Abstracts
Nursing professionals working in Emergency Care suffer from the physical symptoms of stress in their everyday activity. The objective of this study was to characterize these symptoms using the Occupational Stress Indicator, a semi-structured instrument. To do this, the authors created open questions that were applied in interviews that were recorded and analyzed. The researchers listed the following physical symptoms: headache, a sensation of fatigue, leg pain, and tachycardia. According to reports form the workers, pain always resulted from emotional stress or appeared after providing emergency care, which suggests the workers find it very difficult to differentiate physical from mental stress. The investigation found that there is a need for measures to follow workers in their working activity. A manual was created, containing basic suggestions to improve the quality of life of the health team.
Stress; Emergency nursing; Ocupational health; Burnout, professional
O profissional de enfermagem que atua no Pronto Atendimento sofre sintomas físicos de estresse em sua atividade diária. O objetivo desta pesquisa foi caracterizar esses sintomas com utilização do instrumento semiestruturado Occupational Stress Indicator. Para tanto, os autores elaboraram perguntas abertas, aplicadas em entrevistas gravadas e analisadas. Os sintomas físicos listados pelos pesquisadores foram: cefaléia, sensação de fadiga, dores nas pernas e taquicardia. Segundo relatos dos colaboradores, as dores sempre resultavam de estresse emocional ou surgiam após atendimentos emergenciais, o que leva a crer que existe uma grande dificuldade desses colaboradores em separar o estresse físico do psíquico. A investigação determinou a necessidade de medidas para acompanhamento dos funcionários na sua atividade laboral. Elaborou-se uma cartilha com sugestões básicas para a melhoria da qualidade de vida da equipe de saúde.
Estresse; Enfermagem em emergência; Saúde do trabalhador; Esgotamento profissional
El profesional de enfermería que actúa en Emergencias sufre síntomas físicos de estrés en su actividad diaria. Esta investigación objetivó caracterizar tales síntomas con utilización del instrumento semiestructurado Occupational Stress Indicator. Para ello, los autores elaboraron preguntas abiertas, aplicadas en entrevistas grabadas y analizadas. Los síntomas físicos determinados por los investigadores fueron: cefalea, sensación de fatiga, dolor de piernas y taquicardia. Según testimonios de los colaboradores, los dolores siempre derivaban de estrés emocional o surgían luego de atenciones de emergencias, lo que lleva a pensar que existe una gran dificultad en tales colaboradores para separar el estrés físico del psíquico. La investigación determinó la necesidad de medidas para seguimiento de los trabajadores en su actividad laboral. Se elaboró un listado de sugerencias básicas para mejorar la calidad de vida del equipo de salud.
Estrés; Enfermería de urgencia; Salud laboral; Agotamiento profesional
ORIGINAL ARTICLE
Characterization of the physical symptoms of stress in the emergency health care team
Caracterización de los síntomas físicos de estrés en el equipo de Emergencias
Sílvia Maria de Carvalho FariasI; Olga Lúcia de Carvalho TeixeiraII; Walter MoreiraIII; Márcia Aparecida Ferreira de OliveiraIV; Maria Odete PereiraV
IRN. Graduate Student, Instituto Educacional Carapicuíba, SP. Member of the Study Group on Alcohol and Other Drugs (GEAD), University of São Paulo School of Nursing. Lorena, SP, Brazil. silviamcfarias@gmail.com
IIPh.D. in Nursing, University of São Paulo School of Nursing. Post-Doctoral fellow PNDP/CAPES, University of São Paulo School of Nursing. São Paulo, SP, Brazil. mariaodete@usp.br
IIIRN. Graduate Student, Instituto Educacional Carapicuíba, SP. São Paulo, SP, Brazil. olga_tcarvalho@hotmail.com
IVAssociate Professor, Maternal-Infant and Psychiatric Nursing Department, University of São Paulo School of Nursing. São Paulo, SP, Brazil. marciaap@usp.br
VPh.D. in Information Science, University of São Paulo School of Communication and Art. Faculty, Escola Superior de Cruzeiro. Cruzeiro, SP, Brazil. walter.moreira@fatea.br
Correspondence addressed to Correspondence addressed to: Silvia Maria Carvalho Farias Rua Victal Alves de Freitas, 235 - Bairro São Roque CEP 12601-000 - Lorena, SP, Brazil
ABSTRACT
Nursing professionals working in Emergency Care suffer from the physical symptoms of stress in their everyday activity. The objective of this study was to characterize these symptoms using the Occupational Stress Indicator, a semi-structured instrument. To do this, the authors created open questions that were applied in interviews that were recorded and analyzed. The researchers listed the following physical symptoms: headache, a sensation of fatigue, leg pain, and tachycardia. According to reports form the workers, pain always resulted from emotional stress or appeared after providing emergency care, which suggests the workers find it very difficult to differentiate physical from mental stress. The investigation found that there is a need for measures to follow workers in their working activity. A manual was created, containing basic suggestions to improve the quality of life of the health team.
