Abstracts
Endometriosis is characterized by the presence of normal endometrial tissue outside the uterine cavity. In patients with deep pelvic endometriosis, uterosacral ligaments, rectum, rectovaginal septum, vagina or bladder may be involved. Clinical manifestations may be variable, including pelvic pain, dysmenorrhea, dyspareunia, urinary symptoms and infertility. Complete surgical excision is the gold standard for treating this disease, and hence the importance of the preoperative work-up that usually is limited to an evaluation of sonographic and clinical data. Magnetic resonance imaging is of paramount importance in the diagnosis of endometriosis, considering its high accuracy in the identification of lesions intermingled with adhesions, and in the determination of peritoneal lesions extent. The present pictorial review describes the main magnetic resonance imaging findings in deep pelvic endometriosis.
Magnetic resonance imaging; Endometriosis; Female pelvis; Infertility
A endometriose caracteriza-se pela presença de tecido endometrial funcionante heterotópico. Em pacientes com endometriose pélvica profunda pode haver acometimento dos ligamentos útero-sacros, reto, septo retovaginal, vagina ou bexiga. Os sintomas podem ser variados e incluem dor pélvica, dismenorréia, dispareunia, sintomas urinários e infertilidade. O padrão-ouro para o tratamento é a ressecção completa dessas lesões. Assim, é muito importante a avaliação pré-operatória dessas pacientes, sendo esta avaliação, em geral, limitada em relação aos dados clínicos e ultra-sonográficos. A ressonância magnética tem grande importância no diagnóstico da endometriose, principalmente por permitir a identificação das lesões de permeio a aderências e a avaliação da extensão das lesões subperitoneais. Neste estudo são ilustrados, na forma de ensaio iconográfico, os principais achados da endometriose pélvica profunda à ressonância magnética.
Imagem por ressonância magnética; Endometriose; Pelve feminina; Infertilidade
ICONOGRAPHIC ESSAY
Magnetic resonance imaging in deep pelvic endometriosis: iconographic essay*
Antonio Carlos Coutinho JuniorI; Cláudio Márcio Amaral de Oliveira LimaII; Elisa Pompeu Dias CoutinhoI; Érica Barreiros RibeiroII; Marisa Nassar AidarIII; Emerson Leandro GasparettoIV
IMDs, Radiologists at Clínica de Diagnóstico por Imagem (CDPI) and Clínica MultiImagem, Rio de Janeiro, RJ, and Centro de Diagnóstico por Imagem Fátima, Nova Iguaçu, RJ, Brazil
IIMDs, Trainees at Clínica de Diagnóstico por Imagem (CDPI) and Clínica MultiImagem, Radiologists at Hospital Naval Marcílio Dias, Rio de Janeiro, RJ, Brazil
IIIMD, Radiologist at Clínica de Diagnóstico por Imagem (CDPI) and Clínica MultiImagem, Rio de Janeiro, RJ, Brazil
IVAssociate Professor of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Radiologist at Clínica de Diagnóstico por Imagem (CDPI) and Clínica MultiImagem, Rio de Janeiro, RJ, Brazil
Mailing address
ABSTRACT
Endometriosis is characterized by the presence of normal endometrial tissue outside the uterine cavity. In patients with deep pelvic endometriosis, uterosacral ligaments, rectum, rectovaginal septum, vagina or bladder may be involved. Clinical manifestations may be variable, including pelvic pain, dysmenorrhea, dyspareunia, urinary symptoms and infertility. Complete surgical excision is the gold standard for treating this disease, and hence the importance of the preoperative workup that usually is limited to an evaluation of sonographic and clinical data. Magnetic resonance imaging is of paramount importance in the diagnosis of endometriosis, considering its high accuracy in the identification of lesions intermingled with adhesions, and in the determination of peritoneal lesions extent. The present pictorial review describes the main magnetic resonance imaging findings in deep pelvic endometriosis.
Keywords: Magnetic resonance imaging; Endometriosis; Female pelvis; Infertility.
INTRODUCTION
Firstly described in 1860 by Von Rokitansky(1), endometriosis is defined as the presence of functional endometrial tissue outside the endometrial cavity and myometrium(2,3). Endometriosis is a frequent disease attributed to multifactorial causes, affecting 7% to 10% of women in the general population(3,4). The most widely accepted theory is that viable endometrial cells originating from a physiological phenomenon called retrograde menstruation, result in implantation into the peritoneal cavity (Sampson's theory)(2,57). Studies in the literature report a wide range of factors of individual risk such as low parity, age, ethnic origin, height, body mass index, alcohol abuse, tobacco smoking, among others(8).
The significant role of MRI in the diagnosis of endometriosis is related to the identification of intermingled lesions in the presence of adhesions, and also the demonstration and evaluation of subperitoneal lesions extent in cases where these lesion cannot be visualized by laparoscopy, with accuracy, sensitivity and specificity > 90% for deep endometriosis(9,10). MRI findings are more specific than those of ultrasonography and computed tomography(8,9,1113).
