Abstracts
OBJECTIVES:
the aim of this study was to evaluate the surgical technique and determine the initial results, with a minimum follow-up of two years, from total knee arthroplasty revisions in which trabecular metal cones made of tantalum were used at the Knee Surgery Center of the National Institute of Traumatology and Orthopedics (INTO) or at the authors' private clinic between July 2008 and December 2010.
METHODS:
ten patients were included in the study prospectively, through clinical and radiographic evaluations.
RESULTS:
seven patients presented evolution without complications relating to the tantalum cones used. Five of these patients said that they did not have any pain and all of them were able to walk without needing crutches. In all the cases, we observed that osseointegration of the tantalum cones had occurred. No migration or loosening of the implants was observed, nor was osteolysis.
CONCLUSION:
use of trabecular metal cones made of tantalum for treating AORI type II or II bone defects was capable of providing efficient structural support to the prosthetic revision implants, in evaluations with a short follow-up.
Knee arthroplasty; Prostheses and implants; Tantalum; Osseointegration
OBJETIVOS:
avaliar a técnica cirúrgica e determinar os resultados iniciais, com seguimento mínimo de dois anos, das revisões de artroplastia total do joelho nas quais cones de metal trabecular tântalo foram empregados pelo Centro de Cirurgia do Joelho do Instituto Nacional de Traumatologia e Ortopedia (Into) ou na clínica privada dos autores de julho de 2008 a dezembro 2010.
MÉTODOS:
foram incluídos no estudo 10 pacientes, prospectivamente em avaliação clínica e radiográfica.
RESULTADOS:
sete pacientes apresentaram evolução sem complicações relacionadas ao uso de cones de tântalo, cinco negam dor e todos deambulam sem necessidade de muletas. Em todos os casos, verificamos osteointegração dos cones de tântalo e não foi observada migração ou soltura de implantes, assim como osteólise.
CONCLUSÃO:
o uso de cones de metal trabecular tântalo para tratamento de defeitos ósseos tipo II ou III Aori apresenta-se capaz de prover suporte estrutural eficiente aos implantes protéticos de revisão em avaliação de curto seguimento.
Artroplastia do joelho; Próteses e implantes; Tântalo; Osteointegração
Introduction
Since the end of the 1980s, there have been rises of up to 10% per year in the numbers of knee arthroplasty procedures performed in the United States.11. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487-97. Between 1990 and 2002, the number of primary operations per 100,000 inhabitants in that country tripled.11. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487-97. Increased life expectancy together with the rising number primary operations has consequently led to greater numbers of revision surgery procedures.
In 2002, more than 350,000 knee prostheses were implanted in the United States.22. Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222-8. In the same year, the number of revision procedures increased by 7.5%.22. Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222-8. Kurtz et al.33. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-5. estimated that the number of revision procedures would increase by 600% by 2030.
Management of bone loss within the scenario of knee revision arthroplasty represents an enormous challenge. The bone defect may result from the initial disease, the design of the primary prosthesis used, the failure mechanism, technical errors in the primary surgery or difficulty in removing the fixed implants.44. Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90(8):981-7. and 55. Tsahakis PJ, Beaver WB, Brick GW. Technique and results of allograft reconstruction in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;(303):86-94.
Correction of the bone deficiency becomes necessary in order to achieve a stable bone-implant interface. This enables correct alignment of the components, maintenance of adequate height for the joint interline and ligament balance. Thus, this correction is a determining factor in the clinical result.44. Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90(8):981-7. , 55. Tsahakis PJ, Beaver WB, Brick GW. Technique and results of allograft reconstruction in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;(303):86-94. and 66. Bush JL, Wilson JB, Vail TP. Management of bone loss in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;452:186-92.
Bone defects can be managed by filling them using methyl methacrylate, autologous spongy bone grafts, autologous structural graft fragments, modular metallic boosters or thicker polyethylene components. Nonetheless, the correct treatment for large defects remains undefined and homologous structural grafts, impacted spongy grafts or unconventional prostheses can be used.77. Bradley GW. Revision total knee arthroplasty by impaction bone grafting. Clin Orthop Relat Res. 2000;(371):113-8. , 88. Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:99-103. , 99. Huff TW, Sculco TP. Management of bone loss in revision total knee arthroplasty. J Arthroplasty. 2007;22 7 Suppl. 3:32-6. and 1010. Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:104-12.
