Abstract
The aim of the present study was to determine whether specific subgroups of schizophrenic patients, grouped according to electrodermal characteristics, show differences in the N-acetylaspartate/creatine plus choline (NAA / (Cr + Cho)) ratios in the frontal, cingulate and perirolandic cortices. Skin conductance levels (SCL) and skin conductance responses to auditory stimulation were measured in 38 patients with schizophrenia and in the same number of matched healthy volunteers (control). All subjects were submitted to multivoxel proton magnetic resonance spectroscopic imaging. When compared to the control group, patients presented significantly lower NAA / (Cr + Cho) ratios in the right dorsolateral prefrontal cortex (schizophrenia = 0.95 ± 0.03; control = 1.12 ± 0.04) and in the right (schizophrenia = 0.88 ± 0.02; control = 0.94 ± 0.03) and left (schizophrenia = 0.84 ± 0.03; control = 0.94 ± 0.03) cingulates. These ratios did not differ between electrodermally responsive and non-responsive patients. When patients were divided into two groups: lower SCL (less than the mean SCL of the control group minus two standard deviations) and normal SCL (similar to the control group), the subgroup with a lower level of SCL showed a lower NAA / (Cr + Cho) ratio in the left cingulate (0.78 ± 0.05) than the controls (0.95 ± 0.02, P < 0.05) and the subgroup with normal SCL (0.88 ± 0.03, P < 0.05). There was a negative correlation between the NAA / (Cr + Cho) ratio in the left cingulate of patients with schizophrenia and the duration of the disease and years under medication. These data suggest the existence of a schizophrenic subgroup characterized by low SCL that could be a consequence of the lower neuronal viability observed in the left cingulate of these patients.
Magnetic resonance spectroscopy; Skin conductance; Schizophrenia; N-acetylaspartate; Cingulate region; Dorsolateral prefrontal cortex
Braz J Med Biol Res, December 2008, Volume 41(12) 1132-1141
Proton magnetic resonance spectroscopy of the frontal, cingulate and perirolandic cortices and its relationship to skin conductance in patients with schizophrenia
R.F. Sanches1, J.A.S. Crippa1, J.E.C. Hallak1, J.P.M. de Sousa1, D. Araújo2, A.C. Santos2 and  Correspondence and Footnotes
Correspondence and Footnotes
 A.W. Zuardi1
A.W. Zuardi1
1Departamento de Neurociências e Ciências do Comportamento, 2Divisão de Radiologia, Departamento de Clínica Médica, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, SP, Brasil
 Patients and Methods
Patients and Methods
 References
References
 Correspondence and Footnotes
Correspondence and Footnotes=
Correspondence and Footnotes
Correspondence and Footnotes
Correspondence and Footnotes=
Correspondence and Footnotes
Abstract
The aim of the present study was to determine whether specific subgroups of schizophrenic patients, grouped according to electrodermal characteristics, show differences in the N-acetylaspartate/creatine plus choline (NAA / (Cr + Cho)) ratios in the frontal, cingulate and perirolandic cortices. Skin conductance levels (SCL) and skin conductance responses to auditory stimulation were measured in 38 patients with schizophrenia and in the same number of matched healthy volunteers (control). All subjects were submitted to multivoxel proton magnetic resonance spectroscopic imaging. When compared to the control group, patients presented significantly lower NAA / (Cr + Cho) ratios in the right dorsolateral prefrontal cortex (schizophrenia = 0.95 ± 0.03; control = 1.12 ± 0.04) and in the right (schizophrenia = 0.88 ± 0.02; control = 0.94 ± 0.03) and left (schizophrenia = 0.84 ± 0.03; control = 0.94 ± 0.03) cingulates. These ratios did not differ between electrodermally responsive and non-responsive patients. When patients were divided into two groups: lower SCL (less than the mean SCL of the control group minus two standard deviations) and normal SCL (similar to the control group), the subgroup with a lower level of SCL showed a lower NAA / (Cr + Cho) ratio in the left cingulate (0.78 ± 0.05) than the controls (0.95 ± 0.02, P < 0.05) and the subgroup with normal SCL (0.88 ± 0.03, P < 0.05). There was a negative correlation between the NAA / (Cr + Cho) ratio in the left cingulate of patients with schizophrenia and the duration of the disease and years under medication. These data suggest the existence of a schizophrenic subgroup characterized by low SCL that could be a consequence of the lower neuronal viability observed in the left cingulate of these patients.
Key words: Magnetic resonance spectroscopy; Skin conductance; Schizophrenia; N-acetylaspartate; Cingulate region; Dorsolateral prefrontal cortex
Introduction
The diagnosis of schizophrenia is based on a group of symptoms, which may differ from patient to patient. Psychotic symptoms such as hallucinations are usually explained by one mechanism, whereas negative symptoms by another. Therefore, different neural mechanisms may be involved to different extents for individual patients with the same nosological diagnosis (1). An alternative approach would be to assume the heterogeneity of schizophrenia as a nosological entity and to try to identify homogeneous subgroups based on biological and behavioral parameters (2).
