Abstract:
Co-infection of tuberculosis (TB)-HIV/AIDS is a persistent public health problem in Brazil. This study describes epidemiological patterns and time trends of mortality related to TB-HIV/AIDS co-infection. Based on mortality data from 2000-2011 (almost 12.5 million deaths), 19,815 deaths related to co-infection were analyzed. The average age-adjusted mortality rate was 0.97 deaths/100,000 inhabitants. The highest mortality rates were found among males, those in economically productive age groups, black race/color and residents of the South region. There was a significant reduction in the mortality coefficient at the national level (annual average percent change: -1.7%; 95%CI: -2.4; -1.0), with different patterns among regions: increases in the North, Northeast and Central regions, a reduction in the Southeast and a stabilization in the South. The strategic integration of TB-HIV/AIDS control programmes is fundamental to reduce the burden of mortality related to co-infection in Brazil.
Keywords:
Tuberculosis; HIV; Acquired Immunodeficiency Syndrome; Time Series Studies
Resumo:
A coinfecção tuberculose (TB)-HIV/AIDS é um problema de saúde pública persistente no Brasil. Neste estudo, descrevem-se padrões epidemiológicos e tendências temporais da mortalidade relacionada à coinfecção TB-HIV/AIDS. Baseado em dados de mortalidade de 2000-2011 (quase 12,5 milhões de mortes), foram analisados 19.815 óbitos relacionados à coinfecção. O coeficiente médio de mortalidade padronizado por idade foi de 0,97 óbitos/100 mil habitantes. Os maiores coeficientes de mortalidade foram verificados no sexo masculino, grupos etários economicamente produtivos, raça/cor negra e residentes da Região Sul. Houve diminuição significativa dos coeficientes de mortalidade em nível nacional (variação percentual anual média: -1,7%; IC95%: -2,4; -1,0), com diferentes padrões entre regiões: aumento nas regiões Norte, Nordeste e Centro-oeste, redução na Sudeste e estabilização na Sul. A integração estratégica dos programas de controle de TB-HIV/AIDS é fundamental para reduzir a carga de mortalidade relacionada à coinfecção no Brasil.
Palavras-chave:
Tuberculose; HIV; Síndrome de Imunodeficiência Adquirida; Estudos de Séries Temporais
Resumen:
La coinfección tuberculosis (TB)-VIH/SIDA es un problema de salud pública persistente en Brasil. En este estudio, se describen patrones epidemiológicos y tendencias temporales de la mortalidad relacionada con la coinfección TB-VIH/SIDA. Basado en datos de mortalidad de 2000-2011 (casi 12,5 millones de muertes), fueron analizadas 19.815 muertes, todas relacionadas con la coinfección. El coeficiente medio de mortalidad ajustado por edad fue de 0,97 muertes/100.000 habitantes. Los mayores coeficientes se verificaron en el sexo masculino, grupos de edad económicamente productivos, raza negra y residentes de la región Sur. Hubo una disminución significativa del coeficiente de mortalidad a nivel nacional (variación porcentual anual media: -1,7%; IC95%: -2,4; -1,0), con diferentes patrones entre regiones: aumento en las regiones Norte, Nordeste y Centro-oeste, reducción en el Sudeste y estabilización en el Sur. La integración estratégica de los programas de control de TB-VIH/SIDA es fundamental para reducir la carga de mortalidad, relacionada con la coinfección en Brasil.
Palabras-clave:
Tuberculosis; VIH; Síndrome de Inmunodeficiencia Adquirida; Estudios de Series Temporales
Introduction
HIV/AIDS is an important and persistent public health problem in Brazil and worldwide, with a high morbidity and mortality burden, mainly when related to opportunistic infections such as tuberculosis (TB) 11. Gupta S, Granich R, Date A, Lepere P, Hersh B, Gouws E, et al. Review of policy and status of implementation of collaborative HIV-TB activities in 23 high-burden countries. Int J Tuberc Lung Dis 2014; 18:1149-58.), (22. Murray CJ, Ortblad KF, Guinovar C, Lim SS, Wolock TM, Allen Roberts D, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 13:1005-70.. People living with HIV/AIDS are 21-34 times more likely to develop active TB as compared to the general population 33. World Health Organization. Global tuberculosis control. Geneva: World Health Organization; 2011.. Active TB in people living with HIV/AIDS is a significant risk factor to increased HIV/AIDS and TB-related case fatality rates. People living with HIV/AIDS with TB are twice more likely to progress to death, in comparison with people living with HIV/AIDS without TB 44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014..
In 2012, approximately 8.7 million individuals developed TB worldwide, 1.1 million (13%) of them living with HIV/AIDS 44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.. On the other hand, about 20% of the 2.8 million people diagnosed with TB and tested for HIV had a positive HIV status. In this group, 42% were living in Sub-Saharan Africa. More than 75% of new cases of TB in HIV-positive patients are concentrated in 10 countries 44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014..
According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), the global goal is to reduce by half the number of deaths due to TB among people living with HIV/AIDS worldwide (to less than 250,000) 44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.. In fact, about 1.3 million individuals benefitted from the integration of TB and HIV/AIDS control programs, and did not progress to death between 2005 and 2012. In 17 of the 41 countries with a high number of co-infected patients with TB and HIV/AIDS, mortality declined by 50% or more. On the other hand, mortality decreased by less than 25% in Brazil during this period 44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.), (66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014..