Several studies that used homologous structural grafts for managing bone failures during revision surgery have shown nonunion rates of up to 4%, infection risk ranging from 4% to 8% and failure rates from 8% to 23%.1111. Bauman RD, Lewallen DG, Hanssen AD. Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res. 2009;467(3):818-24. , 1212. Mnaymneh W, Emerson RH, Borja F, Head WC, Malinin TI. Massive allografts in salvage revisions of failed total knee arthroplasties. Clin Orthop Relat Res. 1990;(260):144-53. , 1313. Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE. Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Joint Surg Am. 1997;79(1):17-25. and 1414. Berrey Jr BH, Lord CF, Gebhardt MC, Mankin HJ. Fractures of allografts, frequency, treatment, and end-results. J Bone Joint Surg Am. 1990;72(6):825-33. Thus, the capacity of structural grafts to provide effective long-term support can be questioned.
Trabecular metal boosters made of tantalum, in a variety of cone shapes, are currently an option for managing bone failure in complex cases of total knee arthroplasty (TKA) revision and are an option when using structural grafts from a musculoskeletal tissue bank.
The objective of this study was to evaluate the initial results, with a minimum follow-up of two years, from TKA revision in which trabecular metal cones made of tantalum were used to treat large tibial or femoral bone defects.
Materials and methods
Patients who underwent TKA revision surgery between July 2008 and December 2010, for whom trabecular metal cones were needed for adequate treatment of the bone defects, were included in this study.
The procedures were performed at the Knee Surgery Center of the National Institute for Traumatology and Orthopedics (INTO) and at the authors' private clinic. All patients who underwent TKA revision in which the bone defects encountered were treated using other methods were excluded from this series: for example, metal wedges or homologous grafts, or furthermore, those in whom tantalum cones were used in association with structural grafts.
The patients were followed up prospectively with postoperative clinical and radiographic evaluations: 15 days, one month, three months, six months and one year after the operation, and annually thereafter.
The radiographic evaluation was conducted by comparing radiographs of the knee produced during the immediate postoperative period with those produced at subsequent evaluations, in anteroposterior view with weight-bearing and in lateral view. The criterion used to define occurrence of osseointegration of the tantalum cones was the presence of a trabecular reaction at the trabecular metal interface of the host bone, as assessed using sequential radiographs, which was configured by the presence of bone sclerosis together with absence of radiolucency lines.
During the radiographic observation, the criteria of the Knee Society's evaluation and scoring system1515. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;(248):9-12. were used to determine occurrences of loosening or migration of prosthetic components or trabecular cones.
This study was submitted to the Research Ethics Committee of INTO for evaluation and approval, and was conducted at this institution's Knee Surgery Center.
Trabecular metal cones made of tantalum
Trabecular metal consisting of tantalum (Trabecular Metal, Zimmer, Warsaw, Indiana) is a biocompatible material with a low module of elasticity, high porosity and excellent biological potential for fixation. These characteristics enable uniform load distribution, which in theory reduces the occurrences of the phenomenon known as stress shielding.1616. Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009;24(7):1086-92.
Several histological studies have demonstrated that this material has low potential for bacterial adherence and greater leukocyte activation, in comparison with the materials habitually used in orthopedics.17 17. Schildhauer TA, Robie B, Muhr G, Köller M. Bacterial adherence to tantalum versus commonly used orthopedic metallic implant materials. J Orthop Trauma. 2006;20(7):476-84. and 1818. Schildhauer TA, Peter E, Muhr G, Köller M. Activation of human leukocytes on tantalum trabecular metal in comparison to commonly used orthopedic metal implant materials. J Biomed Mater Res A. 2009;88(2): 332-41.
The biological fixation capacity of trabecular metal allows it to act as a substrate for bone growth, with migration of host osteoblasts to gaps in the metal, with consequent replacement of the bone stock.
Because of these potential advantages, interest in using this metal in joint reconstruction surgery is clearly growing.
Cones of different shapes and sizes have been developed to make it possible to fill a large variety of distal femoral or proximal tibial defects located at the center of the metaphysis or associated with cortical bone deficiency.
These cones should be impacted into the bone defects, thereby enabling osseointegration between this material and the host bone and concomitantly making it possible to use prosthetic revision components with intramedullary nails.
Surgical technique
The surgical access was made in accordance with the traditional techniques commonly used in revision surgery.
