ABSTRACT
OBJECTIVE:
To describe a surgical technique for anatomical reconstruction of the medial patellofemoral ligament using the quadriceps tendon, combined with reconstruction of the medial patellotibial ligament using the patellar tendon; and to present the initial results from a case series.
METHOD:
The proposed technique was used on a series of cases of patients with diagnoses of patellofemoral instability and indications for surgical treatment, who were attended by the Knee Group of HC-IOT, University of São Paulo. The following were evaluated before and after the operation: range of motion (ROM), apprehension test, lateral translation test, patellar inclination test, inverted J sign, subluxation upon extension, pain from compression of the patella and pain from contraction of the quadriceps. After the operation, the patients were asked whether any new episode of dislocation had occurred, what their degree of satisfaction with the surgery was (on a scale from 0 to 10) and whether they would be prepared to go through this operation again.
RESULTS:
Seven knees were operated, in seven patients, with a mean follow-up of 5.46 months (±2.07). Four patients who presented apprehension before the operation did not show this after the operation. The lateral translation test became normal for all the patients, while the patellar inclination test remained positive for two patients. The patients with an inverted J sign continued to be positive for this sign. Five patients were positive for subluxation upon extension before the operation, but all patients were negative for this after the operation. None of the patients presented any new episode of dislocation of the patella. All of them stated that they were satisfied: five gave a satisfaction score of 9 and two, a score of 10. All of them said that they would undergo the operation again. Only one patient presented a postoperative complication: dehiscence of the wound.
CONCLUSION:
Reconstruction of the medial patellofemoral ligament using the quadriceps tendon, combined with reconstruction of the medial patellotibial ligament using the patellar tendon, was technically safe and presented good objective and subjective clinical results in this case series with a short follow-up.
Keywords:
Joint instability; Patellofemoral joint/surgery; Patella; Orthopedic procedures
RESUMO
OBJETIVO:
Descrever técnica cirúrgica de reconstrução anatômica do LPFM com tendão quadricipital combinada com a reconstrução do LPTM com tendão patelar e apresentar os resultados iniciais em uma série de casos.
MÉTODO:
Foi aplicada a técnica proposta em uma série de casos de pacientes do Grupo de Joelho do HC-IOT diagnosticados com instabilidade patelofemoral e com indicação de tratamento cirúrgico. No pré e pós-operatório foram avaliados: amplitude de movimento (ADM), teste da apreensão, teste da translação lateral, teste da inclinação patelar, sinal do J invertido, subluxação em extensão, dor a compressão da patela e dor a contração do quadríceps. No pós-operatório também foi perguntado aos pacientes se houve novo episódio de luxação, qual o grau de satisfação com a cirurgia (escala de zero a 10) e se passariam pela cirurgia novamente.
RESULTADOS:
Foram operados sete joelhos em sete pacientes e a média de seguimento foi de 5,46 meses (±2,07). Tivemos quatro pacientes com apreensão no pré-operatório que não tinham apreensão no pós-operatório. O teste de translação lateral foi normalizado em todos os pacientes enquanto o teste da inclinação patelar permaneceu positivo em dois pacientes. Os pacientes com J invertido permaneceram com o sinal positivo. A subluxação em extensão, presente no pré-operatório em cinco pacientes, foi negativa em todos no pós-operatório. Nenhum paciente apresentou novo episódio de luxação da patela. Todos responderam estar satisfeitos. Cinco pacientes referiram satisfação 9 e dois referiram 10. Todas passariam novamente pela cirurgia. Apenas uma paciente apresentou complicação pós-operatória, deiscência de ferida.
CONCLUSÃO:
A reconstrução combinada do LPFM com tendão quadricipital com a reconstrução do LPTM com tendão patelar é tecnicamente segura e apresentou bons resultados clínicos objetivos e subjetivos nesta série de caso de curto seguimento.