In Brazil, TB-HIV/AIDS co-infection presents a heterogeneous distribution among population groups 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.. The occurrence of TB-HIV/AIDS co-infection ranged among Brazilian states, from 2.2% in Acre State in the North region to 19.3% in Rio Grande do Sul State in the South region 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.), (77. Morimoto AA, Bonametti AM, Morimoto HK, Matsuo T. Soroprevalência da infecção pelo vírus da imunodeficiência humana em pacientes com tuberculose, em Londrina, Paraná. J Bras Pneumol 2005; 31:325-31.), (88. Guimarães RM, Lobo AP, Siqueira EA, Borges TF, Melo SC. Tuberculosis, HIV, and poverty: temporal trends in Brazil, the Americas, and worldwide. J Bras Pneumol 2012; 38:511-7..There has been a continuous decrease of nationwide mortality related to HIV/AIDS (by 6.6% in the period 2004-2013) 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1)., and TB (by 2.9% in the period 2001-2010) 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.), (1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.. In 2013, 59.2% of new cases diagnosed with TB performed and received the results of HIV testing, with 9.8% TB-HIV/AIDS co-infections 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014..
Despite the clinical, epidemiological and social relevance of TB-HIV/AIDS co-infection in Brazil, there are few systematic studies of national or regional scale on the epidemiological aspects and temporal evolution of mortality related to this co-infection in the country 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.), (99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).. Knowledge of the impact of mortality related to TB-HIV/AIDS co-infection is important to assess endemic dynamics, and to improve surveillance and control activities 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).), (1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.. In this nationwide study, we analyzed the epidemiological patterns and time trends of mortality related to TB-HIV/AIDS co-infection in Brazil, from 2000 to 2011.
Material and methods
Study area
Brazil has a total area of 8.5 million km2 and, in 2015, had an estimated population of 204,5 million inhabitants (in the study period, ranging from 170 million in 2000 to 192.4 million inhabitants in 2011). The country is divided into five administrative geographic regions (South, Southeast, Central, North and Northeast), 27 Federal Units (26 states and one Federal District), and 5,570 municipalities (Brazilian Institute of Geography and Statistics - IBGE; http://www.ibge.gov.br). There are considerable economic, geographical and cultural diversities in each Brazilian region.
Study design and population
We performed a nationwide population-based study in Brazil using official secondary mortality data. We included all deaths related to TB-HIV/AIDS co-infection recorded in Brazil in the period from 2000 to 2011. Co-infection was defined as the concomitant presence of TB and HIV/AIDS on the same death certificate, either as underlying or as associated causes of death: multiple causes of death 1111. Ministério da Saúde; Conselho Federal de Medicina; Centro Brasileiro de Classificação de Doenças. A declaração de óbito: documento necessário e importante. 3a Ed. Brasília: Ministério da Saúde/Conselho Federal de Medicina/Centro Brasileiro de Classificação de Doenças; 2009..
Tuberculosis as cause of death corresponds to the categories included in the group A15-A19 (Tuberculosis), while HIV/AIDS corresponds to the group B20-B24 (Human immunodeficiency virus [HIV] disease) of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) 1212. World Health Organization. National Statistic Classifications of Diseases and Related Health Problems (ICD): 10th revision. Version 2007. Geneva: World Health Organization; 2007..
Data sources
Mortality data were obtained from the Mortality Information System (SIM) of the Brazilian Ministry of Health. SIM data are available at the website of the Informatics Department of the Brazilian Unified National Health System (DATASUS; http://datasus.saude.gov.br). All information in the SIM database is based on death certificates, consisting of a standardized form to be filled out by physicians, which contains demographic (sex, age, race/color, marital status, education, place of residence and year of occurrence of death), and clinical information (underlying and associated causes of death).
In the SIM database, data sets are separated by Federal Unit and year of death. Thus, a total of 324 data files (27 Federal Units, 12 years) with approximately 12.5 million entries were downloaded and merged into a single data file. In a second stage, field codes of different data sets were standardized, and we eliminated variables not considered in the analysis. All death certificates related to TB and HIV/AIDS as a cause of death in any field were identified. New variables for death causes were coded, as in many cases there was more than one documented cause of death per line.
Population data were obtained from the IBGE, based on data from the National Demographic Censuses (2000 and 2010), and population estimates for inter-census years (2001-2009 and 2011). These population data are available in the DATASUS (http://tabnet.datasus.gov.br/cgi/deftohtm.exe?ibge/cnv/popuf.def).
Data analysis
For the descriptive analysis, we present the mean and standard deviation (SD) for continuous variables, and absolute numbers and proportions with their respective 95% confidence intervals (95%CI) for categorical variables.
We calculated crude mortality rates (per 100,000 inhabitants) by sex, age group, race/color and place of residence (states and regions) by dividing the number of deaths by the population in each calendar year, and expressed per 100,000 inhabitants. We calculated age-adjusted mortality rates by the direct method, using as standard the Brazilian population from the 2010 census. The age groups used for standardization and calculation of age-specific mortality rates were: 0-4, 5-9, 10-19, 20-29, 30-39, 40-49, 50-59, 60-69 and ≥ 70 years. Then, based on the values of crude mortality rates, we calculated the rate ratios (RR) and the respective 95%CI to determine the differences between the study groups (sex, age group, race/color and regions).
