blood pressure (BP) and their percentile distributions. The measurement uses auscultation, taking into consideration sex, age, and height percentile of the child. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,706706. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98(4 Pt 1):649–58.,707707. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114(2):555-76.
In 2017, normative BP scores and HT diagnosis and management recommendations for pediatric HT, excluding overweight and obese children and adolescents, were changed. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. The term prehypertension has been replaced by HBP. The new recommendations, below, redefine HT staging for children and adolescents, simplify recommendations for preventive assessment in routine pediatric visits, structure the initial management of patients diagnosed with HBP or HT, and increase the importance of ABPM readings in diagnosis and management for pediatric HT.
Chart 12.1 presents up-to-date definitions of normal BP, high BP and stages 1 and 2 HT in children and adolescents by age, sex, and height percentile. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. The younger the child and the higher the BP, the greater the chance of secondary HT. Parenchymal and obstructive nephropathies and renal artery stenosis are responsible for approximately 60 to 90% of cases and can affect all age ranges. Endocrine disorders, such as excessive mineralocorticoid, corticoid or catecholamine secretion, thyroid diseases, and hypercalcemia associated with hyperparathyroidism, account for approximately 5% of cases. Coarctation of the aorta is diagnosed in 2% of cases, while 5% of cases are attributed to other etiologies, such as adverse effects of vasoactive and immunosuppressant drugs, steroid abuse, central nervous system changes, and increased intracranial pressure. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
706. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98(4 Pt 1):649–58.-707707. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114(2):555-76.
Primary HT seems to be the most common form of HT in adolescents It is most often associated with overweight, obesity, and family history of HT.
12.3. Diagnostic
12.3.1. BP Measurement Methods
Measuring BP in children is recommended at every clinical assessment. It should be measured annually in children and adolescents ≥ 3 years old, taking into consideration established measurement standards. For children under the age of 3, blood pressure measurements should be performed in certain situations. BP measurements should be repeated at every appointment under conditions, such as obesity, kidney disease, coarctation of the aorta, DM or chronic use of medications known to be associated with increased BP. Correctly measuring BP, following the standards established above, is a precondition for obtaining reliable readings and properly categorizing pediatric BP. 176176. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697-716.,705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. Preferably, it should be measured in the right arm, with the patient lying down until the age of three, and, in older children, with the patient sitting down, their arms lying at heart level, using an adequately sized cuff. The air bag should be 80 to 100% as long as the arm circumference (AC) and at least 40% as wide as the AC. Blood pressure assessments should follow the procedures described in Chapter 3. Use the auscultatory method to check for audible Korotkoff sounds to 0 mm Hg. The point where sounds become muffled is considered for DBP (Korotkoff phase IV). During the first appointment, BP should be measured on the four limbs, and when measured on lower limbs (LLs), the patient should be placed in ventral decubitus position, using an appropriately-sized cuff on their thigh and placing the stethoscope on their popliteal artery. SBP at the LLs is usually 10 to 20% higher than BP measured at the brachial artery. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. Charts 12.2 and 12.3 list normal BP, high BP and stages 1 and 2 HT by sex, age, and height percentile, adapted from Flynn et al., 2017. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. Some authors consider the oscillometric method adequate for initial screening in children and adolescents, which would justifying developing tables using validated devices. 708708. Kulaga Z, Litwin M, Grajda A, Kułaga K, Gurzkowska B, Gó´zd´zM, et al. Oscillometric blood pressure percentiles for Polish normal-weight school-aged children and adolescents. J Hyper-tens. 2012;30(10):1942-54.,709709. Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS. Blood pressure percentiles by age and height from nonover-weight children and adolescents in Germany. Pediatrics.2011;127(4):e978-88. In Brazil, Jardim et al. have developed a blood pressure reference curve for nonoverweight adolescents ages 12 to 17 using the oscillometric method. 710710. Jardim TV, Rosner B, Bloch KV, Kuschnir MC, Szklo M, Jardim PC. Blood pressure reference values for Brazilian adolescents: data from the Study of Cardiovascular Risk in Adolescents (ERICA Study). J Pediatr. 2020;96(2):168-76.
The following clinical risk conditions determine the need for routine BP measurement for children 3 < years old: preterm birth, very low birth weight, intrauterine growth restriction, history of stay at neonatal intensive care unit (ICU) or umbilical catheterization after birth, congenital heart disease with or without surgical repair, recurring urinary tract infections, hematuria or proteinuria, nephropathy, solid organ transplantation, oncological disorders or bone marrow transplantation, chronic use of medications known to increase BP, system disorders associated with HT (neurofibromatosis, tuberous sclerosis, sickle cell anemia, among others), and evidence of intracranial hypertension. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
The oscillometric method is recommended for measuring BP in newborns (NB). Normative BP values for the neonates 15 days old and older and gestational age after birth of 26 to 44 weeks can be found in Chart 12.4 . 711711. Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome [published correction appears in Pediatr Nephrol. 2012;27(1):159-60]. Pediatr Nephrol. 2012;27(1):17–32. Oscillometric devices, duly validated for pediatric age groups, may be used for initial BP assessments. If elevated BP is suspected from oscillometric readings, auscultation should be used to verify the finding. Pediatric HT diagnoses are based on confirming BP values ≥ 95th percentile in three different visits using auscultation. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. Chart 12.5 provides a simplified list of BP values suggesting the need for additional clinical assessments. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,711711. Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome [published correction appears in Pediatr Nephrol. 2012;27(1):159-60]. Pediatr Nephrol. 2012;27(1):17–32.
12.4. History-Taking
Detailed data on birth, growth and development, personal antecedents of kidney, urological, endocrine, heart and neurological diseases, and lifestyle should be collected, in addition to data on the use of medications and other substances that may cause BP alterations. In addition, family antecedents for HT, kidney disease, and other CVRFs should be carefully assessed. Children ≥ 6 years old do not require extensive screening for secondary causes of HT in the presence of positive family history of HT, overweight, or obesity, and/or their history or physical examination do not suggest secondary causes. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,712712. Report of the second task force on blood pressure control in children–1987. Task force on blood pressure control in children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics. 1987;79(1):1–25.
12.5. Physical Examination
On physical examination, the patient's body mass index (BMI) should be calculated 713713. Guimarães IC, Almeida AM, Santos AS, Barbosa DB, Guimarães AC. Blood pressure: effect of body mass index and of waist circumference on adolescents. Arq Bras Cardiol. 2008;90(6):426-32. and the physician should investigate signs of secondary HT (see Chapter 15). 714714. Daniels Sr. Coronary risk factors in children. In: Moss & Adams. Heart disease in infants, children and adolescents. Philadelphia: Williams & Wilkins; 2013. p. 1514-48.
12.6. Additional tests
Laboratory and imaging tests are aimed at defining the etiology of HT (primary or secondary) and detecting end-organ damage (EOD) and cardiovascular risk factors (CVRFs) associated with HT (Charts 12.6 and 12.7 ). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,715715. Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al; European Society of Hypertension. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens. 2009;27(9):1719-42. End-organ assessments should be performed in all children and adolescents with stages 1 and 2 HT. Sleep study by use of polysomnography is indicated for children and adolescents with sleep disorders detected while taking their histories.705
12.7. Ambulatory Blood Pressure Monitoring (ABPM)
ABPM should be used to confirm HT in children and adolescents with office BP readings compatible with high BP for at least a year or with BP readings corresponding to stage 1 HT in three outpatient visits. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. It should also be considered in routine examinations for secondary HT, CKD, diabetes mellitus (DM), obstructive sleep apnea (OSA), obesity, post-operative coarctation of the aorta, preterm birth, solid organ transplantation, and RfHT. The procedure should follow standard techniques and use monitors validated for pediatric use as well as pediatric reference data. 716716. Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, Zachariah JP, Urbina EM Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014 ;63(5):1116-35.
The 6thABPM guidelines and 4thhome blood pressure monitoring (HBPM) guidelines provide the information required to analyze ABPM data from children and adolescents. 186186. Nobre F, Mion Jr. D, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 110(5Supl.1):1-29. BP categorization using ABPM data takes into account, in addition to BP readings, blood pressure load parameters, and BP dipping during nighttime sleep, as shown in Chart 12.7 . 713713. Guimarães IC, Almeida AM, Santos AS, Barbosa DB, Guimarães AC. Blood pressure: effect of body mass index and of waist circumference on adolescents. Arq Bras Cardiol. 2008;90(6):426-32.
12.8. Therapeutic Aspects
The primary objectives of treating HT during childhood and adolescence is preventing EOD and continued HT in adulthood. The plan depends on the etiology of HT, cardiovascular (CV) risk associated with other underlying diseases, and the presence of EOD (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
12.9. Nonpharmacological Therapy
Nonpharmacological therapy should be introduced to all pediatric patients with BP levels above the 90th percentile or BP < 130/80 (≥ 13 years old) (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. This includes weight loss, physical exercise, dietary intervention, and stress control. The combination of these four measures leverages their impact compared to the individual effect of each intervention. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
Weight loss provides good results, and the use of a motivational approach seems to be the most effective method for controlling the association between obesity and HT in childhood (LE: C). 717717. Hansen HS, Hyldebrandt N, Froberg K, Nielsen JR. Blood pressure and physical fitness in a population of children—the Odense Schoolchild Study. J Hum Hypertens. 1990;4(6):615-20. All children and adolescents should perform at least 300 minutes of moderate to vigorous physical activity per week for their health. In addition, sedentary behavior (time spent sitting or lying down) should be restricted for this age group. Structured physical exercise has greater impact on SBP values. 717717. Hansen HS, Hyldebrandt N, Froberg K, Nielsen JR. Blood pressure and physical fitness in a population of children—the Odense Schoolchild Study. J Hum Hypertens. 1990;4(6):615-20. It is recommended that they perform moderate-intensity aerobic exercises (30-60 minutes) at least three times a week, and daily if possible. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. Resistance training can be added to this regimen. Competitive sports are not recommended for patients with uncontrolled stage 2 HT (LE:C). 718718. McCambridge TM, Benjamin HJ, Brenner JS, Cappetta CT, Demorest RA, Gregory AJ, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension Pediatrics. 2010;125(6):1287-94.
Dietary interventions should include restricted sodium intake and may include potassium and calcium supplementation. Observational studies have shown the positive effects of the polyphenols found in olive oil. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,719719. Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M. Sodium intake and blood pressure in children with clinical conditions: A systematic review with meta-analysis. J Clin Hypertens (Greenwich). 2019 Jan;21(1):118-126. This guideline recommends the DASH diet, which emphasizes plant-based foods and decreased intake of sugar and sweets. This measure is especially effective for HT associated with obesity (LE: B). 719719. Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M. Sodium intake and blood pressure in children with clinical conditions: A systematic review with meta-analysis. J Clin Hypertens (Greenwich). 2019 Jan;21(1):118-126.
720. Bricarello P L, Poltronieri F, Fernandes R, Retondario A, Morais EBST, Vasconcelos FAG. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin Nutr ESPEN. 2018 Dec;28:1-11.-721721. Miller JZ, Wienberger MH, Christian JC. Blood pressure response to potassium supplement in normotensive adults and children. Hypertension. 1987;10(4):437-42. Stress control is also recommended for this age group, and may be achieved with various forms of meditation, mindfulness, and yoga (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
12.10. Pharmacological Therapy
Pharmacological therapy should be initiated for children with symptomatic HT, secondary to CKD or DM, presence of EOD, stage 2 HT with no apparent modifiable cause, and persistent HT nonresponsive to lifestyle changes (LSCs) (LE: B). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. The treatment target is to lower BP below the 90th percentile (LE: C). Treatment should begin with an antihypertensive agent at its lowest dose, increased every two to four weeks until the target level is achieved. If this regimen is not sufficiently effective, other medication classes are added in sequence. Since many medication classes increase sodium and fluid retention, considering thiazide diuretics is recommended as the second medication for combination therapies. Overall, adverse events associated with the use of antihypertensive agents in children and adolescents have been mild (LE: B). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,722722. Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580.
All classes of antihypertensive drugs seem safe, at least in the short run. 722722. Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580. However, recent international guidelines recommend preferential use of angiotensin-converting enzyme inhibitors (ACEIs), ARBs, long-acting CCBs, or thiazide DIUs as first-line medications. If a third antihypertensive is needed, the recommended medications are alpha-blockers, BBs, centrally acting sympatholytics, or potassium-sparing diuretics (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,722722. Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580.
In secondary HT, the choice of antihypertensive should follow the physiopathological principle involved, taking into account the comorbidities present in each case. 719719. Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M. Sodium intake and blood pressure in children with clinical conditions: A systematic review with meta-analysis. J Clin Hypertens (Greenwich). 2019 Jan;21(1):118-126.
720. Bricarello P L, Poltronieri F, Fernandes R, Retondario A, Morais EBST, Vasconcelos FAG. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin Nutr ESPEN. 2018 Dec;28:1-11.
721. Miller JZ, Wienberger MH, Christian JC. Blood pressure response to potassium supplement in normotensive adults and children. Hypertension. 1987;10(4):437-42.
722. Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580.
723. Prichard BN, Cruickshank JM, Graham BR. Beta-adrenergic blocking drugs in the treatment of hypertension. Blood Press. 2001;10(5-6):366-86.
724. Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD. Pregnancy outcome following exposure to angiotensin converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension. 2012;60(2):444-50.
725. Ferguson MA, Flynn JT. Rational use of antihypertensive medications in children. Pediatr Nephrol. 2014;29(6):979-88.-726726. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14(6):383-7. Patients with resistant HT require stronger decreases in sodium intake, as well as detailed investigation of their consumption of substances or foods causing HT, adherence to therapy regimen, and maximum optimization of said regimen (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
If the patient does not respond to monotherapy for longer than six months, their referral to a specialist in HT in children and adolescents should be considered (LE: C). 727727. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, et al; Hypertension Canada. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018 May;34(5):506-25. Chart 12.8 provides a list of medications used in pediatric settings and their dosage. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.,725725. Ferguson MA, Flynn JT. Rational use of antihypertensive medications in children. Pediatr Nephrol. 2014;29(6):979-88.,726726. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14(6):383-7.
12.11. Follow-up of Children and Adolescents with HT
Frequency of follow-up in children and adolescents with HT depends on severity and need for treatment. Patients undergoing nonpharmacalogical therapy only should have clinical follow-up visits every 3 to 6 months, with HBPM as an adjuvant for blood pressure control.
For patients requiring medications, soon after treatment onset, follow-up visits should be scheduled every 15 to 30 days after establishing the optimum dose or need for combination. In an intermediate stage, visits should be scheduled every 4 to 6 weeks, and quarterly once HT is controlled.
Follow-up appointments should included a detailed analysis of adherence and side effects. Requesting laboratory tests depends on the medications used and severity of HT and underlying diseases; likewise, how frequently the patient is tested for EOD depends on the underlying disease and on the severity of HT. Requesting ABPM is indicated when there is no HT control or when there is risk of masked hypertension (MH), such as the late post-operative period after surgical correction for coarctation of the aorta (LE: C). 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
12.12. Hypertensive Crisis
Hypertensive emergencies (HEs) and hypertensive urgencies (HUs) are defined in Chapter 13. 727727. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, et al; Hypertension Canada. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018 May;34(5):506-25. There is no consensus BP level that defines HE, 728728. . 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887-920. though some authors suggest a cutoff point 20% above stage 2 HT (> 99th percentile). 729729. Wu HP, Yang WC, Wu YK, Zhao L, Chen CY, Fu YC. Clinical significance of blood pressure ratios in hypertensive crisis in children. Arch Dis Child. 2012; 97(3):200–5. The American Academy of Pediatrics (AAP), in turn, defines HE as any condition in which a child has BP above stage 2 HT. However, the AAP warns that children with BP > 95th percentile + 30 mm Hg run a higher risk of complications. In general, HEs are secondary to underlying diseases still requiring investigation, 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. and most often should be treated with intravenous (IV) medication administered to hospitalized patients, often in the ICU. Patients with HUs and no signs of end-organ impairment may initially receive central alpha-agonists, vasodilators or CCBs. 705705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904. The objective of treatment is to lower BP by 25% during the first 8 hours, followed by a slow decrease over 24 to 48 hours, until reaching the 95th percentile, since accelerated decreases may cause damage, especially to the brain. 730730. Chandar J, Zilleruelo G. Hypertensive crisis in children. Pediatr Nephrol. 2012: 27(5):741-51.,731731. Yang WC, Zhao LL, Chen CY, Wu YK, Chang YJ, Wu HP. First-attack pediatric hypertensive crisis presenting to the pediatric emergency department. BMC Pediatrics. 2012; 12:200. Chart 12.9 shows the most frequently used medications in pediatric HEs (LE: C).13. Crise Hipertensiva
| Key Takeaways |
|---|
| All children and adolescents ≥ 3 years old should have their BP measured annually. |
| Children 3 < years old should undergo BP measurements in case of preterm birth, very low birth weight, intrauterine growth restriction, history of stay at neonatal ICU, congenital heart disease, nephropathy, solid organ transplantation, oncological disorders, chronic use of medications known to increase BP, system disorders associated with HT, and evidence of intracranial hypertension. |
| All children and adolescents ≥ 3 years old should have their BP measured at every medical visit in case of overweight, chronic use of medications known to increase BP, kidney disease, coarctation of the aorta, and diabetes. |
| Children and adolescents should be diagnosed with HT when BP measured by auscultation in three separate visits is above the 95th percentile for their age, sex, and height percentile. |
| In children and adolescents diagnosed with HT, the pharmacological and nonpharmacological treatment goals should be to lower BP to below the 90th percentile for age, sex, and height percentile and to < 130/80 mm Hg in adolescents ≥ 13 years old. |
13. Hypertensive Crisis
13.1. Definition
The terms hypertensive urgency and hypertensive emergency were proposed as an operational classification of hypertensive crises (HCs) in 1993 by the V Joint National Committee on Detection Evaluation and Treatment of High Blood Pressure. 732732. . The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153(2):154-83.
Hypertensive urgencies (HUs) are symptomatic clinical situations in which there is significant blood pressure (BP) elevation (arbitrarily defined as systolic BP (SBP) DBP ≥ 180 mm Hg and/or diastolic BP (DBP) ≥ 120 mm Hg) without acute and progressive end-organ damage (EOD) and no imminent risk of death. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,733733. Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9.,734734. Martin JFV, Ribeiro JM. Urgências e Emergências Hipertensivas. In: Moreira MC, Montenegro ST, Paola AAV, eds. Livro Texto da Sociedade Brazileira de Cardiologia. 2 ed. Barueri (SP): Manole; 2015. P.922-30.
Hypertensive emergencies (HEs), in turn, are symptomatic clinical situations in which there is significant BP elevation (arbitrarily defined as SBP ≥ 180 mm Hg and/or DBP ≥ 120 mm Hg) with acute and progressive EOD and imminent risk of death. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,733733. Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9.,734734. Martin JFV, Ribeiro JM. Urgências e Emergências Hipertensivas. In: Moreira MC, Montenegro ST, Paola AAV, eds. Livro Texto da Sociedade Brazileira de Cardiologia. 2 ed. Barueri (SP): Manole; 2015. P.922-30.
A common condition at emergency rooms is the hypertensive pseudocrisis (HTPC). In HTPCs, there is no acute EOD or immediate risk of death. In general, it is seen in uncontrolled hypertensive patients undergoing treatment, or in untreated hypertensive patients, with very high BP measurements, but who are either olygosymptomatic or asymptomatic. High BP after an emotional, painful or uncomfortable event, such as migraines, dizziness, vascular and musculoskeletal headaches and panic attacks also characterize HTPC. 733733. Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9.,734734. Martin JFV, Ribeiro JM. Urgências e Emergências Hipertensivas. In: Moreira MC, Montenegro ST, Paola AAV, eds. Livro Texto da Sociedade Brazileira de Cardiologia. 2 ed. Barueri (SP): Manole; 2015. P.922-30.
13.2. Classification
HE is not defined by BP level, though it is often very high, but predominantly by the patient's clinical status. It can manifest as a cardiovascular, cerebrovascular, renal, or multi-organ event, or even as pre-eclampsia with severe features or eclampsia. Chart 13.1 shows the classification of HEs. Chart 13.2 differentiates HUs from HEs in terms of diagnosis, prognosis, and management.
13.3. Major Epidemiological, Pathophysiological, and Prognostic Aspects
13.3.1. Epidemiology
Hypertensive crises account for 0.45 to 0.59% of all hospital emergency treatments, while HEs account for 25% of all cases of HC. Ischemic stroke and acute pulmonary edema (APE) are the most common conditions found in HEs 735735. Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83(2):131-6; 125-30.
736. Pinna G, Pascale C, Fornengo P, Arras S, Piras C, Panzarasa P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS One. 2014;9(4):e93542.-737737. Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo AN, Yugar-Toledo JC. Hypertensive crisis: clinical-epidemiological profile. Hypertens Res. 2011;34(3):367-71. , with decreasing incidence in recent decades. 738738. Pierin AMG, Flórido CF, Santos JD. Hypertensive crisis: clinical characteristics of patients with hypertensive urgency, emergency and pseudocrisis at a public emergency department. Einstein (Sao Paulo). 2019;17(4):eAO4685.
739. Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci.1974;268(6):336–45.-740740. Velasco I, Cuadrado L, Fontana A, Reijaili WA, Balbi AL, Barretti P, Franco RJS. Cuadro clínico y evolución de 77 pacientes con hipertensión arterial maligna: comparación de dos épocas y de diferentes niveles de creatinina. Nefrologia. 1993;13 (Suppl 5):8-13.
13.3.2. Pathophysiology
Since systemic BP is the product of cardiac output (CO) by peripheral vascular resistance (PVR), acute increases in BP may be the result of changes to those variables. Therefore, increased intravascular volume and PVR, reduced production of endogenous vasodilators, and/or activation of vasoconstrictor systems may precipitate greater vascular reactivity, resulting in HC. 741741. Almeida FA, Stella RC, Voos A, Ajzen H, Ribeiro AB. Malignant hypertension: a syndrome associated with low plasma kininogen and kinin potentiating factor. Hypertension. 1981;3(6 Pt 2):II-46-9.,742742. Ault MJ, Ellrodt AG. Pathophysiologic events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10–5. Tissue autoregulation is compromised, particularly in the cerebral and renal vascular beds, resulting in local ischemia, which triggers a vicious circle of vasoconstriction, endothelial damage and activation of the platelet, coagulation and immune system, with myointimal proliferation, arteriole fibrinoid necrosis, and end-organ ischemia. 741741. Almeida FA, Stella RC, Voos A, Ajzen H, Ribeiro AB. Malignant hypertension: a syndrome associated with low plasma kininogen and kinin potentiating factor. Hypertension. 1981;3(6 Pt 2):II-46-9.
742. Ault MJ, Ellrodt AG. Pathophysiologic events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10–5.-743743. Strandgaard S, Paulson O. Cerebral autoregulation. Stroke. 1984;15(3):413–6. The autoregulation curve shifts to the right in chronic hypertensive patients, making both actual BP level and rate of increase important to the genesis of HE. On the other hand, that shift in the autoregulation curve predisposes patients to tissue ischemia in aggressive BP reductions in HE treatment. 742742. Ault MJ, Ellrodt AG. Pathophysiologic events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10–5.,743743. Strandgaard S, Paulson O. Cerebral autoregulation. Stroke. 1984;15(3):413–6.
13.3.3. Prognosis
The one-year mortality rate for untreated HE is approximately 80%, 739739. Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci.1974;268(6):336–45. and effective antihypertensive treatment is associated with significant improvements in prognosis. 740740. Velasco I, Cuadrado L, Fontana A, Reijaili WA, Balbi AL, Barretti P, Franco RJS. Cuadro clínico y evolución de 77 pacientes con hipertensión arterial maligna: comparación de dos épocas y de diferentes niveles de creatinina. Nefrologia. 1993;13 (Suppl 5):8-13. Five-year survival rates are higher for individuals with HU than those with HE. 735735. Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83(2):131-6; 125-30.,744744. Martin JFV, Kuniyoshi CH, Andrade LG, Yugar-Toledo JC, Loureiro AC, Cipullo JP. Fatores Preditores de Mortalidade em Pacientes com Crise Hipertensiva. Arq Bras Cardiol. 2007;89(Supl 1): 201.
13.4. Complementary Clinical and Laboratory Investigation 164,733,734
Taking a clinical history directed to the potential cause of the disease is critical. Clinical and laboratory investigation and requesting tests should provide for the proper assessment of BP and the presence of acute EOD. Initially, BP should be measured in both arms, preferably in a calm environment, and repeatedly until stabilization (minimum of three measurements). Data on the patient’s typical BP should be rapidly collected, as well as information on situations that can trigger BP increases and comorbidities; the use or discontinuation of antihypertensive medications (particularly adrenergic antagonists); or the use of substances that can increase BP (see Chapter 15). A systematic approach, including an assessment of signs and symptoms, physical examination and complementary investigation, helps determine the presence of acute and progressive EOD, as shown in Chart 13.3 :
13.5. General Treatment of Hypertensive Crisis
Treatment of HU ( Figure 13.1 ) should begin after a period of clinical observation in a calm environment, which helps rule out cases of pseudocrisis (treated only with rest or the use of painkillers or tranquilizers). Captopril and clonidine are indicated for acute treatment. Captopril, at a dose of 25-50mg, has peak action within 60 to 90 minutes, while clonidine is fast-acting, working in approximately 30 to 60 minutes, at a dose of 0.100 to 0.200mg. The use of immediate-release nifedipine capsules to treat HU should be banned, because it is neither safe nor effective, and causes rapid and marked BP reductions, which can result in tissue ischemia. 745745. Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996; 276(16):1328-31.,746746. CREMESP elabora parecer sobre uso de nifedipina. 2004. [citado 2020 Jul 15]. Disponível em: https://www.cremesp.org.br/?siteAcao=Jornal&id=323 .
https://www.cremesp.org.br/?siteAcao=Jor...
There is no evidence from randomized controlled trials showing antihypertensives reduce morbidity and mortality for individuals with HE. However, based on clinical experience and the progress of patients under treatment, antihypertensive treatment is beneficial and cuts mortality. The treatment of patients with HE is aimed at rapid BP reduction to prevent the progression of EOD. Individuals should be preferentially admitted to the ICU, treated with intravenous (IV) antihypertensives, and carefully monitored during treatment to prevent hypotension. The general recommendations for BP reduction for HE are (LR: I; LE: C): 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
-
• Mean BP ≤ 25% in the 1st hour;
-
• BP 160/100-110 mm Hg in 2 to 6 h;
-
• BP 135/85 mm Hg in 24-48 hours.
However, HEs should be approached considering the impaired system or end-organ.
13.6. Hypertensive Emergencies in Special Situations
Chart 13.4 shows the medications indicated for the main forms of HE.
13.6.1. Hypertensive Encephalopathy 747,748
Hypertensive encephalopathy is a neurological HE characterized by signs and/or symptoms of cerebral edema secondary to sudden and/or sustained BP elevation. In general, it is found in chronic hypertensive patients who develop accelerated/malignant hypertension or in previously normotensive individuals with sudden increases in BP progressing to the failure of cerebral perfusion autoregulation mechanisms. It is also characterized by insidious onset and progresses with headaches, nausea, or vomiting. There may be changes to the visual field, photopsia, blurred vision, visual hallucinations, confusion, coma, generalized convulsive crises, and hyperreflexia. Treatment consists of slowly lowering BP, since rapid and intense decreases may cause cerebral hypoperfusion and loss of cerebral autoregulation mechanism. Sodium nitroprusside (SNP) is recommended in Brazil. In other countries, the following medications are available: nicardipine, clevidipine, labetalol, and fenoldopam. In the first 24 to 48 h, oral antihypertensives should be administered to better control BP.
13.7. Stroke
Hypertension is the primary risk factor for strokes, especially hemorrhagic strokes. 749749. O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–75. Diagnosis is based on a full neurological examination; for severity assessment purposes, use the National Institute of Health Stroke Scale (NIHSS). Head CTs and MNRs enable physicians to define the type of stroke (ischemic stroke in 85% of cases, hemorrhagic stroke in 15% of cases) and the area involved. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,750750. Truelsen T, Heuschmann PU, Bonita R, Arjundas G, Dalal P, Damasceno A, et al. Standard method for developing stroke registers in low-income and middle-income countries: experiences from a feasibility study of a stepwise approach to stroke surveillance (STEPS Stroke). Lancet Neurol. 2007;6(2):134-9. For incipient infarctions, an MNR is more sensitive than a CT.
13.7.1. Ischemic Stroke
BP often decreases spontaneously within 90 to 120 minutes during the acute phase. The recommendations are as follows:
-
1. In case of ischemic stroke with indication for thombolysis, BP reduction < 185/110 mm Hg before fibrinolytic therapy is recommended (LR: I; LE: B). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110. If BP remains > 185/110 mm Hg, thrombolytic therapy should not be administered. That recommendation also applies to individuals who are to undergo thrombectomy. 751751. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306. BP should be maintained < 180/105 mm Hg in the first 24 hours after thrombolysis.
-
2. An initial 15% decrease in BP can be applied in cases of very high BP (≥ 220/120 mm Hg) and other associated HEs (aortic dissection, acute coronary events, eclampsia, post-thrombolysis, and/or APE) (LR: I; LE: C). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
-
3. In patients with BP ≥ 220/120 mm Hg that have not received thrombolytics and do not present with other HE requiring antihypertensive treatment, the benefit of starting or restarting treatment for hypertension in the first 48 to 72 h is unclear. It seems prudent to reduce BP by 15% during the first 24 h after the beginning of the ischemic stroke (LR: IIb; LE: C). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
-
4. Starting or restarting antihypertensive therapy during hospitalization for neurologically stable patients with BP ≥ 140/90 mm Hg is safe for improving long-term BP control (LE: B; LR: IIa). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
-
5. In other cases of ischemic stroke, reducing BP within 5 to 7 days of the event has controversial neurological effects requiring treatments be tailored for individual patients (LR: I; LE: A). 652652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
13.7.2. Hemorrhagic Stroke
Elevated BP increases the risk of hematoma expansion and death, in addition to worsening the prognosis for neurological recovery. However, there is no conclusive evidence in favor of rapid reductions of BP. Cerebral edema occurs in 30% of cases, usually during the first 24 hours. In those cases, decompressive craniectomy should be performed and patients transferred to specialized centers (LR: I; LE: B). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,752752. Hemphill, J.C., 3rd, et al., Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2015. 46(7): 2032-60.
For individuals with acute presentation (< 6 h from onset of hemorrhagic stroke):
-
1. SBP > 220 mm Hg – consider BP reduction with continuous IV infusion and frequent BP monitoring (LR: IIa; LE: C). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,752752. Hemphill, J.C., 3rd, et al., Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2015. 46(7): 2032-60.
-
2. SBP from 150 to 220 mm Hg – lowering BP below 140 mm Hg provides no benefits in terms of lower mortality or severe impairment and is potentially dangerous (LR: III; LE: A). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,752752. Hemphill, J.C., 3rd, et al., Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2015. 46(7): 2032-60. Consider a target SBP < 180 mm Hg. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
13.7.3. Acute Coronary Syndromes
Coronary syndromes can be accompanied by BP elevation due to a reflex triggered by the ischemic myocardium. Consequently, higher PVR increases myocardial oxygen demand. The goal is to reduce the afterload without increasing the heart rate or reducing preload too much, since it would lead to increased myocardial oxygen consumption. The goal should be SBP < 140 mm Hg (avoid < 120 mm Hg) and DBP between 70 and 80 mm Hg using esmolol, metoprolol, or nitroglycerin (LR: I; LE: A). Intravenous nitrates reduce PVR, improve coronary perfusion, and have an important systemic vasodilator effect, reducing preload and myocardial oxygen consumption. Hydralazine, SNP, and nifedipine use is contraindicated, since it may promote flow steal. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,733733. Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9. The recommendations are:
-
a) Intravenous nitroglycerin (NTG) is indicated in the first 48 hours for treatment of hypertension, persistent ischemia3 and HF, as long as hypotension, right ventricular infarction, or use of phosphodiesterase type 5 inhibitors have not been present in the previous 48 h (LR: I; LE: B). NTG use should not exclude other interventions that have proven to reduce mortality, such as beta-blockers (BBs) or ACEIs. 753753. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2): 119–77.,754754. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association for Clinical Chemistry. 2014 AHA/ACC Guideline for the management of patients with non–ST-elevation acute coronary syndromes. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-228.
-
b) The use of IV BBs is indicated for hypertensive individuals who do not present with: 1) signs of HF; 2) clinical evidence of low CO; 3) increased risk for cardiogenic shock; or 4) other contraindications for beta blockade (LR: IIa, LE: B). 753753. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2): 119–77.,756756. Kumar R, Gandhi SK, Little WC. Acute heart failure with preserved systolic function. Crit Care Med. 2008;36(1 Suppl):pS52-6.
13.7.4. Acute Pulmonary Edema (APE)
Approximately one third of the patients admitted with APE and HE have preserved left ventricular function, and myocardial ischemia may also be involved in the pathophysiology of APE associated with HE. 755755. Gandhi SK, Powers JC, Nomeir AM, Fowle K, Kitzman DW, Rankin KM, et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med. 2001;344(1):17-22.,756756. Kumar R, Gandhi SK, Little WC. Acute heart failure with preserved systolic function. Crit Care Med. 2008;36(1 Suppl):pS52-6. HE with APE should be controlled primarily in an ICU setting, with IV medication, monitoring, and gradual BP reduction. NTG and SNP are used to lower preload and afterload. Loop diuretic use also lower volume overload and, consequently, BP. In some cases, the use of noninvasive continuous positive airway pressure may be indicated for decreasing pulmonary edema and venous return.747,748,757
13.7.4.1. Acute Aortic Dissection
In patients with precordial pain and high BP, acute aortic dissection should always be considered. The progression of dissection is related to BP level and ventricular ejection velocity. 758758. Bossone E, La Bounty TM, Eagle KA. Acute aortic syndromes: Diagnosis and management, an update. Eur Heart J. 2018;39(9):739−49. Achieving proper pain management (IV opiates for analgesia), HR < 60 bpm, and SBP between 100 and 120mm Hg are important (LR: I; LE: B). 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,747747. Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.,758758. Bossone E, La Bounty TM, Eagle KA. Acute aortic syndromes: Diagnosis and management, an update. Eur Heart J. 2018;39(9):739−49. SBP < 120 mm Hg should be achieved in 20 minutes. The use of SNP in isolation is not ideal, since it increases HR and aortic ejection velocity, potentially worsening the dissection. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,747747. Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.,758758. Bossone E, La Bounty TM, Eagle KA. Acute aortic syndromes: Diagnosis and management, an update. Eur Heart J. 2018;39(9):739−49. Thus, SNP should be associated with a BBs, initially IV, short, and titrable (metoprolol, labetalol, or esmolol), to decrease the heart rate. Alternately for asthma patients, nondihydropyridine calcium channel blockers (CCBs) may be used.
13.7.5. Pre-eclampsia/Eclampsia (see Chapter 11)
13.7.6. HE from Illicit Drug Use
Illicit substances that increase BP are sympathomimetics, potentiating the effect of catecholamines, including amphetamines and ecstasy, their illegal derivative, in addition to powder cocaine and smokable crack cocaine. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,759759. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Dis. 2003;5(4):253-71.,760760. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201. Amphetamine use causes a dose-dependent increase in BP, 761761. Lester SJ, Baggott M, Welm S, et al. Cardiovascular effects of 3, 4-methylenedioxy-methamphetamine. A double-blind, placebo-controlled trial. Ann Intern Med. 2000;133(12):969–73. leading to tachycardia tachycardia, palpitations, sweating, and arrhythmias, while ecstasy has other effects in addition to HR and BP increases (serotoninergic syndrome). 762762. Gahlinger PM. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004;69(11):2619-27.
Intranasal cocaine use leads to a sudden and dangerous increases in BP levels within 15 minutes of use. In case of preexisting hypertension, higher BP elevations may occur. 763763. Lange RA, Ciggarroa RG, Flores ED, McBride W, Kim AS, Wells PJ, et al. Potentiation of cocaine induced coronary vasoconstriction by beta adrenergic blockade. Ann Intern Med. 1990;112(12):897–903. Cocaine-induced vasoconstriction depends on the central sympathetic discharge, which s suppressed by the intact baroreceptor function. When the baroreflex tamponade is impaired, the result is adrenergic vasoconstriction and HC. 764764. Tuncel M, Wang Z, Arbique D, Fadel PJ, Victor RG, Vongpatanasin W. Mechanism of the blood pressure-raising effect of cocaine in humans. Circulation. 2002;105(9):1054-9.
In lighter cases, benzodiazepines and sublingual NTG may be administered. In more severe cases, IV therapy will probably be required, the agents of choice are NTG, SNP, or phentolamine. 759759. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Dis. 2003;5(4):253-71.,760760. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201. It is important to avoid BBs, since they may lead to alpha-adrenergic receptor stimulation in the presence of beta blockade, thus causing a coronary spasm. 763763. Lange RA, Ciggarroa RG, Flores ED, McBride W, Kim AS, Wells PJ, et al. Potentiation of cocaine induced coronary vasoconstriction by beta adrenergic blockade. Ann Intern Med. 1990;112(12):897–903. An exception might be carvedilol, which is capable of mitigating HR and BP increases induced by smoking crack cocaine. 765765. Sofuoglu M, Brown S, Babb DA, Pentel PR, Hatsukami DK. Carvedilol affects the physiological and behavioral response to smoked cocaine in humans. Drug Alcohol Depend. 2000; 60(1):69-76. CCBs may also be used in cases of cocaine-induced AMI, where the assumed cause is coronary vasoconstriction. 760760. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201.
A complicating factor of those intoxications, whether they are HUs or HEs, is the concomitant ingestion of high doses of caffeine (present in energy drinks), nicotine, or alcohol, which increase plasma NE levels. 766766. Sordo L, Indave BI, Barrio G, Degenhardt L, de la Fuente L, Bravo MJ. Cocaine use and risk of stroke: a systematic review. Drug Alcohol Depend. 2014;142:1-13. In particular, alcohol and cocaine use in combination has a greater toxic effect than the use of either alone, 767767. Wilson LD, Jeromin J, Garvey L, Dorbandt A. Cocaine, ethanol, and cocaethylene cardiotoxicity in an animal model of cocaine and ethanol abuse. Acad Emerg Med. 2001;8(3):211–22.,768768. Mehta MC, Jain AC, Billie M. Effects of cocaine and alcohol alone and in combination on cardiovascular performance in dogs. Am J Med Sci. 2002;324(2):76–83. increasing the risk of sudden death 18- to 25-fold 769769. Wilkerson RD. Cardiovascular effects of cocaine: enhancement by yohimbine and atropine. J Pharmacol Exp Ther. 1989;248(1):57–61. due to increased bioavailability of cocaine. 770770. Perez-Reyes M, Jeffcoat AR. Ethanol/cocaine interactions: cocaine and cocaethylene plasma concentrations and their relationship to subjective and cardiovascular effects. Life Sci. 1992;51(8):553–63. Treatment includes the use of BBs, alpha-blockers, and CCBs, the latter administered before or after cocaine intake. 760760. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201.,771771. Melchert RB, Eselin JA, O’Dell JF, Welder AA. Effects of nitrendipine on cocaine induced toxicity evaluated in primary myocardial cell cultures. J Pharmaceut Sci. 1991;80(7):700–4.
13.7.7. Accelerated/Malignant Hypertension
Malignant hypertension is characterized by the presence of severe general hypertension, retinopathy with papilledema, with or without renal and/or heart failure, fibrinoid necrosis of renal arterioles, and endarteritis obliterans, and may present with rapidly progressive and fatal clinical evolution. Elevated BP in the presence of retinal hemorrhages and exudates in the funds, but in the absence of papilledema, is known as accelerated hypertension. Currently, the terms “malignant” and “accelerated” are considered interchangeable, with “accelerated/malignant hypertension” used more often to define this form of HE, which, though less frequent, represents a devastating form of acute BP elevation. 747747. Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.,772772. Bortolotto LA. Hipertensão acelerada-maligna. Rev Bras Hipertens. 2014;21(4):203-8.,773773. Ahmed ME, Walker JM, Beevers DG, Beevers M. Lack of difference between malignant and accelerated hypertension. Br Med J (Clin Res Ed). 1986;292(6515):235-7. The prognosis is almost always fatal if not properly recognized and left untreated, with two-year mortality rates of approximately 80%, primarily due to HF and CKD. 774774. Kincaid-Smith P, McMichael J, Murphy EA. The clinical course and pathology of hypertension with papilloedema (malignant hypertension). Q J Med. 1958;27(105):117-53.,775775. Clough C, Beevers D, Beevers M. The survival of malignant hypertension in blacks, whites and Asians in Britain. J Hum Hypertens. 1990;4(2):94-6. Effective treatment of malignant hypertension has significantly improved survival, but it is still accompanied by a high rate of complications. 776776. Lip G, Beevers M, Beevers D. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens. 1995;13(8):915-24. The most rational way to manage is to prevent it by treating hypertension early and effectively. Individuals with severe hypertension who present with major LVH and renal failure should be treated as prior accelerated/malignant hypertension patients.
Patients should undergo intensive BP control using immediate-action vasodilator medications, such as SNP, which promotes fast BP control and makes individuals more responsive to classic antihypertensive therapeutics. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,732732. . The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153(2):154-83. During acute control, oral antihypertensives should be administered, including diuretics, renin-angiotensin system blockers, BBs, direct-acting vasodilators (hydralazine), central adrenergic agonists (clonidine and methyldopa), and CCBs, when multiple medications are required. 747747. Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.,774774. Kincaid-Smith P, McMichael J, Murphy EA. The clinical course and pathology of hypertension with papilloedema (malignant hypertension). Q J Med. 1958;27(105):117-53. BB use is indicated for cases of pulmonary congestion caused by diastolic dysfunction due to severe LVH. BP reductions should be gradual, keeping DBP levels above 100 mm Hg during the first few days of treatment. There may be an initial impairment in kidney function with high creatinine levels since the mechanism of autoregulation of renal flow is shifted to much higher levels than those found in mild hypertensive patients and normotensive individuals. Therefore, an adjustment period is required before returns to baseline levels. Sometimes, dialysis treatment may be required during the most acute stage. Antihypertensive treatment for this condition has had a significant impact on survival (LR: IIa; LE: B).
13.7.8. Hypertension with Multi-Organ Damage
Hypertension with multi-organ damage (MOD) is defined by the concurrent involvement of three of the four systems listed below: 777777. Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, et al. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30(8):463-6.
-
• Renal (rapid decline of kidney function or proteinuria);
-
• Cardiac (major LVH or systolic dysfunction, or ventricular repolarization abnormalities, or increased troponin);
-
• Neurological (stroke or hypertensive encephalopathy);
-
• Hematological (microangiopathic hemolysis).
The definition of MOD hypertension (in the presence of multi-organ impairment) does not require the presence of Keith-Wagener Grade III or IV changes, which may be found at a later stage. 778778. Ma H, Jiang M, Fu Z, Wang Z, Shen P, Shi H, et al. Clinical value of multiorgan damage in hypertensive crises: A prospective follow-up study. J Clin Hypertens. (Greenwich). 2020;22(5):914-23.,779779. Lip GY, Beevers M, Dodson PM, Beevers DG. Severe hypertension with lone bilateral papilloedema: a variant of malignant hypertension. Blood Press. 1995;4(6):339-42. When comparing MOD hypertension to accelerated/malignant hypertension, the two are found to have analogous pathogeny, clinical significance, and prognosis, implying similar clinical management (LR: IIa; LE: B). 777777. Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, et al. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30(8):463-6.,780780. Amraoui F, van Montfrans GA, van den Born BJ. Value of retinal examination in hypertensive encephalopathy. J Hum Hypertens. 2010;24(4):274-9.
| Key Takeaways |
|---|
| Hypertensive crisis: acute elevation of systolic blood pressure (BP) ≥ 180 mm Hg and/or diastolic BP ≥120 mm Hg, which may or may not result in end-organ damage (EOD), divided into hypertensive urgencies (BP increase without EOD and no imminent risk of death, allowing for BP reduction within 24 to 48 h) and hypertensive emergencies (BP increase with acute EOD or in progress and immediate risk of death, requiring rapid and gradual BP decrease within minutes to hours using intravenous medication). |
| Hypertensive emergencies may manifest as a cardiovascular, cerebrovascular, renal or multi-organ event, or even as pre-eclampsia with severe features or eclampsia. |
| High BP without acute and progressive EOD rules out HE. |
| Uncontrolled hypertension from low adherence, difficult-to-control hypertensive pseudocrises, hypertensive urgencies, and hypertensive pseudocrises are common situations of high BP without acute or progressive EOD. |
| The severity of the clinical condition is not determined by absolute BP levels, but rather by the magnitude and timing of the increase. Numerical values act as a parameter, but should not be applied as absolute diagnostic criteria. |
14. Hypertension in Older Adults
14.1. Introduction
The United Nations (UN) and the World Health Organization (WHO) consider as older adults all individuals age 60 and older. In high-income countries, where life expectancies are greater, the threshold has been raised to 65. 781781. World Health Organization. (WHO). World Report on Ageing and Health 2015. [Cited in 2020 Feb 10]. Available from: http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 .
http://apps.who.int/iris/bitstream/10665...
A special age group known as the “oldest old,” consisting of individuals ages 80 or older, represents the fastest-growing segment of the population. 782782. United Nations. Department of Economic and Social Affairs Population Division. World Population Ageing 2015. [Cited in 2019 Feb 10] Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf .
http://www.un.org/en/development/desa/po...
The prevalence of multimorbidity increases with age, and over two thirds of the oldest old suffer from two or more chronic illnesses. 783783. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity andimplications for health care, research, and medical education: a cross-sectional study. The Lancet. 2012; 380 (9836): 37-43.,784784. Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing 2017; 46 (6): 882–8. Based on a country-level study of the older adult population (ELSI-Brazil), over 60% of older adults suffered from multiple chronic illnesses, and hypertension (HT) was the second most prevalent, second only to chronic back pain. 785785. Nunes BP, Batista SRR, Andrade FB, Souza Junior PRB, Lima-Costa MF, Facchini LA. Multimorbidity: The Brazilian Longitudinal Study of Aging (ELSI-Brazil). Rev Saude Publica. 2018;52(Suppl 2):10s. These patients usually take multiple medications with hard-to-manage therapy regimens that increase their cost and the risk of drug interactions.
There is a direct and linear relationship between blood pressure (BP) and age, with the prevalence of HT going from approximately 7% in individuals ages 18 to 39 to over 60% in those 65 and older. The Framingham has shown that nearly two thirds of men and three fourths of women have HT at age 70. 786786. Peters R, Beckett N, McCormack T, Fagard R, Fletcher A, Bulpitt C. Treating hypertension in the very elderly—benefits, risks, and future directions, a focus on the hypertension in the very elderly trial. Eur Heart J. 2014; 35 (26):1712-8.,787787. Iadecola C. Hypertension and Dementia. Hypertension. 2014; 64 (1): 3-5.
Though epidemiological studies have suggested greater survival rates for individuals age 80 and older with high levels of BP, this may in part be caused by the fact that people with low BP have higher rates of multimorbidity and frailty, and therefore lower probability of survival. In the geriatric population, HT is the primary modifiable risk factor (RF) for cardiovascular morbidity and mortality, 786786. Peters R, Beckett N, McCormack T, Fagard R, Fletcher A, Bulpitt C. Treating hypertension in the very elderly—benefits, risks, and future directions, a focus on the hypertension in the very elderly trial. Eur Heart J. 2014; 35 (26):1712-8. even at more advanced ages. It is critical that we stress that HT is a modifiable RF for cognitive decline, dementia and disability. 787787. Iadecola C. Hypertension and Dementia. Hypertension. 2014; 64 (1): 3-5.,788788. Costa Filho AM, Mambrini JVM, Malta DC, Lima-Costa MF, Peixoto SV. Contribution of chronic diseases to the prevalence of disability in basic and instrumental activities of daily living in elderly Brazilians: the National Health Survey (2013). Cad. Saúde Pública (Online) 2018; 34(1):e00204016.
In assessing mean survival rates for older adults, one should not use life expectancy at birth, but rather life expectancy “at life.” Therefore, life expectancy at age 80, in 2018, was 10.4 years for women and 8.6 years for men, more than enough time to enjoy the benefits of treatment for HT.
14.2. Physiopathological Mechanisms
Diastolic blood pressure (DBP) increases until approximately age 50, stabilizes from 50 to 60 and then decreases, while systolic blood pressure (SBP) tends to increase throughout the lifespan. Therefore, pulse pressure (PP = SBP – DBP), a useful hemodynamic index of arterial stiffness, increases with age. These changes are consistent with the idea that, for younger individuals, BP is largely determined by peripheral vascular resistance (PVR), while for older adults it is determined by central arterial stiffness. 789789. Kelly R, Hayward C, Avolio A, O’Rourke M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation 1989; 80 (6): 1652–9.
790. Franklin SS, Gustin Wt, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308-15.-791791. Pearson JD, Morrell CH, Brant LJ, Landis PK, Fleg JL. Age-associated changes in blood pressure in a longitudinal study of healthy men and women. J Gerontol A Biol Sci Med Sci. 1997;52(3):M177-83.
The arterial wall thickening and endothelial dysfunction observed during the aging process are accompanied by increased stiffness and lower vascular compliance, attributed to a wide range of factors, such as salt sensitivity, chronic hemodynamic stress, and elastin fiber fragmentation and misalignment, with replacement by collagen fibers, facilitating the deposition of calcium ions. 792792. Lakatta EG. Central arterial aging and the epidemic of systolic hypertension and atherosclerosis. J Am Soc Hypertens. 2007;1(5):302-40.
Aortic stiffening caused by vascular aging accelerates pulse wave velocity (PWV) towards peripheral circulation (centrifugal) and reflected waves returning to the heart (centripetal). The overlap of those two waves during the proto-mesosystolic phase leads to the increases in SBP and wider PP seen in older adults. 793793. O’Rourke MF, Nichols WW. Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension. 2005;45(4):652-8.
Currently, carotid-femoral PWV measurement is considered the gold standard to assess central arterial stiffness. In the absence of comorbidities, older adults with velocities under 7.6 m/s are considered to have good vascular health and, in an isolated sample, represent fewer than 4% of individuals age 60 and older. 794794. Niiranen TJ, Lyass A, Larson MG, Hamburg NM, Benjamin EJ, Mitchell GF, et al. Prevalence, Correlates, and Prognosis of Healthy Vascular Aging in a Western Community-Dwelling Cohort: The Framingham Heart Study. Hypertension. 2017;70(2):267-74.,795795. Freitas EGB, Souza DF, Ferreira-Filho SR. Probability of At Least One High Arterial Blood Pressure Measurement in Elderly Patients with Healthy Vascular Aging in Two Years of Follow-Up. Kidney Blood Press Res. 2018;43(6):1765-71. In a given urban region of Brazil, PWV values found in older adults, adjusted for BP, age and gender, averaged 9.1 m/s for normotensive individuals and 9.4 m/s for uncontrolled hypertensives. 796796. de Mendonca GS, de Souza DF, de Alvarenga Cunha Brunelli AC, de Oliveira Peres CI, Freitas EGB, Lacerda GN, et al. Arterial stiffness in elderly patients with normotension and hypertension in Brazil. J Clin Hypertens (Greenwich). 2018;20(9):1285-93. On the other hand, for many older adults, PP amplification may be a better predictor of events and mortality than PWV. 797797. Benetos A, Gautier S, Labat C, et al. Mortality and Cardiovascular Events Are Best Predicted by Low Central/Peripheral Pulse Pressure Amplification But Not by High Blood Pressure Levels in Elderly Nursing Home Subjects: the PARTAGE (Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Population) study. J Am Coll Cardiol. 2012;60 (16):1503-11.
14.3. Diagnosis and Therapeutic Decision
The presence of multiple comorbidities and polypharmacy may make investigating HT in older adults more difficult. Chapter 3 guidelines on BP measurement and physical and laboratory examinations should also be followed for this age group. However, the investigation of secondary causes of HT should proceed carefully and consider the risks and benefits for each procedure (see Chapter 15). 798798. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.
The clinical assessment of older patients, especially the oldest old, is different from traditional assessments. First, physicians should recognize that the appointment will require more time due to several factors, such as: complexity of multiple associated conditions, physical and cognitive slowness of patient, and presence of caretakers and family members, with whom the physician will have to discuss the issues inherent to the relevant therapeutics and clinical conditions. 799799. Quinn TJ, McArthur K, Ellis G, Stott DJ. Functional assessment in older people. BMJ. 2011;343:d4681. Very frail older adults may require additional visits due to patient exhaustion. 800800. Benetos A, Petrovic M, Strandberg T. Hypertension Management in Older and Frail Older Patients. Circ Res. 2019;124(7):1045-60.
BP measurements may produce inaccurate values due to greater blood pressure variability and a few idiosyncrasies. Major factors interfering with BP measurement in older adults are: 1. auscultatory gap; 2. pseudohypertension; and 3. postural and postprandial variations. 801801. Campana EMG; Freitas EV, Brandão AA et al. Hipertensão Arterial no Idoso. In: Freitas EV, Py L, eds. Tratado de Geriatria e Gerontologia. Rio de Janeiro: GEN. 2016;p 507-21. (see Chapter 3)
Out-of-office BP monitoring, either ambulatory (ABPM) or at home (HBPM), is increasingly valued and indicated as a diagnostic tool for SHT in older adults.. 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,186186. Nobre F, Mion Jr. D, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 110(5Supl.1):1-29. Despite its limitations, self-measured BP should also be considered (see Chapter 3).
Proper blood pressure treatment and control for hypertensive older adults and the oldest old has unequivocal benefits, such as significant decreases in stroke, AMI, HF, and mortality, 8787. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24):2673–82.,509509. . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP-Cooperative Research Group. JAMA. 1991;265(24):3255-64.,572572. Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757-64.,802802. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-98.,803803. Corrao G, Rea F, Monzio Compagnoni M, Merlino L, Mancia G. Protective effects of antihypertensive treatment in patients aged 85 years or older. J Hypertens. 2017;35(7):1432-1. in addition to preventing cognitive decline and possibly dementia. 103103. Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, et al - SPRINT Research Group. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA. 2019;321(6):553-61.,804804. Hansson L, Lithell H, Skoog I, Baro F, Banki CM, Carbonin PU, et al. Study on COgnition and Prognosis in the Elderly (SCOPE). Blood Press; 1999; 8(3):177-83.
805. Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683–9.-806806. White WB, Wakefield DB, Moscufo N, et al. Effects of Intensive Versus Standard Ambulatory Blood Pressure Control on Cerebrovascular Outcomes in Older People (INFINITY). Circulation. 2019;140(20):1626–35. On the other hand, exact BP levels for treating older patients, as well as treatment targets, have been the subject of debate, 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670. and different guidelines provide different recommendations. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,807807. Feitosa-Filho GS, Peixoto JM, Pinheiro JES, et al. Updated Geriatric Cardiology Guidelines of the Brazilian Society of Cardiology - 2019. Arq Bras Cardiol. 2019;112(5):649-705. However, all guidelines, including this one, consider it key to perform individualized assessments. In addition to chronological age, we recommend weighing functional fitness, cognition, degree of frailty, patient expectations, comorbidities, end-organ damage and global CV risk, polypharmacy, and treatment tolerability. Recommended blood-pressure levels for older adults, both for initiating treatment and blood-pressure targets, can be found in Chart 14.1 .
