ABSTRACT
OBJECTIVE:
Sciatic pain secondary to lumbar disc herniation is a complex condition that is often highly limiting. The causes of pain in disc herniation are multifactorial. Two physiopathological mechanisms are involved in discogenic pain: mechanical deformation of nerve roots and a biochemical inflammatory component resulting from contact between the intervertebral disc and neural tissue, by way of the nucleus pulposus. The aim of this study was to evaluate the efficacy and safety of epidural blockade as therapy for bulging lumbar disc herniation.
METHODS:
A clinical study was conducted based on a retrospective and prospective survey. The blockade consisted of interlaminar puncture and bolus drug delivery. The number of procedures varied according to the clinical response, as determined through weekly evaluations and then 30, 90, and 180 days after the final session. A total of 124 patients who received one to five blockades were evaluated.
RESULTS:
The success rate (defining success as a reduction in sciatic pain of at least 80%) was 75.8%.
CONCLUSION:
The results demonstrated the therapeutic action of epidural blockade over the short term, i.e. in cases of acute pain, thus showing that intense and excruciating sciatic pain can be relieved through this technique. Because of the multifactorial genesis of sciatica and the difficulties encountered by healthcare professionals in treating this condition, epidural blockade can become part of therapeutic arsenal available. This procedure is situated between conservative treatment with an eminently clinical focus and surgical approaches.
Keywords:
Intervertebral disc displacement; Lumbar pain; Nerve block
RESUMO
OBJETIVO:
A dor ciática secundária a hérnia discal lombar é condição complexa e, muitas vezes, intensamente limitante. As causas de dor na herniação discal são multifatoriais. Na dor discogênica há envolvimento de dois mecanismos fisiopatológicos: a deformação mecânica das raízes nervosas e o componente bioquímico inflamatório, que resulta do contato do disco intervertebral, através do núcleo pulposo, com o tecido neural. O objetivo desta investigação foi verificar a eficácia e a segurança do bloqueio epidural como terapêutica em hérnias discais lombares protrusas.
MÉTODOS:
Empreendeu-se um ensaio clínico com base em levantamento retrospectivo e prospectivo. O bloqueio foi feito por punção interlaminar com administração de fármacos em bolo. O número de procedimentos variou conforme a evolução clínica, com avaliações semanais e, finalmente, aos 30, 90 e 180 dias da última sessão. Foram avaliados 124 pacientes, que receberam de um a cinco bloqueios.
RESULTADOS:
A taxa de sucesso (considerado como redução de no mínimo 80% na dor ciática) foi de 75,8%.
CONCLUSÃO:
Os resultados revelaram a ação terapêutica do bloqueio epidural em curto prazo - ou seja, na dor aguda - e demonstraram que a dor ciática intensa e excruciante pode ser aliviada com essa técnica. A gênese multifatorial da ciatalgia e as dificuldades encontradas pelos profissionais em seu tratamento permitem que o bloqueio epidural integre o arsenal terapêutico disponível. O procedimento insere-se entre o tratamento conservador, eminentemente clínico, e o cirúrgico.
Palavras-chave:
Deslocamento do disco intervertebral; Dor lombar; Bloqueio nervoso
Introduction
The 1st Brazilian Consensus on low back pain and sciatica11. Cecin HA. Consenso brasileiro sobre lombalgias e lombociatalgias. São Paulo, Uberaba: Sociedade Brasileira de Reumatologia, Faculdade de Medicina do Triângulo Mineiro; 2000. classifies low back pain according to mechanic-degenerative causes and non-mechanical causes (inflammatory, infectious, metabolic, and psychosomatic; fibromyalgia, myofascial syndrome). Mechanic-degenerative causes involve structural, biomechanical, or vascular changes, or an interaction of these.22. Bassam BA. Low back syndromes. The challenge of accurate diagnosis and management. Postgrad Med. 1990;87(4):209-15.,33. McQuay HJ, Moore RA. Epidural corticosteroids for sciatica. In: McQuay HJ, Moore RA, editors. An evidence-based resource for pain relief. New York: Oxford University Press; 1998. p. 216-8.and44. Nachemson AL, Andersson GB. Classification of low- back pain. Scand J Work Environ Health. 1982;8(2):134-6.