Trend analyses of mortality rates were performed using joinpoint regression models 1313. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335-51.. This analysis uses an algorithm which tests whether a multi-segmental line is significantly better than a straight line or a line with fewer segments. The analysis started with a minimum number of joinpoints (for example, 0 joinpoints, resulting in a straight line) and tested if one or more joinpoints (in our analysis up to 3 joinpoints) increased the significance when added to the model. Each joinpoint indicates a statistically significant change in the slope. Statistical significance was tested using the Monte Carlo permutation test, which chooses the best segment for each model. The annual percent change (APC) and 95%CI was calculated for each segment. To simplify trend comparison for the indicators with more than one slope, we also calculated the average annual percent change (AAPC) over the entire period. The AAPC was estimated as the geometric-weighted mean of the APC, with weights equal to the length of each time interval segment. Trends were considered statistically significant when APC and AAPC presented a p-value < 0.05 1313. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335-51..
Data analysis was performed using the Stata software package, version 11.2 (StataCorp LP, College Station, USA). Joinpoint regression analysis was performed using the Regression Joinpoint Program version 4.0.4 (US National Cancer Institute, Bethesda, USA). We created thematic maps of spatial distribution of mortality rates by state of residence using ArcGIS software version 9.3 (Environmental Systems Research Institute, Redlands, USA).
Ethical aspects
SIM and IBGE databases are available in a public domain and do not allow identification of individuals. This study was approved by the Ethical Review Board of the Federal University of Ceará, Fortaleza, Ceará State, Brazil, under protocol number 699,138/2014.
Results
In the period from 2000 to 2011, a total of 12,491,280 deaths were recorded in Brazil, with 92,144 (0.74%) TB-related deaths and 144,175 (1.2%) HIV/AIDS-related deaths. We identified a total of 19,815 deaths in which TB and HIV/AIDS were mentioned on the same death certificates (21.5% of deaths by TB and 13.7% of deaths by HIV/AIDS). HIV/AIDS was mentioned as underlying cause in 98.6% (19,541/19,815) of these deaths, and TB in 0.03% (6/19,815). The average annual crude and age-adjusted mortality rate was 0.89 deaths/100,000 inhabitants and 0.97 deaths/100,000 inhabitants, respectively.
Epidemiological characteristics
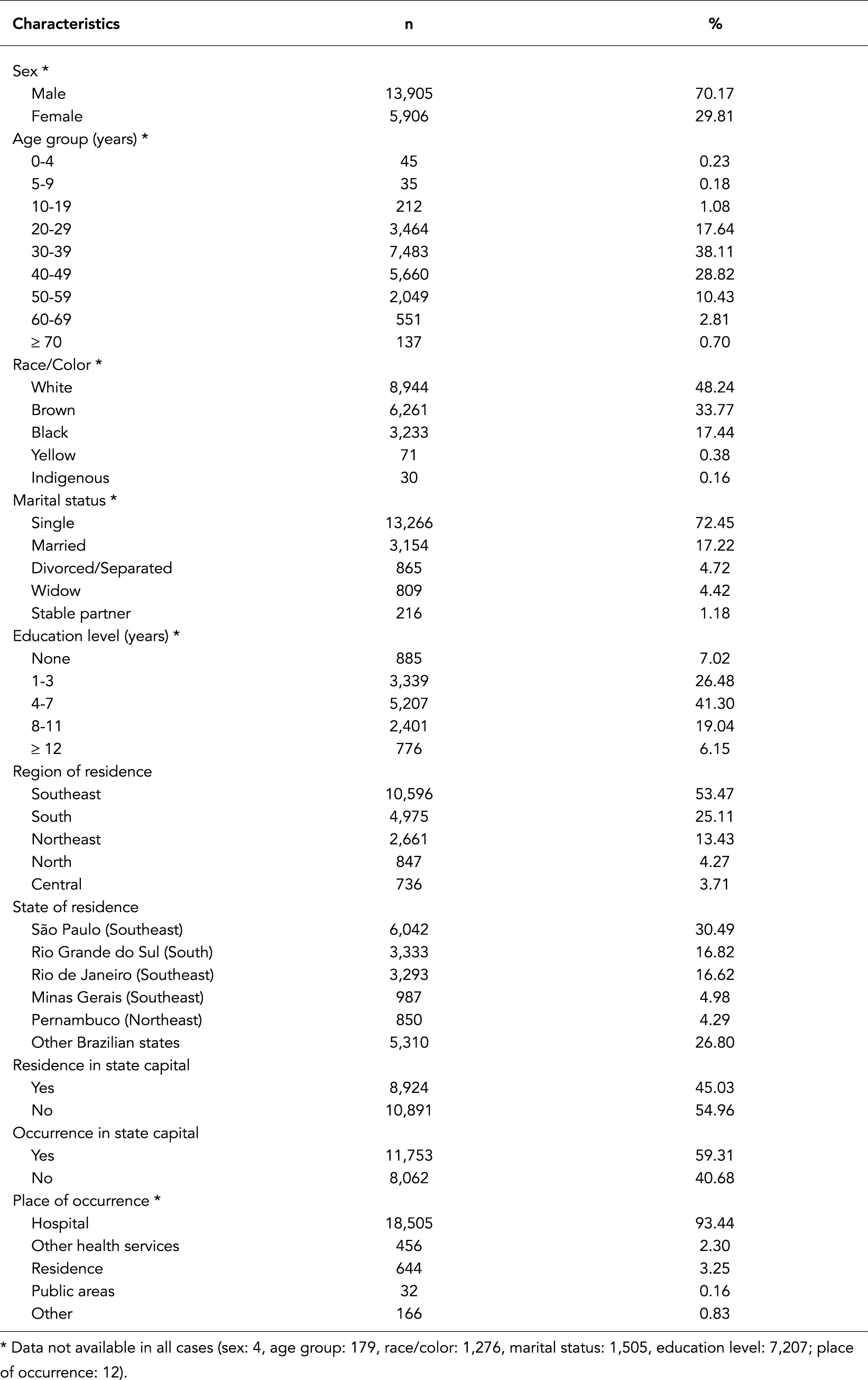
The predominating socio-demographic characteristics were: male sex (70.2%), white race/color (48.2%), single marital status (72.4%), age 30-39 years (38.1%, mean: 38.9; SD ± 10.5; median: 38.1), and residence in the Southeast region (53.5%) (Table 1). São Paulo State (Southeast region) presented about one third of all deaths related to co-infection (30.5%) (Table 1). Although about half did not reside in state capitals (54.9%), the place of occurrence of deaths was almost exclusively in urban hospitals (93.4%) and in the Brazilian state capitals (59.3%) (Table 1).
Epidemiological characteristics of deaths related to TB-HIV/AIDS co-infection in Brazil, 2000-2011 (n = 19,815).
