Abstract:
This article aims to describe the preliminary results of two evaluations studies, one about the Stork Network program and the other about the Adequate Birth program, called Stork Network Assessment and Healthy Birth, and to identify possible improvements in comparison to the Birth in Brazil study. Both studies used a cross-sectional design and were conducted in 2017. The Stork Network Assessment study included all 606 public and mixed maternity hospitals from the Stork Network and a total of 10,675 postpartum women. The Healthy Birth study included a convenience sample of 12 private hospitals and 4,798 women. Indicators of labour and childbirth care were: presence of a companion person, care by obstetric nurse, use of partograph, use of non-pharmacological methods, walking during labor, eating, use of peripheral venous catheter, position for delivery, episiotomy, and Kristeller maneuver. The indicators were compared to those verified in Birth in Brazil, a nationwide population-based study in 2011-2012, before the start of the two intervention programs. Comparisons used the chi-square test for independent samples and 95% confidence interval. There was a significant increase in the number of women with access to appropriate technology for labour and childbirth from 2011 to 2017 and a reduction in harmful practices. The private sector also showed a decrease in cesarean rates and an increase in gestational age at birth. The study’s results show that properly conducted public policies can change the scenario of care for labor and childbirth, helping to reduce in negative maternal and neonatal outcomes.
Keywords:
Obstetric Delivery; Perinatal Care; Maternal Health; Health Policy; Evaluation Studies
Resumo:
Este artigo tem como objetivo descrever os primeiros resultados de dois estudos avaliativos, um sobre a Rede Cegonha e outro sobre o projeto Parto Adequado, denominados, respectivamente, de avaliação da Rede Cegonha e Nascer Saudável, e identificar possíveis melhorias em comparação ao estudo Nascer no Brasil. Ambos os estudos têm desenho seccional, realizados em 2017. O estudo avaliação da Rede Cegonha incluiu todas as 606 maternidades públicas e mistas envolvidas na Rede Cegonha e um total de 10.675 puérperas. O estudo Nascer Saudável incluiu uma amostra de conveniência de 12 hospitais da rede privada e um total de 4.798 mulheres. Os indicadores de atenção ao parto e nascimento avaliados foram: presença de acompanhante, atendimento por enfermeira obstétrica, preenchimento de partograma, uso de métodos não farmacológicos, deambulação, alimentação, uso de cateter venoso periférico, analgesia, posição da mulher para o parto, episiotomia e manobra de Kristeler. Esses indicadores foram comparados aos encontrados no Nascer no Brasil, estudo de base nacional realizado em 2011-2012, antes do início dos dois programas de intervenção. Para as comparações utilizamos o teste do qui-quadrado para amostras independentes e nível de 95% de confiança. Houve um aumento significativo do número de mulheres com acesso à tecnologia apropriada ao parto entre os anos de 2011 e 2017 e redução de práticas consideradas prejudiciais. No setor privado, observou-se também redução nas taxas de cesariana e aumento da idade gestacional ao nascer. Os resultados deste estudo mostram que políticas públicas bem conduzidas podem mudar o cenário da atenção ao parto e nascimento, promovendo a redução de desfechos maternos e neonatais negativos.
Palavras-chave:
Parto Obstétrico; Assistência Perinatal; Saúde Materna; Política de Saúde; Estudos de Avaliação
Resumen:
El objetivo de este artículo es describir los primeros resultados de dos estudios evaluativos, uno sobre la Red Cigüeña y otro sobre el proyecto Parto Adecuado, denominados respectivamente como evaluación de la Red Cigüeña y Nacer Sano, e identificar posibles mejorías en comparación con el estudio Nacer en Brasil. Ambos estudios tienen un diseño transversal, realizados en 2017. El estudio evaluación de la Red Cigüeña incluyó todas las maternidades públicas (606) y mixtas implicadas en la Red Cigüeña y a un total de 10.675 puérperas. El estudio Nacer Sano incluyó una muestra de conveniencia de 12 hospitales privados y a un total de 4.798 mujeres. Los indicadores de atención al parto y nacimiento evaluados fueron: presencia de acompañante, atención por enfermera obstetra, cumplimentación de partograma, uso de métodos no farmacológicos, deambulación, alimentación, uso de catéter venoso periférico, analgesia, posición de la mujer para el parto, episiotomía y maniobra de Kristeler. Estos indicadores se compararon con los encontrados en Nacer en Brasil, un estudio a nivel nacional, realizado en 2011-2012, antes del inicio de los dos programas de intervención. Para las comparaciones utilizamos el test del chi-cuadrado para muestras independientes y nivel de confianza de un 95%. Hubo un aumento significativo del número de mujeres con acceso a la tecnología apropiada para el parto entre los años de 2011 y 2017 y una reducción de las prácticas consideradas perjudiciales. En el sector privado, se observó también una reducción en las tasas de cesárea y aumento de la edad gestacional al nacer. Los resultados de este estudio muestran que las políticas públicas bien dirigidas pueden cambiar el escenario de la atención al parto y nacimiento, promoviendo la reducción de desenlaces maternos y neonatales negativos.
Palabras-clave:
Parto Obstétrico; Atención Perinatal; Salud Materna; Política de Salud; Estudios de Evaluación
Background
Brazil presents a model of labour and birth care that is characterized by the excessive use of obstetric and neonatal interventions 11. Moreira MEL, Gama SGN, Pereira APE, Silva AAM, Lansky S, Pinheiro RS, et al. Práticas de atenção hospitalar ao recém-nascido saudável no Brasil. Cad Saúde Pública 2014; 30 Suppl 1:S128-39.,22. Leal MC, Pereira APE, Domingues RMSM, Theme Filha MM, Dias MAB, Nakamura-Pereira M, et al. Intervenções obstétricas durante o trabalho de parto e parto em mulheres brasileiras de risco habitual. Cad Saúde Pública 2014; 30 Suppl 1:S17-47.. These interventions, either when used routinely or when they are not based on scientific evidence, are associated with unfavourable maternal and perinatal outcomes 33. Esteves-Pereira AP, Deneux-Tharaux C, Nakamura-Pereira M, Saucedo M, Bouvier-Colle MH, Leal MC. Caesarean delivery and postpartum maternal mortality: a population-based case control study in Brazil. PLoS One 2016; 11:e0153396.,44. Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016; 388:2176-92.,55. Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Domingues RMSM, Dias MAB, Moreira ME, et al. Burden of early-term birth on adverse infant outcomes: a population-based cohort study in Brazil. BMJ Open 2017; 7:e017789.,66. Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Domingues RM, Dias MA, et al. Provider-initiated late preterm births in brazil: differences between public and private health services. PLoS One 2016; 11:e0155511.,77. Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health 2016; 13 Suppl 3:115..
