Abstracts
PURPOSE: To determine anatomical and functional pelvic floor measurements performed with three-dimensional (3-D) endovaginal ultrasonography in asymptomatic nulliparous women without dysfunctions detected in previous dynamic 3-D anorectal ultrasonography (echo defecography) and to demonstrate the interobserver reliability of these measurements. METHODS: Asymptomatic nulliparous volunteers were submitted to echo defecography to identify dynamic dysfunctions, including anatomical (rectocele, intussusceptions, entero/sigmoidocele and perineal descent) and functional changes (non-relaxation or paradoxical contraction of the puborectalis muscle) in the posterior compartment and assessed with regard to the biometric index of levator hiatus, pubovisceral muscle thickness, urethral length, anorectal angle, anorectal junction position and bladder neck position with the 3-D endovaginal ultrasonography. All measurements were compared at rest and during the Valsalva maneuver, and perineal and bladder neck descent was determined. The level of interobserver agreement was evaluated for all measurements. RESULTS: A total of 34 volunteers were assessed by echo defecography and by 3-D endovaginal ultrasonography. Out of these, 20 subjects met the inclusion criteria. The 14 excluded subjects were found to have posterior dynamic dysfunctions. During the Valsalva maneuver, the hiatal area was significantly larger, the urethra was significantly shorter and the anorectal angle was greater. Measurements at rest and during the Valsalva maneuver differed significantly with regard to anorectal junction and bladder neck position. The mean values for normal perineal descent and bladder neck descent were 0.6 cm and 0.5 cm above the symphysis pubis, respectively. The intraclass correlation coefficient ranged from 0.62-0.93. CONCLUSIONS: Functional biometric indexes, normal perineal descent and bladder neck descent values were determined for young asymptomatic nulliparous women with the 3-D endovaginal ultrasonography. The method was found to be reliable to measure pelvic floor structures at rest and during Valsalva, and might therefore be suitable for identifying dysfunctions in symptomatic patients.
Pelvic floor; Cervix uteri; Reproducibility of results; Observer variations
OBJETIVO: Avaliar as medidas anatômicas e funcionais do assoalho pélvico utilizando a ultrassonografia tridimensional transvaginal em nulíparas assintomáticas sem disfunções do compartimento posterior evidenciado pela ecodefecografia. Demonstrar o grau de concordância entre observadores do método utilizado para medir as estruturas anatômicas. MÉTODOS: Voluntárias nulíparas assintomáticas foram submetidas à ecodefecografia para identificar alterações dinâmicas no compartimento posterior, incluindo aquelas anatômicas (retocele, intussuscepção, entero/sigmoidocele e descenso perineal) e funcionais (ausência de relaxamento ou contração paradoxal do puborretal) e avaliadas com ultrassonografia tridimensional transvaginal para determinar índices biométricos do hiato dos elevadores do ânus, espessura do músculo pubovisceral, comprimento da uretra, ângulo anorretal, posição da junção anorretal e posição do colo vesical. Todas as medidas foram comparadas em repouso e durante Valsalva; e determinado descenso perineal e do colo da bexiga. A variabilidade interobservador foi avaliada utilizando o coeficiente de correlação intraclasse. RESULTADOS: Foram avaliadas 34 voluntárias com a ecodefecografia e a ultrassonografia tridimensional transvaginal. Dessas, 20 foram incluídas no estudo. As 14 excluídas apresentavam alterações dinâmicas no compartimento posterior. Durante a manobra de Valsalva, a área hiatal foi significativamente maior. A uretra foi significantemente mais curta e o ângulo anorretal foi maior. Medidas em repouso e durante a Valsalva diferiram significativamente em relação à posição da junção anorretal e do colo vesical. A média de valor do descenso perineal e do descenso da bexiga foram de 0,6 cm e 0,5 cm acima da sínfise púbica, respectivamente. O coeficiente de correlação intraclasse variou entre 0,62-0,93. CONCLUSÕES: Foram determinados valores normais para os índices biométricos funcionais, descida perineal e colo vesical em nulíparas assintomáticas utilizando-se a ultrassonografia transvaginal tridimensional. É um método seguro para mensurar a anatomia do assoalho pélvico durante o repouso e a manobra de Valsalva, e pode ser adequado para a identificação de disfunções em pacientes sintomáticos.