A standard technique for removing prosthetic components or spacers was firstly used. After debridement, the bone defects encountered were classified using the Anderson Orthopaedics Research Institute (AORI) system.1919. Engh GA, Parks NL. The use of a bone defect classification system in revision total knee arthroplasty. Orthop Trans. 1995;18:1136-40. The femur and tibia were dealt with separately, in the following manner: type 1 - presenting complete metaphyseal bone with small defects that would not compromise the stability of the revision implant; type 2 - with loss of spongy bone in the metaphyseal region, which could occur in one (A) or in two (B) femoral or tibial condyles; type 3 - with deficient metaphyseal bone, occasionally associated with detachment of the collateral ligaments.
The classification of the bone failure, along with the quantity and location of the remaining cortical and spongy bone, was taken into consideration in deciding whether to manage the bone defect by using a trabecular metal cone. In all the patients, the defect was classified as type 2 or higher.
Tibial and femoral intramedullary guides were used to obtain correct alignment of the prosthetic components and to perform bone cuts using a standard technique. Ligament balance was achieved in conformity with the current concepts.
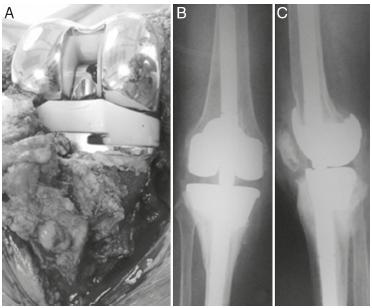
The defects encountered were appropriately filled through testing different shapes and sizes representing the trabecular metal cones available. Bone prominences that made it impossible to impact or maintain the trabecular cones in stable positions were debrided using a burring drill bit, with the aim of achieving greater stability and the greatest bone contact possible (Fig. 1A-C).
The rotation of the tantalum cones was determined by the location, shape and size of the bone defects. The rotational stability of the trabecular cone was evaluated by the surgeon through manipulation after impaction of the implant.
The rotation of the definitive prosthetic components was guided by the parameters of the standard technique, and not by the location and rotation of the trabecular cones.
Areas between the external surface of the tantalum cone and the host bone were grafted using autologous bone coming from the cuts that had been made. The internal surface of the trabecular cones reconstituted the proximal metaphyseal region of the tibia or the distal region of the femur and acted as a surface for cementation of the definitive prosthetic components, using intramedullary nails (Fig. 2A-C).
Tantalum cone in proximal tibia with autologous graft on external surface (A), cementation in interior (B), with implantation of the tibial component (C).
During the immediate postoperative period, the gain in complete range of motion was stimulated and weight-bearing was allowed as tolerated.
Results
Demographic data
Ten patients who underwent TKA revision surgery using trabecular metal cones made of tantalum were included in this study. Three were male and seven were female. Their mean age was 71.1 years, with a range from 59 to 80. The surgery was performed on the right side in three cases and on the left side in seven cases. One patient was lost from the postoperative follow-up due to death that was unrelated to the surgery, one year after the revision; at this patient's last follow-up evaluation, he did not present any complication and maintained good joint function. The mean length of the postoperative follow-up was 34.7 months, with a range from 26 to 45 months.
In eight patients, the trabecular metal cone was used in a first revision. The causes of failure had been infection in two cases, poor alignment and sinking into varus in two, osteolysis in two, worn-out polyethylene in one and aseptic loosening in one.
In one patient, the tantalum booster was used in a second TKA revision procedure. The primary arthroplasty had failed due to sinking of the tibial component into varus. Revision was then performed using a conventional metal booster wedge. Ten days later, the patient suffered a fall from a standing position and developed exposure of the prosthesis, which resulted in infection. This was treated as a two-stage revision procedure and a tantalum cone was then used.
In another case, the cone was used in a third revision procedure. We were unable to identify the cause of the first two revisions. The third revision was performed due to poor alignment and instability.
Surgical data
On the femoral side, trabecular cones were used in three cases: the bone defect was classified as F2B in two cases and F3 in one. The cause of the failure was poor alignment in two cases and osteolysis in one. In one case, the revision implant used was the TC III (Depuy Synthes(r)), which required a cemented femoral nail of dimensions 18 mm × 175 mm, 12 mm distal metal boosters and 4 mm posterior boosters. The trabecular cone used in this case was of medium size, with a height of 40 mm. In the other cases, the implant used was the Rotating Hinge Knee (Zimmer(r)) and cemented nails of dimensions 10 × 145 mm and 15 × 145 mm were implanted. In both cases, 10 mm distal metal booster wedges were used. The trabecular cones used in these cases were of medium size.
On the tibial side, tantalum trabecular cones were used in nine cases. The defects encountered were classified thus: T2A, T2B and T3, in three cases each.