The age-adjusted mortality rates were higher among males than females (1.37 vs. 0.55 deaths/100,000 inhabitants, respectively), with a RR of 2.43 (95%CI: 2.18; 2.70) (Table 2). The mortality rates was higher in the age groups 30-39 and 40-49 years. The black population had a 2.6-fold greater risk as compared to the white population, while brown race/color showed lower mortality rates compared to white race/color (Table 2). The South and Southeast regions showed the highest mortality rates (1.55 and 1.12 deaths/100,000 inhabitants, respectively), with significant differences when compared to the North region (Table 2). The highest average annual mortality rates by state of residence were observed in Rio Grande do Sul (South region) (2.55 deaths/100,000 inhabitants), followed by the states of Rio de Janeiro (1.77 deaths/100,000 inhabitants) and São Paulo (1.24 deaths/100,000 inhabitants), both in the Southeast region (Figure 1).
Average annual mortality rates related to TB-HIV/AIDS co-infection (per 100,000 inhabitants) stratified by sex, age group, race/color and region of residence. Brazil, 2000-2011.
Spatial distribution of average annual mortality rates related to TB-HIV/AIDS co-infection (per 100,000 inhabitants) by states of residence. Brazil, 2000-2011.
Temporal trends
We observed a significant decreasing trend of age-adjusted mortality rates at national level (AAPC: -1.7%; 95%CI: -2.4; -1.0), with considerable regional variations (Figure 2; Table 3). Mortality increased significantly in the North (AAPC: 5.7%; 95%CI: 2.2; 9.4), Northeast (AAPC: 5.4%; 95%CI: 3.3; 7.6), and Central (AAPC: 3.5%; 95%CI: 0.2; 6.9) regions. In contrast, we observed a decreasing trend in the Southeast region over the entire period (AAPC: -4.1%; 95%CI: -2.4; -1.0), with a decrease in the period 2000-2005 and a stabilization in the period 2005-2011. The South region presented a stable trend in the period (AAPC: -0.5%; 95%CI: -2.9; -1.9), with an increase from 2000 to 2004, and a decrease trend in the period 2004-2011 (Table 3).
The sex-specific mortality rate presented a significant decreasing trend for males and a stable trend for females (Table 3). For age-specific rmortality ates, we observed a significant decrease in the 20-29 year-old and 30-39 year-old age groups. The older age groups showed significant increasing trends of mortality rates: 50-59 year-olds, 60-69 year-olds and ≥ 70 year-olds. The mortality in pediatric and younger age groups, and in 40-49 year-olds remained stable during the study period (Table 3).
Trends of age-adjusted mortality rates related to TB-HIV/AIDS co-infection (per 100,000 inhabitants) in Brazil and regions, 2000-2011.
Joinpoint regression analysis of mortality rates related to TB-HIV/AIDS co-infection by region, sex and age group. Brazil, 2000-2011.
Discussion
In this nationwide population-based study, presented a comprehensive overview of magnitude and time trends of mortality related to TB-HIV/AIDS co-infection in Brazil over a 12-year period. Our data show a decreasing trend of mortality in Brazil, but with different patterns among regions, with increasing trends in the poorest regions of the country, such as the North and Northeast regions. There was a higher mortality burden among males, individuals of a working age, those of black race/color and residents in high HIV/AIDS-endemic states/regions 33. World Health Organization. Global tuberculosis control. Geneva: World Health Organization; 2011.), (44. Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.), (55. Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.), (1414. Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Millogo O, et al. HIV/AIDS-related mortality in Africa and Asia: evidence from INDEPTH health and demographic surveillance system sites. Glob Health Action 2014; 7:25370..