Descriptors: Stress; Emergency nursing; Ocupational health; Burnout, professional.
RESUMEN
El profesional de enfermería que actúa en Emergencias sufre síntomas físicos de estrés en su actividad diaria. Esta investigación objetivó caracterizar tales síntomas con utilización del instrumento semiestructurado Occupational Stress Indicator. Para ello, los autores elaboraron preguntas abiertas, aplicadas en entrevistas grabadas y analizadas. Los síntomas físicos determinados por los investigadores fueron: cefalea, sensación de fatiga, dolor de piernas y taquicardia. Según testimonios de los colaboradores, los dolores siempre derivaban de estrés emocional o surgían luego de atenciones de emergencias, lo que lleva a pensar que existe una gran dificultad en tales colaboradores para separar el estrés físico del psíquico. La investigación determinó la necesidad de medidas para seguimiento de los trabajadores en su actividad laboral. Se elaboró un listado de sugerencias básicas para mejorar la calidad de vida del equipo de salud.
Descriptores: Estrés; Enfermería de urgencia; Salud laboral; Agotamiento profesional.
INTRODUCTION
The word stress is relatively new in Brazilian vocabulary. It was used for the first time in the middle of the past century to define the organisms reaction process to a dangerous situation. Stress factors trigger our struggle for life, as we receive stimuli 24 hours per day. Some stimuli are raised to the level of awareness, while others are merely captured by our subconscious; some are pleasant, others are not; some, at first, are insignificant, but through constant repetition become pathogenic(1). In this sense, occupational stress provokes the emergence of diseases that lead to absenteeism, causing losses for both workers and employers.
Health professions rank third as stress creation champions, due to the psychodynamic processes(2). In this context, nursing is classified as the fourth most stressful profession in the public sector. Few studies, however, investigate what problems make the nursing team give in to this stress.
Since its emergence until today, the health team has been linked with pain, disease and death. In Brazil, the large majority of professionals is concentrated in hospitals, dealing with these processes every day. Thus, health professionals live with the patients anxiety, feeling of loss and weakness, resulting from uncomfortable, painful and invasive care procedures, in a strange and cold environment(3). Nurses experience great anguish, which ends up arousing psychic tension. Therefore, professionals psychological aspect needs to be addressed, so that they are able to deal with such exhaustive contents, due to their susceptibility to experience occupational stress(4).
Emergency care to adult and/or child patients is one of the most exhaustive hospital sectors. The surprise factor requires fast and precise procedures from the team, working to provide patients and relatives with comfort and help. By itself this already causes physical and mental exhaustion for care professionals working there. Besides routine care delivery, cardiac arrests, convulsions, acute lung edemas and injuries caused by firearms or melee weapons are characteristic events at that sector.
In view of the above considerations, the aim of this study is to obtain data on the physical symptoms perceived and expressed by the nursing team at the adult and child Emergency Care of a general hospital in a city in the Mid-Vale do Paraíba, according to shift and causal factors.
LITERATURE REVIEW
In 1936, the Austrian physiologist Hans Selye had collected the first observations of stress. He perceived that non-chemical symptoms provoked the same reactions in the organism as toxic-chemical substances(1).
