Introduction
On January 25th, at 12:28, the city of Brumadinho, Minas Gerais State, Brazil, with 39,520 inhabitants distributed across 639,434km2 and with a municipal Human Development Index (HDI) of 0.7046 11. Instituto Brasileiro de Geografia e Estatística. Panorama. https://cidades.ibge.gov.br/brasil/mg/brumadinho/panorama (acessado em 03/Mar/2019).
https://cidades.ibge.gov.br/brasil/mg/br...
, located in the southeast region of Brazil, was severely hit by the rupture of the Vale tailings dam, at the “Mina Córrego do Feijão”, directly reaching 703 people at the disaster site.
At the end of the first month, 395 people had been located and more than 300 had died. Of these, the bodies of more than 100 were not found or recognized, according to data from the Minas Gerais State Civil Defense 22. Defesa Civil Estadual de Minas Gerais. Informações: desastre barragem de rejeitos de Brumadinho. http://www.defesacivil.mg.gov.br/index.php/component/gmg/page/574-inform2808 (acessado em 03/Mar/2019).
http://www.defesacivil.mg.gov.br/index.p...
. Within seconds, the wave of mud and tailings reached the company’s administrative area, the Vila Ferteco community and the Nova Estância inn. At the time of the disaster, the municipality’s main economic pillar was mining 33. Instituto Brasileiro de Geografia e Estatística. Produto Interno Bruto dos municípios. https://cidades.ibge.gov.br/brasil/mg/brumadinho/pesquisa/38/46996 (acessado em 03/Mar/2019).
https://cidades.ibge.gov.br/brasil/mg/br...
, especially as a result of Vale S.A.’s activities.
Some of the mental health impact factors we identified over the course of this first month alongside the management, primary and secondary care teams of the Brazilian Unified National Health System (SUS) were: the magnitude of the disaster, the number of dead and missing, the destruction of houses and public spaces, as well as the direct or indirect exposure, experienced by the population and rescue teams, to water and dust contaminated by heavy metals, the destruction of the ecosystem, especially the contamination of the Paraopeba river, which made it impossible to use its water for human or animal consumption, irrigation, fishing, bathing, among other direct and indirect harms to those who benefited from using this water. We further highlight the social, political, cultural and economic impact of this disaster, since the city’s economy is related to mining.
According to the above-mentioned factors, we may consider that the psychosocial and mental health impact of this event has different implications for the population present in the municipality, including external humanitarian aid teams, volunteers and workers present during the first response phase 44. Abeldaño RA, Fernández R. Community mental health in disaster situations. A review of community-based models of approach. Ciênc Saúde Colet 2016; 21:431-42.. Within this perspective, this article seeks to provide a critical reflection based on the account of one of the author’s experiences, based on her participation in the articulation of the mental health and psychosocial care strategy alongside management and care teams at the federal, state and municipal levels who were responsible for the response in Brumadinho, as well as in the post-disaster psychosocial care and mental health training offered to workers in the SUS front lines.
In order to analyze this experience, we used (inter)national studies, technical reports, guides and protocols from humanitarian organizations specialized in disasters in order to understand the psychosocial and mental health impact of this event on the population present in Brumadinho, including external humanitarian aid teams, volunteers and workers present during the first response phase 44. Abeldaño RA, Fernández R. Community mental health in disaster situations. A review of community-based models of approach. Ciênc Saúde Colet 2016; 21:431-42..
Impact on the psychosocial care and mental health of the population and health workers
It is important that we understand the disaster based on the social, political and cultural context within which it took place. When we call the rupture of Vale’s tailings dam a “disaster”, we consider the physical, psychic, social, political, economic, cultural and other variables that may be implicated in the process of its emergence and maintenance.