Electrodermal activity alterations are among the most cited abnormalities in the psychophysiological study of schizophrenia and have also been postulated to be predictors of functional outcome (3). The main findings that have been identified in schizophrenia in this field are low skin conductance responses to auditory stimulation (SCR) and abnormalities in the skin conductance level (SCL). These parameters are often higher during psychotic states of schizophrenia (4), suggesting that they may be "state" and not "trait"-related abnormalities. However, they also have a "trait" property since significant stability of SCR and SCL over a 1-year period has been reported in both healthy subjects and schizophrenic patients, especially those who are clinically stabilized (5).
In one of our studies on electrodermal activity in clinically stabilized schizophrenic patients, we identified a subgroup with low SCR, low SCL, deficits in selective attention evaluated by the Stroop task performance and predominance of negative symptoms (6). In a voxel-based morphometry study, we observed that schizophrenic patients with low SCL showed lower regional gray matter density in the right frontal areas compared to healthy volunteers and to schizophrenic patients with normal SCL (7). Moreover, prefrontal and anterior cingulate areas were shown to be more activated during the performance of the modified Stroop task in schizophrenic patients than in healthy controls (8). These results suggest that frontal and cingulate areas could be related to the alterations observed in a subgroup of schizophrenic patients with low SCL and deficits in selective attention.
Volumetric regional changes observed with cerebral magnetic resonance imaging (MRI) may be preceded by changes in regional metabolites (9). Magnetic resonance spectroscopy (MRS) is a neuroimaging technique that can quantify chemical cerebral compounds noninvasively (10). Among the substances identified by MRS, N-acetylaspartate (NAA) is one of the most studied, with altered concentrations reported in several neuropsychiatric disorders (11). NAA is present only in neurons, being a marker of neuronal integrity (12), although it has been questioned whether NAA reflects neuronal function alone (13). NAA as a neuronal marker in MRS was reported in many studies, mainly in patients with epilepsy. Li et al. (14) reported low NAA levels in the contralateral hippocampus as a prognostic factor for mesial temporal lobe epilepsy surgery. The same authors later found normalization of the levels of this compound in patients with temporal lobe epilepsy who were seizure-free after surgery.
Schizophrenic patients may present alterations in absolute and relative concentrations of NAA in different cerebral regions, including the frontal lobe and hippocampus (15). Relative ratios may be calculated by dividing NAA concentrations by the concentration of a metabolite whose concentration would be expected to be stable, such as creatine (Cr) or choline (Cho). However, a reduction of NAA in the frontal and cingulate areas of patients with schizophrenia has not been found consistently (16-18). These contradictory findings may be due, in part, to the heterogeneous characteristics of schizophrenia, or to different methodological approaches.
The study of electrodermal activities and NAA / (Cr + Cho) ratios could be an important step towards the understanding of the neurobiology of psychoses in general and of schizophrenia in particular. Discriminating different subgroups can have therapeutic and pathophysiological implications. We determined the NAA / (Cr + Cho) ratios in frontal, cingulated and perirolandic areas of subgroups of schizophrenic patients stratified according to their electrodermal activity (SCR or SCL). The perirolandic area was included in the study as a control area, since it is not expected to be involved (19). The working hypothesis for the present study was that patients with low SCR and SCL would present lower NAA levels in frontal and cingulated areas.
Patients and Methods

Subjects
Thirty-eight volunteers diagnosed with schizophrenia, outpatients of the University Hospital of the Ribeirão Preto Medical School, University of São Paulo, were compared to 38 healthy controls from the general population recruited by an advertisement in a local newspaper. After enrollment, healthy volunteers were screened for psychiatric and neurologic disorders and were matched to the patient group. They received remuneration for their participation in the experiment at a level approved by the local Ethics Committee.
One of the patients could not be screened, and therefore was excluded from the study, along with his respective control.
The clinical diagnosis of schizophrenia was confirmed by means of the "Structured Clinical Interview for DSM-IV", clinical version (SCID-IV-CV) (20), translated and validated for the Portuguese language (21). The schizophrenia subtypes were: paranoid (68.4%), disorganized (18.4%) and undifferentiated (13.2%). Patients in acute episodes of the disorder were excluded after evaluation by the "Brief Psychiatric Rating Scale" (BPRS) (22), version by Bech et al. (23), translated and validated for the Portuguese language (24). The interviews were performed using the Structured Interview Guide for the BPRS (25). Patients were excluded if their scores were higher than two (presence of the symptom in a low degree) for each item (except for the items corresponding to the negative symptoms).