The great variability of clinical presentations reflects the location of pain at various levels.11. Cecin HA. Consenso brasileiro sobre lombalgias e lombociatalgias. São Paulo, Uberaba: Sociedade Brasileira de Reumatologia, Faculdade de Medicina do Triângulo Mineiro; 2000. Lumbar pain that radiates to the distal end of the lower limb and worsens after a Valsalva maneuver indicate a neurological origin; pain that radiates to the buttocks or posterior thigh and change with movement of the lumbar spine are likely to have a mechanical origin. Although vascular causes should also be investigated (claudication, temperature abnormalities, color, etc.),55. Cox JM. Dor lombar: mecanismo, diagnóstico e tratamento. 6th ed. São Paulo: Manole; 2002. p. 17-30, 377-507. properly characterized sciatica tends to be the main indicator of disc herniation.66. Deyo RA, Tsui- Wu YJ. Descriptive epidemiology of low- back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987;12(3):264-8.
Disc herniation results from biomechanical factors, degenerative changes, and situations that increase the pressure on the disc - developments that may or may not prove to be symptomatic.
The relationship between disc degenerative process, displacement of nuclear material, and low back pain remains controversial, although disc herniation tends to resolve spontaneously within the first month.77. Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185(1):135-41.and88. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-8. Through magnetic resonance imaging, disc degenerations have been evidenced in 34% of individuals aged 20-39 years, in 59% of those aged 40-50 years, and in 93% of those aged 60-80 years. Nonetheless, it is difficult to attribute low back pain to these findings.99. Nachemson AL, Jonsson E, editors. Neck and back: the scientific evidence of causes, diagnosis and treatment. Philadelphia: Lippincott Williams & Wilkins; 2000.
In mechanic-degenerative low back pain, epidural blocks are gaining ground in the non-surgical arsenal. Given the multifactorial genesis of sciatica, partly related to inflammatory processes due to the presence of degenerative disc material in the epidural space, the injection of an anti-inflammatory medication near the site of origin of pain is an indicated procedure.
Although some aspects regarding the efficacy of this treatment are yet to be elucidated, and despite the fact that non-uniform procedures were identified in the use of this method in patients with lumbar disc pathologies, particularly in cases of surgical treatment (which is indicated for approximately 1-2% of the patients),1010. Souza FAE, Pereira LV, Hortense P. Avaliação e mensuração da percepção da dor. In: Alves Neto O, Costa CMC, Siqueira JTT, Teixeira MJ, editors. Dor: princípios e prática. Porto Alegre: Artmed; 2009. p. 370-81. epidural blocks are one of the treatments that aim to prevent surgery.
This study aimed to verify the effectiveness and safety of epidural blocks as therapy in protruding lumbar disc herniations; estimate the success rate of the epidural block in protruding herniations; verify the association between the result of epidural block and the variables gender, age, number of blocks, and use of adjuvant medication; and compare the percentage of pain reduction after 30, 90, and 180 days of monitoring, for the following variables: result of epidural blocks, number of blocks, and the use of adjuvant medication.
Materials and methods
This was a clinical trial based on a retrospective (patient records and initial interviews) and prospective survey (interviews after the start of treatment).
Inclusion criteria comprised patients aged ≥18 years; with back pain that radiated to the posterior thigh, extending to the corresponding lower limb; pain whose pathway was compatible with the affected root and associated with sensory-subjective changes; and imaging exam diagnosing lumbar degenerative disc disease like protruding herniation. The exclusion criteria comprised previous surgery, chronic/inflammatory degenerative diseases, extruded or migrated disc herniation, local or systemic infectious diseases, neoplasms, and chronic pain secondary to epidural fibrosis (post-laminectomy syndrome).
The study included all patients who were attended to in 2012 at a pain clinic located in Campo Grande, MS, Brazil and met the inclusion criteria. Patients were retrospectively and prospectively evaluated at 30, 90, and 180 days after receiving an epidural block. They were clinically evaluated by the same examiner, both before and after the start of treatment using the visual analogue scale (VAS),1111. Centers for Diseases Control and Prevention (CDC). Epi Info 2011: version 7: programs for use by public health professionals. Atlanta: CDC; 2011. and underwent simple radiography and magnetic resonance imaging or computed tomography.