Diafragma pélvico; Colo do útero; Reprodutibilidade dos testes; Variações dependentes do observador
ARTIGO ORIGINAL
Anatomical and functional characteristics of the pelvic floor in nulliparous women submitted to three-dimensional endovaginal ultrasonography: case control study and evaluation of interobserver agreement
Características anatômicas e funcionais do assoalho pélvico em nulíparas avaliadas por ultrassonografia tridimensional endovaginal: estudo caso-controle e avaliação da confiabilidade interobservador
Sthela Maria Murad-RegadasI; Leonardo Robson Pinheiro Sobreira BezerraII; Claudio Regis Sampaio SilveiraIII; Jacyara de Jesus Rosa PereiraI; Graziela Olivia da Silva FernandesI; José Ananias Vasconcelos NetoIV; Iris Daiana DealcanfreitasI
IAnorectal Physiology and Pelvic Floor Unit, Hospital das Clínicas, Universidade Federal do Ceará - UFC - Fortaleza (CE), Brazil
IIDepartment of Urogynecology, Hospital Cesar Calls - Fortaleza (CE), Brazil
IIIDepartment of Radiology, Hospital São Carlos - Fortaleza (CE), Brazil
IVDepartment of Urogynecology, Hospital Geral de Fortaleza - Fortaleza (CE), Brazil
Correspondence Correspondence: Sthela Maria Murad-Regadas Centro de Coloproctologia Hospital São Carlos Avenida Pontes Vieira, 2.551, 2nd floor Dionísio Torres Zip code: 60130-240 Fortaleza (CE), Brazil
ABSTRACT
PURPOSE: To determine anatomical and functional pelvic floor measurements performed with three-dimensional (3-D) endovaginal ultrasonography in asymptomatic nulliparous women without dysfunctions detected in previous dynamic 3-D anorectal ultrasonography (echo defecography) and to demonstrate the interobserver reliability of these measurements.
METHODS: Asymptomatic nulliparous volunteers were submitted to echo defecography to identify dynamic dysfunctions, including anatomical (rectocele, intussusceptions, entero/sigmoidocele and perineal descent) and functional changes (non-relaxation or paradoxical contraction of the puborectalis muscle) in the posterior compartment and assessed with regard to the biometric index of levator hiatus, pubovisceral muscle thickness, urethral length, anorectal angle, anorectal junction position and bladder neck position with the 3-D endovaginal ultrasonography. All measurements were compared at rest and during the Valsalva maneuver, and perineal and bladder neck descent was determined. The level of interobserver agreement was evaluated for all measurements.
RESULTS: A total of 34 volunteers were assessed by echo defecography and by 3-D endovaginal ultrasonography. Out of these, 20 subjects met the inclusion criteria. The 14 excluded subjects were found to have posterior dynamic dysfunctions. During the Valsalva maneuver, the hiatal area was significantly larger, the urethra was significantly shorter and the anorectal angle was greater. Measurements at rest and during the Valsalva maneuver differed significantly with regard to anorectal junction and bladder neck position. The mean values for normal perineal descent and bladder neck descent were 0.6 cm and 0.5 cm above the symphysis pubis, respectively. The intraclass correlation coefficient ranged from 0.62-0.93.
CONCLUSIONS: Functional biometric indexes, normal perineal descent and bladder neck descent values were determined for young asymptomatic nulliparous women with the 3-D endovaginal ultrasonography. The method was found to be reliable to measure pelvic floor structures at rest and during Valsalva, and might therefore be suitable for identifying dysfunctions in symptomatic patients.
Keywords: Pelvic floor/anatomy & physiology; Cervix uteri/ultrasonography; Reproducibility of results; Observer variations
RESUMO
OBJETIVO: Avaliar as medidas anatômicas e funcionais do assoalho pélvico utilizando a ultrassonografia tridimensional transvaginal em nulíparas assintomáticas sem disfunções do compartimento posterior evidenciado pela ecodefecografia. Demonstrar o grau de concordância entre observadores do método utilizado para medir as estruturas anatômicas.