Initiatives to qualify this model, based on the appropriate use of technology, coupled to social mobilization, have sought to modify the situation. Two programs sought to improve the quality of labour and birth care: he Stork Network in the public sector, and Adequate Birth program in the private sector.
The Stork Network program (http://dab.saude.gov.br/portaldab/ape_redecegonha.php) was launched in 2011 by the Brazilian Ministry of Health, to address maternal mortality, obstetric violence and low quality of birth care in the public health sector. Actions were taken to increase and improve reproductive and prenatal planning, focusing on humanized care during pregnancy, childbirth and the puerperium period. This strategy promoted an increase in the offer of residency and specialization courses in field of woman and child’s health, especially for obstetric nursing. It also promoted the training of professionals to operate the Hospital Nucleuses and the Surveillance Committees of maternal, child and foetal deaths. More than 600 public (or Brazilian Unified National Health System - SUS-related) maternity hospitals were involved in this process.
Adequate Birth Program was launched in 2015 by the Brazilian National Regulatory for Private Health Insurance and Plans (ANS), through a technical cooperation agreement amongst ANS, the Institute for Healthcare Improvement (IHI) and the Israelita Albert Einstein Hospital (HIAE), with the support of the Brazilian Ministry of Health. Adequate Birth is a quality improvement project that offers institutional, scientific and methodological support to hospitals wanting to reorganize their labour and birth care models. Adequate Birth program strategies have a systemic approach, based on successful experiences of caesarean section reduction in the private sector 88. Torres JA, Domingues RMSM, Sandall J, Hartz Z, Gama SGN, Theme Filha MM, et al. Cesariana e resultados neonatais em hospitais privados no Brasil: estudo comparativo de dois diferentes modelos de atenção perinatal. Cad Saúde Pública 2014; 30 Suppl 1:S220-31.,99. Borem P, Ferreira JB, Silva UJ, Valerio Junior J, Orlanda CM. Increasing the percentage of vaginal birth in the private sector in Brazil through the redesign of care model. Rev Bras Ginecol Obstet 2015; 37:446-54.. They include four primary axes: governance, female empowerment, monitoring of indicators, and reorganization of structure and processes of care. In the first phase of Adequate Birth, 35 hospitals participated over 18 months. The initial results inspired the launch of the second phase, which began in May 2017 with the participation of 137 hospitals and 65 health insurance plans (Adequate Birth - http://www.ans.gov.br/gestao-em-saude/projeto-parto-adequado).
This article aims to describe the first results of two evaluative studies - one that addressed the Stork Network (Stork Network Assessment) and another that addressed the Adequate Birth program (Healthy Birth). It also seeks to identify possible improvements in indicators compared to the Birth in Brazil study, 2011-2012.
Methods
Stork Network Assessment and Healthy Birth are two independent evaluative studies. Both have a cross-sectional design, using mainly quantitative methods, and were carried out in 2017. Their results will be compared to Birth in Brazil, a national base study conducted in 2011-2012, before the start of the two intervention programs (Stork Network program and Adequate Birth).
Birth in Brazil is a national enquiry into labour and birth care that took place between February 2011 and October 2012. It collected a sample of 266 public, mixed and private hospitals and 23,894 puerperal women - 19.128 with public-funded births and 4,766 with private-funded births. In the first stage, hospitals with ≥ 500 births/year were stratified according to the five macroregions of the country (North, Northeast, South, Southeast and Central), location (capital or non-capital) and hospital service type (public, mixed or private). In the second stage, the number of days required to interview 90 puerperal women in each hospital - with a minimum of 7 days - was selected using a reverse sampling method. In the third stage, eligible women were selected on each day of data collection. Sample weights were established by determining the inverse of the probability of inclusion of each woman in the sample. A calibration procedure was used to ensure that the distribution of the sampled women was similar to that observed for the general population in the year 2011. Further details of the methodology used by the Birth in Brazil study are available in Leal et al. 1010. do Carmo Leal M, da Silva AA, Dias MA, da Gama SG, Rattner D, Moreira ME, et al. Birth in Brazil: national survey into labour and birth. Reprod Health 2012; 9:15. and Vasconcellos et al. 1111. Vasconcellos MT, Silva PL, Pereira AP, Schilithz AO, Souza Junior PR, Szwarcwald CL. Desenho da amostra Nascer no Brasil: Pesquisa Nacional sobre Parto e Nascimento. Cad Saúde Pública 2014; 30 Suppl 1:S49-58..
The Stork Network Assessment study is an evaluation of the degree of implementation of best labour and birth practices in public and mixed maternity hospitals involved in the Stork Network strategy in 2017. All maternity hospitals that met the following criteria were included: ≥ 500 births/year, regardless of the release of funding (581 maternities), or with < 500 births and the release of funding (25 maternities). The final selection included 606 maternity hospitals with national representativeness. A sample was stratified according to the five macroregions of the country. The sample size was based on a vaginal delivery rate of 50%, to detect differences of 5%, with a significance level of 5% and power of 80%. A minimum of 1,800 puerperal women were sampled in each macroregion. We established a fixed number of days of data collection in each macroregion, according to population size: 2 days in the South and Northeast region, four days in the North, 5 days in the South and 7 days in the Central. Using this strategy, the sample in each macroregion ranged from 1,800 to 2,500, with a total of 10,675 puerperal women in 606 maternity hospitals. This sampling plan created an over-representation of the North, South and Central macroregions, which was corrected by a calibration procedure.