Other exclusion criteria were: a) history of brain injury; b) other organic mental or neurologic disorders; c) substance abuse within the last year; d) metallic implants, foreign bodies, pregnancy, or other conditions that could prevent patients from being submitted to MRI scanning. characteristics (age at the onset and length of the disease, number of previous hospitalizations, length and type of medication, dose of antiparkinsonian medications). The subjects' handedness was evaluated by the Edinburgh Handedness Inventory (26) and the socioeconomic level of the subjects and their respective parents was assessed by the Brazil Socioeconomic Classification Criteria (Critério de Classificação Sócio-Econômica Brasil, CCSEB) (27). Negative symptoms were evaluated by the negative subscale of the Positive and Negative Syndrome Scale (PANSS) (28) for schizophrenia, translated and validated for the Portuguese language (29). Two psychiatrists (A.W.Z. and J.E.C.H.), experienced in psychopharmacology, blindly and independently categorized the group of medications used by each patient according to the potential for anticholinergic effects (low, moderate and high), and were in agreement for 84% of the patients. Disagreements were solved by consensus between the two evaluators.
Patients and controls were paired according to sex, age, personal and parents' socio-economic level, schooling, and handedness. Table 1 shows the clinical and demographic characteristics of patients and controls.
All subjects and relatives responsible for them (whenever necessary due to cognitive constraints) gave written informed consent after being fully informed of the research procedure. The project was approved by the local Ethics Committee (#HCRP 5428/99).
Skin conductance
Electrodermal measurements were performed as described by Lopes-Machado et al. (6) in a sound-attenuated room under dim light. Subjects were asked to sit still in a comfortable armchair and were observed through a unidirectional mirror. A computer-controlled, voltage-constant (0.6 V) module with automatic back off (Contact Precision Instruments, UK) measured skin conductance. Two standard silver/silver chloride electrodes (Beckman, UK) were fixed with adhesive tape in the medial phalanges of the index and middle fingers of the right hand in right-handed subjects and of the left hand in left-handed subjects. Contact with the skin was improved with high conductance gel (KY gel, Johnson and Johnson, Brazil).
Measurements were made in two phases: A) Experimental tonic period of pre-stimulation (or rest), which lasted 5 min. In this experiment, the SCL and the number of non-specific responses (spontaneous fluctuation, with deflections equal to or greater than 0.05 µS) were recorded. SCL values were the average of the minute-by-minute log SCL measured during the resting phase. B) Phasic experiment of auditory stimulation, which lasted 10 min. The stimulus consisted of ten 1-s tones of 80 dB, 800 Hz and 10 ms rise time, which were presented binaurally at pseudo-random intervals (40-80 s, mean 60 s). In this period, specific responses were recorded (SCR), and the amplitude of each response was measured. SCR were considered if they occurred within a response window of 1 to 5 s after the tone, and with a variation equal to or greater than 0.05 µs. The number of non-specific responses, which occurred during the 20-s interval that preceded each tone, was recorded.
Subjects were grouped according to their electrodermal responses to the tones: non-responsive (absence of SCR to all stimuli) and responsive (at least one SCR response), according to the strict criterion by Dawson et al. (4)
The subjects were also grouped according to their basal level of skin conductance. The mean SCL of the control group less two standard deviations was used as the cut-off to identify schizophrenic patients with low SCL.
Proton magnetic resonance spectroscopy
All subjects were scanned with a 1.5 Tesla magnet with gradients of 25 mT, model Magnetom Vision (Siemens, Germany), using a standard transmitter/receiver head coil of circular polarization. The structural imaging protocol included a gradient-echo 3-D sagittal acquisition, MPRAGE, T1-weighted sequence (TE = 4 ms, TR = 9.7 ms, 1-mm thick slices), and axial, TSE T2-weighted sequence (TE = 90 ms, TR: 4000 ms, 5-mm thick slices). The images were analyzed to exclude structural abnormalities and to localize the volume-of-interest for spectroscopic analysis. Localization was consistent among subjects. A print template image of the ideal positioning was kept in the acquisition console for constant comparison. Landmarks such as the central sulcus, the hand motor area, and the superior frontal sulcus were used as references.
A neurologist (D.A.) with expertise in this technique, who was blind to the diagnoses or groups, performed all examinations. Patients and controls were positioned in the scanner by the same person, using a laser beam to control the degree of neck hyperextension and rotation.
Proton MRS (1H-MRS) was performed with a multivoxel sequence (CSI hybrid), PRESS (point-resolved spectroscopy - TE = 135 ms, TR = 1500 ms) and water suppression with a selective saturation pulse. The volume-of-interest was represented by a grid of 64 juxtaposed voxels of 20 x 10 x 10 mm (covering 20 x 80 x 80 mm), positioned above the corpus callosum, perpendicular to the anterior commissure-posterior commissure line, over the frontal lobe (Figure 1). Four voxels over the anterior middle frontal gyrus were selected to represent the frontal area, four for the perirolandic, over the primary motor and sensitive areas, and six for the cingulate region, on both sides of the interhemispheric fissure (Figure 1). Total scanning time for the spectroscopy sequence was maintained at <10 min, including positioning, to avoid movement artifacts. Saturation bands were used in the external voxels to prevent "voxel bleeding" from peripheral regions with cranial fat or bone.