MÉTODOS: Voluntárias nulíparas assintomáticas foram submetidas à ecodefecografia para identificar alterações dinâmicas no compartimento posterior, incluindo aquelas anatômicas (retocele, intussuscepção, entero/sigmoidocele e descenso perineal) e funcionais (ausência de relaxamento ou contração paradoxal do puborretal) e avaliadas com ultrassonografia tridimensional transvaginal para determinar índices biométricos do hiato dos elevadores do ânus, espessura do músculo pubovisceral, comprimento da uretra, ângulo anorretal, posição da junção anorretal e posição do colo vesical. Todas as medidas foram comparadas em repouso e durante Valsalva; e determinado descenso perineal e do colo da bexiga. A variabilidade interobservador foi avaliada utilizando o coeficiente de correlação intraclasse.
RESULTADOS: Foram avaliadas 34 voluntárias com a ecodefecografia e a ultrassonografia tridimensional transvaginal. Dessas, 20 foram incluídas no estudo. As 14 excluídas apresentavam alterações dinâmicas no compartimento posterior. Durante a manobra de Valsalva, a área hiatal foi significativamente maior. A uretra foi significantemente mais curta e o ângulo anorretal foi maior. Medidas em repouso e durante a Valsalva diferiram significativamente em relação à posição da junção anorretal e do colo vesical. A média de valor do descenso perineal e do descenso da bexiga foram de 0,6 cm e 0,5 cm acima da sínfise púbica, respectivamente. O coeficiente de correlação intraclasse variou entre 0,62-0,93.
CONCLUSÕES: Foram determinados valores normais para os índices biométricos funcionais, descida perineal e colo vesical em nulíparas assintomáticas utilizando-se a ultrassonografia transvaginal tridimensional. É um método seguro para mensurar a anatomia do assoalho pélvico durante o repouso e a manobra de Valsalva, e pode ser adequado para a identificação de disfunções em pacientes sintomáticos.
Palavras-chave: Diafragma pélvico/anatomia & fisiologia; Colo do útero/ultrassonografia; Reprodutibilidade dos testes; Variações dependentes do observador
Introduction
Recent advances in imaging technologies have opened new possibilities of investigation, such as the successful use of magnetic resonance and an array of ultrasound modalities in the evaluation of the anatomical and functional characteristics of the pelvic floor1-16. Some authors have described the pelvic floor anatomy of asymptomatic females and determined normal values for anatomic measurements7,13,16. However, previous studies have reported voiding disorders (rectocele, intussusception and paradoxical contraction) in asymptomatic patients evaluated at random17-19. In addition, gender and age-related differences in the anal canal anatomy have been reported in some series14,20,21, and Regadas et al.22 described variations in the anal canal anatomy of patients with rectocele.
It is therefore important to identify potential dynamic dysfunctions of the pelvic floor of subjects without symptoms to evaluate normal anatomy and establish regular ranges. Posterior pelvic floor dysfunctions may be associated with both anatomical (rectocele, intussusceptions, entero-sigmoidocele and perineal descent) and functional changes (non-relaxation or paradoxical contraction of the puborectalis muscle). A number of different imaging methods (defecography, dynamic ultrasonography and dynamic magnetic resonance imaging) may be used to evaluate such dysfunctions2,6,11,15,23. The purpose of this study was to evaluate anatomical and functional pelvic floor measurements performed with 3-D endovaginal ultrasonography in asymptomatic nulliparous women without dysfunctions detected on previous dynamic 3-D anorectal ultrasonography (echo defecography) and to demonstrate the interobserver agreement of these measurements.
Methods
Subjects
Consecutive asymptomatic nulliparous volunteers (aged up to 50 years) were recruited among the employees of two academic hospitals in Fortaleza (Clinical Hospital of the Federal University of Ceará and São Carlos Hospital) and were enrolled in the study between July 2009 and July 2011. The clinical protocol was approved by the Research Ethics Committee of the Walter Cantídio University Hospital, and all subjects gave their written informed consent.