14.4. Treatment
There is no single therapeutic strategy for older adults, especially those over the age of 80 to 85 ( Chart 14.2 ). Therefore, other factors should be considered above age itself while planning the treatment: presence of comorbidities, autonomy, functional status, and degree of frailty (LR: I; LE: C). That stratification is a better predictor of possible complications both in the short and the long term in relation to different comorbidities. 808808. Butrous H, Hummel SL. Heart Failure in Older Adults. Can J Cardiol. 2016;32(9):1140-7.,809809. Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Juni P, Carrel T, et al. Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):489-96. No therapeutic intervention should be denied or withdrawn based on age alone (LR: I; LE: C).
14.4.1. Nonpharmacological Treatment
All lifestyle change (LSC) measures that apply to younger individuals (see Chapter 8) are valid for older adults as well (LR: I; LE: B), but require greater care and more thoughtful consideration of their actual benefits—and potential risks. Older adults are more salt-sensitive, and dietary salt restrictions are more effective for this age group. 420420. World Health Organization. WHO. Guideline: Sodium intake for adults and children. Geneva;2012. The TONE study showed that there was a 4.3 mm Hg decrease in SBP and a 2.0 mm Hg decrease in DBP for for every 80 mmol of sodium (= 2.0 g of salt) reduction in daily salt intake. Combined with concurrent weight loss, the BP reduction effect was potentiated. 810810. Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group [published correction appears in JAMA 1998 Jun 24;279(24):1954]. JAMA. 1998;279(11):839–46. Excess reduction in salt intake may lead to hyponatremia and loss of appetite and can cause malnutrition. Potassium-rich diets should be encouraged, 811811. Mente A, O’Donnell MJ, Rangarajan S, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371(7):601-11. but require greater attention to the risk of hypercalcemia due to the frequent presence of chronic kidney disease (CKD) and the use of medications that lower potassium excretion.
Physical exercise and aerobic and resistance training are critical for older adults and should be recommended. 5252. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39(2):88-94. In older adults, especially the frail and sarcopenic, weight loss without physical exercise and adequate protein intake may lead to loss of muscle mass and worse functional fitness.
Smoking and alcohol abuse are still prevalent in older populations and should be discussed. Likewise, all medications in use by the patient need to be analyzed, as some may cause BP increases.
In recommending LSCs, physicians should consider the patient's degree of frailty, functional fitness, and other social and clinical aspects. Follow-up by a multidisciplinary team (see Chapter 7) and family/caretaker engagement are even more important for older patients.
14.4.2. Pharmacological Treatment
In choosing antihypertensive medication(s) for older adults, physicians should consider the high rates of comorbidities, specific contraindications, likely drug interactions and cost, as well as the availability of and clinical experience with the medication (LR: I; LE: C). Prudence dictates initiating monotherapy or combination therapy at low doses and, if needed, increase or gradually combine antihypertensives at intervals of at least two weeks (LR: I; LE: C).
Chapter 9 details when to give preference or to avoid specific antihypertensives and their combinations. Here, we highlight aspects peculiar to older patients.
The first antihypertensive may be a thiazide (or thiazide-like) diuretic, a calcium channel blocker (CCB), or a renin-angiotensin-aldosterone system (RAAS) blocker: an angiotensin-converting enzyme inhibitor (ACEI), or an angiotensin II AT1receptor blocker (ARB). A large number of clinical trials have studied these four classes, and they are widely used in guidelines for older adults. 807807. Feitosa-Filho GS, Peixoto JM, Pinheiro JES, et al. Updated Geriatric Cardiology Guidelines of the Brazilian Society of Cardiology - 2019. Arq Bras Cardiol. 2019;112(5):649-705.
808. Butrous H, Hummel SL. Heart Failure in Older Adults. Can J Cardiol. 2016;32(9):1140-7.-809809. Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Juni P, Carrel T, et al. Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):489-96. In terms of monitoring, indications and care are similar to those for other adults (see Chapter 9).
Beta-blockers (BBs) should not be used as initial monotherapy for older adults, 809809. Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Juni P, Carrel T, et al. Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):489-96. except in the presence of certain comorbidities, which may actually make their indication mandatory, such as heart failure (HF) or acute coronary failure (LR; I; LE: A). 812812. Bangalore S, Messerli FH, Kostis JB, Pepine CJ. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol. 2007;50(7):563-72.,813813. Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2017;1(1):CD002003. Patients suffering from bronchial asthma or chronic obstructive pulmonary disease (COPD), but with clinical indication for BBs, should be carefully treated with cardioselective BBs and after receiving respiratory compensation, and should bot be deprived of their benefits. 814814. Finks SW, Rumbak MJ, Self TH. Treating Hypertension in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2020;382(4):353-63. When used in combination with acetylcholinesterase inhibitors, frequently used for Alzheimer's disease, they may induce severe bradycardia. 815815. Isik AT, Soysal P, Stubbs B. Cardiovascular Outcomes of Cholinesterase Inhibitors in Individuals with Dementia: A Meta-Analysis and Systematic Review. J Am Geriatr Soc. 2018;66(9):1805-11.
Other classes of antihypertensives (centrally acting medications, aldosterone antagonists and direct vasodilators), as well as other invasive treatments of the sympathetic nervous system, should be seen as the exception and not used as a matter of course to treat older patients (LR: III; LE: C) (see Chapter 9).
The risk of falls in older adults can increase during the first weeks of treatment with DIUs, and with all other medication classes in the first day. In the long run, antihypertensives may actually have protective effects. 816816. Kahlaee HR, Latt MD, Schneider CR. Association Between Chronic or Acute Use of Antihypertensive Class of Medications and Falls in Older Adults. A Systematic Review and Meta-Analysis. Am J Hypertens. 2018;31(4):467-79.,817817. Ang HT, Lim KK, Kwan YH, Há YC, Lim JY. A Systematic Review and Meta-Analyses of the Association Between Anti-Hypertensive Classes and the Risk of Falls Among Older Adults. Drugs Aging. 2018;35(7):625-35.
14.5. Special Situations
There is some disagreement between results from observational studies and those from randomized clinical trials (RCTs). They come primarily from the fact that frail, multimorbid older adults are underrepresented in RCTs and the high risk of bias in nonrandomized and observational studies, where the longer survival of patients with high BP may be explained by their greater organ reserve. 818818. Mühlbauer V, Dallmeier D, Brefka S, Bollig C, Voigt-Radloff S, Denkinger M: The pharmacological treatment of arterial hypertension in frail, older patients— a systematic review. Dtsch Arztebl Int 2019; 116: 23–30.
819. Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406.
820. Delgado J, Masoli JAH, Bowman K, et al. Outcomes of Treated Hypertension at Age 80 and Older: Cohort Analysis of 79,376 Individuals. J Am Geriatr Soc. 2017;65(5):995–1003.
821. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.-822822. Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE Study. JAMA Intern Med. 2015;175(6):989–995.
14.5.1. Functional Status and Frailty: Assessment and Implications
In older adults, and especially in the oldest old, functional status and frailty require special attention. With the use of systematic tests and scales, the comprehensive geriatric assessment (CGA) enables an accurate global assessment of older adults and the development of therapeutic strategies. 823823. Wu C, Smit E, Peralta CA, Sarathy H, Odden MC. Functional Status Modifies the Association of Blood Pressure with Death in Elders: Health and Retirement Study. J Am Geriatr Soc. 2017;65(7):1482–1489.,824824. Soobiah C, Daly C, Blondal E, Ewusie J, Ho J, Elliott MJ, Yue R, Holroyd-Leduc J, Liu B, Marr S, Basran J, Tricco AC, Hamid J, Straus SE. An evaluation of the comparative effectiveness of geriatrician-led comprehensive geriatric assessment for improving patient and healthcare system outcomes for older adults: a protocol for a systematic review and network meta-analysis. Syst Rev. 2017 Mar 24;6(1):65. Though the ideal form of assessment, it may require the presence of a geriatrician or gerontologist. In day-to-day care for older hypertensive patients, clinicians should assess functional status and capacity to perform the activities of daily living. 825825. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.,826826. Rockwood K, Song X, Mitnitski A: Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. CMAJ 2011; 183: E487–94.
Routine use of the gait speed test (GST) is recommended, as it is easily performed as part of regular visits and has been shown to be a prognostic predictor of survival. 827827. Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668-1676.,828828. Studenski S, Perera S, Patel K, Rosano C, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50. Patients are considered frail or at risk of frailty when GST < 0.8 m/s (unable to walk 6 m in less than 8 seconds), requiring further investigation. 820820. Delgado J, Masoli JAH, Bowman K, et al. Outcomes of Treated Hypertension at Age 80 and Older: Cohort Analysis of 79,376 Individuals. J Am Geriatr Soc. 2017;65(5):995–1003.,829829. Odden MC, Moran AE, Coxson PG, Peralta CA, Goldman L, Bibbins-Domingo K. Gait Speed as a Guide for Blood Pressure Targets in Older Adults: A Modeling Study. J Am Geriatr Soc. 2016;64(5):1015–1023. In addition, this guideline recommends the use of the “Escala Clínica de Fragilidade,” which has already been translated into Brazilian Portuguese and validated in Brazil, 830830. Rodrigues, M.K., Nunes Rodrigues, I., Vasconcelos Gomes da Silva, D.J. et al. Clinical Frailty Scale: Translation and Cultural Adaptation Into the Brazilian Portuguese Language. J Frailty Aging 2020: in press. Published online Feb 14, 2020 7. based on the Canadian Clinical Frailty Scale , widely tested and deployed, as it is simple and reliable, provides a global view of patient condition, and determines the prognosis. 827827. Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668-1676.,828828. Studenski S, Perera S, Patel K, Rosano C, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50.,831831. Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9.,832832. Chong E, Ho E, Baldevarona-Llego J, Chan M, Wu L, Tay L. Frailty and Risk of Adverse Outcomes in Hospitalized Older Adults: A Comparison of Different Frailty Measures. J Am Med Dir Assoc. 2017 Jul;18(7):638.e7-.e11.
Frailty is associated with higher risk of HT, subclinical disease, CV events, and death. 821821. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.,833833. Atkins JL, Delgado J, Pilling LC, et al. Impact of Low Cardiovascular Risk Profiles on Geriatric Outcomes: Evidence From 421,000 Participants in Two Cohorts. J Gerontol A Biol Sci Med Sci. 2019;74(3):350–357.
834. Nadruz W Jr, Kitzman D, Windham BG, et al. Cardiovascular Dysfunction and Frailty Among Older Adults in the Community: The ARIC Study. J Gerontol A Biol Sci Med Sci. 2017;72(7):958–964.-835835. Aprahamian, I, Sassaki, E, dos Santos, MF, et al. Hypertension and frailty in older adults. J Clin Hypertens. 2018; 20: 186– 192. Adequate HT control may influence the trajectory of frailty. On the other hand, advanced levels of frailty are associated with lower BP values, lower body mass index (BMI), less muscle mass, impaired cognition, and higher mortality. 335335. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93.,836836. Ravindrarajah R, Hazra NC, Hamada S, et al. Systolic Blood Pressure Trajectory, Frailty, and All-Cause Mortality >80 Years of Age: Cohort Study Using Electronic Health Records. Circulation. 2017;135(24):2357–68.
Functionally active and independent patients with no severe comorbidities have enough organ reserve and mean survival to enjoy most of the benefits from antihypertensive treatment and should, if well tolerated, have the same blood-pressure targets as younger older adults (LR: I; LE: B). 335335. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93.,805805. Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683–9.,825825. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.,831831. Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9. On the other end of the scale, individuals with major functional loss, sarcopenia, frailty, or advanced dementia, or unable to perform self-care activities, should have their whole treatment regimen and blood-pressure targets reassessed. 821821. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.,825825. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.,831831. Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9.,837837. Gulla C, Flo E, Kjome RL, Husebo BS. Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. J Geriatr Cardiol. 2018;15(4):275–283. The primary goal is to improve symptoms and quality of life. Frailer older adults were systematically excluded from several clinical trials, so studies focused specifically on this population are key. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,821821. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.
Between the two extremes we find older adults with intermediate functional status and multiple non-CV comorbidities who may require very challenging therapeutic decisions. For them, deeper assessments may be critical to define the real risk-benefit ratio and to individualize therapeutic strategies. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,825825. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.,831831. Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9.,838838. Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78. Published 2015 Apr 9.,839839. Russo, G., Liguori, I., Aran, L. et al. Impact of SPRINT results on hypertension guidelines: implications for “frail” elderly patients. J Hum Hypertens 32, 633–638 (2018). https://doi.org/10.1038/s41371-018-0086-6
https://doi.org/10.1038/s41371-018-0086-...
14.5.2. Cognitive Decline and Dementia
In addition to its well-known role as the primary cause of strokes, HT has also been implicated as a pathogenic factor in cognitive impairment, both vascular and from Alzheimer's disease, the main causes of dementia in older adults, and more markedly in the long run. 840840. Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–517.
841. Abell JG, Kivimäki M, Dugravot A, et al. Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertension. Eur Heart J. 2018;39(33):3119–3125.-842842. Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, Coresh J, Knopman D, Power MC, Rawlings A, Sharrett AR, Wruck LM, Mosley TH. Midlife hypertension and 20-year cognitive change: the atherosclerosis risk in communities neurocognitive study. JAMA Neurol. 2014;71:1218–1227.
In several epidemiological studies, use of antihypertensive medications is associated with less cognitive decline and dementia, especially in the long run. 843843. Iadecola C, Gottesman RF. Neurovascular and Cognitive Dysfunction in Hypertension. Circ Res. 2019;124(7):1025–1044. RCTs have found decreased white matter damage and cognitive decline from treatment for HT, with intensive treatment even more efficient in that regard. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,844844. Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–2263. RCTs have not yet clearly proven decreased dementia. This may be because cognition was not the primary outcome in those RCTs, the lack of uniformity in the definition of dementia and in what tests were used, or the short duration of the trials. 806806. White WB, Wakefield DB, Moscufo N, et al. Effects of Intensive Versus Standard Ambulatory Blood Pressure Control on Cerebrovascular Outcomes in Older People (INFINITY). Circulation. 2019;140(20):1626–35.,845845. Flores LM, Mengue SS. Drug use by the elderly in Southern Brazil. Rev Saúde Pública. 2005; 39(6): 924-9.
14.5.3. Polypharmacy and Adherence
Polypharmacy, defined as the regular use of five or more medications, is increasingly frequent with age, 846846. Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17(4):123–132. and is associated with higher probability of adverse events (AE), drug interactions, and worse adherence to treatment. 845845. Flores LM, Mengue SS. Drug use by the elderly in Southern Brazil. Rev Saúde Pública. 2005; 39(6): 924-9.
Improper adherence to pharmacological treatment is a frequent issue for older adults and one of the primary causes of inadequate BP control. Determinants of poor adherence to therapeutic regimens include misunderstanding the disease, polypharmacy, multiple daily doses, and side effects. 847847. Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. To that end, this guideline recommends, especially for older adults with polypharmacy, the periodic review of each prescribed medication, AE assessments, 848848. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834. and that antihypertensive treatment include as few pills and tablets per day as possible, using single-tablet fixed-dose combinations, in addition to emphasizing nonpharmacological measures (LR: I; LE: A) (see Chapter 17).
14.5.4. Deintensification and Deprescription
In different clinical situations, it may be necessary to gradually lower dosage or even deprescribe antihypertensive medications; these include symptomatic hypotension; adverse reactions; persistently below-target SBP detected out-of-office or at the physician's office; 822822. Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE Study. JAMA Intern Med. 2015;175(6):989–995.
823. Wu C, Smit E, Peralta CA, Sarathy H, Odden MC. Functional Status Modifies the Association of Blood Pressure with Death in Elders: Health and Retirement Study. J Am Geriatr Soc. 2017;65(7):1482–1489.-824824. Soobiah C, Daly C, Blondal E, Ewusie J, Ho J, Elliott MJ, Yue R, Holroyd-Leduc J, Liu B, Marr S, Basran J, Tricco AC, Hamid J, Straus SE. An evaluation of the comparative effectiveness of geriatrician-led comprehensive geriatric assessment for improving patient and healthcare system outcomes for older adults: a protocol for a systematic review and network meta-analysis. Syst Rev. 2017 Mar 24;6(1):65. changing blood-pressure targets to less rigid levels (keeping in mind that BP tends to decrease at very advanced ages due to progressively lower organ reserve and greater frailty); and end-of-life palliative care. 837837. Gulla C, Flo E, Kjome RL, Husebo BS. Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. J Geriatr Cardiol. 2018;15(4):275–283.
A key issue in treating HT in older adults, especially in the oldest old, is the careful monitoring of AEs and tolerability, with special attention to atypical signs and symptoms. Discontinuing antihypertensives seems to be safe in the short run, but without proven benefits for cognition or functional fitness to perform the activities of daily living (ADLs). 838838. Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78. Published 2015 Apr 9.,849849. Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of Discontinuation of Antihypertensive Treatment in Elderly People on Cognitive Functioning--the DANTE Study Leiden: A Randomized Clinical Trial [published correction appears in JAMA Intern Med. 2016 Feb;176(2):284]. JAMA Intern Med. 2015;175(10):1622–1630.,850850. Luymes CH, Poortvliet RKE, van Geloven N, et al. Deprescribing preventive cardiovascular medication in patients with predicted low cardiovascular disease risk in general practice - the ECSTATIC study: a cluster randomised non-inferiority trial. BMC Med. 2018;16(1):5.
14.5.5. Orthostatic and Postprandial Hypotension
Because of arterial stiffness, variations in volume significantly interfere with HT control. Older adults have weaker baroreceptor reflex to hypotension, and so are likely to be subject to orthostatic hypotension (OH) and postprandial hypotension (PPH). A higher rate of neurodegenerative disease is also associated with this condition. 851851. Gibbons CH, Schmidt P, Biaggioni I, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264(8):1567–1582. Approximately 20% of older adults have OH and around 30% of institutionalized older adults experience hypotension after meals. 852852. Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. Hypertension 1992;19:508.,853853. Jansen RW, Lipsitz LA. Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med 1995;122:286. Therefore, older adults should be carefully monitored for OH and PPH (LR: I; LE: B).
In RCT, HT control led to fewer CV events with no increased risk of OH or falls with injuries. 854854. Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study [published correction appears in J Am Geriatr Soc. 2011 May;59(5):960]. J Am Geriatr Soc. 2011;59(3):383–389.
855. Margolis KL, Palermo L, Vittinghoff E, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med. 2014;29(12):1599–1606.-856856. Juraschek SP, Taylor AA, Wright JT Jr, et al. Orthostatic Hypotension, Cardiovascular Outcomes, and Adverse Events: Results From SPRINT. Hypertension. 2020;75(3):660–667 Poorly controlled HT and certain antihypertensive medications, such as alpha-blockers, can cause or worsen OH. The best option to control OH is to use nonpharmacological interventions, such as adequate hydration, adequate sodium intake, slow rise from decubitus, higher headrests, and compression socks. 853853. Jansen RW, Lipsitz LA. Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med 1995;122:286.
In postprandial hypotension, older adults should avoid large meals and high intake of alcohol and carbohydrates. They should also avoid exercising after meals. In addition, medication prescriptions should be revised in order to lower polypharmacy as much as possible, paying special attention to drugs that may be contributing to OH or PPH, such as DIU, sympatholytics, nitrates, and tricyclic antidepressants.
| Key Takeaways |
|---|
| HT prevalence increases progressively with age, as do other RFs, leading to sharp rises in CV risk among older adults. |
| Proper diagnosis requires caution with the peculiarities of blood pressure measurement, and out-of-office BP reagins (SMBP, HBPM, ABPM) are key in older adults, for whom inadequate treatment poses more risk. |
| Functional and cognitive status should be evaluated. Therapeutic decisions and BP targets should be based on functional status and survival over chronological age. |
| Treatment lowers CV risk as well as the risk of cognitive decline. Comorbidities, more frequent in older adults, should guide what medications are chosen or avoided. |
| Special attention should be given to family support networks, polypharmacy, adherence, and higher risk of OH. |
15. Secondary Hypertension
15.1. Introduction
Secondary hypertension is the form of hypertension (HT) due to an identifiable cause and treatable by a specific intervention which can improve or resolve blood pressure control. The actual prevalence of secondary HT is unknown, but estimated at 10 to 20%, 857857. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-312. and may be higher or lower, depending on the population cohort (especially in terms of age), diagnostic resources available and physician expertise. It should be investigated when signs (clinical history, physical examination, or routine tests) lead to clinical suspicion 258258. KDIGO CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013, 3(1):1-150.
259. Friedewald WT, Levi RI, Fredrickson DS. Estimation of the concentration of low density lipoproteins cholesterol in plasma without use of the ultracentrifuge. Clin Chem. 1972;18:499-502.
260. Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949; 37(2):161-86.
261. Casalle PN, Devereux RB, Alonso DR, Campo E, Kligfield P. Improved sex specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocadiograms: validation with autopsy findings. Circulation. 1987;75(3):565-72.
262. Rayner BL, Goodman H, Opie LH. The Chest Radiograph. A useful investigationin the evaluation of hypertensive patients. Am J Hypertens. 2004; 17(6):507-10.
263. Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the Use of Echocardiography in Adult Hypertension: A Report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015;28(7):727-54.
264. Tsioufis C, Kokkinos P, Macmanus C, Thomopoulos C, Faselis C, Doumas M, et al. Left ventricular hypertrophy as a determinant of renal outcome in patients with high cardiovascular risk. J Hypertens. 2010;28(11):2299–308.
265. Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010; 55:1600–7.
266. Polak JF, Szklo M, O’Leary DH. Carotid intima-media thickness score, positive coronary artery calcium score, and incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2017;6(1):e004612.
267. Vasbinder GB, Nelemans PJ, Kessels AG, Kroon AA, de Leeuw PW, van Engelshoven JM. Diagnostic tests for renal artery stenosis in patients suspected of having renovascular hypertension: a meta-analysis. Ann Intern Med. 2001;135(6):401-11.
268. Selvin E, Steffes MW, Zhu H, MatsushitaK, Wagenknecht L, Pankow J, et al. Brancati Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults.N Engl J Med. 2010;362(9):800–11.
269. Chin D, Battistoni A, Tocci G, Passerini J, Parati G, Volpe M. Non-invasive diagnostic testing for coronary artery disease in the hypertensive patient: potential advantages of a risk estimation-based algorithm. Am J Hypertens. 2012;25:1226–35.
270. Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003;107(22):2864–9.
271. Mikael LR, Paiva AMG, Mota-Gomes M, Sousa ALL, Jardim PCBV, Vitorino PVO, et al. Envelhecimento vascular e rigidez arterial. Arq Bras Cardiol. 2017;109(3):253-8.
272. de Leeuw FE, de Groot JC, Oudkerk M, Witteman JC, Hofman A, van Gijn J, Breteler MMB. Hypertension and cerebral white matter lesions in a prospective cohort study. Brain 2002;125(Pt 4):765–72
273. NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389 (10064):37-55.
274. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global Burden of hypertension: analysis of worldwide data. Lancet. 2005 Jan 15-21; 365(9455):217-23.
275. Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
276. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H and Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-47.
277. Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(1):56-64.
278. Blood Pressure Lowering Treatment Trialists C. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-8.
279. Matsura Y, Kanter JE, Bornfeldt KE. Highlighting Residual Atherosclerotic Cardiovascular Disease. Arterioscler Thromb Vasc Biol. 2019;39(1):e1-e9.
280. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.
281. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk 2020. Eur Heart J. 2020;41(1):111-88.
282. Sposito AC, Ramires JA, Jukema JW, Molina JC, da Silva PM, Ghadanfar MM, Wilson PW. Physicians’ attitudes and adherence to use of risk scores for primary prevention of cardiovascular disease: cross-sectional survey in three world regions. Curr Med Res Opin. 2009;25(5):1171-8.
283. Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkin et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association, Circulation. 2009;119(7):2408-16.
284. Cooney MT, Dudina AL, Graham IM. Value and Limitations of Existing Scores for the Assessment of Cardiovascular Risk A Review for Clinicians. J Am Coll Cardiol. 2009;54(14):1209-27.
285. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014; 383(9932):1899–911.
286. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364(9438):937-52.
287. Wang OJ, Wang Y, Chen J, Krumholz HM. Recent Trends in Hospitalization for Acute Myocardial Infarction. Am J Cardiol. 2012; 109(11):1589–93.
288. Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583-612.
289. International Diabetes Federation. IDF Consensus Worldwide Definition of the Metabolic Syndrome. 2006. [Cited in 2020 Mar 10]. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html .
https://www.idf.org/e-library/consensus-...
290. Perrone-Filardi P, Coca A, Galderisi M, Paolillo S, Alpendurada F, de Simone G, et al. Noninvasive cardiovascular imaging for evaluating subclinical target organ damage in hypertensive patients: a consensus article from the European Association of Cardiovascular Imaging, the European Society of Cardiology Council on Hypertension and the European Society of Hypertension. J Hypertens. 2017; 35(9):1727–41.
291. PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358(9287):1033-41.
292. Manning LS, Mistri AK, Potter J, Rothwell PM, Robinson TG. Short-term blood pressure variability in acute stroke: post hoc analysis of the controlling hypertension and hypotension immediately post stroke and continue or stop post-stroke antihypertensives collaborative study trials. Stroke. 2015; 46(6):1518-24.
293. Grundvold I, Skretteberg PT, Liestol K, Erikssen G, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: a 35-year follow-up study. Hypertension. 2012; 59(2):198–204.
294. Singer DR, Kite A. Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg. 2008;35(6):701–8.
295. Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Petersen C et al. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010; 31(7):883-91.
296. Orlova IA, Nuraliev EY, Yarovaya EB, Ageev FT. Prognostic value of changes in arterial stiffness in men with coronary artery disease. Vasc Health Risk Manag. 2010; 6:1015–21.
297. Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension. 2009; 54(6):1328–36.
298. Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63.
299. Bertoluci MC, Moreira RO, Faludi A, Izar MC, Schaan BD, Valerio CM et al. Brazilian guidelines on prevention of cardiovascular disease in patients with diabetes: a position statement from the Brazilian Diabetes Society (SBD), the Brazilian Cardiology Society (SBC) and the Brazilian Endocrinology and Metabolism Society (SBEM). Diabetol Metab Syndr. 2017; 9:53.
300. Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, and assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2015; 31(5): 549-68.
301. British Cardiac Society; British Hypertension Society; Diabetes UK; HEART UK; Primary Care Cardiovascular Society; Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005; 91 Suppl 5:v1-52. 6.
302. Sánchez RA, Boggia J, Peñaherrera E, Barroso WS, Barbosa E, Villar R, et al. Ambulatory blood pressure monitoring over 24 h: A Latin American Society of Hypertension position paper-accessibility, clinical use and cost effectiveness of ABPM in Latin America in year 2020. J Clin Hypertens. 2020; 22(4): 527–43.
303. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, et al; European Society of Hypertension Working Group on Blood Pressure Monitoring. J Hypertens. 2013 Sep; 31(9):1731-68.
304. Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018; 378(16):1509–20.
305. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011; 57(1):3–10.
306. Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012 Aug15;(8):CD006742.
307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.
308. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.
309. Lonn EM, Bosch J, López-Jaramillo P, Zhu J, Liu L, Pais P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–20.
310. Lee CJ, Ryu J, Kim HC, Ryu DR, Ihm SH, Kim YJ, et al. Clinical benefit of treatment of stage-1, low-risk hypertension Korean national health insurance database analysis. Hypertension. 2018;72(6):1285–93.
311. Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging?: The Framingham Heart Study. Circulation. 2001;103(9):1245–9.
312. Mahtta D, Elgendy IY, Pepine CJ. Optimal medical treatment of hypertension in patients with coronary artery disease. Expert Rev Cardiovasc. 2018;16(11):815-23.
313. Rosendorff C, Lackland DT, Allison M, Aronow WS, Black HR, Blumenthal RS, et al. Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Am Coll Cardiol. 2015;65(18):1998–2038.
314. Yannoutsos A, Dreyfuss CT, Safar ME, Blacher J. Optimal blood pressure target in stroke prevention. Curr Opin Neurol. 2017;30(1):8-14.
315. Béjot Y. Targeting blood pressure for stroke prevention: current evidence and unanswered questions. J Neurol. 2019; doi: 10.1007/s00415-019-09443-5. Online ahead of print.
316. Pinho-Gomes AC, Rahimi K. Management of blood pressure in heart failure. Heart. 2019;105(8):589-95.
317. Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018;3(4):288–97.
318. Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018 Jul 15;263:69-74.
319. Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, et al. Effects of intensive BP control in CKD. J Am Soc Nephrol. 2017;28(9):2812–23.
320. Filipovsky J, Seidlerova J, Kratochvil Z, Karnosova P, Hronova M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 2016;25(4):228–34.
321. Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67(5):808–12.
322. Heerspink HJ, Ninomiya T, Perkovic V, Woodward M, Zoungas S, Cass A, et al. ADVANCE Collaborative Group: Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Eur Heart J. 2010;31(23):2888–96.
323. Ku E, Gassman J, Appel LJ, Smogorzewski M, Sarnak MJ, Glidden DV, et al. BP control and long-term risk of ESRD and mortality. J Am Soc Nephrol. 2017;28(2):671–7.
324. Chang AR, Appel LJ. Target Blood Pressure for Cardiovascular Disease Prevention in Patients with CKD. Clin J Am Soc Nephrol. 2018; 13(10):1572–4.
325. Chang AR, Lóser M, Malhotra R, Appel LJ. Blood pressure goals in patients with CKD: A review of evidence and guidelines. Clin J Am Soc Nephrol. 2019;14(1):161-9.
326. American Diabetes Association. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S111–34.
327. Toklu B, Bangalore S. Blood pressure lowering in patients with type 2 diabetes improves cardiovascular events including mortality, but more intensive lowering to systolic blood pressure less than 130 mm Hg is associated with further reduction in stroke and albuminuria without further reduction in cardiac events. Evid Based Med. 2015;20(5):183–4.
328. Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC, et al. Effect of Intensive Blood Pressure Lowering on Left Ventricular Hypertrophy in Patients With Diabetes Mellitus: Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial. Hypertension. 2015;66(6):1123–9.
329. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: Systematic review and meta-analyses. BMJ. 2016;24:352 i717.
330. Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85.
331. De Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: A position statement by the American diabetes association. Diabetes Care. 2017;40(9):1273–84.
332. Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mmHg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499-503.
333. Beckett N, Peters R, Leonetti G, et al, HYVET Study Group. Subgroup and per-protocol analyses from the Hypertension in the Very Elderly Trial. J Hypertens 2014;32(7):1478–87.
334. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: A systematic review and meta-analysis. Ann Intern Med. 2017;166(6):419–29.
335. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93.
336. Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47(1): 100-2.
337. Weinstein E, Rucker LM. Team-based care to improve control of hypertension in an inner city practice. Healthc (Amst). 2016; 4(1):52-6.
338. Mansoor SM, Krass I, Aslani P. Multiprofessional interventions to improve patient adherence to cardiovascular medications. J Cardiovasc Pharmacol Ther. 2013; 18(1)19-30.
339. Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009; 169(19): 1748-55.
340. Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006; 44(7): 646-57.
341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.
342. David G, Gunnarsson C, Saynisch PA, Chawla R, Nigam S.. Do patient-centered medical homes reduce emergency department visits? Health Serv Res. 2015; 50(2):418-39.
343. Jacob V, Chattopadhyay SK, Thota AB, et al. Economics of Team-based Care in Controlling Blood Pressure: A Community Guide Systematic Review. Am J Prev Med 2015; 49(5): 772-83.
344. Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45.
345. Jardim LM, Jardim TV, Souza WK, Barroso de Souza WKS, Pimenta CD, Sousa AL, et al. Multiprofessional Treatment of High Blood Pressure in Very Elderly Patients. Arq Bras Cardiol. 2017; 108(1): 53-9.
346. Proia KK, Thota AB, Njie GJ, Finnie R, Hopkins D, Mukhtar Q, et al. Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014; 47(1):86-99.
347. Kuhmmer R, Lazzaretti RK, Guterres CM, Raimundo FV, Leite LE, Delabary TS, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):456.
348. Strumpf E, Ammi M, Diop M, Laniel JF, Tousignant P. The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J Health Econ. 2017;55:76-94.
349. Norouzi Z, Jafarnejad F, Khadivzadeh T, Esmaily H, Headjazi A. Comparison of the effect of standardized patient-based training with team-based learning on the knowledge of midwifery students in providing services to victims of rape. J Educ Health Promot. 2019;8:267.
350. Kravetz JD, Walsh RF. Team-Based Hypertension Management to Improve Blood Pressure Control. J Prim Care Community Health 2016;7(4):272-5.
351. Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001; 21(3):221-32.
352. Overwyk KJ, Dehmer SP, Roy K, Maciosek MV, Hong Y, Baker-Goering MM, et al. Modeling the Health and Budgetary Impacts of a Team-based Hypertension Care Intervention That Includes Pharmacists. Med Care. 2019;57(11):882-9.
353. Tagliacozzo DM, Luskin DB, Lashof JC, Ima K. Nurse intervention and patient behavior: an experimental study. Am J Public Health. 1974; 64(6): 596-603.
354. Dickey FF, Mattar ME, Chudzik GM. Pharmacist counsling increases drug regimen compliance. Hospitals. 1975; 49(9): 85-6, 88.
355. Brazil.Ministério da Saúde. Política Nacional de Educação Permanente em Saúde: o que se tem produzido para o seu fortalecimento. Brasília; 2018.
356. Brazil.Ministério da Saúde. Síntese de evidências para políticas de saúde: adesão ao tratamento medicamentoso por pacientes portadores de doenças crônicas. Brazilia; 2018.
357. Marquez Contreras E, Marquez Rivero S, Rodriguez Garcia E, Ramos LLG, Vilas JCP, Suarez AB, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167-73.
358. Hallberg I, Ranerup A, Bengtsson U, et al. Experiences, expectations and challenges of an interactive mobile phone-based system to support self-management of hypertension: patients’ and professionals’ perspectives. Patient Prefer Adherence. 2018 Mar 28;12:467-76.
359. Hallberg I, Ranerup A, Bengstsson U, Kjellgren K. Supporting the self-management of hypertension: Patients’ experiences of using a mobile phone-based system. J Hum Hypertens. 2016; 30(2):141-6.
360. Schoenthaler A, de la Calle F, Pitaro M, Lum A, Chaplin W, Mogavero J, et al. A Systems-Level Approach to Improving Medication Adherence in Hypertensive Latinos: a Randomized Control Trial. J Gen Intern Med. 2020; 35(1): 182-9. 2019/10/19. DOI: 10.1007/s11606-019-05419-3.
361. Schoenthaler A, De La Calle F, Barrios-Barrios M, Garcia A, Pitaro M, Lum A, et al. A practice-based randomized controlled trial to improve medication adherence among Latinos with hypertension: study protocol for a randomized controlled trial. Trials. 2015;16:290.
362. Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: A randomized controlled trial. Patient Educ Couns. 2020; 103: 336-42.
363. Serene Olin S, Kutash K, Pollock M, et al. Developing quality indicators for family support services in community team-based mental health care. Adm Policy Ment Health. 2014; 41: 7-20.
364. Ranerup A and Hallberg I. Actors and intentions in the development process of a mobile phone platform for self-management of hypertension. Inform Health Soc Care 2015; 40: 299-318.
365. Brazil.Ministério da Saúde. Política Nacional de Atenção Básica. Portaria no 2.436, de 21 de setembro de 2017. Brasília;2017.
366. Riegel GR, Ribeiro PAB, Rodrigues MP, et al.Efficacy of nutritional recommendations given by registered dietitians compared to other healthcare providers in reducing arterial blood pressure: Systematic review and meta-analysis. Clin Nutr. 2018; 37(2): 522-31.
367. Mitchell LJ, Ball LE, Ross LJ, et al. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J Acad Nutr Diet. 2017; 117(1): 1941-62.
368. Sladdin I, Chaboyer W, Ball L. Patients’ perceptions and experiences of patient-centred care in dietetic consultations. J Hum Nutr Diet. 2018; 31I2): 188-96.
369. Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association Between Obesity and Cardiovascular Outcomes: A Systematic Review and Meta-analysis of Mendelian Randomization Studies. JAMA Netw Open. 2018; 1(7): e183788.
370. Dwivedi AK, Dubey P, Cistola DP. Association Between Obesity and Cardiovascular Outcomes: Updated Evidence from Meta-analysis Studies. Curr Cardiol Rep.2020; 22(4):25.
371. Zhao CN, Meng X, Li Ya, Li S, Tang GY, Li HB. Fruits for Prevention and Treatment of Cardiovascular Diseases. Nutrients. 2017; 9(6):598.
372. Mellendick K, Shanahan L, Wideman L, calkins S, Keane S, Lovelady C. et al. Diets Rich in Fruits and Vegetables Are Associated with Lower Cardiovascular Disease Risk in Adolescents. Nutrients. 2018; 10(2):136.
373. Alissa EM. Ferns GA. Dietary fruits and vegetables and cardiovascular diseases risk. Crit Rev Food Sci Nutr. 2017; 57(9):1950-62.
374. Aminde LN, Cobiac LJ, Veerman JL. Potential impact of a modest reduction in salt intake on blood pressure, cardiovascular disease burden and premature mortality: a modelling study. Open Heart. 2019; 6(1): e000943.
375. He FJ, Tan M, Ma Y, et al. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020; 75: 632-47.
376. Graham GN, Ostrowski M, Sabina AB. Population health-based approaches to utilizing digital technology: a strategy for equity. J Public Health Policy 2016; 37(Suppl 2): 154-66.
377. Grahame JA. Digital Note-Taking: Discussion of Evidence and Best Practices. J Physician Assist Educ. 2016; 27(1): 47-50.
378. Zhao R, Bu W, Chen Y, Chen X. The Dose-Response Associations of Sedentary Time with Chronic Diseases and the Risk for All-Cause Mortality Affected by Different Health Status: A Systematic Review and Meta-Analysis. J Nutr Health Aging. 2020; 24(1): 63-70.
379. Ozemek C, Lavie CJ. Rognmo O. Global physical activity levels - Need for intervention. Prog Cardiovasc Dis. 2019; 62(2): 102-7.
380. de Rezende LF, Rabacow FM, Viscondi JY, Luiz O, Matsudo V. Effect of physical inactivity on major noncommunicable diseases and life expectancy in Brazil. J Phys Act Health. 2015; 12(3): 299-306.
381. Ekelund U, Brown WJ, Steene-Johannessen J, Wang M, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019; 53(14): 886-94.
382. Ferreira T, Cipolotti M, Marques B, Miranda M. A inserção do Profissional de Educação Física nos Núcleos de Apoio a Saúde da Família: visão dos profissionais. Rev Bras Ativ Fís Saúde 2016; 21(3):228-36.
383. Balamurugan A, Adolph S, Faramawi M, George M. Community Team-Based Care for Hypertension Management: A Public-Private Partnership in Rural Arkansas. J Ark Med Soc. 2017; 113(7):150-4.
384. Sidney S. Team-Based Care: A Step in the Right Direction for Hypertension Control. Am J Prev Med. 2015; 49(5): e81-e82.
385. Santschi V, Wuerzner G, Chiolero A, Brurnand B. Team-based care for improving hypertension management among outpatients (TBC-HTA): study protocol for a pragmatic randomized controlled trial. BMC Cardiovasc Disord.2017; 17(1): 39.
386. Al-Rubaey MG, Shwaish MI. Impact of hypertension education on treatment compliance among hypertensive patients in Baghdad 2017. J Pak Med Assoc .2019; 69(Suppl 3): S9-S12.
387. Chen Y, Li X, Jing G, Pan B, Long B, Zhi Tong B, et al. Health education interventions for older adults with hypertension: A systematic review and meta-analysis. Public Health Nurs. 2020 ;37(3): 461-9.
388. Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7.
389. Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper P. Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Curr Hypertens Rep. 2015; 17: 94.
390. Conn VS, Ruppar TM, Chase JD. Blood pressure outcomes of medication adherence interventions: systematic review and meta-analysis. J Behav Med. 2016;39:1065-75.
391. Mistry N, Keepanasseril A, Wilczynski NL, Nieuwlaat R, Ravall M, Haynes B, et al. Technology-mediated interventions for enhancing medication adherence. J Am Med Inform Assoc. 2015; 22: e177-193.
392. Lindahl B, Norberg M, Johansson H, Lindvall K, Ng N, Nordin M, et al. Health literacy is independently and inversely associated with carotid artery plaques and cardiovascular risk. Eur J Prev Cardiol. 2020; 27(2): 209-15.
393. Earl GL, Harris EM, Dave M, Jiang JE. Implementing a health literacy module fostering patient-centered written communication in a cardiovascular prevention elective course. Curr Pharm Teach Learn. 2019;11(7):702-9.
394. Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. 10) The Effect of Self-Monitoring of Blood Pressure on Medication Adherence and Lifestyle Factors: A Systematic Review and Meta-Analysis. Am J Hypertens. 2015;28(10):1209-21.
395. Fletcher BR, Hinton L, Hartmann-Boyce J, Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ Couns. 2016;99(2):210-9.
396. Bengtsson U, Kjellgren K, Hallberg I, Lundin M, Makitalo A. Patient contributions during primary care consultations for hypertension after self-reporting via a mobile phone self-management support system. Scand J Prim Health Care. 2018; 36(1):70-9.
397. McLean G, Band R, Saunderson K, Murray HP, Little P, McManus RJ, et al. Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens. 2016; 34(4):600-12.
398. Thakkar J, Kurup R, Laba TL, Mobile Telephone Text Messaging for Medication Adherence in Chronic Disease: A Meta-analysis. JAMA Intern Med. 2016; 176(3): 340-9.
399. John JR, Tannous WK, Jones A. Effectiveness of a patient-centered medical home model of primary care versus standard care on blood pressure outcomes among hypertensive patients. Hypertens Res. 2020;43(9):892-902.
400. Yan R, Li W, Yin L, Wang Y, Bo J; PURE-China Investigators. Cardiovascular Diseases and Risk-Factor Burden in Urban and Rural Communities in High-, Middle-, and Low-Income Regions of China: A Large Community-Based Epidemiological Study. J Am Heart Assoc. 2017;6(2):e004445.
401. Malta DC, Silva AGD, Machado ÍE, Sá ACMGN, Santos FMD, Prates EJS, Cristo EB. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J Bras Pneumol. 2019;45(5):e20180384.
402. Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Smith N, et al. Screening for High Blood Pressure in Adults: A Systematic Evidence Review for the U.S. Rockville MD:Agency Research and Quality;2014. [Evidence Synthesis No. 121. AHRQ / Publication No. 13-05194-EF-1. ]
403. Bhatnagar A, Maziak W, Eissenberg T, Ward KD, Thurston G, King BA, et al. Water Pipe (Hookah) Smoking and Cardiovascular Disease Risk: A Scientific Statement from the American Heart Association. Circulation. 2019;139(19):e917-36.
404. Leone FT, Zhang Y, Evers-Casey S, Evins AE, Eakin MN, Fathi J, et al. Initiating Pharmacologic Treatment in Tobacco-Dependent Adults. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5-e31.
405. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
406. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH–Sodium Collaborative. Research Group. N Engl J Med. 2001;344:3–10.
407. Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2020;11(5):1150-60.
408. Larsson SC, Wallin A, Wolk A. Dietary Approaches to Stop Hypertension diet and incidence of stroke: results from 2 prospective cohorts. Stroke. 2016;47(4):986-90.
409. Mertens E, Markey O, Geleijnse JM, Lovegrove JA, Gibens DI. Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: evidence from the Caerphilly Prospective Study. Eur J Nutr. 2018;57(3):1245-58.
410. Soltani S, Arablou T, Jayedi A, Salehi-Abargouei A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutr J. 2020;19(1):37.
411. Mozaffari H, Ajabshir S, Alizadeh S. Dietary Approaches to Stop Hypertension and risk of chronic kidney disease: A systematic review and meta-analysis of observational studies. Clin Nutr. 2020;39(7):2035-44.
412. Martínez-González MA, Gea A, Ruiz-Canela M. The mediterranean diet and cardiovascular health. Circ Res. 2019;124(5):779-98.
413. Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72(1):30-43.
414. Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173-91.
415. Nissensohn M, Román-Viñas B, Sánchez-Villegas A, Piscopo S, Serra-Majem L. The effect of the mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutr Educ Behav. 2016;48(1):42-53.
416. Jennings A, Berendsen AM, de Groot LCPGM, Feskens EJM, Brzozowska A, Sicinska E, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults. Hypertension. 2019;73(3):578-86.
417. Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64(1):69-76.
418. Fuchs SF. Estudo PREVER: Mudanças de Estilo de Vida. Porto Alegre: Engenho de Idéias; 2011. 47 p.
419. Powles J, Gahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intake in 1990 and 2010: a systematic analysis of 24h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733.
420. World Health Organization. WHO. Guideline: Sodium intake for adults and children. Geneva;2012.
421. Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trial. BMJ. 2020 Feb 24; 368:m315.
422. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on bloodpressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ; 2013;346:f1325.
423. Bernabe-Ortiz A, Sal Y Rosas VG, Ponce-Lucero V, Cárdenas MK, Carrillo-Larco RM, Diez-Canseco F, et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26(3):374-8.
424. Marklund M, Singh G, Greer R, Cudhea F, Matsushita K, Micha R, Brady T, et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: modelling study. BMJ. 2020;369:m824.
425. Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015; 33(8):1509-20.
426. China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007; 25(10):2011-8.
427. Zhou B, Wang HL, Wang WL, Wu XM, Fu LY, Shi JP. Long-term effects of salt substitution on blood pressure in a rural north Chinese population. J Hum Hypertens. 2013; 27(7):427-33.
428. Peng Y-G, Li W, Wen X-X, Li Y, Hu J-H, Zhao L-C. Effects of salt substitutes on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(6):1448-54.
429. Jin A, Xie W, Wu Y. Effect of salt reduction interventions in lowering blood pressure in Chinese populations: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2020;10(2):e032941.
430. Thorning TK, Bertram HC, Bonjour JP, de Groot L, Dupont D, Feeney R, et al. Whole dairy matrix or single nutrients in assessment of health effects: current evidence and knowledge gaps. Am J Clin Nutr. 2017;105(5):1033-45.
431. Mozaffarian D, Wu JHY. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ Res. 2018;122(2):369-84.
432. Dehghan M, Mente A, Rangarajan S, Sheridan P, Mohan V, Igbal R, et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2018;392(10161):2288-97
433. Buendia JR, Li Y, Hu FB, Cabral HJ, Bradlee ML, Quatromoni PA, et al. Regular yougurt intake and risk of cardiovascular disease among hypertensive adults. Am J Hypertens. 2018;31(5):557-65.
434. Machin DR, Park W, Alkatan M, Mouton M, Tanaka H. Hypotensive effects of solitary addition of conventional nonfat dairy products to the routine diet: a randomized controlled trial. Am J Clin Nutr. 2014;100(1):80-7.
435. Rietsema S, Eelderink C, Joustra ML, van Vliet IMY, van Londen M, Corpeleijn E, et al. Effect of high compared with low dairy intake on blood pressure in overweight middle-aged adults: results of a randomized crossover intervention study. Am J Clin Nutr. 2019;110(2):340-8.
436. Hidayat K, Du HZ, Yang J, Chen GC, Zhang Z, Lin ZN, Qin LQ. Effects of milk proteins on blood pressure: a meta-analysis of randomized control trials. Hypertens Res. 2017;40(3):264-70.
437. Brazil.Ministério da Saúde. Guia Alimentar Para a População Brazileira. 2ª ed. Brasília; 2014.
438. Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. U.S. Department of Agriculture, Agricultural Research Service, Washington(DC);2015.
439. Desch S, Schmidt J, Kobler D, Sonnabend M, Eitel I, Sareban M, et al. Effect of cocoa products on blood pressure: systematic review and meta-analysis. Am J Hypertens. 2010;23(1):97-103.
440. Ried K, Fakler P, Stocks NP, and Cochrane Hypertension Group National Institute of Integrative Medicine. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. 2017 Apr 25;4(4):CD008893.
441. Mesas AE, Leon-Munoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr. 2011;94(4):1113-26.
442. van Dam RM, Hu FB, Willett WC. Coffee, caffeine, and health. N Engl J Med. 2020; 383(4):369-78.
443. D´Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose-response meta-analysis of prospective studies. Eur J Nutr. 2019; 58(1):271-80.
444. Grosso G, Micek A, Godos J, Pajak A, Sciacca S, Bes-Rastrollo M, Galvano F, Martinez-Gonzalez MA. Long-Term Coffee Consumption Is Associated with Decreased Incidence of New-Onset Hypertension: A Dose-Response Meta-Analysis. Nutrients. 2017;9(8):890.
445. Ke L, Mason RS, Mpofu E, Vingren JL, Li Y, Graubard BI, et al. Hypertension and other cardiovascular risk factors are associated with vitamin D deficiency in an urban Chinese population: a short report. J Steroid Biochem Mol Biol. 2017;173:286-91.
446. Zhang D, Cheng C, Wang Y, Sun H, Yu S, Xue Y, et al. Effect of vitamin D on blood pressure and hypertension in the general population: an update meta-analysis of cohort studies and randomized controlled trials. Prev Chronic Dis. 2020;17:E03.
447. Pilz S, Gaksch M, Kienreich K, Grubler M, Verheyen N, Fahrleitner-Pammer A, et al. Effects of vitamin D on blood pressure and cardiovascular risk factors: a randomized controlled trial. Hypertension. 2015;65(6):1195-201.
448. Arora P, Song Y, Dusek J, Plotnikoff G, Sabatine MS, Cheng S, et al. Vitamin D therapy in individuals with prehypertension or hypertension: the DAYLIGHT trial. Circulation. 2015;131(3):254-62.
449. Shu L, Huang K. Effect of vitamin D supplementation on blood pressure parameters in patients with vitamin D deficiency: a systematic review and meta-analysis. J Am Soc Hypertens. 2018;12(7):488-96.
450. Cormick G, Ciapponi A, Cafferata ML, Belizán JM. Calcium Supplementation for Prevention of Primary Hypertension. Cochrane Database Syst Rev.2015;(6):CD010037.
451. Li K, Liu C, Kuang X, Deng Q, Zhao F, Li D. Effects of Multivitamin and Multimineral Supplementation on Blood Pressure: A Meta-Analysis of 12 Randomized Controlled Trials. Nutrients. 2018;10(8):1018.
452. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol. 2019;15(6):367-85.
453. Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42(5):878–84.
454. Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86.
455. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126-31.
456. US Department of Health and Human Services. Physical Activity Guidelines for Americans 2018. [Cited in 2020 Apr 12] Available at: https://health.gov/sites/default/files/201909/Physical_Activity_Guidelines_2nd_edition.pdf .
https://health.gov/sites/default/files/2...
457. Ekelund U, Steene-Johannessen J, Brown WJ. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonized meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-10.
458. Liu X, Zhang D, Liu Y, Sun X, Han C, Wang B, et al. Dose-response associations between physical activity and incident hypertension: a systematic review and meta-analysis of cohort studies. Hypertension. 2017; 69(5):813-20.
459. Cao L, Li X, Yan P, Wang X, Li M, Li R, et al. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J Clin Hypertens. 2019;21(7):868-76.
460. MacDonald HV, Johnson BT, Huedo-Medina TB, Livingston J, Forsyth KC, Kraemer WJ, et al. Dynamic Resistance Training as Stand- Alone Antihypertensive Lifestyle Therapy: A Meta-Analysis. J Am Heart Assoc. 2016;5(10): e003231.
461. Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57(1-2):154-60.
462. Igarashi Y, Nogami Y. The effects of regular aquatic exercise on blood pressure: a meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2018;25(2):190-9.
463. Cramer H, Langhorst J, Dobos G, Lauche R. Yoga for metabolic syndrome: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23(18):1982-93.
464. Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, et al. Tai Chi for Essential Hypertension: a Systematic Review of Randomized Controlled Trials. Curr Hypertens Rep. 2020;22(3):25.
465. Costa EC, Hay JL, Kehler DS, Boreskie KF, Arora RC, Umpierre D, et al. Effects of High-Intensity Interval Training Versus Moderate- Intensity Continuous Training on Blood Pressure in Adults with Pre- to Established Hypertension: a Systematic Review and Meta-Analysis of Randomized Trials. Sports Med. 2018;48(9):2127-42.
466. Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, Pescatello LS. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473-9.
467. Meneguelo RS et al. III Diretrizes da Sociedade Brazileira de Cardiologia sobre Teste Ergométrico. Arq Bras Cardiol. 2010;95(5, supl.1):1-26.
468. Mahtani KR, Nunan D, Heneghan CJ. Device-guided breathing exercises in the control of human blood pressure: systematic review and meta-analysis. J Hypertens. 2012; 30(5):852-60.
469. Zou Y, Zhao X, Hou YY, Liu T, Wu Q, Huang YH, et al. Meta-Analysis of Effects of Voluntary Slow Breathing Exercises for Control of Heart Rate and Blood Pressure in Patients with Cardiovascular Diseases. Am J Cardiol. 2017;120(1):148–53.
470. Ubolsakka-Jones C, Tongdee P, Jones DA. The effects of slow loaded breathing training on exercise blood pressure in isolated systolic hypertension. Physiother Res Int. 2019;24(4):e1785.
471. Kow FP, Adlina B, Sivasangari S, Punithavathi N, Ng KK, Ang AH, et al. The impact of music guided deep breathing exercise on blood pressure control - A participant blinded randomised controlled study. Med J Malaysia. 2018;73(4):233–8.
472. Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61(6):1360-83.
473. Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews. 2013,12:CD006577.
474. Do Amaral MAS, Neto MG, de Queiroz JG, Martins-Filho PRS, Saquetto M B, Carvalho VO. Effect of music therapy on blood pressure of individuals with hypertension: A systematic review and Meta-analysis. Int J Cardiol. 2016;214:461–4.
475. Kühlmann AYR, Etnel JRG, Roos-Hesselink JW, Jeekel J, Bogers AJJC, Takkenberg JJM. Systematic review and meta-analysis of music interventions in hypertension treatment: a quest for answers. BMC Cardiovasc Disord. 2016;16:69.
476. Maynard BR, Solis MR, Miller VL, Brendel KE. Mindfulness-based interventions for improving cognition, academic achievement, behavior, and socioemotional functioning of primary and secondary school students. Campbell Systematic Reviews; 2017 https://doi.org/10.4073/CSR.2017.5
https://doi.org/10.4073/CSR.2017.5...
477. Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation Programs for Psychological Stress and Well-being A Systematic Review and Meta-analysis. JAMA Intern Med. 2014;174(3):357-68.
478. Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of systematic reviews and meta-analyses. Complement Ther Med. 2017;34:26-34.83.
479. GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, et al; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Hypertension. Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart Assoc. 2017;6(10):e002218.
480. Steinhauser KE, Fitchett G, Handzo GF, Johnson KS, Koenig HG, Pargament KI, et al. State of the Science of Spirituality and Palliative Care Research Part I: Definitions, Measurement, and Outcomes. J Pain Symptom Manag. 2017;54(3):428-40.
481. Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28.
482. Chida Y, Steptoe A, Powell LH. Religiosity/Spirituality and Mortality A Systematic Quantitative Review. Psychother Psychosom. 2009;78(2):81–90.
483. Li S, Stampfer MJ, Williams DR, VanderWeele TJ. Association of Religious Service Attendance With Mortality Among Women. JAMA Intern Med 2016;176(6):777-85.
