Abstracts
The objective of this study was to verify if replacing the Injury Severity Score (ISS) by the New Injury Severity Score (NISS) in the original Trauma and Injury Severity Score (TRISS) form would improve the survival rate estimation. This retrospective study was performed in a level I trauma center during one year. ROC curve was used to identify the best indicator (TRISS or NTRISS) for survival probability prediction. Participants were 533 victims, with a mean age of 38±16 years. There was predominance of motor vehicle accidents (61.9%). External injuries were more frequent (63.0%), followed by head/neck injuries (55.5%). Survival rate was 76.9%. There is predominance of ISS scores ranging from 9-15 (40.0%), and NISS scores ranging from 16-24 (25.5%). Survival probability equal to or greater than 75.0% was obtained for 83.4% of the victims according to TRISS, and for 78.4% according to NTRISS. The new version (NTRISS) is better than TRISS for survival prediction in trauma patients.
Wounds and injuries; Trauma Severity Indices; Injury Severity Score; Outcome assessment (health care)
O objetivo deste estudo foi verificar se a substituição do Injury Severity Score (ISS) pelo New Injury Severity Score (NISS), na fórmula original do Trauma and Injury Severity Score (TRISS), melhora sua estimativa da taxa de sobrevida. Estudo retrospectivo realizado num centro de trauma nível I, durante um ano. A curva ROC foi utilizada para identificar o melhor indicador (TRISS ou NTRISS) para predição da probabilidade de sobrevida. O estudo incluiu 533 traumatizados, com idade média de 38±16 anos. Houve predomínio de acidentes de transporte (61,9%). Lesões externas foram mais frequentes (63,0%), seguidas por trauma craniencefálico/cervical (55,5%). A taxa de sobrevida foi de 76,9%. Houve predomínio dos valores do ISS variando de 9-15 (40,0%) e, do NISS, de 16-24 (25,5%). Probabilidade de sobrevida igual ou superior a 75,0% foi obtida para 83,4% das vítimas de acordo com o TRISS e por 78,4% de acordo com NTRISS. A nova versão apresentou melhor desempenho que o TRISS na predição de sobrevida dos doentes traumatizados estudados.
Ferimentos e lesões; Índices de Gravidade do Trauma; Escala de Gravidade do Ferimento; Avaliação de resultados (cuidados de saúde)
El estudio objetivó verificar si la substitución del Injury Severity Score (ISS) por el New Injury Severity Score (NISS) en la fórmula original del Trauma and Injury Severity Score (TRISS) mejora su estimación de tasa de sobrevida. Estudio retrospectivo realizado en centro de trauma nivel I durante un año. Se usó curva ROC para identificar el mejor indicador (TRISS o NTRISS) para predicción de probabilidad de sobrevida. El estudio incluyó 533 traumatizados, edad media 38±16 años. Predominaron accidentes de transporte (61,9%). Prevalecieron las lesiones externas (63%), seguidas de trauma cráneo-encefálico/cervical (55,5%). Tasa de sobrevida: 76,9%. Predominaron valores de ISS variando de 9-15 (40,0%) y de NISS, de 16-24 (25,5%). Se obtuvo probabilidad de sobrevida igual o mayor a 75% para 83,4% de víctimas según TRISS y para 78,4% según NTRISS. La nueva versión (NTRISS) presentó mejor desempeño que TRISS en predicción de sobrevida en los pacientes traumatizados estudiados.
