Abstracts
OBJECTIVE: To determine whether the addition of discharge standard illustrated cards improves understanding of patients in the emergency room. METHODS: We conducted a prospective, randomized, interventional study with 228 patients discharged from the emergency department. All patients were interviewed and tested for the level of understanding of discharge instructions. Some of them received the intervention, with the standard cards, and another did not, constituting the control group. RESULTS: The average of followed discharge guidelines of the group that received the cards was higher than the control group, with statistical significance (p=0.009). When segregated by age, the group between 16 and 35 years of both sexes had the best average of followed guidelines, statistically, than the average of the control group (p=0.01). The difference between the mean orientations between the control group and the card for patients undergoing procedures was statistically significant (p=0.02); as for the stratification according to the number of procedures, the significance increases when that is equal to 1 (p=0.001) and decreased the more procedures were carried out. CONCLUSION: The introduction of discharge standard orientation cards was associated with improvement in the understanding of patients. Without replacing the verbal directions, which establishes dialogue and doctor-patient bonding, cards appear as auxiliary elements, facilitating understanding and care guidelines.
Patients; Wounds and injuries; Emergency medical services; Comprehension; Patient discharge
OBJETIVO: determinar se a adição de cartões padronizados de alta ilustrados melhora a compreensão dos pacientes do pronto socorro. MÉTODOS: estudo prospectivo, randomizado e intervencionista com uma amostra de 228 pacientes que receberam alta do pronto socorro. Todos os pacientes foram entrevistados e testados quanto ao grau de compreensão das orientações de alta, sendo que uma parte havia recebido a intervenção com cartões padronizados e outra não, constituindo o grupo controle. RESULTADOS: a média de orientações domiciliares do grupo que recebeu o cartão de alta foi superior ao do grupo controle, com significância estatística de p=0,009. Se fracionado tal dado segundo faixas etárias, aquela compreendida entre 16 e 35 anos, para ambos os sexos, foi a qual a média de orientações do grupo com o cartão é melhor, estatisticamente, do que a média do grupo controle (p=0,01). A diferença entre as médias de orientações entre o grupo controle e o cartão para os pacientes submetidos a procedimentos foi significativa estatisticamente (p= 0,02) e em uma estratificação segundo o número de procedimentos, a significância aumenta quando aquele é igual a 1 (p=0,001) e diminui quanto mais procedimentos são realizados. CONCLUSÃO: A instituição de cartões de alta padronizados foi associada com a melhoria na compreensão dos pacientes. Sem substituir as orientações verbais, que estabelecem o diálogo e a aproximação médico-paciente, os cartões figuram como elementos auxiliares, facilitando as orientações e entendimento do cuidado.
Pacientes; Ferimentos e lesões; Serviços médicos de emergência; Compreensão; Alta do paciente
ORIGINAL ARTICLE
IResident, General Surgery, Júlio de Mesquita Filho São Paulo State University
IIMedical School Graduate, UFPR
IIIAssistant Professor, Discipline of Trauma, UFPR
IVAssistant Professor, Discipline of Trauma, UFPR; General Director, Clinics Hospital, UFPR
VAssistant Professor, Discipline of Trauma, UFPR; Chief, Surgery Service; Academic Director, Workers Hospital
Address correspondence to
ABSTRACT
OBJECTIVE: To determine whether the addition of discharge standard illustrated cards improves understanding of patients in the emergency room.
METHODS: We conducted a prospective, randomized, interventional study with 228 patients discharged from the emergency department. All patients were interviewed and tested for the level of understanding of discharge instructions. Some of them received the intervention, with the standard cards, and another did not, constituting the control group.
RESULTS: The average of followed discharge guidelines of the group that received the cards was higher than the control group, with statistical significance (p=0.009). When segregated by age, the group between 16 and 35 years of both sexes had the best average of followed guidelines, statistically, than the average of the control group (p=0.01). The difference between the mean orientations between the control group and the card for patients undergoing procedures was statistically significant (p=0.02); as for the stratification according to the number of procedures, the significance increases when that is equal to 1 (p=0.001) and decreased the more procedures were carried out.
CONCLUSION: The introduction of discharge standard orientation cards was associated with improvement in the understanding of patients. Without replacing the verbal directions, which establishes dialogue and doctor-patient bonding, cards appear as auxiliary elements, facilitating understanding and care guidelines.
Key words: Patients. Wounds and injuries. Emergency medical services. Comprehension. Patient discharge.
