ABSTRACT
Objective:
to compare the outcome of liver transplantation for hepatocarcinoma in submitted or not to locoregional treatment and downstaging regarding survival and risk of recurrence in transplant waiting list patients.
Methods:
retrospective study of patients with hepatocarcinoma undergoing liver transplantation in the metropolitan region of São Paulo, between January 2007 and December 2011, from a deceased donor. The sample consisted of 414 patients. Of these, 29 patients were included in the list by downstaging. The other 385 were submitted or not to locoregional treatment.
Results:
the analysis of 414 medical records showed a predominance of male patients (79.5%) with average age of 56 years. Treatment of the lesions was performed in 56.4% of patients on the waiting list for transplant. The most commonly used method was chemoembolization (79%). The locoregional patients undergoing treatment had a significant reduction in nodule size greater (p<0.001). There was no statistical difference between groups with and without locoregional treatment (p=0.744) and on mortality among patients enrolled in the Milan criteria or downstaging (p=0.494).
Conclusion:
there was no difference in survival and recurrence rate associated with locoregional treatment. Patients included by downstaging process had comparable survival results to those previously classified as Milan/Brazil criteria.
Keywords:
Liver; Liver Transplantation; Liver Neoplasms
RESUMO
Objetivo:
comparar o resultado do transplante de fígado por hepatocarcinoma em pacientes submetidos ou não ao tratamento loco-regional e downstaging, em relação à sobrevida e risco de recidiva na fila de transplante.
Métodos:
estudo retrospectivo dos pacientes portadores de hepatocarcinoma submetidos a transplante hepático na região metropolitana de São Paulo, entre janeiro de 2007 e dezembro de 2011, a partir de doador falecido. A amostra foi constituída de 414 pacientes. Destes, 29 foram incluídos na lista por downstaging. Os demais 385 foram submetidos ou não ao tratamento loco-regional.
Resultados:
as análises dos 414 prontuários demonstraram um predomínio de pacientes do sexo masculino (79,5%) e com média de idade de 56 anos. O tratamento dos nódulos foi realizado em 56,4% dos pacientes em fila de espera para o transplante. O método mais utilizado foi a quimio-embolização (79%). Os pacientes submetidos ao tratamento loco-regional tiveram redução significativa no tamanho do maior nódulo (p<0,001). Não houve diferença estatística entre grupos com e sem tratamento loco-regional (p=0,744) e em relação à mortalidade entre pacientes incluídos no Critério de Milão ou ao downstaging (p=0,494).
Conclusões:
não houve diferença na sobrevida e ocorrência de recidiva associadas ao tratamento loco-regional. Os pacientes incluídos através do processo de downstaging apresentaram resultados de sobrevida comparáveis àqueles previamente classificados como Critério de Milão/Brasil.
Descritores:
Fígado; Transplante de Fígado; Neoplasias Hepáticas
INTRODUCTION
Hepatocarcinoma (HCC) is the most common malignant neoplasm of the liver and the sixth leading cause of cancer mortality worldwide, with an incidence of 750,000 new cases per year. About 90% of HCCs develop in cirrhotic livers, mainly associated with hepatitis B or C. Liver transplantation (LTx) is now the best treatment for patients with cirrhosis and HCC11 Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893-917.. In 1996, Mazzafero et al.22 Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693-9. proposed what would later be known as the Milan Criterion (MC). Cirrhotic patients with a single nodule up to 5 cm or up to three nodules, the largest of up to 3cm, with no macrovascular invasion or detectable metastases, presented survival of 75% in four years22 Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693-9.. The concepts identified in this study were widely adopted and reproduced In the major transplant centers in the world, including Brazil, which reproduced the good survival results of that population33 Chaib E, Massad E, Varone BB, Bordini AL, Galvão FHF, Crescenzi A, et al. The impact of the introduction of MELD on the dynamics of the liver transplantation waiting list in São Paulo, Brazil. J Transplant. 2014;2014:219789.,44 Salvalaggio P, Afonso RC, Pereira LA, Ferraz-Neto BH. The MELD system and liver transplant waiting-list mortality in developing countries: lessons learned from São Paulo, Brazil. Einstein (Sao Paulo). 2012;10(3):278-85.. However, only a small proportion of HCC patients fit the MC55 Ulahannan SV, Duffy AG, McNeel TS, Kish JK, Dickie LA, Rahma OE, et al. Earlier presentation and application of curative treatments in hepatocellular carcinoma. Hepatology. 2014;60(5):1637-44..
