Abstract
Objective
To prospectively compare the clinical and laboratorial aspects of patients undergoing spine deformity surgery, using the acute normovolemic hemodilution technique with tranexamic acid, versus a control group with tranexamic acid alone, and to evaluate the influence of hemodilution in intraoperative bleeding and the need for homologous transfusion.
Materials and Methods
Comparative prospective study with patients aged between 12 and 65 years undergoing spine deformity surgery with the acute normovolemic hemodilution technique associated with tranexamic acid versus a control group to which only tranexamic acid (15 mg/kg) was administered. Laboratorial exams were performed and analyzed in three different moments.
Results
A total of 30 patients were included in the present study: 17 in the hemodilution group, and 13 in the control group. The mean duration of the surgery in the hemodilution group was longer. The number of levels submitted to surgery ranged from 7 to 16 in the hemodilution group, and from 4 to 13 in the control group. Osteotomy, predominantly of the posterior kind, was performed in 20 patients. There was more intraoperative bleeding in the control group. All patients were stable during the procedures. Only 6 participants needed homologous blood transfusion, mostly from the control group (p > 0.05).
Conclusion
There was no significant difference between the two groups regarding the need for blood transfusion and intraoperative bleeding. The severity of the deformity was the main determinant for homologous blood transfusion.
Keywords
hemodilution/methods; bleeding; autologous blood transfusion; spine; scoliosis
Resumo
Objetivo
Comparar de modo prospectivo os parâmetros clínicos e laboratoriais dos pacientes submetidos a hemodiluição normovolêmica aguda associada ao ácido tranexâmico com um grupo de controle que recebeu apenas ácido tranexâmico, durante cirurgia de correção de deformidades da coluna, e avaliar a influência da técnica de hemodiluição no sangramento perioperatório e a necessidade de transfusão de sangue homólogo.
Materiais e Métodos
Estudo prospectivo comparativo, com pacientes entre 12 e 65 anos submetidos a cirurgia para correção de deformidades da coluna vertebral, com a técnica de hemodiluição normovolêmica aguda associada ao ácido tranexâmico, versus grupo de controle com ácido tranexâmico isolado na dose de 15 mg/kg. Exames laboratoriais foram feitos e analisados em três momentos de avaliação diferentes.
Resultados
Participaram deste estudo 30 pacientes: 17 no grupo de hemodiluição e 13 no grupo de controle. O tempo médio de cirurgia foi maior para o grupo de hemodiluição. O número de níveis operados variou entre 7 e 16 no grupo de hemodiluição, e entre 4 e 13 no grupo de controle. Fez-se osteotomia, predominantemente posterior, em 20 pacientes. O valor médio de sangramento intraoperatório foi maior no grupo de controle. Os parâmetros clínicos se mantiveram estáveis durante todos os procedimentos. Apenas 6 pacientes necessitaram de transfusão sanguínea homóloga, a maioria dos quais pertencia ao grupo de controle (p > 0,05).
Conclusão
Não houve diferença significativa entre os dois grupos quanto à necessidade de transfusão e sangramento intraoperatório. A gravidade da deformidade foi o principal fator determinante da transfusão.
Palavras-chave
hemodiluição/métodos; sangramento; transfusão de sangue autóloga; coluna vertebral; escoliose
Introduction
Major surgeries, such as corrections of spinal deformities, can lead to increased bleeding. In order to control hemostasis, antifibrinolytic agents may be used, as well as intravenous volemic replacement with acellular solutions or with homologous or autologous blood derivatives.11 Baird EO, McAnany SJ, Lu Y, Overley SC, Qureshi SA. Hemostatic agents in spine surgery: A critical analysis review. JBJS Rev2015;3 (01):x
The homologous transfusion exposes the patient to the risk of pulmonary, allergic, hemolytic, immuno-allergic reactions and acquisition of infectious-contagious diseases.22 Maxwell MJ, Wilson MJA. Complications of blood transfusion. BJA Educ 2006;6(06):225-229 Autologous transfusion can be obtained with a low operational cost by previous donations, reutilization of the perioperative blood or acute normovolemic hemodilution (ANH), with which complications are avoided.33 Walunj A, Babb A, Sharpe R. Autologous blood transfusion. BJA Educ 2006;6(05):192-196
The ANH technique consists of blood withdrawal immediately before or after anesthetic induction,33 Walunj A, Babb A, Sharpe R. Autologous blood transfusion. BJA Educ 2006;6(05):192-196 followed by dilution with colloids and/or crystalloids without reducing the circulating volume.44 Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274 Its use has been indicated for surgeries with increased risk of bleeding.55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724
The objective of the present study was to prospectively compare the clinical and laboratory parameters of patients submitted to ANH associated with tranexamic acid with a control group using tranexamic acid alone, during corrective surgery of spinal deformities, in order to evaluate the influence of this technique in bleeding, the necessity of homologous transfusion and to identify adverse reactions and complications.