The word stress is associated with feelings of discomfort that disturb the human bodys homeostasis(5). The study of occupational stress manifestations in the nursing team permits a better understanding of triggering factors, so that interventions can be proposed and solutions sought for this disease(6).
Stress phases are divided in: a) Alarm, which is considered the phase when the organism suffers metabolic
alterations and is recomposed, relaxing; b) Resistance and adaptation, characterized by the continuation of the stress agent over time. Thus, the organism adapts its reactions and metabolism to bear the stress for a longer period; c) Exhaustion or breakdown. In this phase, the organism cannot bear the frequent pressure and starts to collapse, as the energy directed at the persons adaptation to the stressful request is limited, enhancing a drop in the human bodys adaptation capacity. This phase is generally reached only in the most severe and persistent situations(1).
According to the Psychodynamics of Work, identity construction mobilized a symbolic retribution process. The workers singularity is acknowledged by the other, through his/her contribution to the organization of work(4).
At a hospital emergency care unit, common work situations are permeated by unexpected events: crashes, incidents, functional anomalies, organizational incoherence, unexpected circumstances caused by materials, equipment and workers themselves. Hence, non-chemical stimuli cannot be forecasted, which can make workers experience feelings of suffering(4).
People should think about their relation with work, and the consequences of this relation for life outside the work environment and for life in general, that is, to dive into the actor-subject dialectic, which should give them pleasure(4).
OBJECTIVES
The following aims were proposed: to identify triggering factors of stress in the nursing team working at the adult and child Emergency Care unit of a general hospital in a city in the Mid-Vale do Paraíba; to identify the physical symptoms caused by the stress affecting these subjects; to propose strategies with a view to improvement in the work environment and the quality of life of the people involved in the research; to elaboration a stress prevention and control folder in the work environment, aimed at employees from the research institution, for dissemination among other nursing team members at the hospital.
METHOD
This is a quantitative/qualitative research, as overcoming the dualism between quantity and quality is expressed in the fact that any quality always comprises certain quantitative limits and vice-versa(7). The study was accomplished at an Emergency Care (EC) unit of a General Hospital in the mid-Vale do Paraíba.
The ECs physical structure contains a pre-consultation room, four child and adult care boxes, one wound dressing room, one small surgery room, one orthopedic care room, one total emergency room, one nebulization room adjacent to the nursing station; one meeting room, two rooms, one of which for the pediatrician on duty and the other for the general practitioner, waste room and kitchenette for health professionals to have coffee. Every 24h, the service attends approximately sixty consultations.
The nursing team consists of one nurse, who serves as the nurse manager, four nurse supervisors, one relief nurse, 15 nursing technicians and two nursing auxiliaries who work three shifts. Study participants included the four nurse supervisors, 15 nursing technicians and two nursing auxiliaries. Thus, our sample comprised 21 people, corresponding to 91.30% of the Nursing staff working at the EC. In the second part of the research, 20 people participated, corresponding to 86.96% of the target public.
The research obtained a favorable opinion from the Institutional Review Board at Faculdades Integradas Teresa DÁvila de Lorena, under protocol No 27/2006. All recommendations of CONEP Resolution 196/96 for research involving human beings in Brazil was complied with to elaborate the Informed Consent Term the participants signed(8). A priori, confidentiality is fundamental in a research process where a range of individuals is investigated(9).
According to Resolution No 196, issued in October 1996, secrecy was guaranteed in order to preserve the subjects identity. Thus, in this study, collaborators were identified with the names of Brazilian gems when referring to their statements.
Data were collected between February 2007 and January 2008.
In the first research phase, an adapted questionnaire was used, restricted from the Occupational Stress Indicator (OSI) that was developed in 1988(10). This semistructured instrument contained items related to socio-demographic characteristics and other related to the symptoms defined as worker exhaustion(4). The study participants should mark the symptoms manifested in their professional life. Data were analyzed in percentage form and presented as tables, using Excel 2003 software.
The authors elaborated an instrument with open questions for the second research phase, applied during an interview that was recorded and analyzed(11).