All blocks, made by the same anesthesiologist, followed a protocol. An interlaminar puncture performed at the site indicated by the imaging tests; needle bevel faced the side of the lesion. The following were administered in bolus: 0.5% bupivacaine (2 mL), methylprednisolone (80 mg), clonidine (30-75 µg, according to age and clinical conditions), morphine (1 mg), and saline solution qs (10 mL). Patient was sitting, and, when possible, placed in lateral decubitus. In case of pain manifestation, the most convenient antalgic position was adopted. Then, a 15-minute rest followed. In case of complete abolition of pain, the procedure was not repeated. In case of partial improvement, the procedure was repeated seven to ten days after the initial procedure. In case of partial clinical improvement, new blocks were performed (up to five).
Weekly serial clinical assessments were performed during the procedures and at 30, 90, and 180 days of the last (or only) block, following the same guidelines. At such times, general and specific physical examinations were performed, and the VAS was used by the patient and by the physician.
To compare the proportions of patients with or without pain reduction after block (outcome) and the independent variables (gender, age, number of blocks, and adjuvant medication), the chi-squared test and the chi-squared test for trend were used. The relative risks were calculated with their 95% confidence intervals.
Friedman's test for paired samples was used to compare the percentages of reduction of sciatica between the monitoring periods (30, 90, and 180 days). For the variables epidural block outcome, number of blocks, and adjuvant medication, the Kruskal-Wallis (three independent groups) and Mann-Whitney (two groups) tests were used.
A 5% significance level was adopted. Epi-Info, version 7,1212. Ayres M, Ayres JM, Ayres DL, Santos AAS. BioEstat: aplicações estatísticas das ciências bio-médicas: versão 5. 0. Belém: Sociedade Mamirauá; 2007. and Bio-Stat, version 5.31313. Olmarker K, Størkson R, Berge OG. Pathogenesis of sciatic pain: a study of spontaneous behavior in rats exposed to experimental disc herniation. Spine (Phila Pa 1976). 2002;27(12):1312-7. were used for statistical analysis.
The study was approved by the Ethics Committee on Human Research of the Universidade Federal do Mato Grosso do Sul (Protocol No. 2234, CAAE No. 0359.0.049.000-11, November 9, 2011). Informed consents were signed by the participants, and all other ethical requirements were met.
Results
Of the 129 selected patients with lumbar disc herniation, five left the study, resulting in 124 patients (62 men and 62 women), most of them were above 30 years old (Table 1; range: 18-79 years; mean: 50 ± 14 years). Of this total, 66.2% received one or two blocks (range: 1-5; mean: 2 ± 1).
Adjuvant medication was administered to 37.1% of patients, predominantly gabapentin and pregabalin. Corticosteroid therapy, alone or in combination with another medication, was seldom used (criterion: partial improvement associated with interruption of epidural blocks).
Considering the number of blocks and time elapsed since last (or only) block (Table 2), we observed that, at 30-day follow-up, most patients had had one block (35.7%); at 90-day, two blocks (35.2%); and at 180-day, three blocks (36.8%). Clinically, longer treatment periods require more blocks.
Success rate (≥ 80% reduction in sciatica) was of 75.8% (95% CI: 68.3-83.3%). Failure rate was of 24.2% - in 8.9%, block was ineffective, but without subsequent surgery because patients abandoned the protocol, opted for medical therapy or acupuncture, among other approaches; 12.9% received surgery due to adverse clinical outcomes after blockages; and 2.4% had recurrence after reduction of 95-100% of pain with the block.
There was no significant association between failure or success of the technique and sex, age, number of blocks, and use of adjuvant medication (Table 3).
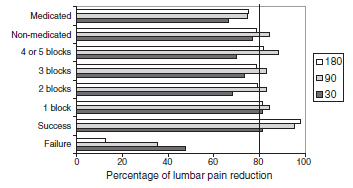
At 90-day post-block follow-up, the percentage of pain reduction increased when compared with 30-day post-block (Fig. 1). Patients who did not receive adjuvant medication had a higher percentage of sciatica reduction after the procedure.
Pain reduction in patients with lumbar disc herniation, according to the assessed variables and days elapsed after epidural block. Campo Grande, MS, 2012 (n = 124).