Spectroscopic data were processed using the Siemens® software, with a standard algorithm that included a fast Fourier transform, zero filling, and apodization, installed in an auxiliary console workstation (Unix Sun Spark Systems). Apodization was performed with a Gaussian filter centered at 0.0 and with a width of 256 ms. The post-processing protocol included a polynomial base-line correction procedure of order 5. The phase was corrected on the basis of the best fit to the NAA peak, trying to match both peak borders. Calculating the area under the peak and fitting were performed automatically by the manufacturer's software. The area was calculated as the integral under the curve. Fitting was carried out by automatic triangulation with 10 iterations. Parameters of precession frequency were set at 2.2 ppm for NAA, 3.0 ppm for Cr, and 3.5 ppm for Cho.
To determine the voxels for analysis (spectrum quality), the following parameters were used: baseline variation, definition of the peaks and maximum width at half length of each peak (less than 10 Hz). Spectra that did not meet these criteria were excluded from the sample. Manual baseline and phase correction were performed whenever possible.
Quantitative spectroscopy maps were transferred as .txt files to Excel (Microsoft®) template tables. The tables were organized to automatically report NAA, Cr, and Cho raw numbers, ratios, and asymmetry indexes. Raw numbers were assumed to be proportional to concentrations.
The NAA / (Cr + Cho) ratios, for each region and each side, was used for comparison among groups. Therefore, six measurements were recorded for each patient: frontal left and right ratios, perirolandic left and right ratios, cingulated left and right ratios.
Procedure
Subjects were evaluated individually in three sessions, with a maximum of 30 days between the first and the last. During the first session, the subjects signed an informed consent form and were then evaluated in terms of the inclusion and exclusion criteria, clinical history, and SCID-IV-CV. In the second session, the patients were once more evaluated with the BPRS and PANSS _ negative subscale. For every 5 patients evaluated, 1 patient was re-interviewed by a different psychiatrist, who also applied the tests independently in order to evaluate their reliability throughout the study. In this session, the subjects were submitted to skin conductance measurements. In the final session, the subjects were submitted to 1H-MRS without sedation. The MRS data were always acquired in non-clinical settings, away from current clinical MRI studies. Usually on the weekends, patients and controls were alternated, without the previous knowledge of the radiologist or the MRI technician.
Analysis of the results
The results of the NAA / (Cr + Cho) ratios for each region of interest in the schizophrenic and control subgroups, organized according to electrodermal responsiveness, were submitted to a two-way ANOVA for the factors diagnosis, responsiveness and interaction, then the Duncan test was used for post hoc comparison test. The same results, organized according to the level of basal conductance, were submitted to a one-way ANOVA.
Correlations between the variables were determined with the Spearman coefficient of correlation procedure. The statistical analysis was performed with the Statistical Package for Social Sciences (SPSS), version 10.0, and the significance level was set at P ≤ 0.05.
Results
Skin conductance respose
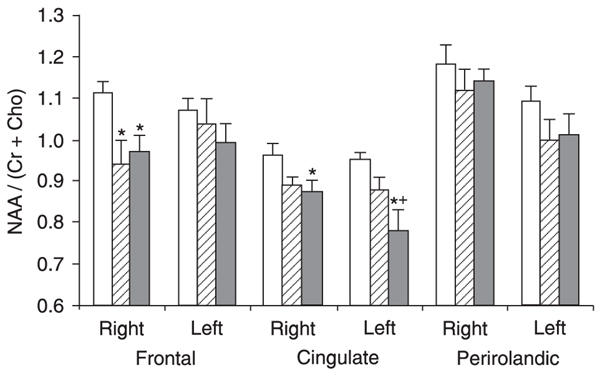
Subjects were divided into four experimental subgroups according to SCR: responsive schizophrenic (SCHIZ-R; N = 16), non-responsive schizophrenic (SCHIZ-N; N = 21), responsive controls (CONT-R; N = 27), and non-responsive controls (CONT-N; N = 10). The demographic, clinical, and electrodermal conductance characteristics of the four groups are shown in Table 2.
There was a predominance of men in the responsive group compared with the non-responsive group. Conversely, no significant differences were observed among the four groups regarding age, schooling and handedness. There were no differences between the two patient groups in terms of antipsychotic equivalence (in mg of chlorpromazine), anticholinergic potential of the medication used, number of hospital admissions, age at disease onset, length of disease, or antipsychotic use. The SCHIZ-N subgroup showed higher values in the PANSS negative subscale than the SCHIZ-R subgroup. The subgroups SCHIZ-N and CONT-N presented significantly less spontaneous fluctuations of skin conductance compared with the SCHIZ-R group. Moreover, the subgroups SCHIZ-N and SCHIZ-R presented significantly lower levels of basal skin conductance than the subgroups CONT-N and CONT-R, and the value of SCHIZ-N was even lower than SCHIZ-R.