Regarding psychosocial care and mental health specifically, disasters are understood as “(…) serious interruptions of a community’s normal functioning which lead to human/material/economic/environmental losses that exceed the capacity of the affected society to deal with the situation using their own resources. (…) [they] cause significant material destruction and social disorganization due to the destruction or alteration of functional networks” 55. Noal DS, Weintraub ACM, Vicente LN, Knoblock F. A atuação do psicólogo em situações de desastres: algumas considerações baseadas em experiências de intervenção. Entrelinhas 2013; XIII (62):4-5. (p. 4). They may further “(…) cause psycho-social disorders in the affected population; often, these are more severe than the physical damage and last over time if not well-managed” 66. Secretaria de Vigilância em Saúde, Ministério da Saúde. Plano Nacional de Preparação e Resposta às Emergências de Saúde Pública: guia de preparação e resposta aos desastres associados às inundações para a gestão municipal do Sistema Único de Saúde. Brasília: Ministério da Saúde; 2011. (p. 8).
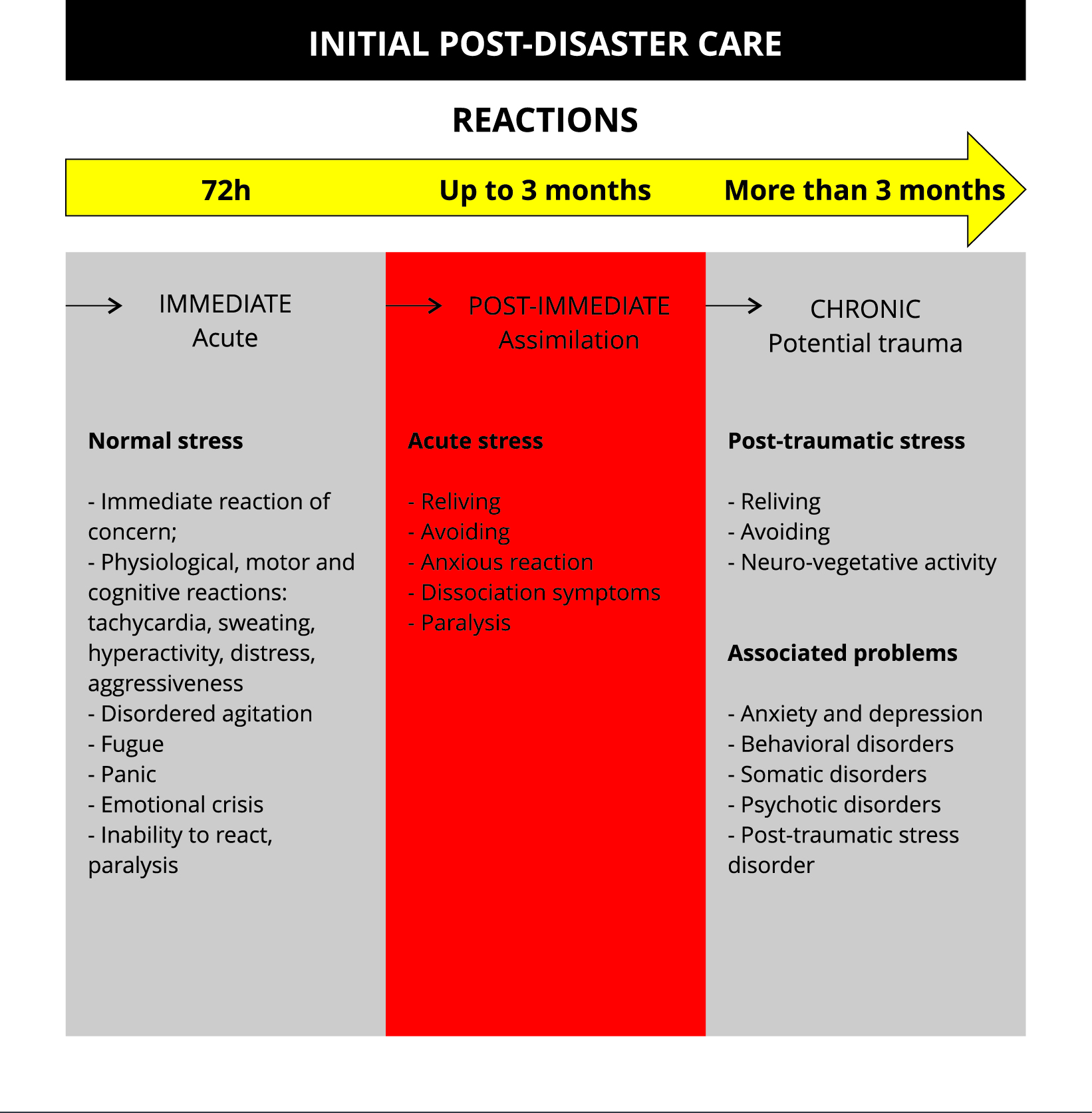
In large-scale disasters, the local population tends to impacted in different and underestimated ways 77. Inter-Agency Standing Committee. IASC Guidelines on mental health and psychosocial support in emergency settings. Geneva: Inter-Agency Standing Committee; 2007., since many reactions, symptoms and psychosocial and mental health consequences are intertwined with biological and cultural illness and reactions, requiring different kinds of support. With regard to immediate human reactions, the most common can be seen in the timeline presented in the Figure 1.
It is worth bearing in mind that these are immediate reactions, which begin at a disaster’s zero hour and last around 72 hours, and tend to be intense, abrupt, unpredictable and uncontrollable for those who experience or witness the disaster, and also cause intense feelings of fear, horror and impotence, characteristics which tend to destabilize mental health, disturbing the beliefs and values of the affected population, as well as their relationship to the environment where they live and their socio-affective relationships.
Particularly in the event we are analyzing, one of the aggravating factors for the mental health of those affected was the fact that most fatal victims worked for the mining company whose dam ruptured, confronting survivors with the loss of a large number of friends and coworkers and their source of employment and income. These characteristics are significant because they alter the community’s socio-affective relationships, creating a large potential for the development of psychopathological disorders in the medium and long term.