The South and Southeast regions (including the states of Rio Grande do Sul, São Paulo and Rio de Janeiro) had the highest mortality rates related to TB-HIV/AIDS co-infection 1515. Coelho L, Cardoso SW, Amancio RT, Moreira RI, Campos DP, Veloso VG, et al. Trends in AIDS-defining opportunistic illnesses incidence over 25 years in Rio de Janeiro, Brazil. PLoS One 2014; 9:e98666., but with a continuous decreasing trend in recent years. These results probably reflect the introduction and spread of the AIDS epidemic in the country. The state of São Paulo presented the first cases of the epidemic, followed by the state of Rio de Janeiro. These states significantly contributed to a rapid growth in the number of AIDS cases in the country 1616. Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40..
We emphasize that the North and Northeast regions, the poorest regions of the country, showed increasing mortality rates in the study period 1717. Parker R, Camargo Jr. KR. Pobreza e HIV/AIDS: aspectos antropológicos e sociológicos. Cad Saúde Pública 2000; 16:89-102.. Our results reinforce the ongoing change of transmission dynamics of HIV/AIDS infection, from socio-economically well-off population groups in urban centers, to more socio-economically deprived vulnerable populations in rural areas, with a consequent increased risk for concomitant TB infection. Our data confirm previous studies indicating tremendous social inequalities being a major risk for co-infection 1717. Parker R, Camargo Jr. KR. Pobreza e HIV/AIDS: aspectos antropológicos e sociológicos. Cad Saúde Pública 2000; 16:89-102.), (1818. Straetemans M, Bierrenbach AL, Nagelkerke N, Glaziou P, Werf MJ. The effect of tuberculosis on mortality in HIV positive people: a meta-analysis. PLoS One 2010; 5:e15241..
The distribution of mortality rates according to demographic characteristics portrays a continuous decreasing trend for males and working age populations (20-49 years) 1818. Straetemans M, Bierrenbach AL, Nagelkerke N, Glaziou P, Werf MJ. The effect of tuberculosis on mortality in HIV positive people: a meta-analysis. PLoS One 2010; 5:e15241.. This trend has been observed in infections caused by TB and HIV/AIDS and similarly overall infection rates can be linked to transmission dynamics, considering socio-economic, environmental and behavioral factors 1919. San Pedro A, Oliveira RM. Tuberculose e indicadores socioeconômicos: revisão sistemática da literatura. Rev Panam Salud Pública 2013; 33:294-301.. Our data also show a significant increase of mortality related to co-infection in the elderly. Two different patterns were identified: those infected < 60 years-old with better survival rates due to improved antiretroviral therapy (ART), including highly active antiretroviral therapy (HAART), and those infected > 60 years-old. The high vulnerability in these population groups increases the risk of developing both diseases as a result of higher previous exposure rates to Mycobacterium tuberculosis. Other factors in the elderly include the increased likelihood of atypical presentations of TB, comorbidity, resistance to condom use and delayed detection of HIV infection 2020. Bierrenbach AL, Gomes ABF, Noronha EF, Souza MFM. Tuberculosis incidence and cure rates, Brazil, 2000-2004. Rev Saúde Pública 2007; 41 Suppl 1:24-33.), (2121. Rezende MCM, Lima TJP, Rezende MHV. Aids na terceira idade: determinantes biopsicossociais. Estudos 2009; 36:235-53..
We have observed a decrease in deaths among children < 10 years. In fact, TB incidence has been reduced in this age group in recent decades 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.), (1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.. BCG vaccination coverage is also very high in Brazil (reaching 100% in recent years) resulting in enhanced protection against invasive forms of childhood TB 2020. Bierrenbach AL, Gomes ABF, Noronha EF, Souza MFM. Tuberculosis incidence and cure rates, Brazil, 2000-2004. Rev Saúde Pública 2007; 41 Suppl 1:24-33.. In addition, mother-to-child transmission of HIV has been reduced effectively in Brazil as a result of integrated control programs 1616. Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40.), (2222. Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.. There has been an increased access to prenatal care services and assisted birth in HIV-positive mothers, including antiretroviral medication in HIV infected pregnant women and exposed newborns 2222. Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.. There was estimated to occur a 78% reduction in mother-to-child transmission of HIV between 2001 and 2013 in Latin America and the Caribbean. Of the total of women who gave birth in 2013 (11 million), 87% had at least four prenatal consultations number (the recommended minimum), 74% had access to HIV testing and counseling, and 93% of HIV-positive pregnant women received HAART (34% increase compared to 2010) 2222. Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.), (2323. Pan American Health Organization. 2014 update: elimination of mother-to-child transmission of HIV and syphilis in the Americas. Washington DC: Pan American Health Organization; 2014.), (2424. Silva PF, Moura GS, Caldas AJM. Fatores associados ao abandono do tratamento da tuberculose pulmonar no Maranhão, Brasil, no período de 2001 a 2010. Cad Saúde Pública 2014; 30:1745-54..