Patients queued for LTxdue to HCC are at risk of increasing the size or number of nodules beyond MC due to the natural evolution of the disease, leading to dropout. To avoid this, locoregional treatments, or bridge treatments, are performed to reduce nodule size, especially when the waiting period can exceed six months66 Cescon M, Cucchetti A, Ravaioli M, Pinna AD. Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. 2013;58(3):609-18.. There is also a group of cirrhotic patients with HCC that have nodules larger than 5cm, or multiple nodules larger than 3cm, but which can reach MC after locoregional treatment, with reduction in nodule size or number. This process, called downstaging, is controversial and benefits an increasing number of patients77 Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11-22..
Our objective was to compare the outcome of LTxdue to HCC in patients submitted or not to locoregional treatment and downstaging regarding survival and risk of relapse.
METHODS
In the study database, we included data from HCC patients submitted to LTx from deceased donors in the metropolitan region of São Paulo between January 2007 and December 2011. The study was approved by the Ethics in Research Commission under to the opinion CEP 81706, of 08/21/2013. The sample consisted of 414 patients. Of these, 29 patients were included in the list due to downstaging. The remaining 385 were divided into two groups: Treatment group (submitted to locoregional treatment) and Group without treatment (without locoregional treatment). We did not obtain the indication of the locoregional treatment, since this was in charge of each transplant team of the metropolitan region of São Paulo and the origin of the patient was kept in confidentiality in the database of the Transplant Center.
Initially, we compared the groups with and without treatment in relation to the outcomes survival and relapse. Next, we compared the results of relapse and survival among the patients included due to downstaging with those who were always within the MC. We performed statistical analyzes using the software packages SPSS 20.0and STATA 12. We analyzed data descriptively. We present categorical variables as absolute and relative frequencies, and numerical variables, as summary statistics (mean, quartiles, minimum, maximum and standard deviation). We verified the associations between categorical variables using the Chi-Square test. When we found differences in distribution, we used the standardized adjusted residue to identify local differences. We compared means between two groups with the Student's t-test for independent samples. For categorical variables, we used the Kaplan-Meier survival analysis models. We estimated survival functions for each level of these variables, and then compared them using the Log Rank test (Mantel-Cox). For the numerical variables, we adjusted the Cox regression models. For all statistical tests, we adopted a significance level of 5%.