Healthy Birth is a case study of the degree of implementation of the strategies proposed by Adequate Birth, and its effects on perinatal outcomes, especially on caesarean section rates. The data were collected from a convenience sample, composed of 12 of 35 hospitals that underwent Adequate Birth intervention since its inception in 2015. We selected these 12 hospitals based on the following criteria: regional representation (nine hospitals from the Southeast, two from the South and one from the Northeast), hospital type (weather it belongs or not to a health insurance plan provider) and Adequate Birth performance (reduction of caesarean section rates), according to information provided by the monitoring team 1212. Torres JA, Leal MDC, Domingues RMSM, Esteves-Pereira AP, Nakano AR, Gomes ML, et al. Evaluation of a quality improvement intervention for labour and birth care in Brazilian private hospitals: a protocol. Reprod Health 2018; 15:194.. Approximately 400 puerperal women were interviewed in each hospital, totalling 4,798 interviews. Data collection occurred simultaneously in all hospitals and was performed by trained nurses/obstetricians. As the number of puerperal women interviewed in each hospital was not proportional to its size, we applied a weighting factor.
We used the same criteria of inclusion for the 2 evaluative studies (Stork Network Assessment and Healthy Birth), as well as for the Birth in Brazil. It included women with single or twin pregnancies, who gave birth to a live new-born, regardless of weight or gestational age (GA). It also included women who gave birth to a stillborn with birth weight ≥ 500g and/or GA ≥ 22 gestational weeks. We excluded women with non-hospital birth, those with communication difficulties (severe mental disorder, foreigners who did not understand Portuguese and deaf/mute patients) and women who legally interrupted pregnancy.
In all three studies, we interviewed the women face-to-face during hospitalization. We collected clinical data from medical records and prenatal cards. Electronic forms were specifically developed for each study, which we used for both interviewing and for data extracting from the hospital records.
In the data analyses, we compared Stork Network Assessment women to those of Birth in Brazil study who gave birth in the public sector (labelled as BB-public), while women from Healthy Birth study were compared to those of Birth in Brazil study who gave birth in the private sector (labelled as BB-private). In Birth in Brazil, women who gave birth in public or mixed hospitals (not covered by a health insurance plan) were considered to have had a “public payment of birth”. Women whose births were covered by private health insurance plans and those who gave birth in private establishments (regardless of whether or not they were covered by a health insurance plan) were considered to have had a “private payment of birth”.
As sociodemographic and obstetric characteristics, we included the woman’s age, skin colour, years of schooling, parity and previous caesarean section. To assess the management of labour, we included the presence of a companion, labour assisted by a nurse/obstetric nurse, partograph in the medical record, use of non-pharmacological methods for pain relief, freedom of movement, eating, and usage of peripheral venous catheter. To evaluate the management of vaginal delivery, we included the presence of a companion, birth assisted by nurse/obstetric nurse, analgesia usage, woman’s position at birth, episiotomy, and fundal pressure (Kristeller maneuver).
We performed the same comparisons with the subjects being selected according to the macroregions of the country, for Stork Network Assessment and BB-public women only. This was not possible for the private sector because Healthy Birth study did not include hospitals in all five macroregions.
Finally, we compared the overall distribution of GA and the distribution of GA according to mode of birth for the four groups of women analysed: BB-public, Stork Network Assessment, BB-private and Healthy Birth.
All comparisons were performed using the chi-square test for independent samples, with a 95% confidence level using the statistical software SPSS version 22.0 (https://www.ibm.com/).
The Birth in Brazil, Stork Network Assessment and Healthy Birth studies are guided by Resolution n. 196/1996, issued by the Brazilian National Health Council, in which the parameters for human research were established. We also comply with Resolution n. 466/2012, issued by the Brazilian National Ethics Research Committee, an institution that acts under the Brazilian Ministry of Health supervision and regulates the Guidelines and Norms of Research in Human Beings. The present study sought to safeguard the ethical principles of autonomy, justice, beneficence and non-maleficence, as defined in the CEP/ENSP n. 92/10, CEP/UFMA and CEP/ENSP n. 01/2017 research protocols. Care was taken to ensure the privacy and confidentiality of data. All hospital directors and postpartum women underwent a prior consent visit and subsequently signed an informed consent form.
Results
In both 2017 studies (Stork Network Assessment and Healthy Birth), we observed a higher proportion of women of ≥35 years of age, with a higher level of schooling, who declared themselves black (in the Stork Network Assessment and Healthy Birth) and white (in Healthy Birth) and that were primiparous, when compared to the two groups of women from Birth in Brazil study (Table 1).
There was a reduction in the rates of antepartum caesarean section, which resulted in an increase in intrapartum caesarean section, with a 50% increase in the public sector (from 8.9% to 13.6%) and a 136% increase in the private sector (5.5% to 13%). In the private sector, there was also an 85% increase in the vaginal delivery rate (from 12.3% to 22.8%) (Table 2).
Best practices in labour care such as the presence of a companion, partograph in medical record, use of non-pharmacological methods for pain relief, the possibility of movement and feeding during labour were significantly higher in the 2017 studies. In the private sector, the increase in partograph usage and the possibility of movement and feeding during labour were higher than in the public sector. In the latter, we noted an increase in the presence of a companion and in the use of non-pharmacological methods to relieve pain during labour (Table 2).
The presence of a companion during vaginal delivery increased by 164% in the public service (31.8% to 83.9%) and 73% (55.8% to 96.8%) in the private service, although the public sector still presented 12.5% less than the private sector (83.9% and 96.8%, respectively). For both sectors, rates of intervention not routinely recommended during vaginal delivery, such as position in lithotomy, episiotomy and fundal pressure were between 20% and 50% lower in the 2017 studies (Table 2).