The impact generated by this type of event is directly related to factors such as resiliency and sociocultural characteristics of coping with suffering, psychic tools, socio-affective networks, as well as strategies and policies for psychosocial care and mental health care to be developed on the short, medium and long term 44. Abeldaño RA, Fernández R. Community mental health in disaster situations. A review of community-based models of approach. Ciênc Saúde Colet 2016; 21:431-42.,88. Cohen RE. Mental health services for victims of disasters. World Psychiatry 2002; 1:149-52..
During follow-up supervisions of workers, they reported that, after the first 72 hours and until the end of the first month, the most frequently expressed psychological reactions among the population who use the municipal SUS were: sadness, frequent crying, depressed mood, sorrow, anxiety, fear, irritability, anger, guilt, disorientation, dissociation reactions, anxiety crises, panic, emotional lability and suicide attempts, in most cases as a result of benzodiazepine use. There was also an increase in alcohol consumption, benzodiazepine use and in interpersonal conflicts and violence.
As for physical reactions, the following were listed as common: intense fatigue, loss of appetite, insomnia and unspecified pain. Based on this, a strategy was designed that contemplated the current demand, seeking to identify, mobilize and strengthen the abilities and capacities of those who were affected, the community and population enrolled in the territory.
Over time, it is estimated that most of the affected population will be able to re-establish themselves from the event’s psychosocial impact. However, even though most of the affected population will not develop psychopathological disorders in the medium and long term, the number of people who will demand specific psychosocial care and mental health help could reach the hundreds, which demands a health service provision and a specific strategy for following these cases that goes beyond routine situations.
On the other hand, with regard to the psychosocial and mental health impact on health workers who were involved with the first response phase, it is important to remember that most municipal health workers lost loved ones or had socio-affective relationships with people who experienced direct losses. Though mourning the expressive number of human, material and sociogeographical losses, the work process demanded from these workers a more extensive and stressful workload, with long, uninterrupted periods of work and prolonged lack of information regarding the slurry’s toxicity and its consequences.