The questions were elaborated to check the collaborators understanding about the stress concept, signs and symptoms; about what discontented them, wore them out and bothered them; how they dealt with human emotions related to the patient, companion, head and health team; and what strategies they used to maintain harmony at the interface between family and work.
All interviews were transcribed, transcreated and recreated. In civil construction, this is equivalent to removing the scaffolds when the work is done, that is, making it grammatically acceptable without removing its essence though. In this perspective, the interviewee is seen as a collaborator, as he is part of the project and its accomplishment would not be possible without him(11).
The term collaborator is important to define the relationship between interviewee and interviewer, as it establishes a relationship of affinity between the parts, fundamental for good research development(11).
The collaborators discourse was submitted to content analysis. Qualitative research is a process and data analysis is one of different periods, part of the process, which identifies the care, sensitivity and respect to conduct the dialogue(9).
RESULTS
The target public under analysis included four nurses, 15 nursing technicians and two nursing auxiliaries. Women (90.48%) and young adults (76.19%) were predominant in the study population.
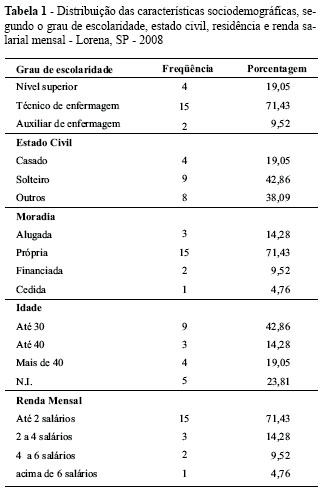
Next, data on the participants socio-demographic characteristics will be presented (Table 1).
As for education, besides the nurses, three nursing technicians were taking an undergraduate program in health. Only two employees did not have a secondary education degree.
Regarding marital status, single people predominated (42,.6%). The age of participants children ranges between one and thirty years.
Table 2 shows the collaborators distribution across the sector according to time of work at the health institution.
Regarding time of work, a majority has worked at the Emergency Care sector for more than four years, suggesting that the team develops its tasks confidently.
Although 76% of the collaborators did not choose to work at the Emergency Care, all of them alleged no difficulties to deal with the situations experienced at the sector.
Hence, it is assumed that this fact decreases the workers anxiety factor and increases the eustress, which is inherent in and necessary for human existence. Nobody lives without stress, as it is present from the beginning until the end of human life, making it intense.
Although it is known that physical stress results in psychological stress and vice-versa, collaborators perceive the physical symptoms, reported when answering the semistructured questionnaire. These symptoms appeared 104 times. Based on this calculation, each respondent manifested, during the time they have worked at the Emergency Care, an average five of the described symptoms.
People normally display resistance to admit psychological stress symptoms, in response to environmental and social demands that require control over the situation, making them "pretend that everything is alright" (authors highlights). Hence, these symptoms emerge when one does no longer manage to mask the process that is experienced.
Table 3 distinguishes the physical symptoms the participants presented.
In response to one of the study objectives, a folder called the "Antistress Folder" was elaborated. The 28-page folder contains topics to describe: stress concept; physiology; signs and symptoms, antistress tips and tips for a good walk, relaxation methods, besides a Theoretical Nursing Model with a stress approach(12). The material was distributed to the collaborators and to all employees at the hospital institution where the study was carried out.
DISCUSSION
The symptoms most of the employees presented were: headaches caused by tension or muscle pain, followed by feelings of fatigue.
A study accomplished at a university hospital to detect the psychosomatic repercussion among nursing workers appointed the same signs and symptoms mentioned above, including decreased memory and premenstrual tension(13).
A study at 23 Health Units in Minas Gerais - Brazil, aiming to identify mental and behavioral disorders nursing workers presented, found that, in 2002, 692 nursing workers received diagnoses related to mental and behavioral disorders. The study also revealed that 40.8% of the diagnoses were related with pathologies that are legally considered occupational illnesses, including depressive episodes, which are considered stress producers(14).
In nursing workers, mental and behavioral disorders represented the second cause of care demands to the Occupational Health Service, which relates stress and depression with physical exhaustion, absenteeism, bad quality of care delivery and workers leave of absence for health treatment(15). In their job, these workers become vulnerable to the psychopathologies, as they physical and psychically suffer the effects another persons pain, suffering and death cause in them, associated with the stress inherent in their existence(16).