RESULTS
The analysis of the 414 charts of patients submitted to liver transplantation specifically due to HCC demonstrated a predominance of male patients (79.5%), with a mean age of 56 years. As of January 2015, three hundred patients were alive (72.5%). They waited for transplant on the list on average for one year.
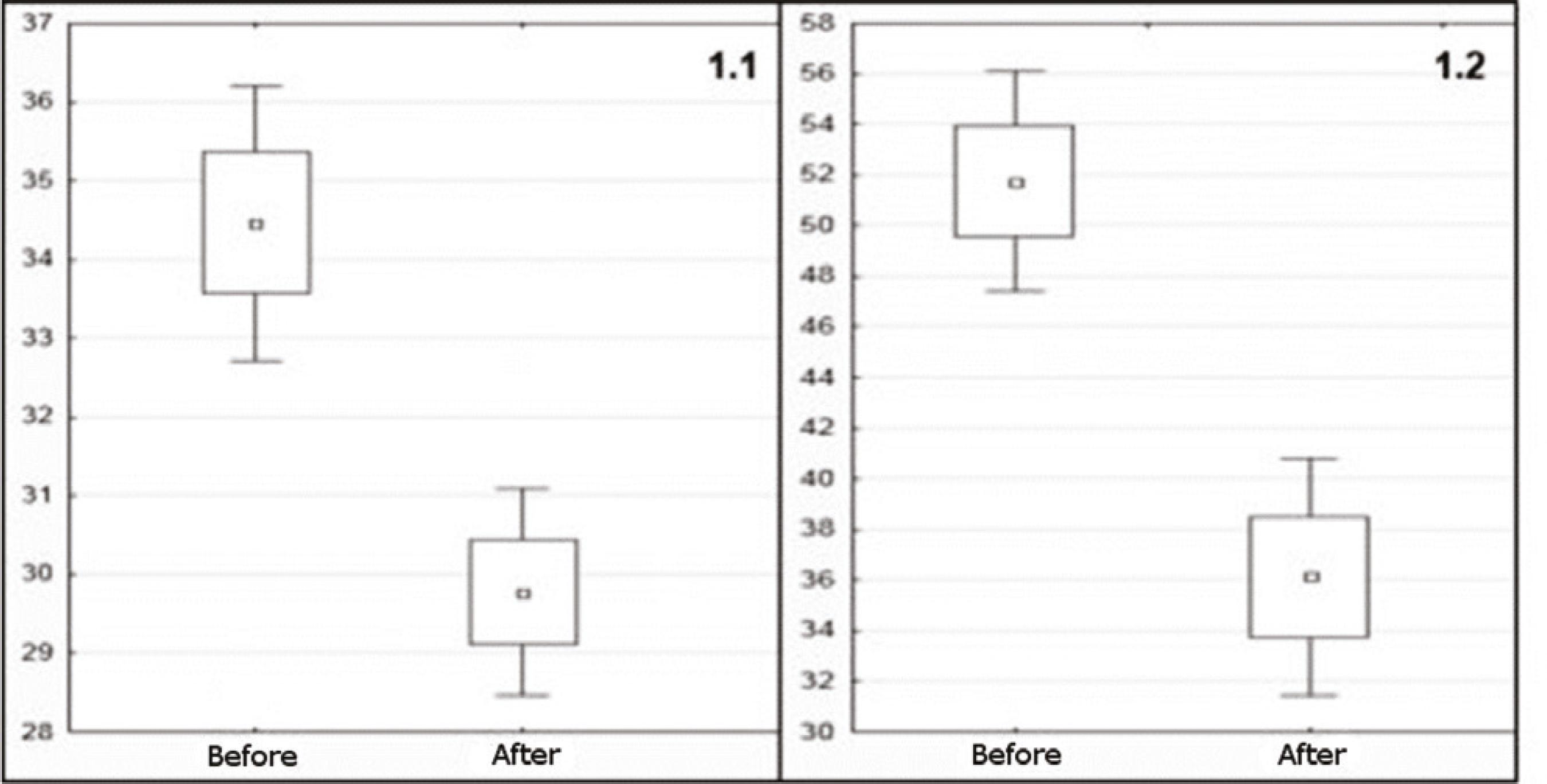
Nodule treatment was performed in 56.4% of patients in the queue for LTx. The most commonly used method was chemo-embolization (79%). Patients submitted to locoregional treatment had a significant reduction, in millimeters,in the largest nodule size before and after treatment (p<0.001) (Figure 1.1). Patients undergoing locoregional treatment for downstaging also showed a significant reduction in the size of the largest nodule in mm before and after treatment (Figure 1.2). There was no interference in mortality due to the preoperative treatment of nodules, as shown in Table 1.
Difference in diameter before and after treatment: 1.1) loco regional treatment; 1.2) downstaging.
Figure 2 presents the survival analysis of the groups submitted or not to locoregional treatment. There was no statistical difference between groups (p=0.744). There were no distinct distributions of relapse according to treatment (p=0.220).
All 414 studied patients met the Milan / Brazil Criteria based on preoperative examinations. Of these, 29 (7%) went through earlier downstaging. Table 2 shows that there was no statistically significant difference in mortality between patients included in the Milan Criterion or those submitted to downstaging.
In January 2015, 72.5% of the patients remained alive after liver transplantation, with follow-up ranging from three to eight years. The Kaplan-Meier survival analysis, presented in Table 3, showed no difference in survival in one, three and five years among patients submitted or not to downstaging. During the study period, there were 30 (7.2%) recurrences.
DISCUSSION
We analyzed 593 medical records of patients submitted to LTx for hepatocarcinoma in the State of São Paulo. The end date of December 2011 was set to end a five-year period of liver transplants after the MELD Era in São Paulo. The selection process of this sample faced difficulties inherent to the method of study of retrospective character with analysis of medical records. The absence of data was the main cause of patient exclusion, justifying the considerable exclusion percentage of the initial sample (30.2%). The final selection of 414 patients provided a very relevant case series when compared with other studies related to LTxdue to HCC, especially when considering that are included patients transplanted only after the implantation of MELD as an allocation criterion.