Working in the first response phase led many professionals to be confronted with situations that exceeded their work routines, triggering in many reactions of acute stress, irritability, depressive mood, excessive involvement or unproductive behavior, or even leading them to manifest cognitive reactions such as difficulty concentrating and making decisions.
Prolonged exposure to disaster and intense stress situations, especially for non-emergency workers who had to perform this kind of work at the moment of the disaster, can lead to similar reaction as those displayed by individuals who were directly affected, such as: sadness, dysphoria, fatigue, difficulty concentrating, anxiety, guilt, anger and, in the medium and long term, even possible triggering traumatic processes 88. Cohen RE. Mental health services for victims of disasters. World Psychiatry 2002; 1:149-52..
The mental health and psychosocial care strategy in Brumadinho
The bases of the post-disaster mental health and psychosocial care strategy were the Sendai Framework 99. United Nations Office for Disaster Risk Reduction. Marco de Sendai para la Reducción del Riesgo de Desastres 2015-2030. https://www.unisdr.org/files/43291_spanishsendaiframeworkfordisasterri.pdf (acessado em 20/Out/18)
https://www.unisdr.org/files/43291_spani...
, the World Health Organization’s guides and protocols for disaster situations 1010. Organização Mundial da Saúde; War Trauma Foundation; Visão Global Internacional. Primeiros cuidados psicológicos: guia para trabalhadores de campo. Geneva: Organização Mundial da Saúde; 2015.,1111. World Health Organization; United Nations High Commissioner for Refugees. mhGAP Humanitarian Intervention Guide (mhGAP-HIG): clinical management of mental, neurological and substance use conditions in humanitarian emergencies. Geneva: World Health Organization; 2015., municipal, state and federal policies 1212. Ministério da Integração Nacional. Instrução Normativa nº 2, de 20 de dezembro de 2016. Estabelece procedimentos e critérios para a decretação de situação de emergência ou estado de calamidade pública pelos Municípios, Estados e pelo Distrito Federal, e para o reconhecimento federal das situações de anormalidade decretadas pelos entes federativos e dá outras providências. Diário Oficial da União 2016; 22 dez.,1313. Brasil. Lei nº 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União 1990; 20 set.,1414. Brasil. Lei nº 8.742, de 7 de dezembro de 1993. Dispõe sobre a organização da Assistência Social e dá outras providências. Diário Oficial da União 1993; 8 dez.,1515. Brasil. Lei nº 10.216, de 6 de abril de 2001. Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde mental. Diário Oficial da União 2001; 9 abr.,1616. Brasil. Lei nº 12.608, de 10 de abril de 2012. Institui a Política Nacional de Proteção e Defesa Civil - PNPDEC; dispõe sobre o Sistema Nacional de Proteção e Defesa Civil - SINPDEC e o Conselho Nacional de Proteção e Defesa Civil - CONPDEC; autoriza a criação de sistema de informações e monitoramento de desastres; altera as Leis nº 12.340, de 1º de dezembro de 2010, 10.257, de 10 de julho de 2001, 6.766, de 19 de dezembro de 1979, 8.239, de 4 de outubro de 1991, e 9.394, de 20 de dezembro de 1996; e dá outras providências. Diário Oficial da União 2012; 11 abr. and the Federal Board of Psychology’s guidelines 1717. Conselho Federal de Psicologia. Nota técnica sobre atuação da psicologia na gestão integral de riscos e de desastres, relacionada com a política de proteção e defesa civil. https://site.cfp.org.br/wp-content/uploads/2016/12/Nota-T%C3%A9cnica-Psicologia-Gestao-de-Riscos-Versao-para-pdf-13-12.pdf (acessado em 20/Set/2017).
https://site.cfp.org.br/wp-content/uploa...
for disaster interventions. The specificities of the affected population were also taken into consideration.
