Abstracts
OBJECTIVE: To evaluate the results obtained from treatment of humeral shaft fractures and their complications using the Osteoline® uniplanar external fixator. METHODS: The radiographic and functional results from 78 patients with humeral shaft fractures treated using the uniplanar external fixation technique were retrospectively assessed. The patients' ages ranged from 23 to 71 years, with a mean of 47 years. Male patients predominated (79%). Out of the 78 patients, 45 presented open fractures, 14 presented pseudarthrosis and six presented synthesis failure. There were no losses during the follow-up and all the patients were discharged after fracture consolidation and functional recovery. The results were evaluated based on the studies by Catagni, as good, fair or poor. RESULTS: Fracture consolidation was observed in 98% of the cases treated with uniplanar external fixation. Only one pseudarthrosis case required conversion to rigid internal fixation and autologous bone grafting. At the end of the treatment, all the patients were discharged with consolidated fractures, without pain, and good limb function. CONCLUSION: The external fixation described in this paper was shown to be an efficient and safe method for treating humeral shaft fractures and their complications. It preserved the local biological status and enabled passive and active movement immediately after surgery.
Humeral Fractures; External Fixators; Pseudoartrhorosis
OBJETIVO: Avaliar os resultados obtidos no tratamento das fraturas diafisárias do úmero e suas complicações com o uso de fixadores externos uniplanares Osteoline®. MÉTODOS: Foram avaliados, retrospectivamente, os resultados radiográficos e funcionais de 78 pacientes com fraturas diafisárias do úmero tratados com a técnica de fixação externa uniplanar. A idade variou de 23 a 71 anos, com média de 47 anos. O sexo masculino foi predominante em 79% dos casos. Dos 78 pacientes, 45 apresentavam fraturas expostas, 14 pseudartroses e seis falhas de síntese. Não houve nenhuma perda durante o seguimento, sendo que todos os pacientes receberam alta após a consolidação da fratura e recuperação funcional. Os resultados foram avaliados com base nos trabalhos de Catagni em bom, regular e mau. RESULTADOS: Observamos a consolidação da fratura em 98% dos casos tratados com fixação externa uniplanar. Somente um caso de pseudartrose necessitou de conversão para fixação interna rígida e enxerto ósseo autólogo. Ao final do tratamento, todos os pacientes receberam alta com consolidação da fratura, sem dor e com boa função do membro. CONCLUSÃO: A fixação externa descrita no presente trabalho mostrou-se eficiente e segura como método de tratamento das fraturas diafisárias do úmero e suas complicações, preservando o status biológico local e propiciando movimentação passiva e ativa no pós-operatório imediato.
Fraturas do Úmero; Fixadores Externos; Pseudartrose
ORIGINAL ARTICLE
IOrthopedist and Head of the Orthopedics and Traumatology Service, São Lucas Accident and Maternity Hospital, Cacoal, Rondônia, Brazil
IIOrthopedist at the Orthopedics Service, Santa Casa de Misericórdia, Marília, São Paulo, and Trainee at São Lucas Accident and Maternity Hospital, Cacoal, Rondônia, Brazil
IIIOrthopedist at the Orthopedics Service, Santa Casa de Misericórdia, Marília, São Paulo, Brazil
Correspondence
ABSTRACT
OBJECTIVE: To evaluate the results obtained from treatment of humeral shaft fractures and their complications using the Osteoline® uniplanar external fixator.
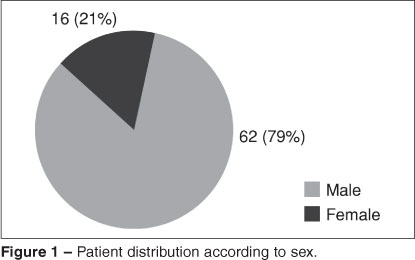
METHODS: The radiographic and functional results from 78 patients with humeral shaft fractures treated using the uniplanar external fixation technique were retrospectively assessed. The patients' ages ranged from 23 to 71 years, with a mean of 47 years. Male patients predominated (79%). Out of the 78 patients, 45 presented open fractures, 14 presented pseudarthrosis and six presented synthesis failure. There were no losses during the follow-up and all the patients were discharged after fracture consolidation and functional recovery. The results were evaluated based on the studies by Catagni, as good, fair or poor.