Subjects were evaluated clinically and assigned fecal incontinence24 and constipation25 scores. They were submitted to 3-D dynamic anorectal ultrasonography (echo defecography) to identify anatomical (rectocele, rectal intussusceptions, entero/sigmoidocele and perineal descent) and functional changes (non-relaxation or paradoxical contraction of the puborectalis muscle) in the posterior compartment. The study population included only females reporting to be fully continent, with Wexner constipation scores under 4 and no anatomical or functional changes detected at the echo defecography. The subjects were prospectively submitted to anatomical and functional measurements with 3-D endovaginal ultrasonography.
Subjects with obstructed defecation symptoms, fecal incontinence or urgency, sphincter damage at the 3-D ultrasonography, symptoms of stress, urge urinary incontinence, obesity and diabetic or neurological disorders were excluded, as well as subjects with a history of colorectal, anorectal or gynecological surgery.
Assessments and variables
All subjects were previously instructed on how to perform the Valsalva maneuver. Subjects were examined in the dorsal lithotomy position with a 3-D ultrasound endoprobe (Pro-Focus 2052; 9-16 MHz; focal distance 2.8-6.2 cm, BK Medical®, Herlev, Denmark). The endoprobe was introduced above the bladder neck. Images up to 6 cm long were captured along the proximal-distal axis for up to 55 seconds by 2 crystals (axial and longitudinal) rotating on the extremity of a stationary transducer. The examination involved a series of transaxial microsections up to 0.20 mm thick producing a high-resolution digital volumetric image. Images acquired at rest and during the Valsalva maneuver were displayed as 3-D cube images and recorded and analyzed in multiple planes. The examination was performed by a single colorectal surgeon with experience in 3-D anorectal ultrasonography (S.M.M.R.). Finally, all images (complete 3-D cubes) were numbered randomly, being reassessed and measured independently by two blinded colorectal surgeons (S.M.M.R. and G.O.S.F.). In their routine clinical practice with 3-D endovaginal ultrasonography, the investigators use the same anatomic landmarks and measurements.
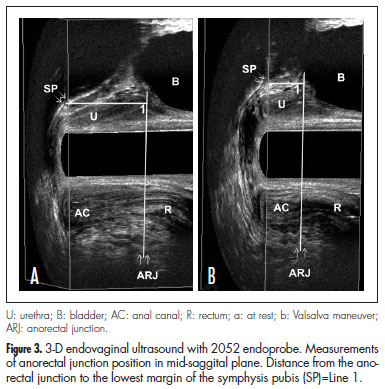
The study parameters included: 1) biometric indexes of the levator hiatus (LH), including the anteroposterior and the latero-lateral diameter (Figure 1) and area16; 2) pubovisceral muscle (PVM) thickness in the left (3 o'clock) and right (9 o'clock) positions; 3) urethral length, measured from the bladder neck to the external urethral orifice; 4) anorectal angle, measured at the intersection of the longitudinal axis of the anal canal and a line drawn along the posterior border of the rectal wall (Figure 2); 5) anorectal junction (ARJ) position, measured from the anorectal junction to the lowest margin of the symphysis pubis (SP) (Figure 3). The displacement of the ARJ position between rest and Valsalva indicates perineal descent and; 6) bladder neck (BN) position, measured from the bladder neck to the lowest margin of the SP (Figure 4). The displacement of the BN position between rest and Valsalva indicates bladder neck descent.
All measurements were registered and compared at rest and during the Valsalva maneuver. Normal values were determined for perineal and bladder neck descent. The level of interobserver agreement was evaluated for all measurements of all study subjects.
Echo defecography was performed with a 3-D ultrasound device (Pro-Focus, endoprobe model 2052, B-K Medical®, Herlev, Denmark) placed in the rectum, as previously described. This procedure had been previously validated and standardized by Murad-Regadas et al.15 and Regadas et al.14,26. Following rectal enema, the subjects were given the instructions for the examination and were evaluated in the left lateral position. Images were acquired by four automatic scans and analyzed in the axial, sagittal and, if necessary, the oblique plane. Scans 1, 3 and 4 used a slice width of 0.25 mm and lasted 55 seconds each. Scan 2 lasted 30 seconds and used a slice width of 0.35 mm.