The target audience of this strategy was the SUS health teams, so that they would be made aware of how to formulate psychosocial and mental health strategies for the Brumadinho population and also so that professionals would be able to identify psychic suffering in the population to whom they provide direct care, as well as in their own team. Rescue workers, volunteers and workers who came into direct contact with the slurry were also trained.
Initially, all public health devices in the municipality were mapped, totaling: 14 Family Health Strategy (ESF, in Portuguese) units, with each including a physician, nurse, nursing technician and community health agents and some also including dentists and oral health technicians.
The municipality also had 22 ESF support points, two of which with teams composed of nurses, nursing technicians, community health agents, general practitioners and psychiatrists, on some weekdays, during the first stage of the disaster response (first 30 days). There were also two Family Health Care Nuclei (NASF, in Portuguese), composed of psychologists, speech therapists, physical educator, occupational therapist, physiotherapists, social workers and nutritionists.
A factor that facilitating the strategy’s design was the fact that, at the moment of the disaster, 100% of the municipality’s population was covered by the ESF, which helped to implement a quick psychosocial care and mental health strategy that was compatible with their demands.
The medium-complexity health devices, located mainly in the urban area, were: Polyclinic, Physiotherapy clinic, Psychosocial Care Center, Child Psychosocial Care Center, Psychosocial Care Center for Alcohol and other drugs, Integrative and Complementary Health Practices Group (NUPIC, in Portuguese), 24-hour Emergency Care Units and small-sized hospital (with 4 psychiatric beds).
After mapping the municipal SUS health devices, the goal was to guarantee that routine care not be interrupted and, at the same time, that emerging, post-disaster cases also receive care, through additional teams. When operationalizing this model, it was necessary to extend working hours, so that Primary Health Units could function on weekends.
It was further considered that, even in cases in which socio-affective networks remained intact, the community would benefit from psychosocial care and mental health support in order to access community, family and public health support tools and devices. Teams were encouraged to help with the mourning process and rites of passage, such as recognizing bodies, funerals and burials, collective reports on the most frequent psychic reactions, reports on health service working hours and locations, identification of possible sociocultural coping tools, as well as providing care based on traditional socio-affective networks of solidarity.
Recently-hired, temporarily-transferred and volunteer professionals from the fields of psychology and medicine were integrated into the original municipal SUS teams in order to meet the emergency demands of the population in the first response phase. Part of these professionals were hired by the municipality or by Vale or were temporarily transferred by the State Health Secretariat, based on the Ordinance no. 30, issued on 25 January 2019 1818. Ministério do Desenvolvimento Regional. Portaria nº 30, de 25 de janeiro de 2019. Reconhece calamidade pública no Município de Brumadinho/MG. Diário Oficial da União 2019; 26 jan..
After guaranteeing the inclusion of these additional teams in to the SUS health devices, while still in the first four weeks following the disaster, specific post-disaster Mental Health and Psychosocial Care training was provided, in an attempt to improve and standardize the care provided to the population dealing with acute suffering 1919. Nahar N, Blomstedt Y, Wu B, Kandarina I, Trisnantoro L, Kinsman J. Increasing the provision of mental health care for vulnerable, disaster-affected people in Bangladesh. BMC Public Health 2014, 14:708.. The focus of the training was on strengthening support networks with proposals to build community strategies for coping with psychological suffering 44. Abeldaño RA, Fernández R. Community mental health in disaster situations. A review of community-based models of approach. Ciênc Saúde Colet 2016; 21:431-42..
It is believed that team training and supervision activities, which are collective spaces for sharing experiences and analyzing activities, help to re-signify the post-disaster work process. The support offered by NUPIC in the SUS teams’ workplaces and the follow-up provided by the Worker Health Reference Center were also important. These care devices sought to construct health promotion and prevention actions, avoiding the medium and long-term chronification and pathologization of psychic suffering.
