ABSTRACT:
Salmonella is a major cause of foodborne illness worldwide, and poultry and its derived products are the most common food products associated with salmonellosis outbreaks. Some countries, including Brazil, have experienced an increased prevalence of Salmonella Heidelberg among their poultry flocks. Some isolates have also presented high resistance to antimicrobial agents and persist in the poultry farm environment. This study aimed to compare the susceptibility of S. Heidelberg strains isolated in 2006 with those isolated in 2016 against disinfectants and antimicrobial agents. The results showed that all the strains were highly susceptible to sodium hypochlorite, regardless of the conditions and year of isolation. Resistance to benzalkonium chloride varied according to the conditions applied, but not to the year of isolation. Increased antimicrobial resistance from 2006-2016 was observed only for tetracycline. The results suggest that the antimicrobial and disinfectant resistance of S. Heidelberg did not increase for ten years (2006-2016). However, further analysis should include a larger number of S. Heidelberg isolates from poultry origin and additional antimicrobial agents for more precise conclusions about the increasing in antimicrobial resistance in the last years.
INDEX TERMS:
Antimicrobial; disinfectant resistance; Salmonella Heidelberg; poultry flocks; Brazil
RESUMO:
Salmonella é uma das principais causas das doenças transmitidas por alimento em todo o mundo, e a carne de frango e produtos derivados são os principais alimentos associados com surtos de salmonelose em humanos. Alguns países, incluindo o Brasil, têm observado um aumento da ocorrência de Salmonella Heidelberg nas suas granjas avícolas. Além disto, alguns isolados têm apresentado alta resistência aos antimicrobianos e têm persistido no ambiente de produção avícola. Neste contexto, o objetivo deste estudo foi comparar a susceptibilidade de cepas de S. Heidelberg isoladas em 2006 com aquelas isoladas em 2016 contra desinfetantes e agentes antimicrobianos. Os resultados demonstraram que as cepas foram altamente resistentes a hipoclorito de sódio, independentemente das condições e do ano de isolamento. A resistência ao cloreto de benzalcônio variou de acordo com as condições testadas, mas não com o ano de isolamento. Um aumento da resistência aos antimicrobianos de 2006 a 2016 foi observado apenas para tetraciclina. Os resultados sugerem que a resistência aos desinfetantes e aos antimicrobianos não aumentou em um período de dez anos (2006-2016). Entretanto, novas análises devem incluir um número maior de cepas de S. Heidelberg isoladas de fontes avícolas e outros agentes antimicrobianos para uma conclusão mais precisa sobre o aumento da resistência antimicrobiana nos últimos anos.
TERMOS DE INDEXAÇÃO:
Salmonella Heidelberg; avicultura; desinfetante; antimicrobiano; resistência; Brasil
Introduction
Salmonellosis is the second main cause of bacterial enteritis in the European Union (EFSA 2019EFSA 2019. Salmonella control in poultry flocks and its public health impact. EFSA J. 17(2):5596. <https://dx.doi.org/10.2903/j.efsa.2019.5596>
https://doi.org/10.2903/j.efsa.2019.5596...
), and the first in the United States (CDC 2020aCDC 2020a. Salmonella. Centers for Disease Control and Prevention, Atlanta, GA. Available at <Available at https://www.cdc.gov/salmonella/index.html > Accessed on Feb. 5, 2020.
https://www.cdc.gov/salmonella/index.htm...
). Salmonella is a major cause of foodborne illness worldwide, affecting nearly one in ten persons, resulting in approximately 550 million infected people per year (WHO 2020WHO 2020. Antimicrobial resistance. World Health Organization. Available at <Available at https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance > Accessed on Jan. 20, 2020.
https://www.who.int/news-room/fact-sheet...
). The US Centers for Disease Control and Prevention (CDC) reports that poultry and its derived products are the most common food products associated with salmonellosis outbreaks and are responsible for more than 47% of all infections (CDC 2020bCDC 2020b. Making food safer to eat: reducing contamination from the farm to the table. Center for Disease Control and Prevention, Atlanta, GA. Available at <Available at http://www.cdc.gov/vitalsigns/foodsafety > Accessed Mar. 3, 2020.
http://www.cdc.gov/vitalsigns/foodsafety...
).
Data from the Brazilian Ministry of Health show that Salmonella is among the most common pathogens isolated from foodborne diseases in Brazil (Brasil 2019bBrasil 2019b. Surtos de doenças transmitidas por alimentos no Brasil - Informe 2018. Ministério da Saúde, Brasília, DF. Available at <Available at https://portalarquivos2.saude.gov.br/images/pdf/2019/fevereiro/15/Apresenta----o-Surtos-DTA---Fevereiro-2019.pdf > Accessed on Sep. 10, 2020.
https://portalarquivos2.saude.gov.br/ima...
). S. Heidelberg is considered one of the most commonly found serotypes in poultry farming worldwide, and previous studies have shown that strains isolated in recent years are highly resistant to antimicrobials (CDC 2016CDC 2016. Salmonella serotypes isolated from animals and related sources. Centers for Disease Control and Prevention, Atlanta, GA. Available at <Available at https://cdc.gov/nationalsurveillance/pdfs/salmonella-serotypesisolated-animals-and-related-sources-508.pdf > Accessed on Jul. 22, 2020.
https://cdc.gov/nationalsurveillance/pdf...
, EFSA 2019EFSA 2019. Salmonella control in poultry flocks and its public health impact. EFSA J. 17(2):5596. <https://dx.doi.org/10.2903/j.efsa.2019.5596>
https://doi.org/10.2903/j.efsa.2019.5596...
, Neves et al. 2020Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027.). In recent years, there has been an increase in the prevalence of Salmonella Heidelberg, especially in the United States and Brazil (CDC 2016CDC 2016. Salmonella serotypes isolated from animals and related sources. Centers for Disease Control and Prevention, Atlanta, GA. Available at <Available at https://cdc.gov/nationalsurveillance/pdfs/salmonella-serotypesisolated-animals-and-related-sources-508.pdf > Accessed on Jul. 22, 2020.
https://cdc.gov/nationalsurveillance/pdf...
, Brasil 2019aBrasil 2019a. Nota Técnica: entenda melhor - Salmonela em carne de frango. Ministério da Agricultura, Pecuária e Abastecimento, Brasília, DF. Available at <Available at https://www.gov.br/agricultura/pt-br/assuntos/inspecao/produtos-animal/arquivos-publicacoes-dipoa/entenda-melhor-salmonela-em-carne-de-frango > Accessed on Jul. 22, 2020.
https://www.gov.br/agricultura/pt-br/ass...
).
Bacterial resistance to antimicrobials and disinfectants has increased considerably over the years, mainly because of their inadequate use in human and veterinary medicine (FAO 2016FAO 2016. The FAO action plan on antimicrobial resistance 2016-2020. Food and Agriculture Organization of the United Nations, Rome. Available at <Available at http://www.fao.org/3/a-i5996e.pdf > Accessed on Jun. 23, 2020.
http://www.fao.org/3/a-i5996e.pdf...
). Recent studies have demonstrated increasing resistance of Salmonella strains isolated from humans and animals to the most commonly used antibiotics (Borges et al. 2019Borges K.A., Furian T.Q., de Souza S.N., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2019. Antimicrobial resistance and molecular characterization of Salmonella enterica serotypes isolated from poultry sources in Brazil. Braz. J. Poult. Sci. 21(1):1-8. <https://dx.doi.org/10.1590/1806-9061-2018-0827>
https://doi.org/10.1590/1806-9061-2018-0...
, EFSA 2020EFSA 2020. The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2017/2018. EFSA J. 18(3):6007. <http://doi.org/10.2903/j.efsa.2020.6007>
https://doi.org/10.2903/j.efsa.2020.6007...
, Elhariri et al. 2020Elhariri M., Elhelw R., Selim S., Ibrahim M., Hamza D. & Hamza E. 2020. Virulence and antibiotic resistance patterns of extended-spectrum beta-lactamase-producing Salmonella enterica serovar Heidelberg isolated from broiler chickens and poultry workers: a potential hazard. Foodborne Pathog. Dis. 17(6):373-381. <https://dx.doi.org/10.1089/fpd.2019.2719> <PMid:31755782>
https://doi.org/10.1089/fpd.2019.2719...
, Souza et al. 2020Souza A.I.S., Saraiva M.M.S., Casas M.R.T., Oliveira G.M., Cardozo M.V., Benevides V.P., Barbosa F.O., Freitas Neto O.C., Almeida A.M. & Berchieri Junior A. 2020. High occurrence of β-lactamase-producing Salmonella Heidelberg from poultry origin. PLoS One 15:1-11. <https://dx.doi.org/10.1371/journal.pone.0230676> <PMid:32231395>
https://doi.org/10.1371/journal.pone.023...
). Despite the development of several alternative products for pathogen control in the food processing chain, the best viable protection against foodborne pathogens are disinfectants and biosecurity (Bragg et al. 2018Bragg R.R., Meyburgh C.M., Lee J.-Y. & Coetzee M. 2018. Potential treatment options in a post-antibiotic era. Adv Exp Med Biol. 1052:51-61. <https://dx.doi.org/10.1007/978-981-10-7572-8_5> <PMid:29785480>
https://doi.org/10.1007/978-981-10-7572-...
, Mc Carlie et al. 2020Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
https://doi.org/10.1016/j.drup.2019.1006...
). Thus, it is of concern that disinfectant resistance could rapidly increase (Mc Carlie et al. 2020Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
https://doi.org/10.1016/j.drup.2019.1006...
). However, unlike antimicrobials, the possible resistance to disinfectants traditionally used in the poultry industry has not been elucidated.
In recent years, the specific resurgence of the serotype S. Heidelberg, followed by its resistance to control programs, has worsened worldwide, including in Brazil (Colla et al. 2012Colla F.L., Rodrigues L.B., Dickel E.L., Borsoi A., Nascimento V.P. & Santos L.R. 2012. Avaliação in vitro de clorexidina, amônia quaternária e ácido peracético frente a amostras de Salmonella Heidelberg isoladas de abatedouro avícola em 2005 e 2009. Pesq. Vet. Bras. 32(4):289-292. <https://dx.doi.org/10.1590/S0100-736X2012000400003>
https://doi.org/10.1590/S0100-736X201200...
, Gieraltowski et al. 2016Gieraltowski L., Higa J., Peralta V., Green A., Schwensohn C., Rosen H., Libby T., Kissler B., Marsden-Haug N., Booth H., Kimura A., Grass J., Bicknese A., Tolar B., Defibaugh-Chávez S., Williams I. & Wise M. 2016. National outbreak of multidrug resistant Salmonella Heidelberg infections linked to a single poultry company. PLoS One 11(9):e0162369. <https://dx.doi.org/10.1371/journal.pone.0162369> <PMid:27631492>
https://doi.org/10.1371/journal.pone.016...
, Stefani et al. 2018Stefani L.M., Neves G.B., Brisola M.C., Crecencio R.B., Pick E.C. & Araujo D.N. 2018. Salmonella Heidelberg resistant to ceftiofur and disinfectants routinely used in poultry. Semina, Ciênc. Agrárias 39(3):1029-1036. <https://dx.doi.org/10.5433/1679-0359.2018v39n3p1029>
https://doi.org/10.5433/1679-0359.2018v3...