LCCK semi-constricted implants (Zimmer(r)) were used in five patients, while TC III semi-constricted implants (Depuy Synthes(r)) were used in two cases and folding constricted implants (Rotating Hinge Knee, Zimmer(r)) were used in a further two cases.
In all the tibial components, a cemented intramedullary nail was used, and no metal booster wedges were used. The cement used in the revision surgery in all cases was Simplex, with addition of 2 g of vancomycin per dose of methyl methacrylate.
The thickness of the polyethylene ranged from 10 to 22.5 mm. The patella was revised in six cases, while the original patellar implant was maintained in the other four cases.
Clinical results and reoperations
One patient died 12 months after the operation from causes unrelated to the revision surgery.
There was one case of reoperation to perform drainage of a voluminous hematoma in the first postoperative month.
One patient presented recurrence of infection after a new surgical intervention to treat an injury to the extensor mechanism, which occurred during a fall from a standing position during the first month after the second TKA revision. This patient underwent removal of the prosthetic components and arthrodesis of the knee and achieved the infection cure criteria.
Two patients presented periprosthetic fracturing of the femur. The first had received trabecular metal cones in femoral and tibial defects and a constricted hinged prosthesis had been implanted one month earlier. This patient underwent osteosynthesis and homologous grafting and then developed loosening of the synthesis, which gave rise to the need for a new surgical approach. He then evolved with infection that was difficult to clinically control, along with loss of the extensor mechanism, and the limb had to be amputated.
The second patient had undergone revision using a tantalum insert in a tibial defect 14 months earlier. During a fall from a standing position, he presented femoral periprosthetic fracturing without loosening of the components, and without signs of osseointegration of the trabecular metal cone. He underwent osteosynthesis and homologous bone grafting of two femoral regions, using tissue bank material, and evolved to consolidation.
Thus, seven patients presented a minimum clinical follow-up of 24 months. The mean flexion was 95°, with a range from 85° to 115°. In six cases, complete extension was observed, while one patient had a 10° deficit of active extension.
Six patients presented varus-valgus stability in extension and anteroposterior stability during an assessment at 90° of flexion. In one patient, after 24 months of evolution of a semi-constricted implant and a tantalum cone in the tibia, we observed evolution toward insufficiency of the medial structures, which caused instability. Revision for a constricted implant was therefore indicated.
In one patient, we observed necrosis of the patella and subluxation. This patient evolved with limitation of the end of active extension, but without limitation relating to activities of daily living. The other patients did not present any patellofemoral complications. Five of these patients said that they were not in pain and all of them were able to walk without the need for crutches.
Radiographic results
Comparison of the sequential radiographic examinations showed that there was a trabecular bone reaction at the interface between the host bone and the trabecular metal and absence of radiolucency lines between the cone and the host bone in these seven patients. These features constituted signs of osseointegration of the implant.
We did not observe any loss or migration of the trabecular metal cone or prosthetic components in any of the patients. No signs of osteolysis were observed in the cases evaluated. During the radiographic follow-up of our sample, we have so far not identified any radiolucency lines that would constitute loosening of the implants (Fig. 3).
Discussion
Management of bone defects during TKA revision is a determining factor in the final clinical result, given that it provides the possibility of achieving a stable bone-implant interface and enables correct alignment of the limb, maintenance of an adequate height for the joint interline and ligament balance. Technical improvement of treatments for large bone defects still remains undefined today.77. Bradley GW. Revision total knee arthroplasty by impaction bone grafting. Clin Orthop Relat Res. 2000;(371):113-8. , 88. Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:99-103. , 99. Huff TW, Sculco TP. Management of bone loss in revision total knee arthroplasty. J Arthroplasty. 2007;22 7 Suppl. 3:32-6. and 1010. Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:104-12.
The studies available that have evaluated the safety and effectiveness of using homologous structural grafts from musculoskeletal tissue banks during revision surgery present limited numbers of cases and lack long-term postoperative follow-up.2020. Hockman DE, Ammeen D, Engh GA. Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. 2005;20(1):35-41. , 2121. Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89(12):2640-7. and 2222. Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am. 2001;83-A(3):404-11.
Hockman et al.2020. Hockman DE, Ammeen D, Engh GA. Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. 2005;20(1):35-41. evaluated 65 revision operations on bone deficiency, with a minimum postoperative follow-up of five years, and concluded that modular metal boosters were not an effective means of treatment for major bone failures within the scenario of TKA. However, in the revisions in which structural grafts were used, failure occurred in approximately 20% of the cases.