484. VanderWeele TJ, Yu J, Cozier YC, Wise L, Argentieri MA, Rosenberg L, et al. Attendance at Religious Services, Prayer, Religious Coping, and Religious/Spiritual Identity as Predictors of All-Cause Mortality in the Black Women’s Health Study. Am J Epidemiol. 2017;185(7):515-22.
485. Abu HO, Ulbricht C, Ding E, Allison JJ, Salmoirago-Blotcher E, Goldberg RJ, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res. 2018;27(11):2777-97.
486. Shattuck EC, Muehlenbein MP. Religiosity/Spirituality and Physiological Markers of Health. J Relig Health. 2020;59(2):1035-54.
487. Spence ND, Farvid MS, Warner ET, et al. Religious Service Attendance, Religious Coping, and Risk of Hypertension in Women Participating in the Nurses’ Health Study II. Am J Epidemiol. 2020;189(3):193-203.
488. Holt-Lunstad J, Steffen PR, Sandberg J, Jensen B. Understanding the connection between spiritual well-being and physical health: an examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. J Behav Med. 2011;34(6):477-88.
489. Fitchett G, Powell LH. Daily spiritual experiences, systolic blood pressure, and hypertension among midlife women in SWAN. Ann Behav Med. 2009;37(3):257-67.
490. Buck AC, Williams DR, Musick MA, Sternthal MJ. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Soc Sci Med. 2009;68(2):314-22.
491. Suh H, Hill TD, Koenig HG. Religious Attendance and Biological Risk: A National Longitudinal Study of Older Adults. J Relig Health. 2019;58(4):1188-202.
492. Badanta-Romero B, de Diego-Cordero R, Rivilla-García E. Influence of Religious and Spiritual Elements on Adherence to Pharmacological Treatment. J Relig Health. 2018;57(5):1905-17.
493. Oliveira JA, Anderson MI, Lucchetti G, Pires EV, Gonçalves LM. Approaching Spirituality Using the Patient-Centered Clinical Method. J Relig Health. 2019;58(1):109-18.
494. Balboni TA, Fitchett G, Handzo GF, et al. State of the Science of Spirituality and Palliative Care Research Part II: Screening, Assessment, and Interventions. J Pain Symptom Manage. 2017;54(3):441-53.
495. Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.
496. Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-598.
497. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
498. Sytkowski PA, D’Agostino RB, Belanger AJ, Kannel WB. Secular trends in long-term sustained hypertension, long-term treatment, and cardiovascular mortality. The Framingham Heart Study 1950 to 1990. Circulation. 1996;93(4): 697–703.
499. Bang CN, Devereux RB, Okin PM. Regression of electrocardiographic left ventricular hypertrophy or strain is associated with lower incidence of cardiovascular morbidity and mortality in hypertensive patients independent of blood pressure reduction - A LIFE review. J Electrocardiol. 2014;47(5):630–35.
500. Fagard RH, Celis H, Thijs L, Wouters S. Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studies. Hypertension. 2009;54(5):1084–91.
501. Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45(2):198–202.
502. Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
503. Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
505. Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42-50.
506. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.
507. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427.
508. Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997;277(9):739-45.
509. . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP-Cooperative Research Group. JAMA. 1991;265(24):3255-64.
510. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcome in high-risk hypertensive patients to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;228(23):2981-97.
511. Dhalla IA, Gomes T, Yao Z, Nagge J, Persaud N, Hellings C, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158(6):447-55.
512. Hripcsak G, Suchard MA, Shea S, Chen R, You SC, Pratt N, et al. Comparison of Cardiovascular and Safety Outcomes of Chlorthalidone vs Hydrochlorothiazide to Treat Hypertension. JAMA Intern Med. 2020;180(4):542–51.
513. Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-Head Comparisons of Hydrochlorothiazide With Indapamide and Chlorthalidone. Antihypertensive and Metabolic Effects. Hypertension 2015; 65(5):1041–6.
514. Elliott WJ, Ram CV. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13(9):687-9.
515. Messerli FH. Calcium antagonists in hypertension: from hemodynamics to outcomes. Am J Hypertens. 2002;15(7 Pt 2):94S-7S.
516. Elliott WJ, Bandari A. The role of calcium antagonists in stroke prevention. J Clin Hypertens (Greenwich). 2005;7(4 Suppl 1):5-8.
517. Nathan S, Pepine CJ, Bakris GL. Calcium antagonists: effects on cardiorenal risk in hypertensive patients. Hypertension 2005;46(4):637-42.
518. Rollins G. Calcium antagonist and beta blocker regimens found equally effective in hypertensive patients with coronary artery disease. Rep Med Guidel Outcomes Res. 2004;15(2):1, 5-6.
519. Vejakama P, Thakkinstian A, Lertrattananon D, Ingsathit A, Ngarmukos C, Attia J. Reno-protective effects of renin-angiotensin system blockade in type 2 diabetic patients: a systematic review and network meta-analysis. Diabetologia 2012;55(3):566-78.
520. Baram M, Kommuri A, Sellers SA, Cohn JR. ACE inhibitor-induced angioedema. J Allergy Clin Immunol Pract. 2013;1(5):442-5.
521. Ryan MJ, Tuttle KR. Elevations in serum creatinine with RAAS blockade: why isn’t it a sign of kidney injury? Curr Opin Nephrol Hypertens. 2008;17(5):443-9.
522. Maschio G, Alberti D, Janin G, Locatelli F, Mann JF, Motolese M, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med. 1996;334(15):939-45.
523. Polifka JE. Is there an embryopathy associated with first-trimester exposure to angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists? A critical review of the evidence. Birth Defects Res A Clin Mol Teratol. 2012;94(8):576-98.
524. Laube GF, Kemper MJ, Schubiger G, Neuhaus TJ. Angiotensin-converting enzyme inhibitor fetopathy: long-term outcome. Arch Dis Child Fetal Neonatal Ed. 2007;92(5):F402-3.
525. Dahlof B, Devereux R, Kjeldsen S, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the losartan intervention or endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):995-1003.
526. Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):1004-10.
527. Julius S, Kejdelsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients in high cardiovascular risk treated with regimens based on valsartan and amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022-31.
528. Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, et al; CHARM Investigators and Committees. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM Overall programme. Lancet. 2003;362(9386):759-66.
529. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861-9.
530. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al; Collaborative Study Group. Renoprotective effect of the angiotensin receptor antagonist irbersartan in patients with nephropathy due to type 2 diabetes. N Eng J Med. 2001;345(12):851-60.
531. Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. The effect of irbersartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345(12):870-8.
532. Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
https://www.ncbi.nlm.nih.gov/books/NBK47...
533. López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al; Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62.
534. Dulin B, Abraham WT. Pharmacology of carvedilol. Am J Cardiol. 2004;93(9A):3B-6B.
535. Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269-77.
536. Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366(9496):1545-1553.
537. Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61.
538. Atlas D, Diamant S, Zonnenschein R. Is the imidazoline site a unique receptor? A correlation with clonidine-displacing substance activity. Am J Hypertens. 1992;5(4 Pt 2):83S.
539. Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
540. Wagner ML, Walters AS, Coleman RG, Hening WA, Grasing K, Chokroverty S. Randomized double-blind, placebo-controlled study of clonidine in restless legs syndrome. Sleep. 1996;19(1):52-8.
541. Bond WS. Psychiatric indications for clonidine. J Clin Psychopharmacol. 1986;6(2):81-7.
542. Pandya KJ, Raubertas RF, Flynn PJ, Hynes HE, Rosenbluth RJ, Kirshner JJ, et al. Oral clonidine in postmenopausal patients with breast cancer experiencing tamoxifen-induced hot flashes: a University of Rochester Cancer Center Community Clinical Oncology Program study. Ann Intern Med. 2000,132(10):788-93.
543. Fedorak RN, Field M, Chang EB. Treatment of diabetic diarrhea with clonidine. Ann Intern Med. 1985;102(2):197-9.
544. Esler M, Dudley F, Jennings G, Debinski H, Lambert G, Jones P, et al. Increased sympathetic nervous activity and the effects of its inhibition with clonidine in alcoholic cirrohosis. Ann Intern Med. 1992;116(6):446-55.
545. Müller DN, Derer W, Dechend R. Aliskiren-mode of action and preclinical data. J Mol Med. 2008;86(6):659-62.
546. Danser AH. (Pro)renin receptors: are they biologically relevant? Curr Opin Nephrol Hypertens. 2009;18(1):74-8.
547. Singh VP, Le B, Khode R, Baker KM, Kumar R. Intracellular angiotensin II production in diabetic rats is correlated with cardiomyocyte apoptosis, oxidative stress, and cardiac fibrosis. Diabetes. 2008;57(12):3297-306. Erratum in: Diabetes. 2009;58(3):770.
548. Musini VM, Fortin PM, Bassett K, Wright JM. Blood pressure lowering efficacy of renin inhibitors for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD007066.
549. Heerspink HJL, Persson F, Brenner BM, Chaturvedi N, Brunel P, McMurray JJ, et al. Renal outcomes with aliskiren in patients with type 2 diabetes: a prespecified secondary analysis of the ALTITUDE randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(4):309-17.
550. Bjerre HL, Christensen JB, Buus NH, Simonsen U, Su J. The role of aliskiren in the management of hypertension and major cardiovascular outcomes: a systematic review and meta-analysis. J Hum Hypertens. 2019;33(11):795-806.
551. Zhang JT, Chen KP, Guan T, Zhang S. Effect of aliskiren on cardiovascular outcomes in patients with prehypertension: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2015;9:1963-71.
552. Gradman AH, Parisé H, Lefebvre P, Falvey H, Lafeuille MH, Duh MS. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension. 2013;61(2):309-18.
553. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-Dose Combinations Improve Medication Compliance: A Meta-Analysis. Am J Med. 2007;120(8):713–9.
554. Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, et al. Benazepril plus Amlodipine or Hydrochlorothiazide for Hypertension in High-Risk Patients. N Engl J Med. 2008;359(23):2417–28.
555. Jamerson KA, Bakris GL, Weber MA. 24-Hour Ambulatory Blood Pressure in the ACCOMPLISH Trial. N Engl J Med. 2010;363(1):98–8.
556. Weber MA, Jamerson K, Bakris GL, Weir MR, Zappe D, Zhang Y, et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the ACCOMPLISH randomised controlled trial. Lancet. 2013;381(9866):537–45.
557. Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–81.
558. Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906.
559. Patel A, ADVANCE Collaborative Group, MacMahon S, Chalmers J, Neal B, Woodward M, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9500):829–40.
560. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of Hypertension in Patients 80 Years of Age or Older. N Engl J Med. 2008;358(18):1887–98.
561. Dahlöf B, Hansson L, Lindholm LH, Scherstén B, Ekbom T, Wester P-O. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281–5.
562. Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751–6.
563. Calhoun DA, Lacourcière Y, Chiang YT, Glazer RD. Triple antihypertensive therapy with amlodipine, valsartan, and hydrochlorothiazide: a randomized clinical trial. Hypertension. 2009;54(1):32-9.
564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.
565. Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, et al. The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies. Am J Hypertens. 2015;28(11):1376–85.
566. Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159-66.
567. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68.
568. Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372(9638):547–53.
569. Parving H-H, Brenner BM, McMurray JJV, de Zeeuw D, Haffner SM, Solomon SD, et al. Cardiorenal End Points in a Trial of Aliskiren for Type 2 Diabetes. N Engl J Med. 2012;367(23):2204–13.
570. Ogihara T, Saruta T, Rakugi H, Saito I, Shimamoto K, Matsuoka H, et al. Combinations of olmesartan and a calcium channel blocker or a diuretic in elderly hypertensive patients: a randomized, controlled trial. J Hypertens. 2014;32(10):2054–63.
571. Liu L, Zhang Y, Liu G, Li W, Zhang X, Zanchetti A. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens. 2005;23(12):2157–72.
572. Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757-64.
573. Liu L, Wang JG, Gong L, Liu G, Staessen JA. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. Systolic Hypertension in China (Syst-China) Collaborative Group. J Hypertens. 1998;16(12 Pt 1):1823-9.
574. Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J Clin Res 1986;293(6555):1145–51.
575. Webster R, Salam A, Silva HA, Selak V, Stepien S, Rajapakse S, et al. Fixed Low-Dose Triple Combination Antihypertensive Medication vs Usual Care for Blood Pressure Control in Patients With Mild to Moderate Hypertension in Sri Lanka: A Randomized Clinical Trial. JAMA. 2018;320(6):566–79.
576. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15.
577. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics – 2018 update: a report from the American Heart Association. Circulation. 2018 Mar 20;137(12):e67-e492.
578. Gaede P, Vedel P, Larsen N, Gunnar VH Jensen, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383-93.
579. . Hypertension in Diabetes Study (HDS): I. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertens. 1993;11(3):309-17.
580. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. Erratum in: JAMA. 2014;311(17):1809.
581. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810.
582. Niskanen L, Hedner T, Hansson L, Lanke J, Niklason A; CAPPP Study Group. Reduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/ beta-blocker-based treatment regimen: a sub analysis of the Captopril Prevention Project. Diabetes Care. 2001;24(12):2091-6.
583. Ostergren J, Poulter NR, Sever PS, Dahlof B, Wedel H, Beevers G, et al. ASCOT Investigators. The Anglo-Scandinavian Cardiac OutcomesTrial: blood pressure-lowering limb: effects in patients with type II diabetes. J Hypertens. 2008;26:2103-.11.
584. Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, et al. ACCOMPLISH Investigators. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010;56(1):77-85.
585. Tocci G, Paneni F, Palano F, Sciarretta S, Ferrucci A, Kurtz T, et al. Angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers and diabetes: a meta-analysis of placebo-controlled clinical trials. Am J Hypertens. 2011;24(5):582-90.
586. Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hipertension in the metabolic syndrome. Nutr J. 2008 Apr 17;7:10.
587. Alberti KG, Zimmet P, Shaw J. Metabolic Syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469-80.
588. Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care. 2005;28(9):2322-5.
589. Kahn R, Buse J, Ferrannini E, Stern M. The metabolic Syndrome: Time for a critical appraisal: Joint statement from American Diabetes Association and European Association for the Study of Diabetes. Diabetes Care. 2005; 84 Supll 1):3-28.
590. Gagliardi ART. Obesidade central, bases hormonais e moleculares da síndrome metabólica. Rev Soc Cardiol Estado de São Paulo. 2004;14(4):557-66.
591. Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al.Prevention of type 2 diabetes mellitus by changes in life style among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344(18):1343–50.
592. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-52. Erratum in: Circulation. 2005;112(17):e298.
593. Stears AJ, Woods SH, Watts MM, Burton TJ, Graggaber J, Mir FA, Brown MJ. A double-blind, placebo-controlled, crossover trial comparing the effects of amiloride and hydrochlorothiazide on glucose tolerance in patients with essential hypertension. Hypertension .2012; 59(5):934–42.
594. Borghi C, Bacchelli S, Degli Esposti D, Bignamini A, Magnani B, Ambrosioni E. Effects of the administration of an angiotensin-converting enzyme inhibitor during the acute pHAe of myocardial infarction in patients with arterial hypertension. SMILE Study Investigators. Survival of Myocardial Infarction Long-term Evaluation. Am J Hypertens. 1999;12(7):665-72.
595. Gustafsson F, Kober L, Torp-Pedersen C, Hildebrandt P, Ottesen MM, Sonne B, et al. Long-term prognosis after acute myocardial infarction in patients with a history of arterial hypertension. TRACE study group. Eur Heart J. 1998;19(4):588-94.
596. Arnold JM, Yusuf S, Young J. Prevention of heart failure in patients in the heart outcomes prevention evaluation (HOPE) study. Circulation. 2003;107(9):1284-90.
597. Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006;144(12):884-93.
598. Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, et al. ONTARGET investigators. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27(7):1360-9.
599. Zanchetti A, Mancia G. Longing for clinical excellence: a critical outlook into the NICE recommendations on hypertension management--is nice always good? J Hypertens. 2012;30(4):660-8.
600. Mancia G, Parati G, Bilo G, Gao P, Fagard R, Redon J, et al. Ambulatory blood pressure values in the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET). Hypertension. 2012;60(6):1400-6.
601. Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al., CLARIFY Investigators. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 2016;388(10056):2142–52.
602. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-43.
603. Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. African American Study of Kidney Disease and Hypertension Study Group: Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: Results from the AASK trial. JAMA. 2002;288(19):2421-31.
604. Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. Modification of Diet in Renal Disease Study Group: The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N Engl J Med.1994;330(13): 877-84.
605. Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(10):1498-505.
606. Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P, et al. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. 2011;29(7):1253-69.
607. Cushman WC, Evans GW, Byington RP, Goff, Jr DC, Grimm RH, Cutler JA, et. al. ACCORD Study Group: Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17): 1575-85.
608. Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, et al. VA NEPHRON-D Investigators. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 2013;369(20):1892-903.
609. Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. ACCOMPLISH Trial Investigators. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomized controlled trial. Lancet. 2010;375(9721):1173-81.
610. Foody JM, Farrell MH, Krumholz HM. beta-blocker therapy in heart failure: Scientific review. JAMA 2002;287(7): 883–9.
611. Clinical Trial. Efficacy and Safety of Finerenone in Subjects with Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (NCT02540993). US: National Institutes of Health; 2020.
612. Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and post-dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. CJASN. May 2006;1(3):389-98.
613. Silva GV, Barros S, Abensur H, Ortega KC, Mion Jr D. Cochrane Renal Group Prospective Trial Register: CRG060800146. Home blood pressure monitoring in monitoring in blood pressure control among hemodialysis patients: an open randomized clinical trial. Nephrol Dial Transplant. 2009; 24(12):3805-11.
614. Georgianos PI, Agarwal R. Blood pressure and mortality in long-term hemodialysis-time to move forward. Am J Hypertens. 2017;30(3):211-22.
615. Bansal N, McCulloch CE, Lin F, Alper A, Anderson AH, Cuevas M, et al. Blood pressure and risk of cardiovascular events in patients on chronic hemodialysis: the CRIC study (Chronic Renal Insufficiency Cohort). Hypertension. 2017;70(2):435-43.
616. Georgianos PI, Agarwal R. Systolic and diastolic hypertension among patients on hemodialysis: Musings on volume overload, arterial stiffness, and erythropoietin. Semin Dial. 2019;32(6):507-12.
617. Tada T, Kusano KF, Ogawa A, Iwasaki J, Sakuragi J, Kusano I, et al. The predictors of central and obstructive sleep apnoea in haemodialysis patients. Nephrol Dial Transplant 2007; 22:1190-7.
618. Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG, et al. Hypertension in hemodialysis patients treated with atenolol or lisinopril: A randomized controlled trial. Nephrol Dial Transplant.2014;29(3):672-81.
619. Kishnan N and Peixoto AJ. We hold antihypertensives prior to dialysis. Semin Dial. 2016 Jul;29(4):323-5.
620. Agarwal R and Sinha AD. Clinical pharmacology of antihypertensive therapy for the treatment of hypertension in chronic kidney disease. Clin J Am Soc of Nephrol 2019;14(5):757-64.
621. Cross NB, Webster AC, Masson P, O’ Connel PJ, Craig JC, et al. Antihypertensive treatment for kidney transplant recipients. Transplantation. 2009;88(1):7-18.
622. Ibrahim HN, Jackson S, Connaire J, Matas A, Ney A, Najafian B, et al. Angiotensin II blockade in kidney transplant recipients. J Am Soc Nephrol. 2013;24(2):320-7.
623. Stokes J 3rd, Kannel WB, Wolf PA, D’Agostino RB, Cupples LA. Blood pressure as a risk factor for cardiovascular disease the framingham study-30 years of follow-up. Hypertension. 1989;13(5):I-13-I–18.
624. Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5(2):167–73.
625. Goyal D, Macfadyen RJ, Watson RD, Lip GYH. Ambulatory blood pressure monitoring in heart failure: A systematic review. Eur J Heart Fail. 2005;7(2):149–56.
626. Pfeffer MA. Heart Failure and Hypertension Importance of Prevention Heart failure Randomized clinical trials Antihypertensive agents Prevention. 2017;101(1):19–28.
627. Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J Am Coll Cardiol. 1996;27(5):1214–8.
628. Tadic M, Cuspidi C, Frydas A, Grassi G. The role of arterial hypertension in development heart failure with preserved ejection fraction: just a risk factor or something more? Heart Fail Rev. 2018;23(5):631–9.
629. Kostis JB, Davis BR, Cutler J, Grimm RH, Berge KG, Cohen JD, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. J Am Med Assoc. 1997;278(3):212–6.
630. Thomopoulus C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment .6.Prevention of heart failure and new-onset heart failure–meta-analyses of randomized trials. J Hypertens. 2016;34(3):373-84.
631. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology / American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017; 136(6):e137-e161.
632. Rohde LEP, Montera MW, Bocchi EA, Clausell NO, Albuquerque DC, Rassi S, et al. Diretriz Brazileira de insuficiência cardíaca crônica e aguda. Arq Bras Cardiol. 2018;111(3):436–539.
633. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371 (11): 993-1004.
634. Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJV, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-preserved trial. Lancet. 2003;362(9386):777–81.
635. Forman D, Gaziano JM. Irbesartan in patients with heart failure and preserved ejection fraction. Curr Cardiovasc Risk Rep. 2009;3(5):311–2.
636. Cleland JGF, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27(19):2338–45.
637. Yamamoto K, Origasa H, Hori M. Effects of carvedilol on heart failure with preserved ejection fraction: The Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15(1):110–8.
638. Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
639. Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20.
640. Lee TT, Chen J, Cohen DJ, Tsao L. The association between blood pressure and mortality in patients with heart failure. Am Heart J. 2006;151(1):76-83.
641. Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43(8):1439–44.
642. Rouleau JL, Roecker EB, Tendera M, Mohacsi P, Krum H, Katus HA, et al. Influence of pretreatment systolic blood pressure on the effect of carvedilol in patients with severe chronic heart failure: The Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) study. J Am Coll Cardiol. 2004;43(8):1423–9.
643. Anand IS, Rector TS, Kuskowski M, Thomas S, Holwerda NJ, Cohn JN. Effect of baseline and changes in systolic blood pressure over time on the effectiveness of valsartan in the Valsartan Heart FailureTrial. Circ Heart Fail. 2008;1(1):34-42
644. Böhm M, Young R, Jhund PS, Solomon SD, Gong J, Lefkowitz MP, et al. Systolic blood pressure, cardiovascular outcomes and efficacy and safety of sacubitril/ valsartan (LCZ696) in patients with chronic heart failure and reduced ejection fraction: Results from PARADIGM-HF. Eur Heart J. 2017;38(15):1132-43.
645. Rashid P. Leornardi-Bee J. Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34(11):2741-8.
646. PATS Collaborating Group. Poststroke antihypertensive treatment study: a preliminary result. Chin Med J (Engl). 1995;108(9):710-7.
647. Gueyffier F, Boissel JP, Boutitie F, Pocock S, Coope J, Cutler J, et al. Effect of antihypertensive treatment in patients having already suffered from stroke. Gathering the evidence. The INDANA (IN-dividual Data Analysis of Antihypertensive intervention trials) Project Collaborators. Stroke. 1997;28(12):2557-62.
648. Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32(11):1032-40.
649. Schrader J, Luders S, Kulschewski A, Hammersen F, Plate K, Berger J, et al; MOSES Study Group. Morbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES). Stroke. 2005;36(6):1218-26.
650. Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, et al; ProFESS Study Group. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med. 2008;359(12):1225-37.
651. White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, et al; SPS3 Investigators. Blood pressure after recent stroke: baseline findings from the secondary prevention of small subcortical strokes trial. Am J Hypertens. 2013;26(9):1114-22.
652. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
653. Rodriguez-Luna D, Pineiro S, Rubiera M, Ribo M, Coscojuela P, Pagola J, et al. Impact of blood pressure changes and courseon hematoma growth in acute intracerebral hemorrhage. Eur J Neurol.2013;20(9):1277–83.
654. Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al, INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355–65.
655. Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, et al. Relationship of blood pressure, antihypertensive therapy, and outcome inischemic stroke treated with intravenous thrombolysis: retrospective analysisfrom Safe Implementation of Thrombolysis in Stroke-International StrokeThrombolysis Register (SITS-ISTR). Stroke. 2009;40(7):2442–9.
656. Wu W, Huo X, Zhao X, Liao X, Wang C, Pan Y, et al.Relationship between blood pressure and outcomes in acute ischemic strokepatients administered lytic medication in the TIMS-China Study. PLoS One.2016;11(2):e0144260.
657. Lee M, Ovbiagele B, Hong KS, Wu YL, Lee JE, Rao NM, et al. Effect of blood pressure lowering in early ischemic stroke: meta-analysis. Stroke. 2015;46(7):1883-9.
658. Zhao R, Liu FD, Wang S, Peng JL, Tao XX, Zheng B, et al. Blood pressure reduction in the acute phase of an ischemic stroke does not improve short- or longtermdependency or mortality: a meta-analysis of current literature. Medicine(Baltimore) 2015;94(23):e896.
659. Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and out-comes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206(2):134.e1–8.
660. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–44.
661. Ramos JGL, Sass N, Costa SHM. Preeclampsia. Rev Bras Ginecol Obstet. 2017;39(9):496–512.
662. Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):1–7.
663. Giordano JC, Parpinelli MA, Cecatti JG, Haddad SM, Costa ML, Surita FG, et al. The burden of eclampsia: results from a multicenter study on surveillance of severe maternal morbidity in Brazil. PLoS One. 2014;9(5):e97401.
664. . American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019 Jan;133(1):e1-e25.
665. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.
666. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291-310.
667. Hofmey GJ, Lawrie TA, Atallah ÁN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014; 6:CD001059.
668. . CLASP: a randomized trial of low-dose aspirin for the prevention and treatment of pre-eclampsia among 9364 pregnant women. CLASP (Collaborative Low dose Aspirin Study in Pregnancy) Collaborative Group. Lancet. 1994; 343(8898):619–29.
669. Duley L, Henderson-Damart DJ, Meher S, King JF. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database of Syst Rev.2004;(1): CD 004659.
670. Rolnik DL, Wright D, Poon L, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk of preterm preeclampsia. N Engl J Med. 2017;377(7):613–22.
671. Hypertension in pregnancy: diagnosis and management NICE guideline Published: 25 June 2019.[Internet] [Cited in 2019 may 23] Available at: www.nice.org.uk/guidance/ng133 .
www.nice.org.uk/guidance/ng133...
672. World Health Organization. WHO. Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia. Geneve: 2011.
673. Poon LC, Shennan A, Hyett JA, Kapur A, Hadar E, Divakar H, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(Suppl 1):1-33.
674. American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180.
675. Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressure. Obstet Gynecol. 2005;105(2):246-54.
676. Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG . 2011;118 (Suppl 1):1-203.
677. Meher S, Abalos E, Carroli G. Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database Syst Rev. 2005;19(4):CD003514.
678. Dowswell T, Middleton P, Weeks A. Antenatal day care units versus hospital admission for women with complicated pregnancy. Cochrane Database of Syst Rev. 2009;(4):CD001803.
679. Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG. Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88.
680. Broekhuijsen K, van Baaren GJ, van Pampus MG, Ganzevoort W, Sikkema JM, Woiski MD, et al. Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. Lancet. 2015;385(9986):2492-501.
681. Ronsmans C, Campbell O. Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health. 2011;11(Suppl 3):S8.
682. Peraçoli JC, Borges VTM, Ramos JG, Cavalli RC, Costa SHAM, Oliveira LG, et al. Pre-eclampsia/Eclampsia. Rev Bras Ginecol Obstet. 2019;41(5):318-32.
683. Duley L, Henderson-Smart DJ, Meher S. Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev. 2006;(3):CD001449.
684. Centers for disease control and prevention. Postmarketing surveillance for angiotensin-converting enzyme inhibitor use during the first trimester of pregnancy – United States, Canada and Israel, 1987-1995. JAMA. 1997; 277(15):1193-4.
685. Abalos E, Duley L, Steyn DW. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database of Syst Rev. 2014;6(2): CD002252.
686. Magee LA, von Dadelszen P, Rey E, Ross S, Asztalos E, Murphy KE, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372(5):407-17.
687. Magee LA, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, et al. The CHIPS randomized controlled trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood pressure? Hypertension. 2016;68(5):1153-9.
688. Butalia S, Audibert F, Côté AM, Firoz T, Logan AG, Magee LA, et al. Hypertension Canada’s 2018. Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34(5):526-31.
689. Easterling T, Mundle S, Bracken H, Parvekar S, Mool S, Magee LA, et al. Oral antihypertensive regimens (nifedipine retard, labetalol, and methyldopa) for management of severe hypertension in pregnancy: an open-label, randomised controlled trial. Lancet 2019;394(10203):1011-21.
690. Sass N, Itamoto CH, Silva MP, Torloni MR, Atallah NA. Does sodium nitroprusside kill babies? A systematic review. Sao Paulo Med J. 2007;125:108-11.
691. Townsend R, O’Brien P, Khalil A. Current best practice in the management of hypertensive disorders in pregnancy. Integr Blood Press Control. 2016:9,79-94.
692. Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-[Internet] [Cited in 2019 May 12] . Available from: https://www.ncbi.nlm.nih.gov/books/NBK501922/ .
https://www.ncbi.nlm.nih.gov/books/NBK50...
693. Regit-Azgrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018; 39(34):3165–241.
694. Halpern DG, Weinberg CR, Pinnelas R, Mehta-Lee S, Economy KE, Valente AM. Use of Medication for Cardiovascular Disease During Pregnancy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(4):457-76.
695. Noronha Neto C C, Maia SSB, Katz L, Coutinho IC, Souza AR, Amorim MM. Clonidine versus Captopril for Severe Postpartum Hypertension: A Randomized Controlled Trial. Plos One. 2017;12(1):e0168124.
696. Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366(9499):1797–803.
697. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
698. Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, et al. Long-Term Cardiovascular Risk in Women With Hypertension During Pregnancy. J Am Coll Cardiol. 2019;74(22):2743-54.
699. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800-9.
700. Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113(3 Pt 1):475-82.
701. McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and prehypertension among adolescents. J Pediatr. 2007;150(6):640-4.
702. Brian KK, Elena K, Margaret DC, Yachim O, David SF, Cynthia LO. Prevalence of and trends in dyslipidemia and blood pressure among us child and adolescents 1999-2012. Jama Pediatr. 2015: 169(3):272-9.
703. Bloch VK, Klein CH, Szklo M, Kuschnir MCC et al. Prevalências de hipertensão arterial e obesidade Brazileiros. Rev. Saúde Pública. 2016: 50(supl 1)1-13.
704. Brady TM, Redwine KM, Flynn JT; American Society of Pediatric Nephrology. Screening blood pressure measurement in children: are we saving lives? Pediatr Nephrol. 2014;29(6):947-50.
705. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
706. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98(4 Pt 1):649–58.
707. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114(2):555-76.
708. Kulaga Z, Litwin M, Grajda A, Kułaga K, Gurzkowska B, Gó´zd´zM, et al. Oscillometric blood pressure percentiles for Polish normal-weight school-aged children and adolescents. J Hyper-tens. 2012;30(10):1942-54.
709. Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS. Blood pressure percentiles by age and height from nonover-weight children and adolescents in Germany. Pediatrics.2011;127(4):e978-88.
710. Jardim TV, Rosner B, Bloch KV, Kuschnir MC, Szklo M, Jardim PC. Blood pressure reference values for Brazilian adolescents: data from the Study of Cardiovascular Risk in Adolescents (ERICA Study). J Pediatr. 2020;96(2):168-76.
711. Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome [published correction appears in Pediatr Nephrol. 2012;27(1):159-60]. Pediatr Nephrol. 2012;27(1):17–32.
712. Report of the second task force on blood pressure control in children–1987. Task force on blood pressure control in children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics. 1987;79(1):1–25.
713. Guimarães IC, Almeida AM, Santos AS, Barbosa DB, Guimarães AC. Blood pressure: effect of body mass index and of waist circumference on adolescents. Arq Bras Cardiol. 2008;90(6):426-32.
714. Daniels Sr. Coronary risk factors in children. In: Moss & Adams. Heart disease in infants, children and adolescents. Philadelphia: Williams & Wilkins; 2013. p. 1514-48.
715. Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al; European Society of Hypertension. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens. 2009;27(9):1719-42.
716. Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, Zachariah JP, Urbina EM Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014 ;63(5):1116-35.
717. Hansen HS, Hyldebrandt N, Froberg K, Nielsen JR. Blood pressure and physical fitness in a population of children—the Odense Schoolchild Study. J Hum Hypertens. 1990;4(6):615-20.
718. McCambridge TM, Benjamin HJ, Brenner JS, Cappetta CT, Demorest RA, Gregory AJ, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension Pediatrics. 2010;125(6):1287-94.
719. Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M. Sodium intake and blood pressure in children with clinical conditions: A systematic review with meta-analysis. J Clin Hypertens (Greenwich). 2019 Jan;21(1):118-126.
720. Bricarello P L, Poltronieri F, Fernandes R, Retondario A, Morais EBST, Vasconcelos FAG. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin Nutr ESPEN. 2018 Dec;28:1-11.
721. Miller JZ, Wienberger MH, Christian JC. Blood pressure response to potassium supplement in normotensive adults and children. Hypertension. 1987;10(4):437-42.
722. Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580.
723. Prichard BN, Cruickshank JM, Graham BR. Beta-adrenergic blocking drugs in the treatment of hypertension. Blood Press. 2001;10(5-6):366-86.
724. Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD. Pregnancy outcome following exposure to angiotensin converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension. 2012;60(2):444-50.
725. Ferguson MA, Flynn JT. Rational use of antihypertensive medications in children. Pediatr Nephrol. 2014;29(6):979-88.
726. Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14(6):383-7.
727. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, et al; Hypertension Canada. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018 May;34(5):506-25.
728. . 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887-920.
729. Wu HP, Yang WC, Wu YK, Zhao L, Chen CY, Fu YC. Clinical significance of blood pressure ratios in hypertensive crisis in children. Arch Dis Child. 2012; 97(3):200–5.
730. Chandar J, Zilleruelo G. Hypertensive crisis in children. Pediatr Nephrol. 2012: 27(5):741-51.
731. Yang WC, Zhao LL, Chen CY, Wu YK, Chang YJ, Wu HP. First-attack pediatric hypertensive crisis presenting to the pediatric emergency department. BMC Pediatrics. 2012; 12:200.
732. . The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153(2):154-83.
733. Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9.
734. Martin JFV, Ribeiro JM. Urgências e Emergências Hipertensivas. In: Moreira MC, Montenegro ST, Paola AAV, eds. Livro Texto da Sociedade Brazileira de Cardiologia. 2 ed. Barueri (SP): Manole; 2015. P.922-30.
735. Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83(2):131-6; 125-30.
736. Pinna G, Pascale C, Fornengo P, Arras S, Piras C, Panzarasa P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS One. 2014;9(4):e93542.
737. Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo AN, Yugar-Toledo JC. Hypertensive crisis: clinical-epidemiological profile. Hypertens Res. 2011;34(3):367-71.
738. Pierin AMG, Flórido CF, Santos JD. Hypertensive crisis: clinical characteristics of patients with hypertensive urgency, emergency and pseudocrisis at a public emergency department. Einstein (Sao Paulo). 2019;17(4):eAO4685.
739. Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci.1974;268(6):336–45.
740. Velasco I, Cuadrado L, Fontana A, Reijaili WA, Balbi AL, Barretti P, Franco RJS. Cuadro clínico y evolución de 77 pacientes con hipertensión arterial maligna: comparación de dos épocas y de diferentes niveles de creatinina. Nefrologia. 1993;13 (Suppl 5):8-13.
741. Almeida FA, Stella RC, Voos A, Ajzen H, Ribeiro AB. Malignant hypertension: a syndrome associated with low plasma kininogen and kinin potentiating factor. Hypertension. 1981;3(6 Pt 2):II-46-9.
742. Ault MJ, Ellrodt AG. Pathophysiologic events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10–5.
743. Strandgaard S, Paulson O. Cerebral autoregulation. Stroke. 1984;15(3):413–6.
744. Martin JFV, Kuniyoshi CH, Andrade LG, Yugar-Toledo JC, Loureiro AC, Cipullo JP. Fatores Preditores de Mortalidade em Pacientes com Crise Hipertensiva. Arq Bras Cardiol. 2007;89(Supl 1): 201.
745. Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996; 276(16):1328-31.
746. CREMESP elabora parecer sobre uso de nifedipina. 2004. [citado 2020 Jul 15]. Disponível em: https://www.cremesp.org.br/?siteAcao=Jornal&id=323 .
https://www.cremesp.org.br/?siteAcao=Jor...
747. Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.
748. van den Born BH, Lip GYH, Brguljan-Hitij J, Cremer A, Segura J, Morales E, et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur Heart J Cardiovasc Pharmacother. 2019;5(1):37-46.
749. O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–75.
750. Truelsen T, Heuschmann PU, Bonita R, Arjundas G, Dalal P, Damasceno A, et al. Standard method for developing stroke registers in low-income and middle-income countries: experiences from a feasibility study of a stepwise approach to stroke surveillance (STEPS Stroke). Lancet Neurol. 2007;6(2):134-9.
751. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306.
752. Hemphill, J.C., 3rd, et al., Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2015. 46(7): 2032-60.
753. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2): 119–77.
754. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association for Clinical Chemistry. 2014 AHA/ACC Guideline for the management of patients with non–ST-elevation acute coronary syndromes. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-228.
755. Gandhi SK, Powers JC, Nomeir AM, Fowle K, Kitzman DW, Rankin KM, et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med. 2001;344(1):17-22.
756. Kumar R, Gandhi SK, Little WC. Acute heart failure with preserved systolic function. Crit Care Med. 2008;36(1 Suppl):pS52-6.
757. Comitê Coordenador da Diretriz de Insuficiência Cardíaca da Sociedade Brazileira de Cardiologia; Rohde LEP, Montera MW, Bocchi EA, Albuquerque DC, Clausell NO, Rassi S, et al. Diretriz Brazileira de Insuficiência Cardíaca Crônica e Aguda. Arq Bras Cardiol. 2018;111(3):436-539.
758. Bossone E, La Bounty TM, Eagle KA. Acute aortic syndromes: Diagnosis and management, an update. Eur Heart J. 2018;39(9):739−49.
759. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Dis. 2003;5(4):253-71.
760. Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201.
761. Lester SJ, Baggott M, Welm S, et al. Cardiovascular effects of 3, 4-methylenedioxy-methamphetamine. A double-blind, placebo-controlled trial. Ann Intern Med. 2000;133(12):969–73.
762. Gahlinger PM. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004;69(11):2619-27.
763. Lange RA, Ciggarroa RG, Flores ED, McBride W, Kim AS, Wells PJ, et al. Potentiation of cocaine induced coronary vasoconstriction by beta adrenergic blockade. Ann Intern Med. 1990;112(12):897–903.
764. Tuncel M, Wang Z, Arbique D, Fadel PJ, Victor RG, Vongpatanasin W. Mechanism of the blood pressure-raising effect of cocaine in humans. Circulation. 2002;105(9):1054-9.
765. Sofuoglu M, Brown S, Babb DA, Pentel PR, Hatsukami DK. Carvedilol affects the physiological and behavioral response to smoked cocaine in humans. Drug Alcohol Depend. 2000; 60(1):69-76.
766. Sordo L, Indave BI, Barrio G, Degenhardt L, de la Fuente L, Bravo MJ. Cocaine use and risk of stroke: a systematic review. Drug Alcohol Depend. 2014;142:1-13.
767. Wilson LD, Jeromin J, Garvey L, Dorbandt A. Cocaine, ethanol, and cocaethylene cardiotoxicity in an animal model of cocaine and ethanol abuse. Acad Emerg Med. 2001;8(3):211–22.
768. Mehta MC, Jain AC, Billie M. Effects of cocaine and alcohol alone and in combination on cardiovascular performance in dogs. Am J Med Sci. 2002;324(2):76–83.
769. Wilkerson RD. Cardiovascular effects of cocaine: enhancement by yohimbine and atropine. J Pharmacol Exp Ther. 1989;248(1):57–61.
770. Perez-Reyes M, Jeffcoat AR. Ethanol/cocaine interactions: cocaine and cocaethylene plasma concentrations and their relationship to subjective and cardiovascular effects. Life Sci. 1992;51(8):553–63.
771. Melchert RB, Eselin JA, O’Dell JF, Welder AA. Effects of nitrendipine on cocaine induced toxicity evaluated in primary myocardial cell cultures. J Pharmaceut Sci. 1991;80(7):700–4.
772. Bortolotto LA. Hipertensão acelerada-maligna. Rev Bras Hipertens. 2014;21(4):203-8.
773. Ahmed ME, Walker JM, Beevers DG, Beevers M. Lack of difference between malignant and accelerated hypertension. Br Med J (Clin Res Ed). 1986;292(6515):235-7.
774. Kincaid-Smith P, McMichael J, Murphy EA. The clinical course and pathology of hypertension with papilloedema (malignant hypertension). Q J Med. 1958;27(105):117-53.
775. Clough C, Beevers D, Beevers M. The survival of malignant hypertension in blacks, whites and Asians in Britain. J Hum Hypertens. 1990;4(2):94-6.
776. Lip G, Beevers M, Beevers D. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens. 1995;13(8):915-24.
777. Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, et al. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30(8):463-6.
778. Ma H, Jiang M, Fu Z, Wang Z, Shen P, Shi H, et al. Clinical value of multiorgan damage in hypertensive crises: A prospective follow-up study. J Clin Hypertens. (Greenwich). 2020;22(5):914-23.
779. Lip GY, Beevers M, Dodson PM, Beevers DG. Severe hypertension with lone bilateral papilloedema: a variant of malignant hypertension. Blood Press. 1995;4(6):339-42.
780. Amraoui F, van Montfrans GA, van den Born BJ. Value of retinal examination in hypertensive encephalopathy. J Hum Hypertens. 2010;24(4):274-9.
781. World Health Organization. (WHO). World Report on Ageing and Health 2015. [Cited in 2020 Feb 10]. Available from: http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 .
http://apps.who.int/iris/bitstream/10665...
782. United Nations. Department of Economic and Social Affairs Population Division. World Population Ageing 2015. [Cited in 2019 Feb 10] Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf .
http://www.un.org/en/development/desa/po...
783. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity andimplications for health care, research, and medical education: a cross-sectional study. The Lancet. 2012; 380 (9836): 37-43.
784. Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing 2017; 46 (6): 882–8.
785. Nunes BP, Batista SRR, Andrade FB, Souza Junior PRB, Lima-Costa MF, Facchini LA. Multimorbidity: The Brazilian Longitudinal Study of Aging (ELSI-Brazil). Rev Saude Publica. 2018;52(Suppl 2):10s.
786. Peters R, Beckett N, McCormack T, Fagard R, Fletcher A, Bulpitt C. Treating hypertension in the very elderly—benefits, risks, and future directions, a focus on the hypertension in the very elderly trial. Eur Heart J. 2014; 35 (26):1712-8.
787. Iadecola C. Hypertension and Dementia. Hypertension. 2014; 64 (1): 3-5.
788. Costa Filho AM, Mambrini JVM, Malta DC, Lima-Costa MF, Peixoto SV. Contribution of chronic diseases to the prevalence of disability in basic and instrumental activities of daily living in elderly Brazilians: the National Health Survey (2013). Cad. Saúde Pública (Online) 2018; 34(1):e00204016.
789. Kelly R, Hayward C, Avolio A, O’Rourke M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation 1989; 80 (6): 1652–9.
790. Franklin SS, Gustin Wt, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308-15.
791. Pearson JD, Morrell CH, Brant LJ, Landis PK, Fleg JL. Age-associated changes in blood pressure in a longitudinal study of healthy men and women. J Gerontol A Biol Sci Med Sci. 1997;52(3):M177-83.
792. Lakatta EG. Central arterial aging and the epidemic of systolic hypertension and atherosclerosis. J Am Soc Hypertens. 2007;1(5):302-40.
793. O’Rourke MF, Nichols WW. Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension. 2005;45(4):652-8.
794. Niiranen TJ, Lyass A, Larson MG, Hamburg NM, Benjamin EJ, Mitchell GF, et al. Prevalence, Correlates, and Prognosis of Healthy Vascular Aging in a Western Community-Dwelling Cohort: The Framingham Heart Study. Hypertension. 2017;70(2):267-74.
795. Freitas EGB, Souza DF, Ferreira-Filho SR. Probability of At Least One High Arterial Blood Pressure Measurement in Elderly Patients with Healthy Vascular Aging in Two Years of Follow-Up. Kidney Blood Press Res. 2018;43(6):1765-71.
796. de Mendonca GS, de Souza DF, de Alvarenga Cunha Brunelli AC, de Oliveira Peres CI, Freitas EGB, Lacerda GN, et al. Arterial stiffness in elderly patients with normotension and hypertension in Brazil. J Clin Hypertens (Greenwich). 2018;20(9):1285-93.
797. Benetos A, Gautier S, Labat C, et al. Mortality and Cardiovascular Events Are Best Predicted by Low Central/Peripheral Pulse Pressure Amplification But Not by High Blood Pressure Levels in Elderly Nursing Home Subjects: the PARTAGE (Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Population) study. J Am Coll Cardiol. 2012;60 (16):1503-11.
798. Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.
799. Quinn TJ, McArthur K, Ellis G, Stott DJ. Functional assessment in older people. BMJ. 2011;343:d4681.
800. Benetos A, Petrovic M, Strandberg T. Hypertension Management in Older and Frail Older Patients. Circ Res. 2019;124(7):1045-60.
801. Campana EMG; Freitas EV, Brandão AA et al. Hipertensão Arterial no Idoso. In: Freitas EV, Py L, eds. Tratado de Geriatria e Gerontologia. Rio de Janeiro: GEN. 2016;p 507-21.
802. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-98.
803. Corrao G, Rea F, Monzio Compagnoni M, Merlino L, Mancia G. Protective effects of antihypertensive treatment in patients aged 85 years or older. J Hypertens. 2017;35(7):1432-1.
804. Hansson L, Lithell H, Skoog I, Baro F, Banki CM, Carbonin PU, et al. Study on COgnition and Prognosis in the Elderly (SCOPE). Blood Press; 1999; 8(3):177-83.
805. Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683–9.
806. White WB, Wakefield DB, Moscufo N, et al. Effects of Intensive Versus Standard Ambulatory Blood Pressure Control on Cerebrovascular Outcomes in Older People (INFINITY). Circulation. 2019;140(20):1626–35.
807. Feitosa-Filho GS, Peixoto JM, Pinheiro JES, et al. Updated Geriatric Cardiology Guidelines of the Brazilian Society of Cardiology - 2019. Arq Bras Cardiol. 2019;112(5):649-705.
808. Butrous H, Hummel SL. Heart Failure in Older Adults. Can J Cardiol. 2016;32(9):1140-7.
809. Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Juni P, Carrel T, et al. Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):489-96.
810. Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group [published correction appears in JAMA 1998 Jun 24;279(24):1954]. JAMA. 1998;279(11):839–46.
811. Mente A, O’Donnell MJ, Rangarajan S, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371(7):601-11.
812. Bangalore S, Messerli FH, Kostis JB, Pepine CJ. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol. 2007;50(7):563-72.
813. Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2017;1(1):CD002003.
814. Finks SW, Rumbak MJ, Self TH. Treating Hypertension in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2020;382(4):353-63.
815. Isik AT, Soysal P, Stubbs B. Cardiovascular Outcomes of Cholinesterase Inhibitors in Individuals with Dementia: A Meta-Analysis and Systematic Review. J Am Geriatr Soc. 2018;66(9):1805-11.
816. Kahlaee HR, Latt MD, Schneider CR. Association Between Chronic or Acute Use of Antihypertensive Class of Medications and Falls in Older Adults. A Systematic Review and Meta-Analysis. Am J Hypertens. 2018;31(4):467-79.
817. Ang HT, Lim KK, Kwan YH, Há YC, Lim JY. A Systematic Review and Meta-Analyses of the Association Between Anti-Hypertensive Classes and the Risk of Falls Among Older Adults. Drugs Aging. 2018;35(7):625-35.
818. Mühlbauer V, Dallmeier D, Brefka S, Bollig C, Voigt-Radloff S, Denkinger M: The pharmacological treatment of arterial hypertension in frail, older patients— a systematic review. Dtsch Arztebl Int 2019; 116: 23–30.
819. Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406.
820. Delgado J, Masoli JAH, Bowman K, et al. Outcomes of Treated Hypertension at Age 80 and Older: Cohort Analysis of 79,376 Individuals. J Am Geriatr Soc. 2017;65(5):995–1003.
821. Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.
822. Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE Study. JAMA Intern Med. 2015;175(6):989–995.
823. Wu C, Smit E, Peralta CA, Sarathy H, Odden MC. Functional Status Modifies the Association of Blood Pressure with Death in Elders: Health and Retirement Study. J Am Geriatr Soc. 2017;65(7):1482–1489.
824. Soobiah C, Daly C, Blondal E, Ewusie J, Ho J, Elliott MJ, Yue R, Holroyd-Leduc J, Liu B, Marr S, Basran J, Tricco AC, Hamid J, Straus SE. An evaluation of the comparative effectiveness of geriatrician-led comprehensive geriatric assessment for improving patient and healthcare system outcomes for older adults: a protocol for a systematic review and network meta-analysis. Syst Rev. 2017 Mar 24;6(1):65.
825. Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.
826. Rockwood K, Song X, Mitnitski A: Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. CMAJ 2011; 183: E487–94.
827. Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668-1676.
828. Studenski S, Perera S, Patel K, Rosano C, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50.
829. Odden MC, Moran AE, Coxson PG, Peralta CA, Goldman L, Bibbins-Domingo K. Gait Speed as a Guide for Blood Pressure Targets in Older Adults: A Modeling Study. J Am Geriatr Soc. 2016;64(5):1015–1023.
830. Rodrigues, M.K., Nunes Rodrigues, I., Vasconcelos Gomes da Silva, D.J. et al. Clinical Frailty Scale: Translation and Cultural Adaptation Into the Brazilian Portuguese Language. J Frailty Aging 2020: in press. Published online Feb 14, 2020 7.
831. Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9.
832. Chong E, Ho E, Baldevarona-Llego J, Chan M, Wu L, Tay L. Frailty and Risk of Adverse Outcomes in Hospitalized Older Adults: A Comparison of Different Frailty Measures. J Am Med Dir Assoc. 2017 Jul;18(7):638.e7-.e11.
833. Atkins JL, Delgado J, Pilling LC, et al. Impact of Low Cardiovascular Risk Profiles on Geriatric Outcomes: Evidence From 421,000 Participants in Two Cohorts. J Gerontol A Biol Sci Med Sci. 2019;74(3):350–357.
834. Nadruz W Jr, Kitzman D, Windham BG, et al. Cardiovascular Dysfunction and Frailty Among Older Adults in the Community: The ARIC Study. J Gerontol A Biol Sci Med Sci. 2017;72(7):958–964.
835. Aprahamian, I, Sassaki, E, dos Santos, MF, et al. Hypertension and frailty in older adults. J Clin Hypertens. 2018; 20: 186– 192.
836. Ravindrarajah R, Hazra NC, Hamada S, et al. Systolic Blood Pressure Trajectory, Frailty, and All-Cause Mortality >80 Years of Age: Cohort Study Using Electronic Health Records. Circulation. 2017;135(24):2357–68.
837. Gulla C, Flo E, Kjome RL, Husebo BS. Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. J Geriatr Cardiol. 2018;15(4):275–283.
838. Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78. Published 2015 Apr 9.
839. Russo, G., Liguori, I., Aran, L. et al. Impact of SPRINT results on hypertension guidelines: implications for “frail” elderly patients. J Hum Hypertens 32, 633–638 (2018). https://doi.org/10.1038/s41371-018-0086-6
https://doi.org/10.1038/s41371-018-0086-...
840. Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–517.
841. Abell JG, Kivimäki M, Dugravot A, et al. Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertension. Eur Heart J. 2018;39(33):3119–3125.
842. Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, Coresh J, Knopman D, Power MC, Rawlings A, Sharrett AR, Wruck LM, Mosley TH. Midlife hypertension and 20-year cognitive change: the atherosclerosis risk in communities neurocognitive study. JAMA Neurol. 2014;71:1218–1227.
843. Iadecola C, Gottesman RF. Neurovascular and Cognitive Dysfunction in Hypertension. Circ Res. 2019;124(7):1025–1044.
844. Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–2263.
845. Flores LM, Mengue SS. Drug use by the elderly in Southern Brazil. Rev Saúde Pública. 2005; 39(6): 924-9.
846. Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17(4):123–132.
847. Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23.
848. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
849. Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of Discontinuation of Antihypertensive Treatment in Elderly People on Cognitive Functioning--the DANTE Study Leiden: A Randomized Clinical Trial [published correction appears in JAMA Intern Med. 2016 Feb;176(2):284]. JAMA Intern Med. 2015;175(10):1622–1630.
850. Luymes CH, Poortvliet RKE, van Geloven N, et al. Deprescribing preventive cardiovascular medication in patients with predicted low cardiovascular disease risk in general practice - the ECSTATIC study: a cluster randomised non-inferiority trial. BMC Med. 2018;16(1):5.
851. Gibbons CH, Schmidt P, Biaggioni I, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264(8):1567–1582.
852. Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. Hypertension 1992;19:508.
853. Jansen RW, Lipsitz LA. Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med 1995;122:286.
854. Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study [published correction appears in J Am Geriatr Soc. 2011 May;59(5):960]. J Am Geriatr Soc. 2011;59(3):383–389.
855. Margolis KL, Palermo L, Vittinghoff E, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med. 2014;29(12):1599–1606.
856. Juraschek SP, Taylor AA, Wright JT Jr, et al. Orthostatic Hypotension, Cardiovascular Outcomes, and Adverse Events: Results From SPRINT. Hypertension. 2020;75(3):660–667
857. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-312.
858. Charles L, Triscott J, Dobbs B. Secondary Hypertension: Discovering the Underlying Cause. Am Fam Physician. 2017;96(7):453-61.
859. Hirsch JS, Hong S. The Demystification of Secondary Hypertension: Diagnostic Strategies and Treatment Algorithms. Current Treatment Options in Cardiovascular Medicine. 2019;21(12):90.-860860. Siddiqui MA, Mittal PK, Little BP, Miller FH, Akduman EI, Ali K, et al. Secondary Hypertension and Complications: Diagnosis and Role of Imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 2019;39(4):1036-55. ( Chart 15.1 ).
The main causes of secondary hypertension, discussed in this chapter, are shown in Figure 151 . Diagnostic investigation can focus on the age of the patient and the type of sign, as seen in Chart 15.2 . Patients with secondary HT are under higher CV and renal risk and have more end-organ damage due to higher and more sustained BP levels, as well as the activation of hormonal and molecular mechanisms. 859859. Hirsch JS, Hong S. The Demystification of Secondary Hypertension: Diagnostic Strategies and Treatment Algorithms. Current Treatment Options in Cardiovascular Medicine. 2019;21(12):90.,861861. Cingolani OH. Cardiovascular Risks and Organ Damage in Secondary Hypertension. Endocrinol Metab Clin North Am. 2019;48(4):657-66.