Generally, endometriosis implants are confined to the pelvis, the most common sites, in order of decreasing frequency, being ovaries, broad ligaments, anterior and posterior culdesac, and uterosacral ligaments; however, distant sites may be involved(2,4,7,9). Endometrial tissue implants are affected by cyclic menstrual changes with periodic bleedings. Hemorrhage inside these implants induces an acute pelvic inflammatory reaction and consequential adhesions development, frequently with Douglas culdesac obliteration, Fallopian tubes and ovaries distortion.
In patients with deep pelvic endometriosis, by definition, there is a subperitoneal ³ 5 mm penetration by endometrial implant. Deep endometriosis generally is found in the retrovaginal septum, rectum, bladder and other pelvic fibromuscular structures such as uterine ligaments and vagina(4,7,8). Despite the asymptomatic nature of the disease in many women affected by peritoneal endometriosis, patients with deep pelvic endometriosis may present with pelvic pain, dysmenorrhea, dyspareunia, urinary symptoms and infertility(2,5,6). MRI presents the advantage of fast acquisition of multiplanar sequences, providing simultaneous images of all the pelvic viscera both at rest and under stress(11,12). Despite some limitations, MRI plays a significant role in the diagnosis of endometriosis, especially for allowing the identification of intermingled lesions in the presence of dense adhesions, and evaluation of subperitoneal lesions extent(4,13,14). In the evaluation of deep endometriosis, MRI presents accuracy, sensitivity and specificity > 90%(13,14). In the present iconographic essay, main MRI findings in deep pelvic endometriosis are described.
MRI PROTOCOLS
The acquisition of appropriate magnetic resonance images for evaluating patients with suspected deep pelvic endometriosis must follow specific protocols. In our clinics, the examination is performed during menses, with a full bladder. Additionally, immediately before the examination, a venous antispasmodic agent (dipyrone, scopolamine butylbromide) is administered and, most recently, vaginal (50 ml) and rectal (100 ml) aqueous gel introduction has been adopted.
The protocol includes the following sequences: axial T1weighted, and sagittal, coronal and axial T2weighted; and, after intravenous gadolinium injection, axial, fatsuppressed T1weighted sequences.
MRI FINDINGS
Imaging findings on MRI of patients with deep pelvic endometriosis depend on the type of the lesion: small infiltrative endometrial implants, deep, solid lesions and visceral endometriosis involving the rectal and vesical walls(4).
MRI may be a limited method in cases where the endometriosis presents with small infiltrative implants. Especially in cases where the lesions are visualized as whitish foci at laparoscopy, MRI may be negative. However, in some patients hyperintense foci may be characterized on fatsuppressed T1weighted sequences, representing small areas of hemorrhage(4,13,14) (Figure 1).
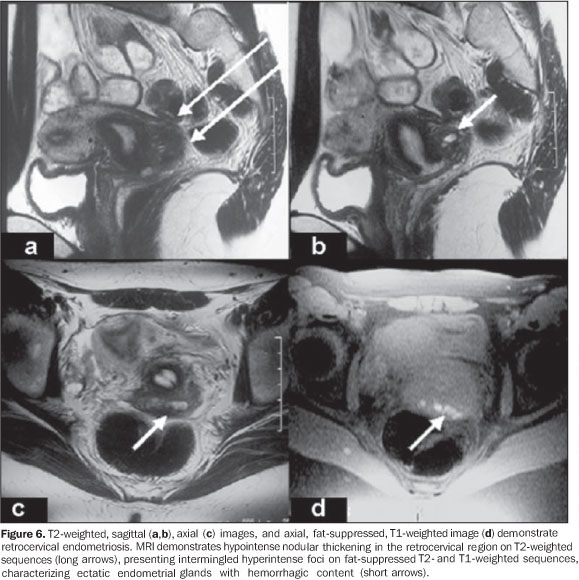
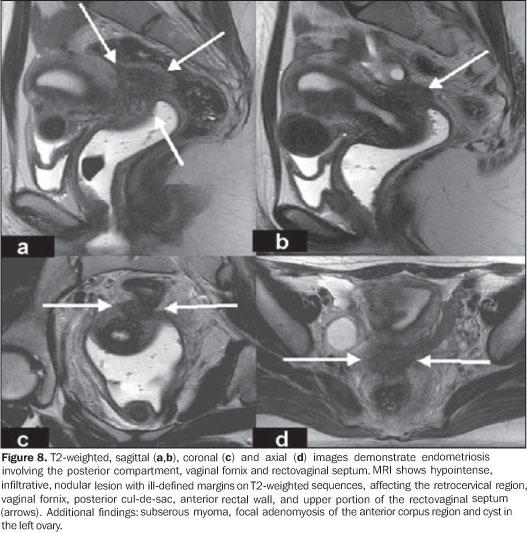
At MRI, deep, solid lesions affecting the posterior culdesac (Figure 2) present low to intermediate intensity signal, with further hyperintense foci on fatsuppressed (blood) T1weighted images, hyperintense signal on T2weighted images with variable contrastenhancement after intravenous gadolinium injection. Hypersignal foci on T1weighted images result from ectatic endometrial glands with hemorrhagic content surrounded by fibrotic tissue. The extensive fibrosis component (Figure 3) generally characterized in the histological study of these lesions is responsible by the variable postcontrastenhancement(4,7). Some foci of endometriosis localized in the Douglas culdesac (Figure 4) may present with abundant glandular component with a mild fibrotic reaction. In these cases, high signal intensity is observed on T1weighted images, and variable signal intensity on t2weighted images, with the solid glandular component demonstrating variable contrastenhancement after gadolinium injection(4,8,14). In cases where the uterosacral ligaments are involved (Figure 5), subtle signal intensity alterations are found at MRI; findings such as bilateral or asymmetrical thickening and nodularity within these ligaments should be taken into consideration(4,8,14).