Moreover, stress and the burnout syndrome are mentioned as dysfunctional consequences nurses develop in their professional lives in the hospital context(17).
The human body can be compared with a very well organized body, with different sectors, which are harmoniously interconnected and commanded by the brain. When the brain interprets a situation as a threat, beyond ones will, the organism starts to develop a range of alterations called the General Adaptation Syndrome, known as the fight or flight response. This mechanism was observed in animal studies, which described stress as an organisms reaction to fight or flee in response to a true or imaginary stimulus(1).
Fatigue, tension headache and muscle pain are symptoms that appear in the Burnout syndrome, characterized by physical and emotional breakdown resulting from chronic stress. Thus, other adverse symptoms are triggered which the study population feels: feeling of discouragement in the morning, sleeping difficulties and interrupted sleep, gastric discomfort and stomach ache, tachycardia, muscle tremors, decreased appetite, feeling short of breath and lack of air, decreased sexual interests, feeling of sweating and facial redness, besides pricks the interviewees felt across their body. These feelings cause harmful effects in human beings(1).
In general, collaborators do not define what stress it, the theme of the first specific script question, but mention feelings, situations leading to stress, always relating it with a negative aspect;
... stress is that moment when you accumulate anxiety, nervousness, fatigue, sadness and when you have a goal but do not manage to accomplish it... (Brilliant);
... Its a lot of responsibility, a lot of tension and a lot of headache, rushing. Its the red sign, the alert sign... (Onyx).
These feelings and symptoms can aggravate or even trigger diseases. In a stress situation, the cortisol hormone, produced by the suprarenal cortex, acts on the glucose, protein and fat metabolism, so as to increase its resistance to physical stress. If the cells do not use this intense fat mobilization, however, its concentration in extracellular fluids can increase sufficiently to cause acidosis, as the liver degrades most of this fat into keto acids(18).
As for the essence of the meaning, stress is defined differently among the collaborators when considering the different nursing categories. According to the nurses, the responsibility of supervising an insecure team is a maximum stress generation factor.
... For me, stress means working with a team that is not well-synchronized and, therefore, its attitudes are insecure.. (Cristal);
For me, it means insecurity. It is difficult for well-trained professionals to stress out the nursing team... (Aquamarine).
A study to characterize stress in nurses concludes that professional activities of supervision and management, in which one assumes the responsibility for another, demand further time dedicated to interaction, increasing stress events due to interpersonal conflicts(19).
The activity the collaborators consider most stressful, although common in the teams experience, is the emergency, which raises adrenaline but is part of the eustress, which drives us in search of the best result for the patient. Adrenaline and circulating noradrenaline exert exciting effects, directly acting on tissues, inhibiting intestinal peristalsis, increasing cardiac activity and all cell metabolisms, besides raising and stimulating the mental activity level(16). This indicates the positive effect of noradrenaline in people, preparing them for the activity they intend to perform.
... At that moment its complete stress. You have to do everything fast to save the patient, you have to act, everything has to be prepared. You have to stay calm and at the same time be fast to perform the interventions... (Tourmaline).
... Emotional exhaustion results from the rush of emergency care, but its dignifying to see the patients recovery... (Emerald).
A study at critical care units found that nurses suffer emotional alterations during their shift, due to the exhaustion and stress characteristic of care work, mainly at those units that demand high skill levels and require immediate reactions in emergency situations(20).
The collaborators mentioned other activities as stress generators: patients impatience, irritated companions, intolerant physicians, childcare, emergency in two sectors at the same time. The situations they experience regularly are in line with Hans Selyes Theory, which disseminates the General Adaptation Syndrome (GAS), in which the organism experiences stress until reaching its limit and giving in to physical and then psychic exhaustion.