, Etter et al. 2019Etter A.J., West A.M., Burnett J.L., Wu S.T., Veenhuizen D.R., Ogas R.A. & Oliver H.F. 2019. Salmonella enterica subsp. enterica Serovar Heidelberg food isolates associated with a salmonellosis outbreak have enhanced stress tolerance capabilities. App. Env. Microbiol. 85(16):e01065-19. <https://dx.doi.org/10.1128/AEM.01065-19> <PMid:31175193>
https://doi.org/10.1128/AEM.01065-19...
, Voss-Rech et al. 2019Voss-Rech D., Kramer B., Silva V.S., Rebelatto R., Abreu P.G., Coldebella A. & Vaz C.S.L. 2019. Longitudinal study reveals persistent environmental Salmonella Heidelberg in Brazilian broiler farms. Vet. Microbiol. 233:118-123. <https://dx.doi.org/10.1016/j.vetmic.2019.04.004>
https://doi.org/10.1016/j.vetmic.2019.04...
). In view of the epidemiological situation in Brazil, the present study aimed to compare the susceptibility of S. Heidelberg strains isolated in 2006 with those isolated in 2016 from poultry sources against two disinfectants and six antimicrobials.
Materials and Methods
Salmonella Heidelberg isolates
A total of 40 S. Heidelberg strains were selected for this study. The strains were isolated in two periods: 2006 (n=20) and 2016 (n=20) from poultry sources (drag swabs, cloacal swab, and chicken carcasses) in Southern Brazil (Table 1). The strains were previously isolated, biochemically characterized, and serotyped. All strains were stored frozen at -80°C in brain heart infusion broth (BHI) (Merck, Darmstadt, Germany) supplemented with 15% glycerin (Synth, Diadema, Brazil). The bacteria were retrieved from frozen culture stocks and cultured overnight at 37°C in xylose lysine deoxycholate (XLD) agar (Merck, Darmstadt, Germany) and incubated at 37°C for 24h. One colony morphologically characteristic of Salmonella spp. was selected and inoculated in BHI and incubated again at 37°C for 24h.
Disinfectant test
Inoculum preparation. To prepare the inoculum, McFarland standard no. 0.5 (Probac do Brasil, São Paulo, Brazil) was used as a reference to adjust the turbidity of the bacterial suspension in 0.1% buffered peptone water (BPW) (Oxoid, Basingstoke, England) to a concentration of 108CFU/mL, corresponding to an optical density interval of 0.08-0.1 in a spectrophotometer (SP 22; Biospectro, Curitiba, Brazil) at a wavelength of 625nm (CLSI 2013aCLSI 2013a. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-A4, Approved Standard - Fourth Edition, Clinical and Laboratory Standards Institute, Wayne, PA.). The bacterial suspension was diluted in 0.1% BPW to a concentration of 106CFU/mL.
Concentrations, time of exposure, temperature conditions, and neutralizer solution. Two commercially available disinfectants were evaluated: sodium hypochlorite (MediQuímica, Juiz de Fora, Brazil) and chloride benzalkonium (Exodus Científica, Sumaré, Brazil). Sodium hypochlorite was evaluated at 0.5% and 1.0%, and benzalkonium chloride at 100 and 200ppm, following the manufacturer’s recommendations for use in poultry industries. Dilutions were performed in sterile distilled water. The products were evaluated at two temperatures: 25°C, to simulate a cleaning scenario, and 12°C, the maximum temperature allowed in cutting rooms, according to Brazilian legislation (Brasil 1998Brasil 1998. Portaria nº 210: regulamento técnico da inspeção tecnológica e higiênico-sanitária de carne de aves. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.). A solution of 1% bovine fetal serum (Gibco, Thermo Fisher Scientific, Waltham, USA) was used to simulate the presence of organic matter. Two exposure times (5 and 15 min) were tested to mimic the cleaning and disinfection processes in the poultry industry. A neutralizer solution was used to inactivate the antimicrobial effect of the disinfectant. The neutralizer was composed of polysorbate Tween 80 (Neon, São Paulo, Brazil), 2g of soy lecithin (Stem, Porto Alegre, Brazil), and 2g of sodium thiosulfate (Dynamic, Diadema, Brazil).
Evaluation test. The evaluation test was performed according to Brazilian legislation guidelines (Brasil 1993Brasil 1993. Portaria nº 101: métodos de análise microbiológica para alimentos. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.) for suspension test in planktonic cells. Briefly, 0.1mL of the inoculum was inoculated in 9.9mL of each disinfectant containing 1% bovine fetal serum. After the exposure time, 10μL of the suspension was inoculated in BHI with a neutralizer solution. The materials were incubated at 37°C for 96h. Tubes presenting turbidity, surface film formation, or background precipitate were considered positive (non-susceptible strains). The tube was considered negative (susceptible strains) when no growth was observed after 96h of incubation. Bacterial viability was confirmed by reseeding an aliquot in the XLD. Plates were incubated at 37°C for 24h.
Minimum inhibitory concentration (MIC)
Inoculum preparation. The bacteria were cultured overnight at 37°C in trypticase soy agar (TSA) (Oxoid, Basingstoke, England). To prepare the inoculum, McFarland standard no. 0.5 (Probac do Brasil, São Paulo, Brazil) was used as a reference to adjust the turbidity of the bacterial suspension in 0.85% saline solution (NaCl; Synth, Diadema, Brazil) to a concentration of 108CFU/mL, corresponding to an optical density interval of 0.08-0.1 in a spectrophotometer (SP 22; Biospectro, Curitiba, Brazil) at a wavelength of 625nm (CLSI 2013aCLSI 2013a. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-A4, Approved Standard - Fourth Edition, Clinical and Laboratory Standards Institute, Wayne, PA.). The bacterial suspension was diluted in cation-adjusted Muller-Hinton broth (CAMBH) (Honeywell Fluka - Fisher Scientific, Loughborough, UK) to reach a concentration of 107CFU/mL.
Antimicrobials and MIC determination. As described by the Clinical and Laboratory Standards Institute (CLSI 2013bCLSI 2013b. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-S2, Second Information Supplement, Clinical and Laboratory Standards Institute, Wayne, PA.), a broth microdilution test was performed to determine the MIC for antimicrobial agents (Sigma-Aldrich, St. Louis, US): gentamicin (0.25-128μg/mL), chloramphenicol (2-128μg/mL), nalidixic acid (1-128μg/mL), ciprofloxacin (0.008-16μg/mL), enrofloxacin (0.008-16μg/mL), and tetracycline (0.5-64μg/mL). The strains were classified as susceptible or non-susceptible (including intermediate strains), according to the breakpoints described in the CLSI standards (CLSI 2013bCLSI 2013b. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-S2, Second Information Supplement, Clinical and Laboratory Standards Institute, Wayne, PA., 2020CLSI 2020. Performance standards for antimicrobial susceptibility testing. M100-30, Clinical and Laboratory Standards Institute, Wayne, PA. Available at <Available at http://em100.edaptivedocs.net/dashboard.aspx > Accessed on May 3, 2020.
http://em100.edaptivedocs.net/dashboard....
). The interpretation of MIC values for enrofloxacin was performed according to previously available data (Hao et al. 2013Hao H., Pan H., Ahmad I., Cheng G., Wang Y., Dai M., Tao Y., Chen D., Peng D., Liu Z., Huang L. & Yuan Z. 2013. Susceptibility breakpoint of enrofloxacin against swine Salmonella spp. J. Clin. Microbiol 51(9):3070-3072. <https://dx.doi.org/10.1128/JCM.01096-13> <PMid:23784134>
https://doi.org/10.1128/JCM.01096-13...
). The strains were also classified as wild type (WT) or non-wild type (nWT) based on their epidemiological MIC cutoff (ECOFFs), which were determined according to the EUCAST guidelines available at the time of data analysis (EUCAST 2020EUCAST 2020. Antimicrobial wild type distributions of microorganisms. European Committee on Antimicrobial Susceptibility Testing. Available at <Available at https://mic.eucast.org/Eucast2/ > Accessed on May 3, 2020.
https://mic.eucast.org/Eucast2/...
). An Escherichia coli reference strain (ATCC 325922) was selected to ensure the validity of the tests. The strains that were resistant to three or more classes of antimicrobials were classified as multidrug-resistant (MDR) strains (Schwarz et al. 2010Schwarz S., Silley P., Simjee S., Woodford N., Van Duijkeren E., Johnson A.P. & Gaastra W. 2010. Editorial: assessing the antimicrobial susceptibility of bacteria obtained from animals. J. Antimicrob. Chemother. 65(4):601-604. <https://dx.doi.org/10.1093/jac/dkq037> <PMid:20181573>
https://doi.org/10.1093/jac/dkq037...
). The multiple antibiotic resistance (MAR) index was determined as previously described (Krumperman 1983Krumperman P.H. 1983. Multiple Antibiotic Resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Env. Microbiol. 46(1):165-170. <https://dx.doi.org/10.1128/aem.46.1.165-170.1983> <PMid:6351743>
https://doi.org/10.1128/aem.46.1.165-170...
). Both MDR and MAR were defined according to CLSI breakpoints.
Statistical analysis
The data were subjected to descriptive statistical analysis using PASW Statistics software (IBM, Hong Kong). Fisher’s exact test was used to compare the periods (2006 and 2016), temperatures (12°C and 25°C), concentrations (100 and 200ppm), and time of exposure (5 and 15min) in the disinfectant test. A 5% level of significance was applied for all tests. The kappa index (Landis & Koch 1977Landis J.R. & Koch G.G. 1977. The measurement of observer agreement for categorical data. Biometrics 33(1):159-174. <https://dx.doi.org/10.2307%2F2529310> <PMid:843571>
https://doi.org/10.2307%2F2529310...
) was used to evaluate the concordance between the classifications based on the CLSI breakpoints and ECOFF values.
Results
Disinfectant tests
The individual results of the susceptibility tests of the disinfectants are described as supplementary material. The strains were highly susceptible to sodium hypochlorite. Among the 20 strains of Salmonella Heidelberg isolated in 2006, only two (10%) were non-susceptible to sodium hypochlorite 0.5%, both at 25°C and after 5 min of contact. All the strains isolated in 2016 were susceptible, regardless of the temperature, concentration of disinfectant, and contact time. In relation to benzalkonium chloride susceptibility, different frequencies of non-susceptible strains were observed for both groups (Table 2). The comparison of S.Heidelberg susceptibility to benzalkonium chloride between strains isolated in 2006 and those isolated in 2016 showed a significant increase in the number of non-susceptible strains only at 200ppm, after a contact time of 5min at 25°C. There were no differences (p>0.05) between the frequencies of the non-susceptible strains isolated in different years when other conditions of temperature, exposure time, and disinfectant concentration were considered (Table 2). Comparisons among the tested conditions for benzalkonium chloride revealed no differences (p>0.05) in the total number of non-susceptible strains between temperatures. The increase in the exposure time led to a significant (p<0.05) decrease in the number of non-susceptible strains isolated in 2016, regardless of the temperature and the concentration of the disinfectant. For strains isolated in 2006, a significant difference (p<0.05) was observed only at 25°C, with a concentration of 100ppm.