Heridas y traumatismos; Índices de Gravedad del Trauma; Puntaje de Gravedad del Traumatismo; Evaluación de resultado (atención de salud)
ORIGINAL ARTICLE
The role of the New Trauma and Injury Severity Score (NTRISS) for survival prediction* * Originated from a dissertation "Survival probability: comparison of the results of Trauma and Injury Severity Score (TRISS) and its new version (NTRISS), University of São Paulo School of Nursing, 2008
El papel del New Trauma and Injury Severity Score (NTRISS) para predicción de sobrevida
Cristiane de Alencar DominguesI; Regina Marcia Cardoso de SousaII; Lilia de Souza NogueiraIII; Renato Sérgio PoggettiIV; Belchor FontesV; Daniele MuñozVI
IDoctoral Student of the Adult Health Care Post-Graduation Program of the University of São Paulo School of Nursing. São Paulo, SP, Brazil. crismingues@usp.br
IIAssociate Professor of the Medical-Surgical Nursing Department of the University of São Paulo School of Nursing. São Paulo, SP, Brazil. vian@usp.br
IIIDoctoral Student of the Adult Health Care Post-Graduation Program of the University of São Paulo School of Nursing. São Paulo, SP, Brazil. lilianogueira@usp.br
IVAssociate Professor of the School Medicine of the University of São Paulo. São Paulo, SP, Brazil. poggetti@terra.com.br
VMedical Assistant 3rd. of the Division of Surgical Clinics, Clinical Hospital School of Medicine, University of São Paulo. São Paulo, SP, Brazil. belchor@uol.com.br
VIPost-Graduate in Forensic Medicine, School of Medicine, University of São Paulo. São Paulo, SP, Brazil. danimunoz@uol.com.br
Correspondence addressed to: Correspondence addressed to: Cristiane de Alencar Domingues Rua Cônego Eugênio Leite, 892 / 73 - Cerqueira César CEP 05414-001 - São Paulo, SP, Brazil
ABSTRACT
The objective of this study was to verify if replacing the Injury Severity Score (ISS) by the New Injury Severity Score (NISS) in the original Trauma and Injury Severity Score (TRISS) form would improve the survival rate estimation. This retrospective study was performed in a level I trauma center during one year. ROC curve was used to identify the best indicator (TRISS or NTRISS) for survival probability prediction. Participants were 533 victims, with a mean age of 38±16 years. There was predominance of motor vehicle accidents (61.9%). External injuries were more frequent (63.0%), followed by head/neck injuries (55.5%). Survival rate was 76.9%. There is predominance of ISS scores ranging from 9-15 (40.0%), and NISS scores ranging from 16-24 (25.5%). Survival probability equal to or greater than 75.0% was obtained for 83.4% of the victims according to TRISS, and for 78.4% according to NTRISS. The new version (NTRISS) is better than TRISS for survival prediction in trauma patients.
DESCRIPTORS: Wounds and injuries; Trauma Severity Indices; Injury Severity Score; Outcome assessment (health care).
RESUMEN
El estudio objetivó verificar si la substitución del Injury Severity Score (ISS) por el New Injury Severity Score (NISS) en la fórmula original del Trauma and Injury Severity Score (TRISS) mejora su estimación de tasa de sobrevida. Estudio retrospectivo realizado en centro de trauma nivel I durante un año. Se usó curva ROC para identificar el mejor indicador (TRISS o NTRISS) para predicción de probabilidad de sobrevida. El estudio incluyó 533 traumatizados, edad media 38±16 años. Predominaron accidentes de transporte (61,9%). Prevalecieron las lesiones externas (63%), seguidas de trauma cráneo-encefálico/cervical (55,5%). Tasa de sobrevida: 76,9%. Predominaron valores de ISS variando de 9-15 (40,0%) y de NISS, de 16-24 (25,5%). Se obtuvo probabilidad de sobrevida igual o mayor a 75% para 83,4% de víctimas según TRISS y para 78,4% según NTRISS. La nueva versión (NTRISS) presentó mejor desempeño que TRISS en predicción de sobrevida en los pacientes traumatizados estudiados.
DESCRIPTORES: Heridas y traumatismos; Índices de Gravedad del Trauma; Puntaje de Gravedad del Traumatismo; Evaluación de resultado (atención de salud).
INTRODUÇÃO
In developed countries, trauma is the third leading cause of death, after heart disease and neoplasms(1-2). In Brazil, according to data from 2006, external causes were responsible for most deaths among individuals between one and 39 years of age(2), although, overall, the trauma patient's chance of survival can be greater than that of the above mentioned diseases if adequate hospital care is provided(3). The use of severity scores allows the documentation of trauma patient injury severity and its relation with clinical parameters(4), registration of epidemiological characteristics, and quality of the emergency care, leading to better results in trauma care(5). The objective assessment of trauma severity and the evaluation of death risk are helpful to guide the quotidian practice in establishing priority measures, especially for professionals with little experience in the care of severe trauma patients(6).