INTRODUCTION
The emergency department of a hospital is that more congested and critic, since it is has a high demand of patients, multiple tasks, large team and proportionally less time for decision making 1. Factors such as attending time, discontinuity of care, lack of privacy, noise and stressful nature of emergency care alter the logic of the doctorpatient relations 2. Therefore, it is a unique, dynamic and complex environment, and as such it has been considered a place prone to errors and target complaints of malpractice 3. Studies such as the Harvard Medical Practice Study reported that approximately 1.5% to 3.0% adverse effects of treatments occur in emergency rooms. More importantly, they concluded that the emergency department is the one that has the highest proportion of errors considered preventable 4.
The importance of providing adequate instruction and guidance on discharge of patients is well understood when it is recognized that such questions are part of the patients' future therapeutic plan 1. However, there is evidence that the information given to patients in the hospital is not enough. Vilke et al. 5 reported that only 39% of patients knew when to take prescribed medications, and only 24% did so in the proper dosage. Engel et al. 6 interviewed patients who were discharged from an emergency department and found that 78% of them demonstrated a poor understanding of discharge instructions. Studies conducted by Crane at Kern Medical Center in Bakersfield, California (USA), assumed that one quarter of patients did not understand any fundamental point of discharge instructions and that the rest of the group, according to the questionnaire, did not understand 1/3 of the information necessary for care after discharge2. In order to analyze the degree of understanding of the diagnosis and management of patients seen in the ER, we found that most of them could correctly report the diagnosis and days off work, however a significant rate of these patients was not able to reference the type and duration of treatment.
This scenario occurs simultaneously with the need for a more active participation of patients in treatment decisions and health care. As a result, the information provided to patients should be a central part of care7. Informed patients are proportionately less anxious and more secure and therefore handle the disease more successfully and adhere to the treatment plan, which is reflected in the health and well being in general. Also, another benefit of information is the ability to help patients use health services effectively, making them more satisfied with the provided service 1.
Many modes of intervention to improve understanding of patients have been suggested. The most basic and crucial, however, is the mandatory inclusion of verbal and written discharge instructions containing specific information about diagnosis, therapy and monitoring. Vukmir et al. 8 suggested the use of "computerized compositions" to avoid the "subjectivity of manuscripts" and the possibility of illegibility of information; Jolly et al.9 proposed a simplification of standardized discharge instructions for better understanding of patients: clear language, short sentences and "small" words. Austin et al. 10 included illustrations in the written discharge instructions, in order to cover the portion of the population with less literary skill. The reported results showed that the group of patients who were discharged with illustrated instruction cards displayed scores 1.5 times better than the group that received instructions without illustrations. Finally, Roberts et al. 11 suggested the printing of discharge guidance on colored paper to help patients not to lose the instructions, and the card should explain the diagnosis, measures taken in the emergency department, the name of the attending physician for specific instructions on activities and medications, prognosis, when and where will the monitoring take place and the warning symptoms and signs to return to the emergency department.
The hospital discharge is a period of vulnerability for the patient, since it marks a transition between the professional assistance and home self-management 12. As important as recognizing such particularity is to understand the discharging process as a key step in medical care. Although not the only time to inform and teach, it is a critical stage to summarize the procedures, provide a diagnosis and recommend a treatment plan and follow-up. For the patient it is the final opportunity to formulate questions and clarify concerns 13.
The person responsible for discharge should be effective in three main areas: communication of crucial information, confirmation of understanding and identification of areas of confusion or misunderstandings 12. There are factors, however, which hinder the practice of this theory in the emergency department. Unmanageable labor demand, overcrowding, simultaneous calls to multiple patients, high levels of uncertainty, constrained time, absence of a prolonged doctor-patient relationship and of feedback from care outcomes are among the major obstacles 14.
Studies with methodology similar to ours, ie, a final interview with the patients after the procedures of discharge, found that many had difficulties to summarize the care to which they were subjected, and to reproduce the guidelines given to them, even when they carried a Discharge card model 2,6,15.
The aim of this study was to assess the degree of understanding of the guidelines for discharge of patients from the emergency department immediately after receiving them; to institute, together with verbal directions, a card with written and illustrated instructions; and, ultimately, to show the effects of the method in the immediate understanding of patients.
METHODS
The Emergency Room of Workers Hospital (PS-HT) in Curitiba, State of Paraná, operates in a dual mechanism for admitting patients: spontaneous demand and referenced (SIATE/SAMU). On the initial care of these patients there is active participation of medical students from the third year on. They are supervised by the residents and Surgery and Orthopedics staff heads, who have the say on therapeutic decisions and discharge. The orientations are provided to patients by the students.