15.2. Nonendocrine Causes
15.2.1. Chronic Kidney Disease (CKD)
CKD is defined by its cause and by functional or morphological abnormalities persisting for over three months with consequences for the patient's health. It is characterized by an estimated glomerular filtration rate (eGFR) < 60 mL/min or alterations in urine tests, especially albuminuria (30 mg/24 h or 30 mg/g albumin/creatinine ratio) and/or in renal morphology (LR: I; LE: C). 862862. . Summary of Recommendation Statements. Kidney Int Suppl (2011). 2013;3(1):5-14. CKD classification and prognosis are based on eGFR and albuminuria levels (Chapter 4). HT is both cause and consequence of CKD and becomes progressively worse as kidney function declines, affecting 90% of stage 5 patients (LR: I; LE: A). 863863. Pugh D, Gallacher PJ, Dhaun N. Management of Hypertension in Chronic Kidney Disease. Drugs. 2019;79(4):365-79.,864864. Sinha AD, Agarwal R. Clinical Pharmacology of Antihypertensive Therapy for the Treatment of Hypertension in CKD. Clinical Journal of the American Society of Nephrology. 2019;14(5):757-64.
Tests for hypertensive patients should include serum creatinine and eGFR calculation (LR: I; LE: B) as well as urine test (LR: I; LE: C) for CKD screening. 859859. Hirsch JS, Hong S. The Demystification of Secondary Hypertension: Diagnostic Strategies and Treatment Algorithms. Current Treatment Options in Cardiovascular Medicine. 2019;21(12):90. Renal ultrasound, computed tomography (CT), or magnetic nuclear resonance (MNR) may also be necessary. Kidney biopsies are only required when there are rapid declines in eGFR, glomerular hematuria, and/or proteinuria/albuminuria in addition to HT. 865865. . Chapter 2: Definition, identification, and prediction of CKD progression. Kidney Int Suppl (2011). 2013;3(1):63-72. HT accelerates the progression of CKD, and lowering BP attenuates the course of CKD. 863863. Pugh D, Gallacher PJ, Dhaun N. Management of Hypertension in Chronic Kidney Disease. Drugs. 2019;79(4):365-79.,864864. Sinha AD, Agarwal R. Clinical Pharmacology of Antihypertensive Therapy for the Treatment of Hypertension in CKD. Clinical Journal of the American Society of Nephrology. 2019;14(5):757-64. Treatment goals and therapy regimens indicated for BP control in CKD patients can be found in Chapters 6 through 9.
15.2.2. Renovascular Hypertension (RVH)
Renovascular hypertension (RVH) is a common and potentially reversible cause of secondary HT due to partial or total, uni- or bilateral renal artery stenosis (RAS) or of one of its branches, triggered and maintained by significant renal ischemia. It is usually found in obstructions greater than 70%. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. Its prevalence and etiology vary with age and blood pressure levels. In young adults, especially women, RVH is more frequently caused by fibromuscular dysplasia (FMD). In older adults, the most common cause is atherosclerosis, usually accompanied by peripheral and/or coronary atherosclerosis. 866866. Herrmann SM, Textor SC. Current Concepts in the Treatment of Renovascular Hypertension. Am J Hypertens. 2018;31(2):139-49. The clinical indicators of RVH can be found in Chart 15.3 .
In patients with potential signs of RVH, the physician should consider diagnostic tests for those with fewer morbidities for whom revascularization treatment is indicated. 867867. Aboyans V, Ricco JB, Bartelink MEL, Bjorck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763-816.,868868. Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(13):1425-43. Renovascular disease has heterogenous clinical manifestations. The damage may evolve with minimal or even silent hemodynamic repercussions before progressing to critical levels associated with triggering hypertensive physiopathological mechanisms and renal ischemia. Revascularization procedures are indicated for FMD patients and patients with atherosclerotic etiology who cannot control BP or are suffering progressive loss of renal function or decompensated heart failure (acute pulmonary edema, heart failure and refractory angina). 869869. Parikh SA, Shishehbor MH, Gray BH, White CJ, Jaff MR. SCAI expert consensus statement for renal artery stenting appropriate use. Catheter Cardiovasc Interv. 2014;84(7):1163-71. A cost-effective investigation requires proper selection of candidates as well as anatomical and functional assessment of the stenosis. 866866. Herrmann SM, Textor SC. Current Concepts in the Treatment of Renovascular Hypertension. Am J Hypertens. 2018;31(2):139-49.
The gold standard is still conventional renal arteriography, but it is invasive and should not be used as the first procedure (LR: I; LE: B). BOLD or digital subtraction MNR angiography (LR: II; LE: B) and spiral CT are as accurate as ultrasounds, and have higher sensitivity and specificity (LR: I; LE: B). Renal Doppler US is the recommended noninvasive method for screening purposes, with 75% sensitivity and 90% specificity. 267267. Vasbinder GB, Nelemans PJ, Kessels AG, Kroon AA, de Leeuw PW, van Engelshoven JM. Diagnostic tests for renal artery stenosis in patients suspected of having renovascular hypertension: a meta-analysis. Ann Intern Med. 2001;135(6):401-11.,869869. Parikh SA, Shishehbor MH, Gray BH, White CJ, Jaff MR. SCAI expert consensus statement for renal artery stenting appropriate use. Catheter Cardiovasc Interv. 2014;84(7):1163-71.
870. Harvin HJ, Verma N, Nikolaidis P, Hanley M, Dogra VS, Goldfarb S, et al. ACR Appropriateness Criteria((R)) Renovascular Hypertension. Journal of the American College of Radiology : JACR. 2017;14(11s):S540-s9.-871871. Rountas C, Vlychou M, Vassiou K, Liakopoulos V, Kapsalaki E, Koukoulis G, et al. Imaging Modalities for Renal Artery Stenosis in Suspected Renovascular Hypertension: Prospective Intraindividual Comparison of Color Doppler US, CT Angiography, GD-Enhanced MR Angiography, and Digital Substraction Angiography. Renal Failure. 2007;29(3):295-302.
The treatment objectives for RVH are reducing the morbidity and mortality associated with high BP and protecting renal function and circulation. Randomized clinical trials 872872. Zeller T, Krankenberg H, Erglis A, Blessing E, Fuss T, Scheinert D, et al. A randomized, multi-center, prospective study comparing best medical treatment versus best medical treatment plus renal artery stenting in patients with hemodynamically relevant atherosclerotic renal artery stenosis (RADAR) – one-year results of a pre-maturely terminated study. Trials. 2017;18(1):380. and a meta-analysis 873873. Raman G, Adam GP, Halladay CW, Langberg VN, Azodo IA, Balk EM. Comparative Effectiveness of Management Strategies for Renal Artery Stenosis: An Updated Systematic Review. Ann Intern Med. 2016;165(9):635-49. have shown 874874. Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13-22.,875875. Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361(20):1953-62. that pharmacological treatment matches revascularization, with similar rates of BP control and cardiovascular mortality.
RAAS-blocking medication is recommended to lower hyperfiltration in the contralateral kidney and proteinuria in unilateral RVH with adequate potassium and creatinine monitoring. The efficacy of pharmacological optimization is an important element for decisions about whether an invasive procedure is indicated. 874874. Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13-22. Atherosclerotic RVH requires lifestyle changes, smoking cessation, glycemic control, and prescription of statins and antiplatelet drugs, unless contraindicated. 874874. Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13-22.,876876. Nicholson J, Alderman M, Pickering T, Teichman S, Sos T, Laragh J. CIGARETTE SMOKING AND RENOVASCULAR HYPERTENSION. The Lancet. 1983;322(8353):765-6.
If the blood-pressure target cannot be reached and/or there are other associated clinical conditions, such as RHT or RfHT, progressive kidney dysfunction or APE episodes, the invasive procedure may be recommended, conditional on the patient's acceptance. The actual benefits of invasive treatment are controversial, and clinical trials are still needed to identify the specific population that would benefit from this sort of treatment. 877877. Piaggio D, Bracale U, Pecchia L, Di Taranto MD, Sodo M, Bracale UM. Endovascular Treatment versus Medical Therapy for Hypertensive Patients with Renal Artery Stenosis: An Updated Systematic Review. Annals of vascular surgery. 2019;61:445-54.,878878. Noory E, Sritharan K, Zeller T. To Stent or Not to Stent? Update on Revascularization for Atherosclerotic Renovascular Disease. Curr Hypertens Rep. 2016;18(6):45. Diagnostic recommendations for renovascular disease can be found in Chart 15.4 .
15.3. Fibromuscular Dysplasia
Fibromuscular dysplasia (FMD) is an idiopathic, segmental, stenotic, nonatherosclerotic, and noninflammatory disease of the small- and medium-caliber muscular arteries. The lesions may be symptomatic or clinically silent, hemodynamically significant or not. Approximately 80 to 90% of patients are females. The First International Consensus 879879. Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vascular medicine (London, England). 2019;24(2):164-89. recommends angiographic classification for focal and multifocal FMD. For screening purposes, Doppler ultrasound of renal arteries is recommended. Other imaging examinations coincide with those used for atherosclerotic RVH: spiral CT if eGFR > 60 mL/min or MNR if eGFR > 30 mL/min. 879879. Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vascular medicine (London, England). 2019;24(2):164-89. Renal artery angiography is the gold standard to identify damage to the renal artery. Measuring the translesional gradient to determine the hemodynamic significance of the stenosis is recommended, especially in multifocal lesions. Identification of other vascular segments affected by the disease and investigation of aneurysms and dissections are recommended 880880. Bolen MA, Brinza E, Renapurkar RD, Kim ESH, Gornik HL. Screening CT Angiography of the Aorta, Visceral Branch Vessels, and Pelvic Arteries in Fibromuscular Dysplasia. JACC Cardiovascular imaging. 2017;10(5):554-61. ( Figure 152 ).
Isolated angioplasty is the recommended procedure, with stenting in case of complications (arterial rupture or dissection). In the absence of contraindications, continuous antiplatelet therapy with acetylsalicylic acid at 75 to 100 mg/day is indicated to prevent thrombotic complications, and dual antiplatelet therapy may be used for a short period of four to six weeks. 881881. Weinberg I, Gu X, Giri J, Kim SE, Bacharach MJ, Gray BH, et al. Anti-platelet and anti-hypertension medication use in patients with fibromuscular dysplasia: Results from the United States Registry for Fibromuscular Dysplasia. Vascular medicine (London, England). 2015;20(5):447-53. Doppler ultrasound of renal arteries 30 days after angioplasty is recommended, repeated every six months for the first two years and annually afterward, to detect restenosis. 879879. Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vascular medicine (London, England). 2019;24(2):164-89. As a matter of course, all patients should be included in follow-up, and optimally undergo yearly clinical and imaging assessments.
15.3.1. Coarctation of the Aorta
Coarctation of the aorta is a congenital anomaly leading to narrowing of the aorta, usually juxtaductal, proximal to the ductus arteriosus or ligament. It is usually underdiagnosed, with diverse clinical presentation, from early symptoms at birth (severe) to asymptomatic into adulthood, 882882. Rao PS. Coarctation of the aorta. Seminars in nephrology. 1995;15(2):87-105. depending on the site and severity of the coarctation as well as the frequent presence of other congenital heart diseases impacting prognosis. 883883. Godart F. [Management of aortic coarctation at the adult age]. Archives des maladies du coeur et des vaisseaux. 2007;100(5):478-83. The definition of significant coarctation requires pre- and post-coarctation pressure gradient > 20 mm Hg. Clinical suspicion is based on symptoms (resistant or refractory HT, epistaxis, headache and weakness of the legs on exertion, manifestations of HF, angina, aortic dissection, or intracerebral hemorrhage) and physical examination (hypertension in the upper limbs [ULs] with SBP at least 10 mm Hg higher in the brachial artery than in the popliteal artery; absent or diminished pulse in lower limbs [LLs]; interscapular and thoracic systolic murmur). 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. Diagnosis is based on imaging examinations: chest X-ray (thoracic aorta with pre- and post-stenosis dilations, costal corrosion); echocardiogram, the primary screening examination (posterior protrusion, expanded isthmus, transverse aortic arch, and high-velocity continuous jet through the coarctation site); CT or MNR angiography 884884. Dijkema EJ, Leiner T, Grotenhuis HB. Diagnosis, imaging and clinical management of aortic coarctation. Heart. 2017;103(15):1148-55. in case of poor acoustic window. The MNR is considered the gold standard for assessment and post-intervention follow-up and, in young individuals, does not require invasive preoperative angiography, indicated when other imaging methods cannot provide visualization of the coarctation, and in older individuals who may have CAD. Intervention treatment includes angioplasty, implantation of vascular endoprosthesis, or open surgery (hypoplasia of the aortic arch and/or need for coarctation resection). The perioperative mortality rate is very low and prognosis is relatively good, though patients with coarctation of the aorta have higher and earlier incidence of CV disease than the general population and require continuous monitoring. 885885. Torok RD, Campbell MJ, Fleming GA, Hill KD. Coarctation of the aorta: Management from infancy to adulthood. World journal of cardiology. 2015;7(11):765-75. The BP response to intervention treatment depends on the duration of AH prior to surgery and the patient’s age.. 886886. Martins JD, Zachariah J, Selamet Tierney ES, Truong U, Morris SA, Kutty S, et al. Impact of Treatment Modality on Vascular Function in Coarctation of the Aorta: The LOVE - COARCT Study. J Am Heart Assoc. 2019;8(7):e011536. Though many lower BP after an invasive procedure, most develop exercise-induced HT. The drugs of choice for both the preoperative period and residual BP after surgery are beta-blockers (BBs) and angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II AT1 receptor blockers (ARBs). 885885. Torok RD, Campbell MJ, Fleming GA, Hill KD. Coarctation of the aorta: Management from infancy to adulthood. World journal of cardiology. 2015;7(11):765-75.,887887. Cangussú LR, Lopes MR, Barbosa RHdA. The importance of the early diagnosis of aorta coarctation. Revista da Associação Médica Brazileira. 2019;65:240-5. Renin-angiotensin-aldosterone system blockers (SRAA) should be used with caution in the preoperative period in order to avoid major decreases in blood flow distally from the coarctation, which would trigger acute kidney damage. 885885. Torok RD, Campbell MJ, Fleming GA, Hill KD. Coarctation of the aorta: Management from infancy to adulthood. World journal of cardiology. 2015;7(11):765-75.,887887. Cangussú LR, Lopes MR, Barbosa RHdA. The importance of the early diagnosis of aorta coarctation. Revista da Associação Médica Brazileira. 2019;65:240-5.
15.3.2. Obstructive Sleep Apnea (OSA)
15.3.2.1. Concept and Epidemiology
OSA is a clinical condition characterized by the intermittent collapse of the upper airways during sleep, causing total (apnea) and partial (hypopnea) obstructions. 888888. Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020;323(14):1389-400. Respiratory pauses lead to greater respiratory efforts and lower intrathoracic pressure, which cause increased left ventricle transmural pressure, cyclical dips in oxygen saturation (intermittent hypoxia), hypercapnia (usually mild), and sleep fragmentation. 889889. Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569-76. The mechanisms involved with HT include activation of the sympathetic nervous system, systemic inflammation, increased production of reactive oxygen species, and endothelial dysfunction, among others. 889889. Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569-76.
Traditionally, OSA severity is determined by adding up apnea and hypopnea events (known as apnea-hypopnea index [AHI]), as determined by objective sleep testing: AHI < 5 events/h: no OSA; AHI 5-14.9 events/h: mild OSA; AHI 15-29.9 events/h: moderate OSA; AHI ≥ 30 events/h: severe OSA. The prevalence of OSA in the general population is high, depending on the diagnostic criteria adopted. In adults, it affects approximately 9.6% of women and 24.8% of men. 890890. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441-6. In hypertensive patients in general, it is estimated that 56% suffer from some degree of OSA. 891891. Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB. Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med. 1985;103(2):190-5.
892. Williams AJ, Houston D, Finberg S, Lam C, Kinney JL, Santiago S. Sleep apnea syndrome and essential hypertension. Am J Cardiol. 1985;55(8):1019-22.
893. Sjostrom C, Lindberg E, Elmasry A, Hagg A, Svardsudd K, Janson C. Prevalence of sleep apnoea and snoring in hypertensive men: a population based study. Thorax. 2002;57(7):602-7.-894894. Drager LF, Genta PR, Pedrosa RP, Nerbass FB, Gonzaga CC, Krieger EM, et al. Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol. 2010;105(8):1135-9. For those with resistant HT, the prevalence is estimated at > 60% and is likely the most frequent cause associated with secondary HT, 895895. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. though it does not mean OSA is the only cause in most cases. Though there is evidence that normotensive OSA patients progress to higher incidence rates of HT regardless of other risk factors, 896896. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-84.,897897. Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307(20):2169-76. in clinical practice, OSA frequently arises in previously hypertensive individuals. However, this in no way minimizes the importance of OSA: there is evidence that the association between OSA and HT is linked to higher rates of end-organ damage compared to hypertensive patients without OSA. 895895. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7.,896896. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-84.
15.3.2.2. Clinical Presentation and Screening of OSA in Hypertension
In the general population, some predisposing factors and clinical signs and symptoms should be assessed during examination and may reinforce the clinical suspicion of OSA 888888. Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020;323(14):1389-400. ( Chart 15.5 ). OSA prevalence rates are two to three times higher in men than in women, but is also common in the latter group, especially after menopause.
However, many of these signs and symptoms may be less prominent in HT. For instance, daytime sleepiness is often absent in HT, especially in patients with resistant HT. 899899. Drager LF, Bortolotto LA, Krieger EM, Lorenzi-Filho G. Additive effects of obstructive sleep apnea and hypertension on early markers of carotid atherosclerosis. Hypertension. 2009;53(1):64-9. Screening surveys for OSA in the general population perform poorly, especially in resistant HT patients. 900900. Gus M, Goncalves SC, Martinez D, de Abreu Silva EO, Moreira LB, Fuchs SC, et al. Risk for Obstructive Sleep Apnea by Berlin Questionnaire, but not daytime sleepiness, is associated with resistant hypertension: a case-control study. Am J Hypertens. 2008;21(7):832-5.
901. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485-91.
902. Margallo VS, Muxfeldt ES, Guimaraes GM, Salles GF. Diagnostic accuracy of the Berlin questionnaire in detecting obstructive sleep apnea in patients with resistant hypertension. J Hypertens. 2014;32(10):2030-6; discussion 7.-903903. Giampa SQC, Pedrosa RP, Gonzaga CC, Bertolami A, Amodeo C, Furlan SF, et al. Performance of NoSAS score versus Berlin questionnaire for screening obstructive sleep apnoea in patients with resistant hypertension. J Hum Hypertens. 2018;32(7):518-23. It should be mentioned that some findings in BP patterns may help screen for patients with OSA. Recent data suggest that changes in nighttime BP dipping, especially the ascending waveform (mean BP during sleep higher than when awake), increase the odds of OSA three to four times. 904904. Genta-Pereira DC, Furlan SF, Omote DQ, Giorgi DMA, Bortolotto LA, Lorenzi-Filho G, et al. Nondipping Blood Pressure Patterns Predict Obstructive Sleep Apnea in Patients Undergoing Ambulatory Blood Pressure Monitoring. Hypertension. 2018;72(4):979-85.
15.3.2.3. Impact of Treatment of OSA on BP
The treatment of choice for OSA, especially in moderate to severe cases, is the use of a continuous positive airway pressure (CPAP) device. 888888. Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020;323(14):1389-400. Mandibular advancement, oropharyngeal exercises, positional therapy, and surgery can be used in less severe and select cases of OSA. 905905. Drager LF, Lorenzi-Filho G, Cintra FD, Pedrosa RP, Bittencourt LRA, Poyares D, et al. Arq Bras Cardiol. 2018;111(2):290-340.
Overall, treatment of OSA has a modest impact on BP (around 2 to 3 mm Hg). 906906. Fatureto-Borges F, Lorenzi-Filho G, Drager LF. Effectiveness of continuous positive airway pressure in lowering blood pressure in patients with obstructive sleep apnea: a critical review of the literature. Integr Blood Press Control. 2016;9:43-7. These results are partially justified by the following factors: 1) many trials and meta-analyses combine controlled and uncontrolled hypertensive and normotensive participants; 906906. Fatureto-Borges F, Lorenzi-Filho G, Drager LF. Effectiveness of continuous positive airway pressure in lowering blood pressure in patients with obstructive sleep apnea: a critical review of the literature. Integr Blood Press Control. 2016;9:43-7. and 2) adherence to CPAP use is not always adequate. 906906. Fatureto-Borges F, Lorenzi-Filho G, Drager LF. Effectiveness of continuous positive airway pressure in lowering blood pressure in patients with obstructive sleep apnea: a critical review of the literature. Integr Blood Press Control. 2016;9:43-7. Randomized trials have shown that the impact of OSA treatment on BP is greater for RHT patients (circa 5 mm Hg, on average), but generally do not lead to blood pressure control them. 907907. Pedrosa RP, Drager LF, de Paula LKG, Amaro ACS, Bortolotto LA, Lorenzi-Filho G. Effects of OSA treatment on BP in patients with resistant hypertension: a randomized trial. Chest. 2013;144(5):1487-94.
908. Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, Diaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407-15.-909909. de Oliveira AC, Martinez D, Massierer D, Gus M, Goncalves SC, Ghizzoni F, et al. The antihypertensive effect of positive airway pressure on resistant hypertension of patients with obstructive sleep apnea: a randomized, double-blind, clinical trial. Am J Respir Crit Care Med. 2014;190(3):345-7. A study found that the presence of altered nighttime dipping was a predictor of better response from CPAP use in lowering BP for OSA patients. 910910. Castro-Grattoni AL, Torres G, Martínez-Alonso M, Barbé F, Turino C, Sánchez-de-la-Torre A, et al. Blood pressure response to CPAP treatment in subjects with obstructive sleep apnoea: the predictive value of 24-h ambulatory blood pressure monitoring. Eur Respir J. 2017;50(4). Another poorly understood finding is that individuals afflicted with excessive sleepiness have greater decreases in BP. 911911. Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587-96.
Chart 15.6 details a few predictors of better blood pressure response to CPAP use. 911911. Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587-96.
15.3.2.4. Antihypertensive Treatment in Hypertensive Patients with OSA
Thus far, there is no conclusive evidence than any particular class of antihypertensive medication is preferable for hypertensive patients suffering from OSA. 905905. Drager LF, Lorenzi-Filho G, Cintra FD, Pedrosa RP, Bittencourt LRA, Poyares D, et al. Arq Bras Cardiol. 2018;111(2):290-340. A few aspects deserve to be highlighted here:
In general, the effect of antihypertensives seems to be more effective than CPAP use on lowering BP, but combining CPAP use and an antihypertensive has additional benefits, especially for nighttime BP; 912912. Pepin JL, Tamisier R, Barone-Rochette G, Launois SH, Levy P, Baguet JP. Comparison of continuous positive airway pressure and valsartan in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;182(7):954-60.
Though more effective than CPAP alone, pharmacological treatment for HT usually does not improve the severity and symptoms of OSA. Even the effect of some diuretics and salt restriction on OSA severity (based on the theory that overnight rostral fluid shift favors upper airway collapsibility) 913913. Yumino D, Redolfi S, Ruttanaumpawan P, Su MC, Smith S, Newton GE, et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation. 2010;121(14):1598-605. has a very modest impact on the severity of OSA. 914914. Gaddam K, Pimenta E, Thomas SJ, Cofield SS, Oparil S, Harding SM, et al. Spironolactone reduces severity of obstructive sleep apnoea in patients with resistant hypertension: a preliminary report. J Hum Hypertens. 2010;24(8):532-7.,915915. Fiori CZ, Martinez D, Montanari CC, Lopez P, Camargo R, Sezera L, et al. Diuretic or sodium-restricted diet for obstructive sleep apnea-a randomized trial. Sleep. 2018;41(4).
15.4. Endocrine Causes
15.4.1. Primary Hyperaldosteronism (PH)
HT accompanied by supressed plasma renin activity (PRA) and increased aldosterone excretion characterizes primary aldosteronism. 916916. Conn JW. Primary aldosteronism. J Lab Clin Med. 1955;45(4):661-4. PH was considered a rare form of secondary HT (1%), but may currently be found in 22% of RHT patients. 917917. Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.,918918. Kline GA, Prebtani APH, Leung AA, Schiffrin EL. Primary aldosteronism: a common cause of resistant hypertension. CMAJ. 2017;189(22):E773-E8. Gordon et al. found the incidence of PH in the primary hypertensive population to range from 5 to 15%, and to probably be approximately 12%. 919919. Gordon RD, Ziesak MD, Tunny TJ, Stowasser M, Klemm SA. Evidence that primary aldosteronism may not be uncommon: 12% incidence among antihypertensive drug trial volunteers. Clin Exp Pharmacol Physiol. 1993;20(5):296-8. Bilateral cortical adrenal hyperplasia is the most frequent cause of PH (50-60%), while aldosterone-producing adenomas (APA) account for 40% of PH cases. 920920. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916. Aldosterone-producing cortical adrenal carcinomas and unilateral cortical adrenal hyperplasia are less frequent causes of PH.
The main confirmatory tests for PH are listed in Chart 15.7 , 920920. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
921. Morera J, Reznik Y. MANAGEMENT OF ENDOCRINE DISEASE: The role of confirmatory tests in the diagnosis of primary aldosteronism. Eur J Endocrinol. 2018.
922. Stowasser M, Ahmed AH, Cowley D, Wolley M, Guo Z, McWhinney BC, et al. Comparison of Seated With Recumbent Saline Suppression Testing for the Diagnosis of Primary Aldosteronism. The Journal of clinical endocrinology and metabolism. 2018;103(11):4113-24.
923. Nanba K, Tamanaha T, Nakao K, Kawashima ST, Usui T, Tagami T, et al. Confirmatory testing in primary aldosteronism. The Journal of clinical endocrinology and metabolism. 2012;97(5):1688-94.-924924. Vilela LAP, Almeida MQ. Diagnosis and management of primary aldosteronism. Arch Endocrinol Metab. 2017;61(3):305-12. while the diagnostic investigation flow chart can be found in Figure 15.3 .
The most accurate imaging examination is the thin-slice CT, and MR provides no advantages. The goal of adrenal venous catheterization with concurrent blood sampling for aldosterone and cortisol is to identify the source of aldosterone secretion, and is considered the most accurate test to differentiate PH subtypes. It is recommended for patients with normal adrenal glands or bilateral abnormalities in CT scans.
In addition, adrenal venous catheterization is indicated in patients with small adrenal nodules (< 1.5 cm) and age 40 or older at HT diagnosis, as it may be a nonfunctioning adenoma. 920920. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
921. Morera J, Reznik Y. MANAGEMENT OF ENDOCRINE DISEASE: The role of confirmatory tests in the diagnosis of primary aldosteronism. Eur J Endocrinol. 2018.
922. Stowasser M, Ahmed AH, Cowley D, Wolley M, Guo Z, McWhinney BC, et al. Comparison of Seated With Recumbent Saline Suppression Testing for the Diagnosis of Primary Aldosteronism. The Journal of clinical endocrinology and metabolism. 2018;103(11):4113-24.
923. Nanba K, Tamanaha T, Nakao K, Kawashima ST, Usui T, Tagami T, et al. Confirmatory testing in primary aldosteronism. The Journal of clinical endocrinology and metabolism. 2012;97(5):1688-94.-924924. Vilela LAP, Almeida MQ. Diagnosis and management of primary aldosteronism. Arch Endocrinol Metab. 2017;61(3):305-12. The method is invasive and depends on the radiologist's experience. The treatment of choice for APA is unilateral adrenalectomy, preferably laparoscopic, unless contraindicated.
In hyperplastic HT, treatment consists of mineralocorticoid antagonists (spironolactone 50 to 400 mg/day). 920920. Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
921. Morera J, Reznik Y. MANAGEMENT OF ENDOCRINE DISEASE: The role of confirmatory tests in the diagnosis of primary aldosteronism. Eur J Endocrinol. 2018.
922. Stowasser M, Ahmed AH, Cowley D, Wolley M, Guo Z, McWhinney BC, et al. Comparison of Seated With Recumbent Saline Suppression Testing for the Diagnosis of Primary Aldosteronism. The Journal of clinical endocrinology and metabolism. 2018;103(11):4113-24.
923. Nanba K, Tamanaha T, Nakao K, Kawashima ST, Usui T, Tagami T, et al. Confirmatory testing in primary aldosteronism. The Journal of clinical endocrinology and metabolism. 2012;97(5):1688-94.-924924. Vilela LAP, Almeida MQ. Diagnosis and management of primary aldosteronism. Arch Endocrinol Metab. 2017;61(3):305-12. The primary target of pharmacological treatment should be the renin blockade (in addition to blood pressure control and correcting hypercalcemia ) in order to lower the cumulative incidence of cardiovascular events. 925925. Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(1):51-9.
15.4.2. Pheochromocytoma
Pheochromocytomas (PHEO) are catecholamine-secreting chromaffin-cell tumors of the sympathetic adrenomedullary axis. 926926. van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. European journal of endocrinology. 2014;170(3):R109-19. Ten to 15% are extra-adrenal (paragangliomas), 10% are bilateral, and 15 to 20% are malignant (from 2 to 50%, depending on genetic defect). 927927. Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Current problems in cancer. 2014;38(1):7-41. The incidence rate for pheochromocytoma and paraganglioma is 0.6 cases per 100 000 persons-year.
The symptoms are the classic triad: headaches, profuse sweating, and palpitations with RHT/RfHT or paroxysmal HT (50%; hypertensive crises alternating with normal BP periods). The simultaneous presence of the classic triad and a hypertensive crisis has 89% diagnostic sensitivity and 67% diagnostic specificity. 926926. van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. European journal of endocrinology. 2014;170(3):R109-19.
Pheochromocytoma or paraganglioma diagnosis requires confirmation of excess catecholamine secretion and documenting the anatomy of the tumor. Laboratory diagnosis is based on blood and urine catecholamine metabolite levels. Free plasma metanephrine (metanephrine and normetanephrine) has 97% sensitivity and 93% specificity, 926926. van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. European journal of endocrinology. 2014;170(3):R109-19. (LR: I; LE: A), but because of its higher cost, urine metanephrine isolated or associated with urine catecholamines (epinephrine, norepinephrine, and dopamine) is indicated. Though less sensitive, high urine catecholamine values (> 2 times the upper bound) indicate high diagnostic probability. 242242. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-42. Urine metanephrine levels are more sensitive than urine catecholamine and vanillylmandelic acid for PHEO and paraganglioma diagnoses (ungraded recommendation). 928928. Lenders JW, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, et al. Biochemical diagnosis of pheochromocytoma: which test is best? Jama. 2002;287(11):1427-34.
In acute stress situations (acute illness, sepsis, AMI, decompensated HF) and the use of tricyclic antidepressants, antipsychotics agents, and levodopa, among others, it may be accompanied by increased catecholamine levels (usually < 2x the upper limit of normality). The medication should be suspended two weeks before sample collection to prevent false positives. The imaging tests to locate adrenal tumors are CTs (preferably; LR: 2; LE: B) and MNRs (hypersignal at T2 for PHEO), with 89% and 98% sensitivity, respectively. 929929. Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, Banerji MA. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-38. An MRI is superior in the identification of paraganglioma or lymph node metastases (LR: I; LE: B). Whole-body scintigraphy using 123I-MIBG or 68Ga DOTATE-PET-CT is very effective at locating PHEOs and paragangliomas, metastases or multiple chromaffin-cell tumors (LR: IIa; LE: C). 930930. Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nature clinical practice Endocrinology & metabolism. 2007;3(2):92-102.,931931. Calabrò D, Allegri V, Fanti S, Ambrosini V. 68Ga-DOTANOC and 18F-DOPA PET/CT: a site-specific approach to the imaging of parangliomas of the head and neck and of the abdomen. European Journal of Nuclear Medicine and Molecular Imaging. 2019;46(6):1393-.
The preferential treatment is minimally invasive surgery (LR: I; LE: B), and preoperative preparation should include alpha-1-blockers (doxazosin or prazosin) and adequate hydration with increased oral sodium intake for at least 2 weeks prior to surgery. 932932. Bravo EL. Pheochromocytoma: an approach to antihypertensive management. Annals of the New York Academy of Sciences. 2002;970:1-10. The chronic pharmacological treatment includes alpha1-blockers, BBs (only after beginning alpha1- blockers, in the presence of symptomatic tachycardia), CCBs, ACEIs, and central action agonists. 932932. Bravo EL. Pheochromocytoma: an approach to antihypertensive management. Annals of the New York Academy of Sciences. 2002;970:1-10. The paroxysmal hypertensive crisis of PHEO is an emergency, and should be treated with sodium nitroprusside or injectable phentolamine and volume replacement, if necessary. 926926. van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. European journal of endocrinology. 2014;170(3):R109-19.
Total and early removal of the neoplasm usually determines total remission of symptoms and cure of AH, in addition to preventing metastatic disease. 927927. Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Current problems in cancer. 2014;38(1):7-41.,929929. Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, Banerji MA. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-38. For malignant PHEO with unresectable metastases, systemic therapy with MIBG-131 is indicated. Cytotoxic chemotherapy is indicated in case of disease progression after high cumulative dose of MIBG-131 or in case of metastasis without MIBG uptake. Zoledronic acid is indicated to fight pain and lower fracture risk in patients with bone metastases. 927927. Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Current problems in cancer. 2014;38(1):7-41.,929929. Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, Banerji MA. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-38. Clinical, biochemical and radiological follow-up of patients is essential to detect malignant recurrences or metastases as well as other tumors in familial syndromes. 242242. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-42.
15.4.3. Hypothyroidism
The clinical signs of hypothyroidism are usually nonspecific, including fatigue, sleepiness and weight gain (mild in most cases). Patients with hypothyroidism have low levels of free thyroxine (T4) and high levels of thyroid-stimulating hormone (TSH), both screening tools for the condition (LR: IIa; LE: B). 933933. Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670-751. In subclinical hypothyroidism, free T4 is normal and TSH is elevated. In hypothyroidism, there is higher risk of diastolic HT. 934934. Jian WX, Jin J, Qin L, Fang WJ, Chen XR, Chen HB, et al. Relationship between thyroid-stimulating hormone and blood pressure in the middle-aged and elderly population. Singapore Med J. 2013;54(7):401-5. Hypothyroidism increases vascular resistance and extracellular volume, but BP increases are usually mild (< 150/100 mm Hg).
15.4.4. Hyperthyroidism
Hyperthyroidism increases cardiac output due to increased peripheral oxygen consumption and increased cardiac contractility. 935935. Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system: from theory to practice. J Clin Endocrinol Metab. 1994;78(5):1026-7. Systolic HT is common, but HT prevalence depends on the severity of hyperthyroidism. Atrial fibrillation occurs in 10 to 20% of hyperthyroidism patients, and is more frequent in patients age 60 and over. 936936. Frost L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter: a population-based study. Arch Intern Med. 2004;164(15):1675-8. The most prominent clinical conditions are Graves' disease (palpitations, weight loss, exophthalmos, goiter, tremors of the extremities, warm skin, and heat intolerance, among other symptoms) or toxic adenoma, which may be more oligosymptomatic in older individuals with toxic multinodular goiters. Diagnosis is based on free thyroxine (T4) and thyroid-stimulating hormone (TSH) levels (LR: IIa; LE: B). usually, free T4 is high and TSH is suppressed. 937937. Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016;26(10):1343-421. In subclinical hyperthyroidism, free T4 is normal and TSH is suppressed. The presence of TSH antireceptor antibodies is diagnostic for Graves' disease, but may be absent in approximately 10% of cases.
15.4.5. Primary Hyperparathyroidism
The frequency of HT in patients with primary hyperparathyroidism ranges from 10 to60%. 938938. Richards AM, Espiner EA, Nicholls MG, Ikram H, Hamilton EJ, Maslowski AH. Hormone, calcium and blood pressure relationships in primary hyperparathyroidism. J Hypertens. 1988;6(9):747-52. Most patients with primary hyperparathyroidism are asymptomatic, while the rest may present with polyuria, polydipsia, osteoporosis, constipation, renal calculi, and HT. The mechanisms involved in HT are undefined, and there is no direct correlation between PHT levels and calcemia with severity of HT. In primary hyperparathyroidism, HT becomes more severe with impaired renal function due to hypercalcemia. Laboratory investigation involves testing calcemia (total and/or ionized calcium), phosphorus, PTH, and 24-hour urine calcium. 939939. Bilezikian JP. Primary Hyperparathyroidism. The Journal of clinical endocrinology and metabolism. 2018;103(11):3993-4004. Vitamin D levels (especially if < 20 ng/dL) should also be measured and supplemented to rule out secondary hyperparathyroidism and vitamin D deficiency from normocalcemic primary hyperparathyroidism.
15.4.6. Cushing's Syndrome
Iatrogenic Cushing's syndrome (from the use of exogenous corticoids) is relatively common, unlike endogenous Cushing's syndrome, which is rare. Among endogenous causes, Cushing's syndrome (ACTH-secreting pituitary adenoma) is responsible for 85% of cases, while 15% are caused by adrenal hyperplasia or tumors (ACTH-independent causes). HT can be found in 75-80% of Cushing's syndrome patients. The mechanisms of HT are the cortisol-enhanced vasopressor effect of catecholamines, the effect of cortisol on mineralocorticoid receptors, and RAAS activation through increased liver production of angiotensinogen. Laboratory diagnosis of hypercortisolism uses baseline cortisol (useful to rule out exogenous use of dexamethasone or betamethasone), midnight salivary cortisol, and 24-h urinary cortisol, in addition to the dexamethasone suppression test (take 1 mg dexamethasone at 11 PM and measure serum cortisol level at 7-8 AM of the following morning). Radiological investigation should be based on adrenal CT scans or pituitary MRI for ACTH-dependent hypercortisolism. Imaging examinations should only be performed after clinical and laboratory diagnosis of hypercortisolism. Treatment of endogenous Cushing's syndrome depends on the etiology of the hypercortisolism. It can be managed surgically or with medications. 940940. Nieman LK, Biller BMK, Findling JW, Murad MH, Newell-Price J, Savage MO, et al. Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2015;100(8):2807-31.
15.4.7. Obesity
Excessive visceral fat is accompanied by major hormonal, inflammatory and endothelial abnormalities. 941941. Fantin F, Giani A, Zoico E, Rossi AP, Mazzali G, Zamboni M. Weight Loss and Hypertension in Obese Subjects. Nutrients. 2019;11(7):1677. All these mechanisms trigger a cascade of cytokine and adipokine release, increasing insulin resistance and determining RAAS and SNS hyperactivity, causing water and sodium retention and, consequently, HT and increased CV and renal risk. Countless studies have shown the close association between increased BP and weight gain. Adopting a weight loss strategy (see Chapter 8) is a key recommendation to lower BP and decrease CV risk as well as associated diseases, such as OSA. 942942. Saliba LJ, Maffett S. Hypertensive Heart Disease and Obesity: A Review. Heart Fail Clin. 2019;15(4):509-17.,943943. Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1-7.
From a practical standpoint, though it has been criticized for ignoring race/ethnicity, age, sex, and other parameters, obesity is categorized according to BMI (kg/m 22. Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65. ) as class 1. BMI 30 to < 35; class 2, BMI 35 to < 40; and class 3, BMI ≥ 40. Measuring abdominal circumference can also help diagnose central obesity. Further studies, such as bioimpedance and more accurate and very expensive imaging examinations may be performed, especially in clinical trials, such as dual-energy x-ray absorptiometry scanning (DEXA), CT and MNR. 944944. Ping Z, Pei X, Xia P, Chen Y, Guo R, Hu C, et al. Anthropometric indices as surrogates for estimating abdominal visceral and subcutaneous adipose tissue: A meta-analysis with 16,129 participants. Diabetes research and clinical practice. 2018;143:310-9.-945945. Nimptsch K, Konigorski S, Pischon T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019;92:61-70.
15.4.8. Acromegaly
In approximately 98% of cases, sporadic or familial acromegaly is caused by growth hormone-secreting pituitary adenomas. Excess growth hormone (GH) stimulates hepatic secretion of insulin-like growth factor-1 (IGF-1), the cause of most clinical manifestations.
They are more frequent between ages 30 and 50 and can be divided into microadenomas (smaller than 1 cm) and macroadenomas (1 cm or larger). The second kind accounts for over 70% of tumors causing acromegaly. HT can occur in approximately 30% of cases and is multifactorial in nature, with a hydrosaline retention component, direct antinatriuretic effect of GH, RAAS and hyperactivity, and endothelial dysfunction, in addition to dysglycemia, left ventricular hypertrophy (LVH) and OSA. Other symptoms can be found in Chart 15.2 . 947947. de Pablos-Velasco P, Venegas EM, Alvarez Escola C, Fajardo C, de Miguel P, Gonzalez N, et al. Diagnosis, treatment and follow-up of patients with acromegaly in a clinical practice setting in Spain: the ACROPRAXIS program Delphi survey. Pituitary. 2020;23(2):129-39.
Laboratory assessment begins with serum IGF-1 and GH levels (LR: I; LE: B). Very low GH levels (below 0.4 ng/mL) rule out acromegaly, especially when associated with normal IGF-1 serum levels. GH level after glucose overload (75 g) can demonstrate the nonsuppression of GH secretion (LR: I; LE: B). IGF-1 levels and GH suppression testing after glucose overload are also employed to evaluate response to treatment. Sella turcica MNR is the best imaging examination to identify the tumor and, if contraindicated, may be replaced by a sella turcica CT scan (LR: IIa; LE: B). 946946. Katznelson L, Atkinson J, Cook D, Ezzat S, Hamrahian A, Miller K. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Diagnosis and Treatment of Acromegaly-2011 Update. Endocrine Practice. 2011;17(Supplement 4):1-44.
947. de Pablos-Velasco P, Venegas EM, Alvarez Escola C, Fajardo C, de Miguel P, Gonzalez N, et al. Diagnosis, treatment and follow-up of patients with acromegaly in a clinical practice setting in Spain: the ACROPRAXIS program Delphi survey. Pituitary. 2020;23(2):129-39.-948948. Silverstein JM, Roe ED, Munir KM, Fox JL, Emir B, Kouznetsova M, et al. Use of electronic health records to characteristize a rare disease in the U.S. : treatment comorbidities and follow-up trends among patients with a confirmed diagnosis of acromegaly.Endocr Pract. 2018;24(6):517-26. Acromegaly treatment may involve surgical procedures, radiotherapy, and pharmacological treatment with somatostatin analogs, with octreotide, lanreotide, and cabergoline available in the Brazilian Unified Health System (SUS). 949949. Brazil.Ministério daSaúde. Secretaria da Ciência e Tecnologia e Insumos Estratégicos .Portaria Conjunta n.2, de 07 de janeiro de 2019. Aprova o protocolo clínico e diretrizes terapêuticas da Acromeagalia. Brazilia;2019.
15.5. Pharmacological Causes, Hormones, and Exogenous Substances
It is a relatively common and underestimated cause of worsening HT or even its induction, frequently circumventable or reversible. A full history of all medications, drugs and supplements in use should be taken for all hypertensive patients. 859859. Hirsch JS, Hong S. The Demystification of Secondary Hypertension: Diagnostic Strategies and Treatment Algorithms. Current Treatment Options in Cardiovascular Medicine. 2019;21(12):90.
Hypertensive mechanisms vary widely and may be multifactorial, such as volume retention (glucocorticoids, ketoconazole, oral contraceptives, androgen therapy, nonsteroidal anti-inflammatory drugs [NSAID]), sympathetic hyperactivity (decongestants, amphetamines, monoamine oxidase inhibitors [MAOIs], antidepressants, other psychiatric medications, cocaine, calcineurin inhibitors), and RAAS hyperactivity (immunosuppressants). 950950. Grossman E, Messerli FH. Drug-induced hypertension: an unappreciated cause of secondary hypertension. Am J Med. 2012;125(1):14-22. Good clinical practice dictates that hypertensive patients should be informed when combining medications can lead to worse blood pressure control. 951951. Diaconu CC, Dediu GN, Iancu MA. Drug-induced arterial hypertension - a frequently ignored cause of secondary hypertension: a review. Acta cardiologica. 2018:1-7.
Angiogenesis inhibition via endothelial vascular growth factor inhibition is an antineoplastic strategy applied in various oncology settings. Blood pressure increases, even acute ones, are a common side effect. 952952. Versmissen J, Mirabito Colafella KM, Koolen SLW, Danser AHJ. Vascular Cardio-Oncology: Vascular Endothelial Growth Factor inhibitors and hypertension. Cardiovasc Res. 2019;115(5):904-14. The mechanisms involved are the activation of the endothelin system, endothelial dysfunction, and capillary rarefaction. It is recommended that blood pressure be below 140/90 mm Hg before initiating this form of treatment and that BP monitoring continue throughout the therapy 953953. Rizzoni D, De Ciuceis C, Porteri E, Agabiti-Rosei C, Agabiti-Rosei E. Use of Antihypertensive Drugs in Neoplastic Patients. High Blood Press Cardiovasc Prev. 2017;24(2):127-32. (see Chart 15.8 ).
| Key Takeaways |
|---|
| In the absence of clinical signs suggestive of secondary hypertension in adults, the indications for additional assessment are resistant hypertension and early- or late-onset hypertension and/or sudden BP increase. |
| Major causes of secondary hypertension, both endocrine and nonendocrine, signs, and diagnostic and screening methods can be found in Table 15.2. |
| The most frequent cause of secondary hypertension is primary aldosteronism (PA). The aldosterone/renin ratio is the best initial test to determine the need for additional PA assessments. Paroxysmal HT with triad consisting of headaches, sweating, and palpitations is found in pheochromocytoma. |
| Renal artery stenosis should be investigated when creatinine levels increase ≥ 50% after ACEI or ARB use. Recent-onset severe HT occurs in individuals > 55 years old with abdominal murmur and a > 1.5 cm size difference in the contralateral kidney. HT is severe in patients suffering from atherosclerosis or recurrent pulmonary edema. In young adults with severe HT, fibromuscular dysplasia of the renal artery should be considered. |
| Other causes of secondary hypertension require more specific diagnostic methods, expert knowledge, and experience in interpreting results. Treatment should be directed by specialists from referral centers. |
– Medications, hormones, and exogenous legal and illegal substances related to the development or increased severity of HT
16. Resistant And Refractory Hypertension
16.1. Definition and Classification
Resistant hypertension (RHT) is defined as office BP that remains ≥ 140/90 mm Hg with the use of three or more classes of antihypertensive medications with synergistic action, in maximum tolerated or recommended doses, one of which preferably a thiazide diuretic. When patients require four or more antihypertensive medications to achieve BP control, they are considered resistant but controlled hypertensives (BP < 140/90 mm Hg) ( Figure 16.1 ). 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.
– Classification of hypertension according to number of antihypertensive medications and blood pressure control.
Refractory hypertension (RfHT) is defined as a subgroup of patients with true RHT that maintain uncontrolled BP (BP ≥ 140/90 mm Hg), even when using four or more antihypertensives, including spironolactone and a long-acting diuretic ( Figure 16.1 ). 955955. Calhoun DA, Booth JN, Oparil S, Irvin MR, Shimbo D, Lackland DT et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63(3):451-8. Pseudo-resistant hypertension is defined as the failure to control BP related to white coat hypertension, failure at BP measurement, therapeutic inertia, or lack of adherence to prescribed pharmacological and nonpharmacological treatment regimens ( Figure 16.2 ). 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90. Identifying patients with true RHT, therefore, requires ruling out pseudo-resistance and associated conditions ( Figure 16.2 ), making it essential to establish specific approaches. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.
16.2. Epidemiology of Resistant Hypertension
In population-based studies, RHT prevalence is estimated at 12 to 15% of the hypertensive population. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90. In Brazil, the multicenter ReHOT study 564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. found an 11.7% prevalence rate for RHT. RfHT corresponds to 3.6% of resistant hypertensives. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
The main clinical conditions and characteristics associated with RHT patients can be found in Chart 16.1 . 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,956956. Oliveras A, de la Sierra A. Resistant hypertension: patient characteristics, risk factors, co-morbidities and outcomes. J Hum Hypertens. 2014;28(4):213-7. Worse prognoses for these patients is especially associated with the following factors: prolonged exposure to high blood pressure levels, end-organ damage, excess mineralocorticoids (aldosterone), and high sodium intake. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,956956. Oliveras A, de la Sierra A. Resistant hypertension: patient characteristics, risk factors, co-morbidities and outcomes. J Hum Hypertens. 2014;28(4):213-7.
16.3. Pathophysiology
Just as the pathophysiology of primary hypertension is multifactorial, multiple factors may also be involved in the genesis of RHT and RfHT. This determines the various degrees of refractoriness to antihypertensive medications ( Figure 16.1 ).
RHT depends more on increased blood volume than RfHT due to persistent fluid retention, increased salt sensitivity, hyperaldosteronism, and renal dysfunction. In addition, the greater expansion of chest plasma, urinary aldosterone concentration, discrete suppression of renin activity957and high plasma aldosterone/renin ratio, as well as high levels of atrial and brain natriuretic peptide (BNP) are found in these individuals. 958958. Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.
959. Calhoun DA. Refractory and Resistant Hypertension: Antihypertensive Treatment Failure versus Treatment Resistance. Korean Circ J. 2016;46(5):593-600.-960960. Eirin A, Textor SC, Lerman LO. Emerging concepts for patients with treatment-resistant hypertension. Trends Cardiovasc Med. 2016;26(8):700-6. The ratio between volume and high blood pressure is the primary physiopathological basis shown in several studies 955955. Calhoun DA, Booth JN, Oparil S, Irvin MR, Shimbo D, Lackland DT et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63(3):451-8.,957957. Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168(11):1159-64.
958. Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.
959. Calhoun DA. Refractory and Resistant Hypertension: Antihypertensive Treatment Failure versus Treatment Resistance. Korean Circ J. 2016;46(5):593-600.-960960. Eirin A, Textor SC, Lerman LO. Emerging concepts for patients with treatment-resistant hypertension. Trends Cardiovasc Med. 2016;26(8):700-6. ( Figure 16.3 ) and justifies the use of diuretic to treat RHT patients.961
In contrast, RfHT patients predominantly suffer from sympathetic nervous system hyperactivity and greater vascular stiffness. 962962. Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA et al. Refractory hypertension: evidence of heightened sympathetic activity as a cause of antihypertensive treatment failure. Hypertension 2015;66(1):126-33. Higher pulse wave velocity values, indicating elevated vascular stiffness and higher cytokine levels, such as tumor necrosis factor-α, 963963. Barbaro NR, de Araújo TM, Tanus-Santos JE, Anhê GF, Fontana V, Moreno H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed Res Int. 2015;1-8. may mediate vascular damage in refractory hypertensive patients. 964964. Barbaro NR, Fontana V, Modolo R, Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Press.2015;24(1):7-13. Other factors, such as age, obesity, obstructive sleep apnea (OSA), African-American descent, altered adipokines, endothelial dysfunction, and higher metalloproteinase-2 and -9 and adhesion molecule activity, are also involved in the process. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,895895. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. Gene polymorphisms, especially for RAAS and the endothelial nitric oxide synthase enzyme, have also been linked to RfHT 965965. Yugar-Toledo JC, Martin JF, Krieger JE, Pereira AC, Demacq C, Coelho OR, et al. Gene variation in resistant hypertension: multilocus analysis of the angiotensin 1-converting enzyme, angiotensinogen, and endothelial nitric oxide synthase genes. DNA Cell Biol. 2011;30(8):555-64. (Figures 16.4 and 16.5 ).
– Biomolecular systems measuring imbalance between increased aldosterone synthesis, sodium retention, OSA, increased RAAS activitity (AT1 and AT2 receptors) and hypertensive cardiac disease, and increased total vascular resistance, primarily induced by expanded plasma volume (salt retention and excess aldosterone) and sympathetic hyperactivity.
16.4. Diagnostic Investigation
Resistant hypertension patients should be treated by specialized HT services, capable of offering a multidisciplinary approach. Diagnostic investigation stands on four pillars: 341341. Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.,504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,966966. Aronow WS. Approaches for the management of resistant hypertension in 2020. Curr Hypertens Rep. 2020;22(1):3.
-
a) Pseudoresistance: Ruling out improper BP measurement (especially cuff width for obese patients), therapeutic inertia, poor adherence, and use of medications that increase BP (see Chapter 15). 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,967967. Corrêa NB, de Faria AP, Ritter AM, Sabbatini AR, Almeida A, Brunelli V, et al. A practical approach for measurement of antihypertensive medication adherence in patients with resistant hypertension. J Am Soc Hypertens. 2016;10(6):510-6.
-
b) Assessment of cardiovascular (CV) risk factor, end-organ damage (EOD), and established CV disease: Once RHT is confirmed, diagnostic investigation should begin with specific tests, following this guideline for hypertension, to assess EOD impairment and secondary hypertension. The presence of associated comorbidities should be detected in specialized tests and examinations, following clinical suspicion.
-
c) Ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM): The diagnosis of RHT is based on office BP, 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90. but out-of-office assessments (ABPM or HBPM) is essential to rule out the white-coat effect and masked hypertension. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,968968. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78. Diagnostic and therapeutic management should be based on ABPM and HBPM levels. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,968968. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.,969969. Muxfeldt ES, Salles GF. How to use ambulatory blood pressure monitoring in resistant hypertension. Hypertens Res. 2013;36:385-9. Patients with daytime and/or nighttime high blood pressure levels (true RHT or masked HT) should have their medications adjusted and repeat ABPM afterward. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,968968. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.,969969. Muxfeldt ES, Salles GF. How to use ambulatory blood pressure monitoring in resistant hypertension. Hypertens Res. 2013;36:385-9. Patients with controlled BP on ABPM should have their therapy regimen maintained, regardless of the office BP levels. For these individuals, ABPM should be repeated annually or semiannually. 968968. Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.,969969. Muxfeldt ES, Salles GF. How to use ambulatory blood pressure monitoring in resistant hypertension. Hypertens Res. 2013;36:385-9. HBPM may also be used when available. Although it does not assess the nocturnal period and overestimates blood pressure levels, HBPM achieves moderate agreement on diagnosis, with high specificity and low sensitivity. 970970. Muxfeldt ES, Barros GS, Viegas BB, Carlos FO, Salles GF. Is home blood pressure monitoring useful in the management of patients with resistant hypertension? Am J Hypertens 2015; 28(2):190-9.
-
d) Investigation of secondary causes: Secondary causes are more frequent for resistant than for nonresistant hypertension, and the most prevalent is OSA (80%), followed by hyperaldosteronism (6-23%), renovascular disease (renal artery stenosis) (2.5-20%), and renal parenchymal disease (2-10%). 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,895895. Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7. Investigating altered thyroid function (1-3%) is also warranted. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.
16.5. Treatment ( Chart 16.2 )
16.5.1. Nonpharmacological Treatment
All RHT patients should be directed and encouraged to adopt lifestyle changes 971971. Ozemek C, Tiwari S, Sabbahi A, Carbone S, Lavie CJ. Impact of therapeutic lifestyle changes in resistant hypertension. Prog Cardiovasc Dis. 2020;63(1):4-9. (see Chapter 8).
16.5.2. Pharmacological Treatment
The basic principle of pharmacological treatment is the combination of antihypertensive medications that act on most physiopathological mechanisms of BP increases: expanded intravascular volume, sympathetic and RAAS activation and increased peripheral vascular resistance. 504504. Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.,954954. Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.,972972. Acelajado MC, Hughes ZH, Oparil S, Calhoun DA. Treatment of resistant and refractory hypertension. Circ Res. 2019;124(7):1061-70. Three-drug treatment should include a thiazide diuretic (DIU), a RAAS blocker (ACE inhibitor or angiotensin II AT1 receptor blocker (ARB)), and long-acting dihydropyridine calcium channel blocker (CCB), at full, well-tolerated doses and adequate intervals. In case of coronary artery disease, heart failure or tachyarrhythmias, a beta-blocker (BB) should replace the CCB in the initial three-drug therapy regimen.