There was a 30% increase in labour attendance by nurses in the private sector (from 70.2% to 97.9%) and 65% in the public sector (from 46.4% to 84.7%). However, obstetric nursing was practically non-existent during vaginal delivery care in the private sector (1.8% in 2017).
In the comparison of macroregions, we observed an increase in intrapartum caesarean, mainly in the Southeast region (from 7% in BB-public to 13% in Stork Network Assessment).
Regarding best practices in labour care, there was an improvement in all practices and in all regions, with emphasis on the use of non-pharmacological methods for pain relief and feeding during labour for the North and Northeast regions, which rose from 20% in the BB-public to approximately 50% of the women in the Stork Network Assessment (Table 3).
The use of analgesia during vaginal delivery, although still low, showed a significant increase in the North and Northeast regions, from approximately 2% in the BB-public to 10% in the Stork Network Assessment. In other regions, the increase was lower, but reached a higher proportion of women - approximately 20% in the Stork Network Assessment study. The South region had the lowest rate of women with vaginal delivery submitted to fundal pressure, at approximately 12.8% (Table 3).
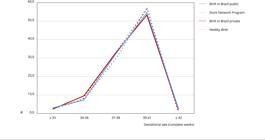
The distribution of GA at birth was very similar in the four groups of women (BB-public, Stork Network Assessment, BB-private and Healthy Birth) with vaginal delivery (Figure 1). Amongst women submitted to caesarean section, GA differed mainly in the private sector, with the Healthy Birth curve shifted to the right compared to the curve observed in the BB-private study, due to the higher proportion of births between 39 and 41 gestational weeks (Figure 2).
Gestational age distribution (complete weeks) of vaginal births: comparison of Birth in Brazil, Stork Network Assessment and Healthy Birth studies.
Gestational age distribution (complete weeks) of caesarean section births: comparison of Birth in Brazil, Stork Network Assessment and Healthy Birth studies.
Discussion
Results from Birth in Brazil, Stork Network Assessment and Healthy Birth highlight a significant increase in access to appropriate technology for labour and birth care in Brazil between the years 2011 and 2017. We observed an increase in the use of beneficial practices and a reduction of practices that are considered harmful. In the private sector, there was also a reduction in caesarean section rates and an increase in GA at birth. Even though during this period there was a change in the women’s profile, with appatent increases in both maternal age and schooling, it is not likely this study’s positive results are due to this change. On the contrary, greater age and higher level of schooling have been associated with higher caesarean section rates in the country 1313. Rebelo F, Rocha CM, Cortes TR, Dutra CL, Kac G. High cesarean prevalence in a national population-based study in Brazil: the role of private practice. Acta Obstet Gynecol Scand 2010; 89:903-8..
and may have attenuated the effect of strategies implemented to reduce caesarean section, especially in the private sector.
Birth in Brazil showed that the main reason women argue to justify their preference for caesarean section in the country is for fear of pain 1414. Domingues RMSM, Dias MAB, Nakamura-Pereira M, Torres JA, Pereira APE, Schilithz AOC, et al. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de parto final. Cad Saúde Pública 2014; 30 Suppl 1:S101-16.. It also showed that the current model of labour and birth care barely uses technologies that favour the physiological progression of labour and excessively uses interventions that cause pain and suffering 22. Leal MC, Pereira APE, Domingues RMSM, Theme Filha MM, Dias MAB, Nakamura-Pereira M, et al. Intervenções obstétricas durante o trabalho de parto e parto em mulheres brasileiras de risco habitual. Cad Saúde Pública 2014; 30 Suppl 1:S17-47.. Therefore, one of the premises for the reduction of caesarean rates in Brazil is the improvement of labour and vaginal birth care, seeking the promotion of female autonomy, empowerment and well-being. In this sense, the reduction of unnecessary interventions, such as episiotomy, fundal pressure and lithotomy position and the appropriate use of beneficial practices, such as the presence of a companion, obstetric nurse assistance, the freedom of movement and the provision of non-pharmacological and pharmacological methods for pain relief constitute improvements to the care model.
Analyses of women from the public sector according to geographical region showed that improvements in the process of attention to labour and birth occurred in all macroregions of the country. Similar increases in the frequencies of recommended obstetric practices were observed, even though these started from different prevalence points. The same was observed with the reduction of non-recommended practices in care routine, proving that interventions had different effects in different regional contexts.
Whilst we have seen many advances, improvements are still needed both in the public and private sectors. The presence of a companion during labour, birth and postpartum is a right granted by law since 2005 in Brazil 1515. Brasil. Lei nº 11.108, de 7 de abril de 2005. Altera a Lei nº 8.080, de 19 de setembro de 1990, para garantir às parturientes o direito à presença de acompanhante durante o trabalho de parto, parto e pós-parto imediato, no âmbito do Sistema Único de Saúde (SUS). Brasília: Diário Oficial da União 2005; 8 abr.. There was a significant increase in the presence of a companion during the period; yet at least 15% of women giving birth in a public sector hospital still experience those moments alone, away from people of their choice who could offer emotional support 1616. Lunda P, Minnie CS, Benade P. Women’s experiences of continuous support during childbirth: a meta-synthesis. BMC Pregnancy Childbirth 2018; 18:167.. In addition to the benefits of labour and birth for perinatal outcomes, such as shorter duration of labour, lower proportion of caesarean section and lower use of analgesics 1717. Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev 2011; (2):CD003766., accompanied women reported less violence during childbirth 1818. d’Orsi E, Bruggemann OM, Diniz CSG, Aguiar JM, Gusman CR, Torres JA, et al. Desigualdades sociais e satisfação das mulheres com o atendimento ao parto no Brasil: estudo nacional de base hospitalar. Cad Saúde Pública 2014; 30 Suppl 1:S154-68. and showed a greater degree of satisfaction with the care given 1818. d’Orsi E, Bruggemann OM, Diniz CSG, Aguiar JM, Gusman CR, Torres JA, et al. Desigualdades sociais e satisfação das mulheres com o atendimento ao parto no Brasil: estudo nacional de base hospitalar. Cad Saúde Pública 2014; 30 Suppl 1:S154-68.,1919. Diniz CS, d’Orsi E, Domingues RMSM, Torres JA, Dias MAB, Schneck CA, et al. Implementação da presença de acompanhantes durante a internação para o parto: dados da pesquisa nacional Nascer no Brasil. Cad Saúde Pública 2014; 30 Suppl 1:S140-53..