Minimum inhibitory concentration
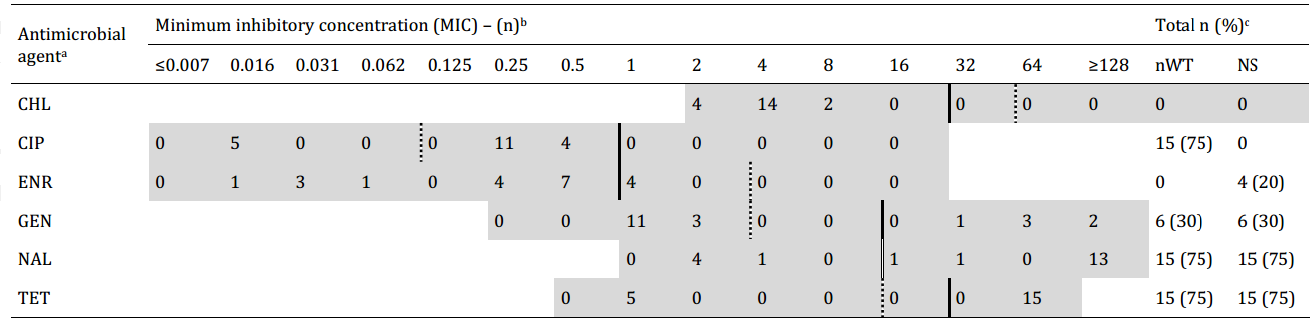
The phenotypic antimicrobial resistance profiles of each strain are described in Table 1. The MIC results are described in Figure 1 and 2. According to the CLSI breakpoints, 45% (9/20) of the strains isolated in 2006 and 20% (4/20) of those from 2016 were susceptible to all the antimicrobials. When ECOFF values were considered, 40% (8/20) of the strains isolated in 2006 and 25% (5/20) of those isolated in 2016 were classified as wild type to all the antimicrobials. There was no significant (p>0.05) difference in overall resistance between the two periods of isolation, regardless of the breakpoint evaluated. Considering all the strains of S. Heidelberg, regardless of the year of isolation, chloramphenicol, nalidix acid, and tetracycline presented similar results between the CLSI and EUCAST breakpoints (Fig.1 and 2). Ciprofloxacin, gentamicin, and enrofloxacin presented significant (p<0.05) differences in antimicrobial susceptibility according to the breakpoint evaluated. Resistance to ciprofloxacin and gentamicin was higher according to the EUCAST parameters compared to the CLSI breakpoints. Resistance to enrofloxacin was lower according to the EUCAST breakpoints. To measure the agreement between the EUCAST and the CLSI breakpoints, a kappa test was applied when the results were different. It showed almost perfect agreement for gentamicin (κ = 0.846), substantial agreement for enrofloxacin (κ = 0.780), and fair agreement (κ = 0.246) for ciprofloxacin (Landis & Koch 1977Landis J.R. & Koch G.G. 1977. The measurement of observer agreement for categorical data. Biometrics 33(1):159-174. <https://dx.doi.org/10.2307%2F2529310> <PMid:843571>
https://doi.org/10.2307%2F2529310...
). The statistical analyses results showed a significant (p<0.05) increase in resistance to tetracycline in strains isolated in 2016 compared to those isolated in 2006, regardless of the breakpoint evaluated. However, there was no significant difference (p>0.05) in resistance to chloramphenicol, ciprofloxacin, enrofloxacin, gentamicin, and nalidixic acid. For both breakpoints, a higher resistance to nalidix acid was observed among strains isolated in 2006. Among strains from 2016, the highest resistance rates were observed for tetracycline and nalidixic acid. Multidrug-resistant strains were identified only among strains from 2016 and represented 20% (4/20) of the total. The individual maximum and minimum multiple-antibiotic resistance (MAR) indices for the strains isolated in 2006 were 0.3 and 0.1, respectively, with an average index of 0.1. Among those isolated in 2016, the maximum and minimum MAR indices were 0.7 and 0.3, respectively, with an average index of 0.3.
Minimum inhibitory concentration (MIC) results for the strains isolated in 2006: non-susceptible strains (CLSI breakpoints) and non-wildtype strains (ECOFF values). a Chloramphenicol (CHL), ciprofloxacin (CIP), enrofloxacin (ENR), gentamycin (GEN), nalidixic acid (NAL), tetracycline (TET). b MIC breakpoints, according to CLSI guidelines, also include “intermediate” strains, which are considered non-susceptible. c Non-wild type (nWT), according to ECOFF values (EUCAST breakpoints). Non-susceptible (NS), according to CLSI breakpoints. Continuous lines indicate CLSI breakpoints. Dotted lines indicate ECOFF values (EUCAST breakpoints). Double lines indicate that CLSI breakpoints and ECOFF values are the same. Shaded areas indicate the tested concentrations.
Minimum inhibitory concentration (MIC) results for the strains isolated in 2016: non-susceptible strains (CLSI breakpoints) and non-wildtype strains (ECOFF values). a Chloramphenicol (CHL), ciprofloxacin (CIP), enrofloxacin (ENR), gentamycin (GEN), nalidixic acid (NAL), tetracycline (TET). b MIC breakpoints, according to CLSI guidelines, also include “intermediate” strains, which are considered non-susceptible. c Non-wild type (nWT), according to ECOFF values (EUCAST breakpoints). Non-susceptible (NS) according to CLSI breakpoints. Continuous lines indicate CLSI breakpoints. Dotted lines indicate ECOFF values (EUCAST breakpoints). Double lines indicate that CLSI breakpoints and ECOFF values are the same. Shaded areas indicate the tested concentrations.
Discussion
Brazil is a leading supplier of poultry meat in the world, and the states of Rio Grande do Sul, Santa Catarina, and Paraná in the southern region are responsible for more than 64% of the total poultry slaughter (ABPA 2020ABPA 2020. Relatório Anual, 2020. Associação Brasileira de Proteína Animal. Available at <Available at http://abpa-br.org/wp-content/uploads/2020/05/abpa_relatorio_anual_2020_portugues_web.pdf > Accessed on Jun. 18, 2020.
http://abpa-br.org/wp-content/uploads/20...
). The spread of diseases, especially foodborne diseases, such as salmonellosis, represents a major economic and public health problem for these states. In the last few years, studies have reported the presence of persistent environmental Salmonella Heidelberg in Brazilian broiler farms, especially in the southern region (Duarte 2018Duarte S.C. 2018. Epidemiologia dos principais sorotipos de salmonela circulantes na avicultura brasileira. Simpósio Salmonella: cenários e desafios, Porto Alegre, RS., Voss-Rech et al. 2019Voss-Rech D., Kramer B., Silva V.S., Rebelatto R., Abreu P.G., Coldebella A. & Vaz C.S.L. 2019. Longitudinal study reveals persistent environmental Salmonella Heidelberg in Brazilian broiler farms. Vet. Microbiol. 233:118-123. <https://dx.doi.org/10.1016/j.vetmic.2019.04.004>
https://doi.org/10.1016/j.vetmic.2019.04...
). In addition, increased antibiotic resistance of S. Heidelberg has been reported in this region (Neves et al. 2020Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027.).
Previous studies have shown that the S. Heidelberg strains isolated in 2016 and 2017 were capable of producing biofilms at 25°C (Lucca et al. 2020Lucca V., Borges K.A., Furian T.Q., Borsoi A., Salle C.T.P., Moraes H.L.S. & Nascimento V.P. 2020. Influence of the norepinephrine and medium acidification in the growth and adhesion of Salmonella Heidelberg isolated from poultry. Microb. Pathog. 138:103799. <https://dx.doi.org/10.1016/j.micpath.2019.103799>
https://doi.org/10.1016/j.micpath.2019.1...
). However, it is important to note that strains isolated from 1996-2006 also have the ability to produce biofilms at similar temperatures (28°C) (Borges et al. 2018Borges K.A., Furian T.Q., Souza S.N., Menezes R., Tondo E.C., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2018. Biofilm formation capacity of Salmonella serotypes at different temperature conditions. Pesq. Vet. Bras. 38(1):71-76. <https://dx.doi.org/10.1590/1678-5150-pvb-4928>
https://doi.org/10.1590/1678-5150-pvb-49...
). Thus, it is probable that the surface adherence capability is not enough to explain and justify the increased isolation and difficulty of the Brazilian poultry chain in removing this serotype from flocks in recent years.
In this context, we evaluated and compared the disinfectant and antibiotic resistance between strains isolated in two periods of time (2006 and 2016). The disinfectant test was performed to evaluate the susceptibility of the tested isolates in the planktonic phase. Sodium hypochlorite and benzalkonium chloride concentrations and contact times were tested as recommended by the manufacturer. In addition, we evaluated a lower concentration, simulating under dosage situations. The antibiotics were selected based on their importance for human and veterinary use.
Sodium hypochlorite is widely used in the food industry as a disinfectant, despite the increasing availability of other products. The main advantages are the low cost, broad antimicrobial spectrum, rapid bactericidal action, and low toxicity to humans and animals (Fukuzaki 2006Fukuzaki S. 2006. Mechanisms of actions of sodium hypochlorite in cleaning and disinfection processes. Biocontrol Sci. 11(4):147-157. <https://dx.doi.org/10.4265/bio.11.147> <PMid:17190269>
https://doi.org/10.4265/bio.11.147...
). The antimicrobial effectiveness of sodium hypochlorite is based on its high pH (hydroxyl ion action), which interferes with the cytoplasmic membrane integrity with an irreversible enzymatic inhibition, biosynthetic alterations in cellular metabolism, and phospholipid degradation observed in lipidic peroxidation (Estrela et al. 2002Estrela C., Estrela C.R.A., Barbin E.L., Spanó J.C.E., Marchesan M.A. & Pécora J.D. 2002. Mechanism of action of sodium hypochlorite. Braz. Dent. J. 13(2):113-117. <https://dx.doi.org/10.1590/s0103-64402002000200007> <PMid:12238801>
https://doi.org/10.1590/s0103-6440200200...
). In the current study, the strains seemed to be highly susceptible to sodium hypochlorite, regardless of the year of isolation and the conditions employed. It is important to highlight that sodium hypochlorite efficacy is highly dependent on organic load (Köhler et al. 2018Köhler A.T., Rodloff A.C., Labahn M., Reinhardt M., Truyen U. & Speck S. 2018. Efficacy of sodium hypochlorite against multidrug-resistant Gram-negative bacteria. J. Hosp. Infec. 100(3):E40-E46. <https://dx.doi.org/10.1016/j.jhin.2018.07.017>
https://doi.org/10.1016/j.jhin.2018.07.0...
), which was simulated by 1% bovine fetal serum. Although specific strains and species differences have been observed (Köhler et al. 2018Köhler A.T., Rodloff A.C., Labahn M., Reinhardt M., Truyen U. & Speck S. 2018. Efficacy of sodium hypochlorite against multidrug-resistant Gram-negative bacteria. J. Hosp. Infec. 100(3):E40-E46. <https://dx.doi.org/10.1016/j.jhin.2018.07.017>
https://doi.org/10.1016/j.jhin.2018.07.0...
), the higher susceptibility of the strains to this disinfectant has already been described by other researchers for several pathogens, including against multidrug-resistant bacteria (Köhler et al. 2018Köhler A.T., Rodloff A.C., Labahn M., Reinhardt M., Truyen U. & Speck S. 2018. Efficacy of sodium hypochlorite against multidrug-resistant Gram-negative bacteria. J. Hosp. Infec. 100(3):E40-E46. <https://dx.doi.org/10.1016/j.jhin.2018.07.017>
https://doi.org/10.1016/j.jhin.2018.07.0...