At 30-day follow-up, a smaller percentage of pain reduction was observed in patients submitted to two blocks (Fig. 1). For the 90- and 180-day follow-ups, this difference was not significant.
Regarding block treatment duration, 14 patients were assessed at 30 days: 14.3% were successful in reducing sciatica; in the 91 reevaluated at 90 days, an 87.9% success rate was observed; in the 19 reassessed at 180 days, a 63.2% rate of successful outcomes after last block was observed (Fig. 2).
Patients with lumbar disc herniation, according to duration of the treatment with epidural block and outcome. Campo Grande, MS, 2012 (n = 124).
Discussion
Pain due to lumbar disc disease, more specifically lumbar disc herniation, radiates along the lower limb and the injured nerve root pathway, with sensory and/or motor deficits secondary to neural dysfunction of that root.1414. Kawakami M, Weinstein JN, Chatani K, Spratt KF, Meller ST, Gebhart GF. Experimental lumbar radiculopathy. Behavioral and histologic changes in a model of radicular pain after spinal nerve root irritation with chromic gut ligatures in the rat. Spine (Phila Pa 1976). 1994;19(16):1795-802. Its pathophysiology involves both mechanical (compression of the lumbar root)1515. Winkelstein BA, Weinstein JN, DeLeo JA. The role of mechanical deformation in lumbar radiculopathy: an in vivo model. Spine (Phila Pa 1976). 2002;27(1):27-33.and1616. Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes inporcine cauda equina nerve roots. Spine (Phila Pa 1976). 1993;18(11):1425-32. and biochemical/inflammatory causes.1717. Mixter WJ. Rupture of the lumbar intervertebral disk: an etiologic factor for so-called sciatic pain. Ann Surg. 1937;106(4):777-87.
Although mechanical factors have been investigated since the description of this condition as an intervertebral disc disease by Mixter,1818. Omarker K, Myers RR. Pathogenesis of sciatic pain: role of herniated nucleus pulposus and deformation of spinal nerve root and dorsal root ganglion. Pain. 1998;78(2):99-105. inflammatory factors have recently been the subject of rigorous research in many experimental studies.1414. Kawakami M, Weinstein JN, Chatani K, Spratt KF, Meller ST, Gebhart GF. Experimental lumbar radiculopathy. Behavioral and histologic changes in a model of radicular pain after spinal nerve root irritation with chromic gut ligatures in the rat. Spine (Phila Pa 1976). 1994;19(16):1795-802.,1919. Kawakami M, Tamaki T, Matsumoto T, Kuribayashi K, Takenaka T, Shinozaki M. Role of leukocytes in radicular pain secondary to herniated nucleus pulposus. Clin Orthop Relat Res. 2000;376:268-77.,2020. Murata Y, Nannmark U, Rydevik B, Takahashi K, Olmarker K. Nucleus pulposus-induced apoptosis in dorsal root ganglion following experimental disc herniation in rats. Spine (Phila Pa 1976). 2006;31(4):382-90.and2121. Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, et al. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine (Phila Pa 1976). 2000;25(4):481-6.
There is evidence of immune system impairment in the reaction between nerve root and exposed nucleus pulposus. The glycosphingolipid (GSL) are cellular components of certain types of central and peripheral nervous system cells.2222. Svennerholm L, Boström K, Fredman P, Månsson JE, Rosengren B, Rynmark BM. Human brain gangliosides: developmental changes from early fetal stage to advanced age. Biochim Biophys Acta. 1989;1005(2):109-17.and2323. Brisby H, Balagué F, Schafer D, Sheikhzadeh A, Lekman A, Nordin M, et al. Glycosphingolipid antibodies in serum in patients with sciatica. Spine (Phila Pa 1976). 2002;27(4): 380-6. A study on disc herniation after discectomy indicated the presence of anti-GSL antibodies at high rates in 54% of patients. In non-operated patients with acute sciatica, high rates were observed in 71% of patients.2424. Vanni SMA. Injeção subaracnoidea inadvertida de corticoide em tratamento de dor crônica da coluna lombar: relato de caso. Rev Bras Anestesiol. 2004;54(6):821-5.