The correct use of DIUs is essential for treating RHT: chlorthalidone (25 mg/day) or indapamide (1.5 mg/day) are the diuretics of choice, as long as the estimated glomerular filtration rate (eGFR) is above 30 mL/min. However, at the time of this writing, only hydrochlorothiazide was available in the Brazilian public health system. In patients with stage 4 or 5 chronic kidney disease or heart failure with fluid retention, loop diuretics (furosemide) should be used instead of thiazides and administered as needed for pressure and volume control. Spironolactone (aldosterone antagonist, 25 to 50 mg/day) is the medication of choice to be added as the 4thdrug for patients with high adherence and true RHT. 564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.,567567. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68. For spironolactone-intolerant patients, amiloride (5 to 10 mg/day) may be used instead. 973973. Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. British Hypertension Society Programme of Prevention And Treatment of Hypertension With Algorithm based Therapy (PATHWAY) Study Group. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet . Diabetes Endocrinol. 2018;6(6):464-75.
For patients with uncontrolled blood pressure after adding spironolactone to the treatment regimen, BBs (especially those with vasodilatory effect) or centrally acting alpha-antagonists (clonidine) 564564. Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90. are the 5th/6th-line medications. If blood pressure control is still out of reach, direct-acting vasodilators (hydralazine and minoxidil) may be used as the 7thoption 974974. Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Hygia Project Investigators. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2019 Oct 22/ehz754 Online ahead of print..,975975. Berra E, Azizi M, Capron A, Høieggen A, Rabbia F, Kjeldsen SE, et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension. 2016;68(2):297-306.
ABPM-guided chronotherapy, with at least one antihypertensive medication administered at night (especially RAAS blockers and BBs) improves blood pressure control and reverses nondipper patterns for RHT patients in addition to lowering cardiovascular morbidity and mortality. 976976. Kunz M, Lauder L, Ewen S, Böhm M, Mahfoud F. The current status of devices for the treatment of resistant hypertension. Am J Hypertens. 2020;33(1):10-8.
Adherence to treatment is key for blood pressure control. However, up to 50% of patients with RHT partially or fully do not adhere to pharmacological treatment. 977977. Muxfeldt ES, Chedier B, Rodrigues CIS. Hipertensão resistente e refratária: duas faces de uma mesma doença? J Bras Nefrol . 2019; 41(2):266-74.
16.5.3. New Treatments
Various invasive treatments, such as endovascular renal sympathetic denervation, carotid baroreflex activation and modulation therapy, carotid body ablation, and central iliac arteriovenous anastomosis, have not been approved and are not to be used to treat resistant hypertensive patients, except as part of research protocols. 55. Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.,978978. Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.
| Key Takeaways |
|---|
| Resistant hypertensives are individuals adhering to treatment involving three or more classes of antihypertensive medications in optimized doses who do not progress to controlled blood pressure. |
| Refractory hypertensives are those adhering to treatment with five or more classes of antihypertensive medications in optimized doses who have uncontrolled blood pressure. |
| In Brazil, the prevalence of true resistant hypertension is 11.7% (ReHot Study). |
| Resistant hypertension depends more on volume, while sympathetic hyperactivity predominates in refractory hypertension. |
| For the three initial classes of medication for resistant hypertension, the keys are using diuretics, blocking the renin-angiotensin-aldosterone system, and using direct-acting vasodilators. |
17. Adherence to Antihypertensive Treatment
17.1. Introduction
The primary goal of initiating pharmacological and nonpharmacological antihypertensive treatment is to reduce the morbidity and mortality caused by high blood pressure (BP) levels. Though treatment has proven effectiveness and efficacy, hypertension (HT) control indices are still inadequate in most countries, including Brazil. 979979. Geldsetzer P, Manne-Goehler J, Marcus ME, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross- sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 2019 Aug 24;394(10199):652-62. A country-level systematic review and meta-analysis performed at the primary care level showed that HT control rates ranged from 43.7% to 67.5%. 980980. Picon RV, Dias-da-Costa JS, Fuchs FD, Olinto MTA, Choudhry NK, Fuchs SC. Hypertension Management in Brazil: Usual Practice in Primary Care. A Meta-Analysis. Int J Hypertens. 2017; 2017: 1274168. There are many reasons for the lack of hypertension control, but one of the most important is the lack of adherence to treatment, which can have various reasons.
17.2. Concept and Adherence
In a 2003 report, 981981. World Health Organization (WHO). : Adherence to long-term therapies: evidence for action. Geneva;2003. the World Health Organization (WHO) defined adherence as “the extent to which a person's behaviour—taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider.” The primary reason for inadequate HT control seems to be nonadherence with long-term treatments, both for lifestyle changes (LSCs) and for taking the medications prescribed. In 2012, in a new WHO report, the authors differentiate the processes involved, such as adherence to medication and adherence management. 982982. Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. ABC Project Team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012; 73:691–705. According to the those guidelines, adherence to medication is made of three major components: initiation, implementation, and discontinuation. Initiation is the time from prescription to taking the first dose of the medication; implementation corresponds to the coincidence between dose taken by the patient and dose prescribed; and discontinuation indicates the break in the process, when the next dose to be taken is skipped and the treatment is later interrupted. 982982. Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. ABC Project Team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012; 73:691–705.
Though there are various synonyms for adherence, such as compliance, conformity and capacitance, the proper term for HT treatment is still “adherence.” Adherence issues are often hard to detect and even harder to quantify. To improve HT control, it is important to combine efforts in order to identify patients who are not adhering to their treatment. Dropout rates are high in the first months of treatment, and patients may also not follow their prescription when taking medications. This situation has been described in medical literature since the 1970s 983983. Haynes RB, Sackett DL, Gibson ES, Taylor DW, Hackett BC, Roberts RS, et al. Improvement of medication compliance in uncontrolled hypertension. Lancet 1976;1(7972):1265-8. and is still found in more recent reports. 984984. Gialamas A, Yelland LN, Ryan P, Willson K, Laurence CO, Bubner TK, et al. Does point-of-care testing lead to the same or better adherence to medication? A randomised controlled trial: the PoCT in General Practice Trial. Med J Austr. 2009;191:487-9.,985985. Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(9):882-7. Lack of adherence to treatment is frequently defined as hypertensive patients taking less than 80% of prescribed medications. However, the spectrum of nonadherence from zero to over a 100% for those who take more than prescribed, which is also considered nonadherence to treatment.
17.3. Treatment Adherence Assessment Methods
There are many ways of measuring adherence to antihypertensive pharmacological treatment in clinical practice and in research, divided into direct methods, in which there is objective proof the patient has taken the medication, and indirect methods, where various strategies estimate whether the prescribed medication has or has not been taken. Choice of methods depends on for what purpose the information obtained will be used, the resources available for assessment, acceptance, how convenient the method is for the patient, and the costs involved. 986986. Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski M. How to Screen for Non-Adherence to Antihypertensive Therapy. Curr Hypertens Rep. 2016;18(12):89. Measuring adherence is a complex task. There is no single gold standard method capable of encompassing the various facets of the process. 344344. Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45.
The WHO suggests combining an indirect method and a direct one to measure adherence 984984. Gialamas A, Yelland LN, Ryan P, Willson K, Laurence CO, Bubner TK, et al. Does point-of-care testing lead to the same or better adherence to medication? A randomised controlled trial: the PoCT in General Practice Trial. Med J Austr. 2009;191:487-9. for chronic illnesses. In HT, indirect methods wind up the most widely utilized, since direct methods still lack validation, are more expensive, and are only available in research environments.
Structured self-reported scales are widely used in clinical research, such as the Morisky-Green Medication Adherence Scale. The Eight-Item Morisky Medication Adherence Scale 987987. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008; 10(5):348-54. evolved from a previous four-item scale, 988988. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care, 1986; 24(1):67-74. is more reliable (α= 0,83 versus α= 0,61) and has been validated for Brazilian Portuguese. 989989. de Oliveira-Filho AD, Morisky DE, Neves SJF, Costa FA, de Lyra Junior DP. The 8-item Morisky Medication Adherence Scale: Validation of a Brazilian–Portuguese version in hypertensive adults. Res Social Adm Pharm. 2014; 10:554–561. The total score is classified as follows: 8 points mean high adherence; 6-7, medium adherence; below 6, low adherence. Another instrument is the three-question Qualiaids Medication Adherence Questionnaire (QAM-Q), created by Brazilian authors. In terms of accurately detecting nonadherence, QAM-Q has 62.5% sensitivity and 85.7% specificity, 74.1% area under the ROC curve, and 90.9% positive predictive value. 990990. Santa Helena ET, Nemes MIB, Eluf-Neto J. Desenvolvimento e validação de questionário multidimensional para medir não-adesão ao tratamento com medicamentos. Rev. Saúde Pública [online]. 2008; 42(4):764- 7.
A review article on the subject of adherence and HT highlights the importance of increasing the availability and accessibility of more accurate measures to assess adherence. It also stresses that this is the main reason recent guidelines have emphasized the need to discuss medication adherence as a key issue in treating HT. 991991. Burnier M, Egan BM. Adherence in Hypertension A Review of Prevalence, Risk Factors, Impact, and Management. Circ Res. 2019;124:1124-40. Chart 17.1 clarifies the advantages and disadvantages of several pharmacological treatment adherence assessment methods. 992992. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-97.
17.4 Factors Interfering in Adherence to Treatment
Adherence to treatment is a complex, multidimensional process, with barriers divided into five different dimensions ( Chart 17.2 ) 985985. Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(9):882-7.,993993. Dhar L, Dantas J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol. 2017; 7(3):211-50.
994. Abegaz TM, Shehab A, Gebreyohanne EA. Nonadherence to Antihypertensive Drugs: A Systematic Review Meta-Analysis. Medicine. 2017;96(4):e5641.
995. Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD005182.-996996. van der Laan DM, Elders PJM, Boons CCLM, Beckeringh JJ, Nijpels G, Hugtenburg JG. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens. 2017;31(11):687-94. that provide health care professionals with a more comprehensive perspective and enable to development of more effective interventions to improve BP control. Factors such as age, income, schooling and ethnicity/race play a major role in low socioeconomic status areas. The local health system and the nature of the health care staff may also influence adherence by hypertensive patients. In terms of disease and treatment, the most relevant factors are the chronic nature of HT and the absence of symptoms, the lifelong nature of the treatment and the complex drug regimen involved in some cases, and the undesirable side effects and drug interactions. Patient-related factors include disengagement with one's health issues and forgetting to take the medication.
17.5. Strategies to promote adherence to antihypertensive treatment
The main consequence of lack of adherence to treatment is the lack of HT control and, therefore, increased end-organ damage (EOD) and cardiovascular (CV) morbidity and mortality. These, in turn, have major economic impact, in consequence of greater health care spending and early retirement. Therefore, adopting strategies to promote better adherence to antihypertensive treatment, either in isolation or in combination, as summarized in Chart 17.3 , intends to change that scenario. 197197. Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens 2013;31(3):455–67; discussion 467–8.,997997. Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension. 2010;55(2):399–407.
998. Santschi V, Chiolero A, Colosimo AL, Platt RW, Taff. P, Burnier M, Burnand B, Paradis G. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
999. Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, Debusk RF. Nurse management for hypertension. A system approaches. Am J Hypertens. 2004;17(10):921–7.
1000. Checchi KD, Huybrechts KF, Avorn J, Kesselheim AS. Electronic medication packaging devices and medication adherence: a systematic review. JAMA. 2014;312((12):1237–47.
1001. Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62(2):218–25.
1002. Christensen A, Osterberg LG, Hansen EH. Electronic monitoring of patient adherence to oral antihypertensive medical treatment: a systematic review. J Hypertens. 2009;27(8):1540–51.
1003. Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone applications for hypertension management: a potential game-changer that needs more control. Curr Hypertens Rep. 2017;19(6):48.
1004. Naik AD, Kallen MA, Walder A, Street RL Jr. Improving hypertension control in diabetes mellitus: the effects of collaborative and proactive health communication. Circulation. 2008;117(11):1361–8.
1005. Conn VS, Ruppara TM, Enriqueza M, Cooper P. Medication adherence interventions that target subjects with adherence problems: Systematic Review and Meta-analysis. Res Social Adm Pharm. 2016; 12(2): 218–46.-10061006. VS, Ruppara TM. Medication Adherence Outcomes of 771 Intervention Trials: Systematic Review and Meta-Analysis. Prev Med. 2017; 99: 269–276.
The strategies with the best evidence available and which could be more feasibly implemented in Brazil include:
-
• Self-measured BP (Level of Recommendation I/Level of Evidence B);
-
• More convenient dosing regimens: lower possible doses, single daily dose, combination of antihypertensives in a single pill (Level of Recommendation I/Level of Evidence A);
-
• Deploying multidisciplinary teams to care for hypertensive patients, including physicians, nurses, pharmacists, physical educators, physical therapists, nutritionists, psychologists, social workers, and community health workers (Level of Recommendation I/Level of Evidence B).
17.6. Conclusion
Optimizing antihypertensive treatment adherence indices contributes to lower morbidity, mortality, and health care costs. Current therapeutic options include both pharmacological and nonpharmacological treatment regimens with proven effectiveness. Adherence to treatment plans and consequent hypertension control is still a major challenge in health care. Thus, combining efforts to met the actual needs of hypertensives has become the primary objective in the work of changing the current hypertension scenario.18. Perspectivas
| Key Takeaways |
|---|
| HT control rates in Brazil are still unsatisfactory. There are many reasons for the lack of hypertension control, but one of the most important is the lack of adherence to treatment. |
| Adherence to treatment is a complex, multidimensional process, where we can identify barriers connected to sociodemographic conditions, pharmacological treatment, health care systems, patients, and the disease itself. |
| Adherence issues are often hard to detect and even harder to quantify. |
| Measuring adherence is a complex task. There is no single gold standard method capable of encompassing the various facets of the process. |
| The strategies with the best evidence available and which could be more feasibly implemented in Brazil are: • Self-measured blood pressure (LR: I, LE: B); • More convenient dosing regimens: lower possible doses, single daily dose, combination of antihypertensives in a single pill (LR I/LE A); • Deploying multidisciplinary teams to care for hypertensive patients, including physicians, nurses, pharmacists, physical educators, physical herapists, nutritionists, psychologists, music therapists, social workers, and community health workers (LR I/LE B). |
18. Perspectives
18.1. Introduction
The goal of this chapter is to discuss, based on evolving scientific knowledge about hypertension in the last few decades and more recent evidence, the possible advances and adjustments that will impact daily clinical practices and the challenges involved in diagnosis, treatment, and follow-up for hypertensive patients. It should be stressed that, unlike the previous chapters, where recommendations were rigorously classified by level of scientific evidence and level of recommendation, this section was designed to introduce possible rational vistas, based on the knowledge we have acquired thus far for this complex, multifactorial disease, with cardiovascular (CV), cerebral, and renal consequences that heavily determine morbidity and mortality, to the point that it has become the leading cause of death throughout the world.
18.2. Definition, Epidemiology, and Primary Prevention
With the gradual rise in life expectancy in both developed and developing countries, prevalence rates for hypertension (HT) are likely to increase even more. On average, there was a 1.4-year gain per decade of life in developed countries and a 1.2-year gain in Latin American countries from 1980 to 2011. 10071007. Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet 2015; 385(9967): 540–8. It is widely known that, as we grow older, blood pressure levels increase, and from age 60 onward, systolic blood pressure (SBP) increases while diastolic blood pressure (DBP) decreases. This leads to higher pulse pressure (PP). These are important aspects when assessing risk factors and treatment strategies ( Figure 18.1 ). 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,10081008. Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Merz NB, et al. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020;5(3):19-26.
18.3. Blood Pressure and Vascular Damage
The increase in CV risk starting at SBP = 115 mm Hg and DBP = 75 mm Hg is well-known, 7878. Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13. and BP measures remain the diagnostic marker of hypertensive disease. However, science is still trying to better understand biomarkers capable of early identification of vascular damage in hypertensive disease, even before the onset of higher BP values, as well as to develop their clinical applicability. The goal is to increase the accuracy of CV risk stratification in low- to moderate-risk individuals. 8282. Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness A Scientific Statement from the American Heart Association. Hypertension. 2015; 66(3):698-722.,139139. Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífkova R, Cosentino F et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241(2):507-32.,10101010. Brandão AB, Amodeo C, Alcantara C, Barbosa E, Nobre F, et al. I Luso Brazilian Positioning Paper on Central Arterial Pressure. Arq Bras Cardiol. 2017; 108(2):100-8.
Central systolic blood pressure assessments and arterial stiffness assessed by pulse wave velocity (PWV) are based on robust evidence with the goal of early identification of vascular damage and the ability to identify and restratify individuals initially classified as having low to moderate risk but who could actually be at high risk. In addition, PWV values above 10 m/s may indicate the presence of subclinical end-organ damage, 156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46.,298298. Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63.,10111011. Hamczyk Nevado RM, Barettino A, Fuster V, Andrés V. Biological Versus Chronological Aging. J Am Coll Cardiol. 2020; 75(8): 919-30. and increased central systolic BP is a predictor of the development of hypertension. 10121012. Sugiura T, Takase H, Machii M, Nonaka D, Ohno K, et al. Central blood pressure predicts the development of hypertension in the general population. Hypertens Res. 2020;43(11):1301-8. Another way of assessing vascular damage is the ability to identify lost or impaired endothelial function, as well as to understand its pathophysiology, which includes genetic predisposition and chronological aging, as well as changes in inflammatory and immune activity, insulin sensitivity, and cholesterol-rich lipoproteins. 112112. Konukoglu D, Uzun H. Endothelial Dysfunction and Hypertension. Adv Exp Med Biol. 2017; 956:511-40.,114114. Boos CJ, Lip GY. Is hypertension an inflammatory process? Curr Pharm Des. 2006; 12(13):1623-35.
Currently, the method most widely used to analyze in vivo endothelial function is flow-mediated dilation (FMD), but it remains restricted to research settings. 118118. Thijssen DHJ, Bruno RM, van Mil ACCM, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019; 40(30):2534-47. It is possible that, with new evidence in hypertensive and cardiovascular disease, the method will become more reliable and safe for use in clinical practice, further enhancing the early identification of vascular damage. 10131013. Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic Value of Flow-Mediated Vasodilation in Brachial Artery and Fingertip Artery for Cardiovascular Events: A Systematic Review and Meta-Analysis J Am Heart Assoc. 2015; 134(11): e002270.,10141014. Wu MY, Li CJ, Hou MF, Chu PY.New Insights into the Role of Inflammation in the Pathogenesis of Atherosclerosis. Int J Mol Sci. 2017;18(10:2034.
18.4. Cardiac Biomarkers
Though there has been great progress in the search for markers to estimate arterial damage, we cannot underestimate older tests that identify CV risk, such as electrocardiogram (ECG), magnetic resonance or, more recently, coronary calcium score, among others, for diagnosis of left ventricular hypertrophy (LVH). 10151015. Grossman C, Levin M, Koren-Morag N, Bornstein G, Leibowitz A, Ben-Zvi I, et al. Left Ventricular Hypertrophy Predicts Cardiovascular Events in Hypertensive Patients with Coronary Artery Calcifications. Am J Hypertens. 2018;31(3):313-20.,10161016. McEvoy JW, Martin SS, Dardari ZA, Miedema MD, Sandfort V, Yeboah J, et al. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation 2017;135(2):153–65. There is robust evidence in favor of using B-type natriuretic peptides and N-terminal pro-B-type natriuretic peptides (NT-proBNP) as well as high-sensitivity Troponin T (hs-TnT), in risk stratification for fatal or nonfatal CV events and all-cause mortality. B-type natriuretic peptides are secreted by myocytes as counterregulatory response to pressure or volume overload of the myocardial wall, to increased sympathetic tone and to vasoconstriction, but also integrate CV stress and hemodynamic from multiple sources. 10171017. Kerkelä R, Ulvila J, Magga J. Natriuretic Peptides in the Regulation of Cardiovascular Physiology and Metabolic Events. J Am Heart Assoc. 2015; 4(10):e002423. Cardiac troponins are structural proteins in the contractile mechanism of heart muscle cells, secreted into circulation after cell damage. 10181018. Willeit P, Welsh P, Evans JDW, Tschiderer I, Boachie C, Jukema JW, et al. High-Sensitivity Cardiac Troponin Concentration and Risk of First-Ever Cardiovascular Outcomes in 154,052 Participants. J Am Coll Cardiol. 2017;70(5):558-68.
A recent study found that simply raising NT-proBNP and/or hs-TnT in prehypertensive patients enabled the identification of approximately 1/3 of those that who would later have CV outcomes or be admitted for heart failure (HF) within 10 years, individuals who could potentially benefit from pharmacological treatment. 10191019. Pandey A, Patel KV, Vongpatanasin W, Ayers c, Berritz JD, Mentz RJ, et al. Incorporation of Biomarkers Into Risk Assessment for Allocation of Antihypertensive Medication According to the 2017 ACC/AHA High Blood Pressure Guideline: A Pooled Cohort Analysis. Circulation. 2019;140(25):2076-88. It has also been shown that NT-proBNP can estimate all-cause mortality and nonfatal CV outcomes for high-risk hypertensive diabetes patients in 2.6 years with the same predictive power as the whole set of the 20 most significant clinical and laboratory variables use most frequently, such as hs-TnT, age, albumin, history of HF, heart rate, history of stroke, HbA1c, smoking, LVH in ECG, ECG Q-waves, history of atrial fibrillation, any branch block in ECG, urine albumin/creatinine ratio, SBP, sex, history of coronary artery disease, low-density lipoprotein cholesterol, estimated glomerular filtration rate, insulin use, and DBP. 10201020. Malachias MVB, Jhund PS, Claggett BL, Wijkman MO, Bentley-Lewis R, Chaturvedi N, et al. NT-pro BNP by Itself Predicts death and cardiovascular events in high-risk patients with type 2 Diabetes Mellitus. J Am Heart Assoc. 2020;9(19):017462.
18.5. Diagnosis and Classification
HT diagnosis, based on in-office measurement results and using proper techniques and devices, is defined as SBP ≥ 140 mm Hg and DBP ≥ 90 mm Hg. 164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83. The latest international guidelines recommend that HT diagnosis, whenever possible, be based on in-office blood pressure measurements, preferably unattended, or else by out-of-office measurements (ABPM and HBPM). In addition, there is a debate whether reference values to establish HT should be even lower or not. 3737. Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.,164164. Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.,186186. Nobre F, Mion Jr. D, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 110(5Supl.1):1-29.,10211021. lar R, Sánchez R, Boggia R, Peñaherrera, Lopez J, Barroso WS. Recommendations for home blood pressure monitoring in Latin American countries: A Latin American Society of Hypertension position paper. J Clin Hypertens(Greenwich).2020;22(4):544-54.
It seems clear that identifying HT, whether treated or untreated, by phenotype allows for risk stratification and for the definition of more individualized treatment strategies. 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,212212. Barroso WKS, Feitosa ADM, Barbosa ECD, Miranda RD, Vitorino PVO, Brandão AA, et al Prevalence of Masked and White-Coat Hypertension in Pre-Hypertensive and Stage 1 Hypertensive patients with the use of TeleMRPA. Arq Bras Cardiol .2019;113(5):970-5. Another interesting topic is the use of self-measured blood pressure (SMBP) as a method for increasing patient engagement with their own illness and improving adherence to treatment, in addition to providing health care professionals with more information about the patient's everyday BP levels. 10221022. Shimbo D, Artenian N, Basile JN, Krakoff LR, Margolis K, Rackotz MK, et al. Self-measured blood pressure monitoring at home. A Joint Policy Statement From the American Heart Association and American Medical Association Circulation.2020;142(4):e42-e63.
The COVID-19 pandemic means acknowledging the global development of telemedicine techniques is critical. Apparently, distance monitoring through digital platforms and mobile applications for hypertensive patients has come to stay, facilitating conversations between health care teams and patients and the consequent information exchange and beneficial adjustments to lifestyle changes and even to treatment itself, with more focus on prevention and improving disease control. However, digital technology may further expand the scope of hypertension, following the lead of diabetes mellitus, enabling the development of increasingly accurate, continuous cuff-less blood pressure monitoring devices, syncing up with the smartphones that are now within reach for most of the population. 388388. Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7.,10231023. Mukherjee R, Ghosh S, Gupta B, Chakravarty T. A Universal Noninvasive Continuous Blood Pressure Measurement System for Remote Healthcare Monitoring. Telemed J E Health. 2018;24(10):803-10.,10241024. Bard DM, Joseph JI, van Helmond N. Cuff-Less Methods for Blood Pressure Telemonitoring. Front Cardiovasc Med. 2019;6:40.
Finally, it is possible that in coming years, more attention given to patients with SBP ≥ 130 mm Hg and DBP ≥ 85 mm Hg (now classified as prehypertensive in these and in other guidelines) will change our understanding of HT diagnoses. 10251025. Fuchs FD, Whelton PK. High Blood Pressure and Cardiovascular Disease. Hypertension 2020 Feb;75(2):285-92.
18.6. Complementary Assessment and Cardiovascular Risk Stratification
The use of biomarkers for early identification of subclinical injuries, as well as higher CV risk, even at the early stages of high BP, brings with it the expectation that, for specific indications, individuals could and should receive early care for their conditions. 139139. Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífkova R, Cosentino F et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241(2):507-32. There are also biomarkers for vascular damage. For some, like the ankle-brachial index (ABI), calcium score and PWV, 298298. Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63.,10111011. Hamczyk Nevado RM, Barettino A, Fuster V, Andrés V. Biological Versus Chronological Aging. J Am Coll Cardiol. 2020; 75(8): 919-30. there is evidence in favor of the previous statements, though they are not widely available in clinical practice. Meanwhile, others, such as FMD, are still restricted to research settings. 118118. Thijssen DHJ, Bruno RM, van Mil ACCM, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019; 40(30):2534-47. Furthermore, researchers are currently working on a set of substances associated with inflammation that may ultimately be closely connected to endothelial dysfunction and to atherosclerosis, but which still require more robust evidence before they can be used in clinical practice. 180180. Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.,271271. Mikael LR, Paiva AMG, Mota-Gomes M, Sousa ALL, Jardim PCBV, Vitorino PVO, et al. Envelhecimento vascular e rigidez arterial. Arq Bras Cardiol. 2017;109(3):253-8.,10141014. Wu MY, Li CJ, Hou MF, Chu PY.New Insights into the Role of Inflammation in the Pathogenesis of Atherosclerosis. Int J Mol Sci. 2017;18(10:2034.,10221022. Shimbo D, Artenian N, Basile JN, Krakoff LR, Margolis K, Rackotz MK, et al. Self-measured blood pressure monitoring at home. A Joint Policy Statement From the American Heart Association and American Medical Association Circulation.2020;142(4):e42-e63.,10261026. Palombo C, Kozakova, M Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vasc Pharmacol. 2016; 77:1–7.
In terms of CV risk stratification, the progressive integration of biomarkers will allow us to more accurately establish the true risk level for each individual, especially for intermediate-risk hypertensive patients. Approaches of this sort offer the possibility of a more personalized medicine, with greater assertiveness in decisions connected to classification and treatment. 156156. Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46.,298298. Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63.,10111011. Hamczyk Nevado RM, Barettino A, Fuster V, Andrés V. Biological Versus Chronological Aging. J Am Coll Cardiol. 2020; 75(8): 919-30.
In addition, in the field of precision medicine, usually based on genomics and metabolomics, there are already validated clinical scores capable of identifying patients at higher risk of early hypertension, as well as reference values for some of those biomarkers for the Brazilian population, adjusted for sex and age. The possibility of less sophisticated markers certainly works towards the improvements in accuracy we want to provide indications for specific assessments in clinically preselected patients, as is already usually the case in the investigation of secondary HT in the presence of clinical signs and positive screening tests. 158158. Xaplanteris P, Vlachopoulos C, Protogerou AD, Aznaouridis K, Terentes-Printzios D, Argyris AA, et al. A clinical score for prediction of elevated aortic stiffness: derivation and validation in 3943 hypertensive patients. J Hypertens. 2019,37:339–4.,159159. Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP et al. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Jun 12.doi: 10.1038/s41440-020-0490 online ahead of print.
https://doi.org/10.1038/s41440-020-0490 ...
18.7. Goals and Treatment
Following the scientific advancements and proofs discussed in the previous sections, it is reasonable to imagine that, in particular situations, early treatment onset and the pursuit of lower BP control targets may be indicated to prevent outcomes associated with increased BP and to minimize the so-called residual risk. 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,10271027. Morales SA, Coca A, Olsen MH, Sanchez RA, Sebba-Barroso WK, Kones R, et al. Clinical Perspective on Antihypertensive Drug Treatment in Adults With Grade 1 Hypertension and Low-to-Moderate Cardiovascular Risk: An International Expert Consultation. Curr Probl Cardiol. 2017 Jul;42(7):198-225. In addition, the pharmacological treatment strategy based on two- or even three-drug combinations (at low doses), even at the early stages of the disease, should become increasingly prominent in guideline recommendations, while monotherapy may become an important strategy for individuals now classified as high-risk prehypertensives or those with changes in biomarkers ( Figure 18.2 ). 307307. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.,10231023. Mukherjee R, Ghosh S, Gupta B, Chakravarty T. A Universal Noninvasive Continuous Blood Pressure Measurement System for Remote Healthcare Monitoring. Telemed J E Health. 2018;24(10):803-10.,10281028. Feitosa AD, Gomes MM, Passarelli Júnior O, Barroso WKS, Miranda RDS, Barbosa EDB, et al. Pharmacological Treatment of Hypertension: From the Golden Trio to the Octet Arq Bras Cardiol. 2020; 115(2):270-2.,10291029. Campana E, Cunha V, Glaveckaite S, Gruev I, Lamirault G, Lehmann E. The use of single-pill combinations as first-line treatment for hypertension: translating guidelines into clinical practice. J Hypertensi. 2020, 38:000-000 ahead of print
It is possible that in the world of hypertension, according to current studies, our goal may be to control central and peripheral BP parameters, as long as that strategy can prove its ability to maximize reductions in major CV and renal outcomes. 10301030. Laurent S, Chatellier G, Azizi M, Calvet D, Choukroun G, Danchin N, et al.A Strategy for Preventing Cardiovascular and Renal Events based on Arterial Stiffness. Protocol of the SPARTE Study.[Cited in 2020 Jul 20] Available from: https://clinicaltrials.gov/ct2/show/NCT02617238
https://clinicaltrials.gov/ct2/show/NCT0...
,10311031. Barroso WKS, Inuzuka S, Guimarães GC, Pacífico RP, Melo VA, Oliveira LF, et al. Pharmacological Management of Hypertension Guided by Central or Peripheral Blood Pressure Measurement: Comparison of Two Strategies on the Incidence of Intermediate Outcome. Artery Research. 2020;26(1):1-4. Finally, though the prospect seems far-off, there is a real possibility that highly specific molecular tools will be available for HT treatment, such as RNA-mediated interference, which is simply post transcription gene silencing (PTGS) of overexpression of the protein of interest. 388388. Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7.,10321032. Arendse LB, Danser AHJ, Poglitsch M, Touyz RM, Burnett JC, Llorens-Cortesc, et al. novel therapeutic approaches targeting the renin-angiotensin system and associated peptides in hypertension and heart failure. Pharmacol Rev. 2019;71(4):539-70. Gene therapy for HT seems promising and has led to proven results in experimental studies involving the target-gene encoding the hepatic angiotensinogen. However, there is a known path for its clinical application after it is proven to be selective, effective and, above all, safe. Though many important perspectives are on the table, apparently the greatest challenge of all, in Brazil and worldwide, is much simpler. Its goals include improving diagnosis, adequate treatment, teamwork, and better blood pressure control in order to achieve significant reductions in renal and cardiovascular morbidity and mortality.
Referências
-
1Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017; 317(2):165-82.
-
2Anderson AH. Yang W, Townsend RR, Pan Q, Chertow GM, Kusek JW, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann. Intern. Med. 2015; 162(4): 258-65.
-
3Précoma DB, Oliveira GMM, Simão AF, Dutra OP, Coelho OR, Izar MCO, et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brazileira de Cardiologia – 2019. Arq Bras Cardiol. 2019; 113(4):787-891.
-
4Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al 2019, ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. JACC. 2019; 74(10):e177-232.
-
5Whelton PK, Carey RM, Aronow WS, Casey Jr. DE, Collins KJ, Himmelfarb CD, et al. 2017 Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol.; 201; 23976.
-
6Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension. JACC Health Promotion Series. J Am Coll Cardiol. 2018;71(19):2199-269.
-
7Menni C, Mangino M, Zhang F, Clement G, Snieder H, Padmanabhan S, et al. Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens. 2013; 31(12):2356-61.
-
8Singh GM, Danaei G, Pelizzari PM, Lin JK, Cowan MJ, Stevens GA, et al. The age associations of blood pressure, cholesterol, and glucose: analysis of health examination surveys from international populations. Circulation. 2012;125(18): 2204-11.
-
9Brazil. Ministério da Saúde. Vigitel Brazil, 2016: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico. Brasília;2016.
-
10Mente A, O’Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392(10146):496–506.
-
11Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, et al. Intersalt revisited: further analyses of 24 hours sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312(7041):1249-53.
-
12Mill JG, Malta DC, Machado ÍE, Pate A, Pereira CA, Jaime PC, et al. Estimativa do consumo de sal pela população Brazileira: resultado da Pesquisa Nacional de Saúde 2013. Rev Bras Epidemiol [Internet]. 2019;22(suppl 2):E190009. [Citado em 2020 Mar 10]. Disponível em: http://www.scielo.br/pdf/rbepid/v22s2/1980-5497-rbepid-22-s2-e190009-supl-2.pdf .
» http://www.scielo.br/pdf/rbepid/v22s2/1980-5497-rbepid-22-s2-e190009-supl-2.pdf -
13Araujo MC, Bezerra IN, Barbosa F dos S, Junger WL, Yokoo EM, Pereira RA, et al. Consumo de macronutrientes e ingestão inadequada de micronutrientes em adultos. Rev Saude Publica [Internet]. 2013;47(Supl.1):1775–895. [Acesso em 10 de mar 2020]. Disponível em: http://dx.doi.org/10.1590/S0034-89102013000700004 .
» http://dx.doi.org/10.1590/S0034-89102013000700004 -
14Guthold R, Stevens, GA, Riley, LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health. 2018;6(10):e1077-e1086.
-
15Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108–e120.
-
16Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: the Atherosclerosis Risk in Communities Study. Hypertension. 2001;37(5):1242–50.
-
17Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.
-
18NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55.
-
19Plavnik FL. Hipertensão arterial induzida por drogas: como detectar e tratar. Rev Bras Hipertens. 2002; 9:185-91.
-
20Ahmad M, Makati D, Akbar S. Review of and Updates on Hypertension in Obstructive Sleep Apnea. Int J Hypertens. 2017; 2017:1848375. https://doi.org/10.1155/2017/1848375 .
» https://doi.org/10.1155/2017/1848375 -
21GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980- 2016: a systematic analysis for the Global Burden of Disease Study . Lancet. 2017;390(10100):1151-210.
-
222017. Lancet. 2016;390:1151–210. Causes of Death 2008 [online database]. Geneva, World Health Organization. [Cited in 2020 Mar 10] Available from: http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf
» http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf -
23Brazil. Ministério da Saúde. DATASUS/MS/SVS/CGIAE - Sistema de Informações sobre Mortalidade SIM. [Acesso em 19 de abr 2020]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID 10-Capitulos I00-I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def .
» http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sim/cnv/obt10uf.def/2017-CID» http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def -
24Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PFA. WHO analysis of causes of maternal death: a systematic review. Lancet.2006;367(9516):1066-74.
-
25Udani S, Lazich I, Bakris GL. Epidemiology of hypertensive kidney disease. Nat Rev Nephrol. 2011;7(1):11-21.
-
26Brazil. Ministério da Saúde. DATASUS. Sistema de Informações Hospitalares do SUS(SIH/SUS). {Internet} Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/nruf.def/2008-2018/ CID 10-Capitulos I00 I99; http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def . Acessado em 19/03/2020.
» http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sih/cnv/nruf.def/2008-2018/» http://tabnet.datasus.gov.br/cgi/tabcgi.exe?ibge/cnv/poptuf.def -
27Malta DC, Gonçalves RPF, Machado IE, Freitas MIF, Azeredo C, Szwarcwald CL et al. Prevalência da hipertensão arterial segundo diferentes critérios diagnósticos. Pesquisa Nacional de Saúde. Rev Bras Epidemiol. 2018; 21(sup 1): E180021.
-
28Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Custos atribuíveis à obesidade, hipertensão e diabetes no Sistema Único de Saúde em 2018. Rev Panam Salud Publica. 2020;44:e32.
-
29EAF, Silva EN, Jaime PC. Developing and applying a costing tool for hypertension and related cardiovascular disease: attributable costs to salt/sodium consumption. J Clin Hypertens. 2020;22(4):642-8.
-
30Dickey RA, Janick JJ. Lifestyle modifications in the prevention and treatment of hypertension. Endocr Pract. 2001; 7 (5):392-9.
-
31Perumareddi P. Prevention of hypertension related to cardiovascular disease. Prim Care. 2019;46(1):27-39.
-
32Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension (Review) Exp Ther Med. 2016;12(4):2395-9.
-
33Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2.3 million participants. Obes Rev. 2018;19(5):654-67.
-
34Zhao Y, Qin P, Sun H, Liu Y, Liu D, Zhou Q, et al. Metabolically healthy general and abdominal obesity are associated with increased risk of hypertension. Br J Nutr. 2020;123(5):583-91.
-
35Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-87.
-
36Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, et al. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database Syst Rev. 2016;Mar 2;3:CD008274.
-
37Williams B, Mancia G, Spiering W, Agabiti RE, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
-
38Schwingshackl L, Chaimani A, Schwedhelm C, Toledo E, Pünsch M, Hoffmann G, et al. Comparative effects of different dietary approaches on blood pressure in hypertensive and pre-hypertensive patients: A systematic review and network meta-analysis. Crit Rev Food Sci Nutr. 2019;59 (16): 2674-87.
-
39Pergola G, D’Alessandro A. Influence of Mediterranean Diet on Blood Pressure. Nutrients. 2018;10 (1700):1-6.
-
40Ozemek C, Laddu DR, Arena R, Lavie CJ. The role of diet for prevention and management of hypertension. Curr Opin Cardiol. 2018;33(4):388-93.
-
41Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium Intake and Hypertension. Nutrients. 2019;11(9):1970.
-
42Jafarnejad S, Mirzaei H, Clark CCT, Taghizadeh M, Ebrahimzadeh. The hypotensive effect of salt substitutes in stage 2 hypertension: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20(98):1-15.
-
43Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. J Am Med Assoc. 1997;277(20):1624–32.
-
44Stone MS, Martyn L, Weaver CM. Potassium Intake, Bioavailability, Hypertension, and Glucose Control. Nutrients. 2016;8(444):1-13.
-
45Filippini T, Violi F, D’Amico R, Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int J Cardiol. 2017. 230:127-35.
-
46Poorolajal J, Zeraati F, Soltanian AR, Sheikh V, Hooshmand E, Maleki A. Oral potassium supplementation for management of essencial hypertension: A meta–analysis of randomized controlled trials. Plos One. 2017;12(4):1- 6.
-
47Caligiuri SPB, Pierce GN. A review of the relative efficacy of dietary, nutritional supplements, lifestyle, and drug therapies in the management of hypertension. Crit Rev Food Sci Nutr. 2017;57(16):3508-27.
-
48World Health Organization. (WHO). Global status report on noncommunicable diseases.Geneva; 2014. ISBN 978 92 4 156485 4.
-
49Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990– 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859): 2224−60.
-
50Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473.
-
51Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(3):327-34.
-
52Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39(2):88-94.
-
53Leitzmann MF, Park Y, Blair A, Ballard-Barbash R, Mouw T, Hollenbeck AR, et al. Physical activity recommendations and decreased risk of mortality. Arch Intern Med. 2007;167(22):2453-60.
-
54Rossi A, Dikareva A, Bacon SL, Daskalopoulou SS. The impact of physical activity on mortality in patients with high blood pressure: a systematic review. J Hypertens. 2012;30(7):1277-88.
-
55Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Eur Heart J. 2016;37(29):2315-81.
-
56MacMahon S. Alcohol consumption and hypertension. Hypertension. 1987;9(2):111-21.
-
57Lang T, Cambien F, Richard JL, Bingham A. Mortality in cerebrovascular diseases and alcoholism in France. Presse Med. 1987;16(28):1351-4.
-
58Fuchs FD, Chambless LE, Folsom AR, Eigenbrodt ML, Duncan BB, Gilbert A, et al. Association between alcoholic beverage consumption and incidence of coronary heart disease in whites and blacks: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2004;160(5):466-74.
-
59World Health Organization.(WHO). Global status report on alcohol and health. Geneva; 2014.
-
60Johnson HM. Anxiety and Hypertension: Is There a Link? A Literature Review of the Comorbidity Relationship Between Anxiety and Hypertension. Curr Hypertens Rep. 2019;21(9):66.
-
61Dalmazo AL, Fetter C, Goldmeier S, Irigoyen MC, Pelanda LC, Barbosa ECD, et al. Stress and Food Consumption Relationship in Hypertensive Patients. Arq Bras Cardiol. 2019;113(3):374-80.
-
62Denollet J, Gidron Y, Vrints CJ, Conraads VM. Anger, suppressed anger, and risk of adverse events in patients with coronary artery disease. Am J Cardiol. 2010;105(11):1555-60.
-
63Bai Z, Chang J, Chen C, Li P, Yang K, Chi I. Investigating the effect of transcendental meditation on blood pressure: a systematic review and meta-analysis. J Hum Hypertens. 2015;29(11):653-62.
-
64Tankeu AT, Agbor VN, Noubiap JJ. Calcium supplementation and cardiovascular risk: A rising concern. J Clin Hypertens. 2017;19(6):640-6.
-
65Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. 2018;380(1):33-44.
-
66Amoh-Mensah K, Ankomah SE, KariKari AK, Arthur JA. Prevention of Hypertension: A critical review of the Health benefits of Salt, Garlic, Fish oil, Chocolate and Vitamin D. Int J Med Sci Tech. 2017;7(7):38-46.
-
67Paula TP, Kramer CK, Viana LV, Azevedo MJ. Effects of individual micronutrients on blood pressure in patients with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2017;7(40751): 1-12.
-
68Gröber U, Schimidt J, Kisters K. Magnesium in Prevention and Therapy. Nutrients. 2015; 7: 8199-226.
-
69Padwal R, Hackam D, Khan N, Tobe S. Primary prevention of CVD: modification of diet in people with hypertension. BMJ Clin Evid. 2016 Jan; 2016:pii:0214.
-
70Flowers N, Hartley L, Todkill D, Stranges S, Rees K. Co-enzyme Q10 supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2014;(12):CD010405.
-
71National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention; 2014.
-
72World Health Organization. (WHO). Report on the global tobacco epidemic. Geneva; 2017.
-
73Center for Disease Control and Prevention. How Tobacco Smoke Causes Disease: The Biology and Behavioural Basis for Smoking-attributable Disease. A Report of the Surgeon General;2010.
-
74Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-centuryhazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-50.
-
75Khoramdad M, Vahedian-azimi A, Karimi L, Rahimi-Bashar F, Amini H, Sahebkar A. Association between passive smoking and cardiovascular disease: A systematic review and meta-analysis. IUBMB Life. 2020;72(4):677-86.
-
76VanderWeele TJ, Balboni TA, Koh HK, Health and Spirituality. JAMA. 2017;318(6):519-20.
-
77Cozier YC, Yu J, Wise LA, VanderWeele TJ, Balboni TA, Argentieri MA, et al. Religious and Spiritual Coping and Risk of Incident Hypertension in the Black Women’s Health Study. Ann Behav Med. 2018;52(12):989-98.
-
78Lewington S, Clarke R, Qizilbash N, Peto R, Collins C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349): 1903–13.
-
79Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med.2001;345(8):1291-7.
-
80Fukuhara M, Arima H, Ninomiya T, Hata J, Yonemoto K, Doi Y, et al. Impact of lower range of prehypertension events in a general population: the Hysayama Study. J Hypertens. 2012;30(5):893-900.
-
81Han M, Li Q, Liu L, Zhang D, Ren Y, Zhao Y, et al. Prehypertension and risk of cardiovascular diseases: a meta-analysis of 47 cohort studies. J Hypertens. 2019; 37(12):2325-32.
-
82Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness A Scientific Statement from the American Heart Association. Hypertension. 2015; 66(3):698-722.
-
83Law MR, Morris JK, Wald NJ. Use of BP lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338(338):b1665.
-
84Bundy JD, Li C, Stuchlik P, Bu X, Bu X, Kelly TN, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017; 2(7):775–81.
-
85Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta- analysis. Lancet. 2016; 387(10022):957–67.
-
86Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al - SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–16.
-
87Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315(24):2673–82.
-
88Ho JE, Enserro D, Brouwers FP, Kizer JR, Shah SJ, Psaty BM, et al. Predicting heart failure with preserved and reduced ejection fraction: The International Collaboration on Heart Failure Subtypes. Circ Heart Fail. 2016;9(6):pii:003026.
-
89Emdin CA, Anderson SG, Salimi-Khorshidi G, Woodward M, MacMahon S, Dwyer T, et al. Usual blood pressure, atrial fibrillation and vascular risk: evidence from 4.3 million adults. Int J Epidemiol. 2017; 46(1):162-2.
-
90Rahimi K, Mohseni H, Kiran A, Tran J, Nazarzadeh M, Rahimian F, et al. Elevated blood pressure and risk of aortic valve disease: a cohort analysis of 5.4 million UK adults. Eur Heart J. 2018;39:3596-603.
-
91Rahimi K, Mohseni H, Otto CM, Conrad N, Tran J, Nazarzadeh M, et al. Elevated blood pressure and risk of mitral regurgitation: A longitudinal cohort study of 5.5 million United Kingdom adults. PLoS Med. 2017; 14(10):e1002404.
-
92Emdin CA, Anderson SG, Callender T, Conrad N, Salimi-Khorshidi G, Mohseni H, et al. Usual blood pressure, peripheral arterial disease, and vascular risk: cohort study of 4.2 million adults. BMJ. 2015;351:h4865.
-
93Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005; 165(8):923-8.
-
94Kanno A, Kikuya M, Ohkubo T, Hashimoto T, Satoh M, Hirose T, et al. Pre-hypertension as a significant predictor of chronic kidney disease in a general population: the Ohasama Study. Nephrol. Dial Transplant. 2012; 27(8):3218-23.
-
95Emdin CA, Rothwell PM, Salimi-Khorshidi G, Kiran A, Conrad N, Callender T, et al. Blood pressure and risk of vascular dementia: evidence from a primary care registry and a cohort study of transient ischemic attack and stroke. Stroke. 2016; 47(6):1429-35.
-
96Walker KA, Sharrett R, Wu A, Schneider AL, Alber M, Lutsey PL, et al. Association of midlife to late-life blood pressure patterns with incident dementia. JAMA. 2019; 322(6):535-45.
-
97Joas E, Bäckman K, Gustafson D, Ostling S, Waern M, Guo X, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 2012; 59(4):796-801.
-
98Emdin CA, Anderson SG, Woodward M, Rahimi K. Usual blood pressure and risk of new-onset diabetes evidence from 4.1 million adults and a meta-analysis of prospective studies. J Am Coll Cardiol. 2015; 66(14):1552–62.
-
99Ning L, Yang L. Hypetension might be a risk factor for erectile dysfunction: a meta-analysis. Andrologia. 2017; 49(4) doi.org/10.1111/and.12644
-
100Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010 Dec 13;10:31. 10:31.
-
101Fuchs FD. Essentials of hypertension. Cham, Switzerland, Springer; 2018. Doi:.org/10.1007/978-3-319-632728
» https://doi.org/10.1007/978-3-319-632728 -
102Fuchs FD, Whelton PK. High Blood Pressure and Cardiovascular Disease. Hypertension. 2020;75(2):285-92.
-
103Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, et al - SPRINT Research Group. Effect of Intensive vs Standard Blood Pressure Control on Probable Dementia: A Randomized Clinical Trial. JAMA. 2019;321(6):553-61.
-
104Nasrallah IM, Pajewski NM, Auchus AP, Chelune G, Cheung AK, Cleveland ML, et al - SPRINT Research Group. Association of intensive versus standard blood pressure control with cerebral write matter lesions. JAMA 2019;322(6):524-34.
-
105Markus MR, Stritzke J, Lieb W, Mayer B, Luchner A, Döring A, et al. Implications of persistent prehypertension for ageing-related changes in left ventricular geometry and function: the MONICA/KORA Augsburg study. J Hypertens. 2008; 26(10):2040–9.
-
106Santos AB, Gupta DK, Bello NA, Gori M, Claggett B, Fuchs FD, et al. Prehypertension is associated with abnormalities of cardiac structure and function in the atherosclerosis risk in communities Study. Am J Hypertens. 2016; 29(5):568–74.
-
107Fuchs SC, Poli-de-Figueiredo Carlos E, Figueiredo-Neto JA, Scala LC, Whelton PK, Mosele F, et al. Effectiveness of chlorthalidone plus amiloride for the prevention of hypertension: the PREVER-Prevention randomized clinical trial. J Am Heart Assoc. 2016;5(12):e004248.
-
108World Health Organization. (WHO) The world health report 2002 - Reducing Risks, Promoting Healthy Life (Internet). Geneva; 2002.
-
109Andersen SL, Sebastiani P, Dworkis DA, Feldman L, Perls TT. Health span approximates life span among many supercentenarians: compression of morbidity at the approximate limit of life span. J Gerontol A Biol Sci Med Sci. 2012; 67(4):395–405.
-
110Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, et al. Association of Normal Systolic Blood Pressure Level with Cardiovascular Disease in the Absence of Risk Factors. JAMA Cardiol.2020:5(9):1011-8.
-
111Kanel WB, Larson M. Long Term epidemiologic prediction of coronary disease. The Framingham Experience. Cardiology. 1993; 82(2-3):137-52.
-
112Konukoglu D, Uzun H. Endothelial Dysfunction and Hypertension. Adv Exp Med Biol. 2017; 956:511-40.
-
113Bautista LE, Lopez-Jaramillo P, Vera LM, Casas JP, Otero AP, Guaracao AI. Is C-reactive protein an independent risk factor for essential hypertension? J Hypertens. 2001; 19(5):857-61.
-
114Boos CJ, Lip GY. Is hypertension an inflammatory process? Curr Pharm Des. 2006; 12(13):1623-35.
-
115Grundy SM. Inflammation, hypertension, and the metabolic syndrome. JAMA. 2003; 290(22):3000-2.
-
116Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002; 39(2):257-65.
-
117Thijssen DHJ, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. 2011; 300(1):2-12.
-
118Thijssen DHJ, Bruno RM, van Mil ACCM, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019; 40(30):2534-47.
-
119Moens AL. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest. 2005; 127(6):2254-63.
-
120Celermajer DS, KE Sorensen, VM Gooch, DJ Spiegelhalter, OI Miller, ID Sullivan, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340(8828):1111-5.
-
121Takase B, A Uehata, T Akima, T Nagai, T Nishioka, A Hamabe, et al. Endothelium-dependent flow-mediated vasodilation in coronary and brachial arteries in suspected coronary artery disease. Am J Cardiol. 1998; 82(12):1535-9.
-
122Ras RT, Streppel MT, Draijer R, Zock PL, et al. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol. 2013; 168(1):344-51.
-
123Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010; 26(6):631-40.
-
124Green D, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-Mediated Dilation and Cardiovascular Event Prediction: Does Nitric Oxide Matter? Hypertension. 2011; 57(3):363-9.
-
125Soloviev MA. Correction of endothelial dysfunction in patients with arterial hypertension. Bull Exp Biol Med. 2011; 151(2):183-5.
-
126Persu A, De Plaen JF. Recent insights in the development of organ damage caused by hypertension. Acta Cardiologica. 2004; 59(4):369-81.
-
127Laurent S, Boutouyrie P, Lacolley P. Structural and Genetic Bases of Arterial Stiffness. Hypertension. 2005; 45(6):1050-5.
-
128Safar ME, Asmar R, Benetos A, Blacher J, Boutouyrie P, Lacolley P, et al. Interaction Between Hypertension and Arterial Stiffness. An Expert Reappraisal. Hypertension. 2018; 72(4):796-805.
-
129Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006; 27(21):2588–605.
-
130Fridez P, Makino A, Kakoi D, Miyazaki H, Meister J, Hayashi K, et al. Adaptation of Conduit Artery Vascular Smooth Muscle Tone to Induced Hypertension. Ann Biomed Eng. 2002; 30(7):905–16.
-
131Bardy N, Merval R, Benessiano J, Samuel JL, Tedgui A. Pressure and angiotensin-II synergistically induce aortic fibronectin expression in organ culture model of rabbit aorta. Circ Res. 1996; 79(1):70-8.
-
132Humphrey JD, Dufrense E, Schwartz MA. Mechanotransduction and extracellular matrix homeostasis. Nat Rev Mol Cell Biol. 2014;15(12):802-12.
-
133Liao D, Arnett DK, Tyroler HA, Riley WA, Chambless LE, Szklo M, et al. Arterial stiffness and the development of hypertension. Hypertension. 1999; 34(2): 201–6.
-
134Humphrey JD, Harrison DG, Figueroa CA, Lacolley P, Laurent S. Central Artery Stiffness in Hypertension and Aging: A Problem with Cause and Consequence. Circ Res. 2016; 118(3):379–81.
-
135Dernellis J, Panaretou M. Aortic stiffness is an independent predictor of progression to hypertension in nonhypertensive subjects. Hypertension. 2005; 45(3):426–31.
-
136Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, et al. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012; 308(9):875–81.
-
137Weisbrod RM, Shiang T, Al Sayah L, Fry JL, Bajpai S, Reinhart-King CA, et al. Arterial stiffening precedes systolic hypertension in diet-induced obesity. Hypertension. 2013;62(6):1105-10.
-
138Van Gorp AW, van Ingen Schenau DS, Hoeks APG, Struijker Boudier HAJ, de Mey JGR, Reneman RS. In spontaneously hypertensive rats alterations in rat aortic wall properties precede development of hypertension. Am J Physiol. 2000;278(4):1241-7.
-
139Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífkova R, Cosentino F et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241(2):507-32.
-
140Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. American Heart Association Council on Peripheral Vascular Disease. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012; 126(24):2890–909.
-
141Rabkin SW, Him S, Sweeney C. Ankle-Brachial Index as an Indicator of Arterial Stiffness in Patients Without Peripheral Artery Disease. Angiology. 2012; 63(2):150-4.
-
142Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019; 42(9):1235–481.
-
143Fowkes FGR, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, et al. Ankle Brachial Index Combined with Framingham Risk Score to Predict Cardiovascular Events and Mortality: A Meta-Analysis. JAMA. 2008. 300(2):197-208.
-
144Mattace-Raso FUS, Hofman A, Verwoert GC, Wittemana JCM, Wilkinson I, Cockcroft J, et al. Determinants of Pulse Wave Velocity in Healthy People and in the Presence of Cardiovascular Risk Factors: ‘Establishing Normal and Reference Values’. Eur Heart J. 2010; 31(19):2338–50.
-
145Boutouyrie P, Bruno RM. The Clinical Significance and Application of Vascular Stiffness Measurements. Am J Hypertens. 2019; 32(1):4-11.
