Abstract
Elevated body mass index (BMI) has been reported as a risk factor for heart failure. Prevention of heart failure through identification and management of risk factors and preclinical phases of the disease is a priority. Levels of natriuretic peptides as well as activity of their receptors have been found altered in obese persons with some conflicting results. We investigated cardiac involvement in severely obese patients by determining N-terminal-pro-brain natriuretic peptide (NT-proBNP) and brain natriuretic peptide (BNP) and attempting to correlate the levels of these peptides in serum and plasma, respectively, with BMI, duration of obesity, waist circumference, and echocardiographic parameters. Thirty-three patients with severe obesity (mean BMI: 46.39 kg/m², mean age: 39 years) were studied. The control group contained 30 healthy age-matched individuals (BMI: <25 kg/m², mean age: 43 years). The t-test and Spearman correlation were used for statistical analysis. Log-NT-proBNP was significantly higher (P = 0.003) in obese patients (mean 1.67, 95% CI: 1.50-1.83 log pg/mL) compared to controls (mean: 1.32, 95% CI: 1.17-1.47 log pg/mL). The Log-NT-proBNP concentration correlated with duration of obesity (r = 0.339, P < 0.004). No difference was detected in the Log-BNP concentration (P = 0.63) of obese patients (mean: 0.73, 95% CI: 0.46-1.00 log pg/mL) compared to controls (mean: 0.66, 95% CI: 0.51-0.81 log pg/mL). NT-proBNP, but not BNP, is increased in severely obese patients and its concentration in serum is correlated with duration of obesity. NT-proBNP may be useful as an early diagnostic tool for the detection of cardiac burden due to severe obesity.
Obesity; Heart failure; NT-proBNP; Brain natriuretic peptide
Braz J Med Biol Res, February 2007, Volume 40(2) 153-158
N-terminal-pro-brain natriuretic peptide, but not brain natriuretic peptide, is increased in patients with severe obesity
 Correspondence and Footnotes
Correspondence and Footnotes
 F. Fernandes1, F.J.A. Ramires1, P.C. Buck1, I.J. Almeida1, R. Rabelo3, S.A. Dantas1, V.M.C. Salemi2, A. Halpern2 and C. Mady1
F. Fernandes1, F.J.A. Ramires1, P.C. Buck1, I.J. Almeida1, R. Rabelo3, S.A. Dantas1, V.M.C. Salemi2, A. Halpern2 and C. Mady1
1Instituto do Coração, 2Departamento de Endocrinologia, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brasil
3Centro de Medicina Diagnóstica Fleury, São Paulo, SP, Brasil
 References
References
 Correspondence and Footnotes
Correspondence and Footnotes
Correspondence and Footnotes
Correspondence and Footnotes
Correspondence and Footnotes
Correspondence and Footnotes
Abstract
Elevated body mass index (BMI) has been reported as a risk factor for heart failure. Prevention of heart failure through identification and management of risk factors and preclinical phases of the disease is a priority. Levels of natriuretic peptides as well as activity of their receptors have been found altered in obese persons with some conflicting results. We investigated cardiac involvement in severely obese patients by determining N-terminal-pro-brain natriuretic peptide (NT-proBNP) and brain natriuretic peptide (BNP) and attempting to correlate the levels of these peptides in serum and plasma, respectively, with BMI, duration of obesity, waist circumference, and echocardiographic parameters. Thirty-three patients with severe obesity (mean BMI: 46.39 kg/m2, mean age: 39 years) were studied. The control group contained 30 healthy age-matched individuals (BMI: <25 kg/m2, mean age: 43 years). The t-test and Spearman correlation were used for statistical analysis. Log-NT-proBNP was significantly higher (P = 0.003) in obese patients (mean 1.67, 95% CI: 1.50-1.83 log pg/mL) compared to controls (mean: 1.32, 95% CI: 1.17-1.47 log pg/mL). The Log-NT-proBNP concentration correlated with duration of obesity (r = 0.339, P < 0.004). No difference was detected in the Log-BNP concentration (P = 0.63) of obese patients (mean: 0.73, 95% CI: 0.46-1.00 log pg/mL) compared to controls (mean: 0.66, 95% CI: 0.51-0.81 log pg/mL). NT-proBNP, but not BNP, is increased in severely obese patients and its concentration in serum is correlated with duration of obesity. NT-proBNP may be useful as an early diagnostic tool for the detection of cardiac burden due to severe obesity.