Therefore, compression-related mechanical, inflammatory, and immune components are involved in the genesis of sciatica
The pathophysiology of sciatica is characterized by the fact that the nucleus pulposus, which causes inflammation, causes the involvement of key inflammatory mediators and leads to demyelination, root ganglion ischemia, and increased endoneural pressure, with consequent reduction of nerve stimulus speed.2424. Vanni SMA. Injeção subaracnoidea inadvertida de corticoide em tratamento de dor crônica da coluna lombar: relato de caso. Rev Bras Anestesiol. 2004;54(6):821-5. This inflammatory reaction is followed by the immune response.
The use of corticosteroids associated with local anesthetics at the epidural site is common in several reference centers for the treatment of radiculopathy.2525. Cannon DT, Aprill CN. Lumbosacral epidural steroid injections. Arch Phys Med Rehabil. 2000;81 3 (Suppl. 1):S87-98.and2626. Castro AB. Tratamento da dor no Brasil: evolução histórica. Curitiba: Maio; 1999. In Brazil, the procedure has spread from the ideas of John Bonica apud Castro.2727. Carneiro AF, Alves Neto O. Corticoides espinais. In: Alves Neto O, Costa CMC, Siqueira JTT, Teixeira MJ, editors. Dor: princípios e prática. Porto Alegre: Artmed; 2009. p. 1320-6. Multimodal analgesia is recognized as the most adequate for the treatment of sciatica.2828. Scott DB. Bloqueio peridural. In: Rogers MC, Tinker JH, Covino BC, Longnecker DE, editors. Princípios e prática de anestesiologia. Rio de Janeiro: Guanabara Koogan; 1993. p. 955-71.
Lumbar puncture (both median and paramedian) is preferable to sacral puncture due to lower anatomical variation, as well as greater ease of location and deposition of the solution closer to the injury.2929. Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol. 1999;20(4):697-705. Use of fluoroscopy is controversial. Cannon and Aprill2626. Castro AB. Tratamento da dor no Brasil: evolução histórica. Curitiba: Maio; 1999. indicate the occurrence of route diversion in 18-52% of cases, depending on the route used and the experience of the professional. According to Johnson et al.,3030. Gonçalves BMV. Sobre o uso de corticosteroides por via peridural no tratamento das radiculopatias [tese]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 1976. results are positive in approximately 95% of cases, without using contrast and fluoroscopy.
When the desired effect is achieved with a single procedure, the need for repetition becomes unlikely.3131. Swerdlow M, Sayle-Creer WS. A study of extradural medication in the relief of the lumbosciatic syndrome. Anaesthesia. 1970;25(3):341-5. Nonetheless, there are patients who do not present an initial satisfactory response, but respond to a second or third procedure.2626. Castro AB. Tratamento da dor no Brasil: evolução histórica. Curitiba: Maio; 1999. Swerdlow and Sayle-Creer3232. Chen B, Stitik TP, Foye PM, Castro CP, Mehnert FJ. Epidural steroid injections; 2011. Available from: http://emedicine. medscape.com/article/325733-overview#showall [cited 24.09.12].
http://emedicine. medscape.com/article/3...
postulate that the solution should remain in place for more than two weeks. Chen et al.3333. Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow- up. Spine (Phila Pa 1976). 1992;17(10):1205-12. supported the two-week range of validity, but admitted repeating the procedure in a smaller interval if the clinical setting so requested. However, they did not agree with the idea of "standardizing" a series of three blocks without intercurrent clinical evaluation, despite the fact that experience shows the number of procedures to be typically three or four. These authors indicate that there is no support for this conduct in the literature.
In the present series, a success rate of 75.8% was achieved - 12.9% of patients subsequently underwent surgery: one patient had significant urinary retention for about 6 h after the procedure, with no associated analgesic benefit, and two had no success with the technique (puncture error or dura mater puncture), and procedure was aborted. These three patients were included in the group that was later referred to surgery.
Literature indicates that 10-15% of patients with sciatica secondary to a disc herniation undergo surgery,3434. Loy TT. Epidural steroid injection for sciatica: an analysis of 526 consecutive cases with measurements and the whistle test. J Orthop Surg (Hong Kong). 2000;8(1):39-44. which corresponded with the present findings (Table 3).