The Injury Severity Score (ISS), the anatomic trauma index most employed worldwide, is based on the Abbreviated Injury Scale (AIS) that codifies the severity of any traumatic injury to the different body regions (head and neck, face, chest, abdominal or pelvic contents, extremities or pelvic girdle, and external). Quantifying trauma patient survival rate is the basis for evaluating the effectiveness of the health care provided, as well as the efficacy of new therapeutic alternatives(7).The Trauma and Injury Severity Score (TRISS), an index to estimate the trauma patient's chances of survival, was developed based on the Major Trauma Outcome Study (MTOS) performed in 1982 (8). The TRISS is calculated using the Revised Trauma Score (RTS), the ISS, the patient's age, and the trauma mechanism - blunt or penetrating. The TRISS permits identification of patients who develop unexpected outcomes, as well as the comparison of outcomes of different patients groups(9).
Although the ISS was considered the best index to determine trauma severity for almost 20 years, it includes only one (the most severe) injury in each body region, however, a polytrauma patient may have two of the most severe injuries in the same body region. In this case, the ISS underestimates the trauma severity. In order to correct this ISS flaw, the New Injury Severity Score (NISS)(10) was developed, aiming to more precisely predict patient mortality(11). The NISS comprises the patient´s three most severe injuries, regardless of the affected body region(12-13). Thus, dividing the body in regions appears to be unnecessary, and in fact is not recommended today. The ability of the ISS versus the NISS for mortality prediction has been studied by different authors. Although the advantages of the NISS are controversial(6), diverse studies(7,10,12,14-16) have shown that the NISS is the more effective, while others(11,17) have not revealed significant differences between the ISS and the NISS in predicting trauma patients mortality. Nonetheless, none of the studies have shown the ISS to be superior to the NISS.
Considering the replacement of the ISS with the NISS in the original TRISS form, three studies have already been carried in the world, however the results were inconclusive. One of them concerned a population of Brazilian patients with abdominal trauma, another was a multi-center study performed in Iran and the final one was a study in a trauma center in Turkey(18-20).
The objective of this study was to verify if replacing the ISS with the NISS, for calculating the survival probability expressed in terms of the New Trauma and Injury Severity Score (NTRISS) instead of the TRISS, improves the estimation of survival rates.
METHOD
This retrospective study was performed at a level I trauma center (Clinical Hospital of the School of Medicine, University of São Paulo) in Brazil, and was based on data collected from the hospital records and autopsy reports of the patients. The study population consisted of adult (older than 18 years) patients admitted to this trauma center's emergency room from March 1st, 2006 to February 28th, 2007, due to blunt and/or penetrating trauma events. The patients were excluded from the study if they had been admitted to this trauma center more than 24 hours after the traumatic event, or if they were transferred from other hospitals without relevant data collected within the first hours post trauma for RTS calculation.
This study was approved by the Ethics Committee for Analysis of Research Projects of the Clinical Hospital of the School of Medicine. For the data collection, a list was elaborated containing all the items needed for calculating the ISS, the NISS, the TRISS and the NTRISS, including patient age, trauma mechanism, and injuries severity. In order to verify whether the replacement of the ISS with the NISS in the calculation of the TRISS improves its performance, the chance of survival for each victim was obtained using both equations: one using the ISS (TRISS), and the other replacing the ISS with the NISS (NTRISS)(19) in the equation. In this study, the 2005 AIS (Abbreviated Injury Scale) was used to obtain the injury codes. A descriptive analysis of the variables was performed and the ROC (Receiver Operating Characteristic) curve was used to determine whether the TRISS or the NTRISS was the better indicator to estimate the survival prediction, and to establish the most appropriate cutoff point. A 5% (p-value <0.05) level of significance was used in all tests.
RESULTS
A total of 533 patients were included in the study. The demographic characteristics of victims, the trauma mechanisms and the injured body regions are shown in Table 1. The victims presented a mean of 2.4 injured body regions. Blunt trauma was more common than penetrating, corresponding to 87.1%. The majority of patients (82.9%) received systematized prehospital care; 76.2% were assisted and taken to the hospital by road transport and the remaining 23.8% by air transport.