-
146Van Bortel L, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Expert Consensus Document on the Measurement of Aortic Stiffness in Daily Practice Using Carotid-Femoral Pulse Wave Velocity. J Hypertens. 2012; 30(3):445-8.
-
147Butlin M, Qasem A. Large Artery Stiffness Assessment Using SphygmoCor Technology. Pulse. 2016; 4(4):180–92.
-
148Weber T, M Ammer M, Rammer M, Adji A, O’Rourke MF, Siegfried Wassertheurer S, et al. Noninvasive determination of carotid–femoral pulse wave velocity depends critically on assessment of travel distance: a comparison with invasive measurement. Journal of Hypertension. 2009; 27(8):1624–30.
-
149Stea F, Bozec E, Millasseau S, Khettab H, Boutouyrie P, Laurent S. Comparison of the Complior Analyse device with Sphygmocor and Complior SP for pulse wave velocity and central pressure assessment. J Hypertens. 2014; 32(4):873–80.
-
150Sztrymf B, Jacobs F, Chemla D, Richard C, Millasseau S. Validation of the new Complior sensor to record pressure signals non-invasively. J Clin Monit Comput. 2013; 27(6):613-9.
-
151Jones CR, Taylor K, Chowienczyk P, Poston L, Shennan AH. A validation of the Mobil O Graph (version 12) ambulatory blood pressure monitor. Blood Pressure Monitoring. 2000; 5(4):233–8.
-
152Hametner B, Wassertheurer S, Kropf J, Mayer C, Eber B, Weber T. Oscillometric estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood Press Monit. 2013; 18(3):173–6.
-
153Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001; 37(5): 1236-1241.
-
154Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002; 39(1): 10-5.
-
155Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010; 55(13):1318-27.
-
156Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014; 63(7): 636-46.
-
157Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010; 121(4): 505-11.
-
158Xaplanteris P, Vlachopoulos C, Protogerou AD, Aznaouridis K, Terentes-Printzios D, Argyris AA, et al. A clinical score for prediction of elevated aortic stiffness: derivation and validation in 3943 hypertensive patients. J Hypertens. 2019,37:339–4.
-
159Paiva AMG, Mota-Gomes MA, Brandão AA, Silveira FS, Silveira MS, Okawa RTP et al. Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil-O-Graph PWA monitor. Hypertens Res. 2020 Jun 12.doi: 10.1038/s41440-020-0490 online ahead of print.
-
160Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar M, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2013; 31:1865–71.
-
161Ding FH, Fan WX, Zhang RY, Zhang Q, Li Y, Wang JG. Validation of the Noninvasive Assessment of Central Blood Pressure by the SphygmoCor and Omron Devices Against the Invasive Catheter Measurement. American Journal of Hypertension. 2011; 24(12):1306-1311.
-
162Pereira T, Maldonado J, Coutinho R, Cardoso E, Laranjeiro M, Andrade I, et al. Invasive validation of the Complior Analyse in the assessment of central artery pressure curves: a methodological study. Blood Press Monit. 2014; 19(5):280–7.
-
163Herbert A, Cruickshank JK, Laurent S, Boutouyrie P, on behalf of The Reference Values for Arterial Measurements Collaboration. Establishing reference values for central blood pressure andi ts amplification in a general healthy population and according to cardiovascular risk factors. Eur Heart J.2014; 35(44):3122-3.
-
164Malachias MVB, Souza WKSB, Plavnik FL, Rodrigues CIS, Brandão AA, Neves MFT, et al. 7ª Diretriz Brazileira de Hipertensão Arterial. Arq Bras Cardiol. 2016;107(3Supl.3):1-83.
-
165Stergiou GS, Alpert B, Mieke S, Asmar R, Atkins N, Eckert S, et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. J Hypertens. 2018;36(3):472-8.
-
166Brazil. Ministério do Desenvolvimento, Indústria e Comércio Exterior. Instituto Nacional de Metrologia, Qualidade e Tecnologia – Portaria n.46 de 22 de janeiro de 2016. Esfigmomanometros. [Internet] [Acesso em 25 fev 2020]. Disponível em: http://www.inmetro.gov.br/legislacao/rtac/pdf/RTAC002373.pdf .
» http://www.inmetro.gov.br/legislacao/rtac/pdf/RTAC002373.pdf -
167Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet 2012;379(9819):905–14.
-
168Saedon NI, Pin Tan M, Frith J. The Prevalence of Orthostatic Hypotension: A Systematic Review and Meta-Analysis. J Gerontol A Biol Sci Med Sci. 2020 Jan 1;75(1):117-22.
-
169Fagard RH, De Cort P. Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. Hypertension 2010;56(1):56–61.
-
170Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, Zarnke KB. et al. Hypertension Canada’s 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults. Can J Cardiol. 2017;33(5):557-76.
-
171Myers MG. A short history of automated office blood pressure - 15 years to SPRINT. J Clin Hypertens (Greenwich) 2016;18:721–724.
-
172Parati G, Pomidossi G, Casadei ParatiR, Mancia G. Lack of alerting reactions to intermitent cuff inflations during noninvasive blood pressure monitoring. Hypertension 1985;7:597–601.
-
173Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension 2010;55:195–200.
-
174Palatini P, Asmar R. Cuff challenges in blood pressure measurement. J Clin Hypertens. 2018; 20:1100–3
-
175Leblanc MÈ, Auclair A, Leclerc J, Bussières J, Agharazii M, Hould FS, et al. Blood pressure measurement in severely obese patients: validation of the forearm approach in different arm positions. Am J. Hypertens 2019;32(2):175–85
-
176Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697-716.
-
177Senarclens et al.Brachial or wrist blood pressure in obese patients:which is the best? Blood Pressure Monitoring 2008, 13:149–151.
-
178Irving G, Holden J, Stevens R, McManus RJ. Which cuff should I use? Indirect blood pressure measurement for the diagnosis of hypertension in patients with obesity: a diagnostic accuracy review. BMJ Open.2016;6:e012429. doi: 10.1136/bmjopen-2016-012429
-
179Fuchs FD, Scala LC, Vilela-Martin JF, de Mello, RB, Mosele, F, Whelton, PK, et al. Effectiveness of chlorthalidone/amiloride versus losartan in patients with stage I hypertension: results from the PREVER-treatment randomized trial. J Hypertens. 2016;34(4):798-806.
-
180Feitosa ADM, Mota-Gomes MA, Barroso WS, Miranda RD, Barbosa ECD, Pedrosa RP, et al. Relationship between office isolated systolic or diastolic hypertension and white-coat hypertension across the age spectrum: a home blood pressure study. J Hypertens. 2020;38(4):663-670.
-
181Weber MA, Schiffrin EL, White WA, Mann S, Lindbolm LH, Venerson JG, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15.
-
182Egan BM, Stevens-Fabry S. Prehypertension-prevalence, health risks, and management strategies. Nat Rev Cardiol. 2015;12(5):289-300.
-
183Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens 2014;32(7):1359–66.
-
184Stergiou GS, Parati G, Vlachopoulos C, Achimastos A, Andreadis E, Asmar R, et al. Methodology and technology for peripheral and central blood pressure and blood pressure variability measurement: current status and future directions - Position statement of the European Society of Hypertension Working Group on blood pressure monitoring and cardiovascular variability. J Hypertens 2016;34(9):1665–77.
-
185O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on Blood Pressure M. European Society of Hypertension position paper on ambulatory blood pressure monitoring. Hypertens 2013;31(9):1731–68.
-
186Nobre F, Mion Jr. D, Gomes MAM, Barbosa ECD, Rodrigues CIS, Neves MFT et al. 6ª Diretrizes de Monitorização Ambulatorial da Pressão Arterial e 4ª Diretrizes de Monitorização Residencial da Pressão Arterial. Arq Bras Cardiol 2018; 110(5Supl.1):1-29.
-
187Souza WK, Jardim PC, Porto LB, Araújo FA, Sousa AL, Salgado CM. Comparison and correlation between self-measured blood pressure, casual blood pressure measurement and ambulatory blood pressure monitoring. Arq Bras Cardiol. 2011;97(2):148-55.
-
188Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30(7):1289–99.
-
189WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167-74.
-
190Park JS, Rhee MY, Namgung J, Lee SY, Cho DK, Choi TY, et al. Comparison of Optimal Diagnostic Thresholds of Hypertension With Home Blood Pressure Monitoring and 24-Hour Ambulatory Blood Pressure Monitoring. Am J Hypertens. 2017 Nov 6;30(12):1170-6.
-
191Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, et al. Outcome-Driven Thresholds for Home Blood Pressure Measurement: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 2012, 61(1), 27–34.
-
192D, Asayama K, Ohkubo T, Kikuya M, Kanno A, Hara A, et al. Stroke Risk in Treated Hypertension Based on Home Blood Pressure: the Ohasama Study. Am J Hypertens. 2010;23(5):508-14.
-
193Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens 2012;30(3):449–56.
-
194McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, et al. Telemonitoring and selfmanagement in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet 2010;376(9736):163–72.
-
195McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312(8):799–808.
-
196Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS One.2017;14:e1002389.
-
197Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens 2013;31(3):455–67; discussion 467–8.
-
198Parati G, Omboni S. Role of home blood pressure telemonitoring in hypertension management: an update. Blood Press Monit. 2010;15(6):285–95.
-
199Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens. 2008;26(10):1919–27.
-
200Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348(24):2407–15.
-
201Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111(14):1777–83.
-
202ABC-H Investigators, Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32(12):2332–40; discussion 2340.
-
203Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51(1):55–61.
-
204Parati G, Ochoa JE, Bilo G, Agarwal R, Covic A, Dekker FW, et al. Hypertension in chronic kidney disease part 2: role of ambulatory and home blood pressure monitoring for assessing alterations in blood pressure variability and blood pressure profiles. Hypertension. 2016;67(6):1102–10.
-
205Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162(3):192–204.
-
206Mancia G, Zanchetti A. White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do next? J Hypertens. 1996;14(9):1049–52.
-
207Bobrie G, Clerson P, Menard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens. 2008;26(9):1715–25.
-
208Feitosa ADM, Mota-Gomes MA, Miranda RD, Barroso WS, Barbosa ECB, Pedrosa RP, et al. Impact of 2017 ACC/AHA hypertension guidelines on the prevalence of white-coat and masked hypertension: A home blood pressure monitoring study. J Clin Hypertens. 2018;20(12):1745-7.
-
209Paiva AMG, Gomes MICM, Campana EMG, Feitosa ADM, Sposito AC, Mota-Gomes MA, et al. Impact of hypertension phenotypes on the office and 24-h pulse wave velocity and augmentation index in individuals with or without antihypertensive medication use. Hypertens Res. 2019;42(12):1989-95.
-
210Fagard RH, Cornelissen VA. Incidence of cardiovascular events in whitecoat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25(11):2193-8.
-
211Staessen JA, O’Brien ET, Amery AK, Atkins N, Baumgart P, De Cort P, et al. Ambulatory blood pressure in normotensive and hypertensive subjects: results from an international database. J Hypertens Suppl. 1994;12(7):S1-12.
-
212Barroso WKS, Feitosa ADM, Barbosa ECD, Miranda RD, Vitorino PVO, Brandão AA, et al Prevalence of Masked and White-Coat Hypertension in Pre-Hypertensive and Stage 1 Hypertensive patients with the use of TeleMRPA. Arq Bras Cardiol .2019;113(5):970-5.
-
213Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35(4):677–88.
-
214Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White-coat hypertension and cardiovascular events: a meta-analysis. J Hypertens. 2016;34(4):593–9.
-
215Kikuya M, Ohkubo T, Metoki H, Asayama K, Hara A, Obara T, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52(6):1045–50.
-
216Rassi G, Seravalle G, Trevano FQ, Dell’oro R, Bolla G, Cuspidi C, Arenare F, Mancia G. Neurogenic abnormalities in masked hypertension. Hypertension 2007;50(3):537–42.
-
217Parati G, Omboni S, Staessen J, Thijs L, Fagard R, Ulian L, et al. Limitations of the difference between clinic and daytime blood pressure as a surrogate measure of the ‘white-coat’ effect. Syst-Eur investigators. J Hypertens. 1998;16(1):23–9.
-
218Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J.2014;35(46):3304–12.
-
219Mancia G. Clinical significance of white-coat hypertension. J Hypertens. 2016;34(4):623–6.
-
220Mancia G. White-coat hypertension: growing evidence in favour of its adverse prognostic significance. J Hypertens. 2017;35(4):710–2.
-
221Mancia G, Grassi G. The heterogeneous nature of white-coat hypertension. J Am Coll Cardiol. 2016;68(19):2044–6.
-
222Mancia G, Bombelli M, Cuspidi C, Facchetti R, Grassi G. Cardiovascular risk associated with white-coat hypertension: pro side of the argument. Hypertension. 2017;70(4):668–75.
-
223Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219.
-
224Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24(1):52-8.
-
225Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J, Staessen JA. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45(4):493–8.
-
226Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006;47(5):846–53.
-
227Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291(11):1342–9.
-
228Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, et al. Response to masked hypertension in untreated and treated patients with diabetes mellitus: attractive but questionable interpretations and response to Is masked hypertension related to diabetes mellitus? Hypertension. 2013;62(4):e23–e25.
-
229Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–68.
-
230Lindholt JS, Sogaard R. Population screening and intervention for vascular disease in Danish men (VIVA): a randomised controlled trial. Lancet. 2017;390(10109):2256–65.
-
231Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011 Jun 24;342:d3621.
-
232Vinyoles E, Felip A, Pujol E, de la Sierra A, Dura R, del Rey RH, et al. Clinical characteristics of isolated clinic hypertension. J Hypertens, 2008;26(3):438–45.
-
233Picone DS, Schultz MG, Otahal P, Aakhus S, Al-Jumaily AM, Black JA, et al. Accuracy of cuff-measured blood pressure: systematic reviews and meta-analyses. J Am Coll Cardiol. 2017;70(5):572–86.
-
234Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–5.
-
235Lurbe E, Redon J. Isolated systolic hypertension in young people is not spurious and should be treated: con side of the argument. Hypertension. 2016;68(2):276–80.
-
236McEniery CM, Franklin SS, Cockcroft JR, Wilkinson IB. Isolated systolic hypertension in young people is not spurious and should be treated: pro side of the argument. Hypertension 2016;68(2):269–75.
-
237Miall WE, Oldham PD. The hereditary factor in arterial blood-pressure. BMJ. 1963 Jan;1(5323):75–80.
-
238Snieder H, Hayward CS, Perks U, Kelly RP, Kelly PJ, Spector TD SO. Heritability of central systolic pressure augmentation: a twin study. Hypertension. 2000 Feb;35(2):574-9.
-
239Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50(10): 1412–25.
-
240Raina R, Krishnappa V, Das A, Amin H, Radhakrishnan Y, Nair NR et al. Overview of Monogenic or Mendelian Forms of Hypertension. Front Pediatr. 2019 Jul 01 ;7:263.
-
241Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol. 2015;11(2):101–11.
-
242Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-42.
-
243Murabito JM, Nam BH, D’Agostino RB Sr, Lloyd-Jones DM, O’Donnell CJ, Wilson PW. Accuracy of offspring reports of parenteral cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. 2004;140(6):434-40.
-
244Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr. J, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-52.
-
245Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321-9.
-
246Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159(10):1104-9.
-
247Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation. 2014;130(19):1692-9.
-
248Obesity Classification – World Obesity Federation. [Cited in 2020 Jan 12].Avaliable from: https://www.worldobesity.org/about/about-obesity/obesity-classification?_ga=2.27200504.476223329.1582981112-571126236.1582981112
» https://www.worldobesity.org/about/about-obesity/obesity-classification?_ga=2.27200504.476223329.1582981112-571126236.1582981112 -
249Carter SA. Indirect systolic pressures and pulses waves in arterial occlusive disease of the lower extremities. Circulation. 1968;37(4):624-37.
-
250Newman AB, Siscovick DS, Manolio TA, Polak J, Fried LP, Borhani NO, et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular Health Study. Cardiovascular Health Study (CHS) Collaborative Reserch Group. Circulation. 1993;88(3):837-45.
-
251Rourke MF, Adji A. Guidelines on guidelines: focus on isolated systolic hypertension in youth. J Hypertens. 2013;31(4):649–54.
-
252Brandão AA, Amodeo C, Alcantara C, Barbosa E, Nobre F, Pinto F, et al. I Posicionamento Luso-Brazileiro de Pressão Arterial Central. Arq Bras Cardiol. 2017;108(2):100-8.
-
253Mancia G, Narkiewiczk, Redon J, Zanchetti A, Bohm M, Christiaens T et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: theTask Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357.
-
254D’Agostino Sr RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WBl. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6): 743–53.
-
255Levey AS, Bosch JP, Lewis JB, Greene LT, Rogers N, Roth D. A more accurate accurate method to estimate GFR from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461-70.
-
256. A New Equation to Estimate Glomerular Filtration Rate. Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI). Ann Intern Med. 2009;150(9):604-12.
-
257Levey AS, Eckardt K-U, Dorman NM, Christiansen SL, Hoorn EJ, Ingelfinger JR, et al. Nomenclature for kidney function and disease: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Inter. 2020 97(6):1117–29.
-
258KDIGO CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013, 3(1):1-150.
-
259Friedewald WT, Levi RI, Fredrickson DS. Estimation of the concentration of low density lipoproteins cholesterol in plasma without use of the ultracentrifuge. Clin Chem. 1972;18:499-502.
-
260Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J. 1949; 37(2):161-86.
-
261Casalle PN, Devereux RB, Alonso DR, Campo E, Kligfield P. Improved sex specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocadiograms: validation with autopsy findings. Circulation. 1987;75(3):565-72.
-
262Rayner BL, Goodman H, Opie LH. The Chest Radiograph. A useful investigationin the evaluation of hypertensive patients. Am J Hypertens. 2004; 17(6):507-10.
-
263Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the Use of Echocardiography in Adult Hypertension: A Report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015;28(7):727-54.
-
264Tsioufis C, Kokkinos P, Macmanus C, Thomopoulos C, Faselis C, Doumas M, et al. Left ventricular hypertrophy as a determinant of renal outcome in patients with high cardiovascular risk. J Hypertens. 2010;28(11):2299–308.
-
265Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. 2010; 55:1600–7.
-
266Polak JF, Szklo M, O’Leary DH. Carotid intima-media thickness score, positive coronary artery calcium score, and incident coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2017;6(1):e004612.
-
267Vasbinder GB, Nelemans PJ, Kessels AG, Kroon AA, de Leeuw PW, van Engelshoven JM. Diagnostic tests for renal artery stenosis in patients suspected of having renovascular hypertension: a meta-analysis. Ann Intern Med. 2001;135(6):401-11.
-
268Selvin E, Steffes MW, Zhu H, MatsushitaK, Wagenknecht L, Pankow J, et al. Brancati Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults.N Engl J Med. 2010;362(9):800–11.
-
269Chin D, Battistoni A, Tocci G, Passerini J, Parati G, Volpe M. Non-invasive diagnostic testing for coronary artery disease in the hypertensive patient: potential advantages of a risk estimation-based algorithm. Am J Hypertens. 2012;25:1226–35.
-
270Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003;107(22):2864–9.
-
271Mikael LR, Paiva AMG, Mota-Gomes M, Sousa ALL, Jardim PCBV, Vitorino PVO, et al. Envelhecimento vascular e rigidez arterial. Arq Bras Cardiol. 2017;109(3):253-8.
-
272de Leeuw FE, de Groot JC, Oudkerk M, Witteman JC, Hofman A, van Gijn J, Breteler MMB. Hypertension and cerebral white matter lesions in a prospective cohort study. Brain 2002;125(Pt 4):765–72
-
273NCD Risk Factor Collaboration. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389 (10064):37-55.
-
274Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global Burden of hypertension: analysis of worldwide data. Lancet. 2005 Jan 15-21; 365(9455):217-23.
-
275Ungera T, Borghib C, Charcharc F, Khanf NA, Poulterh NR, Prabhakarani D, et al. International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334-57.
-
276Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H and Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-47.
-
277Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med. 1992;152(1):56-64.
-
278Blood Pressure Lowering Treatment Trialists C. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-8.
-
279Matsura Y, Kanter JE, Bornfeldt KE. Highlighting Residual Atherosclerotic Cardiovascular Disease. Arterioscler Thromb Vasc Biol. 2019;39(1):e1-e9.
-
280Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143.
-
281Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk 2020. Eur Heart J. 2020;41(1):111-88.
-
282Sposito AC, Ramires JA, Jukema JW, Molina JC, da Silva PM, Ghadanfar MM, Wilson PW. Physicians’ attitudes and adherence to use of risk scores for primary prevention of cardiovascular disease: cross-sectional survey in three world regions. Curr Med Res Opin. 2009;25(5):1171-8.
-
283Hlatky MA, Greenland P, Arnett DK, Ballantyne CM, Criqui MH, Elkin et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association, Circulation. 2009;119(7):2408-16.
-
284Cooney MT, Dudina AL, Graham IM. Value and Limitations of Existing Scores for the Assessment of Cardiovascular Risk A Review for Clinicians. J Am Coll Cardiol. 2009;54(14):1209-27.
-
285Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014; 383(9932):1899–911.
-
286Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364(9438):937-52.
-
287Wang OJ, Wang Y, Chen J, Krumholz HM. Recent Trends in Hospitalization for Acute Myocardial Infarction. Am J Cardiol. 2012; 109(11):1589–93.
-
288Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583-612.
-
289International Diabetes Federation. IDF Consensus Worldwide Definition of the Metabolic Syndrome. 2006. [Cited in 2020 Mar 10]. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html .
» https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html -
290Perrone-Filardi P, Coca A, Galderisi M, Paolillo S, Alpendurada F, de Simone G, et al. Noninvasive cardiovascular imaging for evaluating subclinical target organ damage in hypertensive patients: a consensus article from the European Association of Cardiovascular Imaging, the European Society of Cardiology Council on Hypertension and the European Society of Hypertension. J Hypertens. 2017; 35(9):1727–41.
-
291PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001; 358(9287):1033-41.
-
292Manning LS, Mistri AK, Potter J, Rothwell PM, Robinson TG. Short-term blood pressure variability in acute stroke: post hoc analysis of the controlling hypertension and hypotension immediately post stroke and continue or stop post-stroke antihypertensives collaborative study trials. Stroke. 2015; 46(6):1518-24.
-
293Grundvold I, Skretteberg PT, Liestol K, Erikssen G, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Upper normal blood pressures predict incident atrial fibrillation in healthy middle-aged men: a 35-year follow-up study. Hypertension. 2012; 59(2):198–204.
-
294Singer DR, Kite A. Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg. 2008;35(6):701–8.
-
295Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Petersen C et al. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010; 31(7):883-91.
-
296Orlova IA, Nuraliev EY, Yarovaya EB, Ageev FT. Prognostic value of changes in arterial stiffness in men with coronary artery disease. Vasc Health Risk Manag. 2010; 6:1015–21.
-
297Cecelja M, Chowienczyk P. Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension. 2009; 54(6):1328–36.
-
298Chirinos JA, Segers P, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease JACC State-of-the-Art Review, J Am Coll Cardiol. 2019;74(9):1237-63.
-
299Bertoluci MC, Moreira RO, Faludi A, Izar MC, Schaan BD, Valerio CM et al. Brazilian guidelines on prevention of cardiovascular disease in patients with diabetes: a position statement from the Brazilian Diabetes Society (SBD), the Brazilian Cardiology Society (SBC) and the Brazilian Endocrinology and Metabolism Society (SBEM). Diabetol Metab Syndr. 2017; 9:53.
-
300Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, and assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2015; 31(5): 549-68.
-
301British Cardiac Society; British Hypertension Society; Diabetes UK; HEART UK; Primary Care Cardiovascular Society; Stroke Association. JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005; 91 Suppl 5:v1-52. 6.
-
302Sánchez RA, Boggia J, Peñaherrera E, Barroso WS, Barbosa E, Villar R, et al. Ambulatory blood pressure monitoring over 24 h: A Latin American Society of Hypertension position paper-accessibility, clinical use and cost effectiveness of ABPM in Latin America in year 2020. J Clin Hypertens. 2020; 22(4): 527–43.
-
303O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, et al; European Society of Hypertension Working Group on Blood Pressure Monitoring. J Hypertens. 2013 Sep; 31(9):1731-68.
-
304Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018; 378(16):1509–20.
-
305Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011; 57(1):3–10.
-
306Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012 Aug15;(8):CD006742.
-
307Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32(12):2285-95.
-
308Brunstrom M, Carlberg B. Association of blood pressure lowering with mortal- ity and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28–36.
-
309Lonn EM, Bosch J, López-Jaramillo P, Zhu J, Liu L, Pais P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–20.
-
310Lee CJ, Ryu J, Kim HC, Ryu DR, Ihm SH, Kim YJ, et al. Clinical benefit of treatment of stage-1, low-risk hypertension Korean national health insurance database analysis. Hypertension. 2018;72(6):1285–93.
-
311Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging?: The Framingham Heart Study. Circulation. 2001;103(9):1245–9.
-
312Mahtta D, Elgendy IY, Pepine CJ. Optimal medical treatment of hypertension in patients with coronary artery disease. Expert Rev Cardiovasc. 2018;16(11):815-23.
-
313Rosendorff C, Lackland DT, Allison M, Aronow WS, Black HR, Blumenthal RS, et al. Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J Am Coll Cardiol. 2015;65(18):1998–2038.
-
314Yannoutsos A, Dreyfuss CT, Safar ME, Blacher J. Optimal blood pressure target in stroke prevention. Curr Opin Neurol. 2017;30(1):8-14.
-
315Béjot Y. Targeting blood pressure for stroke prevention: current evidence and unanswered questions. J Neurol. 2019; doi: 10.1007/s00415-019-09443-5. Online ahead of print.
-
316Pinho-Gomes AC, Rahimi K. Management of blood pressure in heart failure. Heart. 2019;105(8):589-95.
-
317Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018;3(4):288–97.
-
318Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol. 2018 Jul 15;263:69-74.
-
319Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, et al. Effects of intensive BP control in CKD. J Am Soc Nephrol. 2017;28(9):2812–23.
-
320Filipovsky J, Seidlerova J, Kratochvil Z, Karnosova P, Hronova M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press. 2016;25(4):228–34.
-
321Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67(5):808–12.
-
322Heerspink HJ, Ninomiya T, Perkovic V, Woodward M, Zoungas S, Cass A, et al. ADVANCE Collaborative Group: Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Eur Heart J. 2010;31(23):2888–96.
-
323Ku E, Gassman J, Appel LJ, Smogorzewski M, Sarnak MJ, Glidden DV, et al. BP control and long-term risk of ESRD and mortality. J Am Soc Nephrol. 2017;28(2):671–7.
-
324Chang AR, Appel LJ. Target Blood Pressure for Cardiovascular Disease Prevention in Patients with CKD. Clin J Am Soc Nephrol. 2018; 13(10):1572–4.
-
325Chang AR, Lóser M, Malhotra R, Appel LJ. Blood pressure goals in patients with CKD: A review of evidence and guidelines. Clin J Am Soc Nephrol. 2019;14(1):161-9.
-
326American Diabetes Association. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S111–34.
-
327Toklu B, Bangalore S. Blood pressure lowering in patients with type 2 diabetes improves cardiovascular events including mortality, but more intensive lowering to systolic blood pressure less than 130 mm Hg is associated with further reduction in stroke and albuminuria without further reduction in cardiac events. Evid Based Med. 2015;20(5):183–4.
-
328Soliman EZ, Byington RP, Bigger JT, Evans G, Okin PM, Goff DC, et al. Effect of Intensive Blood Pressure Lowering on Left Ventricular Hypertrophy in Patients With Diabetes Mellitus: Action to Control Cardiovascular Risk in Diabetes Blood Pressure Trial. Hypertension. 2015;66(6):1123–9.
-
329Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: Systematic review and meta-analyses. BMJ. 2016;24:352 i717.
-
330Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85.
-
331De Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, et al. Diabetes and hypertension: A position statement by the American diabetes association. Diabetes Care. 2017;40(9):1273–84.
-
332Wright JT Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mmHg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499-503.
-
333Beckett N, Peters R, Leonetti G, et al, HYVET Study Group. Subgroup and per-protocol analyses from the Hypertension in the Very Elderly Trial. J Hypertens 2014;32(7):1478–87.
-
334Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: A systematic review and meta-analysis. Ann Intern Med. 2017;166(6):419–29.
-
335Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. J Am Coll Cardiol. 2017;69(5):486-93.
-
336Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med 2014; 47(1): 100-2.
-
337Weinstein E, Rucker LM. Team-based care to improve control of hypertension in an inner city practice. Healthc (Amst). 2016; 4(1):52-6.
-
338Mansoor SM, Krass I, Aslani P. Multiprofessional interventions to improve patient adherence to cardiovascular medications. J Cardiovasc Pharmacol Ther. 2013; 18(1)19-30.
-
339Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009; 169(19): 1748-55.
-
340Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006; 44(7): 646-57.
-
341Potthoff SA, Vonend O. Multidisciplinary Approach in the Treatment of Resistant Hypertension. Curr Hypertens Rep. 2017; 19(1): 9.
-
342David G, Gunnarsson C, Saynisch PA, Chawla R, Nigam S.. Do patient-centered medical homes reduce emergency department visits? Health Serv Res. 2015; 50(2):418-39.
-
343Jacob V, Chattopadhyay SK, Thota AB, et al. Economics of Team-based Care in Controlling Blood Pressure: A Community Guide Systematic Review. Am J Prev Med 2015; 49(5): 772-83.
-
344Peacock E, Krousel-Wood M. Adherence to Antihypertensive Therapy. Med Clin North Am. 2017; 101(1): 229-45.
-
345Jardim LM, Jardim TV, Souza WK, Barroso de Souza WKS, Pimenta CD, Sousa AL, et al. Multiprofessional Treatment of High Blood Pressure in Very Elderly Patients. Arq Bras Cardiol. 2017; 108(1): 53-9.
-
346Proia KK, Thota AB, Njie GJ, Finnie R, Hopkins D, Mukhtar Q, et al. Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014; 47(1):86-99.
-
347Kuhmmer R, Lazzaretti RK, Guterres CM, Raimundo FV, Leite LE, Delabary TS, et al. Effectiveness of multidisciplinary intervention on blood pressure control in primary health care: a randomized clinical trial. BMC Health Serv Res. 2016;16(1):456.
-
348Strumpf E, Ammi M, Diop M, Laniel JF, Tousignant P. The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J Health Econ. 2017;55:76-94.
-
349Norouzi Z, Jafarnejad F, Khadivzadeh T, Esmaily H, Headjazi A. Comparison of the effect of standardized patient-based training with team-based learning on the knowledge of midwifery students in providing services to victims of rape. J Educ Health Promot. 2019;8:267.
-
350Kravetz JD, Walsh RF. Team-Based Hypertension Management to Improve Blood Pressure Control. J Prim Care Community Health 2016;7(4):272-5.
-
351Boulware LE, Daumit GL, Frick KD, Minkovitz CS, Lawrence RS, Powe NR. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001; 21(3):221-32.
-
352Overwyk KJ, Dehmer SP, Roy K, Maciosek MV, Hong Y, Baker-Goering MM, et al. Modeling the Health and Budgetary Impacts of a Team-based Hypertension Care Intervention That Includes Pharmacists. Med Care. 2019;57(11):882-9.
-
353Tagliacozzo DM, Luskin DB, Lashof JC, Ima K. Nurse intervention and patient behavior: an experimental study. Am J Public Health. 1974; 64(6): 596-603.
-
354Dickey FF, Mattar ME, Chudzik GM. Pharmacist counsling increases drug regimen compliance. Hospitals. 1975; 49(9): 85-6, 88.
-
355Brazil.Ministério da Saúde. Política Nacional de Educação Permanente em Saúde: o que se tem produzido para o seu fortalecimento. Brasília; 2018.
-
356Brazil.Ministério da Saúde. Síntese de evidências para políticas de saúde: adesão ao tratamento medicamentoso por pacientes portadores de doenças crônicas. Brazilia; 2018.
-
357Marquez Contreras E, Marquez Rivero S, Rodriguez Garcia E, Ramos LLG, Vilas JCP, Suarez AB, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin. 2019;35(1):167-73.
-
358Hallberg I, Ranerup A, Bengtsson U, et al. Experiences, expectations and challenges of an interactive mobile phone-based system to support self-management of hypertension: patients’ and professionals’ perspectives. Patient Prefer Adherence. 2018 Mar 28;12:467-76.
-
359Hallberg I, Ranerup A, Bengstsson U, Kjellgren K. Supporting the self-management of hypertension: Patients’ experiences of using a mobile phone-based system. J Hum Hypertens. 2016; 30(2):141-6.
-
360Schoenthaler A, de la Calle F, Pitaro M, Lum A, Chaplin W, Mogavero J, et al. A Systems-Level Approach to Improving Medication Adherence in Hypertensive Latinos: a Randomized Control Trial. J Gen Intern Med. 2020; 35(1): 182-9. 2019/10/19. DOI: 10.1007/s11606-019-05419-3.
-
361Schoenthaler A, De La Calle F, Barrios-Barrios M, Garcia A, Pitaro M, Lum A, et al. A practice-based randomized controlled trial to improve medication adherence among Latinos with hypertension: study protocol for a randomized controlled trial. Trials. 2015;16:290.
-
362Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: A randomized controlled trial. Patient Educ Couns. 2020; 103: 336-42.
-
363Serene Olin S, Kutash K, Pollock M, et al. Developing quality indicators for family support services in community team-based mental health care. Adm Policy Ment Health. 2014; 41: 7-20.
-
364Ranerup A and Hallberg I. Actors and intentions in the development process of a mobile phone platform for self-management of hypertension. Inform Health Soc Care 2015; 40: 299-318.
-
365Brazil.Ministério da Saúde. Política Nacional de Atenção Básica. Portaria no 2.436, de 21 de setembro de 2017. Brasília;2017.
-
366Riegel GR, Ribeiro PAB, Rodrigues MP, et al.Efficacy of nutritional recommendations given by registered dietitians compared to other healthcare providers in reducing arterial blood pressure: Systematic review and meta-analysis. Clin Nutr. 2018; 37(2): 522-31.
-
367Mitchell LJ, Ball LE, Ross LJ, et al. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J Acad Nutr Diet. 2017; 117(1): 1941-62.
-
368Sladdin I, Chaboyer W, Ball L. Patients’ perceptions and experiences of patient-centred care in dietetic consultations. J Hum Nutr Diet. 2018; 31I2): 188-96.
-
369Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association Between Obesity and Cardiovascular Outcomes: A Systematic Review and Meta-analysis of Mendelian Randomization Studies. JAMA Netw Open. 2018; 1(7): e183788.
-
370Dwivedi AK, Dubey P, Cistola DP. Association Between Obesity and Cardiovascular Outcomes: Updated Evidence from Meta-analysis Studies. Curr Cardiol Rep.2020; 22(4):25.
-
371Zhao CN, Meng X, Li Ya, Li S, Tang GY, Li HB. Fruits for Prevention and Treatment of Cardiovascular Diseases. Nutrients. 2017; 9(6):598.
-
372Mellendick K, Shanahan L, Wideman L, calkins S, Keane S, Lovelady C. et al. Diets Rich in Fruits and Vegetables Are Associated with Lower Cardiovascular Disease Risk in Adolescents. Nutrients. 2018; 10(2):136.
-
373Alissa EM. Ferns GA. Dietary fruits and vegetables and cardiovascular diseases risk. Crit Rev Food Sci Nutr. 2017; 57(9):1950-62.
-
374Aminde LN, Cobiac LJ, Veerman JL. Potential impact of a modest reduction in salt intake on blood pressure, cardiovascular disease burden and premature mortality: a modelling study. Open Heart. 2019; 6(1): e000943.
-
375He FJ, Tan M, Ma Y, et al. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020; 75: 632-47.
-
376Graham GN, Ostrowski M, Sabina AB. Population health-based approaches to utilizing digital technology: a strategy for equity. J Public Health Policy 2016; 37(Suppl 2): 154-66.
-
377Grahame JA. Digital Note-Taking: Discussion of Evidence and Best Practices. J Physician Assist Educ. 2016; 27(1): 47-50.
-
378Zhao R, Bu W, Chen Y, Chen X. The Dose-Response Associations of Sedentary Time with Chronic Diseases and the Risk for All-Cause Mortality Affected by Different Health Status: A Systematic Review and Meta-Analysis. J Nutr Health Aging. 2020; 24(1): 63-70.
-
379Ozemek C, Lavie CJ. Rognmo O. Global physical activity levels - Need for intervention. Prog Cardiovasc Dis. 2019; 62(2): 102-7.
-
380de Rezende LF, Rabacow FM, Viscondi JY, Luiz O, Matsudo V. Effect of physical inactivity on major noncommunicable diseases and life expectancy in Brazil. J Phys Act Health. 2015; 12(3): 299-306.
-
381Ekelund U, Brown WJ, Steene-Johannessen J, Wang M, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019; 53(14): 886-94.
-
382Ferreira T, Cipolotti M, Marques B, Miranda M. A inserção do Profissional de Educação Física nos Núcleos de Apoio a Saúde da Família: visão dos profissionais. Rev Bras Ativ Fís Saúde 2016; 21(3):228-36.
-
383Balamurugan A, Adolph S, Faramawi M, George M. Community Team-Based Care for Hypertension Management: A Public-Private Partnership in Rural Arkansas. J Ark Med Soc. 2017; 113(7):150-4.
-
384Sidney S. Team-Based Care: A Step in the Right Direction for Hypertension Control. Am J Prev Med. 2015; 49(5): e81-e82.
-
385Santschi V, Wuerzner G, Chiolero A, Brurnand B. Team-based care for improving hypertension management among outpatients (TBC-HTA): study protocol for a pragmatic randomized controlled trial. BMC Cardiovasc Disord.2017; 17(1): 39.
-
386Al-Rubaey MG, Shwaish MI. Impact of hypertension education on treatment compliance among hypertensive patients in Baghdad 2017. J Pak Med Assoc .2019; 69(Suppl 3): S9-S12.
-
387Chen Y, Li X, Jing G, Pan B, Long B, Zhi Tong B, et al. Health education interventions for older adults with hypertension: A systematic review and meta-analysis. Public Health Nurs. 2020 ;37(3): 461-9.
-
388Dzau VJ, Balatbat CA. Future of Hypertension. Hypertension. 2019;74(3): 450-7.
-
389Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper P. Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Curr Hypertens Rep. 2015; 17: 94.
-
390Conn VS, Ruppar TM, Chase JD. Blood pressure outcomes of medication adherence interventions: systematic review and meta-analysis. J Behav Med. 2016;39:1065-75.
-
391Mistry N, Keepanasseril A, Wilczynski NL, Nieuwlaat R, Ravall M, Haynes B, et al. Technology-mediated interventions for enhancing medication adherence. J Am Med Inform Assoc. 2015; 22: e177-193.
-
392Lindahl B, Norberg M, Johansson H, Lindvall K, Ng N, Nordin M, et al. Health literacy is independently and inversely associated with carotid artery plaques and cardiovascular risk. Eur J Prev Cardiol. 2020; 27(2): 209-15.
-
393Earl GL, Harris EM, Dave M, Jiang JE. Implementing a health literacy module fostering patient-centered written communication in a cardiovascular prevention elective course. Curr Pharm Teach Learn. 2019;11(7):702-9.
-
394Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. 10) The Effect of Self-Monitoring of Blood Pressure on Medication Adherence and Lifestyle Factors: A Systematic Review and Meta-Analysis. Am J Hypertens. 2015;28(10):1209-21.
-
395Fletcher BR, Hinton L, Hartmann-Boyce J, Self-monitoring blood pressure in hypertension, patient and provider perspectives: A systematic review and thematic synthesis. Patient Educ Couns. 2016;99(2):210-9.
-
396Bengtsson U, Kjellgren K, Hallberg I, Lundin M, Makitalo A. Patient contributions during primary care consultations for hypertension after self-reporting via a mobile phone self-management support system. Scand J Prim Health Care. 2018; 36(1):70-9.
-
397McLean G, Band R, Saunderson K, Murray HP, Little P, McManus RJ, et al. Digital interventions to promote self-management in adults with hypertension systematic review and meta-analysis. J Hypertens. 2016; 34(4):600-12.
-
398Thakkar J, Kurup R, Laba TL, Mobile Telephone Text Messaging for Medication Adherence in Chronic Disease: A Meta-analysis. JAMA Intern Med. 2016; 176(3): 340-9.
-
399John JR, Tannous WK, Jones A. Effectiveness of a patient-centered medical home model of primary care versus standard care on blood pressure outcomes among hypertensive patients. Hypertens Res. 2020;43(9):892-902.
-
400Yan R, Li W, Yin L, Wang Y, Bo J; PURE-China Investigators. Cardiovascular Diseases and Risk-Factor Burden in Urban and Rural Communities in High-, Middle-, and Low-Income Regions of China: A Large Community-Based Epidemiological Study. J Am Heart Assoc. 2017;6(2):e004445.
-
401Malta DC, Silva AGD, Machado ÍE, Sá ACMGN, Santos FMD, Prates EJS, Cristo EB. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J Bras Pneumol. 2019;45(5):e20180384.
-
402Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, Smith N, et al. Screening for High Blood Pressure in Adults: A Systematic Evidence Review for the U.S. Rockville MD:Agency Research and Quality;2014. [Evidence Synthesis No. 121. AHRQ / Publication No. 13-05194-EF-1. ]
-
403Bhatnagar A, Maziak W, Eissenberg T, Ward KD, Thurston G, King BA, et al. Water Pipe (Hookah) Smoking and Cardiovascular Disease Risk: A Scientific Statement from the American Heart Association. Circulation. 2019;139(19):e917-36.
-
404Leone FT, Zhang Y, Evers-Casey S, Evins AE, Eakin MN, Fathi J, et al. Initiating Pharmacologic Treatment in Tobacco-Dependent Adults. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5-e31.
-
405Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
-
406Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH–Sodium Collaborative. Research Group. N Engl J Med. 2001;344:3–10.
-
407Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2020;11(5):1150-60.
-
408Larsson SC, Wallin A, Wolk A. Dietary Approaches to Stop Hypertension diet and incidence of stroke: results from 2 prospective cohorts. Stroke. 2016;47(4):986-90.
-
409Mertens E, Markey O, Geleijnse JM, Lovegrove JA, Gibens DI. Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: evidence from the Caerphilly Prospective Study. Eur J Nutr. 2018;57(3):1245-58.
-
410Soltani S, Arablou T, Jayedi A, Salehi-Abargouei A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutr J. 2020;19(1):37.
-
411Mozaffari H, Ajabshir S, Alizadeh S. Dietary Approaches to Stop Hypertension and risk of chronic kidney disease: A systematic review and meta-analysis of observational studies. Clin Nutr. 2020;39(7):2035-44.
-
412Martínez-González MA, Gea A, Ruiz-Canela M. The mediterranean diet and cardiovascular health. Circ Res. 2019;124(5):779-98.
-
413Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72(1):30-43.
-
414Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58(1):173-91.
-
415Nissensohn M, Román-Viñas B, Sánchez-Villegas A, Piscopo S, Serra-Majem L. The effect of the mediterranean diet on hypertension: a systematic review and meta-analysis. J Nutr Educ Behav. 2016;48(1):42-53.
-
416Jennings A, Berendsen AM, de Groot LCPGM, Feskens EJM, Brzozowska A, Sicinska E, et al. Mediterranean-style diet improves systolic blood pressure and arterial stiffness in older adults. Hypertension. 2019;73(3):578-86.
-
417Domenech M, Roman P, Lapetra J, Garcia de la Corte FJ, Sala-Vila A, de la Torre R, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64(1):69-76.
-
418Fuchs SF. Estudo PREVER: Mudanças de Estilo de Vida. Porto Alegre: Engenho de Idéias; 2011. 47 p.
-
419Powles J, Gahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intake in 1990 and 2010: a systematic analysis of 24h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3(12):e003733.
-
420World Health Organization. WHO. Guideline: Sodium intake for adults and children. Geneva;2012.
-
421Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trial. BMJ. 2020 Feb 24; 368:m315.
-
422He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on bloodpressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ; 2013;346:f1325.
-
423Bernabe-Ortiz A, Sal Y Rosas VG, Ponce-Lucero V, Cárdenas MK, Carrillo-Larco RM, Diez-Canseco F, et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26(3):374-8.
-
424Marklund M, Singh G, Greer R, Cudhea F, Matsushita K, Micha R, Brady T, et al. Estimated population wide benefits and risks in China of lowering sodium through potassium enriched salt substitution: modelling study. BMJ. 2020;369:m824.
-
425Binia A, Jaeger J, Hu Y, Singh A, Zimmermann D. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2015; 33(8):1509-20.
-
426China Salt Substitute Study Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007; 25(10):2011-8.
-
427Zhou B, Wang HL, Wang WL, Wu XM, Fu LY, Shi JP. Long-term effects of salt substitution on blood pressure in a rural north Chinese population. J Hum Hypertens. 2013; 27(7):427-33.
-
428Peng Y-G, Li W, Wen X-X, Li Y, Hu J-H, Zhao L-C. Effects of salt substitutes on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2014;100(6):1448-54.
-
429Jin A, Xie W, Wu Y. Effect of salt reduction interventions in lowering blood pressure in Chinese populations: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2020;10(2):e032941.
-
430Thorning TK, Bertram HC, Bonjour JP, de Groot L, Dupont D, Feeney R, et al. Whole dairy matrix or single nutrients in assessment of health effects: current evidence and knowledge gaps. Am J Clin Nutr. 2017;105(5):1033-45.
-
431Mozaffarian D, Wu JHY. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ Res. 2018;122(2):369-84.
-
432Dehghan M, Mente A, Rangarajan S, Sheridan P, Mohan V, Igbal R, et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2018;392(10161):2288-97
-
433Buendia JR, Li Y, Hu FB, Cabral HJ, Bradlee ML, Quatromoni PA, et al. Regular yougurt intake and risk of cardiovascular disease among hypertensive adults. Am J Hypertens. 2018;31(5):557-65.
-
434Machin DR, Park W, Alkatan M, Mouton M, Tanaka H. Hypotensive effects of solitary addition of conventional nonfat dairy products to the routine diet: a randomized controlled trial. Am J Clin Nutr. 2014;100(1):80-7.
-
435Rietsema S, Eelderink C, Joustra ML, van Vliet IMY, van Londen M, Corpeleijn E, et al. Effect of high compared with low dairy intake on blood pressure in overweight middle-aged adults: results of a randomized crossover intervention study. Am J Clin Nutr. 2019;110(2):340-8.
-
436Hidayat K, Du HZ, Yang J, Chen GC, Zhang Z, Lin ZN, Qin LQ. Effects of milk proteins on blood pressure: a meta-analysis of randomized control trials. Hypertens Res. 2017;40(3):264-70.
-
437Brazil.Ministério da Saúde. Guia Alimentar Para a População Brazileira. 2ª ed. Brasília; 2014.
-
438Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. U.S. Department of Agriculture, Agricultural Research Service, Washington(DC);2015.
-
439Desch S, Schmidt J, Kobler D, Sonnabend M, Eitel I, Sareban M, et al. Effect of cocoa products on blood pressure: systematic review and meta-analysis. Am J Hypertens. 2010;23(1):97-103.
-
440Ried K, Fakler P, Stocks NP, and Cochrane Hypertension Group National Institute of Integrative Medicine. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. 2017 Apr 25;4(4):CD008893.
-
441Mesas AE, Leon-Munoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr. 2011;94(4):1113-26.
-
442van Dam RM, Hu FB, Willett WC. Coffee, caffeine, and health. N Engl J Med. 2020; 383(4):369-78.
-
443D´Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose-response meta-analysis of prospective studies. Eur J Nutr. 2019; 58(1):271-80.
-
444Grosso G, Micek A, Godos J, Pajak A, Sciacca S, Bes-Rastrollo M, Galvano F, Martinez-Gonzalez MA. Long-Term Coffee Consumption Is Associated with Decreased Incidence of New-Onset Hypertension: A Dose-Response Meta-Analysis. Nutrients. 2017;9(8):890.
-
445Ke L, Mason RS, Mpofu E, Vingren JL, Li Y, Graubard BI, et al. Hypertension and other cardiovascular risk factors are associated with vitamin D deficiency in an urban Chinese population: a short report. J Steroid Biochem Mol Biol. 2017;173:286-91.
-
446Zhang D, Cheng C, Wang Y, Sun H, Yu S, Xue Y, et al. Effect of vitamin D on blood pressure and hypertension in the general population: an update meta-analysis of cohort studies and randomized controlled trials. Prev Chronic Dis. 2020;17:E03.
-
447Pilz S, Gaksch M, Kienreich K, Grubler M, Verheyen N, Fahrleitner-Pammer A, et al. Effects of vitamin D on blood pressure and cardiovascular risk factors: a randomized controlled trial. Hypertension. 2015;65(6):1195-201.
-
448Arora P, Song Y, Dusek J, Plotnikoff G, Sabatine MS, Cheng S, et al. Vitamin D therapy in individuals with prehypertension or hypertension: the DAYLIGHT trial. Circulation. 2015;131(3):254-62.
-
449Shu L, Huang K. Effect of vitamin D supplementation on blood pressure parameters in patients with vitamin D deficiency: a systematic review and meta-analysis. J Am Soc Hypertens. 2018;12(7):488-96.
-
450Cormick G, Ciapponi A, Cafferata ML, Belizán JM. Calcium Supplementation for Prevention of Primary Hypertension. Cochrane Database Syst Rev.2015;(6):CD010037.
-
451Li K, Liu C, Kuang X, Deng Q, Zhao F, Li D. Effects of Multivitamin and Multimineral Supplementation on Blood Pressure: A Meta-Analysis of 12 Randomized Controlled Trials. Nutrients. 2018;10(8):1018.
-
452Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat Rev Nephrol. 2019;15(6):367-85.
-
453Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42(5):878–84.
-
454Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, Berrington de Gonzalez A, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86.
-
455Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126-31.
-
456US Department of Health and Human Services. Physical Activity Guidelines for Americans 2018. [Cited in 2020 Apr 12] Available at: https://health.gov/sites/default/files/201909/Physical_Activity_Guidelines_2nd_edition.pdf .
» https://health.gov/sites/default/files/201909/Physical_Activity_Guidelines_2nd_edition.pdf -
457Ekelund U, Steene-Johannessen J, Brown WJ. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonized meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-10.
-
458Liu X, Zhang D, Liu Y, Sun X, Han C, Wang B, et al. Dose-response associations between physical activity and incident hypertension: a systematic review and meta-analysis of cohort studies. Hypertension. 2017; 69(5):813-20.
-
459Cao L, Li X, Yan P, Wang X, Li M, Li R, et al. The effectiveness of aerobic exercise for hypertensive population: A systematic review and meta-analysis. J Clin Hypertens. 2019;21(7):868-76.
-
460MacDonald HV, Johnson BT, Huedo-Medina TB, Livingston J, Forsyth KC, Kraemer WJ, et al. Dynamic Resistance Training as Stand- Alone Antihypertensive Lifestyle Therapy: A Meta-Analysis. J Am Heart Assoc. 2016;5(10): e003231.
-
461Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57(1-2):154-60.
-
462Igarashi Y, Nogami Y. The effects of regular aquatic exercise on blood pressure: a meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2018;25(2):190-9.
-
463Cramer H, Langhorst J, Dobos G, Lauche R. Yoga for metabolic syndrome: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23(18):1982-93.
-
464Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, et al. Tai Chi for Essential Hypertension: a Systematic Review of Randomized Controlled Trials. Curr Hypertens Rep. 2020;22(3):25.
-
465Costa EC, Hay JL, Kehler DS, Boreskie KF, Arora RC, Umpierre D, et al. Effects of High-Intensity Interval Training Versus Moderate- Intensity Continuous Training on Blood Pressure in Adults with Pre- to Established Hypertension: a Systematic Review and Meta-Analysis of Randomized Trials. Sports Med. 2018;48(9):2127-42.
-
466Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, Pescatello LS. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473-9.
-
467Meneguelo RS et al. III Diretrizes da Sociedade Brazileira de Cardiologia sobre Teste Ergométrico. Arq Bras Cardiol. 2010;95(5, supl.1):1-26.
-
468Mahtani KR, Nunan D, Heneghan CJ. Device-guided breathing exercises in the control of human blood pressure: systematic review and meta-analysis. J Hypertens. 2012; 30(5):852-60.
-
469Zou Y, Zhao X, Hou YY, Liu T, Wu Q, Huang YH, et al. Meta-Analysis of Effects of Voluntary Slow Breathing Exercises for Control of Heart Rate and Blood Pressure in Patients with Cardiovascular Diseases. Am J Cardiol. 2017;120(1):148–53.
-
470Ubolsakka-Jones C, Tongdee P, Jones DA. The effects of slow loaded breathing training on exercise blood pressure in isolated systolic hypertension. Physiother Res Int. 2019;24(4):e1785.
-
471Kow FP, Adlina B, Sivasangari S, Punithavathi N, Ng KK, Ang AH, et al. The impact of music guided deep breathing exercise on blood pressure control - A participant blinded randomised controlled study. Med J Malaysia. 2018;73(4):233–8.
-
472Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61(6):1360-83.
-
473Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews. 2013,12:CD006577.
-
474Do Amaral MAS, Neto MG, de Queiroz JG, Martins-Filho PRS, Saquetto M B, Carvalho VO. Effect of music therapy on blood pressure of individuals with hypertension: A systematic review and Meta-analysis. Int J Cardiol. 2016;214:461–4.
-
475Kühlmann AYR, Etnel JRG, Roos-Hesselink JW, Jeekel J, Bogers AJJC, Takkenberg JJM. Systematic review and meta-analysis of music interventions in hypertension treatment: a quest for answers. BMC Cardiovasc Disord. 2016;16:69.
-
476Maynard BR, Solis MR, Miller VL, Brendel KE. Mindfulness-based interventions for improving cognition, academic achievement, behavior, and socioemotional functioning of primary and secondary school students. Campbell Systematic Reviews; 2017 https://doi.org/10.4073/CSR.2017.5
» https://doi.org/10.4073/CSR.2017.5 -
477Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation Programs for Psychological Stress and Well-being A Systematic Review and Meta-analysis. JAMA Intern Med. 2014;174(3):357-68.
-
478Ooi SL, Giovino M, Pak SC. Transcendental meditation for lowering blood pressure: An overview of systematic reviews and meta-analyses. Complement Ther Med. 2017;34:26-34.83.
-
479GN, Lange RA, Bairey-Merz CN, Davidson RJ, Jamerson K, Mehta PK, et al; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Hypertension. Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart Assoc. 2017;6(10):e002218.
-
480Steinhauser KE, Fitchett G, Handzo GF, Johnson KS, Koenig HG, Pargament KI, et al. State of the Science of Spirituality and Palliative Care Research Part I: Definitions, Measurement, and Outcomes. J Pain Symptom Manag. 2017;54(3):428-40.
-
481Lucchese FA, Koenig HG. Religion, spirituality and cardiovascular disease: research, clinical implications, and opportunities in Brazil. Rev Bras Cir Cardiovasc. 2013;28(1):103-28.
-
482Chida Y, Steptoe A, Powell LH. Religiosity/Spirituality and Mortality A Systematic Quantitative Review. Psychother Psychosom. 2009;78(2):81–90.
-
483Li S, Stampfer MJ, Williams DR, VanderWeele TJ. Association of Religious Service Attendance With Mortality Among Women. JAMA Intern Med 2016;176(6):777-85.