RESULTS: Fracture consolidation was observed in 98% of the cases treated with uniplanar external fixation. Only one pseudarthrosis case required conversion to rigid internal fixation and autologous bone grafting. At the end of the treatment, all the patients were discharged with consolidated fractures, without pain, and good limb function.
CONCLUSION: The external fixation described in this paper was shown to be an efficient and safe method for treating humeral shaft fractures and their complications. It preserved the local biological status and enabled passive and active movement immediately after surgery.
Keywords: Humeral Fractures; External Fixators; Pseudarthrosis
INTRODUCTION
Fractures of the humeral diaphysis account for around 1% of all fractures. They are fractures that present a high consolidation rate with conservative or surgical treatment(1). Functional orthoses generally lead to consolidation with acceptable limits of bone deformity while maintaining the mobility of adjacent joints during the treatment. On average, the consolidation rate in these cases is 90 to 98%, in series using functional immobilization(1-4). Although conservative treatment methods usually provide excellent results, some problems may persist, which has stimulated development of a variety of techniques for internal and external fixation(5).
The option of surgery is generally reserved for exposed fractures, fractures that remain unstable after reduction, pathological fractures, intolerance to conservative treatment, multiple-trauma patients, floating shoulder, floating elbow, bilateral fractures, progressive deficit of the radial nerve, lesions of the brachial plexus and vascular lesions(6). All other indications for surgery, including the use of external fixation as a means of treatment, would be exceptional. When surgical treatment is indicated, the surgeon should select the most appropriate method for each patient, based on the reason for fixation, the bone quality and the surgeon's own technical capacity.
External fixation for humeral fractures presents limited indications. These include exposed fractures in which the injuries sustained by soft tissues prevent the surgeon from safely accomplishing internal fixation, and fractures in which a segment of bone is lost(7,8). Furthermore, use of external fixation may be the fastest way to stabilize a fracture and make it possible for vascular surgeons to reconstitute the damages vessels, when there are vascular injuries with the capacity to put the affected limb at risk(9). Most clinical reports have concentrated on the use of external fixation to stabilize fractures caused by firearms(7,8).
Failure of a fracture of the humeral diaphysis to consolidate over a 24-week period(3) configures a situation of pseudarthrosis. Although this is an infrequent occurrence, it is considered to be serious because of the potential complications that accompany it. Effective treatment is fundament, in order to avoid persistent functional loss for the patient(10). Benedetti and Argnani(11), Catagni et al(12), Lopes Neto et al(13) and Pallazo Neto(14) analyzed the advantages and inconveniences of using an Ilizarov external fixator, highlighting the possibilities of consolidating the pseudarthrosis, treating the infection, correcting the displacements and filling in the bone loss through bone transportation.
In the present study, 78 cases of patients treated with external fixators in the humerus were studied retrospectively. For all of these patients, who had had various types of fractures with different degrees of comminution, as well as preoperative complications, periodic functional evaluations were made on the limbs. The aim was to assess the evolution and degree of functional recovery of upper-limb fractures that were treated using the Osteoline® external fixator.
PATIENT SAMPLE AND METHOD
The medical files of 78 patients with humeral fractures that were treated using external fixators between June 1996 and March 2009 were evaluated retrospectively. The medical files were reviewed in accordance with a previously drawn up protocol, in order to record all the information relating to the fractures, the treatment carried out and the follow-up on the patient. Following this, the radiographic examinations on the injuries that were available, from the date of the trauma and over the follow-up period until discharge from the outpatient clinic, were studied with the aim of evaluating the consolidation, evolution and return to function of the injured limb.