, Borges et al. 2020Borges T.J., Moretti L.K., Silva M.M.N., Tondo E.C. & Pereira K.S. 2020. Salmonella sensitivity to sodium hypochlorite and citric acid in washing water of lettuce residues. J. Food Safety 40(2):e12748. <https://dx.doi.org/10.1111/jfs.12748>
https://doi.org/10.1111/jfs.12748...
).
Benzalkonium chloride is a broad spectrum quaternary ammonium antibacterial agent with widespread applications. Several mechanisms of action have been described, mostly related to the cell membrane, such as changes in the overall membrane composition and downregulation of porins (Pereira & Tagkopoulos 2019Pereira B.M.P. & Tagkopoulos I. 2019. Benzalkonium chlorides: uses, regulatory status, and microbial resistance. Appl. Environ. Microbiol. 85(13):e00377-19. <https://dx.doi.org/10.1128/AEM.00377-19> <PMid:31028024>
https://doi.org/10.1128/AEM.00377-19...
). In the current study, a large number of the strains were not susceptible to benzalkonium chloride for both years of isolation. However, a significant increase in the resistance of the strains isolated in 2016 was observed only when the strains were exposed to 200ppm for 5 min at 25°C. Low susceptibility to benzalkonium chloride has been previously described for some Salmonella serotypes (Long et al. 2016Long M., Lai H., Deng W., Zhou K., Li B., Liu S., Fan L., Wang H. & Zou L. 2016. Disinfectant susceptibility of different Salmonella serotypes isolated from chicken and egg production chains. J. Appl. Microbiol. 121(3):672-681. <https://dx.doi.org/10.1111/jam.13184> <PMid:27206326>
https://doi.org/10.1111/jam.13184...
). Its effectiveness is reduced against Gram-negative bacteria, such as Salmonella spp., owing to the outer membrane, once the lipopolysaccharide layer act as a barrier against harmful external conditions (Bragg et al. 2014Bragg R., Jansen A., Coetzee M., van der Westhuizen W. & Boucher C. 2014. Bacterial resistance to quaternary ammonium compounds (QAC) disinfectants. Adv. Exp. Med. Biol. 808:1-13. <https://dx.doi.org/10.1007/978-81-322-1774-9_1> <PMid:24595606>
https://doi.org/10.1007/978-81-322-1774-...
). The efflux pump system may be another possible mechanism of resistance, and at least nine genes have been described for the Salmonella genus. Among them, three (acrAB, acrEF, and mdsABC) are known to expel benzalkonium chloride from the cell (Møretrø et al. 2012Møretrø T., Heir E., Nesse L.L., Vestby L.K. & Langsrud S. 2012. Control of Salmonella in food related environments by chemical disinfection. Food Res. Int. 45(2):532-544. <https://dx.doi.org/10.1016/j.foodres.2011.02.002>
https://doi.org/10.1016/j.foodres.2011.0...
). Most studies did not find significant differences in resistance based on the temperature of incubation in in vitro tests with Salmonella serotypes (Kich et al. 2004Kich J.D., Borowsky L.M., Silva V.S., Ramenzoni M., Triques N., Kooler F.L. & Cardoso M.R.I. 2004. Avaliação da atividade antibacteriana de seis desinfetantes comerciais frente a amostras de Salmonella Typhimurium isoladas de suínos. Acta Scient. Vet. 32(1):33-39. <https://dx.doi.org/10.22456/1679-9216.16792>
https://doi.org/10.22456/1679-9216.16792...
, Stringfellow et al. 2009Stringfellow K., Anderson P., Caldwell D., Lee J., Byrd J., McReynolds J., Carey J., Nisbet D. & Farnell M. 2009. Evaluation of disinfectants commonly used by the commercial poultry industry under simulated field conditions. Poult. Sci. 88(6):1151-1155. <https://dx.doi.org/10.3382/ps.2008-00455> <PMid:19439623>
https://doi.org/10.3382/ps.2008-00455...
, Jaenisch et al. 2010Jaenisch F.R.F., Kuchiishi S.S. & Coldebella A. 2010. Atividade antibacteriana de desinfetantes para uso na produção orgânica de aves. Ciência Rural 40(2):384-388. <https://dx.doi.org/10.1590/S0103-84782010000200020>
https://doi.org/10.1590/S0103-8478201000...
). However, Camilotti et al. (2015)Camilotti E., Rocha S.L.S., Tejkowski T.M., Moraes H.L.S., Salle C.T.P. & Avancini C.A.M. 2015. Simulação de condições de uso de quaternário de amônio frente amostras de Salmonella Hadar isoladas de carcaças de frango. Revta Bras. Saúde Prod. Anim. 16(1):66-72. <https://dx.doi.org/10.1590/S1519-99402015000100008>
https://doi.org/10.1590/S1519-9940201500...
found that benzalkonium chloride activity was reduced at 8°C in relation to 20°C when tested against S. Hadar. In addition, the mechanisms of resistance to benzalkonium chloride may also be related to the conditions of use, especially according to the amount of organic matter, not only by the resistance profile of Salmonella strains (Kich et al. 2004Kich J.D., Borowsky L.M., Silva V.S., Ramenzoni M., Triques N., Kooler F.L. & Cardoso M.R.I. 2004. Avaliação da atividade antibacteriana de seis desinfetantes comerciais frente a amostras de Salmonella Typhimurium isoladas de suínos. Acta Scient. Vet. 32(1):33-39. <https://dx.doi.org/10.22456/1679-9216.16792>
https://doi.org/10.22456/1679-9216.16792...
).
Brazilian reports have shown decreased susceptibility to chlorhexidine, but higher susceptibility to sodium hypochlorite and benzalkonium chloride among S. Heidelberg strains (Colla et al. 2012Colla F.L., Rodrigues L.B., Dickel E.L., Borsoi A., Nascimento V.P. & Santos L.R. 2012. Avaliação in vitro de clorexidina, amônia quaternária e ácido peracético frente a amostras de Salmonella Heidelberg isoladas de abatedouro avícola em 2005 e 2009. Pesq. Vet. Bras. 32(4):289-292. <https://dx.doi.org/10.1590/S0100-736X2012000400003>
https://doi.org/10.1590/S0100-736X201200...
, Stefani et al. 2018Stefani L.M., Neves G.B., Brisola M.C., Crecencio R.B., Pick E.C. & Araujo D.N. 2018. Salmonella Heidelberg resistant to ceftiofur and disinfectants routinely used in poultry. Semina, Ciênc. Agrárias 39(3):1029-1036. <https://dx.doi.org/10.5433/1679-0359.2018v39n3p1029>
https://doi.org/10.5433/1679-0359.2018v3...
). Studies evaluating the susceptibility of S. Heidelberg serotype to disinfectants are still uncommon. Our findings demonstrate that the resistance to disinfectants did not increase over time among the analyzed strains, although this result has been observed previously. Riazi & Matthews (2011)Riazi S. & Matthews K.R. 2011. Failure of foodborne pathogens to develop resistance to sanitizers following repeated exposure to common sanitizers. Int. Biodet. Biodegr. 65(2):374-378. <https://dx.doi.org/10.1016/j.ibiod.2010.12.001>
https://doi.org/10.1016/j.ibiod.2010.12....
evaluated the susceptibility of foodborne pathogens to common disinfectants after repeated exposure, and they observed that the bacterial pathogens tested remain susceptible under the conditions evaluated.
Antimicrobial resistance represents a public health risk owing to the decrease in available treatment options for patients. In addition, it increases the costs of healthcare for these patients. Thus, this is a serious threat that requires immediate action worldwide (WHO 2020WHO 2020. Antimicrobial resistance. World Health Organization. Available at <Available at https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance > Accessed on Jan. 20, 2020.
https://www.who.int/news-room/fact-sheet...
). It has already been proven that the increase in antimicrobial resistance is closely related to the use of these substances, which leads to selection pressure and consequently to the emergence of non-susceptible strains (Balsalobre et al. 2014Balsalobre L.C., Dropa M. & Matté M.H. 2014. An overview of antimicrobial resistance and its public health significance. Braz. J. Microbiol. 45(1):1-5. <https://dx.doi.org/10.1590/S1517-83822014005000033> <PMid:24948906>
https://doi.org/10.1590/S1517-8382201400...
, WHO 2020WHO 2020. Antimicrobial resistance. World Health Organization. Available at <Available at https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance > Accessed on Jan. 20, 2020.
https://www.who.int/news-room/fact-sheet...
).
To determine whether resistance increased over time and may have contributed to the persistence of S. Heidelberg in the flock, the current study evaluated the antimicrobial resistance of both groups to commonly used antimicrobials. Our results indicate that despite the overall increase in resistance from 2006-2016, the differences were not significant for both of the breakpoints evaluated (CLSI and EUCAST). As the misuse of antimicrobials in humans and animals over time may accelerate the process of resistance, the results were unexpected. However, these findings are not unique. A recent study analyzing the antimicrobial resistance of Salmonella strains isolated over 20 years reported increased resistance rates to third-generation cephalosporins, but not to quinolones and sulfonamides (Lo et al. 2020Lo H.-Y., Lai F.-P. & Yang Y.-J. 2020. Changes in epidemiology and antimicrobial susceptibility of nontyphoid Salmonella in children in southern Taiwan, 1997-2016. J. Microbiol. Immunol. Infect. 53(4):585-591. <https://dx.doi.org/10.1016/j.jmii.2018.06.004> <PMid:30017562>
https://doi.org/10.1016/j.jmii.2018.06.0...
). The detection of MDR strains among the S. Heidelberg strains isolated in 2016 was an indicator of an increase in antimicrobial resistance over time. However, this situation is probably due to a higher number of resistant strains to only one antimicrobial, tetracycline, in 2016.
The MAR index can be applied to differentiate low (MAR < 0.2) and high-risk (MAR > 0.2) regions where antimicrobials are overused (Proroga et al. 2016Proroga Y.T.R., Capuano F., Carullo M.R., La Tela I., Capparelli R., Barco L. & Pasquale V. 2016. Occurrence and antimicrobial resistance of Salmonella strains from food of animal origin in southern Italy. Folia Microbiol. 61(1):21-27. <https://dx.doi.org/10.1007/s12223-015-0407-x> <PMid:26084745>
https://doi.org/10.1007/s12223-015-0407-...
). Strains isolated in 2016 presented an average index of 0.3, which could indicate high antibiotic usage and high selective pressure. However, the widespread use of antibiotics in developing countries, including Brazil, probably reduces the practical significance of this finding (Davis & Brown 2016Davis R. & Brown P.D. 2016. Multiple antibiotic resistance index, fitness and virulence potential in respiratory Pseudomonas aeruginosa from Jamaica. J. Med. Microbiol. 65(4):261-271. <https://dx.doi.org/10.1099/jmm.0.000229> <PMid:26860081>
https://doi.org/10.1099/jmm.0.000229...
).