The two-way ANOVA indicated a significant effect for diagnostic factor in the right frontal cortex (F = 9.9; P < 0.01) and cingulate bilaterally (right F = 5.9; P < 0.05/left F = 7.4; P < 0.01). There was no main effect for the SCR factor or diagnostic by SCR interaction. The average NAA / (Cr + Cho) ratio in the right frontal cortex was significantly lower for schizophrenic patients (0.95 ± 0.03) than for controls (1.12 ± 0.04). This was also the finding in the right cingulate (SCHIZ = 0.88 ± 0.02; CONT = 0.94 ± 0.03), and left cingulate (SCHIZ = 0.84 ± 0.03; CONT = 0.94 ± 0.03) comparisons. No differences were observed in SCR in any of the areas investigated by spectroscopy, nor was there any interaction between the factors diagnosis and SCR.
Basal conductance level
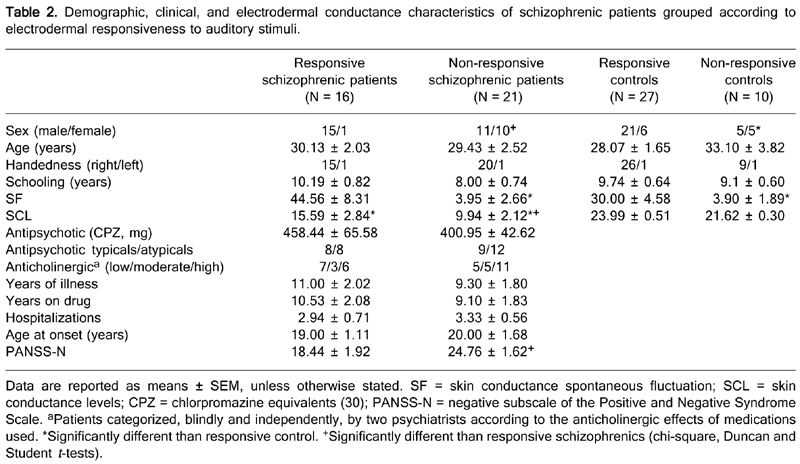
Figure 2 shows the distribution of subjects according to their basal conductance level. Three groups are presented. The schizophrenic patients were divided into two groups, one with low conductance level (SCHIZ-L; N = 19) and the other with conductance level similar to that of the controls (SCHIZ-N; N = 18).
Table 3 shows the clinical and demographic characteristics of the three subgroups, grouped according to basal electrodermal conductance levels. No statistically significant differences were observed among the three subgroups, except for the basal conductance level of subgroup SCHIZ-L, which was significantly lower than that of the two other subgroups.
Figure 3 shows the values for NAA / (Cr + Cho) of the three subgroups with respect to basal electrodermal conductance levels in the frontal, cingulate and perirolandic areas. Ratios were different comparing patients and controls in the right frontal region. The subgroup of schizophrenics with low basal SCL differed from the control group in the cingulate, bilaterally. In the left cingulate, this subgroup (low basal SCL) of schizophrenics also differed from the other subgroup (normal level) of patients.
Correlations
Negative correlations were observed between age and NAA / (Cr + Cho) ratios in the right and left cingulate gyrus for controls (r = -0.39, P < 0.02; r = -0.44, P < 0.01; respectively) and patients (r = -0.37, P = 0.02; r = -0.43, P < 0.01, respectively). Among the patients, the NAA / (Cr + Cho) ratios correlated negatively with duration of disease (r = - 0.39, P < 0.02) and years on medication (r = -0.41, P < 0.02) in the left but not in the right cingulate gyrus.
Midsaggital (A), axial (B) and coronal (C) magnetic resonance spectroscopy images of a normal comparison subject with the representative voxel box superimposed.
Scatter diagram of skin conductance levels during a 5-min rest period. Points indicate mean value for each subject.
NAA / (Cr + Cho) ratio for the control group (N = 37; open bars), patients with normal conductance levels (N = 18; stripped lined bars) and schizophrenic patients with low conductance levels (N = 19; closed bars) in the frontal, cingulate and perirolandic cortices. Asterisks indicate a statistically significant difference compared to controls and the plus indicates a significant difference between the subgroups of schizophrenics (ANOVA).
Demographic, clinical, and electrodermal conductance characteristics of schizophrenic patients grouped according to electrodermal responsiveness to auditory stimuli.
Demographic, clinical, and electrodermal conductance characteristics of subjects grouped according to basal skin conductance level.
Discussion
In this study, the group of schizophrenic patients had significantly lower NAA / (Cr + Cho) ratios compared to controls in the right frontal and bilateral cingulate areas. There were no differences in the perirolandic areas.
Other results reported in the literature should be treated with some caution because of methodological differences among the studies. One of the main limitations of MRS is its relatively low spatial resolution. In single voxel techniques, some studies report voxels as large as 8.0 cm3. For that reason, conclusions at the cellular level cannot be made. The voxel size in our study was 2.0 cm3, and with volumes much larger, one must be careful to describe regional metabolic alterations. A critical review of the methodology used in 1H-MRS studies of the frontal lobe in schizophrenics (18) selected 6 studies with a methodological rigor similar to that of the present study, including the appropriate number of subjects, long echo time (ideal for NAA quantification) and small voxel volume. From the 6 studies selected, 4 reported similar findings to the present study, showing NAA reduction in frontal regions (17,31-33) and 2 reported negative results (16,34).