In accordance with existing international protocols, positive results required two blocks, on average. Adjuvant medication was administered to 37.1% of the patients (Table 1).
Epidural block is considered to be safe, presenting good cost-effectiveness and representing a minimally invasive treatment for sciatica, particularly in acute cases. This procedure should be used in clinical situations of pain crisis, and it also allows for the prognosis of future surgery.3535. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double- blind study. J Bone Joint Surg Am. 2000;82(11):1589-93.
In a prospective study, Riew et al.3636. Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, et al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five- year follow- up. J Bone Joint Surg Am. 2006;88(8):1722-5. concluded that patients with lumbar radiculopathy at one or two levels are candidates for epidural block in an attempt to avoid surgical procedures. Subsequently, Riew et al. observed that patients who had managed to avoid surgery due to epidural blocks for at least one year continued to show favorable development after five years.
Study limitations
The sample size (124 patients) and the selection of subjects (restricted to those who attended a single clinic located in Campo Grande, Brazil, in the period investigated) can be considered as inherent limitations to this study. For ethical reasons, the study did not include a control group, in order to avoid depriving any patients from the treatment administered.
Conclusions
Considering the limitations of this study, the procedure was proven to be effective, as it provided relief from sciatica in 75.8% of patients, and safe, as only three cases (2.4%) had technical problems (bladder function disorder in one puncture and error in two).
Best clinical outcome (87.9% success) with the largest number of patients (91) was observed at 90 days of follow-up.
There was no association between epidural blocks (success/failure) and the variables gender, age, number of procedures, and use of adjuvant medication.
References
-
1Cecin HA. Consenso brasileiro sobre lombalgias e lombociatalgias. São Paulo, Uberaba: Sociedade Brasileira de Reumatologia, Faculdade de Medicina do Triângulo Mineiro; 2000.
-
2Bassam BA. Low back syndromes. The challenge of accurate diagnosis and management. Postgrad Med. 1990;87(4):209-15.
-
3McQuay HJ, Moore RA. Epidural corticosteroids for sciatica. In: McQuay HJ, Moore RA, editors. An evidence-based resource for pain relief. New York: Oxford University Press; 1998. p. 216-8.
-
4Nachemson AL, Andersson GB. Classification of low- back pain. Scand J Work Environ Health. 1982;8(2):134-6.
-
5Cox JM. Dor lombar: mecanismo, diagnóstico e tratamento. 6th ed. São Paulo: Manole; 2002. p. 17-30, 377-507.
-
6Deyo RA, Tsui- Wu YJ. Descriptive epidemiology of low- back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987;12(3):264-8.
-
7Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185(1):135-41.
-
8Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(3):403-8.
-
9Nachemson AL, Jonsson E, editors. Neck and back: the scientific evidence of causes, diagnosis and treatment. Philadelphia: Lippincott Williams & Wilkins; 2000.
-
10Souza FAE, Pereira LV, Hortense P. Avaliação e mensuração da percepção da dor. In: Alves Neto O, Costa CMC, Siqueira JTT, Teixeira MJ, editors. Dor: princípios e prática. Porto Alegre: Artmed; 2009. p. 370-81.
-
11Centers for Diseases Control and Prevention (CDC). Epi Info 2011: version 7: programs for use by public health professionals. Atlanta: CDC; 2011.
-
12Ayres M, Ayres JM, Ayres DL, Santos AAS. BioEstat: aplicações estatísticas das ciências bio-médicas: versão 5. 0. Belém: Sociedade Mamirauá; 2007.
-
13Olmarker K, Størkson R, Berge OG. Pathogenesis of sciatic pain: a study of spontaneous behavior in rats exposed to experimental disc herniation. Spine (Phila Pa 1976). 2002;27(12):1312-7.
-
14Kawakami M, Weinstein JN, Chatani K, Spratt KF, Meller ST, Gebhart GF. Experimental lumbar radiculopathy. Behavioral and histologic changes in a model of radicular pain after spinal nerve root irritation with chromic gut ligatures in the rat. Spine (Phila Pa 1976). 1994;19(16):1795-802.
-
15Winkelstein BA, Weinstein JN, DeLeo JA. The role of mechanical deformation in lumbar radiculopathy: an in vivo model. Spine (Phila Pa 1976). 2002;27(1):27-33.