The MIC results are based on pre-established breakpoints, including those from EUCAST and CLSI agencies. The variations in the breakpoints can result in significant changes in the final MIC, which will affect clinical decisions and official data reports (Kassim et al. 2016Kassim A., Omuse G., Premji Z. & Revathi G. 2016. Comparison of Clinical Laboratory Standards Institute and European Committee on Antimicrobial Susceptibility Testing guidelines for the interpretation of antibiotic susceptibility at a University teaching hospital in Nairobi, Kenya: a cross-sectional study. Ann. Clin. Microbiol. Antimicrob. 15:21. <https://dx.doi.org/10.1186/s12941-016-0135-3>
https://doi.org/10.1186/s12941-016-0135-...
). A previous study compared the MIC results for Campylobacter jejuni strains according to the EUCAST and CLSI values and showed an agreement between these guidelines, which indicates that data based on both parameters could be compared (Paravisi et al. 2020Paravisi M., Laviniki V., Bassani J., Kunert-Filho H.C., Carvalho D., Wilsmann D.E., Borges K.A., Furian T.Q., Salle C.T.P., Moraes H.L.S. & Nascimento V.P.N. 2020. Antimicrobial resistance in Campylobacter jejuni isolated from Brazilian poultry slaughterhouses. Braz. J. Poult. Sci. 22(2):1-9. <https://dx.doi.org/10.1590/1806-9061-2020-1262>
https://doi.org/10.1590/1806-9061-2020-1...
). A similar analysis was performed in the current study, and the results showed good agreement for gentamicin and enrofloxacin, indicating that the results from both breakpoints were similar. Tetracycline, nalidix acid, and chloramphenicol presented equal results. However, a fair agreement was obtained for ciprofloxacin, which implies a separate analysis and discussion of this antimicrobial. The kappa analysis for ciprofloxacin resulted in a fair agreement, which means that it was significantly (p<0.05) variable according to the breakpoint evaluated. When the CLSI breakpoint was applied, only one strain, isolated in 2006, was resistant. In contrast, analysis with the EUCAST breakpoint resulted in 45% (9/20) and 75% (15/20) of non-susceptible strains in 2006 and 2016, respectively. The majority of previous studies evaluating the resistance of S. Heidelberg for ciprofloxacin used the CLSI breakpoint, which is a possible reason for the lower resistance rate found elsewhere for this substance (Elhariri et al. 2020Elhariri M., Elhelw R., Selim S., Ibrahim M., Hamza D. & Hamza E. 2020. Virulence and antibiotic resistance patterns of extended-spectrum beta-lactamase-producing Salmonella enterica serovar Heidelberg isolated from broiler chickens and poultry workers: a potential hazard. Foodborne Pathog. Dis. 17(6):373-381. <https://dx.doi.org/10.1089/fpd.2019.2719> <PMid:31755782>
https://doi.org/10.1089/fpd.2019.2719...
, Souza et al. 2020Souza A.I.S., Saraiva M.M.S., Casas M.R.T., Oliveira G.M., Cardozo M.V., Benevides V.P., Barbosa F.O., Freitas Neto O.C., Almeida A.M. & Berchieri Junior A. 2020. High occurrence of β-lactamase-producing Salmonella Heidelberg from poultry origin. PLoS One 15:1-11. <https://dx.doi.org/10.1371/journal.pone.0230676> <PMid:32231395>
https://doi.org/10.1371/journal.pone.023...
). Our results suggest that the guidelines for the breakpoints should be chosen carefully as well as the comparison of results with previously published studies.
All the strains were susceptible to chloramphenicol, which is probably related to its banishment in production animals since 2003 in Brazil (Brasil 2003Brasil 2003. Instrução Normativa nº 9. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.). The resistance to gentamicin in the present study varied from 5% (2006) to 30% (2016). Although not significant, this high resistance rate is not commonly observed in Salmonella strains, and especially among S. Heidelberg (Pandini et al. 2014Pandini J.A., Pinto F.G.S., Muller J.M., Weber L.D. & Moura A.C. 2014. Ocorrência e perfil de resistência antimicrobiana de sorotipos de Salmonella spp. isolados de aviários do Paraná, Brasil. Arqs Inst. Biológico, São Paulo, 20(10):1-6. <https://dx.doi.org/10.1590/1808-1657000352013>
https://doi.org/10.1590/1808-16570003520...
, Mendonça 2016Mendonça E.P. 2016. Características de virulência, resistência e diversidade genética de sorovares de Salmonella com impacto na saúde pública, isolados de frangos de corte no Brasil. Doctoral Dissertation, Universidade Federal de Uberlândia, Uberlândia. 134p., Saifuddin et al. 2016Saifuddin A.K.M., Isalm S.K.M.A. & Anwar M.D.N. 2016. Molecular characterization and antimicrobial resistance patterns of Salmonella spp. and Escherichia coli of laying chicken. Microbes Health 5(1):4-6. <https://dx.doi.org/10.3329/mh.v5i1.31189>
https://doi.org/10.3329/mh.v5i1.31189...
, Neves et al. 2020Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027.), probably because the use of gentamicin in poultry production is restricted (Giacomelli et al. 2014Giacomelli M., Salata C., Martini M., Montesissa C. & Piccirillo A. 2014. Antimicrobial resistance of Campylobacter jejuni and Campylobacter coli from poultry in Italy. Microb. Drug Resist. 20(2):181-188. <https://dx.doi.org/10.1089/mdr.2013.0110> <PMid:24320689>
https://doi.org/10.1089/mdr.2013.0110...
).
Tetracycline was the only antibiotic that showed a significant increase over the period from 2006-2016, and 75% of the strains isolated in 2016 were non-susceptible. In contrast, only one strain (5%) was non-susceptible among those isolated in 2006. The resistance of Salmonella to tetracycline is variable in the literature (Mion et al. 2016Mion L., Parizotto L., Calasans M., Dickel E.L., Pilotto F., Rodrigues L.B., Nascimento V.P. & Santos L.R. 2016. Effect of antimicrobials on Salmonella spp. strains isolated from poultry processing plants. Braz. J. Poult. Sci. 18(2):337-342. <https://dx.doi.org/10.1590/1806-9061-2015-0127>
https://doi.org/10.1590/1806-9061-2015-0...
, El-Tayeb et al. 2017El-Tayeb M.A., Ibrahim A.S.S., Al-Salamah A.A., Almaary K.S. & Elbadawi Y.B. 2017. Prevalence, serotyping and antimicrobials resistance mechanism of Salmonella enterica isolated from clinical and environmental samples in Saudi Arabia. Braz. J. Microbiol. 48(3):499-508. <https://dx.doi.org/10.1016/j.bjm.2016.09.021>
https://doi.org/10.1016/j.bjm.2016.09.02...
, Nair et al. 2018Nair D.V.T., Venkitanarayanan K. & Johny A.K. 2018. Antibiotic-resistant Salmonella in the food supply and the potential role of antibiotic alternatives for control. Foods 7:167. <https://dx.doi.org/10.3390/foods7100167> <PMid:30314348>
https://doi.org/10.3390/foods7100167...
, Borges et al. 2019Borges K.A., Furian T.Q., de Souza S.N., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2019. Antimicrobial resistance and molecular characterization of Salmonella enterica serotypes isolated from poultry sources in Brazil. Braz. J. Poult. Sci. 21(1):1-8. <https://dx.doi.org/10.1590/1806-9061-2018-0827>
https://doi.org/10.1590/1806-9061-2018-0...
). A recent study found high non-susceptibility rates among S. Heidelberg isolated from Brazilian flocks (Neves et al. 2020Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027.). The resistance of Salmonella to tetracycline may be related to the widespread of tet resistance genes among Salmonella serotypes (Khoshbakht et al. 2018Khoshbakht R., Derakhshandeh A., Jelviz L. & Azhdari F. 2018. Tetracycline resistance genes in Salmonella enterica serovars with animal and human origin. Int. J. Ent. Pathog. 6(3):60-64. <https://dx.doi.org/10.15171/ijep.2018.17>
https://doi.org/10.15171/ijep.2018.17...
). Tetracycline was commonly used as a feed additive for prophylactic purposes in broiler rations in Brazil, and its use was restricted for therapeutic purposes in animals since 2009 (Brasil 2009Brasil 2009. Instrução Normativa nº 26. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.). Even if its use has been considerably reduced, it contributed to the maintenance of the circulation of resistance genes. In addition, opportunistic pathogens and commensal bacteria can serve as reservoirs for these genes, through mobile genetic elements, and may transfer them to Salmonella strains and other pathogens. Thus, its increased resistance may also be a result of the presence of plasmids or transposons that carry antimicrobial resistance genes for other substances, which continue to suffer selective pressure (Frye & Jackson 2013Frye J.G. & Jackson C.R. 2013. Genetic mechanisms of antimicrobial resistance identified in Salmonella enterica, Escherichia coli, and Enteroccocus spp. isolated from U.S. food animals. Front. Microbiol. 4:135. <https://dx.doi.org/10.3389/fmicb.2013.00135> <PMid:23734150>
https://doi.org/10.3389/fmicb.2013.00135...
).
Resistance to nalidixic acid (quinolone) and enrofloxacin (fluoroquinolone) did not vary according to the year of isolation or the breakpoint evaluated. However, resistance to nalidix acid was higher than that of enrofloxacin. High resistance rates to nalidix acid among S. Heidelberg isolated from Brazilian poultry flocks have been previously described (Giuriatti et al. 2017Giuriatti J., Stefani L.M., Brisola M.C., Crecencio R.B., Bitner D.S. & Faria G.A. 2017. Salmonella Heidelberg: genetic profile of its antimicrobial resistance related to extended spectrum β-lactamases (ESBLs). Microb. Pathog. 109:195-199. <https://dx.doi.org/10.1016/j.micpath.2017.05.040> <PMid:28578094>
https://doi.org/10.1016/j.micpath.2017.0...
, Neves et al. 2020Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027., Souza et al. 2020Souza A.I.S., Saraiva M.M.S., Casas M.R.T., Oliveira G.M., Cardozo M.V., Benevides V.P., Barbosa F.O., Freitas Neto O.C., Almeida A.M. & Berchieri Junior A. 2020. High occurrence of β-lactamase-producing Salmonella Heidelberg from poultry origin. PLoS One 15:1-11. <https://dx.doi.org/10.1371/journal.pone.0230676> <PMid:32231395>
https://doi.org/10.1371/journal.pone.023...
), and it is probably related to its wide use in poultry therapy for many years (Neves 2014Neves G.B. 2014. Diferenças na expressão gênica de isolados de campo e de frigorífico de Salmonella resistente aos antimicrobianos e desinfetantes. Master’s Thesis, Universidade do Estado de Santa Catarina, Lages, SC. 120p.). In contrast to what happens with first-generation quinolones, the resistance levels to fluoroquinolones, such as enrofloxacin and ciprofloxacin, are usually lower among Salmonella serotypes (Dallal et al. 2010Dallal M.M.S., Doyle M.P., Rezadehbashi M., Dabiri H., Sanaei M., Modarresi S., Bakhtiari R., Sharifiy K., Taremi M., Zali M.R. & Sharifi-Yazdi M.K. 2010. Prevalence and antimicrobial resistance profiles of Salmonella serotypes, Campylobacter and Yersinia spp. isolated from retail chicken and beef, Tehran, Iran. Food Control 21(4):388-392. <https://dx.doi.org/10.1016/j.foodcont.2009.06.001>
https://doi.org/10.1016/j.foodcont.2009....