Final thoughts
The Brumadinho health teams and central management showed availability and pragmatism when implementing and training health teams in the initial response phase. In the intervention model that was adopted, the focus was the minimization on the mental health of those affected. Thus, the proposal prioritized immediate care to human suffering to the detriment of the technicist model of care. We also highlight the 100% coverage of the territory by ESF teams, the prior experience of some technicians who supported teams after the Samarco dam rupture in 2015, as well as the quick hiring of more professionals, some of whom were funded by lawsuits the compelled Vale to pay for the costs.
The development of this strategy model, in which additional teams that were added in the first response phase were allocated in the health devices of an already-existing system that was known to the affected population, made it easier to identify care entry points and mental health registration forms, in order to systematize and monitor data, seeking to provide better health care.
We can thus understand the ruptures experienced by a population that was already receiving routine care, as well as understand their coping tools, shortening the bonding process and intensifying a broadened care, given the previous knowledge regarding these users, and consequently reducing the impact on their mental health.
We emphasize that the care strategy, developed alongside SUS teams, can be maintained in the medium and long term and enables the strengthening of socio-affective support networks, as long as professionals pay attention to the different forms of suffering that can develop in subsequent months, for example: increased alcohol consumption and use of benzodiazepines, painkillers and anti-inflammatory medication. This increase indicates that new psycho-social support strategies must be designed so that psychic suffering is heard and not just silenced through medication.
Strengthening social bonds and empowering support networks are the basis of psycho-social support and, therefore, are intrinsically connected with the community being cared for. Important challenges are the dialogue between surveillance and health care systems, for both data collection and systematization, which can feedback into new care strategies.
SUS teams must also analyze cultural aspects when designing care strategies that go beyond knowing the territory and analyzing epidemiological data. Economic and political aspects permeate survivors’ experiences and must be considered when proposing strengthening the protagonism of those affected. This strategy reaffirms autonomy and the search for dignity, which are important mediators of psychic suffering.
Acknowledgments
We thank Doctors Without Borders, who enabled the presence of mental health teams in the first disaster response phase, and to the Brazilian National Unified Health System professionals from the federal, state and municipal levels who participated in the first response phase.
-
1Instituto Brasileiro de Geografia e Estatística. Panorama. https://cidades.ibge.gov.br/brasil/mg/brumadinho/panorama (acessado em 03/Mar/2019).
» https://cidades.ibge.gov.br/brasil/mg/brumadinho/panorama -
2Defesa Civil Estadual de Minas Gerais. Informações: desastre barragem de rejeitos de Brumadinho. http://www.defesacivil.mg.gov.br/index.php/component/gmg/page/574-inform2808 (acessado em 03/Mar/2019).
» http://www.defesacivil.mg.gov.br/index.php/component/gmg/page/574-inform2808 -
3Instituto Brasileiro de Geografia e Estatística. Produto Interno Bruto dos municípios. https://cidades.ibge.gov.br/brasil/mg/brumadinho/pesquisa/38/46996 (acessado em 03/Mar/2019).
» https://cidades.ibge.gov.br/brasil/mg/brumadinho/pesquisa/38/46996 -
4Abeldaño RA, Fernández R. Community mental health in disaster situations. A review of community-based models of approach. Ciênc Saúde Colet 2016; 21:431-42.
-
5Noal DS, Weintraub ACM, Vicente LN, Knoblock F. A atuação do psicólogo em situações de desastres: algumas considerações baseadas em experiências de intervenção. Entrelinhas 2013; XIII (62):4-5.
-
6Secretaria de Vigilância em Saúde, Ministério da Saúde. Plano Nacional de Preparação e Resposta às Emergências de Saúde Pública: guia de preparação e resposta aos desastres associados às inundações para a gestão municipal do Sistema Único de Saúde. Brasília: Ministério da Saúde; 2011.
-
7Inter-Agency Standing Committee. IASC Guidelines on mental health and psychosocial support in emergency settings. Geneva: Inter-Agency Standing Committee; 2007.
-
8Cohen RE. Mental health services for victims of disasters. World Psychiatry 2002; 1:149-52.