The length of hospital stay ranged from less than 24 hours to 225 days, with a mean of 11±18 days. Of all patients, 32.4% were hospitalized for 24 hours or less; 23.3% for three to seven days, and 8.8% for more than 30 days; 42.2% required hospitalization in the Intensive Care Unit (ICU). Of the 533 patients, 410 (76.9%) survived, and 123 patients died. The majority of patients (56.5%) had a Glasgow Coma Scale (GCS) score from 13 to 15. GCS score 8 was presented in 33.5% of the victims. Systolic blood pressure (SBP) > 89 mmHg on admission was present in 82.9% patients, however, 7.7% of patients presented SBP equal to zero. Respiratory rate from 10 to 29 breaths/minute was present in 76.4% of the victims. Patients with apnea on admission totaled 7.1%. For 15 patients, the medical records had no information on respiratory rate on admission to the hospital. As this information is necessary to calculate the RTS and, consequently, the TRISS, these patients were not considered when obtaining the trauma indices. The RTS, TRISS and NTRISS were determined for a group of 518 patients who presented the data necessary for the calculations.
The RTS presented a mean of 6.3±2.3; and the majority of victims (54.5%) presented RTS > 7. The victim distribution according to trauma severity from the ISS and the NISS are presented in Table 2, and the distribution according to survival probability from the TRISS and the NTRISS are showed in Table 3. The TRISS presented a greater value than the NTRISS in 63.3% of 518 patients. The difference between the chances of survival as predicted by TRISS and NTRISS ranged from 0.1% to 67.9%.
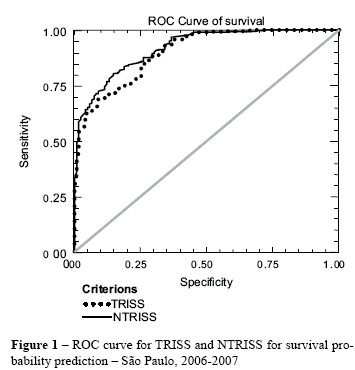
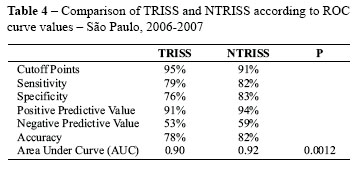
The analyses of the ROC curve for TRISS and NTRISS are demonstrated in Table 4 and Figure 1. The curve calibration by the Hosmer-Lemeshow Goodness-of-Fit was 0.0000 for the TRISS e 0.0002 for the NTRISS.
DISCUSSION
In 1966 trauma was already referred to as a "neglected disease of social modernity". This condition persists until today and kills millions of people around the world in both developed and underdeveloped countries, affecting mainly the productive age group of the population. Despite affecting mainly young adult people, the nature and severity of traumatic injuries are very heterogeneous, requiring emergency and complex medical attention and care. The use of trauma scores developed to quantify the traumatic injury severity in terms of risk of death has become an invaluable tool in trauma care.
In the present study, the role of the NTRISS versus that of the TRISS in the estimation of trauma patient survival was evaluated in a level I trauma center in a developing country where trauma patients are mostly young adult males and road traffic accidents were the highest cause of traumatic injuries, followed by falls. Most patients had external injuries, followed by head and neck injuries, and extremities and pelvic girdle, as in another similar study(20). Of the 123 patients who died, 70.7% presented head or neck injuries. The high frequency of systematized prehospital care received by the patients, including air transport, could be associated with the patients' severity. The death rate observed (24.1%) was higher than that of the MTOS (9.0%)(8) a fact that might be due to the MTOS having included trauma victims from trauma centers of different levels, and possibly less severely injured. For 2.8% of the population the respiratory rate (RR) was not available. In the MTOS, 11.1% of the population did not have information available regarding the values of all variables necessary to obtain the RTS; 57.0% of which had no recorded RR value at hospital admission(8).
Due to the difference in AIS values in their formulae, NISS scores are always equal to or greater than the ISS scores for the same patient. Of all patients of this study, 62.9% presented NISS values greater than their ISS values. A study performed at two level I trauma centers in the United States of America (USA) showed a difference between the ISS and NISS for 59.0% and 60.0% of patients(10). A similar result was found in a study performed with blunt trauma victims, in which 68% of cases showed a difference between the ISS and NISS score values(12). According to some authors, the NISS presents practical and clinical advantages over the ISS. From a clinical point of view, it is more logical since it gives the same priority to all injuries, regardless of the body region. From a practical point of view, it is easier to calculate, as it does not require dividing the body into regions(15,21).