Palavras-chave:
Instabilidade articular; Articulação patelofemoral/cirurgia; Patela; Procedimentos ortopédicos
Introduction
Lateral dislocation of the patella is responsible for 2-3% of all knee injuries and is the second biggest cause of hemarthrosis.11. Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21(3):499-519.
The stability of the patellofemoral joint is maintained through complex interactions between active, passive and static stabilizers.
The medial ligaments responsible for maintaining the stability of the patellofemoral joint are the medial patellofemoral ligament, medial patellotibial ligament and medial patellomeniscal ligament.
There have been many studies on the medial patellofemoral ligament (MPFL) and its anatomical and biomechanical characteristics.22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6.,33. Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):7-12.,44. Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121-7.,55. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.,66. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93.,77. Steensen RN, Dopirak RM, McDonald WG 3rd. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32(6):1509-13.,88. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215-20.,99. Tuxoe JI, Teir M, Winge S, Nielsen PL. The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):138-40.and1010. Feller JA, Feagin JA Jr, Garrett WE Jr. The medial patellofemoral ligament revisited: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):184-6. However, little is known about the medial patellotibial ligament (MPTL) and medial patellomeniscal ligament (MPML).22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6.,33. Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):7-12.,55. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.and66. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93.
The initial biomechanical studies, in the 1990s, which evaluated the contribution of the medial ligaments in restricting lateralization of the patella showed that the MPFL contributed 50-60% of the medial restriction during the initial flexion (flexion of between 0° and 30°).44. Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121-7.,55. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.and66. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93. The contributions of the secondary restrictors have varied according to the study: for the MPTL from 0% to 24%; and for the MPML from 8% to 38%.22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6.,55. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.and66. Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93. However, in a more recent study, Philippot et al.22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6. demonstrated that the contributions that the MPTL and MPML make toward restriction of lateral translation increased from 26% when the joint was extended to 46% at flexion of 90°. Furthermore, the influence of the MPTL and MPML at flexion of 90° was found to be 72% in relation to patellar tilt and 92% in relation to patellar rotation.22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6. In a clinical study, Garth et al.1111. Garth WP Jr, Connor GS, Futch L, Belarmino H. Patellar subluxation at terminal knee extension: isolated deficiency of the medial patellomeniscal ligament. J Bone Joint Surg Am. 2011;93(10):954-62. observed that clinical and arthroscopic subluxation was present in patients who only had injuries to the MPML, when the knee was extended. Thus, the MPTL and MPML are important in maintaining the normal kinematics of the patellofemoral joint across the entire range of motion, and especially at higher degrees of flexion.
Surgical treatment usually consists of a combination of reconstruction of the injured MPFL with an adjuvant procedure for improving the alignment and congruence of the patellofemoral joint. Several types of graft for reconstructing the MPFL with good results have been described.1212. Hernandez AJ, Favaro E, Almeida A, Bonavides A, Demange MK, Camanho GL. Reconstruction of the medial patellofemoral ligament in skeletally immature patients: description of technique. Tech Knee Surg. 2009;8(1):42-6.,1313. Camanho GL, Bitar AC, Hernandez AJ, Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23(1), 108.e1-e4.and1414. Farr J, Schepsis AA. Reconstruction of the medial patellofemoral ligament for recurrent patellar instability. J Knee Surg. 2006;19(4):307-16. It is important to have different types of graft with similar results in order to make it possible to individualize the treatment and to perform revision on the reconstruction.