The profile of the transplanted patient in this series is of a white (80%),middle-aged (mean of 56 years)man (79.5%), with slight overweight (BMI: 26.5) and low real MELD 12.7). The waiting time for hepatic transplantation in patients with HCC is determinant for a better prognosis, since the disease progression can exclude them from MC and, consequently, from transplantation list. The risk of dropping out is due to the intra- or extrahepatic progression of the tumor. This rate varies from 7% to 11% in six months, and approaches 40% in one year88 Yao FY, Bass NM, Nikolai B, Davern TJ, Kerlan R, Wu V, et al. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl. 2002;8(10):873-83.. On the other hand, some authors suggest that delay in the queue may provide a better selection of LTx candidates99 Sumie S, Kuromatsu R, Okuda K, Ando E, Takata A, Fukushima N, et al. Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol. 2008;15(5):1375-82.. Patients with tumors of more aggressive behavior and greater risk of recurrence would present a greater dropout due to the faster progression of the neoplasia and would not be transplanted. Recent studies have shown an increase in survival after LTxdue to HCC in patients who waited longer in the queue1010 Schlansky B, Chen Y, Scott DL, Austin D, Naugler WE. Waiting time predicts survival after liver transplantation for hepatocellular carcinoma: a cohort study using the United Network for Organ Sharing registry. Liver Transpl. 2014;20(9):1045-56.. It appears that patients with HCC have an advantage in the current organ allocation system when compared with non-tumor patients, raising the question of the inclusion of biological factors of poor prognosis, such as alpha-fetoprotein, and tumor growth rate1111 Washburn K, Edwards E, Harper A, Freeman RB. Hepatocellular carcinoma patients are advantaged in the current liver transplant allocation system. Am J Transplant. 2010;10(7):1643-8.. In this series, there was no association of time in the waiting queue with survival. The mean time to transplant was 11.5 months in the alive patients and 13 months in the deceased patients (p>0.1). According to the São Paulo State Transplantation System, the waiting time in the list for LTx of patients without special situation was 16.6 months on average in the same period of this study.
The main goal of treating HCC lesions in patients listed for transplant is to avoid dropout, which is called bridge treatment. This method comprises locoregional therapies, which act directly on the nodules, and surgical resection. Lymph node treatment is recommended when the waiting period in the transplant queue is longer than six months and aims to decrease dropout and increase survival, in addition to reducing the risk of tumor recurrence after LTx66 Cescon M, Cucchetti A, Ravaioli M, Pinna AD. Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. 2013;58(3):609-18.,1212 Nicolini D, Svegliati-Baroni G, Candelari R, Mincarelli C, Mandolesi A, Bearzi I, et al. Doxorubicin-eluting bead vs conventional transcatheter arterial chemoembolization for hepatocellular carcinoma before liver transplantation. World J Gastroenterol. 2013;19(34):5622-32.. However, some services have performed treatment in all patients in the queue due to the unpredictability of the waiting period, and this strategy showed good results1313 Llovet JM, Mas X, Aponte JJ, Fuster J, Navasa M, Christensen E, et al. Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut. 2002;50(1):123-8.. Compared with non-surgical treatments, liver resections in cirrhotic patients listed for transplantation imply high costs, higher morbidity and mortality, should only be indicated in well-compensated patients without severe portal hypertension, and may make transplantation more difficult by prior surgical manipulation, with greater risk of postoperative complications44 Salvalaggio P, Afonso RC, Pereira LA, Ferraz-Neto BH. The MELD system and liver transplant waiting-list mortality in developing countries: lessons learned from São Paulo, Brazil. Einstein (Sao Paulo). 2012;10(3):278-85.. Nevertheless, resection is the most frequently performed treatment as a bridge for LTx in some centers of excellence in liver surgery, with morbidity of 39% and mortality of 3%1414 Xu XS, Liu C, Qu K, Song YZ, Zhang P, Zhang YL. Liver transplantation versus liver resection for hepatocellular carcinoma: a meta-analysis. Hepatobiliary Pancreat Dis Int. 2014;13(3):234-41.. It presents the major advantage of removing the entire lesion for histological evaluation, which may bring relevant information regarding the prognosis. Some services keep the patient in the list after resection, while others, such as in Brazil, remove the extra score if there is resection of the nodule, and only in case of recurrence of the HCC the special situation is reestablished. Transplants in this context are known as Liver Rescue Transplantation and result in worse survival rates and high risk of relapse1515 Wang HQ, Yang J, Zhang X, Yan L, Yang J. Liver resection in hepatitis B-related hepatocellular carcinoma: clinical outcomes and safety in overweight and obese patients. PLoS One. 2014;9(6):e99281..