, Panzenhagen et al. 2016Panzenhagen P.H.N., Aguiar W.S., Frasão B.S., Pereira V.L.A., Abreu D.C., Rodrigues D.P., Nascimento E.R. & Aquino M.H.C. 2016. Prevalence and fluoroquinolones resistance of Campylobacter and Salmonella isolates from poultry carcasses in Rio de Janeiro, Brazil. Food Control 61:243-247. <https://dx.doi.org/10.1016/j.foodcont.2015.10.002>
https://doi.org/10.1016/j.foodcont.2015....
, Proroga et al. 2016Proroga Y.T.R., Capuano F., Carullo M.R., La Tela I., Capparelli R., Barco L. & Pasquale V. 2016. Occurrence and antimicrobial resistance of Salmonella strains from food of animal origin in southern Italy. Folia Microbiol. 61(1):21-27. <https://dx.doi.org/10.1007/s12223-015-0407-x> <PMid:26084745>
https://doi.org/10.1007/s12223-015-0407-...
, Danish 2018Danish 2018. Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark, 2018. The Danish Integrated Antimicrobial Resistance Monitoring and Research Programme (DANMAP), Ministry of Food, Agriculture and Fisheries, Ministry of Health, Available at <Available at http://www.danmap.org/Downloads/Reports.aspx > Accessed Mar. 5, 2020.
http://www.danmap.org/Downloads/Reports....
).
Resistance to disinfectants is probably because of the excessive use of these substances, imposing selective pressure and, consequently, vertical and horizontal gene transfer from resistant bacteria. However, the mechanisms of transfer of disinfectant resistance genes remain unclear, and only a few have been described (Mc Carlie et al. 2020Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
https://doi.org/10.1016/j.drup.2019.1006...
). Cross-resistance between antimicrobial substances is becoming an increasing concern because of the possible positive correlation between resistance to disinfectants and resistance to antibiotics (Cadena et al. 2019Cadena M., Froenicke L., Britton M., Settles M.L., Durbin-Johnson B., Kumimoto E., Gallardo R.A., Ferreiro A., Chylkova T., Zhou H. & Pitesky M. 2019. Transcriptome analysis of Salmonella Heidelberg after exposure to cetylpyridinium chloride, acidified calcium hypochlorite, and peroxyacetic acid. J. Food Prot. 82(1):109-119. <https://dx.doi.org/10.4315/0362-028x.jfp-18-235> <PMid:30702951>
https://doi.org/10.4315/0362-028x.jfp-18...
, Mc Carlie et al. 2020Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
https://doi.org/10.1016/j.drup.2019.1006...
). The major concern is based on the hypothesis that disinfectant exposure can promote antibiotic resistance, thus generating MDR bacteria (Mc Carlie et al. 2020Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
https://doi.org/10.1016/j.drup.2019.1006...
). Jin et al. (2020)Jin M., Liu L., Wang D.-N., Yang D., Liu W.-L., Yin J., Yang Z.-W., Wang H.-R., Qiu Z.-G., Shen Z.-Q., Shi D.-Y., Li H.-B., Guo J.-H. & Li J.-W. 2020. Chlorine disinfection promotes the exchange of antibiotic resistance genes across bacterial genera by natural transformation. ISME J. 14(7):1847-1856. <https://dx.doi.org/10.1038/s41396-020-0656-9> <PMid:32327733>
https://doi.org/10.1038/s41396-020-0656-...
demonstrated that the process of chlorination promoted the horizontal transfer of plasmids and the exchange of antimicrobial resistance genes, highlighting its potential risk to public health. According to Joynson et al. (2002)Joynson J.A., Forbes B.A. & Lambert R.J.W. 2002. Adaptive resistance to benzalkonium chloride, amikacin and tobramycin: the effect on susceptibility to other antimicrobials. J. Appl. Microbiol. 93(1):96-107. <https://dx.doi.org/10.1046/j.1365-2672.2002.01667.x> <PMid:12067378>
https://doi.org/10.1046/j.1365-2672.2002...
, increased resistance to benzalkonium chloride does not confer cross-resistance to antibiotics, but increased MIC to some antibiotics resulted in a slightly increased MIC of this disinfectant. However, this cross-resistance is not a consensus among researchers, and some studies have shown that bacteria remain susceptible to disinfectant products when they are correctly used. According to Maertens et al. (2019)Maertens H., De Reu K., Meyer E., Van Coillie E. & Dewulf J. 2019. Limited association between disinfectant use and either antibiotic or disinfectant susceptibility of Escherichia coli in both poultry and pig husbandry. BMC Vet. Res. 15:310. <https://dx.doi.org/10.1186/s12917-019-2044-0>
https://doi.org/10.1186/s12917-019-2044-...
, disinfectants are generally used at concentrations above the MIC of wild-type isolates. In contrast, antibiotics are commonly used in concentrations closer to their MIC.
In the current study, there was no relationship between antimicrobial and disinfectant resistance. The reasons for the emergence of S. Heidelberg in broiler farms in southern of Brazil are still not clear. Complementary studies, including the whole-genome sequencing analysis and the pulsed-field gel electrophoresis patterns determination could elucidate the predominance of this serotype (Voss-Rech et al. 2019Voss-Rech D., Kramer B., Silva V.S., Rebelatto R., Abreu P.G., Coldebella A. & Vaz C.S.L. 2019. Longitudinal study reveals persistent environmental Salmonella Heidelberg in Brazilian broiler farms. Vet. Microbiol. 233:118-123. <https://dx.doi.org/10.1016/j.vetmic.2019.04.004>
https://doi.org/10.1016/j.vetmic.2019.04...
).
Unfortunately, the Brazilian government does not have an integrated program for monitoring antimicrobial and disinfectant resistance in human and animal foodborne pathogens, making the adoption of new measures to control and restrict the use of antimicrobials difficult (Borges et al. 2019Borges K.A., Furian T.Q., de Souza S.N., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2019. Antimicrobial resistance and molecular characterization of Salmonella enterica serotypes isolated from poultry sources in Brazil. Braz. J. Poult. Sci. 21(1):1-8. <https://dx.doi.org/10.1590/1806-9061-2018-0827>
https://doi.org/10.1590/1806-9061-2018-0...
). The benefits of monitoring antimicrobial resistance in foodborne pathogens are well-known. However, monitoring disinfectant resistance is also important to define sanitation programs, which include appropriate compounds, specific contact times, and concentrations of these products.
Conclusions
Salmonella Heidelberg strains were highly susceptible to sodium hypochlorite, regardless of the conditions applied and the year of isolation.
Increased resistance to benzalkonium chloride from 2006 to 2016 was observed only under specific conditions (200ppm for 5min at 25°C), and probably it is not related to the continuous use of this substance.
Similar results were obtained for antimicrobial resistance since increased resistance from 2006-2016 was observed only for tetracycline.
Further analysis should include a larger number of S.Heidelberg isolates from poultry origin and additional antimicrobial agents for more precise conclusions about the increasing in the antimicrobial resistance in the last years.
References
- ABPA 2020. Relatório Anual, 2020. Associação Brasileira de Proteína Animal. Available at <Available at http://abpa-br.org/wp-content/uploads/2020/05/abpa_relatorio_anual_2020_portugues_web.pdf > Accessed on Jun. 18, 2020.
» http://abpa-br.org/wp-content/uploads/2020/05/abpa_relatorio_anual_2020_portugues_web.pdf - Balsalobre L.C., Dropa M. & Matté M.H. 2014. An overview of antimicrobial resistance and its public health significance. Braz. J. Microbiol. 45(1):1-5. <https://dx.doi.org/10.1590/S1517-83822014005000033> <PMid:24948906>
» https://doi.org/10.1590/S1517-83822014005000033 - Borges K.A., Furian T.Q., de Souza S.N., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2019. Antimicrobial resistance and molecular characterization of Salmonella enterica serotypes isolated from poultry sources in Brazil. Braz. J. Poult. Sci. 21(1):1-8. <https://dx.doi.org/10.1590/1806-9061-2018-0827>
» https://doi.org/10.1590/1806-9061-2018-0827 - Borges K.A., Furian T.Q., Souza S.N., Menezes R., Tondo E.C., Salle C.T.P., Moraes H.L. & Nascimento V.P. 2018. Biofilm formation capacity of Salmonella serotypes at different temperature conditions. Pesq. Vet. Bras. 38(1):71-76. <https://dx.doi.org/10.1590/1678-5150-pvb-4928>
» https://doi.org/10.1590/1678-5150-pvb-4928 - Borges T.J., Moretti L.K., Silva M.M.N., Tondo E.C. & Pereira K.S. 2020. Salmonella sensitivity to sodium hypochlorite and citric acid in washing water of lettuce residues. J. Food Safety 40(2):e12748. <https://dx.doi.org/10.1111/jfs.12748>
» https://doi.org/10.1111/jfs.12748 - Bragg R., Jansen A., Coetzee M., van der Westhuizen W. & Boucher C. 2014. Bacterial resistance to quaternary ammonium compounds (QAC) disinfectants. Adv. Exp. Med. Biol. 808:1-13. <https://dx.doi.org/10.1007/978-81-322-1774-9_1> <PMid:24595606>
» https://doi.org/10.1007/978-81-322-1774-9_1 - Bragg R.R., Meyburgh C.M., Lee J.-Y. & Coetzee M. 2018. Potential treatment options in a post-antibiotic era. Adv Exp Med Biol. 1052:51-61. <https://dx.doi.org/10.1007/978-981-10-7572-8_5> <PMid:29785480>
» https://doi.org/10.1007/978-981-10-7572-8_5 - Brasil 1993. Portaria nº 101: métodos de análise microbiológica para alimentos. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.
- Brasil 1998. Portaria nº 210: regulamento técnico da inspeção tecnológica e higiênico-sanitária de carne de aves. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.
- Brasil 2003. Instrução Normativa nº 9. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.
- Brasil 2009. Instrução Normativa nº 26. Diário Oficial da União, Ministério da Agricultura, Pecuária e Abastecimento, Poder Executivo, Brasília, DF.
- Brasil 2019a. Nota Técnica: entenda melhor - Salmonela em carne de frango. Ministério da Agricultura, Pecuária e Abastecimento, Brasília, DF. Available at <Available at https://www.gov.br/agricultura/pt-br/assuntos/inspecao/produtos-animal/arquivos-publicacoes-dipoa/entenda-melhor-salmonela-em-carne-de-frango > Accessed on Jul. 22, 2020.
» https://www.gov.br/agricultura/pt-br/assuntos/inspecao/produtos-animal/arquivos-publicacoes-dipoa/entenda-melhor-salmonela-em-carne-de-frango - Brasil 2019b. Surtos de doenças transmitidas por alimentos no Brasil - Informe 2018. Ministério da Saúde, Brasília, DF. Available at <Available at https://portalarquivos2.saude.gov.br/images/pdf/2019/fevereiro/15/Apresenta----o-Surtos-DTA---Fevereiro-2019.pdf > Accessed on Sep. 10, 2020.