In a systematic review on the complications arising from reconstruction of the MPFL alone, the complication rate found was 26.1%. Clinical failures that presented subluxation or dislocation occurred in 3.7% of the cases. Alterations seen in physical examinations, such as positive apprehension test, patellar hypermobility or episodes of feelings of instability in the knee operated, occurred in 8.3% of the cases. Thus, objective or subjective instability persisted in 12% of the cases.1515. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916-23. We put forward the hypothesis that this subluxation might result from progressive slackening of the MPFL due to higher stress subsequent to its reconstruction. Reconstruction of one of the secondary restrictor ligaments (MPTL or MPML) may diminish the stress on the MPFL and improve the functional results. The MPTL may decrease the angle of the quadriceps (Q angle), thus improving patellar excursion without causing as many changes to the kinematics of the tibiofemoral joint as would medialization osteotomy of the anterior tibial tuberosity (ATT), which is the method used today for decreasing the Q angle.1616. Mani S, Kirkpatrick MS, Saranathan A, Smith LG, Cosgarea AJ, Elias JJ. Tibial tuberosity osteotomy for patellofemoral realignment alters tibiofemoral kinematics. Am J Sports Med. 2011;39(5):1024-31. In children, when it is not possible to perform osteotomy to correct risk factors, reconstruction of these secondary ligaments becomes even more important. There have been some descriptions of series of cases of MPFL reconstruction combined with MPTL reconstruction, with good results.1717. Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23(4):465-70.,1818. Giordano M, Falciglia F, Aulisa AG, Guzzanti V. Patellar dislocation in skeletally immature patients: semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1594-8.,1919. Ebied AM, El- Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):926-32.,2020. Brown GD, Ahmad CS. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg. 2008;21(4):328-32.and2121. Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298-306. Series of cases of MPTL reconstruction using the patellar tendon combined with procedures other than MPFL construction (lateral release of the retinaculum, advancement of the vastus medialis obliquus and medial retinaculum, and osteotomy of the ATT) also exist.2222. Myers P, Williams A, Dodds R, Bulow J. The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27(5):575-9.,2323. Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37(9):1814-20.and2424. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, et al. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2491-8. The objectives of the present study were to describe a surgical technique for anatomical reconstruction of the MPFL using the quadriceps tendon, combined with reconstruction of the MPTL using the patellar tendon, and to present the initial results from a series of cases.
Materials and methods
This study was approved by our institution's ethics committee under the number CEP 333/13, and all the patients signed a consent statement in order to participate.
The proposed technique was applied to a series of cases of patients seen by the Knee Group of Hospital das Clínicas, Institute of Orthopedics and Traumatology (HC-IOT), who were diagnosed as presenting patellofemoral instability with an indication for surgical treatment. All the patients had a clinical diagnosis of patellar dislocation, with at least two episodes.
The indications for combined reconstruction of the MPFL and MPTL were:
- Subluxation in extension (lateral and proximal displacement of the patella with contraction of the quadriceps, with the knee extended). - Instability in flexion (spontaneous dislocation or positive lateral translation test with the knee flexed). - Hyperextension of the knee with ligament laxity. - Open growth plate in association with predisposing factors (increased Q angle, high patella and trochlear dysplasia).
The following were evaluated before and after the operation: range of motion (ROM), apprehension test, lateral translation test, patellar inclination test, inverted J sign, subluxation in extension, pain on compression of the patella and pain on contraction of the quadriceps. The following predisposing factors were evaluated using magnetic resonance imaging: Q angle (TT-TG: distance of the patellar tendon from the trochlear throat); high patella (modified Insall-Salvati index, Caton-Deschamps index and length of the patellar tendon); and trochlear dysplasia (Dejour classification). After the operation, the patients were asked whether there had been any new episode of dislocation; what their degree of satisfaction with the surgery was (scale from 0 to 10); and whether they would undergo the operation again (yes or no). The surgical complications were also evaluated.
Surgical reconstruction technique:
- Skin incisions: Two small anterior incisions, each measuring 2-3 cm (minimally invasive technique), were made in order to harvest quadriceps and patellar grafts, and an incision of 1-2 cm was made in the medial epicondyle in order to insert the MPFL in the femur. When additional procedures were indicated and required wider exposure, an anterior incision of 8 cm was made (open technique). - Harvesting of the quadriceps graft (Fig. 1, Fig. 2 and Fig. 3)1212. Hernandez AJ, Favaro E, Almeida A, Bonavides A, Demange MK, Camanho GL. Reconstruction of the medial patellofemoral ligament in skeletally immature patients: description of technique. Tech Knee Surg. 2009;8(1):42-6.: An incision of 3 cm was made proximally to the patella. Using a scalpel blade, a strip of 8 mm in width from the medial portion of the quadriceps tendon containing the superficial portion of the quadriceps (in relation to the rectus femoris) was cut out, while its patellar insertion was maintained. The distal extremity of the graft was carefully partially detached from the patella, as far as the transition between the upper and middle thirds of the patellar height. Two adjuvant stitches were made in the periosteum using slowly absorbable thread, in order to maintain the insertion.