Greater grey matter volume in the dorsomedial prefrontal cortex was associated with better performance in the Stroop task with respect to interference (35). In this way, the lower levels of NAA in the right anterior middle frontal gyrus observed in the present study may reflect reduction of neuronal viability in this area and might be associated with the attention deficits previously observed in schizophrenic patients with low SCL, through the higher interference time in the Stroop task (6).
The anterior cingulate gyrus is active in cognitive, motor and affective functions, but it also has an important role in selective attention and achievement-oriented behaviors (36).
Primary motor and sensitive areas did not show any differences. This result can give some credibility to the present study, since positive findings in these areas were not expected a priori.
The NAA / (Cr + Cho) ratios did not differ between SCHIZ-R and SCHIZ-N. Electrodermal responsiveness to auditory stimuli failed to identify a subgroup of schizophrenics with lower values of NAA, at least for those areas.
The individual results of basal SCL suggest that two subgroups of schizophrenic patients can be identified: one with SCL similar to that of the healthy control, and another with low SCL. This is a very unusual finding, since a continuous distribution should be expected here. Previous studies have shown lower mean SCL in patients compared to controls (37), but the present study suggests that this occurs only in one subgroup of patients. There were no differences between these two subgroups regarding the mean doses of antipsychotic and anticholinergic medications or the proportion of patients receiving typical and atypical antipsychotic agents, which suggests that the patients' treatment does not explain the low conductance levels found for one of the patient subgroups.
The results of the present study do not confirm the observation by Dawson et al. (4), in which a group of patients showed higher SCL than controls. This discrepancy may have occurred because only patients who were not in acute episodes were enrolled in our study. It is well-known that SCL may be higher during acute episodes of schizophrenia. Age and duration of illness may also account for the discrepancies between the studies (4). For instance, the electrodermal nonresponsiveness, negative symptoms, poor functional outcome, and cognitive deficits are all more often seen in older patients with longer duration of illness (3).
The subgroup of patients with low SCL also has lower NAA / (Cr + Cho) ratio in the left cingulate compared to controls and to the other subgroup of patients. Thus, it was possible to identify a subgroup of patients who, in addition to lower SCL, also have shown lower neuronal viability in the anterior left cingulate.
Lower neuronal viability may be related to the duration of the disease. Duration of illness and years on medication were about 3 years longer in the low conductance subgroup, although not statistically significant. Moreover, only in the left cingulate, a negative correlation of the NAA / (Cr + Cho) ratios was observed with duration of disease and years on medication. A correlation between NAA levels in the anterior cingulate and duration of schizophrenia was also reported by Ende et al. (38), who showed that this correlation remained significant even when the levels had been corrected for the age effect in the control group. These results differ from those reported by Deicken et al. (32). A possible explanation for the absence of correlations in their studies could be the longer time of illness in their sample (mean = 16.5 years). There is evidence suggesting that a degenerative process of the disorder may occur more expressively in the first years (36).
A possible influence of the type of antipsychotic drug used could account for the lower NAA levels observed in the low SCL subgroup, since typical antipsychotics, differently from atypical ones, are associated with lower NAA levels in the anterior cingulate (38). However, the proportion of patients receiving typical and atypical antipsychotics was the same in the present study. This suggests that the type of antipsychotic is not likely to explain the differences in NAA / (Cr + Cho) ratios between the two subgroups.
The lower neuronal viability in the left anterior cingulate could be related to deficient autonomic responses. Patients with pure autonomic failure who do not activate autonomic responses, including skin conductance, in response to physical or cognitive efforts, have shown a smaller volume of gray matter in the left anterior cingulate (39). Also, Critchley et al. (40), using positron emission tomography in healthy volunteers, observed that the left anterior cingulate was activated during the voluntary effort for relaxation through biofeedback, resulting in reduction of the level of skin conductance. Such observations suggest that the left anterior cingulate is involved in the intentional modulation of alert states and their peripheral body repercussions, such as skin conductance. This could be a physiological explanation to the lower SCL found in our sample.
The results of the present study suggest a decrease of neuronal viability in the left anterior cingulate of patients with schizophrenia, associated with the duration of the disease and that this change could justify the observed decrease in SCL. Further studies may possibly identify cognitive and emotional characteristics specific to this subgroup of schizophrenic patients.
 Address for correspondence: A.W. Zuardi, Departamento de Neurociências e Ciências do Comportamento, FMRP, USP, Av. Bandeirantes, 3900, 14040-900 Ribeirão Preto, SP, Brasil. Fax: +55-16-3602-2544. E-mail: awzuardi@fmrp.usp.br
Address for correspondence: A.W. Zuardi, Departamento de Neurociências e Ciências do Comportamento, FMRP, USP, Av. Bandeirantes, 3900, 14040-900 Ribeirão Preto, SP, Brasil. Fax: +55-16-3602-2544. E-mail: awzuardi@fmrp.usp.br
Research supported in part by CNPq (#554490/2005-6) and FAPESP (#02/13197-2). J.A.S. Crippa and A.W. Zuardi are recipients of CNPq Productivity fellowships (#303546/2005-0 and #302542/2007-8, respectively). Received March 24, 2008. Accepted December 4, 2008.