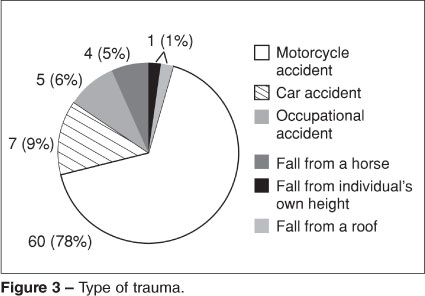
Among the 78 patients studied, 62 were men and 16 were women (Figure 1), with a mean age of 47 years (range: 23 to 71 years). There were 45 cases of exposed fractures, 13 cases of closed fractures, 14 cases of pseudarthrosis and six cases of synthesis failure (Figure 2). None of the patients died due to the initial injuries, or subsequently during the treatment. There was no loss from follow-up among the patients studied. The trauma mechanism was predominantly of high-energy type, including motorcycle accidents (60 cases), car accidents (seven cases) and occupational accidents (five cases) (Figure 3).
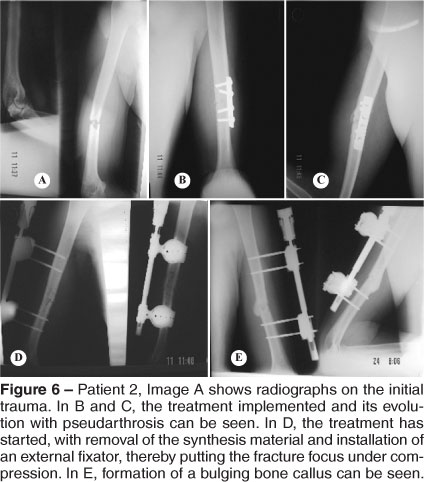
All the cases of humeral pseudarthrosis (Figures 4 and 5) and synthesis failure (Figure 6) came from other services. The cases of pseudarthrosis were treated by means of surgical stabilization using an external fixator (Figure 5). In five of these, this was done in association with implantation of an autologous graft from the iliac crest. In another three, the treatment also included local infiltration of 20 ml of bone marrow aspirate.
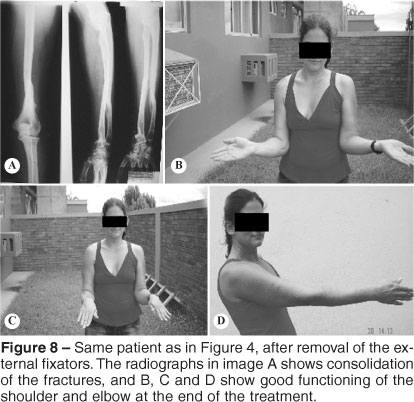
Among the comorbidities, three patients presented cranial-encephalic trauma, two had femoral fractures, six had tibial fractures and one had a floating elbow (Figures 7 and 8) and arrived with compartment syndrome of the forearm that required fasciotomy (Figure 9).
For all the 78 fracture cases, a rigid treatment scheme was followed. This consisted of reduction and stabilization of the bone lesion, early mobility and periodic outpatient follow-up.
The results were classified based on the studies by Catagni(12), into good, fair and poor. The result was considered to be good when there was consolidation without infection, absence of pain and good functioning of the affected limb. It was considered to be fair when there was consolidation without infection, but pain and/or joint movement limitation continued; and poor when consolidation did not occur, or infection or limiting joint stiffness was present, with poor limb functioning. Limb functioning was considered to be good when the patient was able to move the treated arm to his head, mouth, buttocks and contra-lateral shoulder.
Osteoline® external fixators (Figure 10) are unilateral and uniplanar and are compatible with cylindrical non-transfixing bone half-pins. This apparatus has a metal rod with a mechanism that allows it to be lengthened or shortened without altering the structure that was first set up. In assembling it, bone half-pins were used (Schanz pins). Two to three pins were inserted proximally and distally to the fracture focus, with a soft-tissue protector and template (Figure 11), which remained parallel longitudinally and at a predetermined distance. The Schanz pins were firmly fixed to a circular structure called a ring coupling. To connect between the pins and rods, there was a piece that firmly attached the rod to the ring coupling, in a ball-and-socket assembly (Figure 10). With the screws that lock the ring coupling to the connection piece only half tightened and the ring coupling fixed to the bone pins, we were able to use this setup as a "joystick", thereby aiding in reducing and aligning the fracture. The sum of the movements of the bar and the ring coupling allowed this assembly to have a wide variety of movements, as well as enabling adjustment within the outpatient setting.