Chemo embolization is the gold standard treatment for patients with intermediate-stage HCC, according to the Barcelona Classification, presenting a good response in 15% to 55% of patients and an increase in the average survival from 16 to 20 months1616 Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003;37(2):429-42.. It has been used as bridge treatment for a number of years, and several studies have already demonstrated its effectiveness. An analysis done in the larger series indicated that 27% to 57% of the patients within MC had complete necrosis of the treated lesion1717 Millonig G, Graziadei IW, Freund MC, Jaschke W, Stadlmann S, Ladurner R, et al. Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 2007;13(2):272-9.,1818 Tsochatzis E, Garcovich M, Marelli L, Papastergiou V, Fatourou E, Rodriguez-Peralvarez ML, et al. Transarterial embolization as neo-adjuvant therapy pretransplantation in patients with hepatocellular carcinoma. Liver Int. 2013;33(6):944-9.. Patients with a reduction of at least 30% in tumor size until complete devascularization after chemo-embolization have a better LTx prognosis1717 Millonig G, Graziadei IW, Freund MC, Jaschke W, Stadlmann S, Ladurner R, et al. Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 2007;13(2):272-9.. Some studies report good results with radioablation used as a bridge treatment for HCC. The analysis of the explanted livers showed 47% to 75% of complete necrosis of the treated nodules, especially in those smaller than 3 cm1919 Rodríguez-Sanjuán JC, González F, Juanco C, Herrera LA, López-Bautista M, González-Noriega M, et al. Radiological and pathological assessment of hepatocellular carcinoma response to radiofrequency. A study on removed liver after transplantation. World J Surg. 2008;32(7):1489-94.. Alcohololation achieves good results in nodules smaller than 3 cm. Branco et al.2020 Branco F, Brú C, Vilana R, Bianchi L, Alves de Mattos A. Percutaneous ethanol injection before liver transplantation in the hepatocellular carcinoma. Ann Hepatol. 2009;8(3):220-7. demonstrated complete necrosis in 64% of 59 patients analyzed within MC. They did not have good results in nodules larger than 3 cm, though2020 Branco F, Brú C, Vilana R, Bianchi L, Alves de Mattos A. Percutaneous ethanol injection before liver transplantation in the hepatocellular carcinoma. Ann Hepatol. 2009;8(3):220-7.. Studies comparing chemo-embolization with radioablation suggest better results for the latter, both in relation to nodule response and to dropout risk2121 Cucchetti A, Cescon M, Bigonzi E, Piscaglia F, Golfieri R, Ercolani G, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011;17(11):1344-54..
The bridge treatment is able to reduce the dropout by up to 21%2222 Bhoori S, Sposito C, Germini A, Coppa J, Mazzaferro V. The challenges of liver transplantation for hepatocellular carcinoma on cirrhosis. Transpl Int. 2010;23(7):712-22.. On the other hand, an inadequate response to locoregional treatment was shown to be a predictive factor for dropout in Italian centers, as well as a relationship with relapse and death after transplantation, especially if it was associated with elevated AFP2121 Cucchetti A, Cescon M, Bigonzi E, Piscaglia F, Golfieri R, Ercolani G, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011;17(11):1344-54.. The radiological response to locoregional treatment can help to identify the tumor biological behavior1717 Millonig G, Graziadei IW, Freund MC, Jaschke W, Stadlmann S, Ladurner R, et al. Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 2007;13(2):272-9. and to prioritize these patients for LTx2121 Cucchetti A, Cescon M, Bigonzi E, Piscaglia F, Golfieri R, Ercolani G, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011;17(11):1344-54.. Few studies have shown negative impact of locoregional treatment on survival. In a retrospective study published in 2015, Li et al.2323 Li HL, Ji WB, Zhao R, Duan WD, Chen YW, Wang XQ, et al. Poor prognosis for hepatocellular carcinoma with transarterial chemoembolization pre-transplantation: retrospective analysis. World J Gastroenterol. 2015;21(12):3599-606. attributed worsening survival in five years to treatment with chemoembolization performed as a bridge treatment. However, there is sufficient evidence in the literature to conclude that locoregional treatment provides partial or total necrosis of the lesions, with consequent reduction in nodule size and reduction in patient withdrawal from the waiting list. Moreover, there appears to be a decrease in relapse rates in patients with good response to locoregional treatment 77 Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11-22..