Grafts harvested from the patellar and quadriceps tendons by means of the minimally invasive technique.
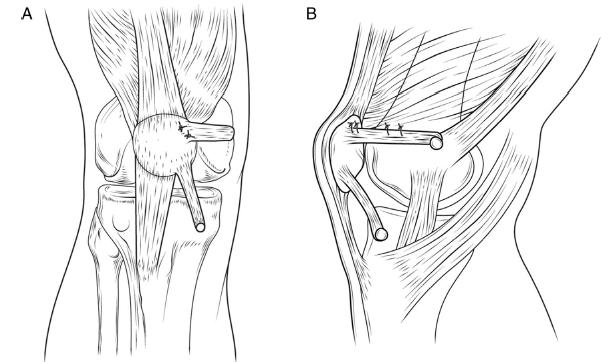
- Harvesting of the patellar graft (Fig. 1,Fig. 2 and Fig. 3)1313. Camanho GL, Bitar AC, Hernandez AJ, Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23(1), 108.e1-e4.: A medial incision was made in the patellar tendon between the lower pole of the patella and the anterior tuberosity of the tibia. Dissection was performed layer by layer down to the patellar peritendon, and a vertical incision was then made in its middle third. Using a scalpel blade, a 6-mm strip from the middle third of the patellar tendon was separated out and deinserted from the anterior tuberosity of the tibia. The origin of the patellar tendon was then detached proximally and superiorly and it was maintained in the distal third of the patella. - Insertion of the MPFL in the femur (Fig. 4A and B): The free proximal end was rotated through 90° and was passed under the medial retinaculum through the incision. The insertion point was between the medial epicondyle and the tubercle of the adductors, at the radiographic point.2525. Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801-4. A 5-mm anchor was fixed at this point. IN patients with an open growth plate, a 3.5-mm anchor was used and its insertion was in the distal epiphysis of the femur.2626. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58-63.
(A) Illustration of reconstruction of the MPFL using a graft from the quadriceps tendon and of the MPTL using a graft from the patellar tendon, in anterior view. (B) Illustration of reconstruction of the MPFL using a graft from the quadriceps tendon and of the MPTL using a graft from the patellar tendon, in mediolateral view.
- Insertion of the MPTL (Fig. 4A and B): The free end was passed under the medial reticulum toward the proximal tibia. A 5-mm anchor was fixed in the tibia, 1.5-2.5 cm below the joint line and 1.5 and 2.5 cm medially to the patellar tendon, which formed an angle of 20-25° with the patellar tendon.33. Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):7-12.and55. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65. In patients with an open growth plate, a 3.5-mm anchor was used, with an angle of 20-25° in relation to the patellar tendon, fixed just above the growth plate, in the proximal epiphysis of the tibia, so that its tensioning would be maintained during growth. Since the insertion in the tibial plateau was close to the growth plate scar, the fixation of the graft close to the growth plate reconstituted the anatomy of the MPTL well in adulthood. - Tensioning and fixation of the grafts (Fig. 4A and B): The patellar tendon was firstly fixed at the point described for the MPTL. The knee was positioned at 90° of flexion, which is the position of greatest tension and contribution of the MPTL to the lateral restriction,22. Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6. and also a position at which the patella is well reduced between the condyles. The MPTL was placed under traction with sufficient tension to contribute toward maintaining the patella in this position. It was important to place the graft under tension similar to that of the remnant patellar tendon, so that they could act synergistically over the entire range of motion. Overtensioning of the tendon also needed to be avoided so as not to cause an increase in pressure in the patellofemoral compartment.2727. Beck P, Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557-63. The graft was then sutured to the anchor that had previously been fixed in the MPTL. The knee was then placed at 30° of flexion, such that the patella was positioned at the trochlea. The quadriceps graft was placed under sufficient traction to keep the patella at a reduced position. With this degree of tension, the patella needed to be capable of making a mediolateral excursion of one to two quadrants, and it was important that the graft was not overtensioned, for the reasons mentioned earlier.2828. Beaty C. Campbell's operative orthopaedics. 11th ed. Elsevier; 2009. Lastly, two or three stitches were inserted between the quadriceps graft of the MPFL and the vastus medialis, for dynamism.