SURGICAL TECHNIQUE
All the patients were operated by the same surgeon. It was decided to use brachial plexus blocks, both because of the quality of anesthesia and because of the postoperative analgesic effect. After rigorous asepsis and antisepsis covering the entire affected limb, we determined the lateral-access insertion points for the bone pins. We then opened the skin using a scalpel and continued with careful blunt dissection as far as the bone. We then carefully introduced the soft-tissue protector as far as the bone, so that there would not be any interposition of soft tissues. Each step was checked using radioscopy. We drilled a pilot hole with a 3.0 mm bit and introduced the 4.0 mm pin manually using a chuck key (Figure 11), with the aim of avoiding bone thermal necrosis.
Two to three bone pins were introduced proximally and distally to the focus of the fracture, parallel to each other. Each pin was at a distance predetermined by the soft-tissue protector and was fixed firmly to the external fixator structure. Following this, without completely tightening the screws and the aid of radioscopy, the fracture was reduced by using the pins as a "joystick" and the rod as an extension or compression structure (Figure 10). After achieving the desired reduction, the final tightening was performed, thus locking the fixator. The pins used were always chosen to be suitable for the bone quality of the region, i.e. in the metaphyseal region we used pins appropriate for spongy bone, and in the diaphyseal region we used pins appropriate for cortical bone.
POSTOPERATIVE PERIOD
Most of the patients were discharge after the effect of the anesthetic block wore off. Only the patients with comorbidities were kept in hospital, until they achieved clinical compensation.
During the immediate postoperative period, the patients were given guidance regarding hygienic care for the bone half-pins, dressings, passive mobility and early active mobility. We always advised the patients to remove the bandages before having a shower and to wash both the limb and the external fixator with running water and soap. Our advice for after the shower was that the patients should apply ointment containing neomycin and bacitracin to the bone half-pins, followed by bandaging including dry gauze, in order to diminish skin movement at the pin-skin interface.
Radiographs were requested on the 15th day after surgery and subsequently as required, on a case-by-case basis. After a bone callus had become visible radiographically, dynamization was started by adding flexibility to the external fixator through axial release. If the patient remained free from pain and showed adequate limb function over the next 15 days, the external fixator was removed.
In cases of pseudarthrosis or delayed consolidation, the technique described by Catagni was used(12). In this, compression was applied for three days and extension for three days, with one day of rest per week. This process was repeated for three weeks, and then a new assessment was made.
All the fixators were removed as outpatient procedures without anesthesia, although with sedation in some situations.
RESULTS
Consolidation was achieved in 98% of the cases. It only failed to occur in one of the cases of pseudarthrosis, in which intense osteolysis occurred because of lack of hygienic care with the external fixator. Because of this patient's non-cooperation and his intolerance of the fixator, we decided to use the orthosis described by Sarmiento et al(1) for three weeks, until good skin healing was achieved. Subsequently, osteosynthesis was performed, with rigid internal fixation and an autologous bone graft.
Taking into consideration only the pseudarthrosis cases (14 patients), consolidation occurred in 93% (Figure 5). In five of these cases, autologous bone grafting from the iliac crest was also performed, and in three cases, local infiltration of 20 ml of bone marrow aspirate.
The mean time taken to achieve consolidation was six months, with a range from three to nine months. The longest time taken was in the case of a patient with infected pseudarthrosis in the humeral diaphysis (Figures 4 and 5).
Most of the patients presented local inflammatory reactions in the regions of the pins, but without any significant clinical manifestation continuing to the end of the treatment.