» https://portalarquivos2.saude.gov.br/images/pdf/2019/fevereiro/15/Apresenta----o-Surtos-DTA---Fevereiro-2019.pdf - Cadena M., Froenicke L., Britton M., Settles M.L., Durbin-Johnson B., Kumimoto E., Gallardo R.A., Ferreiro A., Chylkova T., Zhou H. & Pitesky M. 2019. Transcriptome analysis of Salmonella Heidelberg after exposure to cetylpyridinium chloride, acidified calcium hypochlorite, and peroxyacetic acid. J. Food Prot. 82(1):109-119. <https://dx.doi.org/10.4315/0362-028x.jfp-18-235> <PMid:30702951>
» https://doi.org/10.4315/0362-028x.jfp-18-235 - Camilotti E., Rocha S.L.S., Tejkowski T.M., Moraes H.L.S., Salle C.T.P. & Avancini C.A.M. 2015. Simulação de condições de uso de quaternário de amônio frente amostras de Salmonella Hadar isoladas de carcaças de frango. Revta Bras. Saúde Prod. Anim. 16(1):66-72. <https://dx.doi.org/10.1590/S1519-99402015000100008>
» https://doi.org/10.1590/S1519-99402015000100008 - CDC 2016. Salmonella serotypes isolated from animals and related sources. Centers for Disease Control and Prevention, Atlanta, GA. Available at <Available at https://cdc.gov/nationalsurveillance/pdfs/salmonella-serotypesisolated-animals-and-related-sources-508.pdf > Accessed on Jul. 22, 2020.
» https://cdc.gov/nationalsurveillance/pdfs/salmonella-serotypesisolated-animals-and-related-sources-508.pdf - CDC 2020a. Salmonella Centers for Disease Control and Prevention, Atlanta, GA. Available at <Available at https://www.cdc.gov/salmonella/index.html > Accessed on Feb. 5, 2020.
» https://www.cdc.gov/salmonella/index.html - CDC 2020b. Making food safer to eat: reducing contamination from the farm to the table. Center for Disease Control and Prevention, Atlanta, GA. Available at <Available at http://www.cdc.gov/vitalsigns/foodsafety > Accessed Mar. 3, 2020.
» http://www.cdc.gov/vitalsigns/foodsafety - CLSI 2013a. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-A4, Approved Standard - Fourth Edition, Clinical and Laboratory Standards Institute, Wayne, PA.
- CLSI 2013b. Performance standards for antimicrobial disk and dilution susceptibility test for bacteria isolated from animals. VET01-S2, Second Information Supplement, Clinical and Laboratory Standards Institute, Wayne, PA.
- CLSI 2020. Performance standards for antimicrobial susceptibility testing. M100-30, Clinical and Laboratory Standards Institute, Wayne, PA. Available at <Available at http://em100.edaptivedocs.net/dashboard.aspx > Accessed on May 3, 2020.
» http://em100.edaptivedocs.net/dashboard.aspx - Colla F.L., Rodrigues L.B., Dickel E.L., Borsoi A., Nascimento V.P. & Santos L.R. 2012. Avaliação in vitro de clorexidina, amônia quaternária e ácido peracético frente a amostras de Salmonella Heidelberg isoladas de abatedouro avícola em 2005 e 2009. Pesq. Vet. Bras. 32(4):289-292. <https://dx.doi.org/10.1590/S0100-736X2012000400003>
» https://doi.org/10.1590/S0100-736X2012000400003 - Dallal M.M.S., Doyle M.P., Rezadehbashi M., Dabiri H., Sanaei M., Modarresi S., Bakhtiari R., Sharifiy K., Taremi M., Zali M.R. & Sharifi-Yazdi M.K. 2010. Prevalence and antimicrobial resistance profiles of Salmonella serotypes, Campylobacter and Yersinia spp. isolated from retail chicken and beef, Tehran, Iran. Food Control 21(4):388-392. <https://dx.doi.org/10.1016/j.foodcont.2009.06.001>
» https://doi.org/10.1016/j.foodcont.2009.06.001 - Danish 2018. Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark, 2018. The Danish Integrated Antimicrobial Resistance Monitoring and Research Programme (DANMAP), Ministry of Food, Agriculture and Fisheries, Ministry of Health, Available at <Available at http://www.danmap.org/Downloads/Reports.aspx > Accessed Mar. 5, 2020.
» http://www.danmap.org/Downloads/Reports.aspx - Davis R. & Brown P.D. 2016. Multiple antibiotic resistance index, fitness and virulence potential in respiratory Pseudomonas aeruginosa from Jamaica. J. Med. Microbiol. 65(4):261-271. <https://dx.doi.org/10.1099/jmm.0.000229> <PMid:26860081>
» https://doi.org/10.1099/jmm.0.000229 - Duarte S.C. 2018. Epidemiologia dos principais sorotipos de salmonela circulantes na avicultura brasileira. Simpósio Salmonella: cenários e desafios, Porto Alegre, RS.
- EFSA 2019. Salmonella control in poultry flocks and its public health impact. EFSA J. 17(2):5596. <https://dx.doi.org/10.2903/j.efsa.2019.5596>
» https://doi.org/10.2903/j.efsa.2019.5596 - EFSA 2020. The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2017/2018. EFSA J. 18(3):6007. <http://doi.org/10.2903/j.efsa.2020.6007>
» https://doi.org/10.2903/j.efsa.2020.6007 - Elhariri M., Elhelw R., Selim S., Ibrahim M., Hamza D. & Hamza E. 2020. Virulence and antibiotic resistance patterns of extended-spectrum beta-lactamase-producing Salmonella enterica serovar Heidelberg isolated from broiler chickens and poultry workers: a potential hazard. Foodborne Pathog. Dis. 17(6):373-381. <https://dx.doi.org/10.1089/fpd.2019.2719> <PMid:31755782>
» https://doi.org/10.1089/fpd.2019.2719 - El-Tayeb M.A., Ibrahim A.S.S., Al-Salamah A.A., Almaary K.S. & Elbadawi Y.B. 2017. Prevalence, serotyping and antimicrobials resistance mechanism of Salmonella enterica isolated from clinical and environmental samples in Saudi Arabia. Braz. J. Microbiol. 48(3):499-508. <https://dx.doi.org/10.1016/j.bjm.2016.09.021>
» https://doi.org/10.1016/j.bjm.2016.09.021 - Estrela C., Estrela C.R.A., Barbin E.L., Spanó J.C.E., Marchesan M.A. & Pécora J.D. 2002. Mechanism of action of sodium hypochlorite. Braz. Dent. J. 13(2):113-117. <https://dx.doi.org/10.1590/s0103-64402002000200007> <PMid:12238801>
» https://doi.org/10.1590/s0103-64402002000200007 - Etter A.J., West A.M., Burnett J.L., Wu S.T., Veenhuizen D.R., Ogas R.A. & Oliver H.F. 2019. Salmonella enterica subsp. enterica Serovar Heidelberg food isolates associated with a salmonellosis outbreak have enhanced stress tolerance capabilities. App. Env. Microbiol. 85(16):e01065-19. <https://dx.doi.org/10.1128/AEM.01065-19> <PMid:31175193>
» https://doi.org/10.1128/AEM.01065-19 - EUCAST 2020. Antimicrobial wild type distributions of microorganisms. European Committee on Antimicrobial Susceptibility Testing. Available at <Available at https://mic.eucast.org/Eucast2/ > Accessed on May 3, 2020.
» https://mic.eucast.org/Eucast2/ - FAO 2016. The FAO action plan on antimicrobial resistance 2016-2020. Food and Agriculture Organization of the United Nations, Rome. Available at <Available at http://www.fao.org/3/a-i5996e.pdf > Accessed on Jun. 23, 2020.
» http://www.fao.org/3/a-i5996e.pdf - Frye J.G. & Jackson C.R. 2013. Genetic mechanisms of antimicrobial resistance identified in Salmonella enterica, Escherichia coli, and Enteroccocus spp. isolated from U.S. food animals. Front. Microbiol. 4:135. <https://dx.doi.org/10.3389/fmicb.2013.00135> <PMid:23734150>
» https://doi.org/10.3389/fmicb.2013.00135 - Fukuzaki S. 2006. Mechanisms of actions of sodium hypochlorite in cleaning and disinfection processes. Biocontrol Sci. 11(4):147-157. <https://dx.doi.org/10.4265/bio.11.147> <PMid:17190269>
» https://doi.org/10.4265/bio.11.147 - Giacomelli M., Salata C., Martini M., Montesissa C. & Piccirillo A. 2014. Antimicrobial resistance of Campylobacter jejuni and Campylobacter coli from poultry in Italy. Microb. Drug Resist. 20(2):181-188. <https://dx.doi.org/10.1089/mdr.2013.0110> <PMid:24320689>
» https://doi.org/10.1089/mdr.2013.0110 - Gieraltowski L., Higa J., Peralta V., Green A., Schwensohn C., Rosen H., Libby T., Kissler B., Marsden-Haug N., Booth H., Kimura A., Grass J., Bicknese A., Tolar B., Defibaugh-Chávez S., Williams I. & Wise M. 2016. National outbreak of multidrug resistant Salmonella Heidelberg infections linked to a single poultry company. PLoS One 11(9):e0162369. <https://dx.doi.org/10.1371/journal.pone.0162369> <PMid:27631492>
» https://doi.org/10.1371/journal.pone.0162369 - Giuriatti J., Stefani L.M., Brisola M.C., Crecencio R.B., Bitner D.S. & Faria G.A. 2017. Salmonella Heidelberg: genetic profile of its antimicrobial resistance related to extended spectrum β-lactamases (ESBLs). Microb. Pathog. 109:195-199. <https://dx.doi.org/10.1016/j.micpath.2017.05.040> <PMid:28578094>
» https://doi.org/10.1016/j.micpath.2017.05.040 - Hao H., Pan H., Ahmad I., Cheng G., Wang Y., Dai M., Tao Y., Chen D., Peng D., Liu Z., Huang L. & Yuan Z. 2013. Susceptibility breakpoint of enrofloxacin against swine Salmonella spp. J. Clin. Microbiol 51(9):3070-3072. <https://dx.doi.org/10.1128/JCM.01096-13> <PMid:23784134>
» https://doi.org/10.1128/JCM.01096-13 - Jaenisch F.R.F., Kuchiishi S.S. & Coldebella A. 2010. Atividade antibacteriana de desinfetantes para uso na produção orgânica de aves. Ciência Rural 40(2):384-388. <https://dx.doi.org/10.1590/S0103-84782010000200020>
» https://doi.org/10.1590/S0103-84782010000200020 - Jin M., Liu L., Wang D.-N., Yang D., Liu W.-L., Yin J., Yang Z.-W., Wang H.-R., Qiu Z.-G., Shen Z.-Q., Shi D.-Y., Li H.-B., Guo J.-H. & Li J.-W. 2020. Chlorine disinfection promotes the exchange of antibiotic resistance genes across bacterial genera by natural transformation. ISME J. 14(7):1847-1856. <https://dx.doi.org/10.1038/s41396-020-0656-9> <PMid:32327733>
» https://doi.org/10.1038/s41396-020-0656-9 - Joynson J.A., Forbes B.A. & Lambert R.J.W. 2002. Adaptive resistance to benzalkonium chloride, amikacin and tobramycin: the effect on susceptibility to other antimicrobials. J. Appl. Microbiol. 93(1):96-107. <https://dx.doi.org/10.1046/j.1365-2672.2002.01667.x> <PMid:12067378>