For 20 years, TRISS has been the most widely used model to determine the chances of survival, although it does not present good calibration(9). In addition, it was developed from a databank of American and Canadian trauma cases, and the regression coefficients are related to the healthcare model used in these patients. Nevertheless, its limitations do not impede its use; they only require a critical analysis of the results regarding the population under study(19).
In this study, the chance of survival of 75% or more was presented by 83.4% and 78.4% of patients according to the TRISS and the NTRISS, respectively. Compared with the actual survival observed (76.9%), the results presented by the NTRISS were significantly closer to those observed than those presented by the TRISS. In 63.3% of patients, the chance of survival as calculated using the TRISS was higher than that calculated using the NTRISS. In the other cases, the TRISS value was equal to that yielded by the NTRISS. Just as the ISS does not yield higher values than the NISS for the indication of trauma severity, the chance of survival indicated by the TRISS is always greater than or equal to that of the NTRISS.
The ROC curve was used to verify whether the TRISS or the NTRISS was the best model for predicting the chance of survival. The cutoff points established for the TRISS and the NTRISS were, respectively, 95% and 91%. A lower cutoff point increased the sensitivity (82% vs. 79%) and specificity (83% vs. 76%) of the NTRISS. This signifies that the NTRISS more reliably identified surviving patients (sensitivity) and deaths (specificity). However, the Hosmer-Lemeshow Goodness-of-Fit values showed that the curves did not present a good calibration.
The first study in which the ISS was replaced by the NISS in the original TRISS form, the TRISS and the NTRISS were excellent predictors of survival, since they possessed high sensitivity (98.5% and 97.4%, respectively); however, in contrast to the present study, they presented a high rate of unexpected developments and low specificity (37.9% and 45.7%, respectively)(19). When conditional probabilities for the TRISS and the NTRISS were compared in this study, positive and negative predictive values were greater for the NTRISS (94% and 59% versus 91% and 53%, respectively). The NTRISS was also more accurate than the TRISS; the NTRISS made correct predictions in 82% of cases, compared to 78% for the TRISS. Another concept related to the ROC curve is the area under the curve (AUC), which is described as the global test accuracy. The larger the area, the greater the discriminatory power of the indicator for chance of survival. Comparing the area under the ROC curve, it was greater for the NTRISS than for the TRISS, with a significant p-value (p = 0.0012).
In the study performed with mostly penetrating, abdominal trauma victims, the NTRISS also showed better performance than the TRISS in estimating the chances of survival in the studied population(19). A multi-center study performed in Iran over a period of one year obtained different results. In the study population, 10% of patients presented an ISS score >12. In this study, the authors found the TRISS was a better predictor of survival than the NTRISS for penetrating trauma victims, but not for blunt trauma victims(20). The study performed in Turkey over a period of four years, with patients who had injuries in at least two organ systems found that the use of the NISS instead of the ISS in the TRISS model demonstrated no significant difference, and that it could therefore be recommended for use(18).
One limitation of the present study is that it was performed at a single, level I trauma center with a population of severely injured trauma victims. Another limitation, that has already been evaluated(22), is that some victims received neuromuscular blockers and were intubated during prehospital transport, thus interfering with data collection (respiratory rate for RTS and reactions for GCS) for the TRISS/NTRISS calculation.
In summary, the ISS is largely used to assess patients' injury severity; and the NISS has been considered better or at least equal to the ISS for this purpose. The TRISS (RTS + ISS) continues to be the most commonly used index for survival prediction in trauma patients. The NTRISS (RTS + NISS) was developed to improve the TRISS for survival prediction. Studies comparing TRISS vs. NTRISS have failed to reach a consensus regarding this purpose. In the present study, the NTRISS was better for identifying survivors and, compared to the TRISS, indicated survival in fewer cases where death occurred.
CONCLUSION
The NTRISS is more accurate than the TRISS for survival prediction in trauma patients.
Received: 06/09/2010
Approved: 03/21/2011
- 1. Gioffrè Florio M, Famà F, Gullo G, Buccheri G, Beccaria A, Caruso A, et al. Polytrauma management: our experience. Chir Ital. 2005;57(4):485-9.