Additional procedures (shortening of the patellar tendon, lateral retinacular release and stretching of the quadriceps) were performed concomitantly in accordance with the predisposing factors.2929. Dejour D, Saggin P. In: Scott WN, editor. Disorders of the patellofemoral joint. 5th ed. Philadelphia: Elsevier/Churchill Livingstone; 2012. p. 592-623.
After the operation, the patients used immobilization in extension for walking, from the first postoperative day until completion of six weeks after the operation. Passive movement was made through physiotherapy and at home under guidance from a physiotherapist, with progression only limited by pain.
Results
Seven knees were operated, in seven patients of mean age 15.4 years (all of them female): six right knees and one left knee.
The evaluation on predisposing factors and surgical indications is shown in Table 1. The mean length of the patellar tendon was 47.57 mm (±10.78 mm). Two patients had lengths of more than 52 mm. The mean for the modified Insall-Salvati index was 1.84 (±0.31), and two of the patients had indexes above normal values (i.e. >2). The mean for the Caton-Deschamps index was 1.39 (±0.30), and five patients had indexes above normal values (i.e. >1.2). The mean TT-TG distance was 1.6 cm (±0.44 cm), and four patients had values greater than 1.5 cm. Three patients presented high-grade trochlear dysplasia (B, C or D). The main indications for combined reconstruction of the MPFL and MPTL were subluxation in extension, open growth plate in association with predisposing factors and instability in flexion, in decreasing order of frequency (Table 1).
In the preoperative evaluation, only one patient did not have a complete range of motion and presented contracture in flexion; four had a positive apprehension test; all the patients presented abnormalities in the lateral translation test; only one presented normal values in the patellar tilt test; two patients presented the inverted J sign; only one did not have subluxation in extension; four had pain upon compression of the patella; and four presented pain upon compression of the quadriceps (Table 2).
The mean length of follow-up was 5.46 months (±2.07). The four patients with positive apprehension tests before the operation did not show this after the operation. The lateral translation test results became normal in all the patients, while the patellar tilt test remained positive in the cases of two patients. The patients with a positive inverted J sign continued to present this, but because this sign is related to an abnormal path for the patella caused by high-grade trochlear dysplasia, it was already expected that this sign would be maintained in the patients with high-grade dysplasia, given that no procedure for correcting the trochlear dysplasia was undertaken. The subluxation in extension that was present before the operation in five patients was not present in any patient after the operation. In relation to pain, among the four patients with preoperative pain, three showed improvement of pain and one patient who had not had pain before the operation started to present it (Table 2).
None of the patients presented any new episode of patella dislocation. All of them said that they were satisfied. Five patients rated their satisfaction as 9 and two as 10. All of the patients said that they would go through the surgery again.
Only one patient presented any postoperative complication, which consisted of dehiscence of the wound. This patient required two surgical debridement procedures and new suturing of the skin and subcutaneous tissue, for healing to take place.