- 1. Andreasen NC. Schizophrenia: the fundamental questions. Brain Res Brain Res Rev 2000; 31: 106-112.
- 2. Buchsbaum MS, Haier RJ. Psychopathology: biological approaches. Annu Rev Psychol 1983; 34: 401-430.
- 3. Schell AM, Dawson ME, Rissling A, Ventura J, Subotnik KL, Gitlin MJ, et al. Electrodermal predictors of functional outcome and negative symptoms in schizophrenia. Psychophysiology 2005; 42: 483-492.
- 4. Dawson ME, Nuechterlein KH, Schell AM, Gitlin M, Ventura J. Autonomic abnormalities in schizophrenia. State or trait indicators? Arch Gen Psychiatry 1994; 51: 813-824.
- 5. Schell AM, Dawson ME, Nuechterlein KH, Subotnik KL, Ventura J. The temporal stability of electrodermal variables over a one-year period in patients with recent-onset schizophrenia and in normal subjects. Psychophysiology 2002; 39: 124-132.
- 6. Lopes-Machado EZ, Crippa JA, Hallak JE, Guimaraes FS, Zuardi AW. Electrodermically nonresponsive schizophrenic patients make more errors in the Stroop Color Word Test, indicating selective attention deficit. Schizophr Bull 2002; 28: 459-466.
- 7. Zuardi AW, Borduqui T, Hallak JC, Crippa JA, Araújo D, Santos AC. Grey matter correlates of skin conductance levels in patients with schizophrenia and healthy volunteers: a voxel-based morphometry study. World J Biol Psych 2007; 8: 143.
- 8. Weiss EM, Golaszewski S, Mottaghy FM, Hofer A, Hausmann A, Kemmler G, et al. Brain activation patterns during a selective attention test - a functional MRI study in healthy volunteers and patients with schizophrenia. Psychiatry Res 2003; 123: 1-15.
- 9. Narayana PA, Doyle TJ, Lai D, Wolinsky JS. Serial proton magnetic resonance spectroscopic imaging, contrast-enhanced magnetic resonance imaging, and quantitative lesion volumetry in multiple sclerosis. Ann Neurol 1998; 43: 56-71.
- 10. Matson GB, Weiner M. Spectroscopy. In: Stark DD, Bradley WG (Editors), Magnetic resonance imaging 3rd edn. St. Louis: Mosby; 1999. p 181-214.
- 11. Buckley PF, Friedman L. Magnetic resonance spectroscopy. Bridging the neurochemistry and neuroanatomy of schizophrenia. Br J Psychiatry 2000; 176: 203-205.
- 12. Meyerhoff DJ, MacKay S, Bachman L, Poole N, Dillon WP, Weiner MW, et al. Reduced brain N-acetylaspartate suggests neuronal loss in cognitively impaired human immunodeficiency virus-seropositive individuals: in vivo 1H magnetic resonance spectroscopic imaging. Neurology 1993; 43: 509-515.
- 13. Bhakoo KK, Pearce D. In vitro expression of N-acetyl aspartate by oligodendrocytes: implications for proton magnetic resonance spectroscopy signal in vivo J Neurochem 2000; 74: 254-262.
- 14. Li LM, Cendes F, Antel SB, Andermann F, Serles W, Dubeau F, et al. Prognostic value of proton magnetic resonance spectroscopic imaging for surgical outcome in patients with intractable temporal lobe epilepsy and bilateral hippocampal atrophy. Ann Neurol 2000; 47: 195-200.
- 15. Steen RG, Hamer RM, Lieberman JA. Measurement of brain metabolites by 1H magnetic resonance spectroscopy in patients with schizophrenia: a systematic review and meta-analysis. Neuropsychopharmacology 2005; 30: 1949-1962.
- 16. Callicott JH, Egan MF, Bertolino A, Mattay VS, Langheim FJ, Frank JA, et al. Hippocampal N-acetyl aspartate in unaffected siblings of patients with schizophrenia: a possible intermediate neurobiological phenotype. Biol Psychiatry 1998; 44: 941-950.
- 17. Bertolino A, Callicott JH, Mattay VS, Weidenhammer KM, Rakow R, Egan MF, et al. The effect of treatment with antipsychotic drugs on brain N-acetylaspartate measures in patients with schizophrenia. Biol Psychiatry 2001; 49: 39-46.
- 18. Sanches RF, Crippa JA, Hallak JE, Araujo D, Zuardi AW. Proton magnetic resonance spectroscopy of the frontal lobe in schizophrenics: a critical review of the methodology. Rev Hosp Clin Fac Med São Paulo 2004; 59: 145-152.