Key words: Obesity, Heart failure, NT-proBNP, Brain natriuretic peptide
Introduction
Severe obesity is now recognized as a risk factor for heart failure (1). Epidemiological (2), echocardiographic (3), and autopsy (4,5) studies have identified obesity cardiomyopathy as an isolated clinical entity. In these studies, elevated body mass index (BMI) is described as a risk factor for left ventricular remodeling and overt heart failure.
Left ventricular enlargement and eccentric hypertrophy are the most common morphological cardiac abnormalities in obese individuals (3). This cardiac remodeling depends on the severity and duration of obesity and the influence of adverse loading conditions (6,7).
N-terminal-pro-brain natriuretic peptide (NT-proBNP) and brain natriuretic peptide (BNP) are useful for the diagnosis of heart failure, and their high levels in serum and plasma, respectively, are related to wall stress, which is often increased in severe obesity. They are sensitive markers of cardiac dysfunction and may be useful as early diagnostic tools for the detection of cardiac overload in this group of patients (8,9). However, NT-proBNP has a slower plasma clearance than when compared to the biologically active peptide BNP, resulting in higher circulating concentrations of NT-proBNP, although both peptides are released by cardiomyocytes on an equimolar basis (10). Furthermore, the different mechanisms of plasma clearance (neutral endopeptidase clearance receptors for BNP versus renal clearance for NT-proBNP) may be different in obese patients. The potential differences of either BNP or NT-proBNP concentration in plasma and serum, respectively, for the diagnosis of cardiac involvement in patients with severe obesity have not been established.
The aim of the present study was to compare BNP and NT-proBNP with respect to their diagnostic utility for the detection of cardiac involvement in patients with severe obesity and to correlate their levels in plasma, BMI, duration of obesity, waist circumference (WC), and echocardiographic parameters.
Material and Methods
Patients
We selected 33 consecutive patients with level III obesity and BMI >40, 23 females (mean age: 39 years). BMI was defined as weight in kilograms divided by height in square meters (kg/m2). The exclusion criteria were myocardial infarction (evaluated by Q waves on an electrocardiogram, segmental dysfunction by 2-D echocardiography) and valvar disease (evaluated by clinical examination and by Doppler echocardiography). Hypertension was defined as systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg. A control group comprised 30 healthy, thin individuals (BMI <25, 9 females, mean age: 43 years).
This investigation conforms to the principles outlined in the Declaration of Helsinki. All patients signed a written informed consent form, and the Ethics Committee of the Heart Institute of the University of São Paulo approved the study.
Procedures
Two-dimensional echocardiography complemented by M-mode and color-Doppler recordings was obtained according to the recommendations of the American Society of Echocardiography (11,12). The following indices were obtained: septum and posterior wall left ventricular (LV) thickness in diastole, LV internal end-diastolic dimension, LV internal end-systolic dimension, left atrium size, LV mass, and LV mass index. Also, the ejection fraction was calculated using the Teichholz method. E and A mitral wave peak velocities and E/A ratio were also analyzed.
Serum NT-proBNP levels were measured by immunoassay with detection by electro-chemiluminescence (Roche Diagnostics, São Paulo, SP, Brazil) using 20 µL of serum and polyclonal antibodies that detect epitopes in the N-terminal region (amino acids 1-76) of the proBNP (108 amino acids). Cross-reactivity with other natriuretic peptides (BNP, proANP1, CNP2) and the renin-angiotensin system were <0.001% (data from the manufacturer). The assay is fully automated using the Elecsys 2010 automated analyzer (Roche Diagnostics).
Plasma BNP levels were measured by a two-site dual-monoclonal immunochemiluminescent assay (Bayer ADVIA Centaur, Bayer Diagnostics, São Paulo, SP, Brazil) using 100 µL of plasma and monoclonal antibodies that detect epitopes in the C-terminal region of the BNP (amino acids 14-21). Both antibodies were supplied by Shionogi Co., Ltd. (Osaka, Japan). The assay was tested for several BNP fragments and other neuropeptides: a-atrial natriuretic peptide; NT-proBNP amino acids 1-21; NT-proBNP 22-46; NT-proBNP 1-46; NT-proBNP 1-76; NT-proBNP 47-76; urodilatin; C-, D-, and V-natriuretic peptides; adrenomedullin-52; angiotensin III; arg-vasopressin (all at 1.0 ng/L). There was no significant cross-reactivity of the ADVIA Centaur assay against other BNP fragments and neuropeptides (cross-reactivities ranging from -2.2% for adrenomedullin to 1.6% for atrial natriuretic peptide).