For scan 1 (at rest): the transducer was positioned proximally to the PR (anorectal junction) to verify the anatomical integrity of anal sphincters. For scan 2, the transducer was positioned proximally to the PR. The scan started with the patient at rest (3 seconds), followed by maximum strain with the transducer in a fixed position. When PR became visible distally, the scan was stopped. Perineal descent was quantified by measuring the distance between the position of the proximal border of the PR at rest and the point to which it had been displaced by maximum strain (PR descent). For Scan 3, the transducer was positioned 6 cm from the anal verge. The patient was requested to rest for the first 15 seconds, to strain at most for 20 seconds, then relax again, with the transducer following the movement. The purpose of the scan was to evaluate the movement of the PR and the external anal sphincter during strain, identifying normal relaxation, non-relaxation and paradoxical contraction. Scan 4: after the injection of 120-180 mL of ultrasound gel into the rectal ampulla, the transducer was positioned 7 cm from the anal verge. The scanning sequence was the same as in scan 3. The purpose of the scan was to visualize and quantify all anatomical structures and functional changes associated with voiding (rectocele, intussusception, sigmoidocele/enterocele).
Statistical analysis
The data were analyzed with SPSS for Windows (version 14.0). Differences between the measurements registered at rest and during the Valsalva maneuver were assessed with the Student's t test. The level of statistical significance was set at p<0.05. The level of interobserver agreement was evaluated with the intraclass correlation coefficient (ICC), with a 95% confidence interval. ICC values greater than 0.70 are acceptable in research, but for clinical purposes the coefficient should be 0.90 or higher, and at least 0.95 when used to subsidize important decisions27.
Results
Subject characteristics
A total of 34 volunteers were assessed by echo defecography and by 3-D endovaginal ultrasonography at rest and during the Valsalva maneuver. Of these, 20 subjects met the inclusion criteria. The 14 excluded subjects were found to have grade I or II rectocele (n=4; 12%) or non-relaxation/paradoxical contraction of the puborectalis (n=10; 27%). Mean age was 30.3±7.4 years (ranging from 18-44). Mean body mass index was 25.5 kg/m2 (ranging from 18.8 to 28.6).
3-D dynamic endovaginal ultrasonography measurements
During the Valsalva maneuver, biometric indexes of LH, including the anteroposterior and latero-lateral diameters, increased (though not significantly) whereas the hiatal area was significantly larger. PVM thickness in the right and left position was similar at rest and during Valsalva (Table 1).
The urethra was significantly shorter and the anorectal angle was greater during Valsalva. Measurements at rest and during Valsalva differed significantly with regard to the ARJ position (2.1 versus 1.4 cm above the SP) (p=0.01) and the BN position (2.9 versus 2.3 cm above the SP) (p=0.0004) (Table 1). Mean values for normal perineal descent and bladder neck descent were 0.6 cm (range: 0.0-1.6) and 0.5 cm (range: 0.0-1.4) above the SP, respectively. In 2 subjects, the ARJ position was 0.1 and 0.4 cm below the SP, respectively.
Interobserver variability
As shown in Table 2, the ICC (average measures) for evaluations performed by the two blinded examiners ranged from 0.62 to 0.93 in the sample of 20 participants (including measurements at rest and during Valsalva). Thus, for almost all measurements the level of interobserver agreement was acceptable for research purposes. The agreement between LH measurements (anteroposterior diameter), at rest and during Valsalva, was acceptable for clinical purposes.
Discussion
This study provides anatomical and functional measurements of the pelvic floor at rest and during Valsalva for a sample of asymptomatic nulliparous women submitted to automatic 3-D endovaginal ultrasonography. In addition, normal range and cut-off values of physiological perineal descent and bladder neck descent were established. This was made possible by recruiting asymptomatic, nulliparous volunteers without symptoms of incontinence or obstructed defecation and without anatomic and functional posterior dysfunctions at echo defecography.