In the present study, 56.4% of the patients underwent some kind of locoregional treatment while waiting for LTx. Of these, in nearly 80% chemo-embolization was the method of choice. After locoregional treatment, there was a significant reduction in nodule size. Patients submitted to locoregional treatment had results similar to patients without treatment regarding mortality, both globally and with individualization of the methods. Survival analysis at one, three and five years did not present a significant difference between groups submitted to locoregional treatment or not (p = 0.744). There was also no difference in relapse between groups (p = 0.220).
Locoregional therapies are also used to include patients in MC by means of downstaging77 Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11-22.. Transarterial chemo-embolization is the treatment modality most used in downstaging protocols, especially in multiple nodules. A periodof three to six months after treatment is recommended to stabilize the lesion before the patient is scheduled for transplantation. This period can select patients with better response, less aggressive tumors and less chance of recurrence after transplantation2424 Yao FY, Kerlan RK, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008;48(3):819-27.. The combination of different locoregional therapies, such as chemo-embolization, radioablation, alcoholization and resection have shown better results in downstaging (about 70% success), when compared with isolated chemo-embolization (40% success)2525 Xiao GQ, Song JL, Shen S, Yang JY, Yan LN. Living donor liver transplantation does not increase tumor recurrence of hepatocellular carcinoma compared to deceased donor transplantation. World J Gastroenterol. 2014;20(31):10953-9.. Prospective studies have shown that the survival of patients submitted to downstaging that reach MC is similar to that of patients transplanted without previous treatment77 Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11-22.,2424 Yao FY, Kerlan RK, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008;48(3):819-27.. Retrospective studies have also reached similar results2626 Lei J, Wang W, Yan L. Downstaging advanced hepatocellular carcinoma to the Milan criteria may provide a comparable outcome to conventional Milan criteria. J Gastrointest Surg. 2013;17(8):1440-6.,2727 Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006;12(8):1260-7..
The 29 downstaging cases analyzed in this study were successful in the locoregional treatment, and were submitted to LTx under the Milan/Brazil Criteria. All patients in this group had a significant reduction in nodule size. There was no statistically significant difference in survival when compared to groups of patients submitted to downstaging, who had 71.9% and 71.5%, respectively, in five years. This result confirms data widely published in the literature2222 Bhoori S, Sposito C, Germini A, Coppa J, Mazzaferro V. The challenges of liver transplantation for hepatocellular carcinoma on cirrhosis. Transpl Int. 2010;23(7):712-22.,2424 Yao FY, Kerlan RK, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008;48(3):819-27.,2626 Lei J, Wang W, Yan L. Downstaging advanced hepatocellular carcinoma to the Milan criteria may provide a comparable outcome to conventional Milan criteria. J Gastrointest Surg. 2013;17(8):1440-6.,2727 Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006;12(8):1260-7..
The recurrence rate in our study did not present a statistically significant difference between groups, but there seems to be a tendency to relapse in the downstaging group that could be confirmed with a larger sample.
We conclude that there is no difference in survival or in relapse associated with locoregional treatment. Patients included through the downstaging process presented survival and recurrence results comparable to those previously classified as the Milan / Brazil Criteria.
-
Source of funding: none.
REFERÊNCIAS
-
1Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893-917.
-
2Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693-9.
-
3Chaib E, Massad E, Varone BB, Bordini AL, Galvão FHF, Crescenzi A, et al. The impact of the introduction of MELD on the dynamics of the liver transplantation waiting list in São Paulo, Brazil. J Transplant. 2014;2014:219789.
-
4Salvalaggio P, Afonso RC, Pereira LA, Ferraz-Neto BH. The MELD system and liver transplant waiting-list mortality in developing countries: lessons learned from São Paulo, Brazil. Einstein (Sao Paulo). 2012;10(3):278-85.
-
5Ulahannan SV, Duffy AG, McNeel TS, Kish JK, Dickie LA, Rahma OE, et al. Earlier presentation and application of curative treatments in hepatocellular carcinoma. Hepatology. 2014;60(5):1637-44.