-
16Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes inporcine cauda equina nerve roots. Spine (Phila Pa 1976). 1993;18(11):1425-32.
-
17Mixter WJ. Rupture of the lumbar intervertebral disk: an etiologic factor for so-called sciatic pain. Ann Surg. 1937;106(4):777-87.
-
18Omarker K, Myers RR. Pathogenesis of sciatic pain: role of herniated nucleus pulposus and deformation of spinal nerve root and dorsal root ganglion. Pain. 1998;78(2):99-105.
-
19Kawakami M, Tamaki T, Matsumoto T, Kuribayashi K, Takenaka T, Shinozaki M. Role of leukocytes in radicular pain secondary to herniated nucleus pulposus. Clin Orthop Relat Res. 2000;376:268-77.
-
20Murata Y, Nannmark U, Rydevik B, Takahashi K, Olmarker K. Nucleus pulposus-induced apoptosis in dorsal root ganglion following experimental disc herniation in rats. Spine (Phila Pa 1976). 2006;31(4):382-90.
-
21Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, et al. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine (Phila Pa 1976). 2000;25(4):481-6.
-
22Svennerholm L, Boström K, Fredman P, Månsson JE, Rosengren B, Rynmark BM. Human brain gangliosides: developmental changes from early fetal stage to advanced age. Biochim Biophys Acta. 1989;1005(2):109-17.
-
23Brisby H, Balagué F, Schafer D, Sheikhzadeh A, Lekman A, Nordin M, et al. Glycosphingolipid antibodies in serum in patients with sciatica. Spine (Phila Pa 1976). 2002;27(4): 380-6.
-
24Vanni SMA. Injeção subaracnoidea inadvertida de corticoide em tratamento de dor crônica da coluna lombar: relato de caso. Rev Bras Anestesiol. 2004;54(6):821-5.
-
25Cannon DT, Aprill CN. Lumbosacral epidural steroid injections. Arch Phys Med Rehabil. 2000;81 3 (Suppl. 1):S87-98.
-
26Castro AB. Tratamento da dor no Brasil: evolução histórica. Curitiba: Maio; 1999.
-
27Carneiro AF, Alves Neto O. Corticoides espinais. In: Alves Neto O, Costa CMC, Siqueira JTT, Teixeira MJ, editors. Dor: princípios e prática. Porto Alegre: Artmed; 2009. p. 1320-6.
-
28Scott DB. Bloqueio peridural. In: Rogers MC, Tinker JH, Covino BC, Longnecker DE, editors. Princípios e prática de anestesiologia. Rio de Janeiro: Guanabara Koogan; 1993. p. 955-71.
-
29Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol. 1999;20(4):697-705.
-
30Gonçalves BMV. Sobre o uso de corticosteroides por via peridural no tratamento das radiculopatias [tese]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 1976.
-
31Swerdlow M, Sayle-Creer WS. A study of extradural medication in the relief of the lumbosciatic syndrome. Anaesthesia. 1970;25(3):341-5.
-
32Chen B, Stitik TP, Foye PM, Castro CP, Mehnert FJ. Epidural steroid injections; 2011. Available from: http://emedicine. medscape.com/article/325733-overview#showall [cited 24.09.12].
» http://emedicine. medscape.com/article/325733-overview#showall -
33Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow- up. Spine (Phila Pa 1976). 1992;17(10):1205-12.
-
34Loy TT. Epidural steroid injection for sciatica: an analysis of 526 consecutive cases with measurements and the whistle test. J Orthop Surg (Hong Kong). 2000;8(1):39-44.
-
35Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, et al. The effect of nerve root injections on the need for operative treatment of lumbar radicular pain: a prospective, randomized, controlled, double- blind study. J Bone Joint Surg Am. 2000;82(11):1589-93.
-
36Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, et al. Nerve root blocks in the treatment of lumbar radicular pain: a minimum five- year follow- up. J Bone Joint Surg Am. 2006;88(8):1722-5.
-
☆
Study conducted at Clínica de Dor, Campo Grande, MS, Brazil.
Publication Dates
-
Publication in this collection
Jul-Aug 2016
History
-
Received
05 Aug 2015 -
Accepted
25 Sept 2015