We excluded 12% of the initial sample of volunteers due to anatomic changes (rectocele) and 27% due to functional changes (non-relaxation/paradoxical contraction of the PR) in order to rule out any effect of such dysfunctions on the pelvic floor anatomy, even in asymptomatic subjects. Regadas et al.22 clearly demonstrated the presence of anatomical changes in the anal canal of patients with rectocele. Large rectocele is a common cause of obstructed defecation due to anatomical changes, but smaller forms have been observed in up to 80% of asymptomatic subjects17.
Nevertheless, the definition of rectocele and the factors of prevalence are still controversial. For gynecologists, rectocele is a prolapse of the posterior vaginal wall associated with a rectovaginal septum defect28, whereas for colorectal surgeons, rectocele is a hernia of the anterior wall into the vagina detectable during functional defecation maneuvers6,11,15,17,26. Different imaging modalities, such as dynamic ultrasonography and magnetic resonance imaging, have been used to evaluate posterior pelvic floor dysfunctions, with good correlation2,6,11,15,23,26,28.
Paradoxical contraction of the PR (or non-relaxation) is not uncommonly found in asymptomatic subjects and should be recognized at examination. In a study on pregnant nulliparous women, Orno and Dietz29 demonstrated that the Valsalva maneuver is frequently accompanied by pelvic floor muscle contraction due to levator coactivation and associated with significant differences in pelvic floor measurements when comparing the first and the optimal Valsalva maneuvers. In their study, levator coactivation was found to be associated with significantly reduced bladder neck descent and lower hiatal diameter and area measurements. The authors suggested that subjects be instructed and trained as to how to perform the functional maneuver prior to dynamic scanning. The expressions "non-relaxation", "paradoxical contraction of the puborectalis muscle" and "levator coactivation" refer to the same dysfunction.
All subjects were previously evaluated with echo defecography to assess the posterior compartment for possible dysfunctions. The echo defecography technique and the parameters used in the present study have been previously described by Murad-Regadas et al.15. Using a 360º transducer, automatic scanning and high frequencies for high-resolution images, the authors validated the technique in a prospective multicenter study by demonstrating agreement between echo defecography and conventional defecography26. The advantage of echo defecography lies in the possibility of visualizing all anatomical structures of the pelvic floor, changes during strain and evacuation disorders, without exposing the patient to radiation.
Our findings for biometric indexes of the levator hiatus and PVM thickness at rest match the results published by Santoro et al.16 based on nulliparous patients submitted to 3-D endovaginal ultrasonography. They are also similar to those published by Shobeiri et al.13 in a study determining normal ranges for anatomical measurements of the pelvic floor in nulliparous subjects using 3-D endovaginal ultrasonography, although measurements were only taken at rest. Using 3-D endovaginal ultrasound, images acquired automatically with a 16-Mhz transducer are merged into a 3-D cube and recorded in real time for subsequent analysis. The cube image can be freely manipulated in all planes and allows the visualization of anatomical structures simultaneously after image processing.
The biometric indexes of the LH increased and the hiatal area was significantly larger during the Valsalva maneuver, while PVM thickness in the right and left positions remained unchanged. In addition, BN and ARJ positions differed significantly in relation to the lower margin of the SP between rest and Valsalva. To our knowledge, this is the first study using dynamic 3-D endovaginal ultrasonography to evaluate the position of the anorectal junction and the bladder neck at rest and during Valsalva, determining the difference between these measurements and establishing cut-off values for normal perineal descent and normal bladder neck descent in nulliparous subjects. Dietz et al.7 studied the position of the bladder neck during Valsalva with transperineal ultrasonography. Despite differences in technique, their results match the findings of this study. Shobeiri et al.13 evaluated the muscles comprising the minimal levator hiatus, determined the minimal levator hiatus area and the anorectal angle, and described a new measurement called levator plate descent angle at rest, establishing normal ranges to enable the identification of abnormalities. Likewise, the results of a study by Beer-Gabel et al.6 using dynamic transperineal ultrasonography to determine the anorectal position at rest and during maximal strain in female patients with obstructed defecation are comparable to measurements obtained with defecography; however, the authors did not establish normal perineal descent values for the technique. Some authors used dynamic ultrasonography to measure the anorectal angle at rest16 and during squeezing.12 In our study, the anorectal angle was significantly larger during Valsalva than at rest in women without dysfunctions, matching the results of Beer-Gabel et al.6 for normal relaxation and anismus in their comparison of dynamic transperineal ultrasonography and defecography.