The complications rate was 8%, including the case of pseudarthrosis mentioned above and one case of compartment syndrome that necessitated fasciotomy (Figure 12). Four events of pin breakage occurred, in three fixators, and there was one case of osteolysis. All of these cases already presented signs of consolidation and the treatment was completed using a Sarmiento orthosis, without other intercurrences. There were no cases of lesions of the radial nerve.
Taking into consideration the associated treatments described above, all the patients were discharged at the end of the treatment with consolidated fractures and good functional results in accordance with the criteria of Catagni et al(12) (Figure 8).
DISCUSSION
Humeral fractures represent 10% of all long-bone fractures, and the humeral diaphysis is affected in 30% of the cases. Although conservative treatment is emphasized in the literature as the preferred method for treating fractures of the humeral diaphysis, surgical indications are now increasing(10). The osteosynthesis techniques include compression or bridge plates, intramedullary nails and external fixators(15).
Treatment of humeral fractures and, especially, the complications from such treatments are always challenging for surgeons. External fixation is an option with a low complication rate and good clinical results, thereby reducing the length of hospitalization and the interval between hospital admission and the procedure, and hence minimizing the morbid condition.
Indication and correct application of an external fixation system depends on three basic concepts(16): anatomical knowledge of the region(17), knowledge of the physiopathology of the injury and biomechanical knowledge about external fixators(18). The surgeon's ability to manipulate these devices and the patient's socioeconomic and psychological characteristics should also be taken into consideration.
External fixators present several advantages(19,20): containment of the fracture hematoma, little disturbance of soft tissues and enabling of dynamization. According to Ruland(19), they combine the advantages of conservative and surgical treatment and influence bone callus formation through dynamization, extension and compression.
Clearly, external fixators also have disadvantages. One of these is the risk of infection along the path of the pins(19), which cross all the skin tissues to reach the bone, thereby placing these tissues in relative contact with each other and triggering friction with muscle masses. Another disadvantage is non-consolidation, which has particularly been associated with cases of severe compromising of the limb(19).
Orthopedic surgeons have to remain attentive to the prerequisites that are needed for consolidation of the lesion that is under treatment. Fixator assemblies that are unsuitable because of excessive rigidity or instability give rise to consolidation delays and pseudarthrosis(21).
Most studies in the literature have dealt with treatments for exposed fractures using external fixation. Among our patient sample, consolidation occurred in 98% of the cases treated with definitive external fixation. This result was higher than the findings of Mostafavi and Tornetta(7) and Wisniewski and Radziejowski(8) (94% and 89% respectively), and lower than the findings of Ruland(19), who achieved 100% consolidation in their series, in which external fixators were applied as the first choice. The mean time taken to achieve consolidation was 24 weeks, which was greater than the 11 weeks(7) and 16 weeks(8) cited. The more extensive lesions, cases of pseudarthrosis and synthesis failures necessitated longer times to reach a cure, including the use of autologous bone grafts subsequently, while maintaining the external fixation.
Watson-Jones(22), Sarmiento et al(23), Shapiro and Kozhokmatov(24) and Taylor(25) affirmed that consolidation of acute humeral fractures is relatively easy to achieve, but that if pseudarthrosis occurs, treatment success rarely comes from a single method or surgical technique(26). For such situations, use of associated techniques such as bone grafting, bone marrow aspirates, dynamization or flexibilization of the apparatus, or compression/extension techniques are of fundamental importance for increasing the consolidation. We agree that dynamization after formation of the radiographic bone callus is especially important in relation to the humerus, given that unlike in the lower-limb bones, there is no axial cyclic demand.
Focusing just on our pseudarthrosis cases, consolidation occurred in 93% of the cases. This result was comparable with the findings of Baptistão and Targa (92%)(26) and Silva and Catagni (95.7%)(27). For five patients, we also used autologous bone grafting, and for three patients, bone marrow aspirate.
The complication rate (8%) was lower than the findings in other series. Wisniewski and Radziejowski(8) reported a complication rate of 36%, which included two cases of deep infection and two cases of pseudarthrosis. Mostafavi and Tornetta(7) presented a complication rate of 22%, which included three cases of defective consolidation and one case of pseudarthrosis.