-
484VanderWeele TJ, Yu J, Cozier YC, Wise L, Argentieri MA, Rosenberg L, et al. Attendance at Religious Services, Prayer, Religious Coping, and Religious/Spiritual Identity as Predictors of All-Cause Mortality in the Black Women’s Health Study. Am J Epidemiol. 2017;185(7):515-22.
-
485Abu HO, Ulbricht C, Ding E, Allison JJ, Salmoirago-Blotcher E, Goldberg RJ, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res. 2018;27(11):2777-97.
-
486Shattuck EC, Muehlenbein MP. Religiosity/Spirituality and Physiological Markers of Health. J Relig Health. 2020;59(2):1035-54.
-
487Spence ND, Farvid MS, Warner ET, et al. Religious Service Attendance, Religious Coping, and Risk of Hypertension in Women Participating in the Nurses’ Health Study II. Am J Epidemiol. 2020;189(3):193-203.
-
488Holt-Lunstad J, Steffen PR, Sandberg J, Jensen B. Understanding the connection between spiritual well-being and physical health: an examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. J Behav Med. 2011;34(6):477-88.
-
489Fitchett G, Powell LH. Daily spiritual experiences, systolic blood pressure, and hypertension among midlife women in SWAN. Ann Behav Med. 2009;37(3):257-67.
-
490Buck AC, Williams DR, Musick MA, Sternthal MJ. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Soc Sci Med. 2009;68(2):314-22.
-
491Suh H, Hill TD, Koenig HG. Religious Attendance and Biological Risk: A National Longitudinal Study of Older Adults. J Relig Health. 2019;58(4):1188-202.
-
492Badanta-Romero B, de Diego-Cordero R, Rivilla-García E. Influence of Religious and Spiritual Elements on Adherence to Pharmacological Treatment. J Relig Health. 2018;57(5):1905-17.
-
493Oliveira JA, Anderson MI, Lucchetti G, Pires EV, Gonçalves LM. Approaching Spirituality Using the Patient-Centered Clinical Method. J Relig Health. 2019;58(1):109-18.
-
494Balboni TA, Fitchett G, Handzo GF, et al. State of the Science of Spirituality and Palliative Care Research Part II: Screening, Assessment, and Interventions. J Pain Symptom Manage. 2017;54(3):441-53.
-
495Task Force of the Latin American Society of Hypertension. Guidelines on the management of arterial hypertension and related comorbidities in Latin America. Journal of Hypertension. 2017;35(8):1529–45.
-
496Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384(9943):591-598.
-
497Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
-
498Sytkowski PA, D’Agostino RB, Belanger AJ, Kannel WB. Secular trends in long-term sustained hypertension, long-term treatment, and cardiovascular mortality. The Framingham Heart Study 1950 to 1990. Circulation. 1996;93(4): 697–703.
-
499Bang CN, Devereux RB, Okin PM. Regression of electrocardiographic left ventricular hypertrophy or strain is associated with lower incidence of cardiovascular morbidity and mortality in hypertensive patients independent of blood pressure reduction - A LIFE review. J Electrocardiol. 2014;47(5):630–35.
-
500Fagard RH, Celis H, Thijs L, Wouters S. Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studies. Hypertension. 2009;54(5):1084–91.
-
501Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45(2):198–202.
-
502Mancia G, Rea F, Corrao G, Grassi G. Two-Drug Combinations as First-Step Antihypertensive Treatment. Circ Res. 2019;124(7):1113-23.
-
503Póvoa R, Barroso WS, Brandão AA, Jardim PC, Barroso O, Passarelli O Jr, et al. I Brazilian position paper on antihypertensive drug combination. Arq Bras Cardiol. 2014;102(3):203-10.
-
504Yugar-Toledo JC, Moreno Júnior H, Gus M, Rosito GBA, Scala LCN, Muxfeldt ES et al. Brazilian Position Statement on Resistant Hypertension - 2020. Arq Bras Cardiol. 2020;114(3):576-96.
-
505Gradman AH, Basile JN, Carter BL, Bakris GL; American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(1):42-50.
-
506Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: metaanalysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300.
-
507Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427.
-
508Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997;277(9):739-45.
-
509. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP-Cooperative Research Group. JAMA. 1991;265(24):3255-64.
-
510ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcome in high-risk hypertensive patients to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;228(23):2981-97.
-
511Dhalla IA, Gomes T, Yao Z, Nagge J, Persaud N, Hellings C, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158(6):447-55.
-
512Hripcsak G, Suchard MA, Shea S, Chen R, You SC, Pratt N, et al. Comparison of Cardiovascular and Safety Outcomes of Chlorthalidone vs Hydrochlorothiazide to Treat Hypertension. JAMA Intern Med. 2020;180(4):542–51.
-
513Roush GC, Ernst ME, Kostis JB, Tandon S, Sica DA. Head-to-Head Comparisons of Hydrochlorothiazide With Indapamide and Chlorthalidone. Antihypertensive and Metabolic Effects. Hypertension 2015; 65(5):1041–6.
-
514Elliott WJ, Ram CV. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13(9):687-9.
-
515Messerli FH. Calcium antagonists in hypertension: from hemodynamics to outcomes. Am J Hypertens. 2002;15(7 Pt 2):94S-7S.
-
516Elliott WJ, Bandari A. The role of calcium antagonists in stroke prevention. J Clin Hypertens (Greenwich). 2005;7(4 Suppl 1):5-8.
-
517Nathan S, Pepine CJ, Bakris GL. Calcium antagonists: effects on cardiorenal risk in hypertensive patients. Hypertension 2005;46(4):637-42.
-
518Rollins G. Calcium antagonist and beta blocker regimens found equally effective in hypertensive patients with coronary artery disease. Rep Med Guidel Outcomes Res. 2004;15(2):1, 5-6.
-
519Vejakama P, Thakkinstian A, Lertrattananon D, Ingsathit A, Ngarmukos C, Attia J. Reno-protective effects of renin-angiotensin system blockade in type 2 diabetic patients: a systematic review and network meta-analysis. Diabetologia 2012;55(3):566-78.
-
520Baram M, Kommuri A, Sellers SA, Cohn JR. ACE inhibitor-induced angioedema. J Allergy Clin Immunol Pract. 2013;1(5):442-5.
-
521Ryan MJ, Tuttle KR. Elevations in serum creatinine with RAAS blockade: why isn’t it a sign of kidney injury? Curr Opin Nephrol Hypertens. 2008;17(5):443-9.
-
522Maschio G, Alberti D, Janin G, Locatelli F, Mann JF, Motolese M, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med. 1996;334(15):939-45.
-
523Polifka JE. Is there an embryopathy associated with first-trimester exposure to angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists? A critical review of the evidence. Birth Defects Res A Clin Mol Teratol. 2012;94(8):576-98.
-
524Laube GF, Kemper MJ, Schubiger G, Neuhaus TJ. Angiotensin-converting enzyme inhibitor fetopathy: long-term outcome. Arch Dis Child Fetal Neonatal Ed. 2007;92(5):F402-3.
-
525Dahlof B, Devereux R, Kjeldsen S, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the losartan intervention or endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):995-1003.
-
526Lindholm LH, Ibsen H, Dahlof B, Devereux RB, Beevers G, de Faire U, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359(9311):1004-10.
-
527Julius S, Kejdelsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients in high cardiovascular risk treated with regimens based on valsartan and amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022-31.
-
528Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, et al; CHARM Investigators and Committees. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM Overall programme. Lancet. 2003;362(9386):759-66.
-
529Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al; RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861-9.
-
530Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, et al; Collaborative Study Group. Renoprotective effect of the angiotensin receptor antagonist irbersartan in patients with nephropathy due to type 2 diabetes. N Eng J Med. 2001;345(12):851-60.
-
531Parving HH, Lehnert H, Brochner-Mortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. The effect of irbersartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345(12):870-8.
-
532Helfand M, Peterson K, Christensen V, Dana T, Thakurta S. Drug class review: Beta adrenergic blockers. Update 4. 2009. [Internet]. [Cited in 2020 apr 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK47172/ .
» https://www.ncbi.nlm.nih.gov/books/NBK47172/ -
533López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al; Task Force on Beta-Blockers of the European Society of Cardiology. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25(15):1341-62.
-
534Dulin B, Abraham WT. Pharmacology of carvedilol. Am J Cardiol. 2004;93(9A):3B-6B.
-
535Pedersen ME, Cockcroft JR. The vasodilatory beta-blockers. Curr Hypertens Rep. 2007;9(4):269-77.
-
536Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366(9496):1545-1553.
-
537Vongpatanasin W, Kario K, Atlas SA, Victor RG. Central sympatholitic drugs. J Clin Hypertens 2011;13(9):658-61.
-
538Atlas D, Diamant S, Zonnenschein R. Is the imidazoline site a unique receptor? A correlation with clonidine-displacing substance activity. Am J Hypertens. 1992;5(4 Pt 2):83S.
-
539Kaplan NM, Victor RG. Clinical hypertension. 11th ed. China: Wolters Kluwer; 2015. p. 198-262.
-
540Wagner ML, Walters AS, Coleman RG, Hening WA, Grasing K, Chokroverty S. Randomized double-blind, placebo-controlled study of clonidine in restless legs syndrome. Sleep. 1996;19(1):52-8.
-
541Bond WS. Psychiatric indications for clonidine. J Clin Psychopharmacol. 1986;6(2):81-7.
-
542Pandya KJ, Raubertas RF, Flynn PJ, Hynes HE, Rosenbluth RJ, Kirshner JJ, et al. Oral clonidine in postmenopausal patients with breast cancer experiencing tamoxifen-induced hot flashes: a University of Rochester Cancer Center Community Clinical Oncology Program study. Ann Intern Med. 2000,132(10):788-93.
-
543Fedorak RN, Field M, Chang EB. Treatment of diabetic diarrhea with clonidine. Ann Intern Med. 1985;102(2):197-9.
-
544Esler M, Dudley F, Jennings G, Debinski H, Lambert G, Jones P, et al. Increased sympathetic nervous activity and the effects of its inhibition with clonidine in alcoholic cirrohosis. Ann Intern Med. 1992;116(6):446-55.
-
545Müller DN, Derer W, Dechend R. Aliskiren-mode of action and preclinical data. J Mol Med. 2008;86(6):659-62.
-
546Danser AH. (Pro)renin receptors: are they biologically relevant? Curr Opin Nephrol Hypertens. 2009;18(1):74-8.
-
547Singh VP, Le B, Khode R, Baker KM, Kumar R. Intracellular angiotensin II production in diabetic rats is correlated with cardiomyocyte apoptosis, oxidative stress, and cardiac fibrosis. Diabetes. 2008;57(12):3297-306. Erratum in: Diabetes. 2009;58(3):770.
-
548Musini VM, Fortin PM, Bassett K, Wright JM. Blood pressure lowering efficacy of renin inhibitors for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD007066.
-
549Heerspink HJL, Persson F, Brenner BM, Chaturvedi N, Brunel P, McMurray JJ, et al. Renal outcomes with aliskiren in patients with type 2 diabetes: a prespecified secondary analysis of the ALTITUDE randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(4):309-17.
-
550Bjerre HL, Christensen JB, Buus NH, Simonsen U, Su J. The role of aliskiren in the management of hypertension and major cardiovascular outcomes: a systematic review and meta-analysis. J Hum Hypertens. 2019;33(11):795-806.
-
551Zhang JT, Chen KP, Guan T, Zhang S. Effect of aliskiren on cardiovascular outcomes in patients with prehypertension: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2015;9:1963-71.
-
552Gradman AH, Parisé H, Lefebvre P, Falvey H, Lafeuille MH, Duh MS. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension. 2013;61(2):309-18.
-
553Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-Dose Combinations Improve Medication Compliance: A Meta-Analysis. Am J Med. 2007;120(8):713–9.
-
554Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, et al. Benazepril plus Amlodipine or Hydrochlorothiazide for Hypertension in High-Risk Patients. N Engl J Med. 2008;359(23):2417–28.
-
555Jamerson KA, Bakris GL, Weber MA. 24-Hour Ambulatory Blood Pressure in the ACCOMPLISH Trial. N Engl J Med. 2010;363(1):98–8.
-
556Weber MA, Jamerson K, Bakris GL, Weir MR, Zappe D, Zhang Y, et al. Effects of body size and hypertension treatments on cardiovascular event rates: subanalysis of the ACCOMPLISH randomised controlled trial. Lancet. 2013;381(9866):537–45.
-
557Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–81.
-
558Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906.
-
559Patel A, ADVANCE Collaborative Group, MacMahon S, Chalmers J, Neal B, Woodward M, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9500):829–40.
-
560Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of Hypertension in Patients 80 Years of Age or Older. N Engl J Med. 2008;358(18):1887–98.
-
561Dahlöf B, Hansson L, Lindholm LH, Scherstén B, Ekbom T, Wester P-O. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281–5.
-
562Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751–6.
-
563Calhoun DA, Lacourcière Y, Chiang YT, Glazer RD. Triple antihypertensive therapy with amlodipine, valsartan, and hydrochlorothiazide: a randomized clinical trial. Hypertension. 2009;54(1):32-9.
-
564Krieger EM, Drager LF, Giorgi DMA, Pereira AC, Barreto-Filho JAS, Nogueira AR, et al. Spironolactone Versus Clonidine as a Fourth-Drug Therapy for Resistant Hypertension: The ReHOT Randomized Study (Resistant Hypertension Optimal Treatment). Hypertension. 2018;71(4):681-90.
-
565Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, et al. The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies. Am J Hypertens. 2015;28(11):1376–85.
-
566Liu G, Zheng XX, Xu YL, Lu J, Hui RT, Huang XH. Effect of aldosterone antagonists on blood pressure in patients with resistant hypertension: a meta-analysis. J Hum Hypertens. 2015;29(3):159-66.
-
567Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386(10008):2059–68.
-
568Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372(9638):547–53.
-
569Parving H-H, Brenner BM, McMurray JJV, de Zeeuw D, Haffner SM, Solomon SD, et al. Cardiorenal End Points in a Trial of Aliskiren for Type 2 Diabetes. N Engl J Med. 2012;367(23):2204–13.
-
570Ogihara T, Saruta T, Rakugi H, Saito I, Shimamoto K, Matsuoka H, et al. Combinations of olmesartan and a calcium channel blocker or a diuretic in elderly hypertensive patients: a randomized, controlled trial. J Hypertens. 2014;32(10):2054–63.
-
571Liu L, Zhang Y, Liu G, Li W, Zhang X, Zanchetti A. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens. 2005;23(12):2157–72.
-
572Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757-64.
-
573Liu L, Wang JG, Gong L, Liu G, Staessen JA. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. Systolic Hypertension in China (Syst-China) Collaborative Group. J Hypertens. 1998;16(12 Pt 1):1823-9.
-
574Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J Clin Res 1986;293(6555):1145–51.
-
575Webster R, Salam A, Silva HA, Selak V, Stepien S, Rajapakse S, et al. Fixed Low-Dose Triple Combination Antihypertensive Medication vs Usual Care for Blood Pressure Control in Patients With Mild to Moderate Hypertension in Sri Lanka: A Randomized Clinical Trial. JAMA. 2018;320(6):566–79.
-
576Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15.
-
577Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics – 2018 update: a report from the American Heart Association. Circulation. 2018 Mar 20;137(12):e67-e492.
-
578Gaede P, Vedel P, Larsen N, Gunnar VH Jensen, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383-93.
-
579. Hypertension in Diabetes Study (HDS): I. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertens. 1993;11(3):309-17.
-
580James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. Erratum in: JAMA. 2014;311(17):1809.
-
581Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810.
-
582Niskanen L, Hedner T, Hansson L, Lanke J, Niklason A; CAPPP Study Group. Reduced cardiovascular morbidity and mortality in hypertensive diabetic patients on first-line therapy with an ACE inhibitor compared with a diuretic/ beta-blocker-based treatment regimen: a sub analysis of the Captopril Prevention Project. Diabetes Care. 2001;24(12):2091-6.
-
583Ostergren J, Poulter NR, Sever PS, Dahlof B, Wedel H, Beevers G, et al. ASCOT Investigators. The Anglo-Scandinavian Cardiac OutcomesTrial: blood pressure-lowering limb: effects in patients with type II diabetes. J Hypertens. 2008;26:2103-.11.
-
584Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, et al. ACCOMPLISH Investigators. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010;56(1):77-85.
-
585Tocci G, Paneni F, Palano F, Sciarretta S, Ferrucci A, Kurtz T, et al. Angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers and diabetes: a meta-analysis of placebo-controlled clinical trials. Am J Hypertens. 2011;24(5):582-90.
-
586Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hipertension in the metabolic syndrome. Nutr J. 2008 Apr 17;7:10.
-
587Alberti KG, Zimmet P, Shaw J. Metabolic Syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469-80.
-
588Lebovitz HE, Banerji MA. Point: visceral adiposity is causally related to insulin resistance. Diabetes Care. 2005;28(9):2322-5.
-
589Kahn R, Buse J, Ferrannini E, Stern M. The metabolic Syndrome: Time for a critical appraisal: Joint statement from American Diabetes Association and European Association for the Study of Diabetes. Diabetes Care. 2005; 84 Supll 1):3-28.
-
590Gagliardi ART. Obesidade central, bases hormonais e moleculares da síndrome metabólica. Rev Soc Cardiol Estado de São Paulo. 2004;14(4):557-66.
-
591Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al.Prevention of type 2 diabetes mellitus by changes in life style among subjects with impaired glucose tolerance. N Engl J Med. 2001; 344(18):1343–50.
-
592Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-52. Erratum in: Circulation. 2005;112(17):e298.
-
593Stears AJ, Woods SH, Watts MM, Burton TJ, Graggaber J, Mir FA, Brown MJ. A double-blind, placebo-controlled, crossover trial comparing the effects of amiloride and hydrochlorothiazide on glucose tolerance in patients with essential hypertension. Hypertension .2012; 59(5):934–42.
-
594Borghi C, Bacchelli S, Degli Esposti D, Bignamini A, Magnani B, Ambrosioni E. Effects of the administration of an angiotensin-converting enzyme inhibitor during the acute pHAe of myocardial infarction in patients with arterial hypertension. SMILE Study Investigators. Survival of Myocardial Infarction Long-term Evaluation. Am J Hypertens. 1999;12(7):665-72.
-
595Gustafsson F, Kober L, Torp-Pedersen C, Hildebrandt P, Ottesen MM, Sonne B, et al. Long-term prognosis after acute myocardial infarction in patients with a history of arterial hypertension. TRACE study group. Eur Heart J. 1998;19(4):588-94.
-
596Arnold JM, Yusuf S, Young J. Prevention of heart failure in patients in the heart outcomes prevention evaluation (HOPE) study. Circulation. 2003;107(9):1284-90.
-
597Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006;144(12):884-93.
-
598Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, et al. ONTARGET investigators. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27(7):1360-9.
-
599Zanchetti A, Mancia G. Longing for clinical excellence: a critical outlook into the NICE recommendations on hypertension management--is nice always good? J Hypertens. 2012;30(4):660-8.
-
600Mancia G, Parati G, Bilo G, Gao P, Fagard R, Redon J, et al. Ambulatory blood pressure values in the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET). Hypertension. 2012;60(6):1400-6.
-
601Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al., CLARIFY Investigators. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet 2016;388(10056):2142–52.
-
602Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-43.
-
603Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. African American Study of Kidney Disease and Hypertension Study Group: Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: Results from the AASK trial. JAMA. 2002;288(19):2421-31.
-
604Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. Modification of Diet in Renal Disease Study Group: The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. N Engl J Med.1994;330(13): 877-84.
-
605Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(10):1498-505.
-
606Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P, et al. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73,913 patients. J Hypertens. 2011;29(7):1253-69.
-
607Cushman WC, Evans GW, Byington RP, Goff, Jr DC, Grimm RH, Cutler JA, et. al. ACCORD Study Group: Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17): 1575-85.
-
608Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, et al. VA NEPHRON-D Investigators. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med 2013;369(20):1892-903.
-
609Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, et al. ACCOMPLISH Trial Investigators. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomized controlled trial. Lancet. 2010;375(9721):1173-81.
-
610Foody JM, Farrell MH, Krumholz HM. beta-blocker therapy in heart failure: Scientific review. JAMA 2002;287(7): 883–9.
-
611Clinical Trial. Efficacy and Safety of Finerenone in Subjects with Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (NCT02540993). US: National Institutes of Health; 2020.
-
612Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and post-dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. CJASN. May 2006;1(3):389-98.
-
613Silva GV, Barros S, Abensur H, Ortega KC, Mion Jr D. Cochrane Renal Group Prospective Trial Register: CRG060800146. Home blood pressure monitoring in monitoring in blood pressure control among hemodialysis patients: an open randomized clinical trial. Nephrol Dial Transplant. 2009; 24(12):3805-11.
-
614Georgianos PI, Agarwal R. Blood pressure and mortality in long-term hemodialysis-time to move forward. Am J Hypertens. 2017;30(3):211-22.
-
615Bansal N, McCulloch CE, Lin F, Alper A, Anderson AH, Cuevas M, et al. Blood pressure and risk of cardiovascular events in patients on chronic hemodialysis: the CRIC study (Chronic Renal Insufficiency Cohort). Hypertension. 2017;70(2):435-43.
-
616Georgianos PI, Agarwal R. Systolic and diastolic hypertension among patients on hemodialysis: Musings on volume overload, arterial stiffness, and erythropoietin. Semin Dial. 2019;32(6):507-12.
-
617Tada T, Kusano KF, Ogawa A, Iwasaki J, Sakuragi J, Kusano I, et al. The predictors of central and obstructive sleep apnoea in haemodialysis patients. Nephrol Dial Transplant 2007; 22:1190-7.
-
618Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG, et al. Hypertension in hemodialysis patients treated with atenolol or lisinopril: A randomized controlled trial. Nephrol Dial Transplant.2014;29(3):672-81.
-
619Kishnan N and Peixoto AJ. We hold antihypertensives prior to dialysis. Semin Dial. 2016 Jul;29(4):323-5.
-
620Agarwal R and Sinha AD. Clinical pharmacology of antihypertensive therapy for the treatment of hypertension in chronic kidney disease. Clin J Am Soc of Nephrol 2019;14(5):757-64.
-
621Cross NB, Webster AC, Masson P, O’ Connel PJ, Craig JC, et al. Antihypertensive treatment for kidney transplant recipients. Transplantation. 2009;88(1):7-18.
-
622Ibrahim HN, Jackson S, Connaire J, Matas A, Ney A, Najafian B, et al. Angiotensin II blockade in kidney transplant recipients. J Am Soc Nephrol. 2013;24(2):320-7.
-
623Stokes J 3rd, Kannel WB, Wolf PA, D’Agostino RB, Cupples LA. Blood pressure as a risk factor for cardiovascular disease the framingham study-30 years of follow-up. Hypertension. 1989;13(5):I-13-I–18.
-
624Kannel WB. Incidence and epidemiology of heart failure. Heart Fail Rev. 2000;5(2):167–73.
-
625Goyal D, Macfadyen RJ, Watson RD, Lip GYH. Ambulatory blood pressure monitoring in heart failure: A systematic review. Eur J Heart Fail. 2005;7(2):149–56.
-
626Pfeffer MA. Heart Failure and Hypertension Importance of Prevention Heart failure Randomized clinical trials Antihypertensive agents Prevention. 2017;101(1):19–28.
-
627Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J Am Coll Cardiol. 1996;27(5):1214–8.
-
628Tadic M, Cuspidi C, Frydas A, Grassi G. The role of arterial hypertension in development heart failure with preserved ejection fraction: just a risk factor or something more? Heart Fail Rev. 2018;23(5):631–9.
-
629Kostis JB, Davis BR, Cutler J, Grimm RH, Berge KG, Cohen JD, et al. Prevention of heart failure by antihypertensive drug treatment in older persons with isolated systolic hypertension. J Am Med Assoc. 1997;278(3):212–6.
-
630Thomopoulus C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment .6.Prevention of heart failure and new-onset heart failure–meta-analyses of randomized trials. J Hypertens. 2016;34(3):373-84.
-
631Yancy CW, Jessup M, Bozkurt B, Butler J, Casey Jr DE, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology / American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017; 136(6):e137-e161.
-
632Rohde LEP, Montera MW, Bocchi EA, Clausell NO, Albuquerque DC, Rassi S, et al. Diretriz Brazileira de insuficiência cardíaca crônica e aguda. Arq Bras Cardiol. 2018;111(3):436–539.
-
633McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, et al; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371 (11): 993-1004.
-
634Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJV, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-preserved trial. Lancet. 2003;362(9386):777–81.
-
635Forman D, Gaziano JM. Irbesartan in patients with heart failure and preserved ejection fraction. Curr Cardiovasc Risk Rep. 2009;3(5):311–2.
-
636Cleland JGF, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27(19):2338–45.
-
637Yamamoto K, Origasa H, Hori M. Effects of carvedilol on heart failure with preserved ejection fraction: The Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15(1):110–8.
-
638Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
-
639Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20.
-
640Lee TT, Chen J, Cohen DJ, Tsao L. The association between blood pressure and mortality in patients with heart failure. Am Heart J. 2006;151(1):76-83.
-
641Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43(8):1439–44.
-
642Rouleau JL, Roecker EB, Tendera M, Mohacsi P, Krum H, Katus HA, et al. Influence of pretreatment systolic blood pressure on the effect of carvedilol in patients with severe chronic heart failure: The Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) study. J Am Coll Cardiol. 2004;43(8):1423–9.
-
643Anand IS, Rector TS, Kuskowski M, Thomas S, Holwerda NJ, Cohn JN. Effect of baseline and changes in systolic blood pressure over time on the effectiveness of valsartan in the Valsartan Heart FailureTrial. Circ Heart Fail. 2008;1(1):34-42
-
644Böhm M, Young R, Jhund PS, Solomon SD, Gong J, Lefkowitz MP, et al. Systolic blood pressure, cardiovascular outcomes and efficacy and safety of sacubitril/ valsartan (LCZ696) in patients with chronic heart failure and reduced ejection fraction: Results from PARADIGM-HF. Eur Heart J. 2017;38(15):1132-43.
-
645Rashid P. Leornardi-Bee J. Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke. 2003;34(11):2741-8.
-
646PATS Collaborating Group. Poststroke antihypertensive treatment study: a preliminary result. Chin Med J (Engl). 1995;108(9):710-7.
-
647Gueyffier F, Boissel JP, Boutitie F, Pocock S, Coope J, Cutler J, et al. Effect of antihypertensive treatment in patients having already suffered from stroke. Gathering the evidence. The INDANA (IN-dividual Data Analysis of Antihypertensive intervention trials) Project Collaborators. Stroke. 1997;28(12):2557-62.
-
648Liu L, Wang Z, Gong L, Zhang Y, Thijs L, Staessen JA, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32(11):1032-40.
-
649Schrader J, Luders S, Kulschewski A, Hammersen F, Plate K, Berger J, et al; MOSES Study Group. Morbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention: principal results of a prospective randomized controlled study (MOSES). Stroke. 2005;36(6):1218-26.
-
650Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, et al; ProFESS Study Group. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med. 2008;359(12):1225-37.
-
651White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, et al; SPS3 Investigators. Blood pressure after recent stroke: baseline findings from the secondary prevention of small subcortical strokes trial. Am J Hypertens. 2013;26(9):1114-22.
-
652Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
-
653Rodriguez-Luna D, Pineiro S, Rubiera M, Ribo M, Coscojuela P, Pagola J, et al. Impact of blood pressure changes and courseon hematoma growth in acute intracerebral hemorrhage. Eur J Neurol.2013;20(9):1277–83.
-
654Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al, INTERACT2 Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355–65.
-
655Ahmed N, Wahlgren N, Brainin M, Castillo J, Ford GA, Kaste M, et al. Relationship of blood pressure, antihypertensive therapy, and outcome inischemic stroke treated with intravenous thrombolysis: retrospective analysisfrom Safe Implementation of Thrombolysis in Stroke-International StrokeThrombolysis Register (SITS-ISTR). Stroke. 2009;40(7):2442–9.
-
656Wu W, Huo X, Zhao X, Liao X, Wang C, Pan Y, et al.Relationship between blood pressure and outcomes in acute ischemic strokepatients administered lytic medication in the TIMS-China Study. PLoS One.2016;11(2):e0144260.
-
657Lee M, Ovbiagele B, Hong KS, Wu YL, Lee JE, Rao NM, et al. Effect of blood pressure lowering in early ischemic stroke: meta-analysis. Stroke. 2015;46(7):1883-9.
-
658Zhao R, Liu FD, Wang S, Peng JL, Tao XX, Zheng B, et al. Blood pressure reduction in the acute phase of an ischemic stroke does not improve short- or longtermdependency or mortality: a meta-analysis of current literature. Medicine(Baltimore) 2015;94(23):e896.
-
659Bateman BT, Bansil P, Hernandez-Diaz S, Mhyre JM, Callaghan WM, Kuklina EV. Prevalence, trends, and out-comes of chronic hypertension: a nationwide sample of delivery admissions. Am J Obstet Gynecol. 2012;206(2):134.e1–8.
-
660Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–44.
-
661Ramos JGL, Sass N, Costa SHM. Preeclampsia. Rev Bras Ginecol Obstet. 2017;39(9):496–512.
-
662Abalos E, Cuesta C, Grosso AL, Chou D, Say L. Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):1–7.
-
663Giordano JC, Parpinelli MA, Cecatti JG, Haddad SM, Costa ML, Surita FG, et al. The burden of eclampsia: results from a multicenter study on surveillance of severe maternal morbidity in Brazil. PLoS One. 2014;9(5):e97401.
-
664. American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019 Jan;133(1):e1-e25.
-
665American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26-e50.
-
666Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291-310.
-
667Hofmey GJ, Lawrie TA, Atallah ÁN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2014; 6:CD001059.
-
668. CLASP: a randomized trial of low-dose aspirin for the prevention and treatment of pre-eclampsia among 9364 pregnant women. CLASP (Collaborative Low dose Aspirin Study in Pregnancy) Collaborative Group. Lancet. 1994; 343(8898):619–29.
-
669Duley L, Henderson-Damart DJ, Meher S, King JF. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database of Syst Rev.2004;(1): CD 004659.
-
670Rolnik DL, Wright D, Poon L, O’Gorman N, Syngelaki A, de Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk of preterm preeclampsia. N Engl J Med. 2017;377(7):613–22.
-
671Hypertension in pregnancy: diagnosis and management NICE guideline Published: 25 June 2019.[Internet] [Cited in 2019 may 23] Available at: www.nice.org.uk/guidance/ng133 .
» www.nice.org.uk/guidance/ng133 -
672World Health Organization. WHO. Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia. Geneve: 2011.
-
673Poon LC, Shennan A, Hyett JA, Kapur A, Hadar E, Divakar H, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019;145(Suppl 1):1-33.
-
674American College of Obstetricians and Gynecologists (ACOG). ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet Gynecol. 2019;133(2):e174-e180.
-
675Martin JN Jr, Thigpen BD, Moore RC, Rose CH, Cushman J, May W. Stroke and severe preeclampsia and eclampsia: a paradigm shift focusing on systolic blood pressure. Obstet Gynecol. 2005;105(2):246-54.
-
676Cantwell R, Clutton-Brock T, Cooper G, Dawson A, Drife J, Garrod D, et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG . 2011;118 (Suppl 1):1-203.
-
677Meher S, Abalos E, Carroli G. Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database Syst Rev. 2005;19(4):CD003514.
-
678Dowswell T, Middleton P, Weeks A. Antenatal day care units versus hospital admission for women with complicated pregnancy. Cochrane Database of Syst Rev. 2009;(4):CD001803.
-
679Koopmans CM, Bijlenga D, Groen H, Vijgen SMC, Aarnoudse JG. Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374(9694):979–88.
-
680Broekhuijsen K, van Baaren GJ, van Pampus MG, Ganzevoort W, Sikkema JM, Woiski MD, et al. Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. Lancet. 2015;385(9986):2492-501.
-
681Ronsmans C, Campbell O. Quantifying the fall in mortality associated with interventions related to hypertensive diseases of pregnancy. BMC Public Health. 2011;11(Suppl 3):S8.
-
682Peraçoli JC, Borges VTM, Ramos JG, Cavalli RC, Costa SHAM, Oliveira LG, et al. Pre-eclampsia/Eclampsia. Rev Bras Ginecol Obstet. 2019;41(5):318-32.
-
683Duley L, Henderson-Smart DJ, Meher S. Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev. 2006;(3):CD001449.
-
684Centers for disease control and prevention. Postmarketing surveillance for angiotensin-converting enzyme inhibitor use during the first trimester of pregnancy – United States, Canada and Israel, 1987-1995. JAMA. 1997; 277(15):1193-4.
-
685Abalos E, Duley L, Steyn DW. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database of Syst Rev. 2014;6(2): CD002252.
-
686Magee LA, von Dadelszen P, Rey E, Ross S, Asztalos E, Murphy KE, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372(5):407-17.
-
687Magee LA, von Dadelszen P, Singer J, Lee T, Rey E, Ross S, et al. The CHIPS randomized controlled trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood pressure? Hypertension. 2016;68(5):1153-9.
-
688Butalia S, Audibert F, Côté AM, Firoz T, Logan AG, Magee LA, et al. Hypertension Canada’s 2018. Guidelines for the Management of Hypertension in Pregnancy. Can J Cardiol. 2018;34(5):526-31.
-
689Easterling T, Mundle S, Bracken H, Parvekar S, Mool S, Magee LA, et al. Oral antihypertensive regimens (nifedipine retard, labetalol, and methyldopa) for management of severe hypertension in pregnancy: an open-label, randomised controlled trial. Lancet 2019;394(10203):1011-21.
-
690Sass N, Itamoto CH, Silva MP, Torloni MR, Atallah NA. Does sodium nitroprusside kill babies? A systematic review. Sao Paulo Med J. 2007;125:108-11.
-
691Townsend R, O’Brien P, Khalil A. Current best practice in the management of hypertensive disorders in pregnancy. Integr Blood Press Control. 2016:9,79-94.
-
692Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-[Internet] [Cited in 2019 May 12] . Available from: https://www.ncbi.nlm.nih.gov/books/NBK501922/ .
» https://www.ncbi.nlm.nih.gov/books/NBK501922/ -
693Regit-Azgrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018; 39(34):3165–241.
-
694Halpern DG, Weinberg CR, Pinnelas R, Mehta-Lee S, Economy KE, Valente AM. Use of Medication for Cardiovascular Disease During Pregnancy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(4):457-76.
-
695Noronha Neto C C, Maia SSB, Katz L, Coutinho IC, Souza AR, Amorim MM. Clonidine versus Captopril for Severe Postpartum Hypertension: A Randomized Controlled Trial. Plos One. 2017;12(1):e0168124.
-
696Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366(9499):1797–803.
-
697Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
-
698Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, et al. Long-Term Cardiovascular Risk in Women With Hypertension During Pregnancy. J Am Coll Cardiol. 2019;74(22):2743-54.
-
699Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359(8):800-9.
-
700Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113(3 Pt 1):475-82.
-
701McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and prehypertension among adolescents. J Pediatr. 2007;150(6):640-4.
-
702Brian KK, Elena K, Margaret DC, Yachim O, David SF, Cynthia LO. Prevalence of and trends in dyslipidemia and blood pressure among us child and adolescents 1999-2012. Jama Pediatr. 2015: 169(3):272-9.
-
703Bloch VK, Klein CH, Szklo M, Kuschnir MCC et al. Prevalências de hipertensão arterial e obesidade Brazileiros. Rev. Saúde Pública. 2016: 50(supl 1)1-13.
-
704Brady TM, Redwine KM, Flynn JT; American Society of Pediatric Nephrology. Screening blood pressure measurement in children: are we saving lives? Pediatr Nephrol. 2014;29(6):947-50.
-
705Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al; Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3):e20171904.
-
706National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;98(4 Pt 1):649–58.
-
707National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics. 2004;114(2):555-76.
-
708Kulaga Z, Litwin M, Grajda A, Kułaga K, Gurzkowska B, Gó´zd´zM, et al. Oscillometric blood pressure percentiles for Polish normal-weight school-aged children and adolescents. J Hyper-tens. 2012;30(10):1942-54.
-
709Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS. Blood pressure percentiles by age and height from nonover-weight children and adolescents in Germany. Pediatrics.2011;127(4):e978-88.
-
710Jardim TV, Rosner B, Bloch KV, Kuschnir MC, Szklo M, Jardim PC. Blood pressure reference values for Brazilian adolescents: data from the Study of Cardiovascular Risk in Adolescents (ERICA Study). J Pediatr. 2020;96(2):168-76.
-
711Dionne JM, Abitbol CL, Flynn JT. Hypertension in infancy: diagnosis, management and outcome [published correction appears in Pediatr Nephrol. 2012;27(1):159-60]. Pediatr Nephrol. 2012;27(1):17–32.
-
712Report of the second task force on blood pressure control in children–1987. Task force on blood pressure control in children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics. 1987;79(1):1–25.
-
713Guimarães IC, Almeida AM, Santos AS, Barbosa DB, Guimarães AC. Blood pressure: effect of body mass index and of waist circumference on adolescents. Arq Bras Cardiol. 2008;90(6):426-32.
-
714Daniels Sr. Coronary risk factors in children. In: Moss & Adams. Heart disease in infants, children and adolescents. Philadelphia: Williams & Wilkins; 2013. p. 1514-48.
-
715Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al; European Society of Hypertension. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens. 2009;27(9):1719-42.
-
716Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, Zachariah JP, Urbina EM Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension. 2014 ;63(5):1116-35.
-
717Hansen HS, Hyldebrandt N, Froberg K, Nielsen JR. Blood pressure and physical fitness in a population of children—the Odense Schoolchild Study. J Hum Hypertens. 1990;4(6):615-20.
-
718McCambridge TM, Benjamin HJ, Brenner JS, Cappetta CT, Demorest RA, Gregory AJ, et al; Council on Sports Medicine and Fitness. Athletic participation by children and adolescents who have systemic hypertension Pediatrics. 2010;125(6):1287-94.
-
719Rios-Leyvraz M, Bloetzer C, Chatelan A, Bochud M, Burnier M. Sodium intake and blood pressure in children with clinical conditions: A systematic review with meta-analysis. J Clin Hypertens (Greenwich). 2019 Jan;21(1):118-126.
-
720Bricarello P L, Poltronieri F, Fernandes R, Retondario A, Morais EBST, Vasconcelos FAG. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin Nutr ESPEN. 2018 Dec;28:1-11.
-
721Miller JZ, Wienberger MH, Christian JC. Blood pressure response to potassium supplement in normotensive adults and children. Hypertension. 1987;10(4):437-42.
-
722Chaturvedi S, Lipszyc DH, Licht C, Craig JC, Parekh P. Pharmacological interventions for hypertension in children. Evid Based Child Health. 2014;9(3):498-580.
-
723Prichard BN, Cruickshank JM, Graham BR. Beta-adrenergic blocking drugs in the treatment of hypertension. Blood Press. 2001;10(5-6):366-86.
-
724Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD. Pregnancy outcome following exposure to angiotensin converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension. 2012;60(2):444-50.
-
725Ferguson MA, Flynn JT. Rational use of antihypertensive medications in children. Pediatr Nephrol. 2014;29(6):979-88.
-
726Blowey DL. Update on the pharmacologic treatment of hypertension in pediatrics. J Clin Hypertens (Greenwich). 2012;14(6):383-7.
-
727Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, et al; Hypertension Canada. Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2018 May;34(5):506-25.
-
728. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887-920.
-
729Wu HP, Yang WC, Wu YK, Zhao L, Chen CY, Fu YC. Clinical significance of blood pressure ratios in hypertensive crisis in children. Arch Dis Child. 2012; 97(3):200–5.
-
730Chandar J, Zilleruelo G. Hypertensive crisis in children. Pediatr Nephrol. 2012: 27(5):741-51.
-
731Yang WC, Zhao LL, Chen CY, Wu YK, Chang YJ, Wu HP. First-attack pediatric hypertensive crisis presenting to the pediatric emergency department. BMC Pediatrics. 2012; 12:200.
-
732. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153(2):154-83.
-
733Bortolotto LA, Silveira JV, Vilela-Martin JF. Crises Hipertensivas: Definindo a gravidade e o tratamento. Rev Soc Cardiol Estado de São Paulo. 2018; 28 (3):254-9.
-
734Martin JFV, Ribeiro JM. Urgências e Emergências Hipertensivas. In: Moreira MC, Montenegro ST, Paola AAV, eds. Livro Texto da Sociedade Brazileira de Cardiologia. 2 ed. Barueri (SP): Manole; 2015. P.922-30.
-
735Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83(2):131-6; 125-30.
-
736Pinna G, Pascale C, Fornengo P, Arras S, Piras C, Panzarasa P, et al. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PLoS One. 2014;9(4):e93542.
-
737Vilela-Martin JF, Vaz-de-Melo RO, Kuniyoshi CH, Abdo AN, Yugar-Toledo JC. Hypertensive crisis: clinical-epidemiological profile. Hypertens Res. 2011;34(3):367-71.
-
738Pierin AMG, Flórido CF, Santos JD. Hypertensive crisis: clinical characteristics of patients with hypertensive urgency, emergency and pseudocrisis at a public emergency department. Einstein (Sao Paulo). 2019;17(4):eAO4685.
-
739Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci.1974;268(6):336–45.
-
740Velasco I, Cuadrado L, Fontana A, Reijaili WA, Balbi AL, Barretti P, Franco RJS. Cuadro clínico y evolución de 77 pacientes con hipertensión arterial maligna: comparación de dos épocas y de diferentes niveles de creatinina. Nefrologia. 1993;13 (Suppl 5):8-13.
-
741Almeida FA, Stella RC, Voos A, Ajzen H, Ribeiro AB. Malignant hypertension: a syndrome associated with low plasma kininogen and kinin potentiating factor. Hypertension. 1981;3(6 Pt 2):II-46-9.
-
742Ault MJ, Ellrodt AG. Pathophysiologic events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985;3(6 Suppl):10–5.
-
743Strandgaard S, Paulson O. Cerebral autoregulation. Stroke. 1984;15(3):413–6.
-
744Martin JFV, Kuniyoshi CH, Andrade LG, Yugar-Toledo JC, Loureiro AC, Cipullo JP. Fatores Preditores de Mortalidade em Pacientes com Crise Hipertensiva. Arq Bras Cardiol. 2007;89(Supl 1): 201.
-
745Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996; 276(16):1328-31.
-
746CREMESP elabora parecer sobre uso de nifedipina. 2004. [citado 2020 Jul 15]. Disponível em: https://www.cremesp.org.br/?siteAcao=Jornal&id=323 .
» https://www.cremesp.org.br/?siteAcao=Jornal&id=323 -
747Vilela-Martin JF, Yugar-Toledo JF, Rodrigues MC, Barroso WS, Bronze L, Torres F, et al. Luso-Brazilian Position Statement on Hypertensive Emergencies – 2020. Arq Bras Cardiol. 2020;114(4):736-51.
-
748van den Born BH, Lip GYH, Brguljan-Hitij J, Cremer A, Segura J, Morales E, et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur Heart J Cardiovasc Pharmacother. 2019;5(1):37-46.
-
749O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388(10046):761–75.
-
750Truelsen T, Heuschmann PU, Bonita R, Arjundas G, Dalal P, Damasceno A, et al. Standard method for developing stroke registers in low-income and middle-income countries: experiences from a feasibility study of a stepwise approach to stroke surveillance (STEPS Stroke). Lancet Neurol. 2007;6(2):134-9.
-
751Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306.
-
752Hemphill, J.C., 3rd, et al., Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2015. 46(7): 2032-60.
-
753Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2): 119–77.
-
754Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association for Clinical Chemistry. 2014 AHA/ACC Guideline for the management of patients with non–ST-elevation acute coronary syndromes. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-228.
-
755Gandhi SK, Powers JC, Nomeir AM, Fowle K, Kitzman DW, Rankin KM, et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med. 2001;344(1):17-22.
-
756Kumar R, Gandhi SK, Little WC. Acute heart failure with preserved systolic function. Crit Care Med. 2008;36(1 Suppl):pS52-6.
-
757Comitê Coordenador da Diretriz de Insuficiência Cardíaca da Sociedade Brazileira de Cardiologia; Rohde LEP, Montera MW, Bocchi EA, Albuquerque DC, Clausell NO, Rassi S, et al. Diretriz Brazileira de Insuficiência Cardíaca Crônica e Aguda. Arq Bras Cardiol. 2018;111(3):436-539.
-
758Bossone E, La Bounty TM, Eagle KA. Acute aortic syndromes: Diagnosis and management, an update. Eur Heart J. 2018;39(9):739−49.
-
759Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Dis. 2003;5(4):253-71.
-
760Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Dis. 2003;5(3):187-201.
-
761Lester SJ, Baggott M, Welm S, et al. Cardiovascular effects of 3, 4-methylenedioxy-methamphetamine. A double-blind, placebo-controlled trial. Ann Intern Med. 2000;133(12):969–73.
-
762Gahlinger PM. Club drugs: MDMA, gamma-hydroxybutyrate (GHB), Rohypnol, and ketamine. Am Fam Physician. 2004;69(11):2619-27.
-
763Lange RA, Ciggarroa RG, Flores ED, McBride W, Kim AS, Wells PJ, et al. Potentiation of cocaine induced coronary vasoconstriction by beta adrenergic blockade. Ann Intern Med. 1990;112(12):897–903.
-
764Tuncel M, Wang Z, Arbique D, Fadel PJ, Victor RG, Vongpatanasin W. Mechanism of the blood pressure-raising effect of cocaine in humans. Circulation. 2002;105(9):1054-9.
-
765Sofuoglu M, Brown S, Babb DA, Pentel PR, Hatsukami DK. Carvedilol affects the physiological and behavioral response to smoked cocaine in humans. Drug Alcohol Depend. 2000; 60(1):69-76.
-
766Sordo L, Indave BI, Barrio G, Degenhardt L, de la Fuente L, Bravo MJ. Cocaine use and risk of stroke: a systematic review. Drug Alcohol Depend. 2014;142:1-13.
-
767Wilson LD, Jeromin J, Garvey L, Dorbandt A. Cocaine, ethanol, and cocaethylene cardiotoxicity in an animal model of cocaine and ethanol abuse. Acad Emerg Med. 2001;8(3):211–22.
-
768Mehta MC, Jain AC, Billie M. Effects of cocaine and alcohol alone and in combination on cardiovascular performance in dogs. Am J Med Sci. 2002;324(2):76–83.
-
769Wilkerson RD. Cardiovascular effects of cocaine: enhancement by yohimbine and atropine. J Pharmacol Exp Ther. 1989;248(1):57–61.
-
770Perez-Reyes M, Jeffcoat AR. Ethanol/cocaine interactions: cocaine and cocaethylene plasma concentrations and their relationship to subjective and cardiovascular effects. Life Sci. 1992;51(8):553–63.
-
771Melchert RB, Eselin JA, O’Dell JF, Welder AA. Effects of nitrendipine on cocaine induced toxicity evaluated in primary myocardial cell cultures. J Pharmaceut Sci. 1991;80(7):700–4.
-
772Bortolotto LA. Hipertensão acelerada-maligna. Rev Bras Hipertens. 2014;21(4):203-8.
-
773Ahmed ME, Walker JM, Beevers DG, Beevers M. Lack of difference between malignant and accelerated hypertension. Br Med J (Clin Res Ed). 1986;292(6515):235-7.
-
774Kincaid-Smith P, McMichael J, Murphy EA. The clinical course and pathology of hypertension with papilloedema (malignant hypertension). Q J Med. 1958;27(105):117-53.
-
775Clough C, Beevers D, Beevers M. The survival of malignant hypertension in blacks, whites and Asians in Britain. J Hum Hypertens. 1990;4(2):94-6.
-
776Lip G, Beevers M, Beevers D. Complications and survival of 315 patients with malignant-phase hypertension. J Hypertens. 1995;13(8):915-24.
-
777Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, et al. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30(8):463-6.
-
778Ma H, Jiang M, Fu Z, Wang Z, Shen P, Shi H, et al. Clinical value of multiorgan damage in hypertensive crises: A prospective follow-up study. J Clin Hypertens. (Greenwich). 2020;22(5):914-23.
-
779Lip GY, Beevers M, Dodson PM, Beevers DG. Severe hypertension with lone bilateral papilloedema: a variant of malignant hypertension. Blood Press. 1995;4(6):339-42.
-
780Amraoui F, van Montfrans GA, van den Born BJ. Value of retinal examination in hypertensive encephalopathy. J Hum Hypertens. 2010;24(4):274-9.
-
781World Health Organization. (WHO). World Report on Ageing and Health 2015. [Cited in 2020 Feb 10]. Available from: http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 .
» http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 -
782United Nations. Department of Economic and Social Affairs Population Division. World Population Ageing 2015. [Cited in 2019 Feb 10] Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf .
» http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf -
783Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity andimplications for health care, research, and medical education: a cross-sectional study. The Lancet. 2012; 380 (9836): 37-43.
-
784Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing 2017; 46 (6): 882–8.
-
785Nunes BP, Batista SRR, Andrade FB, Souza Junior PRB, Lima-Costa MF, Facchini LA. Multimorbidity: The Brazilian Longitudinal Study of Aging (ELSI-Brazil). Rev Saude Publica. 2018;52(Suppl 2):10s.
-
786Peters R, Beckett N, McCormack T, Fagard R, Fletcher A, Bulpitt C. Treating hypertension in the very elderly—benefits, risks, and future directions, a focus on the hypertension in the very elderly trial. Eur Heart J. 2014; 35 (26):1712-8.
-
787Iadecola C. Hypertension and Dementia. Hypertension. 2014; 64 (1): 3-5.
-
788Costa Filho AM, Mambrini JVM, Malta DC, Lima-Costa MF, Peixoto SV. Contribution of chronic diseases to the prevalence of disability in basic and instrumental activities of daily living in elderly Brazilians: the National Health Survey (2013). Cad. Saúde Pública (Online) 2018; 34(1):e00204016.
-
789Kelly R, Hayward C, Avolio A, O’Rourke M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation 1989; 80 (6): 1652–9.
-
790Franklin SS, Gustin Wt, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308-15.
-
791Pearson JD, Morrell CH, Brant LJ, Landis PK, Fleg JL. Age-associated changes in blood pressure in a longitudinal study of healthy men and women. J Gerontol A Biol Sci Med Sci. 1997;52(3):M177-83.
-
792Lakatta EG. Central arterial aging and the epidemic of systolic hypertension and atherosclerosis. J Am Soc Hypertens. 2007;1(5):302-40.
-
793O’Rourke MF, Nichols WW. Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension. 2005;45(4):652-8.
-
794Niiranen TJ, Lyass A, Larson MG, Hamburg NM, Benjamin EJ, Mitchell GF, et al. Prevalence, Correlates, and Prognosis of Healthy Vascular Aging in a Western Community-Dwelling Cohort: The Framingham Heart Study. Hypertension. 2017;70(2):267-74.
-
795Freitas EGB, Souza DF, Ferreira-Filho SR. Probability of At Least One High Arterial Blood Pressure Measurement in Elderly Patients with Healthy Vascular Aging in Two Years of Follow-Up. Kidney Blood Press Res. 2018;43(6):1765-71.
-
796de Mendonca GS, de Souza DF, de Alvarenga Cunha Brunelli AC, de Oliveira Peres CI, Freitas EGB, Lacerda GN, et al. Arterial stiffness in elderly patients with normotension and hypertension in Brazil. J Clin Hypertens (Greenwich). 2018;20(9):1285-93.
-
797Benetos A, Gautier S, Labat C, et al. Mortality and Cardiovascular Events Are Best Predicted by Low Central/Peripheral Pulse Pressure Amplification But Not by High Blood Pressure Levels in Elderly Nursing Home Subjects: the PARTAGE (Predictive Values of Blood Pressure and Arterial Stiffness in Institutionalized Very Aged Population) study. J Am Coll Cardiol. 2012;60 (16):1503-11.
-
798Rimoldi SF, Scherrer U, Messerli FH. Secondary arterial hypertension: when, who, and how to screen? Eur Heart J. 2014;35(19):1245-54.
-
799Quinn TJ, McArthur K, Ellis G, Stott DJ. Functional assessment in older people. BMJ. 2011;343:d4681.
-
800Benetos A, Petrovic M, Strandberg T. Hypertension Management in Older and Frail Older Patients. Circ Res. 2019;124(7):1045-60.
-
801Campana EMG; Freitas EV, Brandão AA et al. Hipertensão Arterial no Idoso. In: Freitas EV, Py L, eds. Tratado de Geriatria e Gerontologia. Rio de Janeiro: GEN. 2016;p 507-21.
-
802Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-98.
-
803Corrao G, Rea F, Monzio Compagnoni M, Merlino L, Mancia G. Protective effects of antihypertensive treatment in patients aged 85 years or older. J Hypertens. 2017;35(7):1432-1.
-
804Hansson L, Lithell H, Skoog I, Baro F, Banki CM, Carbonin PU, et al. Study on COgnition and Prognosis in the Elderly (SCOPE). Blood Press; 1999; 8(3):177-83.
-
805Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683–9.
-
806White WB, Wakefield DB, Moscufo N, et al. Effects of Intensive Versus Standard Ambulatory Blood Pressure Control on Cerebrovascular Outcomes in Older People (INFINITY). Circulation. 2019;140(20):1626–35.
-
807Feitosa-Filho GS, Peixoto JM, Pinheiro JES, et al. Updated Geriatric Cardiology Guidelines of the Brazilian Society of Cardiology - 2019. Arq Bras Cardiol. 2019;112(5):649-705.
-
808Butrous H, Hummel SL. Heart Failure in Older Adults. Can J Cardiol. 2016;32(9):1140-7.
-
809Stortecky S, Schoenenberger AW, Moser A, Kalesan B, Juni P, Carrel T, et al. Evaluation of multidimensional geriatric assessment as a predictor of mortality and cardiovascular events after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2012;5(5):489-96.
-
810Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group [published correction appears in JAMA 1998 Jun 24;279(24):1954]. JAMA. 1998;279(11):839–46.
-
811Mente A, O’Donnell MJ, Rangarajan S, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371(7):601-11.
-
812Bangalore S, Messerli FH, Kostis JB, Pepine CJ. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol. 2007;50(7):563-72.
-
813Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2017;1(1):CD002003.
-
814Finks SW, Rumbak MJ, Self TH. Treating Hypertension in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2020;382(4):353-63.
-
815Isik AT, Soysal P, Stubbs B. Cardiovascular Outcomes of Cholinesterase Inhibitors in Individuals with Dementia: A Meta-Analysis and Systematic Review. J Am Geriatr Soc. 2018;66(9):1805-11.
-
816Kahlaee HR, Latt MD, Schneider CR. Association Between Chronic or Acute Use of Antihypertensive Class of Medications and Falls in Older Adults. A Systematic Review and Meta-Analysis. Am J Hypertens. 2018;31(4):467-79.
-
817Ang HT, Lim KK, Kwan YH, Há YC, Lim JY. A Systematic Review and Meta-Analyses of the Association Between Anti-Hypertensive Classes and the Risk of Falls Among Older Adults. Drugs Aging. 2018;35(7):625-35.
-
818Mühlbauer V, Dallmeier D, Brefka S, Bollig C, Voigt-Radloff S, Denkinger M: The pharmacological treatment of arterial hypertension in frail, older patients— a systematic review. Dtsch Arztebl Int 2019; 116: 23–30.
-
819Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406.