In the present study, the level of interobserver agreement for measurements taken at rest and during Valsalva was within the acceptable range for research purposes, as established elsewhere7,30. Technological advances and new high-resolution modalities of ultrasonography have brought innovation to research on pelvic floor anatomy and made it possible to standardize techniques and identify landmarks. Several studies have shown that these techniques are reproducible7,12,30.
3-D endovaginal ultrasonography allows to visualize the morphology and function of the pelvic floor in multiple planes and at high resolution, and constitutes an alternative imaging modality for pelvic floor dysfunctions. Although our sample was relatively small, the present series has significant implications on anatomical and functional measurements of the pelvic floor in selected asymptomatic women submitted to 3-D endovaginal ultrasonography, following evaluation by echo defecography. Further studies on other patient series are required to demonstrate the relation between biometric indexes in patients with multiple dysfunctions such as perineal descent and∕or significant rectocele.
In conclusion, functional biometric indexes, normal perineal descent and bladder neck descent values were determined for young asymptomatic nulliparous women using 3-D endovaginal ultrasonography. The method was found to be reliable for measuring pelvic floor structures at rest and during Valsalva, and might therefore be a suitable method for identifying dysfunctions in symptomatic patients.
Received 11/13/2012
Accepted with modifications 02/25/2013
Conflict of interest: none
Study carried out at the Coloproctology Service, Hospital das Clínicas, Universidade Federal do Ceará - UFC - Fortaleza (CE), Brazil.
- 1. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46-53.
- 2. Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M. Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol. 1997;7(8):1309-17.
- 3. Luo J, Larson KA, Fenner DE, Ashton-Miller JA, DeLancey JO. Posterior vaginal prolapse shape and position changes at maximal Valsalva seen in 3-D MRI-based models. Int Urogynecol J. 2012;23(9):1301-6.
- 4. Guo M, Li D. Pelvic floor images: anatomy of the levator ani muscle. Dis Colon Rectum. 2007;50(10):1647-55.
- 5. Williams AB, Bartram CI, Halligan S, Marshall MM, Nicholls RJ, Kmiot WA. Multiplanar anal endosonography - normal anal canal anatomy. Colorectal Dis. 2001;3(3):169-74.
- 6. Beer-Gabel M, Teshler M, Barzilai N, Lurie Y, Malnick S, Bass D, et al. Dynamic transperineal ultrasound in the diagnosis of pelvic floor disorders: pilot study. Dis Colon Rectum. 2002;45(2):239-45.
- 7. Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25(6):580-5.
- 8. Huang WC, Yang SH, Yang JM. Three-dimensional transperineal sonographic characteristics of the anal sphincter complex in nulliparous women. Ultrasound Obstet Gynecol. 2007;30(2):210-20.
- 9. Shobeiri SA, Leclaire E, Nihira MA, Quiroz LH, O'Donoghue D. Appearance of the levator ani muscle subdivisions in endovaginal three-dimensional ultrasonography. Obstet Gynecol. 2009;114(1):66-72.
- 10. Shek KL, Dietz HP. The effect of childbirth on hiatal dimensions. Obstet Gynecol. 2009;113(6):1272-8.
- 11. Steensma AB, Oom DM, Burger CW, Schouten RW. Assessment of posterior compartment prolapse: a comparison of evacuation proctography and 3D transperineal ultrasound. Colorectal Dis. 2010;12(6):533-9.