Only half of the women served in the public sector had access to low-cost and beneficial practices, such as the possibility of ambulation, food consumption and the use of non-pharmacological methods, all of which are recommended in the World Health Organization’s (WHO) most recent intrapartum care manual 2020. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018.. Access to non-pharmacological treatment was even lower in the private sector, reported by only a third of women. The private sector showed a greater use of pharmacological analgesia.
On the other hand, in both sectors, more than half of the interviewees used a venous catheter, often an unnecessary and uncomfortable intervention that entails additional costs to the system. The lithotomy position still predominates in childbirth care, while the WHO recommends that women should be given the freedom to choose the best birth position, including vertical ones. Although the usage of episiotomy declined in the period, it is still performed in almost 40% of women in the private sector and in almost a third of women in the public sector. The liberal or routine use of episiotomy is not recommended for women with spontaneous vaginal birth. Moreover, there is no definition of an acceptable rate, since the available evidence does not support episiotomy in routine care 2121. Francke AL, Smit MC, Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 2008; 8 :38.. Therefore, the recommendation is not to perform episiotomy routinely. Nonetheless, this still seems to happen for a significant number of Brazilian women. Finally, the use of the fundal pressure - manual pressure in the uterus fundus during the expulsion period - is not recommended under any circumstances. Even so, it was reported by a sixth of women in both sectors.
The low adoption of clinical protocols is reported worldwide. It may be associated with the characteristics of the clinical protocol itself, of the health professional, of the patient or of the external environment 2121. Francke AL, Smit MC, Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 2008; 8 :38.. Equally, it can be attributed to the existence of incentives and regulatory mechanisms 2222. Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ 1997; 157:408-16.. Therefore, it is necessary to develop a further understanding of the existing barriers to the implementation of these protocols, aiming at expanding the access of Brazilian women to good care.
The presence of nursing care in childbirth is another bottleneck in the implementation of the new model of care. A large number of studies show that the presence of nursing care in childbirth is associated with better results in labour and birth; reduces unnecessary interventions, including caesarean section; increases satisfaction; and generates improved perinatal outcomes 2323. Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016; 4:CD004667.,2424. ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet 2014; 384:1226-35.,2525. Horton R, Astudillo O. The power of midwifery. Lancet 2014; 384:1075-6.. Moreover, in Brazil, studies 2626. Gama SGN, Viellas EF, Torres JA, Bastos MH, Brüggewrmann OM, Theme Filha MM, et al. Labor and birth care by nurse with midwifery skills in Brazil. Reprod Health 2016; 13 Suppl 3:123,2727. Vogt SE, Silva KS, Dias MA. Comparison of childbirth care models in public hospitals, Brazil. Rev Saúde Pública 2014; 48:304-13. have shown that women who were treated by nurses during labour and birth had greater access to “good care”, as recommended by WHO 2020. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018. and the Brazilian Ministry of Health 2828. Departamento de Gestão e Incorporação de Tecnologias em Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Ministério da Saúde. Diretrizes nacionais de assistência ao parto normal: versão resumida (recurso eletrônico). Brasília: Ministério da Saúde; 2017., than when they were treated according to the traditional model (without the presence of a nurse). The study by Gama et al. 2626. Gama SGN, Viellas EF, Torres JA, Bastos MH, Brüggewrmann OM, Theme Filha MM, et al. Labor and birth care by nurse with midwifery skills in Brazil. Reprod Health 2016; 13 Suppl 3:123 also demonstrated a positive impact of the nursing presence among the members of the care team on the reduction of caesarean section in Brazil. Despite these favourable results, nursing participation in childbirth care was still small. Even with an impressive increase in the presence of obstetric nursing in the public sector, its presence was registered in only 27% of vaginal deliveries performed in the public sector. The practice is almost non-existent in the private sector.
Of the best practices currently recommended by WHO 2020. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018., the one that presented the lowest cost was epidural analgesia. While its use doubled in the public sector during the 2011-2017 period, it was made available to only 16% of the puerperal women, reaching half the women cared for in the private sector. It is widely acknowledged that the greatest fear of women in childbirth is the fear of pain 1414. Domingues RMSM, Dias MAB, Nakamura-Pereira M, Torres JA, Pereira APE, Schilithz AOC, et al. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de parto final. Cad Saúde Pública 2014; 30 Suppl 1:S101-16., which has resulted in an increase in the number of elective caesarean section. The availability of epidural analgesia may be another factor encouraging vaginal birth, allowing women to go into labour and request analgesia if they deem it necessary. France is an example of a country that has maintained low caesarean rates, close to 20%, with the high use of pharmacological analgesia, especially epidural analgesia. In 2016, 81.4% of the women received epidural analgesia during labour, while only 17.3% did not receive any type of analgesia 2929. Blondel B, Coulm B, Bonnet C, Goffinet F, Le Ray C; National Coordination Group of the National Perinatal Surveys. Trends in perinatal health in metropolitan France from 1995 to 2016: results from the French National Perinatal Surveys. J Gynecol Obstet Hum Reprod 2017; 46:701-13.. The most recent Cochrane review on the subject, published in 2018, does not indicate an increase in the risk of caesarean section or risk for the new-born with the use of epidural analgesia. Conversely, several (now dated) studies indicate an association between caesarean section and greater use of operative vaginal birth (forceps and vacuum extractor) 3030. Anim Somuah M, Smyth RMD, Cyna AM, Cuthbert A. Epidural versus non‐epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 2018; 5:CD000331.