The defense system, which the GAS puts to work, acts as if it were the headquarters, following a strategic plan. Thus, as from the moment when the stress agent attacks, the organism sends a message to the hypophysis to produce the hormones that will strengthen the defense system to fight the enemy. The adrenocorticotrophic hormone (ACTH), which will defend the organism against the harmful effect of stress, receives cooperation, after acting on the suprarenal cortex, from the glucocorticoids and the mineralocorticoids, both extremely important for our organism. Based on this hormone mechanism, the human organism primarily joins phenomena that will recognize a similar situation and, when necessary, will react efficiently(18-21).
If the aggression continues, however, resistance grows weak and the organism gets exhausted, creating opportunity for the appearance of opportunistic illnesses.
... You are already facing the stress of pleasing the child and, in addition, you have to convince the family that everything that is being done is for her good... (Brilliant).
... Look, dealing with people is not easy, besides dealing with people we deal with sick people, with unintelligible physicians and thats the problem... (Ruby).
Stress can appear in response to the persons reaction to the current situation, which echoes past experiences lived in similar situations(21).
According to the team, what causes emotional and physical exhaustion is to work in an upright position for twelve hours without a pause: patient transportation and shift transfers, due to the proximity of the nebulization room; besides the companions.
... Another task I consider stressful is the noise caused by the proximity between the nebulization room and the nursing station. There is no specific room for inhalation. At lunchtime and during shift transfers, which are peak hours for nebulization care, that causes some confusion... (Opal);
... During shift transfers, because the oxygen exits are next to the nursing station. That hampers the shift transfer because of the noise and the patients curiosity, who keep on paying attention to what the nursing staff is saying... (Tourmaline);
... the only thing is that the inhalation room is next to the station and that there is no divider to decrease the noise... (Sapphire).
Answers include accumulated work, a lot of rushing, pressure and charges, showing that people do not always manage to conceptualize stress. Thus, they refer to stress through feelings, actions and/or situations.
Losing a patient saddens the team and arouses feelings of void and powerlessness in view of death. The collaborators report that giving this bad news to the relatives is a factor that causes physical and psychic disorders.
... At the Emergency Care, patients arrive in severe conditions, they die and informing the relatives about the patients death, mainly when unexpected, is something that makes me feel a lot of anguish and pity... (Aquamarine)
Among the collaborators answers on what bothers them, the answer about the cleaning product used for floor maintenance at the sector stood out, due to the connotation and pitch;
... What bothers me is that, the day they have to clean the whole floor at the sector. That causes a lot of disorder, because you cant step on it while its wet, and its exactly at that time when nobody can get through that an emergency or even a routine care case arrives... (Brilliant).
... The activity that really stresses me is the day when the cleaning team has to pass a product to clean the floor. It takes 40 minutes for the product to dry and we cant step on it during that time. Now, using that kind of product at an Emergency Care where people are arriving the whole time is always complicated. You cant tell when a patient will arrive or not to be able to pass the product. Theyd have to change to type of product... (Turquoise).
The questions about the strategies to conciliate work and the family-work interface intermingle, leading to one single response. Therefore, the analysis was combined. Employees manage to perform daily housework and work-related tasks well, using relaxation mechanisms that involve reading, sports and going out for lunch and/or dinner, according to each professionals purchasing power, besides attempting not to mix domestic and professional problems. Relaxation is also part of recommended practice to relieve tension and enhance physical and mental recovery(1).
The study population presented a range of answers common to the human essence, which is that we are unique beings and therefore have different opinions on the same topic and similar reactions to the same problem and/or stimulus.
As for the hour load, most collaborators like the current times, i.e. 12 hours of work and 36 hours of rest, with two extra times off per month. Only one employee works eight hours/day and is satisfied; as her time off is on Saturdays, Sundays and holidays. Three of the collaborators who mentioned that they did not like the times are nurse supervisors. Thus, in total, 75% of the interviewed nurses report that their performance considerably decreases during the last four hours of their shift. They relate the final work hours with concentration loss, due to physical and mental fatigue, mainly when working night shifts. Most of the interviewed workers, when asked about shift preferences, answered that they prefer to work at night, due to the fact that less sectors are functioning and less people are passing by.