Some strategies have favored an improvement in mortality indicators related to TB-HIV/AIDS co-infection. These strategies include: free dispensing of antiretroviral drugs for treatment of AIDS since 1996, continuous updating of clinical protocols and therapeutic guidelines for the management of HIV infection in adults (2014), children and adolescents (2014), and prophylaxis of vertical transmission of HIV and antiretroviral therapy in pregnant women (2010) 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).), (1616. Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40.), (2222. Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.), (2525. TB Diagnostics Market Analysis Consortium. Market assessment of tuberculosis diagnostics in Brazil in 2012. PLoS One 2014; 9:e104105.. In 2014, HIV infection was included in the Brazilian list of notifiable diseases, further aiming at improving disease control 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1)..
Our data show regional differences, which may reflect operational factors in the implementation of these measures. Mortality rates were higher in regions considered as more economically developed, with increasing trends in other regions, consistent with the AIDS expansion process in Brazil. The presence of variables considered indicators for poverty in Brazil and a higher risk among those with a low education and the black population, confirms the increased mortality in these regions 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.), (99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).), (1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.), (1515. Coelho L, Cardoso SW, Amancio RT, Moreira RI, Campos DP, Veloso VG, et al. Trends in AIDS-defining opportunistic illnesses incidence over 25 years in Rio de Janeiro, Brazil. PLoS One 2014; 9:e98666.), (1616. Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40.), (2626. Sanchez M, Bartholomay P, Arakaki-Sanchez D, Enarson D, Bissell K, Barreira D, et al. Outcomes of TB treatment by HIV status in national recording systems in Brazil, 2003-2008. PLoS One 2012; 7:e33129.), (2727. Teixeira TRA, Gracie R, Malta MS, Bastos FI. Social geography of AIDS in Brazil: identifying patterns of regional inequalities. Cad Saúde Pública 2014; 30:259-71..
Similar to other infectious diseases, poverty may have increased the vulnerability for TB and HIV/AIDS cases. There is a clear link between TB, poverty and social exclusion, hampering control efforts in many Brazilian regions 1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.), (2727. Teixeira TRA, Gracie R, Malta MS, Bastos FI. Social geography of AIDS in Brazil: identifying patterns of regional inequalities. Cad Saúde Pública 2014; 30:259-71.), (2828. Bastos FI, Szwarcwald CL. AIDS e pauperizac¸a~o: principais conceitos e evide^ncias empi´ricas. Cad Sau´de Pu´blica 2000; 16:65-76.. Those who are mostly affected live in poor, urban neighborhoods, with a trend to more and more rural areas 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).. HIV/AIDS is being spread within the poorest populations in the country, with negative impacts on clinical and epidemiological aspects 2222. Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.), (2727. Teixeira TRA, Gracie R, Malta MS, Bastos FI. Social geography of AIDS in Brazil: identifying patterns of regional inequalities. Cad Saúde Pública 2014; 30:259-71.. In cases with TB-HIV/AIDS co-infection, poverty has previously been shown to be related to higher mortality rates 1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.), (2626. Sanchez M, Bartholomay P, Arakaki-Sanchez D, Enarson D, Bissell K, Barreira D, et al. Outcomes of TB treatment by HIV status in national recording systems in Brazil, 2003-2008. PLoS One 2012; 7:e33129.), (2929. Neves LAS, Reis RK, Gir E. Adesão ao tratamento por indivíduos com a co-infecção HIV/tuberculose: revisão integrativa da literatura. Rev Esc Enferm USP 2010; 44:1135-41..
Reduced access to information, insufficient knowledge, and reduced access to health care may result in a delay of diagnosis, late treatment and low adherence to treatment 1818. Straetemans M, Bierrenbach AL, Nagelkerke N, Glaziou P, Werf MJ. The effect of tuberculosis on mortality in HIV positive people: a meta-analysis. PLoS One 2010; 5:e15241.), (2323. Pan American Health Organization. 2014 update: elimination of mother-to-child transmission of HIV and syphilis in the Americas. Washington DC: Pan American Health Organization; 2014.. The current challenge is to integrate TB and AIDS control programs effectively 1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.), (3030. Portal Brasil. Medicamento 3 em 1 para tratamento da Aids começa a ser distribuído em todo o país. http://www.brasil.gov.br/saude/2015/01/medicamento-3-em-1-para-a-aids-comeca-a-ser-distribuido-em-todo-o-pais (accessed on 02/Feb/2015).
http://www.brasil.gov.br/saude/2015/01/m...
. The contrast of the reduction of mortality in the South region and the increase of mortality rates in the North, Northeast and Central regions reflects socio-economic differences between these regions. Regional disparities and social determinants directly reflected in different patterns of the quality of health care and information systems 1010. Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.), (2828. Bastos FI, Szwarcwald CL. AIDS e pauperizac¸a~o: principais conceitos e evide^ncias empi´ricas. Cad Sau´de Pu´blica 2000; 16:65-76..