Engh and Ammeen2121. Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89(12):2640-7. conducted a study in which they evaluated 35 revision arthroplasty procedures in cases with AORI type II or II bone defects that were treated using structural grafts, with postoperative follow-up of 4.2 years, and they showed good or excellent results in 87% of the cases. Clatworthy et al.2222. Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am. 2001;83-A(3):404-11. showed that 72% of their results were good, in a study in which 66 structural grafts were used to manage 52 knee arthroplasty revision surgery procedures, thus providing corroboration for such data.
Lonner et al.2323. Lonner JH, Lotke PA, Kim J, Nelson C. Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res. 2002;(404):145-51. reported on TKA revision performed in 17 cases, in which uncontained large bone defects were managed using impacted bone grafts. In this study, no graft failures were reported, although the postoperative follow-up in 15 cases was less than 24 months.
Over recent years, use of trabecular metal cones made of tantalum, in different shapes and sizes, has formed an important option for treating large metaphyseal bone defects in cases of complex revision of knee arthroplasty.
The technique of implantation of tantalum cones is relatively simple in relation to the use of structural grafts and it thus reduces the duration of the operation and consequently the risk of infection. Another advantage is the elimination of the potential risk of transmission of contagious diseases that is associated with homologous bone transplantation.
Several characteristics of trabecular metal favor its use as a biomaterial in orthopedic surgery. Thus, the following can be highlighted: the high coefficient of friction, which makes it possible for the tantalum cone to present excellent initial mechanical stability, even with a reduced contact area with the host bone; the low elastic modulus of the metal, which is similar to that of spongy bone and enables better load distribution and reduction of the phenomenon of stress shielding; and the high porosity, which provides a cell migration surface and enables osseointegration when the material is in contact with the host bone and interfingering of cement when in contact with the implants and cemented nails.
Difficulty in removing trabecular metal implants represents a theoretical disadvantage in comparison with other methods for managing bone failure. In our series, one patient presented a need for removal of the implants and the tantalum cone in the tibia, because of infection. We did not identify any additional difficulties, probably because of the short time that had elapsed since the initial surgery.
Because studies evaluating the safety and effectiveness of trabecular metal comprise a recent option for managing bone failure, there are not many of them and the sample size is limited. Nonetheless, the initial results have been satisfactory.2424. Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90(1):78-84. , 2525. Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83-92. , 2626. Howard JL, Kudera J, Lewallen DG, Hanssen AD. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011;93(5):478-84. and 2727. Lachiewicz PF, Bolognesi MP, Henderson RA, Soileau ES, Vail TP. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012;470(1):199-204.
Meneghini et al.2424. Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90(1):78-84. conducted a study in which they evaluated 15 revision procedures on tibial defects greater than T2B, with the use of trabecular metaphyseal cones in the proximal tibia, with 34 months of follow-up. They did not find any evidence of loosening or migration of the cones or the prosthetic components and they noted radiological signs of osseointegration in all the cases.
In the same way, Radnay and Scuderi2525. Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83-92. did not note any migration or loosening of implants after 10 months of postoperative follow-up, in an evaluation on 10 patients with proximal tibial defects that were managed using tibial metaphyseal cones.
Howard et al.2626. Howard JL, Kudera J, Lewallen DG, Hanssen AD. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011;93(5):478-84. studied 24 TKA revision surgery procedures with bone failure in the distal femur that were treated using femoral metaphyseal cones. Over a postoperative follow-up of 33 months, they did not find any complications associated with using the tantalum cone. All the patients showed radiographic signs of osseointegration. These authors therefore concluded that femoral metaphyseal cones were capable of providing effective structural support for femoral revision implants.
Lachiewics et al.2727. Lachiewicz PF, Bolognesi MP, Henderson RA, Soileau ES, Vail TP. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012;470(1):199-204. reported on implantation of 33 tantalum cones in 27 revision surgery procedures with a minimum follow-up of two years. They observed loosening of the implants and lack of osseointegration of a femoral tantalum cone in one case, which therefore required a new surgical approach.
Our data are concordant with the literature. We observed radiographic signs of osseointegration in all of our patients and did not note any case of migration or loosening of components. The complications that occurred, such as infection and periprosthetic fracturing, were not associated with use of the trabecular metal but, rather, to the complexity of the cases. In our sample, most of the defects occurred on the tibial side. However, we did not observe any difference in the capacity of the trabecular cone to provide support for the prosthetic implant, between the femoral and tibial sides.