Discussion
The technique described here has the advantages that it enables anatomical reconstruction of the MPFL and MPTL and tensioning of the grafts at different degrees of flexion, thereby respecting the function of each ligament. In addition, maintenance of the patellar insertion of the quadriceps tendon and patellar tendon avoids the need to use synthesis material at the site, or perforation, which possibly would have led to fracturing of the patella.1515. Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916-23.,3030. Lippacher S, Reichel H, Nelitz M. Patellar fracture after patellar stabilization. Orthopade. 2010;39(5):516-8.and3131. Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am. 2011;93(17), e97(1-8).
In reconstructions described previously, the distal insertions of the flexor tendons were maintained. These did not coincide with the insertions of either the MPTL or the MPML. The tibial insertion of the flexor tendons was located at distances of 41 ± 6.6 mm from the tibial plateau and 6.88 ± 1 mm medially to the patellar tendon. The MPTL was located between 15 and 20 mm medially to the patellar tendon, in adults.3232. Grassi CA, Fruheling VM, Abdo JC, De Moura MFA, Namba M, Da Silva JLV, et al. Estudo anatômico da inserç ão dos tendões flexores do joelho. Rev Bras Ortop. 2013;48(5):417-20. With free distal borders, the graft can be placed in an anatomical position. In addition, this allows tensioning of the MPFL and MPTL reconstructions at different angles of flexion. Because the positioning in previous descriptions was non-anatomical, only one instance of tensioning of the MPFL and MPTL at different angles of flexion was described.1717. Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23(4):465-70.
Furthermore, fixation of the MPTL in the proximal epiphysis of the tibia, and not in the proximal metaphysis of the tibia, reduces the risk of distal migration of the graft insertion over the course of growth, which would change its tensioning and functioning.3333. Kupczik F, Schiavon ME, Sbrissia B, Vieira L.de A., Bonilha Tde M. Migraç ão proximal da âncora na reconstruç ão do ligamento patelofemoral medial em pacientes esqueleticamente imaturos. Rev Bras Ortop. 2013;48(5):465-8. The principle of insertion in the epiphysis is analogous to that used in reconstructing the MPFL.2626. Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58-63.
Reconstruction of the MPFL together with the MPTL, using grafts from flexor tendons, has also produced proven good results in five case series totaling 74 patients.1717. Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23(4):465-70.,1818. Giordano M, Falciglia F, Aulisa AG, Guzzanti V. Patellar dislocation in skeletally immature patients: semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1594-8.,1919. Ebied AM, El- Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):926-32.,2020. Brown GD, Ahmad CS. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg. 2008;21(4):328-32.and2121. Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298-306. The difference in our proposal lies only in the grafts used. Use of grafts from the patellar and quadriceps tendons for reconstructing the MPFL is already well known and disseminated. Use of the patellar tendon for reconstructing the MPTL alone has also been described.2222. Myers P, Williams A, Dodds R, Bulow J. The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27(5):575-9.,2323. Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37(9):1814-20.and2424. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, et al. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2491-8.
In our initial series of cases, the patients presented improvements in various signs and symptoms of patellar instability and only case of a minor complication of the operative wound. We believe that this case was due to use of inappropriate sizing and tissue pull-back in the incision. None of the patients presented recurrence of the patellar dislocation and all of them said that they were satisfied with the result.
Thus, we believe that our new proposal for combined MPFL reconstruction using the quadriceps tendon and MPTL reconstruction using the patellar tendon is technically safe, given that it consists of procedures and concepts used routinely by knee surgeons. In addition, its good results are predictable, based on the current evidence from the literature. The technique presented good objective and subjective clinical results in the series of the present study.
The major limitation of this study is its short follow-up, given that instability may recur at a later stage. For this reason, we chose not to include the Kujala score, which might have indicated results that were unsatisfactory given that many of the patients assessed were still undergoing rehabilitation. Thus, a longer follow-up is necessary in order to have a better assessment of the results over a longer period. The aim of this article was to present a new and alternative surgical technique for combined reconstruction of the MPFL and MPTL and its complication and success rates over the short term.