Regarding the physical conditions of the workplace, the collaborators showed to be satisfied, as the hospital is investing in infrastructure. The Emergency Care was constructed with a view to better attending partners and users, with modern equipment that facilitated the health teams work. Among the collaborators, 95% approve the new structure and give only few suggestions which, if put in practice, will contribute to service excellence: separation between the nebulization room and nursing station, so as not to hamper the shift transfer; placement of automatic doors to facilitate patient transformation on stretchers and in wheelchairs; and mainly to increase the number of boxes for patient care, as delayed attention due to a lack of beds is patients main complaint. Only one collaborator did not adapt to the air-conditioning and lack of windows in the sector.
Interpersonal relations are important for the good flow of teamwork. When answering the question about the theme, the collaborators discussed the reason for their answers, anxious for the authors not to misinterpret them.
In this respect, the authors believe that oral language stimulates the collaborators, during personal analysis, to discover what takes them to their stress limit and how it will affect the organization as a whole.
Many interviewed employees complain of the companions, associating them with a very relevant stress factor:
... As for the companions, we try to put ourselves in their place but do not always manage to,... theyre on one side and were on the other. Some really surpass the limits because they think they can give you orders... they rarely say please. Ugly faces and bad moods, we have to bear it all, thats very stressful... (Agate).
... Sometimes its the companion who wears us out, not so much the patient... (Pearl).
... Only stressy companions make me lose my temper, but I control myself, I try to put myself in their place with their sick relative... (Nacre).
The fact that the nursing team works in adverse situations, imposing great demands for varying activities and
in different shifts, can affect physical performance and cause mental, neurological, psychiatric and gastrointestinal disorders(22).
Thus, the authors agree that occupational stress can also be seen from a kaleidoscopic perspective, marked by interaction between the person, situation and stress agent.
CONCLUSION
Finally, the physical symptoms the researchers listed as stress characteristics were: headache, feeling of fatigue, leg pain and tachycardia. When asked about the meaning of stress, however, these pains always appeared associated with emotional stress or after emergency care, leading to the belief that great difficulty exists to distinguish between physical and psychic stress.
The physiology of stress involves hormonal mechanisms that stress in the brain when the neuro-hypophysis is stimulated and trigger a chain of events that include the suprarenal glands, which act on the stomach, the heart, the lymphatic system, even mobilizing the immunological system. Thus, not only is the organisms defense jeopardized, but endorphin and serotonin levels also drop, which raise human beings self-esteem(18).
The predominant complaints are related to the companions, the proximity of the inhalation room to the nursing station, the cleaning and maintenance process of the sector floor and the physicians impatience. The signs and symptoms the team mentions are typical of stress, determining these professionals exhaustion.
As proposed, the authors will present the following to the Hospital administration and board: suggestions for an occupational gymnastics program for employees, involving one staff worker (a physiotherapist), without any additional cost for the company; the creation of a reading space, where employees can enjoy reading during their break. With a view to decreasing the costs to establish this project, donations from the health team and relatives are suggested to acquire books and magazines.
In addition, the employees received a folder with simple concepts related to stress and the appearance of its signs and symptoms, with a view to promoting self-knowledge. This promotion will facilitate the understanding on how to proceed to impede or interrupt the establishment of stress as a disease. Self-knowledge is essential to human beings, as it clarifies and raises their awareness on what is afflicting them. This state of knowledge will decrease absenteeism and leaves of absence for health treatment, entailing benefits for employees as well as employers.
These measures will certainly enhance the health teams quality of life and will improve the quality of care delivery to the patients who need care.
At the start of the research, the researchers aimed to characterize the physical stress symptoms but, during the investigation, they found that the theme and the essence of human beings are too complex to be characterized in fragments. Therefore, at the end of the study, the comprehensive picture of the collaborators organization and their holistic look prevailed.
REFERENCES
Received: 04/09/2009
Approved: 09/06/2010
- 1. Datti D. Mecanismos e prevenção do stress. Rio de Janeiro: Rosa dos Tempos; 1987.
- 2. Lazarus RS, Folkman S. Stress: appraisal and coping. New York: Springer; 1984.
- 3. Cooper CL, Sloan SJ, Willians S. Ocupational stress indicator management guide. Oxford: NFER-NELSON; 1988.