Regarding outcome indicators, we observed a reduction in caesarean section (intrapartum and antepartum combined) in the private sector, while in the public sector this reduction did not occur. In fact, there was a replacement of antepartum caesarean section by intrapartum caesarean section, with a stable rate of vaginal births in the public sector. It is important to note that the percentage of caesarean section in the private sector is almost twice that of the public sector. Therefore, interventions aimed at reducing caesarean section are likely to be more easily achieved in the private sector. In both sectors, the increase in intrapartum caesarean section to the detriment of the antepartum denotes a change in care practice, with a higher proportion of women entering the active phase of labour, whether spontaneously or by labour induction.
An important beneficial outcome observed in the private sector was the increase in births of infants with GA ≥ 39 weeks. This was probably due to the reduction of antepartum caesarean section and the increase in vaginal deliveries. In a national study, Barros et al. 3131. Barros FC, Rabello Neto DL, Villar J, Kennedy SH, Silveira MF, Diaz-Rossello JL, et al. Caesarean sections and the prevalence of preterm and early-term births in Brazil: secondary analyses of national birth registration. BMJ Open 2018; 8:e021538. analysed data from the Brazilian Information System on Live Birth (SINASC). They found an association between type of birth and GA at birth: the higher the caesarean rate in Brazilian municipalities the higher the proportion babies born with GA between 37 and 38 weeks (early-term births) 3131. Barros FC, Rabello Neto DL, Villar J, Kennedy SH, Silveira MF, Diaz-Rossello JL, et al. Caesarean sections and the prevalence of preterm and early-term births in Brazil: secondary analyses of national birth registration. BMJ Open 2018; 8:e021538.. In Brazil, in 2011-12, early-term births made up 35% of total births. It is estimated that 300,000 preterm new-borns are born per year in the country via antepartum caesarean in women who present no sign of medical complication 55. Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Domingues RMSM, Dias MAB, Moreira ME, et al. Burden of early-term birth on adverse infant outcomes: a population-based cohort study in Brazil. BMJ Open 2017; 7:e017789.. Early-term new-borns are at increased risk of respiratory diseases 3232. Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ 2008; 336:85-7.,3333. Engle WA, Kominiarek MA. Late preterm infants, early term infants, and timing of elective deliveries. Clin Perinatol 2008; 35:325-41.,3434. Brown HK, Speechley KN, Macnab J, Natale R, Campbell MK. Neonatal morbidity associated with late preterm and early term birth: the roles of gestational age and biological determinants of preterm birth. Int J Epidemiol 2014; 43:802-14.,3535. Prefumo F, Ferrazzi E, Di Tommaso M, Severi FM, Locatelli A, Chirico G, et al. Neonatal morbidity after cesarean section before labor at 34(+0) to 38(+6) weeks: a cohort study. J Matern Fetal Neonatal Med 2016; 29:1334-8.,3636. Sengupta S, Carrion V, Shelton J, Wynn RJ, Ryan RM, Singhal K, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr 2013; 167:1053-9., neonatal intensive care unit admission 3434. Brown HK, Speechley KN, Macnab J, Natale R, Campbell MK. Neonatal morbidity associated with late preterm and early term birth: the roles of gestational age and biological determinants of preterm birth. Int J Epidemiol 2014; 43:802-14.,3636. Sengupta S, Carrion V, Shelton J, Wynn RJ, Ryan RM, Singhal K, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr 2013; 167:1053-9.,3737. Clark SL, Frye DR, Meyers JA, Belfort MA, Dildy GA, Kofford S, et al. Reduction in elective delivery at < 39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol 2010; 203:449. e1-6,3838. Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med 2009; 360:111-20.,3939. Bailey BA, Mc Cook JG, Chaires C. Burden of elective early-term births in rural Appalachia. South Med J 2014; 107:624-9., prolonged hospitalization 3333. Engle WA, Kominiarek MA. Late preterm infants, early term infants, and timing of elective deliveries. Clin Perinatol 2008; 35:325-41., neonatal mortality 4040. Reddy UM, Ko CW, Raju TN, Willinger M. Delivery indications at late-preterm gestations and infant mortality rates in the United States. Pediatrics 2009; 124:234-40., rehospitalization 4141. Dietz PM, Rizzo JH, England LJ, Callaghan WM, Vesco KK, Bruce FC, et al. Early term delivery and health care utilization in the first year of life. J Pediatr 2012; 161:234-9.e1., developmental delays 4242. Schonhaut L, Armijo I, Perez M. Gestational age and developmental risk in moderately and late preterm and early term infants. Pediatrics 2015; 135:e835-41., and early childhood illness 4343. Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, et al. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ 2012; 344:e896,4444. Edwards MO, Kotecha SJ, Lowe J, Richards L, Watkins WJ, Kotecha S. Early-term birth is a risk factor for wheezing in childhood: a cross-sectional population study. J Allergy Clin Immunol 2015; 136:581-7 e2.. In Brazil, the unfavourable outcomes associated with early-term birth include delayed initiation of breastfeeding, transient tachypnoea and hypoglycaemia, especially in those born via antepartum caesarean section. Due to the increased morbidity rate in early-term new-borns, several medical organizations 4545. American College of Obstetricians and Gynecologists. ACOG committee opinion no. 559: Cesarean delivery on maternal request. Obstet Gynecol 2013; 121:904-7.,4646. NICE: National Institute for Health and Clinical Excellence. Caesarean section (update). (Clinical guideline 132). http://guidance.nice.org.uk/CG132 (acessado em 26/Jan/2018).
http://guidance.nice.org.uk/CG132...