- 19. Clarke E, Dewhurst K, Aminoff MJ. An illustrated history of brain function: imaging the brain from antiquity to the present San Francisco: Norman Pub, 1996.
- 20. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV axis I disorders - Clinician Version (SCID-CV) Washington: American Psychiatric Press; 1997.
- 21. Del-Ben CM, Vilela JAA, Crippa JAS, Hallak JEC, Zuardi AW. Confiabilidade teste-reteste da Entrevista Clínica Estruturada para o DSM-IV - Versão Clínica (SCID-CV) traduzida para o português". Rev Bras Psiq 2001; 23: 156-159.
- 22. Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10: 799-812.
- 23. Bech P, Kastrup M, Rafaelsen OJ. Mini-compendium of rating scales for states of anxiety depression mania schizophrenia with corresponding DSM-III syndromes. Acta Psychiatr Scand Suppl 1986; 326: 1-37.
- 24. Zuardi AW, Loureiro SR, Rodrigues CRC, Correa AJ, Glock SS. Estudo da estrutura fatorial, fidedignidade e validade da tradução e adaptação para o português da Escala de Avaliação Psiquiátrica Breve (BPRS) Modificada. Rev Assoc Bras Psiq Assoc Psiq Am Lat 1994; 16: 63-68.
- 25. Crippa JA, Sanches RF, Hallak JE, Loureiro SR, Zuardi AW. A structured interview guide increases Brief Psychiatric Rating Scale reliability in raters with low clinical experience. Acta Psychiatr Scand 2001; 103: 465-470.
- 26. Oldfield RC. The assessment and analysis of handedness: the Edinburgh Inventory. Neuropsychologia 1971; 9: 97-113.
-
27Associação Brasileira de Anunciantes, Associação Nacional das Empresas de Pesquisa de Mercado (ANEP), Associação Brasileira dos Institutos de Pesquisa de Mercado (ABIPEME). Critério de Classificação Sócio-Econômica Brasil (CCSEB) 1997.
- 28. Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13: 261-276.
- 29. Chaves AC, Shirakava I. Escala das síndromes negativa e positiva - PANSS e seu uso no Brasil. Rev Psiquiatr Clín 1998; 25: 337-343.
- 30. Atkins M, Burgess A, Bottomley C, Riccio M. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatr Bull 1997; 21: 224-226.
- 31. Deicken RF, Zhou L, Corwin F, Vinogradov S, Weiner MW. Decreased left frontal lobe N-acetylaspartate in schizophrenia. Am J Psychiatry 1997; 154: 688-690.
- 32. Deicken RF, Zhou L, Schuff N, Weiner MW. Proton magnetic resonance spectroscopy of the anterior cingulate region in schizophrenia. Schizophr Res 1997; 27: 65-71.
- 33. Callicott JH, Bertolino A, Mattay VS, Langheim FJ, Duyn J, Coppola R, et al. Physiological dysfunction of the dorsolateral prefrontal cortex in schizophrenia revisited. Cereb Cortex 2000; 10: 1078-1092.
- 34. Sigmundsson T, Maier M, Toone BK, Williams SC, Simmons A, Greenwood K, et al. Frontal lobe N-acetylaspartate correlates with psychopathology in schizophrenia: a proton magnetic resonance spectroscopy study. Schizophr Res 2003; 64: 63-71.
- 35. Premkumar P, Fannon D, Kuipers E, Cooke MA, Simmons A, Kumari V. Association between a longer duration of illness, age and lower frontal lobe grey matter volume in schizophrenia. Behav Brain Res 2008; 193: 132-139.
- 36. Marquardt RK, Levitt JG, Blanton RE, Caplan R, Asarnow R, Siddarth P, et al. Abnormal development of the anterior cingulate in childhood-onset schizophrenia: a preliminary quantitative MRI study. Psychiatry Res 2005; 138: 221-233.
- 37. Perry W, Felger T, Braff D. The relationship between skin conductance hyporesponsivity and perseverations in schizophrenia patients. Biol Psychiatry 1998; 44: 459-465.
- 38. Ende G, Braus DF, Walter S, Weber-Fahr W, Soher B, Maudsley AA, et al. Effects of age, medication, and illness duration on the N-acetyl aspartate signal of the anterior cingulate region in schizophrenia. Schizophr Res 2000; 41: 389-395.
- 39. Critchley HD, Good CD, Ashburner J, Frackowiak RS, Mathias CJ, Dolan RJ. Changes in cerebral morphology consequent to peripheral autonomic denervation. Neuroimage 2003; 18: 908-916.
- 40. Critchley HD, Melmed RN, Featherstone E, Mathias CJ, Dolan RJ. Brain activity during biofeedback relaxation: a functional neuroimaging investigation. Brain 2001; 124: 1003-1012.
Correspondence and Footnotes
Publication Dates
-
Publication in this collection
12 Jan 2009 -
Date of issue
Dec 2008
History
-
Received
24 Mar 2008 -
Accepted
04 Dec 2008