-
820Delgado J, Masoli JAH, Bowman K, et al. Outcomes of Treated Hypertension at Age 80 and Older: Cohort Analysis of 79,376 Individuals. J Am Geriatr Soc. 2017;65(5):995–1003.
-
821Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality [published online ahead of print, 2020 Mar 5]. Age Ageing. 2020;afaa028.
-
822Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE Study. JAMA Intern Med. 2015;175(6):989–995.
-
823Wu C, Smit E, Peralta CA, Sarathy H, Odden MC. Functional Status Modifies the Association of Blood Pressure with Death in Elders: Health and Retirement Study. J Am Geriatr Soc. 2017;65(7):1482–1489.
-
824Soobiah C, Daly C, Blondal E, Ewusie J, Ho J, Elliott MJ, Yue R, Holroyd-Leduc J, Liu B, Marr S, Basran J, Tricco AC, Hamid J, Straus SE. An evaluation of the comparative effectiveness of geriatrician-led comprehensive geriatric assessment for improving patient and healthcare system outcomes for older adults: a protocol for a systematic review and network meta-analysis. Syst Rev. 2017 Mar 24;6(1):65.
-
825Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495.
-
826Rockwood K, Song X, Mitnitski A: Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. CMAJ 2011; 183: E487–94.
-
827Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668-1676.
-
828Studenski S, Perera S, Patel K, Rosano C, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50.
-
829Odden MC, Moran AE, Coxson PG, Peralta CA, Goldman L, Bibbins-Domingo K. Gait Speed as a Guide for Blood Pressure Targets in Older Adults: A Modeling Study. J Am Geriatr Soc. 2016;64(5):1015–1023.
-
830Rodrigues, M.K., Nunes Rodrigues, I., Vasconcelos Gomes da Silva, D.J. et al. Clinical Frailty Scale: Translation and Cultural Adaptation Into the Brazilian Portuguese Language. J Frailty Aging 2020: in press. Published online Feb 14, 2020 7.
-
831Darvall JN, Greentree K, Braat MS, Story DA, Lim WK. Contributors to frailty in critical illness: Multi-dimensional analysis of the Clinical Frailty Scale. J Crit Care. 2019 Aug;52:193-9.
-
832Chong E, Ho E, Baldevarona-Llego J, Chan M, Wu L, Tay L. Frailty and Risk of Adverse Outcomes in Hospitalized Older Adults: A Comparison of Different Frailty Measures. J Am Med Dir Assoc. 2017 Jul;18(7):638.e7-.e11.
-
833Atkins JL, Delgado J, Pilling LC, et al. Impact of Low Cardiovascular Risk Profiles on Geriatric Outcomes: Evidence From 421,000 Participants in Two Cohorts. J Gerontol A Biol Sci Med Sci. 2019;74(3):350–357.
-
834Nadruz W Jr, Kitzman D, Windham BG, et al. Cardiovascular Dysfunction and Frailty Among Older Adults in the Community: The ARIC Study. J Gerontol A Biol Sci Med Sci. 2017;72(7):958–964.
-
835Aprahamian, I, Sassaki, E, dos Santos, MF, et al. Hypertension and frailty in older adults. J Clin Hypertens. 2018; 20: 186– 192.
-
836Ravindrarajah R, Hazra NC, Hamada S, et al. Systolic Blood Pressure Trajectory, Frailty, and All-Cause Mortality >80 Years of Age: Cohort Study Using Electronic Health Records. Circulation. 2017;135(24):2357–68.
-
837Gulla C, Flo E, Kjome RL, Husebo BS. Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. J Geriatr Cardiol. 2018;15(4):275–283.
-
838Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78. Published 2015 Apr 9.
-
839Russo, G., Liguori, I., Aran, L. et al. Impact of SPRINT results on hypertension guidelines: implications for “frail” elderly patients. J Hum Hypertens 32, 633–638 (2018). https://doi.org/10.1038/s41371-018-0086-6
» https://doi.org/10.1038/s41371-018-0086-6 -
840Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–517.
-
841Abell JG, Kivimäki M, Dugravot A, et al. Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertension. Eur Heart J. 2018;39(33):3119–3125.
-
842Gottesman RF, Schneider AL, Albert M, Alonso A, Bandeen-Roche K, Coker L, Coresh J, Knopman D, Power MC, Rawlings A, Sharrett AR, Wruck LM, Mosley TH. Midlife hypertension and 20-year cognitive change: the atherosclerosis risk in communities neurocognitive study. JAMA Neurol. 2014;71:1218–1227.
-
843Iadecola C, Gottesman RF. Neurovascular and Cognitive Dysfunction in Hypertension. Circ Res. 2019;124(7):1025–1044.
-
844Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–2263.
-
845Flores LM, Mengue SS. Drug use by the elderly in Southern Brazil. Rev Saúde Pública. 2005; 39(6): 924-9.
-
846Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract. 2005;17(4):123–132.
-
847Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23.
-
848Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
-
849Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of Discontinuation of Antihypertensive Treatment in Elderly People on Cognitive Functioning--the DANTE Study Leiden: A Randomized Clinical Trial [published correction appears in JAMA Intern Med. 2016 Feb;176(2):284]. JAMA Intern Med. 2015;175(10):1622–1630.
-
850Luymes CH, Poortvliet RKE, van Geloven N, et al. Deprescribing preventive cardiovascular medication in patients with predicted low cardiovascular disease risk in general practice - the ECSTATIC study: a cluster randomised non-inferiority trial. BMC Med. 2018;16(1):5.
-
851Gibbons CH, Schmidt P, Biaggioni I, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol. 2017;264(8):1567–1582.
-
852Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS. Orthostatic hypotension in older adults. The Cardiovascular Health Study. Hypertension 1992;19:508.
-
853Jansen RW, Lipsitz LA. Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med 1995;122:286.
-
854Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study [published correction appears in J Am Geriatr Soc. 2011 May;59(5):960]. J Am Geriatr Soc. 2011;59(3):383–389.
-
855Margolis KL, Palermo L, Vittinghoff E, et al. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med. 2014;29(12):1599–1606.
-
856Juraschek SP, Taylor AA, Wright JT Jr, et al. Orthostatic Hypotension, Cardiovascular Outcomes, and Adverse Events: Results From SPRINT. Hypertension. 2020;75(3):660–667
-
857Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-312.
-
858Charles L, Triscott J, Dobbs B. Secondary Hypertension: Discovering the Underlying Cause. Am Fam Physician. 2017;96(7):453-61.
-
859Hirsch JS, Hong S. The Demystification of Secondary Hypertension: Diagnostic Strategies and Treatment Algorithms. Current Treatment Options in Cardiovascular Medicine. 2019;21(12):90.
-
860Siddiqui MA, Mittal PK, Little BP, Miller FH, Akduman EI, Ali K, et al. Secondary Hypertension and Complications: Diagnosis and Role of Imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 2019;39(4):1036-55.
-
861Cingolani OH. Cardiovascular Risks and Organ Damage in Secondary Hypertension. Endocrinol Metab Clin North Am. 2019;48(4):657-66.
-
862. Summary of Recommendation Statements. Kidney Int Suppl (2011). 2013;3(1):5-14.
-
863Pugh D, Gallacher PJ, Dhaun N. Management of Hypertension in Chronic Kidney Disease. Drugs. 2019;79(4):365-79.
-
864Sinha AD, Agarwal R. Clinical Pharmacology of Antihypertensive Therapy for the Treatment of Hypertension in CKD. Clinical Journal of the American Society of Nephrology. 2019;14(5):757-64.
-
865. Chapter 2: Definition, identification, and prediction of CKD progression. Kidney Int Suppl (2011). 2013;3(1):63-72.
-
866Herrmann SM, Textor SC. Current Concepts in the Treatment of Renovascular Hypertension. Am J Hypertens. 2018;31(2):139-49.
-
867Aboyans V, Ricco JB, Bartelink MEL, Bjorck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763-816.
-
868Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(13):1425-43.
-
869Parikh SA, Shishehbor MH, Gray BH, White CJ, Jaff MR. SCAI expert consensus statement for renal artery stenting appropriate use. Catheter Cardiovasc Interv. 2014;84(7):1163-71.
-
870Harvin HJ, Verma N, Nikolaidis P, Hanley M, Dogra VS, Goldfarb S, et al. ACR Appropriateness Criteria((R)) Renovascular Hypertension. Journal of the American College of Radiology : JACR. 2017;14(11s):S540-s9.
-
871Rountas C, Vlychou M, Vassiou K, Liakopoulos V, Kapsalaki E, Koukoulis G, et al. Imaging Modalities for Renal Artery Stenosis in Suspected Renovascular Hypertension: Prospective Intraindividual Comparison of Color Doppler US, CT Angiography, GD-Enhanced MR Angiography, and Digital Substraction Angiography. Renal Failure. 2007;29(3):295-302.
-
872Zeller T, Krankenberg H, Erglis A, Blessing E, Fuss T, Scheinert D, et al. A randomized, multi-center, prospective study comparing best medical treatment versus best medical treatment plus renal artery stenting in patients with hemodynamically relevant atherosclerotic renal artery stenosis (RADAR) – one-year results of a pre-maturely terminated study. Trials. 2017;18(1):380.
-
873Raman G, Adam GP, Halladay CW, Langberg VN, Azodo IA, Balk EM. Comparative Effectiveness of Management Strategies for Renal Artery Stenosis: An Updated Systematic Review. Ann Intern Med. 2016;165(9):635-49.
-
874Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014;370(1):13-22.
-
875Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009;361(20):1953-62.
-
876Nicholson J, Alderman M, Pickering T, Teichman S, Sos T, Laragh J. CIGARETTE SMOKING AND RENOVASCULAR HYPERTENSION. The Lancet. 1983;322(8353):765-6.
-
877Piaggio D, Bracale U, Pecchia L, Di Taranto MD, Sodo M, Bracale UM. Endovascular Treatment versus Medical Therapy for Hypertensive Patients with Renal Artery Stenosis: An Updated Systematic Review. Annals of vascular surgery. 2019;61:445-54.
-
878Noory E, Sritharan K, Zeller T. To Stent or Not to Stent? Update on Revascularization for Atherosclerotic Renovascular Disease. Curr Hypertens Rep. 2016;18(6):45.
-
879Gornik HL, Persu A, Adlam D, Aparicio LS, Azizi M, Boulanger M, et al. First International Consensus on the diagnosis and management of fibromuscular dysplasia. Vascular medicine (London, England). 2019;24(2):164-89.
-
880Bolen MA, Brinza E, Renapurkar RD, Kim ESH, Gornik HL. Screening CT Angiography of the Aorta, Visceral Branch Vessels, and Pelvic Arteries in Fibromuscular Dysplasia. JACC Cardiovascular imaging. 2017;10(5):554-61.
-
881Weinberg I, Gu X, Giri J, Kim SE, Bacharach MJ, Gray BH, et al. Anti-platelet and anti-hypertension medication use in patients with fibromuscular dysplasia: Results from the United States Registry for Fibromuscular Dysplasia. Vascular medicine (London, England). 2015;20(5):447-53.
-
882Rao PS. Coarctation of the aorta. Seminars in nephrology. 1995;15(2):87-105.
-
883Godart F. [Management of aortic coarctation at the adult age]. Archives des maladies du coeur et des vaisseaux. 2007;100(5):478-83.
-
884Dijkema EJ, Leiner T, Grotenhuis HB. Diagnosis, imaging and clinical management of aortic coarctation. Heart. 2017;103(15):1148-55.
-
885Torok RD, Campbell MJ, Fleming GA, Hill KD. Coarctation of the aorta: Management from infancy to adulthood. World journal of cardiology. 2015;7(11):765-75.
-
886Martins JD, Zachariah J, Selamet Tierney ES, Truong U, Morris SA, Kutty S, et al. Impact of Treatment Modality on Vascular Function in Coarctation of the Aorta: The LOVE - COARCT Study. J Am Heart Assoc. 2019;8(7):e011536.
-
887Cangussú LR, Lopes MR, Barbosa RHdA. The importance of the early diagnosis of aorta coarctation. Revista da Associação Médica Brazileira. 2019;65:240-5.
-
888Gottlieb DJ, Punjabi NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA. 2020;323(14):1389-400.
-
889Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569-76.
-
890Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441-6.
-
891Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB. Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med. 1985;103(2):190-5.
-
892Williams AJ, Houston D, Finberg S, Lam C, Kinney JL, Santiago S. Sleep apnea syndrome and essential hypertension. Am J Cardiol. 1985;55(8):1019-22.
-
893Sjostrom C, Lindberg E, Elmasry A, Hagg A, Svardsudd K, Janson C. Prevalence of sleep apnoea and snoring in hypertensive men: a population based study. Thorax. 2002;57(7):602-7.
-
894Drager LF, Genta PR, Pedrosa RP, Nerbass FB, Gonzaga CC, Krieger EM, et al. Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol. 2010;105(8):1135-9.
-
895Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011;58(5):811-7.
-
896Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378-84.
-
897Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307(20):2169-76.
-
898Drager LF, Bortolotto LA, Figueiredo AC, Silva BC, Krieger EM, Lorenzi-Filho G. Obstructive sleep apnea, hypertension, and their interaction on arterial stiffness and heart remodeling. Chest. 2007;131(5):1379-86.
-
899Drager LF, Bortolotto LA, Krieger EM, Lorenzi-Filho G. Additive effects of obstructive sleep apnea and hypertension on early markers of carotid atherosclerosis. Hypertension. 2009;53(1):64-9.
-
900Gus M, Goncalves SC, Martinez D, de Abreu Silva EO, Moreira LB, Fuchs SC, et al. Risk for Obstructive Sleep Apnea by Berlin Questionnaire, but not daytime sleepiness, is associated with resistant hypertension: a case-control study. Am J Hypertens. 2008;21(7):832-5.
-
901Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485-91.
-
902Margallo VS, Muxfeldt ES, Guimaraes GM, Salles GF. Diagnostic accuracy of the Berlin questionnaire in detecting obstructive sleep apnea in patients with resistant hypertension. J Hypertens. 2014;32(10):2030-6; discussion 7.
-
903Giampa SQC, Pedrosa RP, Gonzaga CC, Bertolami A, Amodeo C, Furlan SF, et al. Performance of NoSAS score versus Berlin questionnaire for screening obstructive sleep apnoea in patients with resistant hypertension. J Hum Hypertens. 2018;32(7):518-23.
-
904Genta-Pereira DC, Furlan SF, Omote DQ, Giorgi DMA, Bortolotto LA, Lorenzi-Filho G, et al. Nondipping Blood Pressure Patterns Predict Obstructive Sleep Apnea in Patients Undergoing Ambulatory Blood Pressure Monitoring. Hypertension. 2018;72(4):979-85.
-
905Drager LF, Lorenzi-Filho G, Cintra FD, Pedrosa RP, Bittencourt LRA, Poyares D, et al. Arq Bras Cardiol. 2018;111(2):290-340.
-
906Fatureto-Borges F, Lorenzi-Filho G, Drager LF. Effectiveness of continuous positive airway pressure in lowering blood pressure in patients with obstructive sleep apnea: a critical review of the literature. Integr Blood Press Control. 2016;9:43-7.
-
907Pedrosa RP, Drager LF, de Paula LKG, Amaro ACS, Bortolotto LA, Lorenzi-Filho G. Effects of OSA treatment on BP in patients with resistant hypertension: a randomized trial. Chest. 2013;144(5):1487-94.
-
908Martinez-Garcia MA, Capote F, Campos-Rodriguez F, Lloberes P, Diaz de Atauri MJ, Somoza M, et al. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013;310(22):2407-15.
-
909de Oliveira AC, Martinez D, Massierer D, Gus M, Goncalves SC, Ghizzoni F, et al. The antihypertensive effect of positive airway pressure on resistant hypertension of patients with obstructive sleep apnea: a randomized, double-blind, clinical trial. Am J Respir Crit Care Med. 2014;190(3):345-7.
-
910Castro-Grattoni AL, Torres G, Martínez-Alonso M, Barbé F, Turino C, Sánchez-de-la-Torre A, et al. Blood pressure response to CPAP treatment in subjects with obstructive sleep apnoea: the predictive value of 24-h ambulatory blood pressure monitoring. Eur Respir J. 2017;50(4).
-
911Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587-96.
-
912Pepin JL, Tamisier R, Barone-Rochette G, Launois SH, Levy P, Baguet JP. Comparison of continuous positive airway pressure and valsartan in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;182(7):954-60.
-
913Yumino D, Redolfi S, Ruttanaumpawan P, Su MC, Smith S, Newton GE, et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation. 2010;121(14):1598-605.
-
914Gaddam K, Pimenta E, Thomas SJ, Cofield SS, Oparil S, Harding SM, et al. Spironolactone reduces severity of obstructive sleep apnoea in patients with resistant hypertension: a preliminary report. J Hum Hypertens. 2010;24(8):532-7.
-
915Fiori CZ, Martinez D, Montanari CC, Lopez P, Camargo R, Sezera L, et al. Diuretic or sodium-restricted diet for obstructive sleep apnea-a randomized trial. Sleep. 2018;41(4).
-
916Conn JW. Primary aldosteronism. J Lab Clin Med. 1955;45(4):661-4.
-
917Calhoun DA. Is there an unrecognized epidemic of primary aldosteronism? Pro. Hypertension. 2007;50(3):447-53; discussion -53.
-
918Kline GA, Prebtani APH, Leung AA, Schiffrin EL. Primary aldosteronism: a common cause of resistant hypertension. CMAJ. 2017;189(22):E773-E8.
-
919Gordon RD, Ziesak MD, Tunny TJ, Stowasser M, Klemm SA. Evidence that primary aldosteronism may not be uncommon: 12% incidence among antihypertensive drug trial volunteers. Clin Exp Pharmacol Physiol. 1993;20(5):296-8.
-
920Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-916.
-
921Morera J, Reznik Y. MANAGEMENT OF ENDOCRINE DISEASE: The role of confirmatory tests in the diagnosis of primary aldosteronism. Eur J Endocrinol. 2018.
-
922Stowasser M, Ahmed AH, Cowley D, Wolley M, Guo Z, McWhinney BC, et al. Comparison of Seated With Recumbent Saline Suppression Testing for the Diagnosis of Primary Aldosteronism. The Journal of clinical endocrinology and metabolism. 2018;103(11):4113-24.
-
923Nanba K, Tamanaha T, Nakao K, Kawashima ST, Usui T, Tagami T, et al. Confirmatory testing in primary aldosteronism. The Journal of clinical endocrinology and metabolism. 2012;97(5):1688-94.
-
924Vilela LAP, Almeida MQ. Diagnosis and management of primary aldosteronism. Arch Endocrinol Metab. 2017;61(3):305-12.
-
925Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(1):51-9.
-
926van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. European journal of endocrinology. 2014;170(3):R109-19.
-
927Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Current problems in cancer. 2014;38(1):7-41.
-
928Lenders JW, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, et al. Biochemical diagnosis of pheochromocytoma: which test is best? Jama. 2002;287(11):1427-34.
-
929Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, Banerji MA. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-38.
-
930Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nature clinical practice Endocrinology & metabolism. 2007;3(2):92-102.
-
931Calabrò D, Allegri V, Fanti S, Ambrosini V. 68Ga-DOTANOC and 18F-DOPA PET/CT: a site-specific approach to the imaging of parangliomas of the head and neck and of the abdomen. European Journal of Nuclear Medicine and Molecular Imaging. 2019;46(6):1393-.
-
932Bravo EL. Pheochromocytoma: an approach to antihypertensive management. Annals of the New York Academy of Sciences. 2002;970:1-10.
-
933Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670-751.
-
934Jian WX, Jin J, Qin L, Fang WJ, Chen XR, Chen HB, et al. Relationship between thyroid-stimulating hormone and blood pressure in the middle-aged and elderly population. Singapore Med J. 2013;54(7):401-5.
-
935Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system: from theory to practice. J Clin Endocrinol Metab. 1994;78(5):1026-7.
-
936Frost L, Vestergaard P, Mosekilde L. Hyperthyroidism and risk of atrial fibrillation or flutter: a population-based study. Arch Intern Med. 2004;164(15):1675-8.
-
937Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016;26(10):1343-421.
-
938Richards AM, Espiner EA, Nicholls MG, Ikram H, Hamilton EJ, Maslowski AH. Hormone, calcium and blood pressure relationships in primary hyperparathyroidism. J Hypertens. 1988;6(9):747-52.
-
939Bilezikian JP. Primary Hyperparathyroidism. The Journal of clinical endocrinology and metabolism. 2018;103(11):3993-4004.
-
940Nieman LK, Biller BMK, Findling JW, Murad MH, Newell-Price J, Savage MO, et al. Treatment of Cushing’s Syndrome: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2015;100(8):2807-31.
-
941Fantin F, Giani A, Zoico E, Rossi AP, Mazzali G, Zamboni M. Weight Loss and Hypertension in Obese Subjects. Nutrients. 2019;11(7):1677.
-
942Saliba LJ, Maffett S. Hypertensive Heart Disease and Obesity: A Review. Heart Fail Clin. 2019;15(4):509-17.
-
943Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1-7.
-
944Ping Z, Pei X, Xia P, Chen Y, Guo R, Hu C, et al. Anthropometric indices as surrogates for estimating abdominal visceral and subcutaneous adipose tissue: A meta-analysis with 16,129 participants. Diabetes research and clinical practice. 2018;143:310-9.
-
945Nimptsch K, Konigorski S, Pischon T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019;92:61-70.
-
946Katznelson L, Atkinson J, Cook D, Ezzat S, Hamrahian A, Miller K. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Diagnosis and Treatment of Acromegaly-2011 Update. Endocrine Practice. 2011;17(Supplement 4):1-44.
-
947de Pablos-Velasco P, Venegas EM, Alvarez Escola C, Fajardo C, de Miguel P, Gonzalez N, et al. Diagnosis, treatment and follow-up of patients with acromegaly in a clinical practice setting in Spain: the ACROPRAXIS program Delphi survey. Pituitary. 2020;23(2):129-39.
-
948Silverstein JM, Roe ED, Munir KM, Fox JL, Emir B, Kouznetsova M, et al. Use of electronic health records to characteristize a rare disease in the U.S. : treatment comorbidities and follow-up trends among patients with a confirmed diagnosis of acromegaly.Endocr Pract. 2018;24(6):517-26.
-
949Brazil.Ministério daSaúde. Secretaria da Ciência e Tecnologia e Insumos Estratégicos .Portaria Conjunta n.2, de 07 de janeiro de 2019. Aprova o protocolo clínico e diretrizes terapêuticas da Acromeagalia. Brazilia;2019.
-
950Grossman E, Messerli FH. Drug-induced hypertension: an unappreciated cause of secondary hypertension. Am J Med. 2012;125(1):14-22.
-
951Diaconu CC, Dediu GN, Iancu MA. Drug-induced arterial hypertension - a frequently ignored cause of secondary hypertension: a review. Acta cardiologica. 2018:1-7.
-
952Versmissen J, Mirabito Colafella KM, Koolen SLW, Danser AHJ. Vascular Cardio-Oncology: Vascular Endothelial Growth Factor inhibitors and hypertension. Cardiovasc Res. 2019;115(5):904-14.
-
953Rizzoni D, De Ciuceis C, Porteri E, Agabiti-Rosei C, Agabiti-Rosei E. Use of Antihypertensive Drugs in Neoplastic Patients. High Blood Press Cardiovasc Prev. 2017;24(2):127-32.
-
954Carey RM, Calhoun DA, Bakris GL, Brook RB, Daugherty SL, Dennison-Himmelfarb CR et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018;72(5): e53-e90.
-
955Calhoun DA, Booth JN, Oparil S, Irvin MR, Shimbo D, Lackland DT et al. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63(3):451-8.
-
956Oliveras A, de la Sierra A. Resistant hypertension: patient characteristics, risk factors, co-morbidities and outcomes. J Hum Hypertens. 2014;28(4):213-7.
-
957Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S et al. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168(11):1159-64.
-
958Shimosawa T. Salt, the renin-angiotensin-aldosterone system and resistant hypertension. Hypertens Res. 2013;36(8):657-60.
-
959Calhoun DA. Refractory and Resistant Hypertension: Antihypertensive Treatment Failure versus Treatment Resistance. Korean Circ J. 2016;46(5):593-600.
-
960Eirin A, Textor SC, Lerman LO. Emerging concepts for patients with treatment-resistant hypertension. Trends Cardiovasc Med. 2016;26(8):700-6.
-
961Judd EK, Calhoun DA, Warnock DG. Pathophysiology and treatment of resistant hypertension: the role of aldosterone and amiloride-sensitive sodium channels. Semin Nephrol. 2014;34(5):532-9.
-
962Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA et al. Refractory hypertension: evidence of heightened sympathetic activity as a cause of antihypertensive treatment failure. Hypertension 2015;66(1):126-33.
-
963Barbaro NR, de Araújo TM, Tanus-Santos JE, Anhê GF, Fontana V, Moreno H. Vascular Damage in Resistant Hypertension: TNF-Alpha Inhibition Effects on Endothelial Cells. Biomed Res Int. 2015;1-8.
-
964Barbaro NR, Fontana V, Modolo R, Faria AP, Sabbatini AR, Fonseca FH, et al. Increased arterial stiffness in resistant hypertension is associated with inflammatory biomarkers. Blood Press.2015;24(1):7-13.
-
965Yugar-Toledo JC, Martin JF, Krieger JE, Pereira AC, Demacq C, Coelho OR, et al. Gene variation in resistant hypertension: multilocus analysis of the angiotensin 1-converting enzyme, angiotensinogen, and endothelial nitric oxide synthase genes. DNA Cell Biol. 2011;30(8):555-64.
-
966Aronow WS. Approaches for the management of resistant hypertension in 2020. Curr Hypertens Rep. 2020;22(1):3.
-
967Corrêa NB, de Faria AP, Ritter AM, Sabbatini AR, Almeida A, Brunelli V, et al. A practical approach for measurement of antihypertensive medication adherence in patients with resistant hypertension. J Am Soc Hypertens. 2016;10(6):510-6.
-
968Lazaridis AA, Sarafidis PA, Ruilope LM. Ambulatory Blood Pressure Monitoring in the Diagnosis, Prognosis, and Management of Resistant Hypertension: Still a Matter of our Resistance? Curr Hypertens Rep. 2015;17(10):78.
-
969Muxfeldt ES, Salles GF. How to use ambulatory blood pressure monitoring in resistant hypertension. Hypertens Res. 2013;36:385-9.
-
970Muxfeldt ES, Barros GS, Viegas BB, Carlos FO, Salles GF. Is home blood pressure monitoring useful in the management of patients with resistant hypertension? Am J Hypertens 2015; 28(2):190-9.
-
971Ozemek C, Tiwari S, Sabbahi A, Carbone S, Lavie CJ. Impact of therapeutic lifestyle changes in resistant hypertension. Prog Cardiovasc Dis. 2020;63(1):4-9.
-
972Acelajado MC, Hughes ZH, Oparil S, Calhoun DA. Treatment of resistant and refractory hypertension. Circ Res. 2019;124(7):1061-70.
-
973Williams B, MacDonald TM, Morant SV, Webb DJ, Sever P, McInnes GT, et al. British Hypertension Society Programme of Prevention And Treatment of Hypertension With Algorithm based Therapy (PATHWAY) Study Group. Endocrine and haemodynamic changes in resistant hypertension, and blood pressure responses to spironolactone or amiloride: the PATHWAY-2 mechanisms substudies. Lancet . Diabetes Endocrinol. 2018;6(6):464-75.
-
974Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Hygia Project Investigators. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2019 Oct 22/ehz754 Online ahead of print..
-
975Berra E, Azizi M, Capron A, Høieggen A, Rabbia F, Kjeldsen SE, et al. Evaluation of adherence should become an integral part of assessment of patients with apparently treatment-resistant hypertension. Hypertension. 2016;68(2):297-306.
-
976Kunz M, Lauder L, Ewen S, Böhm M, Mahfoud F. The current status of devices for the treatment of resistant hypertension. Am J Hypertens. 2020;33(1):10-8.
-
977Muxfeldt ES, Chedier B, Rodrigues CIS. Hipertensão resistente e refratária: duas faces de uma mesma doença? J Bras Nefrol . 2019; 41(2):266-74.
-
978Alessi A, Brandao AA, Coca A, Cordeiro AC, Nogueira AR, Diogenes de Magalhaes F, et al. First Brazilian position on resistant hypertension. Arq Bras Cardiol. 2012;99(1):576-85.
-
979Geldsetzer P, Manne-Goehler J, Marcus ME, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross- sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 2019 Aug 24;394(10199):652-62.
-
980Picon RV, Dias-da-Costa JS, Fuchs FD, Olinto MTA, Choudhry NK, Fuchs SC. Hypertension Management in Brazil: Usual Practice in Primary Care. A Meta-Analysis. Int J Hypertens. 2017; 2017: 1274168.
-
981World Health Organization (WHO). : Adherence to long-term therapies: evidence for action. Geneva;2003.
-
982Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. ABC Project Team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012; 73:691–705.
-
983Haynes RB, Sackett DL, Gibson ES, Taylor DW, Hackett BC, Roberts RS, et al. Improvement of medication compliance in uncontrolled hypertension. Lancet 1976;1(7972):1265-8.
-
984Gialamas A, Yelland LN, Ryan P, Willson K, Laurence CO, Bubner TK, et al. Does point-of-care testing lead to the same or better adherence to medication? A randomised controlled trial: the PoCT in General Practice Trial. Med J Austr. 2009;191:487-9.
-
985Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(9):882-7.
-
986Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski M. How to Screen for Non-Adherence to Antihypertensive Therapy. Curr Hypertens Rep. 2016;18(12):89.
-
987Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008; 10(5):348-54.
-
988Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care, 1986; 24(1):67-74.
-
989de Oliveira-Filho AD, Morisky DE, Neves SJF, Costa FA, de Lyra Junior DP. The 8-item Morisky Medication Adherence Scale: Validation of a Brazilian–Portuguese version in hypertensive adults. Res Social Adm Pharm. 2014; 10:554–561.
-
990Santa Helena ET, Nemes MIB, Eluf-Neto J. Desenvolvimento e validação de questionário multidimensional para medir não-adesão ao tratamento com medicamentos. Rev. Saúde Pública [online]. 2008; 42(4):764- 7.
-
991Burnier M, Egan BM. Adherence in Hypertension A Review of Prevalence, Risk Factors, Impact, and Management. Circ Res. 2019;124:1124-40.
-
992Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-97.
-
993Dhar L, Dantas J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol. 2017; 7(3):211-50.
-
994Abegaz TM, Shehab A, Gebreyohanne EA. Nonadherence to Antihypertensive Drugs: A Systematic Review Meta-Analysis. Medicine. 2017;96(4):e5641.
-
995Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010 Mar 17;(3):CD005182.
-
996van der Laan DM, Elders PJM, Boons CCLM, Beckeringh JJ, Nijpels G, Hugtenburg JG. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens. 2017;31(11):687-94.
-
997Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension. 2010;55(2):399–407.
-
998Santschi V, Chiolero A, Colosimo AL, Platt RW, Taff. P, Burnier M, Burnand B, Paradis G. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
-
999Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, Debusk RF. Nurse management for hypertension. A system approaches. Am J Hypertens. 2004;17(10):921–7.
-
1000Checchi KD, Huybrechts KF, Avorn J, Kesselheim AS. Electronic medication packaging devices and medication adherence: a systematic review. JAMA. 2014;312((12):1237–47.
-
1001Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J. Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension. 2013;62(2):218–25.
-
1002Christensen A, Osterberg LG, Hansen EH. Electronic monitoring of patient adherence to oral antihypertensive medical treatment: a systematic review. J Hypertens. 2009;27(8):1540–51.
-
1003Parati G, Torlasco C, Omboni S, Pellegrini D. Smartphone applications for hypertension management: a potential game-changer that needs more control. Curr Hypertens Rep. 2017;19(6):48.
-
1004Naik AD, Kallen MA, Walder A, Street RL Jr. Improving hypertension control in diabetes mellitus: the effects of collaborative and proactive health communication. Circulation. 2008;117(11):1361–8.
-
1005Conn VS, Ruppara TM, Enriqueza M, Cooper P. Medication adherence interventions that target subjects with adherence problems: Systematic Review and Meta-analysis. Res Social Adm Pharm. 2016; 12(2): 218–46.
-
1006VS, Ruppara TM. Medication Adherence Outcomes of 771 Intervention Trials: Systematic Review and Meta-Analysis. Prev Med. 2017; 99: 269–276.
-
1007Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet 2015; 385(9967): 540–8.
-
1008Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Merz NB, et al. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020;5(3):19-26.
-
1009Olsen MH, Angell S, Asmar S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on hypertension Lancet.2016;388(10060):2665-712.
-
1010Brandão AB, Amodeo C, Alcantara C, Barbosa E, Nobre F, et al. I Luso Brazilian Positioning Paper on Central Arterial Pressure. Arq Bras Cardiol. 2017; 108(2):100-8.
-
1011Hamczyk Nevado RM, Barettino A, Fuster V, Andrés V. Biological Versus Chronological Aging. J Am Coll Cardiol. 2020; 75(8): 919-30.
-
1012Sugiura T, Takase H, Machii M, Nonaka D, Ohno K, et al. Central blood pressure predicts the development of hypertension in the general population. Hypertens Res. 2020;43(11):1301-8.
-
1013Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic Value of Flow-Mediated Vasodilation in Brachial Artery and Fingertip Artery for Cardiovascular Events: A Systematic Review and Meta-Analysis J Am Heart Assoc. 2015; 134(11): e002270.
-
1014Wu MY, Li CJ, Hou MF, Chu PY.New Insights into the Role of Inflammation in the Pathogenesis of Atherosclerosis. Int J Mol Sci. 2017;18(10:2034.
-
1015Grossman C, Levin M, Koren-Morag N, Bornstein G, Leibowitz A, Ben-Zvi I, et al. Left Ventricular Hypertrophy Predicts Cardiovascular Events in Hypertensive Patients with Coronary Artery Calcifications. Am J Hypertens. 2018;31(3):313-20.
-
1016McEvoy JW, Martin SS, Dardari ZA, Miedema MD, Sandfort V, Yeboah J, et al. Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation 2017;135(2):153–65.
-
1017Kerkelä R, Ulvila J, Magga J. Natriuretic Peptides in the Regulation of Cardiovascular Physiology and Metabolic Events. J Am Heart Assoc. 2015; 4(10):e002423.
-
1018Willeit P, Welsh P, Evans JDW, Tschiderer I, Boachie C, Jukema JW, et al. High-Sensitivity Cardiac Troponin Concentration and Risk of First-Ever Cardiovascular Outcomes in 154,052 Participants. J Am Coll Cardiol. 2017;70(5):558-68.
-
1019Pandey A, Patel KV, Vongpatanasin W, Ayers c, Berritz JD, Mentz RJ, et al. Incorporation of Biomarkers Into Risk Assessment for Allocation of Antihypertensive Medication According to the 2017 ACC/AHA High Blood Pressure Guideline: A Pooled Cohort Analysis. Circulation. 2019;140(25):2076-88.
-
1020Malachias MVB, Jhund PS, Claggett BL, Wijkman MO, Bentley-Lewis R, Chaturvedi N, et al. NT-pro BNP by Itself Predicts death and cardiovascular events in high-risk patients with type 2 Diabetes Mellitus. J Am Heart Assoc. 2020;9(19):017462.
-
1021lar R, Sánchez R, Boggia R, Peñaherrera, Lopez J, Barroso WS. Recommendations for home blood pressure monitoring in Latin American countries: A Latin American Society of Hypertension position paper. J Clin Hypertens(Greenwich).2020;22(4):544-54.
-
1022Shimbo D, Artenian N, Basile JN, Krakoff LR, Margolis K, Rackotz MK, et al. Self-measured blood pressure monitoring at home. A Joint Policy Statement From the American Heart Association and American Medical Association Circulation.2020;142(4):e42-e63.
-
1023Mukherjee R, Ghosh S, Gupta B, Chakravarty T. A Universal Noninvasive Continuous Blood Pressure Measurement System for Remote Healthcare Monitoring. Telemed J E Health. 2018;24(10):803-10.
-
1024Bard DM, Joseph JI, van Helmond N. Cuff-Less Methods for Blood Pressure Telemonitoring. Front Cardiovasc Med. 2019;6:40.
-
1025Fuchs FD, Whelton PK. High Blood Pressure and Cardiovascular Disease. Hypertension 2020 Feb;75(2):285-92.
-
1026Palombo C, Kozakova, M Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vasc Pharmacol. 2016; 77:1–7.
-
1027Morales SA, Coca A, Olsen MH, Sanchez RA, Sebba-Barroso WK, Kones R, et al. Clinical Perspective on Antihypertensive Drug Treatment in Adults With Grade 1 Hypertension and Low-to-Moderate Cardiovascular Risk: An International Expert Consultation. Curr Probl Cardiol. 2017 Jul;42(7):198-225.
-
1028Feitosa AD, Gomes MM, Passarelli Júnior O, Barroso WKS, Miranda RDS, Barbosa EDB, et al. Pharmacological Treatment of Hypertension: From the Golden Trio to the Octet Arq Bras Cardiol. 2020; 115(2):270-2.
-
1029Campana E, Cunha V, Glaveckaite S, Gruev I, Lamirault G, Lehmann E. The use of single-pill combinations as first-line treatment for hypertension: translating guidelines into clinical practice. J Hypertensi. 2020, 38:000-000 ahead of print
-
1030Laurent S, Chatellier G, Azizi M, Calvet D, Choukroun G, Danchin N, et al.A Strategy for Preventing Cardiovascular and Renal Events based on Arterial Stiffness. Protocol of the SPARTE Study.[Cited in 2020 Jul 20] Available from: https://clinicaltrials.gov/ct2/show/NCT02617238
» https://clinicaltrials.gov/ct2/show/NCT02617238 -
1031Barroso WKS, Inuzuka S, Guimarães GC, Pacífico RP, Melo VA, Oliveira LF, et al. Pharmacological Management of Hypertension Guided by Central or Peripheral Blood Pressure Measurement: Comparison of Two Strategies on the Incidence of Intermediate Outcome. Artery Research. 2020;26(1):1-4.
-
1032Arendse LB, Danser AHJ, Poglitsch M, Touyz RM, Burnett JC, Llorens-Cortesc, et al. novel therapeutic approaches targeting the renin-angiotensin system and associated peptides in hypertension and heart failure. Pharmacol Rev. 2019;71(4):539-70.
-
Note: These guidelines are for information purposes and should not replace the clinical judgment of a physician, who must ultimately determine the appropriate treatment for each patient.
Publication Dates
-
Publication in this collection
23 Apr 2021 -
Date of issue
Mar 2021


 Source: Carey et al. 2008.
Source: Carey et al. 2008. 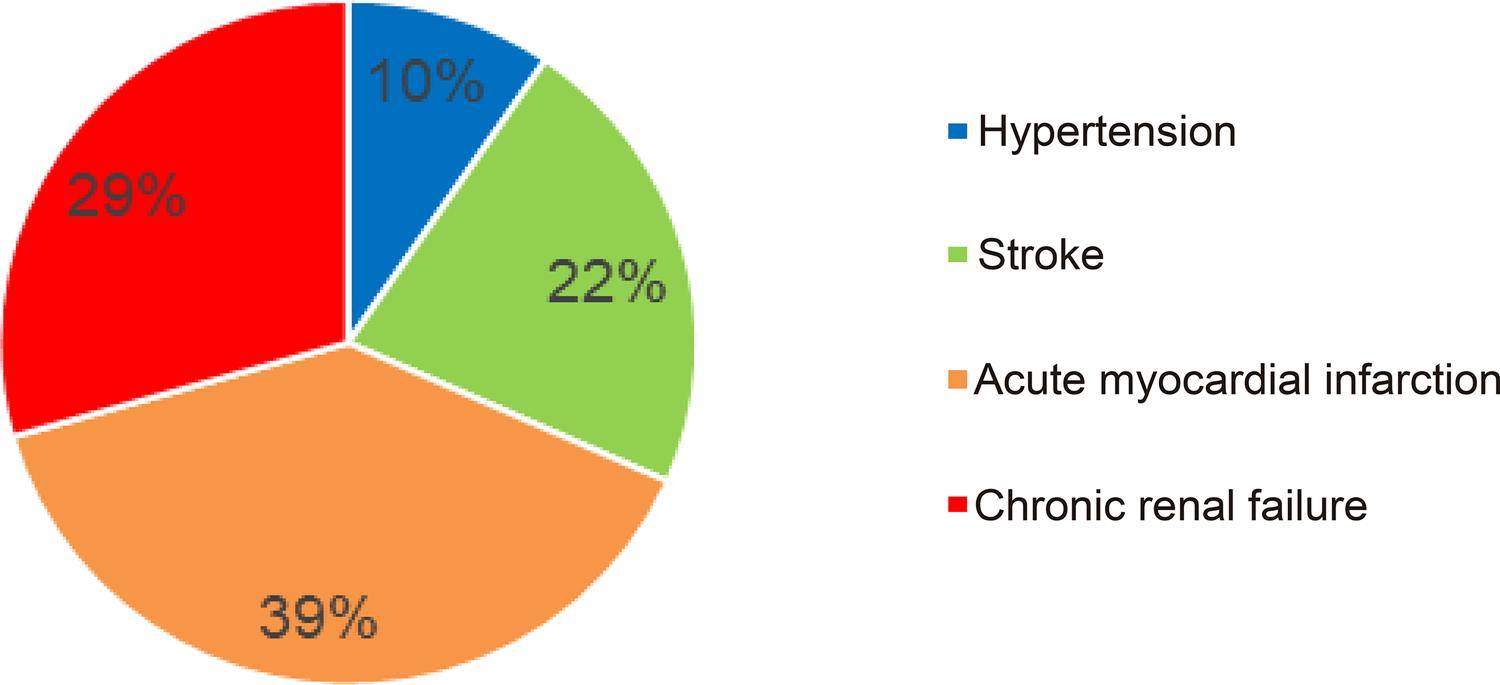
 Source: Nilson et al., 2020.
Source: Nilson et al., 2020.  MAPA: monitorização ambulatorial da pressão arterial; MRPA: monitorização residencial da pressão arterial.
MAPA: monitorização ambulatorial da pressão arterial; MRPA: monitorização residencial da pressão arterial.
 ABPM: ambulatory blood pressure monitoring; BP: blood pressure; HBPM: home blood pressure monitoring; MH: masked hypertension; SHT: sustained hypertension; TNT: true normotension; WCH: white coat hypertension.
ABPM: ambulatory blood pressure monitoring; BP: blood pressure; HBPM: home blood pressure monitoring; MH: masked hypertension; SHT: sustained hypertension; TNT: true normotension; WCH: white coat hypertension.
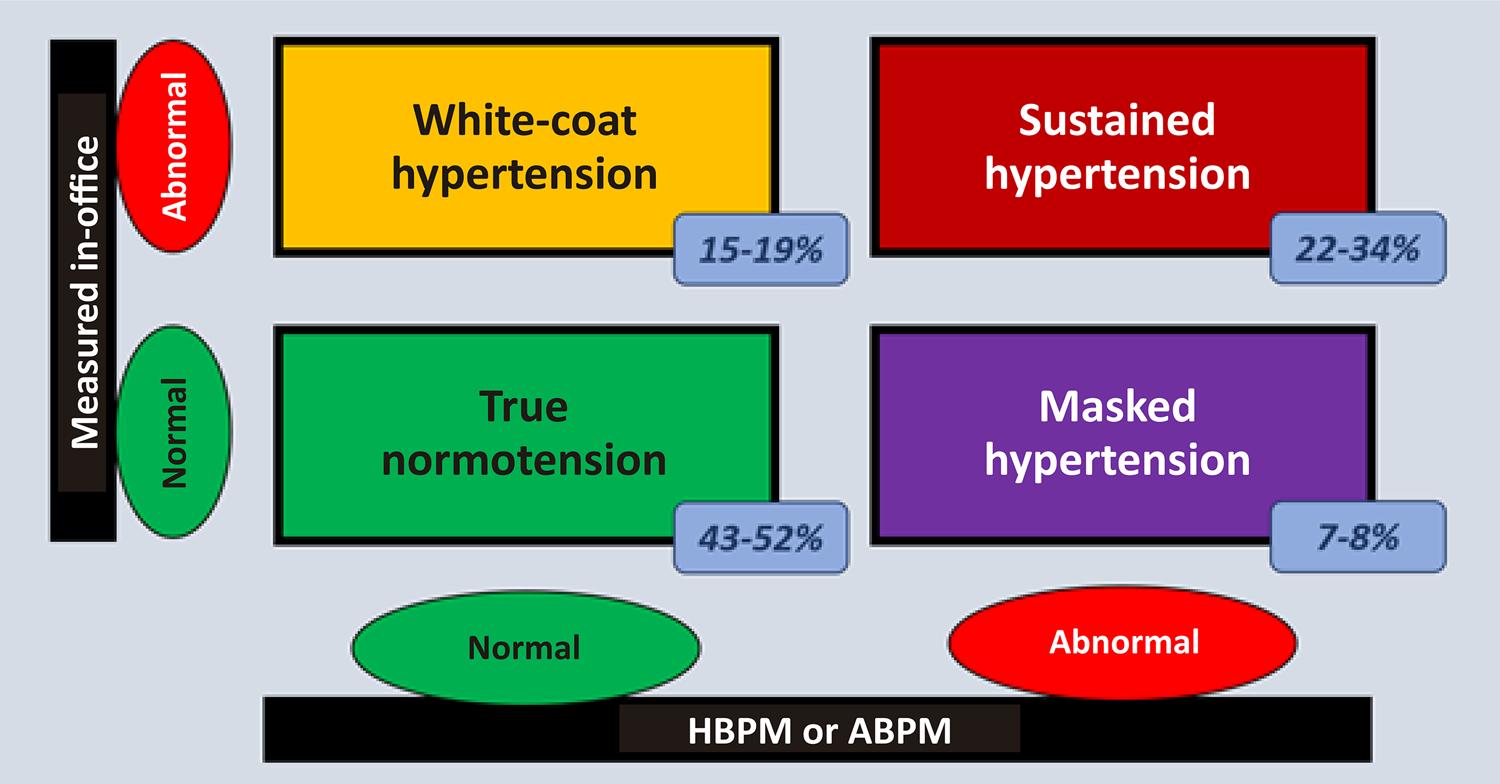 ABPM: ambulatory blood pressure monitoring; HBPM: home blood pressure monitoring.
ABPM: ambulatory blood pressure monitoring; HBPM: home blood pressure monitoring.
 CKD: Chronic kidney disease, eGFR: estimated glomerular filtration rate; KDIGO: Kidney Diseases Improving Global Outcomes.
CKD: Chronic kidney disease, eGFR: estimated glomerular filtration rate; KDIGO: Kidney Diseases Improving Global Outcomes.

 Source: Malachias et al., 2016.164
Source: Malachias et al., 2016.164
 Adapted from Whelton et al., 2018.
Adapted from Whelton et al., 2018.  Adapted from Vilela & Almeida, 2016.
Adapted from Vilela & Almeida, 2016. 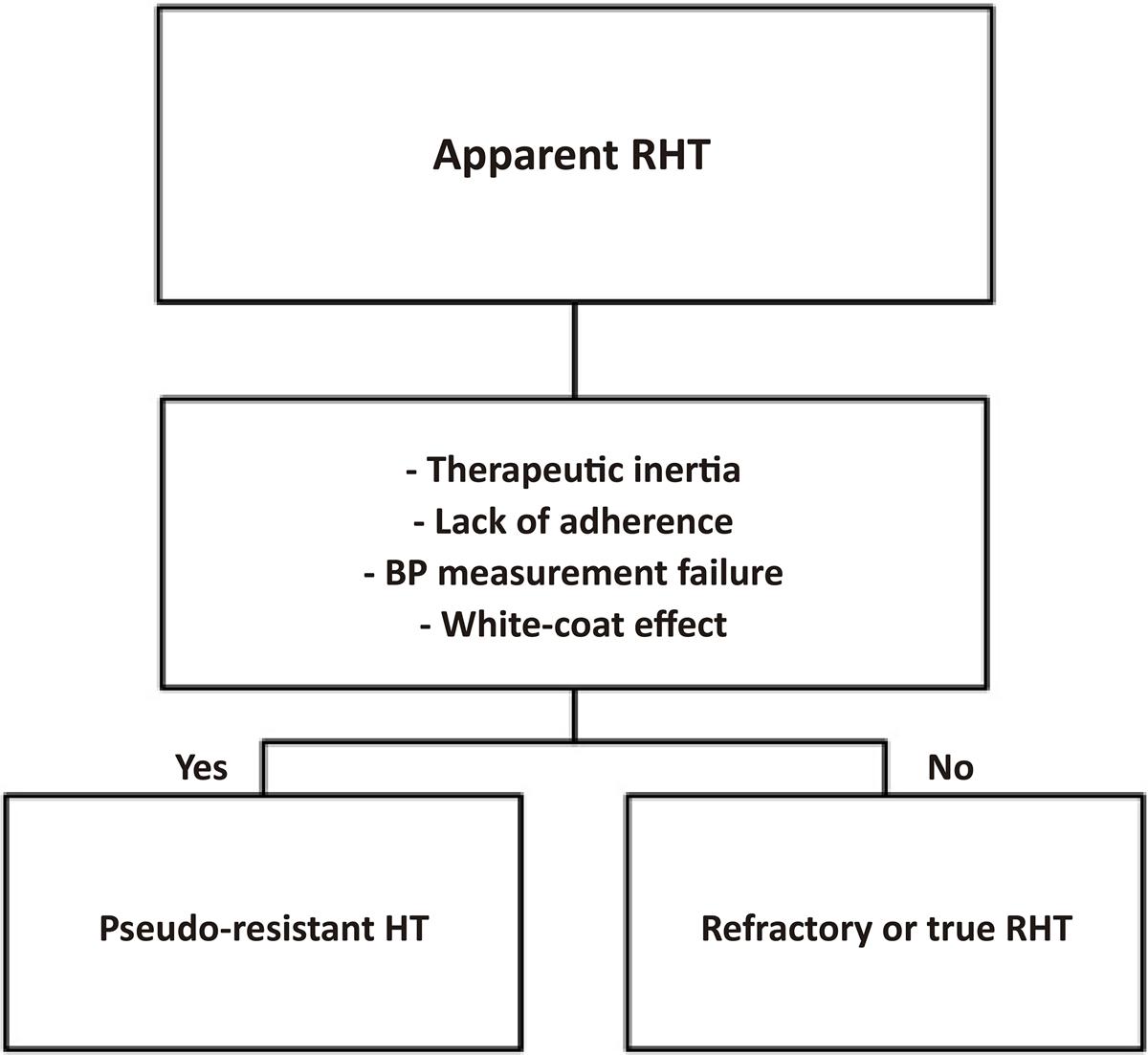
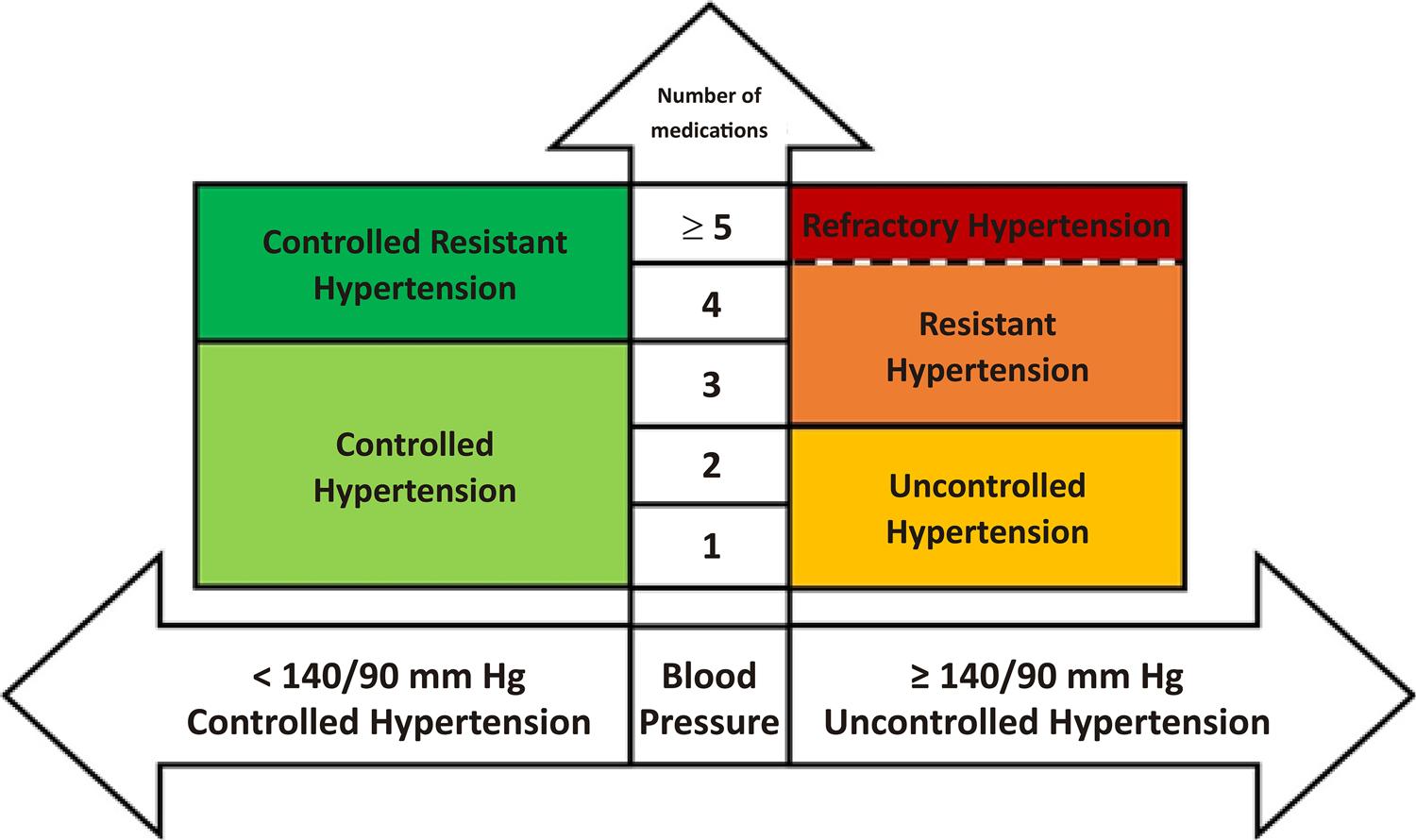 Adapted from Malachias et al., 2016;
Adapted from Malachias et al., 2016;  HR: Heart rate. Refractory (uncontrolled) individuals with five classes of antihypertensives are included in the refractory group (3-5%).
HR: Heart rate. Refractory (uncontrolled) individuals with five classes of antihypertensives are included in the refractory group (3-5%).
 JG cells: juxtaglomerular cells; LV: left ventricle; OSAS: obstructive sleep apnea syndrome; Oxidized FA: oxidized fatty acids; RAAS: renin-angiotensin-aldosterone system; SNS: sympathetic nervous system; UAW: upper airways.
JG cells: juxtaglomerular cells; LV: left ventricle; OSAS: obstructive sleep apnea syndrome; Oxidized FA: oxidized fatty acids; RAAS: renin-angiotensin-aldosterone system; SNS: sympathetic nervous system; UAW: upper airways.
 Source: Ji H et al., 2020.
Source: Ji H et al., 2020.  Source: Feitosa et al., 2020.
Source: Feitosa et al., 2020.