In our outpatient clinic, we have sought to create a relaxed environment, such that patients can get to know each other and share their personal experiences with fixators. We consider that this interchange is fundamental for demystifying fixators among patients. At these return visits to the clinic, the dressings, the condition of the soft tissue, the patient's state of hygiene, the state of hygiene of the external fixator and the functional condition of the injured limb are assessed in order to avoid future complications. We always advise patients to institute early mobility, with the aim of achieving rapid and better functional recovery.
Compared with other surgical treatment methods, the consolidation rates were better than or the same as the rates from using intramedullary nails or plates and screws. Crates and Whittle(28) and Lin and Hou(29) presented consolidation in 71% to 100% of their cases treated using anterograde intramedullary nails. Using osteosynthesis with plates and screws, Lin(30) and McCormack et al(31) reported consolidation rates of 96%, while Jawa et al(32) presented consolidation in 100% of their cases.
It is important to emphasize that the indication for treatment with an external fixator does not lie only in the fact that the case is one of an exposed or closed fracture. Rather, it lies in the current concept that the magnitude of soft-tissue lesions may be intense even in closed fractures. In such cases, the external fixator method contributes towards not increasing this damage. The fixator that we choose needs to be malleable in relation to its spatial configuration, and adaptable to the anatomical conditions of each body segment and to the different clinical situations caused by soft-tissue lesions.
In addition to the established preference for external fixators in treating exposed and multi-fragmented fractures, this method was shown to be effective and safe for simpler fractures, as an alternative to internal fixation. This method gives full regard to the soft tissues without interfering with the natural evolution of fracture consolidation, and without damaging the irrigation or drainage of the injured tissues. Application of external fixators to treat humeral pseudarthrosis does not have a negative influence on the biological potential of pseudarthrosis. It promotes stable fixation and maintains the mobility of adjacent joints, which is an important factor.
CONCLUSION
The Osteoline® external fixator was shown to be safe and efficient. It facilitated injury management and rehabilitation, and maintained the functionality of the adjacent joints. The external fixator used in the present study was capable of promoting consolidation in cases of acute fracture and pseudarthrosis of the humerus.
REFERENCES
- 1. Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(4):478-86.
- 2. Ward EF, Savoie FH, Hughes JL. "Fractures of the diaphyseal humerus". In: Browner BD, ed. Skeletal trauma. Philadelphia: Saunders; 1992. p. 1177-200.
- 3. Jupiter JB, von Deck M. Ununited humeral diaphyses. J Shoulder Elbow Surg.1998;7(6):644-53.
- 4. Zagorski JB, Latta LL, Zych GA, Finnieston AR. Diaphyseal fractures of the humerus. Treatment with prefabricated braces. J Bone Joint Surg Am. 1988;70(4):607-10.
- 5. Gregory PR. Fraturas da diáfise do úmero. In: Rockwood e Green. Fraturas em adultos. 5Ş edição. São Paulo: Manole; 2006. p.973-96.
- 6. Sarmiento A, Waddell JP, Latta LL. Diaphyseal humeral fractures: treatment options. Instr Course Lect. 2002;51:257-69.
- 7. Mostafavi HR, Tornetta P 3rd. Open fractures of the humerus treated with external fixation. Clin Orthop Relat Res. 1997;(337):187-97.
- 8. Wisniewski TF, Radziejowski MJ. Gunshot fractures of the humeral shaft treated with external fixation. J Orthop Trauma. 1996;10(4):273-8.
- 9. McNamara JJ, Brief DK, Stremple JF, Wright JK. Management of fractures with associated arterial injury in combat casualties. J Trauma. 1973;13(1):17-9.
- 10. Targa WHC, Baptistão JAB, Reis PR, Gangeiro PM. Tratamento da pseudoartrose da diáfise do úmero com fixação externa. In: 2º Curso Internacional de Reconstrução Osteo-Articular, Tomar, Portugal, 2008.