This was a prospective, interventional study with approval by the Ethics in Research Committee of the Workers Hospital (CEP-SESA/HT No 507 /2012), which waived the application of informed consent to patients.
The study included patients who communicated in Portuguese, who consented to participate and did not require hospitalization greater than 24 hours. We excluded those under the age of 16 years, demented, not speaking Portuguese, admitted to the hospital for more than 24 hours and those who refused to answer the questionnaire.
The intervention process was structured in two stages. The first consisted of a questionnaire to patients willing to respond immediately after discharge, through a live interview conducted by the research team, in order to assess the level of understanding of discharge instructions. The questionnaire collected information about the study sample (gender, age and education level) and tested the ability of patients to mention what was their diagnosis, procedures performed, understanding of prescriptions, other guidelines, who provided most of the information and what were the directions given on outpatient or reference units 2.
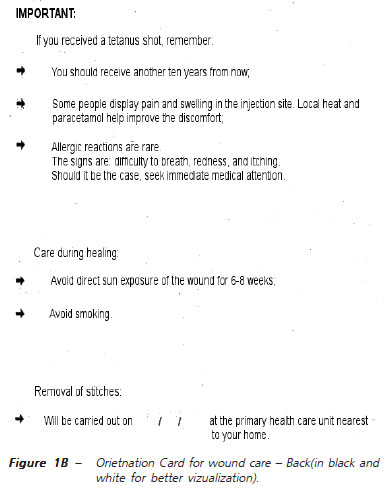
The second stage of the project was developed after the intervention. Models of guidance discharge cards were developed (Figures 1A and 1B), free of medical jargon, with objective language, illustrated and printed on colored paper, which were first explained to the medical students at the beginning of the shift on randomly chosen days of the survey period, so they could have enough ability to guide patients to allow proper written and verbal discharge instructions 8-11. Once this phase of the project was held, we proceeded to reapplication of the questionnaire, the same way as in the first stage, to the patients who received the new mode of guidance for assessing the impact of the intervention.
The data collected were subjected to statistical tests adjusted to a model of analysis of variance (ANOVA) 16. Descriptive statistics were used to assess demographics and the Student t and Z tests were applied for comparison of groups when appropriate. The level of significance was p d" 0.05.
RESULTS
The sampled comprised 228 patients, 80 women and 148 men. The age group that demanded the highest number of visits to the ER was the 16-35 years, accounting for 58% of the study population. Most patients (33%) stated 11 years of schooling, which is equivalent to completion of high school.
The most prevalent mechanism of injury was fall from height (30%). The most frequent diagnosis was contusion (29%), followed by bone fracture (15%) and laceration (14%). When asked, 17% of patients were unaware of the diagnosis, 59% of patients underwent only one procedure, this latter being mainly radiographic examination. As for procedures that require greater home care, 27 (12%) patients had sutured skin, 24 (11%) received immobilization, and three (1%) patients required both.
As for prescriptions, 91% of patients were instructed to take medication at home, 56% of them considering the prescription legible. As for the name of prescription drugs, 56% reported drug names correctly, 9% incorrectly and 26% were unaware of such information. Only 17% ignored the purpose of the prescribed medication; 88% could not mention any adverse reaction to the medication prescribed. Regarding the responsible for providing the discharge guidelines, 44% of patients indicated the doctor, 11% the medical student, 7% the nursing staff members and 35% were unaware of the position of the person who last directed them. Only 10% of patients expressed doubts about their care at the end of the interview.
Of the 228 patients, 139 of them (61%), constituting the control group, were discharged from the ER according to routine procedures and 89 (39%) received the instruction card during discharge, forming the other study group.
The average household guidelines of the control group was 1.2 and the average group card, 1.6. The change was statistically significant with p = 0.009 (Figures 2 and 3).
A comparison of the averages of discharge guidelines by age and gender showed no statistically significant difference when using the entire sample. However, if such fractionated averages were compared between the card and control group, there was a statistically significant difference (p = 0.01) for the age group 16-35 years in both genders, with higher means of orientations in the card group (Figures 4 and 5). For the other age groups the mean difference in orientation was not statistically significant, regardless of superiority of one group over another.
The difference between the mean orientations between the control group and the card one for patients undergoing procedures was statistically significant (p = 0.02) and in a stratification according to the number of procedures the significance increased when that was equal to 1 (p = 0.001) and decreased the more procedures were carried out.