Conclusion
From a short-term follow-up, trabecular metal cones made of tantalum for treating AORI type II or type III bone defects were capable of providing efficient structural for prosthetic implants within the scenario of knee revision arthroplasty.
Over this short-term evaluation, we did not observe any loosening or migration of components and we identified osseointegration in all the cases. Nonetheless, studies with greater numbers of cases and longer postoperative follow-up are necessary.
REFERENCES
-
1Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487-97.
-
2Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87(6):1222-8.
-
3Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-5.
-
4Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90(8):981-7.
-
5Tsahakis PJ, Beaver WB, Brick GW. Technique and results of allograft reconstruction in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;(303):86-94.
-
6Bush JL, Wilson JB, Vail TP. Management of bone loss in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;452:186-92.
-
7Bradley GW. Revision total knee arthroplasty by impaction bone grafting. Clin Orthop Relat Res. 2000;(371):113-8.
-
8Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:99-103.
-
9Huff TW, Sculco TP. Management of bone loss in revision total knee arthroplasty. J Arthroplasty. 2007;22 7 Suppl. 3:32-6.
-
10Backstein D, Safir O, Gross A. Management of bone loss: structural grafts in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:104-12.
-
11Bauman RD, Lewallen DG, Hanssen AD. Limitations of structural allograft in revision total knee arthroplasty. Clin Orthop Relat Res. 2009;467(3):818-24.
-
12Mnaymneh W, Emerson RH, Borja F, Head WC, Malinin TI. Massive allografts in salvage revisions of failed total knee arthroplasties. Clin Orthop Relat Res. 1990;(260):144-53.
-
13Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE. Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Joint Surg Am. 1997;79(1):17-25.
-
14Berrey Jr BH, Lord CF, Gebhardt MC, Mankin HJ. Fractures of allografts, frequency, treatment, and end-results. J Bone Joint Surg Am. 1990;72(6):825-33.
-
15Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;(248):9-12.
-
16Long WJ, Scuderi GR. Porous tantalum cones for large metaphyseal tibial defects in revision total knee arthroplasty: a minimum 2-year follow-up. J Arthroplasty. 2009;24(7):1086-92.
-
17Schildhauer TA, Robie B, Muhr G, Köller M. Bacterial adherence to tantalum versus commonly used orthopedic metallic implant materials. J Orthop Trauma. 2006;20(7):476-84.
-
18Schildhauer TA, Peter E, Muhr G, Köller M. Activation of human leukocytes on tantalum trabecular metal in comparison to commonly used orthopedic metal implant materials. J Biomed Mater Res A. 2009;88(2): 332-41.
-
19Engh GA, Parks NL. The use of a bone defect classification system in revision total knee arthroplasty. Orthop Trans. 1995;18:1136-40.
-
20Hockman DE, Ammeen D, Engh GA. Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. 2005;20(1):35-41.
-
21Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am. 2007;89(12):2640-7.
-
22Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty. A minimum five-year review. J Bone Joint Surg Am. 2001;83-A(3):404-11.
-
23Lonner JH, Lotke PA, Kim J, Nelson C. Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res. 2002;(404):145-51.
-
24Meneghini RM, Lewallen DG, Hanssen AD. Use of porous tantalum metaphyseal cones for severe tibial bone loss during revision total knee replacement. J Bone Joint Surg Am. 2008;90(1):78-84.
-
25Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83-92.
-
26Howard JL, Kudera J, Lewallen DG, Hanssen AD. Early results of the use of tantalum femoral cones for revision total knee arthroplasty. J Bone Joint Surg Am. 2011;93(5):478-84.
-
27Lachiewicz PF, Bolognesi MP, Henderson RA, Soileau ES, Vail TP. Can tantalum cones provide fixation in complex revision knee arthroplasty? Clin Orthop Relat Res. 2012;470(1):199-204.
-
☆
Please cite this article as: Mozella AP, Olivero RR, Alexandre H, Cobra AB. Uso de cone de metal trabecular tântalo para tratamento de defeitos ósseos na artroplastia de revisão do joelho. Rev Bras Ortop. 2014;49:245-251.
-
☆☆
Work developed at the Knee Surgery Center, Instituto Nacional de Traumatologia e Ortopedia, Rio de Janeiro, RJ, Brazil.
Publication Dates
-
Publication in this collection
May-June 2014
History
-
Received
07 Dec 2012 -
Accepted
12 July 2013