MRI may demonstrate focal or diffuse vesical involvement by endometriosis (Figure 6). The majority of patients present focal areas of parietal thickening with eventual hypersignal foci on fatsuppressed T1weighted images. Invasion of the mucosa is not frequent in cases of vesical endometriosis and MRI can demonstrate alterations even in cases of asymptomatic patients with normal cystoscopy(4,8,13).
MRI sensitivity in the diagnosis of endometriosis with rectal involvement is relatively low, because of artifacts associated with the rectal content. In our practice, vaginal and rectal introduction of aqueous gel immediately before the examination may improve the MRI accuracy in the evaluation of rectal and retrocervical lesions (Figure 7), lesions in the rectovaginal septum (Figure 8), and in the vaginal wall. Rectal involvement generally is demonstrated by MRI as a parietal thickening with hypointense signal on T2weighted images. Hyperintense hemorrhagic foci may be identified on fatsuppressed T1weighted images(4,7,8,13).
CONCLUSION
In patients with deep pelvic endometriosis, clinical and sonographic results may be normal or poorly elucidative, difficulting the diagnosis determination. In these cases, MRI is essential for an accurate differential diagnosis. MRI can evaluate areas otherwise inaccessible by laparoscopy, identifying and evaluating the extent of lesions in the subperitoneal region and in the presence of dense adhesions. Because of its multiplanar capacity and excellent tissue characterization, MRI plays an essential role in the preoperative evaluation of patients with deep pelvic endometriosis.
ACKNOWLEDGEMENTS
The authors thank Dr. Cláudio Crispi, for kindly letting the author have the material utilized in the present study.
REFERENCES
- 1. Craig V. Endometriosis of the urinary tract. Urol Clin North Am. 2002;29:62535.
- 2. Brandão A. Endometriose. In: Brandão A, Werner Jr H, Daltro P, editores. Ressonância magnética em obstetrícia e ginecologia. Rio de Janeiro: Revinter; 2003. p.13350.
- 3. Kuligowska E, Deeds L, Lu K. Pelvic pain: overlooked and underdiagnosed gynecologic conditions. Radiographics. 2005;25:320.
- 4. Frate CD, Girometti R, Pittinno M, et al. Deep retroperitoneal pelvic endometriosis: MR imaging appearance with laparoscopic correlation. Radiographics. 2006;26:170518.
- 5. Zacharia TT, O'Neill MJ. Prevalence and distribution of adnexal findings suggesting endometriosis in patients with MR diagnosis of adenomyosis. Br J Radiol. 2006;104:3037.
- 6. Crosignani P, Olive D, Bergqvist A, et al. Advances in the management of endometriosis: an update for clinicians. Hum Reprod. 2006;12: 17989.
- 7. Bazot M, Darai E, Hourani R, et al. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology. 2004;232:37989.
- 8. Woodward PJ, Sohaey R, Mezzetti Jr TP. Endometriosis: radiologicpathologic correlation. Radiographics. 2001;21:193216.
- 9. Olive DL, Schwartz LB. Endometriosis. N Engl J Med. 1993;328:175969.
- 10. Wykes CB, Clark TJ, Khan KS. Accuracy of laparoscopy in the diagnosis of endometriosis: a systematic quantitative review. Br J Obstet Gynaecol. 2004;111:120412.
- 11. Francisco VV, D'Ippolito G, Silva GPA, et al. Prevalência de artefatos em exames de ressonância magnética do abdome utilizando a seqüência GRASE: comparável com as melhores seqüências rápidas? Radiol Bras. 2005;38:3238.
- 12. Bezerra MRL, Soares AFF, Faintuch S, et al. Identificação das estruturas músculoligamentares do assoalho pélvico na ressonância magnética. Radiol Bras. 2001;34:3236.
- 13. Kinkel K, Chapron C, Balleyguier C, et al. Magnetic resonance imaging characteristics of deep endometriosis. Hum Reprod. 1999;14:10806.
- 14. Kataoka ML, Togashi K, Yamaoka T, et al. Posterior culdesac obliteration associated with endometriosis: MR imaging evaluation. Radiology. 2005;234:81523.
Publication Dates
-
Publication in this collection
13 May 2008 -
Date of issue
Apr 2008
History
-
Received
09 Aug 2007 -
Accepted
11 Sept 2007