The average orientation of the card group (95%CI 1.17-2.03) was higher than the control group (95%CI 0.972.03) when the procedure was cast immobilization, but without statistical significance. The same was true when comparing the averages for the suturing procedure.
DISCUSSION
Our results show that 17% of patients did not know their diagnosis. As with the previously published results by Kerzman et al. 17, most of our patients could correctly report the purpose of the prescription. However, a large number of them showed little knowledge about the name of drugs and adverse reactions.
The patients in the emergency room of a Spanish hospital easily identified Professional titles in 68.9% of cases 18. In this study, 35% of patients did not know which professional was responsible for their discharge, and from the 65% answered, many confused students with physicians or nursing staff members.
The difficult understanding of patients regarding discharge guidance is consistent with the results obtained in this study, as the average household guidelines of both the group that received the discharge card and the control one is unsatisfactory to ensure a good self-management, despite the statistical significance.
In the analysis of paired data, however, using the same diagnosis and considering a card and a control group, the inclusion of handling card to the patients in the process was of high relevance. The card has standardized discharge guidelines and served as a check list for those who applied it; the simple discharge card reading demanded potentially more time with the patient, which increased the opportunity of better guidance, diverging from a recent study that showed that the average discharge time was 76 seconds, and less than 65% of the time was spent on home care management guidelines 19.
A study of patients from an emergency room pointed out that printed discharge instructions were written to be intelligible to people with at least eleven years of study 20. Based on this premise, we developed the discharge cards with simple language and illustrations, which may have played a beneficial role, since 93% of our study population reported eleven years or less of schooling.
The use of discharge cards was better for patients undergoing only one procedure and the significance of the finding was progressively decreased as more procedures were added to the service. A plausible explanation is that more complex cases require more care and attention on the part of patients. A study of China and Thailand reported that some patients felt pressured or anxious when they had to show a greater amount of knowledge during the final interview 21.
Clark et al. 22 designed a study on the information wishes of patients about the hospital. Management of symptoms, when and where to seek help and continuity of care are examples. However, Isaacman et al. 23 found that less than half of the patients could repeat such information soon after discharge. Moreover, 90% of our patients had no doubts to be clarified, despite the low performance when asked about key aspects of the discharge. This fact can be justified, a priori, by the lack of bond between emergency service staff and the patient, as well as the persistence of the asymmetry of the doctor-patient and hospital-pharmacy relations (in which the patient still hesitate in the presence of the doctor and culturally accepts the pharmacy attendant at the prescription supervisor). In addition to this, Rhodes et al. 19 analyzed recorded audios of discharge instructions, in which only 16% of patients were asked about the existence of doubts and none of the patients had a confirmed understanding by the responsible for discharge.
The successful communication of discharge information is critical, since comprehension deficits can result in risks to the patient. Among these, inappropriate home care, including the misuse of medication, failure to identify the warning signs and loss of follow-up 12.
Efforts to improve communication have therefore a positive influence on emotional health, symptom resolution and recovery of functional status. The high quality of instruction can maximize patient adherence to prescriptions, optimize self-care and avoid complications. Such quality is closely related to patient satisfaction with the emergency department 13. A multivariate analysis revealed that the best predictor of satisfaction with the ER, despite the waiting time for the service, is how satisfied they are with interpersonal relationships with physicians and the multidisciplinary team 24.
This study has some limitations. The card consisted of a set of instructions, but even with the most complete guidance, the patient may have a poor understanding. In an attempt to compensate for it, verbal instructions were added, but depended on the flexibility and consistency of the interlocutor. The sample size may have reduced power to show differences between the variables and, furthermore, the interviewers were not blinded as to a patient belonging to one group or the other, enabling measurement bias. However, the inclusion of standard discharge cards was associated with improvement in the understanding of patients. Without replacing the verbal directions, which establish dialogue and doctorpatient bonding, cards appear as auxiliary elements, facilitating understanding of the guidelines and care, as well as contributing to health education.
The components of the health team and training students should be instructed to identify themselves to patients when they have contact with them, to avoid possible deficits in understanding the roles and responsibilities in a health team.
Acknowledgements
We thank Kássio Days Nery in particular for the dedication and commitment in illustrating our cards in record time; Dayane Raquel Paula for her invaluable aid; Eder David Borges da Silva for readiness and solicitude in doing statistical analysis of the work, despite other commitments; and Wagner Bonato for helping us to understand all the data from the perspective of significance.