-
9United Nations Office for Disaster Risk Reduction. Marco de Sendai para la Reducción del Riesgo de Desastres 2015-2030. https://www.unisdr.org/files/43291_spanishsendaiframeworkfordisasterri.pdf (acessado em 20/Out/18)
» https://www.unisdr.org/files/43291_spanishsendaiframeworkfordisasterri.pdf -
10Organização Mundial da Saúde; War Trauma Foundation; Visão Global Internacional. Primeiros cuidados psicológicos: guia para trabalhadores de campo. Geneva: Organização Mundial da Saúde; 2015.
-
11World Health Organization; United Nations High Commissioner for Refugees. mhGAP Humanitarian Intervention Guide (mhGAP-HIG): clinical management of mental, neurological and substance use conditions in humanitarian emergencies. Geneva: World Health Organization; 2015.
-
12Ministério da Integração Nacional. Instrução Normativa nº 2, de 20 de dezembro de 2016. Estabelece procedimentos e critérios para a decretação de situação de emergência ou estado de calamidade pública pelos Municípios, Estados e pelo Distrito Federal, e para o reconhecimento federal das situações de anormalidade decretadas pelos entes federativos e dá outras providências. Diário Oficial da União 2016; 22 dez.
-
13Brasil. Lei nº 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União 1990; 20 set.
-
14Brasil. Lei nº 8.742, de 7 de dezembro de 1993. Dispõe sobre a organização da Assistência Social e dá outras providências. Diário Oficial da União 1993; 8 dez.
-
15Brasil. Lei nº 10.216, de 6 de abril de 2001. Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde mental. Diário Oficial da União 2001; 9 abr.
-
16Brasil. Lei nº 12.608, de 10 de abril de 2012. Institui a Política Nacional de Proteção e Defesa Civil - PNPDEC; dispõe sobre o Sistema Nacional de Proteção e Defesa Civil - SINPDEC e o Conselho Nacional de Proteção e Defesa Civil - CONPDEC; autoriza a criação de sistema de informações e monitoramento de desastres; altera as Leis nº 12.340, de 1º de dezembro de 2010, 10.257, de 10 de julho de 2001, 6.766, de 19 de dezembro de 1979, 8.239, de 4 de outubro de 1991, e 9.394, de 20 de dezembro de 1996; e dá outras providências. Diário Oficial da União 2012; 11 abr.
-
17Conselho Federal de Psicologia. Nota técnica sobre atuação da psicologia na gestão integral de riscos e de desastres, relacionada com a política de proteção e defesa civil. https://site.cfp.org.br/wp-content/uploads/2016/12/Nota-T%C3%A9cnica-Psicologia-Gestao-de-Riscos-Versao-para-pdf-13-12.pdf (acessado em 20/Set/2017).
» https://site.cfp.org.br/wp-content/uploads/2016/12/Nota-T%C3%A9cnica-Psicologia-Gestao-de-Riscos-Versao-para-pdf-13-12.pdf -
18Ministério do Desenvolvimento Regional. Portaria nº 30, de 25 de janeiro de 2019. Reconhece calamidade pública no Município de Brumadinho/MG. Diário Oficial da União 2019; 26 jan.
-
19Nahar N, Blomstedt Y, Wu B, Kandarina I, Trisnantoro L, Kinsman J. Increasing the provision of mental health care for vulnerable, disaster-affected people in Bangladesh. BMC Public Health 2014, 14:708.
-
20Médicos Sin Fronteras. Manual práctico de diseño e implementación de intervenciones en salud mental y psicosocial en desastres naturales. Barcelona: Médicos Sin Fronteras; 2009.
Publication Dates
-
Publication in this collection
20 May 2019 -
Date of issue
2019
History
-
Received
13 Mar 2019 -
Reviewed
25 Mar 2019 -
Accepted
26 Mar 2019



 Source: Médicos Sin Fronteras
Source: Médicos Sin Fronteras