, including the Brazilian Federal Council of Medicine 4747. Conselho Federal de Medicina. Resolução CFM nº 2.144, de 17 de março de 2016. Art. 2º. Para garantir a segurança do feto, a cesariana a pedido da gestante, nas situações de risco habitual, somente poderá ser realizada a partir da 39ª semana de gestação, devendo haver o registro em prontuário. Diário Oficial da União 2016; 22 jun., recommend that elective discontinuations of gestation should not be performed before 39 gestational weeks.
A limitation of the present analysis is the disparity between the representativeness of samples from the studies that are being compared. Stork Network Assessment involved the total number of maternity wards that received the intervention of the Stork Network strategy, with national representation, similar to the Birth in Brazil study in Brazil. While 24 maternity wards with less than 500 births/year were included in Stork Network Assessment (something that did not occur in Birth in Brazil), it is unlikely that the results of these maternity hospitals significantly affected the improvement observed in care practices. On the other hand, the Healthy Birth study evaluated a convenience sample of the hospitals that participated in the Adequate Birth, a project that involved hospitals that voluntarily joined a quality improvement project. Most of these (9 of 12) were located in the Southeast region, which differentiates them from the set of private hospitals listed in the Birth in Brazil study. Therefore, interpretations of the private sector should be made with caution.
The comparison of the rate of caesarean section measured in hospitals evaluated in Healthy Birth with the rate that was observed in the same hospitals in SINASC in 2014 - a year prior to the implementation of the Adequate Birth - shows an overall reduction of 10% in the caesarean section rate. This indicates that the observed advances probably cannot be considered as resulting from sample differences.
On the other hand, the fact that the three studies used the same criterion for inclusion of women and adopted the same procedures and instruments for data collection (with the exception of the episiotomy variable), means that this study provides a unique evaluation of care practices in the country during this period.
In conclusion, the results of this study show that well-conducted public policies can positively affect labour and birth care, promoting the reduction of unnecessary caesarean section and negative maternal and neonatal outcomes. An increase in satisfaction on behalf of women undergoing birth care in the country is also a likely result. The process of change of labour and birth care in Brazil is in full development.
Acknowledgments
To the coordinators, supervisors, interviewers and technical staff of the three studies, and the participating mothers who made this evaluation possible. To the Brazilian National Research Council, Brazilian Ministry of Health, Bill and Melinda Gates Foundation and Rio de Janeiro State Research Foundation.
Referências
-
1Moreira MEL, Gama SGN, Pereira APE, Silva AAM, Lansky S, Pinheiro RS, et al. Práticas de atenção hospitalar ao recém-nascido saudável no Brasil. Cad Saúde Pública 2014; 30 Suppl 1:S128-39.
-
2Leal MC, Pereira APE, Domingues RMSM, Theme Filha MM, Dias MAB, Nakamura-Pereira M, et al. Intervenções obstétricas durante o trabalho de parto e parto em mulheres brasileiras de risco habitual. Cad Saúde Pública 2014; 30 Suppl 1:S17-47.
-
3Esteves-Pereira AP, Deneux-Tharaux C, Nakamura-Pereira M, Saucedo M, Bouvier-Colle MH, Leal MC. Caesarean delivery and postpartum maternal mortality: a population-based case control study in Brazil. PLoS One 2016; 11:e0153396.
-
4Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016; 388:2176-92.
-
5Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Domingues RMSM, Dias MAB, Moreira ME, et al. Burden of early-term birth on adverse infant outcomes: a population-based cohort study in Brazil. BMJ Open 2017; 7:e017789.
-
6Leal MC, Esteves-Pereira AP, Nakamura-Pereira M, Torres JA, Domingues RM, Dias MA, et al. Provider-initiated late preterm births in brazil: differences between public and private health services. PLoS One 2016; 11:e0155511.
-
7Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health 2016; 13 Suppl 3:115.
-
8Torres JA, Domingues RMSM, Sandall J, Hartz Z, Gama SGN, Theme Filha MM, et al. Cesariana e resultados neonatais em hospitais privados no Brasil: estudo comparativo de dois diferentes modelos de atenção perinatal. Cad Saúde Pública 2014; 30 Suppl 1:S220-31.
-
9Borem P, Ferreira JB, Silva UJ, Valerio Junior J, Orlanda CM. Increasing the percentage of vaginal birth in the private sector in Brazil through the redesign of care model. Rev Bras Ginecol Obstet 2015; 37:446-54.
-
10do Carmo Leal M, da Silva AA, Dias MA, da Gama SG, Rattner D, Moreira ME, et al. Birth in Brazil: national survey into labour and birth. Reprod Health 2012; 9:15.
-
11Vasconcellos MT, Silva PL, Pereira AP, Schilithz AO, Souza Junior PR, Szwarcwald CL. Desenho da amostra Nascer no Brasil: Pesquisa Nacional sobre Parto e Nascimento. Cad Saúde Pública 2014; 30 Suppl 1:S49-58.
-
12Torres JA, Leal MDC, Domingues RMSM, Esteves-Pereira AP, Nakano AR, Gomes ML, et al. Evaluation of a quality improvement intervention for labour and birth care in Brazilian private hospitals: a protocol. Reprod Health 2018; 15:194.
-
13Rebelo F, Rocha CM, Cortes TR, Dutra CL, Kac G. High cesarean prevalence in a national population-based study in Brazil: the role of private practice. Acta Obstet Gynecol Scand 2010; 89:903-8.
-
14Domingues RMSM, Dias MAB, Nakamura-Pereira M, Torres JA, Pereira APE, Schilithz AOC, et al. Processo de decisão pelo tipo de parto no Brasil: da preferência inicial das mulheres à via de parto final. Cad Saúde Pública 2014; 30 Suppl 1:S101-16.
-
15Brasil. Lei nº 11.108, de 7 de abril de 2005. Altera a Lei nº 8.080, de 19 de setembro de 1990, para garantir às parturientes o direito à presença de acompanhante durante o trabalho de parto, parto e pós-parto imediato, no âmbito do Sistema Único de Saúde (SUS). Brasília: Diário Oficial da União 2005; 8 abr.