Conclusion
Combined reconstruction of the MPFL using the quadriceps tendon and of the MPTL using the patellar tendon is technically safe and presented good objective and subjective clinical results in this series of cases with a short follow-up.
References
-
1Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21(3):499-519.
-
2Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):331-6.
-
3Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(1):7-12.
-
4Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7(2):121-7.
-
5Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65.
-
6Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93.
-
7Steensen RN, Dopirak RM, McDonald WG 3rd. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32(6):1509-13.
-
8Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215-20.
-
9Tuxoe JI, Teir M, Winge S, Nielsen PL. The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):138-40.
-
10Feller JA, Feagin JA Jr, Garrett WE Jr. The medial patellofemoral ligament revisited: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):184-6.
-
11Garth WP Jr, Connor GS, Futch L, Belarmino H. Patellar subluxation at terminal knee extension: isolated deficiency of the medial patellomeniscal ligament. J Bone Joint Surg Am. 2011;93(10):954-62.
-
12Hernandez AJ, Favaro E, Almeida A, Bonavides A, Demange MK, Camanho GL. Reconstruction of the medial patellofemoral ligament in skeletally immature patients: description of technique. Tech Knee Surg. 2009;8(1):42-6.
-
13Camanho GL, Bitar AC, Hernandez AJ, Olivi R. Medial patellofemoral ligament reconstruction: a novel technique using the patellar ligament. Arthroscopy. 2007;23(1), 108.e1-e4.
-
14Farr J, Schepsis AA. Reconstruction of the medial patellofemoral ligament for recurrent patellar instability. J Knee Surg. 2006;19(4):307-16.
-
15Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916-23.
-
16Mani S, Kirkpatrick MS, Saranathan A, Smith LG, Cosgarea AJ, Elias JJ. Tibial tuberosity osteotomy for patellofemoral realignment alters tibiofemoral kinematics. Am J Sports Med. 2011;39(5):1024-31.
-
17Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23(4):465-70.
-
18Giordano M, Falciglia F, Aulisa AG, Guzzanti V. Patellar dislocation in skeletally immature patients: semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1594-8.
-
19Ebied AM, El- Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):926-32.
-
20Brown GD, Ahmad CS. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg. 2008;21(4):328-32.
-
21Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17(3):298-306.
-
22Myers P, Williams A, Dodds R, Bulow J. The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27(5):575-9.
-
23Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37(9):1814-20.
-
24Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, et al. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2491-8.
-
25Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801-4.
-
26Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med. 2013;41(1):58-63.
-
27Beck P, Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557-63.
-
28Beaty C. Campbell's operative orthopaedics. 11th ed. Elsevier; 2009.
-
29Dejour D, Saggin P. In: Scott WN, editor. Disorders of the patellofemoral joint. 5th ed. Philadelphia: Elsevier/Churchill Livingstone; 2012. p. 592-623.
-
30Lippacher S, Reichel H, Nelitz M. Patellar fracture after patellar stabilization. Orthopade. 2010;39(5):516-8.
-
31Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am. 2011;93(17), e97(1-8).
-
32Grassi CA, Fruheling VM, Abdo JC, De Moura MFA, Namba M, Da Silva JLV, et al. Estudo anatômico da inserç ão dos tendões flexores do joelho. Rev Bras Ortop. 2013;48(5):417-20.
-
33Kupczik F, Schiavon ME, Sbrissia B, Vieira L.de A., Bonilha Tde M. Migraç ão proximal da âncora na reconstruç ão do ligamento patelofemoral medial em pacientes esqueleticamente imaturos. Rev Bras Ortop. 2013;48(5):465-8.
-
☆
Work performed in the Laboratório de Investigação Médica do Sistema Músculo-Esquelético (LIM-41), Department of Orthopedics and Traumatology, School of Medicine, Universidade de São Paulo, São Paulo, SP, Brazil.
Publication Dates
-
Publication in this collection
jan-feb 2016
History
-
Received
22 Feb 2015 -
Accepted
19 Mar 2015