- 4. Dejours C. A loucura do trabalho: estudo de psicopatologia do trabalho. São Paulo: Cortez; 1992.
- 5. Ferreira ABH. Novo dicionário da língua portuguesa. Rio de Janeiro: Nova Fronteira; 1986.
-
6Brasil. Ministério da Saúde; Organização Pan-Americana da Saúde, Escritório de Representação no Brasil. Doenças relacionadas ao trabalho: manual de procedimentos para os serviços de saúde [Internet]. Brasília; 2001 [citado 2010 nov. 10]. Disponível em: http://www.opas.org.br/publicmo.cfm?codigo=48
- 7. Minayo MCS. O desafio do conhecimento: pesquisa qualitativa em saúde. 11ª ed. São Paulo Hucitec; 2008.
- 8. Conselho Nacional de Saúde. Resolução n. 196, de 10 de outubro de 1996. Dispõe sobre diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Bioética. 1996;4(2 Supl):15-25.
- 9. Ângelo M. Rigor and ethics: challenges in qualitative research. Ciênc Saúde Coletiva. 2008;13(2):312-28.
- 10. Moraes LFR, Swan JA, Cooper CL. A study of occupacional stress among government collar works in Brazil using the Occupacional Stress Indicator. Stress Med. 1993;9(1):91-104.
- 11. Meihy JCS, Holanda F. História oral: como fazer como pensar. São Paulo: Contexto; 2007.
- 12. Farias SMC, Carvalho OLT, Moreira W, Oliveira MAF, Pereira MO. Cartilha antiestresse [Internet]. Lorena; 2009 [citado 2009 ago. 02]. Disponível em: http://www.unimed-lorena.com.br/sites/File/pdf/cartilha.pdf
- 13. Belanciere MF, Bianco MHBC. Estresse e repercussões psicossomáticas em trabalhadores da área da enfermagem de um hospital universitário. Texto Contexto Enferm. 2004;13(1):124-31.
- 14. Murofuse NT, Abranches SS, Napoleão AA. Reflexões sobre estresse e Burnout e a relação com a enfermagem. Rev Lat Am Enferm. 2005;13(2):255-61.
- 15. Manetti ML, Marziale MHP. Fatores associados à depressão relacionada ao trabalho de enfermagem. Est Psicol [Internet]. 2007 [citado 2008 mar. 15];12(1):79-85. Disponível em: http://www.scielo.br/pdf/epsic/v12n1/a10v12n1.pdf
- 16. Camarotti H, Teixeira HA. Saúde mental e trabalho: estudo da regional norte de saúde do DF. Rev Saúde Dist Federal. 1996;7(1):29-40.
- 17. Baba V, Galaperin BL, Lituchy TR. Occupational mental health: a study of work related depression among nurses in the Caribbean. Int J Nurs Stud. 1999;36(2):163-9.
- 18. Guyton AC. Fisiologia humana. 6ª ed. Rio de Janeiro: Guanabara Koogan; 1988.
- 19. Guerrer FJL, Bianchi ERF. Caracterização do estresse nos enfermeiros de Unidades de Terapia Intensiva. Rev Esc Enferm USP. 2008;42(2):355-62.
- 20. De Martino MMF, Misko MD. Estados emocionais de enfermeiros no desempenho profissional em unidades críticas. Rev Esc Enferm USP. 2004;38(2):161-7.
- 21. Pafaro RC, De Martino NMF. Estudo do estresse do enfermeiro com dupla jornada de trabalho em um hospital de oncologia pediátrica de Campinas. Rev Esc Enferm USP. 2004;38(2):152-60.
- 22. Silva JLL, Melo ECP. Estresse e implicações para o trabalho de enfermagem. Inf Promoção Saúde [Internet]. 2006 [citado 2008 mar. 14];2(2):16-8. Disponível em: http://www.uff.br/promocaodasaude/estr.trab.pdf
Publication Dates
-
Publication in this collection
22 June 2011 -
Date of issue
June 2011
History
-
Accepted
06 Sept 2010 -
Received
09 Apr 2009