-
16Lunda P, Minnie CS, Benade P. Women’s experiences of continuous support during childbirth: a meta-synthesis. BMC Pregnancy Childbirth 2018; 18:167.
-
17Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev 2011; (2):CD003766.
-
18d’Orsi E, Bruggemann OM, Diniz CSG, Aguiar JM, Gusman CR, Torres JA, et al. Desigualdades sociais e satisfação das mulheres com o atendimento ao parto no Brasil: estudo nacional de base hospitalar. Cad Saúde Pública 2014; 30 Suppl 1:S154-68.
-
19Diniz CS, d’Orsi E, Domingues RMSM, Torres JA, Dias MAB, Schneck CA, et al. Implementação da presença de acompanhantes durante a internação para o parto: dados da pesquisa nacional Nascer no Brasil Cad Saúde Pública 2014; 30 Suppl 1:S140-53.
-
20World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018.
-
21Francke AL, Smit MC, Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 2008; 8 :38.
-
22Davis DA, Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ 1997; 157:408-16.
-
23Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016; 4:CD004667.
-
24ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet 2014; 384:1226-35.
-
25Horton R, Astudillo O. The power of midwifery. Lancet 2014; 384:1075-6.
-
26Gama SGN, Viellas EF, Torres JA, Bastos MH, Brüggewrmann OM, Theme Filha MM, et al. Labor and birth care by nurse with midwifery skills in Brazil. Reprod Health 2016; 13 Suppl 3:123
-
27Vogt SE, Silva KS, Dias MA. Comparison of childbirth care models in public hospitals, Brazil. Rev Saúde Pública 2014; 48:304-13.
-
28Departamento de Gestão e Incorporação de Tecnologias em Saúde, Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Ministério da Saúde. Diretrizes nacionais de assistência ao parto normal: versão resumida (recurso eletrônico). Brasília: Ministério da Saúde; 2017.
-
29Blondel B, Coulm B, Bonnet C, Goffinet F, Le Ray C; National Coordination Group of the National Perinatal Surveys. Trends in perinatal health in metropolitan France from 1995 to 2016: results from the French National Perinatal Surveys. J Gynecol Obstet Hum Reprod 2017; 46:701-13.
-
30Anim Somuah M, Smyth RMD, Cyna AM, Cuthbert A. Epidural versus non‐epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 2018; 5:CD000331
-
31Barros FC, Rabello Neto DL, Villar J, Kennedy SH, Silveira MF, Diaz-Rossello JL, et al. Caesarean sections and the prevalence of preterm and early-term births in Brazil: secondary analyses of national birth registration. BMJ Open 2018; 8:e021538.
-
32Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ 2008; 336:85-7.
-
33Engle WA, Kominiarek MA. Late preterm infants, early term infants, and timing of elective deliveries. Clin Perinatol 2008; 35:325-41.
-
34Brown HK, Speechley KN, Macnab J, Natale R, Campbell MK. Neonatal morbidity associated with late preterm and early term birth: the roles of gestational age and biological determinants of preterm birth. Int J Epidemiol 2014; 43:802-14.
-
35Prefumo F, Ferrazzi E, Di Tommaso M, Severi FM, Locatelli A, Chirico G, et al. Neonatal morbidity after cesarean section before labor at 34(+0) to 38(+6) weeks: a cohort study. J Matern Fetal Neonatal Med 2016; 29:1334-8.
-
36Sengupta S, Carrion V, Shelton J, Wynn RJ, Ryan RM, Singhal K, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr 2013; 167:1053-9.
-
37Clark SL, Frye DR, Meyers JA, Belfort MA, Dildy GA, Kofford S, et al. Reduction in elective delivery at < 39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol 2010; 203:449. e1-6
-
38Tita AT, Landon MB, Spong CY, Lai Y, Leveno KJ, Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med 2009; 360:111-20.
-
39Bailey BA, Mc Cook JG, Chaires C. Burden of elective early-term births in rural Appalachia. South Med J 2014; 107:624-9.
-
40Reddy UM, Ko CW, Raju TN, Willinger M. Delivery indications at late-preterm gestations and infant mortality rates in the United States. Pediatrics 2009; 124:234-40.
-
41Dietz PM, Rizzo JH, England LJ, Callaghan WM, Vesco KK, Bruce FC, et al. Early term delivery and health care utilization in the first year of life. J Pediatr 2012; 161:234-9.e1.
-
42Schonhaut L, Armijo I, Perez M. Gestational age and developmental risk in moderately and late preterm and early term infants. Pediatrics 2015; 135:e835-41.
-
43Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, et al. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ 2012; 344:e896
-
44Edwards MO, Kotecha SJ, Lowe J, Richards L, Watkins WJ, Kotecha S. Early-term birth is a risk factor for wheezing in childhood: a cross-sectional population study. J Allergy Clin Immunol 2015; 136:581-7 e2.
-
45American College of Obstetricians and Gynecologists. ACOG committee opinion no. 559: Cesarean delivery on maternal request. Obstet Gynecol 2013; 121:904-7.
-
46NICE: National Institute for Health and Clinical Excellence. Caesarean section (update). (Clinical guideline 132). http://guidance.nice.org.uk/CG132 (acessado em 26/Jan/2018).
» http://guidance.nice.org.uk/CG132 -
47Conselho Federal de Medicina. Resolução CFM nº 2.144, de 17 de março de 2016. Art. 2º. Para garantir a segurança do feto, a cesariana a pedido da gestante, nas situações de risco habitual, somente poderá ser realizada a partir da 39ª semana de gestação, devendo haver o registro em prontuário. Diário Oficial da União 2016; 22 jun.
Publication Dates
-
Publication in this collection
22 July 2019 -
Date of issue
2019
History
-
Received
21 Nov 2018 -
Reviewed
27 Feb 2019 -
Accepted
06 Mar 2019