» https://doi.org/10.1046/j.1365-2672.2002.01667.x - Kassim A., Omuse G., Premji Z. & Revathi G. 2016. Comparison of Clinical Laboratory Standards Institute and European Committee on Antimicrobial Susceptibility Testing guidelines for the interpretation of antibiotic susceptibility at a University teaching hospital in Nairobi, Kenya: a cross-sectional study. Ann. Clin. Microbiol. Antimicrob. 15:21. <https://dx.doi.org/10.1186/s12941-016-0135-3>
» https://doi.org/10.1186/s12941-016-0135-3 - Khoshbakht R., Derakhshandeh A., Jelviz L. & Azhdari F. 2018. Tetracycline resistance genes in Salmonella enterica serovars with animal and human origin. Int. J. Ent. Pathog. 6(3):60-64. <https://dx.doi.org/10.15171/ijep.2018.17>
» https://doi.org/10.15171/ijep.2018.17 - Kich J.D., Borowsky L.M., Silva V.S., Ramenzoni M., Triques N., Kooler F.L. & Cardoso M.R.I. 2004. Avaliação da atividade antibacteriana de seis desinfetantes comerciais frente a amostras de Salmonella Typhimurium isoladas de suínos. Acta Scient. Vet. 32(1):33-39. <https://dx.doi.org/10.22456/1679-9216.16792>
» https://doi.org/10.22456/1679-9216.16792 - Köhler A.T., Rodloff A.C., Labahn M., Reinhardt M., Truyen U. & Speck S. 2018. Efficacy of sodium hypochlorite against multidrug-resistant Gram-negative bacteria. J. Hosp. Infec. 100(3):E40-E46. <https://dx.doi.org/10.1016/j.jhin.2018.07.017>
» https://doi.org/10.1016/j.jhin.2018.07.017 - Krumperman P.H. 1983. Multiple Antibiotic Resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Env. Microbiol. 46(1):165-170. <https://dx.doi.org/10.1128/aem.46.1.165-170.1983> <PMid:6351743>
» https://doi.org/10.1128/aem.46.1.165-170.1983 - Landis J.R. & Koch G.G. 1977. The measurement of observer agreement for categorical data. Biometrics 33(1):159-174. <https://dx.doi.org/10.2307%2F2529310> <PMid:843571>
» https://doi.org/10.2307%2F2529310 - Lo H.-Y., Lai F.-P. & Yang Y.-J. 2020. Changes in epidemiology and antimicrobial susceptibility of nontyphoid Salmonella in children in southern Taiwan, 1997-2016. J. Microbiol. Immunol. Infect. 53(4):585-591. <https://dx.doi.org/10.1016/j.jmii.2018.06.004> <PMid:30017562>
» https://doi.org/10.1016/j.jmii.2018.06.004 - Long M., Lai H., Deng W., Zhou K., Li B., Liu S., Fan L., Wang H. & Zou L. 2016. Disinfectant susceptibility of different Salmonella serotypes isolated from chicken and egg production chains. J. Appl. Microbiol. 121(3):672-681. <https://dx.doi.org/10.1111/jam.13184> <PMid:27206326>
» https://doi.org/10.1111/jam.13184 - Lucca V., Borges K.A., Furian T.Q., Borsoi A., Salle C.T.P., Moraes H.L.S. & Nascimento V.P. 2020. Influence of the norepinephrine and medium acidification in the growth and adhesion of Salmonella Heidelberg isolated from poultry. Microb. Pathog. 138:103799. <https://dx.doi.org/10.1016/j.micpath.2019.103799>
» https://doi.org/10.1016/j.micpath.2019.103799 - Maertens H., De Reu K., Meyer E., Van Coillie E. & Dewulf J. 2019. Limited association between disinfectant use and either antibiotic or disinfectant susceptibility of Escherichia coli in both poultry and pig husbandry. BMC Vet. Res. 15:310. <https://dx.doi.org/10.1186/s12917-019-2044-0>
» https://doi.org/10.1186/s12917-019-2044-0 - Mc Carlie S., Boucher C.E. & Bragg R.R. 2020. Molecular basis of bacterial disinfectant resistance. Drug Resist. Updat. 48:100672. <https://dx.doi.org/10.1016/j.drup.2019.100672> <PMid:31830738>
» https://doi.org/10.1016/j.drup.2019.100672 - Mendonça E.P. 2016. Características de virulência, resistência e diversidade genética de sorovares de Salmonella com impacto na saúde pública, isolados de frangos de corte no Brasil. Doctoral Dissertation, Universidade Federal de Uberlândia, Uberlândia. 134p.
- Mion L., Parizotto L., Calasans M., Dickel E.L., Pilotto F., Rodrigues L.B., Nascimento V.P. & Santos L.R. 2016. Effect of antimicrobials on Salmonella spp. strains isolated from poultry processing plants. Braz. J. Poult. Sci. 18(2):337-342. <https://dx.doi.org/10.1590/1806-9061-2015-0127>
» https://doi.org/10.1590/1806-9061-2015-0127 - Møretrø T., Heir E., Nesse L.L., Vestby L.K. & Langsrud S. 2012. Control of Salmonella in food related environments by chemical disinfection. Food Res. Int. 45(2):532-544. <https://dx.doi.org/10.1016/j.foodres.2011.02.002>
» https://doi.org/10.1016/j.foodres.2011.02.002 - Nair D.V.T., Venkitanarayanan K. & Johny A.K. 2018. Antibiotic-resistant Salmonella in the food supply and the potential role of antibiotic alternatives for control. Foods 7:167. <https://dx.doi.org/10.3390/foods7100167> <PMid:30314348>
» https://doi.org/10.3390/foods7100167 - Neves G.B. 2014. Diferenças na expressão gênica de isolados de campo e de frigorífico de Salmonella resistente aos antimicrobianos e desinfetantes. Master’s Thesis, Universidade do Estado de Santa Catarina, Lages, SC. 120p.
- Neves G.B., Pick E., Giuriatti .J., Araujo D.N. & Stefani LM. 2020. A comparative study on Salmonella Enteritidis, S. Heidelberg and S. Typhimurium of poultry origin from Southern Brazil. Ann. Med. Medic. Res. 3:1027.
- Pandini J.A., Pinto F.G.S., Muller J.M., Weber L.D. & Moura A.C. 2014. Ocorrência e perfil de resistência antimicrobiana de sorotipos de Salmonella spp. isolados de aviários do Paraná, Brasil. Arqs Inst. Biológico, São Paulo, 20(10):1-6. <https://dx.doi.org/10.1590/1808-1657000352013>
» https://doi.org/10.1590/1808-1657000352013 - Panzenhagen P.H.N., Aguiar W.S., Frasão B.S., Pereira V.L.A., Abreu D.C., Rodrigues D.P., Nascimento E.R. & Aquino M.H.C. 2016. Prevalence and fluoroquinolones resistance of Campylobacter and Salmonella isolates from poultry carcasses in Rio de Janeiro, Brazil. Food Control 61:243-247. <https://dx.doi.org/10.1016/j.foodcont.2015.10.002>
» https://doi.org/10.1016/j.foodcont.2015.10.002 - Paravisi M., Laviniki V., Bassani J., Kunert-Filho H.C., Carvalho D., Wilsmann D.E., Borges K.A., Furian T.Q., Salle C.T.P., Moraes H.L.S. & Nascimento V.P.N. 2020. Antimicrobial resistance in Campylobacter jejuni isolated from Brazilian poultry slaughterhouses. Braz. J. Poult. Sci. 22(2):1-9. <https://dx.doi.org/10.1590/1806-9061-2020-1262>
» https://doi.org/10.1590/1806-9061-2020-1262 - Pereira B.M.P. & Tagkopoulos I. 2019. Benzalkonium chlorides: uses, regulatory status, and microbial resistance. Appl. Environ. Microbiol. 85(13):e00377-19. <https://dx.doi.org/10.1128/AEM.00377-19> <PMid:31028024>
» https://doi.org/10.1128/AEM.00377-19 - Proroga Y.T.R., Capuano F., Carullo M.R., La Tela I., Capparelli R., Barco L. & Pasquale V. 2016. Occurrence and antimicrobial resistance of Salmonella strains from food of animal origin in southern Italy. Folia Microbiol. 61(1):21-27. <https://dx.doi.org/10.1007/s12223-015-0407-x> <PMid:26084745>
» https://doi.org/10.1007/s12223-015-0407-x - Riazi S. & Matthews K.R. 2011. Failure of foodborne pathogens to develop resistance to sanitizers following repeated exposure to common sanitizers. Int. Biodet. Biodegr. 65(2):374-378. <https://dx.doi.org/10.1016/j.ibiod.2010.12.001>
» https://doi.org/10.1016/j.ibiod.2010.12.001 - Saifuddin A.K.M., Isalm S.K.M.A. & Anwar M.D.N. 2016. Molecular characterization and antimicrobial resistance patterns of Salmonella spp. and Escherichia coli of laying chicken. Microbes Health 5(1):4-6. <https://dx.doi.org/10.3329/mh.v5i1.31189>
» https://doi.org/10.3329/mh.v5i1.31189 - Schwarz S., Silley P., Simjee S., Woodford N., Van Duijkeren E., Johnson A.P. & Gaastra W. 2010. Editorial: assessing the antimicrobial susceptibility of bacteria obtained from animals. J. Antimicrob. Chemother. 65(4):601-604. <https://dx.doi.org/10.1093/jac/dkq037> <PMid:20181573>
» https://doi.org/10.1093/jac/dkq037 - Souza A.I.S., Saraiva M.M.S., Casas M.R.T., Oliveira G.M., Cardozo M.V., Benevides V.P., Barbosa F.O., Freitas Neto O.C., Almeida A.M. & Berchieri Junior A. 2020. High occurrence of β-lactamase-producing Salmonella Heidelberg from poultry origin. PLoS One 15:1-11. <https://dx.doi.org/10.1371/journal.pone.0230676> <PMid:32231395>
» https://doi.org/10.1371/journal.pone.0230676 - Stefani L.M., Neves G.B., Brisola M.C., Crecencio R.B., Pick E.C. & Araujo D.N. 2018. Salmonella Heidelberg resistant to ceftiofur and disinfectants routinely used in poultry. Semina, Ciênc. Agrárias 39(3):1029-1036. <https://dx.doi.org/10.5433/1679-0359.2018v39n3p1029>
» https://doi.org/10.5433/1679-0359.2018v39n3p1029 - Stringfellow K., Anderson P., Caldwell D., Lee J., Byrd J., McReynolds J., Carey J., Nisbet D. & Farnell M. 2009. Evaluation of disinfectants commonly used by the commercial poultry industry under simulated field conditions. Poult. Sci. 88(6):1151-1155. <https://dx.doi.org/10.3382/ps.2008-00455> <PMid:19439623>
» https://doi.org/10.3382/ps.2008-00455 - Voss-Rech D., Kramer B., Silva V.S., Rebelatto R., Abreu P.G., Coldebella A. & Vaz C.S.L. 2019. Longitudinal study reveals persistent environmental Salmonella Heidelberg in Brazilian broiler farms. Vet. Microbiol. 233:118-123. <https://dx.doi.org/10.1016/j.vetmic.2019.04.004>
» https://doi.org/10.1016/j.vetmic.2019.04.004 - WHO 2020. Antimicrobial resistance. World Health Organization. Available at <Available at https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance > Accessed on Jan. 20, 2020.
» https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
Publication Dates
-
Publication in this collection
03 Sept 2021 -
Date of issue
2021
History
-
Received
18 Feb 2021 -
Accepted
08 Apr 2021