Our study is subject to limitations. The use of secondary data may have limited the analysis, as many variables of interest are not available with under registering of deaths. On the other hand, we assume that the databases are of acceptable quality, considering the improvement of coverage and quality of SIM records during recent years 99. Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).), (1616. Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40.), (3131. Oliveira GPI, Pinheiro RS, Coeli CM, Barreira D, Codenotti SB. Uso do sistema de informação sobre mortalidade para identificar subnotificação de casos de tuberculose no Brasil. Rev Bras Epidemiol 2012; 15:468-77.. However, there still may exist regional differences in the performance and quality of data, and the number of deaths related to TB-HIV/AIDS co-infections may have been underestimated 3131. Oliveira GPI, Pinheiro RS, Coeli CM, Barreira D, Codenotti SB. Uso do sistema de informação sobre mortalidade para identificar subnotificação de casos de tuberculose no Brasil. Rev Bras Epidemiol 2012; 15:468-77., especially in the North and Northeast regions. There were a considerable number of data sets with missing information, especially for race/color, education and marriage status, thus the respective analyses and interpretation should be performed with caution 3232. Rodrigues Jr. AL, Ruffino-Netto A, Castilho EA. Distribuição espacial da co-infecção M. tuberculosis/HIV no Estado de São Paulo, 1991-2001. Rev Saúde Pública 2006; 40:265-70.), (3333. Ferreira VMB, Portela MC, Vasconcelos MTL. Fatores associados à subnotificação de pacientes com Aids, no Rio de Janeiro, RJ, 1996. Rev Saúde Pública 2000; 34:170-7.), (3434. Martins-Melo FR, Lima MS, Ramos Jr. AN, Alencar CH, Heukelbach J. Mortality and case fatality due to visceral leishmaniasis in Brazil: a nationwide analysis of epidemiology, trends and spatial patterns. PLoS One 2014; 9:e93770.. Despite these limitations, the results of this study are highly representative, as all death certificates recorded in Brazil have been included, during a period of 12 years (2000-2011) 3434. Martins-Melo FR, Lima MS, Ramos Jr. AN, Alencar CH, Heukelbach J. Mortality and case fatality due to visceral leishmaniasis in Brazil: a nationwide analysis of epidemiology, trends and spatial patterns. PLoS One 2014; 9:e93770.), (3535. Martins-Melo FR, Lima MS, Ramos Jr. AN, Alencar CH, Heukelbach J. Epidemiological patterns of mortality due to visceral leishmaniasis and HIV/AIDS co-infection in Brazil, 2000-2011. Trans R Soc Trop Med Hyg 2014; 108:338-47..
In conclusion, our study shows a consistent decline of the mortality related to TB-HIV/AIDS co-infection in Brazil, despite the high levels still observed. Population groups at high risk have been identified, with consistent regional differences. The increasing mortality trend in the socio-economically most disadvantaged North, Northeast and Central regions is worrying. We recognize the need for implementation and monitoring the control actions for TB/HIV co-infection to reduce the morbidity and mortality burden in all Brazilian regions.
Acknowledgments
We thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes/Brazil) for granting a Masters Scholarship to M.S.L. J.H. is research fellow at the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq/Brazil).
References
-
1Gupta S, Granich R, Date A, Lepere P, Hersh B, Gouws E, et al. Review of policy and status of implementation of collaborative HIV-TB activities in 23 high-burden countries. Int J Tuberc Lung Dis 2014; 18:1149-58.
-
2Murray CJ, Ortblad KF, Guinovar C, Lim SS, Wolock TM, Allen Roberts D, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 13:1005-70.
-
3World Health Organization. Global tuberculosis control. Geneva: World Health Organization; 2011.
-
4Joint United Nations Programme on HIV/AIDS. Global Aids response progress reporting 2014: construction of core indicators for monitoring the 2011 United Nations Political declaration on HIV and Aids. Geneva: Joint United Nations Programme on HIV/AIDS; 2013.
-
5Joint United Nations Programme on HIV/AIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.
-
6Secretaria de Vigilância em Saúde, Ministério da Saúde. O controle da tuberculose no Brasil: avanços, inovações e desafios. Brasília: Ministério da Saúde; 2014.
-
7Morimoto AA, Bonametti AM, Morimoto HK, Matsuo T. Soroprevalência da infecção pelo vírus da imunodeficiência humana em pacientes com tuberculose, em Londrina, Paraná. J Bras Pneumol 2005; 31:325-31.
-
8Guimarães RM, Lobo AP, Siqueira EA, Borges TF, Melo SC. Tuberculosis, HIV, and poverty: temporal trends in Brazil, the Americas, and worldwide. J Bras Pneumol 2012; 38:511-7.
-
9Secretaria de Vigilância em Saúde, Ministério da Saúde. Boletim Epidemiológico HIV/AIDS 2014; ano III, (1).
-
10Oliveira GP, Torrens AW, Bartholomay P, Barreira D. Tuberculosis in Brazil: last ten years analysis - 2001-2010. Braz J Infect Dis 2013; 17:218-33.
-
11Ministério da Saúde; Conselho Federal de Medicina; Centro Brasileiro de Classificação de Doenças. A declaração de óbito: documento necessário e importante. 3a Ed. Brasília: Ministério da Saúde/Conselho Federal de Medicina/Centro Brasileiro de Classificação de Doenças; 2009.
-
12World Health Organization. National Statistic Classifications of Diseases and Related Health Problems (ICD): 10th revision. Version 2007. Geneva: World Health Organization; 2007.
-
13Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335-51.
-
14Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Millogo O, et al. HIV/AIDS-related mortality in Africa and Asia: evidence from INDEPTH health and demographic surveillance system sites. Glob Health Action 2014; 7:25370.