-
6Cescon M, Cucchetti A, Ravaioli M, Pinna AD. Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. 2013;58(3):609-18.
-
7Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A; OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11-22.
-
8Yao FY, Bass NM, Nikolai B, Davern TJ, Kerlan R, Wu V, et al. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl. 2002;8(10):873-83.
-
9Sumie S, Kuromatsu R, Okuda K, Ando E, Takata A, Fukushima N, et al. Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors. Ann Surg Oncol. 2008;15(5):1375-82.
-
10Schlansky B, Chen Y, Scott DL, Austin D, Naugler WE. Waiting time predicts survival after liver transplantation for hepatocellular carcinoma: a cohort study using the United Network for Organ Sharing registry. Liver Transpl. 2014;20(9):1045-56.
-
11Washburn K, Edwards E, Harper A, Freeman RB. Hepatocellular carcinoma patients are advantaged in the current liver transplant allocation system. Am J Transplant. 2010;10(7):1643-8.
-
12Nicolini D, Svegliati-Baroni G, Candelari R, Mincarelli C, Mandolesi A, Bearzi I, et al. Doxorubicin-eluting bead vs conventional transcatheter arterial chemoembolization for hepatocellular carcinoma before liver transplantation. World J Gastroenterol. 2013;19(34):5622-32.
-
13Llovet JM, Mas X, Aponte JJ, Fuster J, Navasa M, Christensen E, et al. Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut. 2002;50(1):123-8.
-
14Xu XS, Liu C, Qu K, Song YZ, Zhang P, Zhang YL. Liver transplantation versus liver resection for hepatocellular carcinoma: a meta-analysis. Hepatobiliary Pancreat Dis Int. 2014;13(3):234-41.
-
15Wang HQ, Yang J, Zhang X, Yan L, Yang J. Liver resection in hepatitis B-related hepatocellular carcinoma: clinical outcomes and safety in overweight and obese patients. PLoS One. 2014;9(6):e99281.
-
16Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003;37(2):429-42.
-
17Millonig G, Graziadei IW, Freund MC, Jaschke W, Stadlmann S, Ladurner R, et al. Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 2007;13(2):272-9.
-
18Tsochatzis E, Garcovich M, Marelli L, Papastergiou V, Fatourou E, Rodriguez-Peralvarez ML, et al. Transarterial embolization as neo-adjuvant therapy pretransplantation in patients with hepatocellular carcinoma. Liver Int. 2013;33(6):944-9.
-
19Rodríguez-Sanjuán JC, González F, Juanco C, Herrera LA, López-Bautista M, González-Noriega M, et al. Radiological and pathological assessment of hepatocellular carcinoma response to radiofrequency. A study on removed liver after transplantation. World J Surg. 2008;32(7):1489-94.
-
20Branco F, Brú C, Vilana R, Bianchi L, Alves de Mattos A. Percutaneous ethanol injection before liver transplantation in the hepatocellular carcinoma. Ann Hepatol. 2009;8(3):220-7.
-
21Cucchetti A, Cescon M, Bigonzi E, Piscaglia F, Golfieri R, Ercolani G, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011;17(11):1344-54.
-
22Bhoori S, Sposito C, Germini A, Coppa J, Mazzaferro V. The challenges of liver transplantation for hepatocellular carcinoma on cirrhosis. Transpl Int. 2010;23(7):712-22.
-
23Li HL, Ji WB, Zhao R, Duan WD, Chen YW, Wang XQ, et al. Poor prognosis for hepatocellular carcinoma with transarterial chemoembolization pre-transplantation: retrospective analysis. World J Gastroenterol. 2015;21(12):3599-606.
-
24Yao FY, Kerlan RK, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008;48(3):819-27.
-
25Xiao GQ, Song JL, Shen S, Yang JY, Yan LN. Living donor liver transplantation does not increase tumor recurrence of hepatocellular carcinoma compared to deceased donor transplantation. World J Gastroenterol. 2014;20(31):10953-9.
-
26Lei J, Wang W, Yan L. Downstaging advanced hepatocellular carcinoma to the Milan criteria may provide a comparable outcome to conventional Milan criteria. J Gastrointest Surg. 2013;17(8):1440-6.
-
27Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006;12(8):1260-7.
Publication Dates
-
Publication in this collection
Jul-Aug 2017
History
-
Received
22 Dec 2016 -
Accepted
28 Apr 2017