-
2Brasil. Ministério da Saúde. DATASUS. Informações de Saúde. Estatísticas vitais: mortalidade e nascidos vivos [Internet]. Brasília; 2010 [citado 2010 jun. 12]. Disponível em: http://tabnet.datasus.gov.br/cgi/idb2008/matriz.htm#mort
- 3. National Association of Emergency Medical Technicians, Pre-Hospital Trauma Life Support Committee; American College of Surgeons, Committee on Trauma. Atendimento pré-hospitalar ao traumatizado: básico e avançado. Tradução de R. S. Poggetti. Rio de Janeiro: Elsevier; 2004.
- 4. Calil AM, Pimenta CAM. Relationship between trauma severity and analgesia standarts used in traffic accident victims. Rev Esc Enferm USP [Internet]. 2009 [cited 2010 June 12];43(2):328-34. Available from: http://www.scielo.br/pdf/reeusp/v43n2/en_a11v43n2.pdf
- 5. Champion HR. Trauma scoring. Scand J Surg. 2002;91(1):12-22.
- 6. Gennari TD, Koizumi MS. Determinação do nível de gravidade do trauma. Rev Saúde Pública. 1995;29(5):333-41.
- 7. Frankema SP, Steyerberg EW, Edwards MJ, van Vugt AB. Comparison of current injury scales for survival chance estimation: an evaluation comparing the predictive performance of the ISS, NISS, and AP scores in a Dutch local trauma registration. J Trauma. 2005;58(3):596-604.
- 8. Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW Jr, et al. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356-65.
- 9. Osler TM, Rogers FB, Badger GJ, Healey M, Vane DW, Shackford SR. A simple mathematical modification of TRISS markedly improves calibration. J Trauma. 2002;53(4):630-4.
- 10. Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43(6):922-5.
- 11. Tay SY, Sloan EP, Zun L, Zaret P. Comparison of the New Injury Severity Score and the Injury Severity Score. J Trauma. 2004;56(1):162-4.
- 12. Brenneman FD, Boulanger BR, McLellan BA, Redelmeier DA. Measuring injury severity: time for a change? J Trauma . 1998;44(4):580-2.
- 13. Sutherland AG, Johnston AT, Hutchison JD. The new injury severity score: better prediction of functional recovery after muscoloskeletal injury. Value Health. 2006;9(1):24-7.
- 14. Harwood PJ, Giannoudis PV, Probst C, Van Griensven M, Krettek C, Pape HC, et al. Which AIS based scoring system is the best predictor of outcome in orthopaedic blunt trauma patients? J Trauma. 2006;60(2):334-40.
- 15. Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The New Injury Severity Score: a more accurate predictor of in-hospital mortality than the Injury Severity Score. J Trauma. 2004;56(6):1312-20.
- 16. Whitaker IY, Gennari TD, Whitaker AL. The difference between ISS and NISS in a series of trauma patients in Brazil. Annu Proc Assoc Adv Automot Med. 2003;47:301-9.
- 17. Husum H, Strada G. Injury Severity Score versus New Injury Severity Score for penetrating injuries. Prehospital Disaster Med. 2002;17(1):27-32.
- 18. Aydin SA, Bulut M, Ozgüç H, Ercan I, Türkmen N, Eren B, et al. Should the New Injury Severity Score replace the Injury Severity Score in the Trauma and Injury Severity Score? Ulus Travma Acil Cerrahi Derg. 2008;14(4):308-12.
- 19. Fraga GP, Mantovani M, Magna LA. Índices de trauma em pacientes submetidos à laparotomia. Rev Col Bras Cir. 2004;31(5):299-306.
- 20. Moini M, Rezaishiraz H, Zafarghandi MR. Characteristics and outcome of injured patients treated in urban trauma centers in Iran. J Trauma. 2000;48(3):503-7.
- 21. Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The Injury Severity Score or the New Injury Severity Score for predicting intensive care unit admission and hospital length of stay? Injury. 2005;36(4):477-83.
- 22. Davis EG, MacKenzie EJ, Sacco WJ, Bain LW Jr, Buckman RF Jr, Champion HR, et al. A new "TRISS-Like" probability of survival model for intubated trauma patients. J Trauma. 2003;55(1):53-61.
Correspondence addressed to:
Publication Dates
-
Publication in this collection
12 Jan 2012 -
Date of issue
Dec 2011
History
-
Accepted
21 Mar 2011 -
Received
06 Sept 2010