Blood was collected by venipuncture into plastic evacuated tubes containing EDTA for BNP determination. Samples were kept at room temperature for a maximum of 1 h before centrifugation and plasma separation. Plasma was immediately frozen and stored at -20ºC. The sample was thawed just before the analysis, which was carried out within 6 months of blood collection. BNP is stable for at least 1 year when frozen at -20ºC.
For the determination of NT-proBNP, blood was collected into glass tubes without additives and centrifuged within 1 h. In the meantime, samples were kept at room temperature. The serum was immediately frozen and stored at -20ºC. The sample was thawed just before the analysis, which was carried out within 6 months of blood collection. NT-proBNP is stable for at least 1 year when frozen at -20ºC.
For the BNP assay the coefficient of variation was 4.7% (mean concentration 29.4 pg/mL) and the inter- and intra-assay variations were 4.3 and 1.9%. The upper and lower limit concentrations are 5 and 5000 pg/mL, respectively (data from the manufacturer).
For the NT-proBNP assay the coefficient of variation was 7.0% (mean concentration 57 pg/mL) and the inter- and intra-assay variations were 4.0 and 2.6%, respectively. Concentration ranged from 5 up to 35,000 pg/mL (data from the manufacturer).
The threshold (lower limit of detection) was 5 pg/mL for both assays.
Statistical analysis
NT-proBNP and BNP data were log transformed in order to obtain a normal distribution of the sample that would permit to use parametric methods for statistical analysis. The Student t-test for unpaired data was used to compare the log transformed means of the circulating level of the hormone in morbidly obese and control subjects. Spearman correlations were used to assess the relation between hormone levels and BMI, duration of obesity, or WC in morbidly obese subjects. P < 0.05 was considered to be statistically significant.
Results
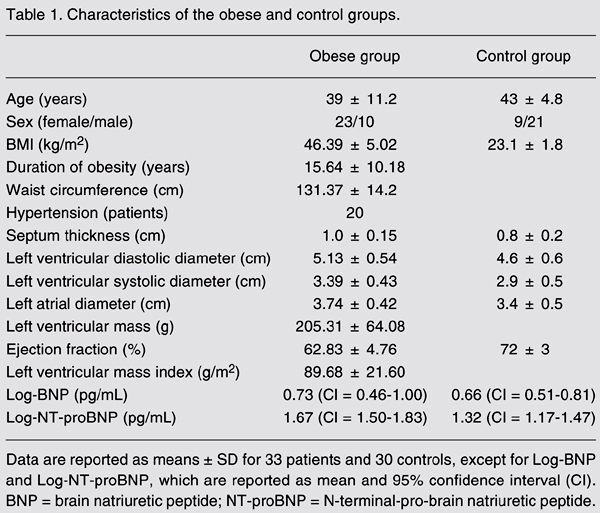
All patients had level III obesity with very high BMI (mean: 46.39 ± 5.02 kg/m2), long-term duration of obesity ranging from 2 to 40 years (mean: 15.64 ± 10.18 years), WC ranging from 103 to 157 cm (mean: 131.37 ± 14.2 cm). Twenty patients in the obese group had mild hypertension (Table 1).
Log-NT-proBNP (P = 0.003) was higher in patients with severe obesity (mean: 1.67, 95% CI: 1.50-1.83 log pg/mL) compared to the control group (mean: 1.32, 95% CI: 1.17-1.47 log pg/mL). Log-NT-proBNP correlated only with duration of obesity in these patients (P < 0.004, r = 0.339; Figure 1), but not with WC, BMI (Table 2), echocardiographic parameters (Table 1) and with the presence of hypertension.
However, no differences were found in the Log-BNP (P = 0.63) in patients with severe obesity (mean 0.73, 95% CI: 0.46-1.00 log pg/mL) compared with that in the control group (mean 0.66, 95% CI: 0.51-0.81 log pg/mL).
Spearman correlation between Log-N-terminal-pro-brain natriuretic peptide (NT-proBNP) and the duration of obesity (N = 33).
Discussion
The main finding in the present study was that patients with level III obesity had higher NT-proBNP compared to control. Therefore, NT-proBNP could be used as an early marker of cardiac involvement.