-
15Coelho L, Cardoso SW, Amancio RT, Moreira RI, Campos DP, Veloso VG, et al. Trends in AIDS-defining opportunistic illnesses incidence over 25 years in Rio de Janeiro, Brazil. PLoS One 2014; 9:e98666.
-
16Granjeiro A, Escuder MML, Castilho EA. Magnitude e tendência da epidemia de Aids em municípios brasileiros de 2002-2006. Rev Saúde Pública 2010; 44:430-40.
-
17Parker R, Camargo Jr. KR. Pobreza e HIV/AIDS: aspectos antropológicos e sociológicos. Cad Saúde Pública 2000; 16:89-102.
-
18Straetemans M, Bierrenbach AL, Nagelkerke N, Glaziou P, Werf MJ. The effect of tuberculosis on mortality in HIV positive people: a meta-analysis. PLoS One 2010; 5:e15241.
-
19San Pedro A, Oliveira RM. Tuberculose e indicadores socioeconômicos: revisão sistemática da literatura. Rev Panam Salud Pública 2013; 33:294-301.
-
20Bierrenbach AL, Gomes ABF, Noronha EF, Souza MFM. Tuberculosis incidence and cure rates, Brazil, 2000-2004. Rev Saúde Pública 2007; 41 Suppl 1:24-33.
-
21Rezende MCM, Lima TJP, Rezende MHV. Aids na terceira idade: determinantes biopsicossociais. Estudos 2009; 36:235-53.
-
22Ramos Jr. AN, Matida LH, Hearst N, Heukelbach J. AIDS in Brazilian children: history, surveillance, antiretroviral therapy, and epidemiologic transition, 1984-2008. AIDS Patient Care STDS 2011; 25:245-55.
-
23Pan American Health Organization. 2014 update: elimination of mother-to-child transmission of HIV and syphilis in the Americas. Washington DC: Pan American Health Organization; 2014.
-
24Silva PF, Moura GS, Caldas AJM. Fatores associados ao abandono do tratamento da tuberculose pulmonar no Maranhão, Brasil, no período de 2001 a 2010. Cad Saúde Pública 2014; 30:1745-54.
-
25TB Diagnostics Market Analysis Consortium. Market assessment of tuberculosis diagnostics in Brazil in 2012. PLoS One 2014; 9:e104105.
-
26Sanchez M, Bartholomay P, Arakaki-Sanchez D, Enarson D, Bissell K, Barreira D, et al. Outcomes of TB treatment by HIV status in national recording systems in Brazil, 2003-2008. PLoS One 2012; 7:e33129.
-
27Teixeira TRA, Gracie R, Malta MS, Bastos FI. Social geography of AIDS in Brazil: identifying patterns of regional inequalities. Cad Saúde Pública 2014; 30:259-71.
-
28Bastos FI, Szwarcwald CL. AIDS e pauperizac¸a~o: principais conceitos e evide^ncias empi´ricas. Cad Sau´de Pu´blica 2000; 16:65-76.
-
29Neves LAS, Reis RK, Gir E. Adesão ao tratamento por indivíduos com a co-infecção HIV/tuberculose: revisão integrativa da literatura. Rev Esc Enferm USP 2010; 44:1135-41.
-
30Portal Brasil. Medicamento 3 em 1 para tratamento da Aids começa a ser distribuído em todo o país. http://www.brasil.gov.br/saude/2015/01/medicamento-3-em-1-para-a-aids-comeca-a-ser-distribuido-em-todo-o-pais (accessed on 02/Feb/2015).
» http://www.brasil.gov.br/saude/2015/01/medicamento-3-em-1-para-a-aids-comeca-a-ser-distribuido-em-todo-o-pais -
31Oliveira GPI, Pinheiro RS, Coeli CM, Barreira D, Codenotti SB. Uso do sistema de informação sobre mortalidade para identificar subnotificação de casos de tuberculose no Brasil. Rev Bras Epidemiol 2012; 15:468-77.
-
32Rodrigues Jr. AL, Ruffino-Netto A, Castilho EA. Distribuição espacial da co-infecção M. tuberculosis/HIV no Estado de São Paulo, 1991-2001. Rev Saúde Pública 2006; 40:265-70.
-
33Ferreira VMB, Portela MC, Vasconcelos MTL. Fatores associados à subnotificação de pacientes com Aids, no Rio de Janeiro, RJ, 1996. Rev Saúde Pública 2000; 34:170-7.
-
34Martins-Melo FR, Lima MS, Ramos Jr. AN, Alencar CH, Heukelbach J. Mortality and case fatality due to visceral leishmaniasis in Brazil: a nationwide analysis of epidemiology, trends and spatial patterns. PLoS One 2014; 9:e93770.
-
35Martins-Melo FR, Lima MS, Ramos Jr. AN, Alencar CH, Heukelbach J. Epidemiological patterns of mortality due to visceral leishmaniasis and HIV/AIDS co-infection in Brazil, 2000-2011. Trans R Soc Trop Med Hyg 2014; 108:338-47.
Publication Dates
-
Publication in this collection
Oct 2016
History
-
Received
22 Feb 2015 -
Reviewed
10 Sept 2015 -
Accepted
20 Oct 2015