- 11. Benedetti GB, Argnani F. "Prime applicazioni cliniche dell'apparato compressore-distrattore di Ilizarov". In: Bianchi-Maiocchi A. L'osteosintesi transossea secondo G.A Ilizarov. Milano: Medsi; 1985. p. 319-25.
- 12. Catagni MA, Guerreschi F, Probe RA. Treatment of humeral nonunions with the Ilizarov technique. Bull Hosp Jt Dis Orthop Inst. 1991;51(1):74-83.
- 13. Lopes Neto LL, Barcellos L, Freitas FF, Cardoso SMM. Tratamento de pseudartrose da diáfise umeral pelo método de Ilizarov. Rev Bras Ortop. 1992;27(7):628-32.
- 14. Pallazzo Neto E. Tratamento da pseudartrose traumática infectada e não infectada do úmero pelo método de Ilizarov [dissertação]. São Paulo: Escola Paulista de Medicina, Universidade Federal de São Paulo; 1995.
- 15. Rommens PM, McCormack R. Úmero, diáfise. In Rüedi TP, Buckley RE, Moran CG. Princípios AO do tratamento de fraturas. 2a. edição. Porto Alegre: Artmed; 2009. p. 677-89.
- 16. Fernandez A. Modular external fixation in emergency using the AO tubular system. Montevidéu: Ed. Mor Adentro; 1991.
- 17. Barral JP, Gil DR, Vergana SS. Atlas Anatomotropográfico de lãs estremidades y fijación externa anular. Barcelona: Jins; 1988. p. 32-51.
- 18. Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989;(241):15-23.
- 19. Ruland WO. Is there a place for external fixation in humeral shaft fractures? Injury. 2000;31(Suppl 1):27-34.
- 20. Johnson EC, Strauss E. Recent advances in the treatment of gunshot fractures of the humeral shaft. Clin Orthop Relat Res. 2003;(408):126-32.
- 21. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24(8):742-6.
- 22. Watson-Jones R. "Retardo y falta de consolidacion". In: Fracturas y traumatismos articulares. 2Ş ed. Barcelona: Salvat; 1965. p. 14-40.
- 23. Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(5):596-601.
- 24. Shapiro AS, Kozhokmatov SK. "Il trattamento in compressionedistrazione extra-focolaio secondo Ilizarov delle frature diafisarie e delle pseudoartrosi delle ossa lunghe tubolari complicate da osteomielite". In: Bianchi-Maiocchi A. L'osteosintesi transossea secondo G.A. Ilizarov. Milano: Medsi; 1985. p. 218-9.
- 25. Taylor JC. Delayed union and nonunion of fractures. In: Crenshaw AH editor. Campbell's operative orthopaedics. 8th ed. St. Louis: Mosby; 1992. p. 1287-1345.
- 26. Baptistão JAB, Targa WHC, Catena RS, Bolliger Neto R, Reis PR. Tratamento das pseudartroses da diáfise umeral pelo método de Ilizarov. Res Bras Ortop. 1997; 32(8):647-52.
- 27. Silva WN, Catagni MA. Pseudartrose do úmero: tratamento com a técnica de Ilizarov. Res Bras Ortop. 1996;31(8): 633-7.
- 28. Crates J, Whittle AP. Antegrade interlocking nailing of acute humeral shaft fractures. Clin Orthop Relat Res. 1998;(350):40-50.
- 29. Lin J, Hou SM. Antegrade locked nailing for humeral shaft fractures. Clin Orthop Relat Res. 1999;(365):201-10.
- 30. Lin J. Treatment of humeral shaft fractures with humeral locked nail and comparison with plate fixation. J Trauma. 1998;44(5):859-64.
- 31. McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336-9.
- 32. Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am. 2006;88(11):2343-7.
Treatment of post-traumatic humeral fractures and complications using the Osteoline® external fixator: a treatment option
Publication Dates
-
Publication in this collection
18 Oct 2011 -
Date of issue
2011
History
-
Accepted
29 Oct 2010 -
Received
25 May 2010