Obesity produces a variety of structural cardiac changes secondary to hemodynamic alterations. The increased metabolic demand imposed by the expanded adipose tissue and increased fat-free mass causes hyperdynamic circulation with increased blood volume (13, 14). Alexander et al. (13) demonstrated a positive linear correlation between the amount of overweight and both blood volume and cardiac output. Adipose tissue blood flow averages 2 to 3 mL min-1 100 g-1 under resting conditions (15). Thus, 100 kg of fat would require as much as 3 L/min blood flow to fulfill the requirement of adipose tissue flow (14,15). These changes may increase intracardiac pressures (16). BMI emerged as a significant independent predictor of heart failure in both sexes. Approximately 11% of cases of heart failure among men and 14% among women in the community could be attributable to obesity alone (17).
However, when we analyzed BNP, we did not detect differences in plasma levels compared to the control group. Wang et al. (17) observed a progressive decrease in plasma natriuretic peptides with increasing BMI. Similar to our results, Hanusch-Enserer et al. (18) found higher levels of NT-proBNP in morbidly obese subjects, with a significant decrease during weight loss after laparoscopic-adjustable gastric banding. Hermann-Arnhof et al. (19), analyzing NT-proBNP as an indicator of possible cardiovascular disease in severely obese individuals and comparing it with that of patients in different stages of heart failure, concluded that NT-proBNP was increased in obese individuals and the levels were similar in patients with NYHA class I heart failure. Our results were similar to those obtained by Wang et al. (17) regarding BNP levels, which were not increased in level III obese patients.
Previous studies on BNP and NT-proBNP within a large, heterogeneous population of patients with suspected cardiovascular disease at risk of cardiovascular dysfunction have suggested that NT-proBNP might be a more discerning marker of early cardiac dysfunction than BNP (20,21). Therefore, it is useful to use NT-proBNP instead of BNP to evaluate cardiac dysfunction in obese individuals.
NT-proBNP and BNP are secreted by the myocardium on an equimolar basis in cases of volume overload and increased wall tension. The elevated circulating NT-proBNP levels do not support the fact of diminished myocardial release or impaired synthesis for low BNP levels, suggesting that adipose tissues are intimately related to the natriuretic clearance receptor (17).
The diagnosis of heart failure in obese patients is difficult because such patients often have very limited mobility and may appear to be asymptomatic, even when they have significant cardiovascular disease. Moreover, in some patients the symptoms of heart failure are misdiagnosed as symptoms of obesity. The signs of left and right failure may be difficult to elicit in morbidly obese subjects and complementary examinations like echocardiography may also be difficult to perform due to a poor acoustic window (21).
The use of a noninvasive complementary method like NT-proBNP to diagnose myocardial overload in these patients may provide additional information regarding the risk of heart failure. Noninvasive imaging examinations may only identify cardiac damage later. We believe that an earlier diagnosis of cardiac burden due to obesity could avoid the subsequent evolution to myocardial dilation and to obesity cardiomyopathy.
Duration of obesity is also an important determinant of LV systolic function. It correlates positively with LV end-systolic stress, LV dimension in diastole, and LV mass/height index. It also contributes to impairment in left diastolic function. We observed higher NT-proBNP levels in patients with a longer duration of obesity. The clinical syndrome of obesity cardiomyopathy has been described in patients with a duration of obesity longer than 10 years (6,7).
We did not observe a correlation betweenNT-proBNP and the presence of hypertension. However, Wang et al. (17) noticed lower BNP levels in hypertensive obese patients compared to non-hypertensive individuals. Similar to our results, Grandi et al. (22) observed that plasma levels of BNP were not significantly different between normotensive and hypertensive obese subjects with the same morpho-functional characteristics.
NT-proBNP, but not BNP, may be useful as an early diagnostic tool for the detection of cardiac burden due to severe obesity.
Acknowledgments
We are grateful to Márcia Moreira Holckman for help and support with the statistical analysis, and for Cintia Cerquato for the selection of obese patients.
 Address for correspondence: F. Fernandes, Instituto do Coração, FM, USP, Av. Dr. Eneas C. Aguiar, 44, 05403-900 São Paulo, SP, Brasil. Fax: +55-11-3069-5346. E-mail: car_fabio@incor.usp.br
Address for correspondence: F. Fernandes, Instituto do Coração, FM, USP, Av. Dr. Eneas C. Aguiar, 44, 05403-900 São Paulo, SP, Brasil. Fax: +55-11-3069-5346. E-mail: car_fabio@incor.usp.br
Publication supported by FAPESP. Received December 20, 2005. Accepted November 22, 2006.