REFERENCES
- 1. Bulut H, Tanrikulu G, Dal Ü, Kapucu S. How much do ED patients know about medication prescribed for them on discharge? A pilot study in Turkey. J Emerg Nurs. 2009. [Epub ahead of print]
- 2. Crane JA. Pacient comprehension of doctor-pacient communication on discharge from the emergency department. J Emerg Med. 1997;15(1):1-7.
- 3. Yu KT, Green RA. Critical aspects of emergency department documentation and communication. Emerg Med Clin Nor Am. 2009;27(4):641-54.
- 4. Leape LL, Brennan TA, Laird N, Lawthers AG, Localio R, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377-84.
- 5. Vilke GM, Marino A, Iskander J, Chan TC. Emergency department patient knowledge of medications. J Emerg Med. 2000;19(4):327-30.
- 6. Engel KG, Heisler M, Smith DM, Robinson CH, Forman JH, Ubel PA. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med. 2009;53(4):454-61.
- 7. Moret L, Rochedreux A, Chevalier S, Lombrail P, Gasquet I. Medical information delivered to patients: discrepancies concerning roles as perceived by physicians and nurses set against patient satisfaction. Patient Educ Couns. 2008;70(1):94-101.
- 8. Vukmir RB, Kremen R, Ellis GL, DeHart DA, Plewa MC, Menegazzi J. Compliance with emergency department referral: the effect of computerized discharge instructions. Ann Emerg Med. 1993;22(5):819-23.
- 9. Jolly BT, Scott JL, Sanford SM. Simplification of emergency department discharge instructions improves patient comprehension. Ann Emerg Med. 1995;26(4):443-6.
- 10. Austin PE, Matlack R 2nd, Dunn KA, Kesler C, Brown CK. Discharge instructions: do illustrations help our patients understand them? Ann Emerg Med. 1995;25(3):317-20.
- 11. Roberts JR. ED discharge instructions: another chance to help patients and prove your worth. Emerg Med News. 2006;28(1):17-20.
- 12. Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012;60(2):152-9.
- 13. Vashi A, Rhodes KV. "Sign right here and you're good to go": a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315-22.
- 14. Einsenberg E, Murphy A, Sutcliffe K, Wears R, Schenkel S, Perry S, et al. Communication in emergency medicine: implications for patient safety 1. Communic Monogr. 2005;72(4):390-413.
- 15. Logan PD, Schwab RA, Salomone JA 3rd, Watson WA. Patient understanding of emergency department discharge instructions. South Med J. 1996;89(8):770-4.
- 16. Cox DR. Planning of experiments. 12Ş ed. Michigan:Wiley; 1992.
- 17. Kerzman H, Baron-Epel O, Toren O. What do discharged patients know about their medication? Patient Educ Couns. 2005;56(3):276-82.
- 18. Ruiz Romero V, Fajardo Molina J, García-Garmendia JL, Cruz Villalón F, Rodríguez Ortiz R, Varela Ruiz FJ. Satisfacción de los pacientes atendidos en el Servicio de Urgencias del Hospital San Juan de Dios del Aljarafe. Rev Calid Asist. 2011;26(2):111-22.
- 19. Rhodes KV, Vieth T, He T, Miller A, Howes DS, Bailey O, Walter J, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44(3):262-7.
- 20. Spandorfer JM, Karras DJ, Hughes LA, Caputo C. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995;25(1):71-4.
- 21. Sugarman J, Corneli A, Donnell D, Liu TY, Rose S, Celentano D, et al. Are there adverse consequences of quizzing during informed consent for HIV research? J Med Ethics. 2011;37(11):693-7.
- 22. Clark PA, Drain M, Gesell S, Mylod DM, Kaldenberg DO, Hamilton J. Patient perceptions of quality in discharge instruction. Patient Educ Couns. 2005;59(1):56-68.
- 23. Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: do they improve communication of discharge information from the emergency department? Pediatrics. 1992;89(6 Pt 2):1204-8.
- 24. Boudreaux ED, O'Hea EL. Patient satisfaction in the emergency departament: a review of the literature and implications for practice. J Emer Med. 2004;26(1):13-26.
Guidelines for discharge: do standardized cards help in patient understanding?
Publication Dates
-
Publication in this collection
29 Oct 2013 -
Date of issue
Aug 2013
History
-
Received
16 Aug 2012 -
Accepted
20 Oct 2012