- 12. Olsen IP, Wilsgaard T, Kiserud T. Transvaginal three-dimensional ultrasound: a method of studying anal anatomy and function. Ultrasound Obstet Gynecol. 2011;37(3):353-60.
- 13. Shobeiri SA, Rostaminia G, White D, Quiroz LH. The determinants of minimal levator hiatus and their relationship to the puborectalis muscle and the levator plate. BJOG. 2013;120(2):205-11.
- 14. Regadas FS, Murad-Regadas SM, Lima DM, Silva FR, Barreto RG, Souza MH, et al. Anal canal anatomy showed by three-dimensional anorectal ultrasonography. Surg Endosc. 2007;21(12):2207-11.
- 15. Murad-Regadas SM, Regadas FS, Rodrigues LV, Silva FR, Soares FA, Escalante RD. A novel three-dimensional dynamic anorectal ultrasonography technique (echodefecography) to assess obstructed defecation, a comparison with defecography. Surg Endosc. 2008;22(4):974-9.
- 16. Santoro GA, Wieczorek AP, Stankiewicz A, Woniak MM, Bogusiewicz M, Rechberger T. High-resolution three-dimensional endovaginal ultrasonography in the assessment of pelvic floor anatomy: a preliminary study. Int Urogynecol J. Pelvic Floor Dysfunct. 2009;20(10):1213-22.
- 17. Shorvon PJ, McHugh S, Diamant NE, Somers S, Stevenson GW. Defecography in normal volunteers: results and implications. Gut. 1989;30(12):1737-49.
- 18. Freimanis MG, Wald A, Caruana B, Bauman DH. Evacuation proctography in normal volunteers. Invest Radiol. 1991;26(6):581-5.
- 19. Schouten WR, Briel JW, Auwerda JJ, van Dam JH, Gosselink MJ, Ginai AZ, et al. Anismus: fact or fiction? Dis Colon Rectum. 1997;40(9):1033-41.
- 20. Frudinger A, Halligan S, Bartram CI, Price AB, Kamm MA, Winter R. Female anal sphincter: age-related differences in asymptomatic volunteers with high-frequency endoanal US. Radiology. 2002;224(2):417-23.
- 21. Knowles AM, Knowles CH, Scott SM, Lunniss PJ. Effects of age and gender on three-dimensional endoanal ultrasonography measurements: development of normal ranges. Tech Coloproctol. 2008;12(4):323-9.
- 22. Regadas FS, Murad-Regadas SM, Wexner SD, Rodrigues LV, Souza MH, Silva FR, et al. Anorectal three-dimensional endosonography and anal manometry in assessing anterior rectocele in women: a new pathogenesis concept and the basic surgical principle. Colorectal Dis. 2007;9(1):80-5.
- 23. Mahieu P, Pringot J, Bodart P. Defecography: I. Description of a new procedure and results in normal patients. Gastrointest Radiol. 1984;9(3):247-51.
- 24. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36(1):77-97.
- 25. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39(6):681-5.
- 26. Regadas FS, Haas EM, Abbas MA, Marcio Jorge J, Habr-Gama A, Sands D, et al. Prospective multicenter trial comparing echodefecography with defecography in the assessment of anorectal dysfunctions in patients with obstructed defecation. Dis Colon Rectum. 2011;54(6):686-92.
- 27. Kottner J, Audige L, Brorson S, Donner A, Gajewski BJ, Hróbjartssonf A, et al. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. Int J Nurs Stud. 2011;48(6):661-71.
- 28. Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol. 2005;26(1):73-7.
- 29. Ornö AK, Dietz HP. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol. 2007;30(3):346-50.
- 30. Santoro GA, Wieczorek AP, Shobeiri SA, Mueller ER, Pilat J, Stankiewicz A, et al. Interobserver and interdisciplinary reproducibility of 3D endovaginal ultrasound assessment of pelvic floor anatomy. Int Urogynecol J. 2011;22(1):53-9.
Correspondence:
Publication Dates
-
Publication in this collection
25 Mar 2013 -
Date of issue
Mar 2013
History
-
Received
13 Nov 2012 -
Accepted
25 Feb 2013