- 1. Coviello JS, Nystrom KV. Obesity and heart failure. J Cardiovasc Nurs 2003; 18: 360-366.
- 2. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. Obesity and the risk of heart failure. N Engl J Med 2002; 347: 305-313.
- 3. Alpert MA, Terry BE, Kelly DL. Effect of weight loss on cardiac chamber size, wall thickness and left ventricular function in morbid obesity. Am J Cardiol 1985; 55: 783-786.
- 4. Smith HL, Willius FA. Adiposity of the heart. Arch Intern Med 1933; 52: 911-931.
- 5. Amad KH, Brennan JC, Alexander JK. The cardiac pathology of chronic exogenous obesity. Circulation 1965; 32: 740-745.
- 6. Nakajima T, Fujioka S, Tokunaga K, Hirobe K, Matsuzawa Y, Tarui S. Noninvasive study of left ventricular performance in obese patients: influence of duration of obesity. Circulation 1985; 71: 481-486.
- 7. Alpert MA, Lambert CR, Panayiotou H, Terry BE, Cohen MV, Massey CV, et al. Relation of duration of morbid obesity to left ventricular mass, systolic function, and diastolic filling, and effect of weight loss. Am J Cardiol 1995; 76: 1194-1197.
- 8. Munagala VK, Burnett JC Jr, Redfield MM. The natriuretic peptides in cardiovascular medicine. Curr Probl Cardiol 2004; 29: 707-769.
- 9. Machado M, Falcão LM, Ravara L. The clinical role of natriuretic peptides - importance of BNP and NT-proBNP. Implications in heart failure and acute coronary syndrome. Rev Port Cardiol 2004; 23: 1005-1032.
- 10. Pfister R, Scholz M, Wielckens K, Erdmann E, Schneider CA. Use of NT-proBNP in routine testing and comparison to BNP. Eur J Heart Fail 2004; 6: 289-293.
- 11. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2: 358-367.
- 12. Sahn DJ, DeMaria AN, Kisslo J, Weyman A. The Committee on M-mode Standardization of the American Society of Echocardiography. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978; 58: 1072-1083.
- 13. Alexander JK, Dennis EW, Smith WG, Mad KH, Duncan WC, Austin RC. Blood volume, cardiac output, and distribution of systemic blood flow in extreme obesity. Cardiovasc Res Cent Bull 1962; 1: 39-44.
- 14. Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 2001; 321: 225-236.
- 15. Nielsen SL. Measurement of blood flow in adipose tissue from the washout of Xenon-133 after atraumatic labelling. Acta Physiol Scand 1972; 84: 187-196.
- 16. Vasan RS. Cardiac function and obesity. Heart 2003; 89: 1127-1129.
- 17. Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Wilson PW, et al. Impact of obesity on plasma natriuretic peptide levels. Circulation 2004; 109: 594-600.
- 18. Hanusch-Enserer U, Hermann KM, Cauza E, Spak M, Mahr B, Dunky A, et al. Effect of gastric banding on aminoterminal pro-brain natriuretic peptide in the morbidly obese. Obes Res 2003; 11: 695-698.
- 19. Hermann-Arnhof KM, Hanusch-Enserer U, Kaestenbauer T, Publig T, Dunky A, Rosen HR, et al. N-terminal pro-B-type natriuretic peptide as an indicator of possible cardiovascular disease in severely obese individuals: comparison with patients in different stages of heart failure. Clin Chem 2005; 51: 138-143.
- 20. Hunt PJ, Richards AM, Nicholls MG, Yandle TG, Doughty RN, Espiner EA. Immunoreactive amino-terminal pro-brain natriuretic peptide (NT-PROBNP): a new marker of cardiac impairment. Clin Endocrinol 1997; 47: 287-296.
- 21. Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth 2000; 85: 91-108.
- 22. Grandi AM, Laurita E, Selva E, Piantanida E, Imperiale D, Giovanella L, et al. Natriuretic peptides as markers of preclinical cardiac disease in obesity. Eur J Clin Invest 2004; 34: 342-348.
Correspondence and Footnotes
Publication Dates
-
Publication in this collection
07 Jan 2007 -
Date of issue
Feb 2007
History
-
Accepted
22 Nov 2006 -
Received
20 Dec 2005