Materials and Methods
The present study was approved by the Ethics Committee of our institution through “Plataforma Brasil” with the number of the Certificate of Presentation for Ethical Appreciation (CAAE- 47883615.0.0000.0020).
A total of 30 patients undergoing elective surgery to correct deformities in the spine were included. They were aged between 12 and 65 years, and were divided according to the classification of the American Society of Anestesiology (ASA) as ASA I, II or III, without contraindications to the proposed anesthetic/surgical technique. The exclusion criteria were increased risk of coronary artery disease, cerebrovascular disease and valvulopathy, and patients with acute renal failure, bronchopneumonia and coagulopathies.
The patients were divided randomly between the ANH and control groups. All patients underwent total venous general anesthesia with remifentanil (0.1-0.3 mcg/kg/min), propofol (100-200 mcg/kg/min) and cisatracurium (attack: 0.15 mg/kg; maintenance: 03 mg/kg) when the potential evoked was not monitored. After anesthetic induction, every patient received 15 mg/kg of tranexamic acid and 0.1 mg/kg of morphine. The use of adjuvant drugs, as it did not interfere in the results, was left at the discretion of the anesthesiologist. The heart rate, neuromuscular blockade (train of four), pulse oximetry, cardioscopy, ST segment variation, invasive blood pressure and probe diuresis were monitored.
Laboratory tests (hemoglobin [Hb], hematocrit [Ht], prothrombin activation time [PAT], activated partial thromboplastin time [APTT], sodium, potassium, magnesium, ionic calcium, arterial blood gas, and lactate) were performed shortly after the anesthetic induction, after the blood collection for ANH, in the immediate postoperative period, and 24 hours later.
The ANH was performed in 17 patients, based on the Gross formula (Fig. 1), with collection between 80% and 100% of the volume to be withdrawn via peripheral artery or vein (maximum of 500 mL per bag collected).44 Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274,55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724 In case of hemodynamic instability, the ANH would be suspended. The bags were identified according to the order of collection, stored in a thermal box, and reinfused in the reverse order of collection. The hemodilution was performed in a 3:1 ratio with 0.9% saline solution and Ringer lactate. The additional volemic replacement was calculated to cover preoperative fasting, surgical loading (6 mL/kg/h)44 Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274,55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724 while the volume loss in the perioperative (3:1 ratio), was answer only if the urinary output < 0.5–1.0 mL/kg/h, and/or in case of hemodynamic instability.
Gross formula. Abbreviations: V, volume of blood to be withdrawn; EBV, estimated blood volume (65 mL/kg in women, and 70 mL/kg in men); Hto, initial hematocrit; Htf, final hematocrit; Htm, mean hematocrit (difference between Hto and Htf).
As for the surgical technique, the decision between pedicle instrumentation or association with osteotomies (of posterior elements, pedicle subtraction, or vertebral body resection [VCR]) was determined according to the deformity.
Homologous blood transfusion was performed only if the levels of Hb were < 7 mg/dL (or 9 mg/dL in the case of elderly patients or low cardiovascular reserve), with hemodynamic changes or persistence of bleeding.
The data were tabulated using the Microsoft Excel 2016 (Microsoft Corp., Redmond WA, US) software. For the comparison of the quantitative variables, the Student t-test or the nonparametric Mann-Whitney test were used. For the categorical variables, the Fisher exact test was used. The normality condition of the variables was evaluated using the Kolmogorov-Smirnov test. Values of p < 0.05 indicated statistical significance. The data were analyzed with the Statistical Package for the Social Sciences (SPSS, IBM Corp., Armonk, NY, US), version 20. The quantitative variables were described by means, medians, minimums, maximums and standard deviations. The qualitative variables were described by frequencies and percentages. After this analysis, a comparison was made with data from the literature.
Results
The sample consisted of 30 patients aged between 12 and 61 years (mean of 27.1 for the ANH group and of 21.2 for the control group; p > 0.05), predominantly female (76.6%). The main etiologies were adolescent idiopathic scoliosis (AIS) and congenital scoliosis (CS), as shown in Figure 2. Most patients denied comorbidities (76.6%). A mean of 622.6 mL of blood was withdrawn for hemodilution (400-940 mL). The clinical parameters remained stable during all of the procedures. The mean time of surgery for the ANH group was of 5.2 h, whereas for the control group it was of 4.4 h (p > 0.05). The number of levels operated ranged from 7 to 16 (mean: 10.7) for the ANH group, and from 4 to 13 for the control group (mean: 9.58). As for the number of instrumented levels, it ranged from 6 14 (mean 9.82) for the ANH group, and from 4 to 13 for the control group (mean: 9.66).
Etiology of spinal deformities submitted to surgery and their frequency. Abbreviations: AIS, adolescent idiopathic scoliosis; CS, congenital scoliosis; NMS, neuromuscular scoliosis; AS, adult scoliosis; KS, kyphoscoliosis; HL, hyperlordosis; TB, tuberculosis.
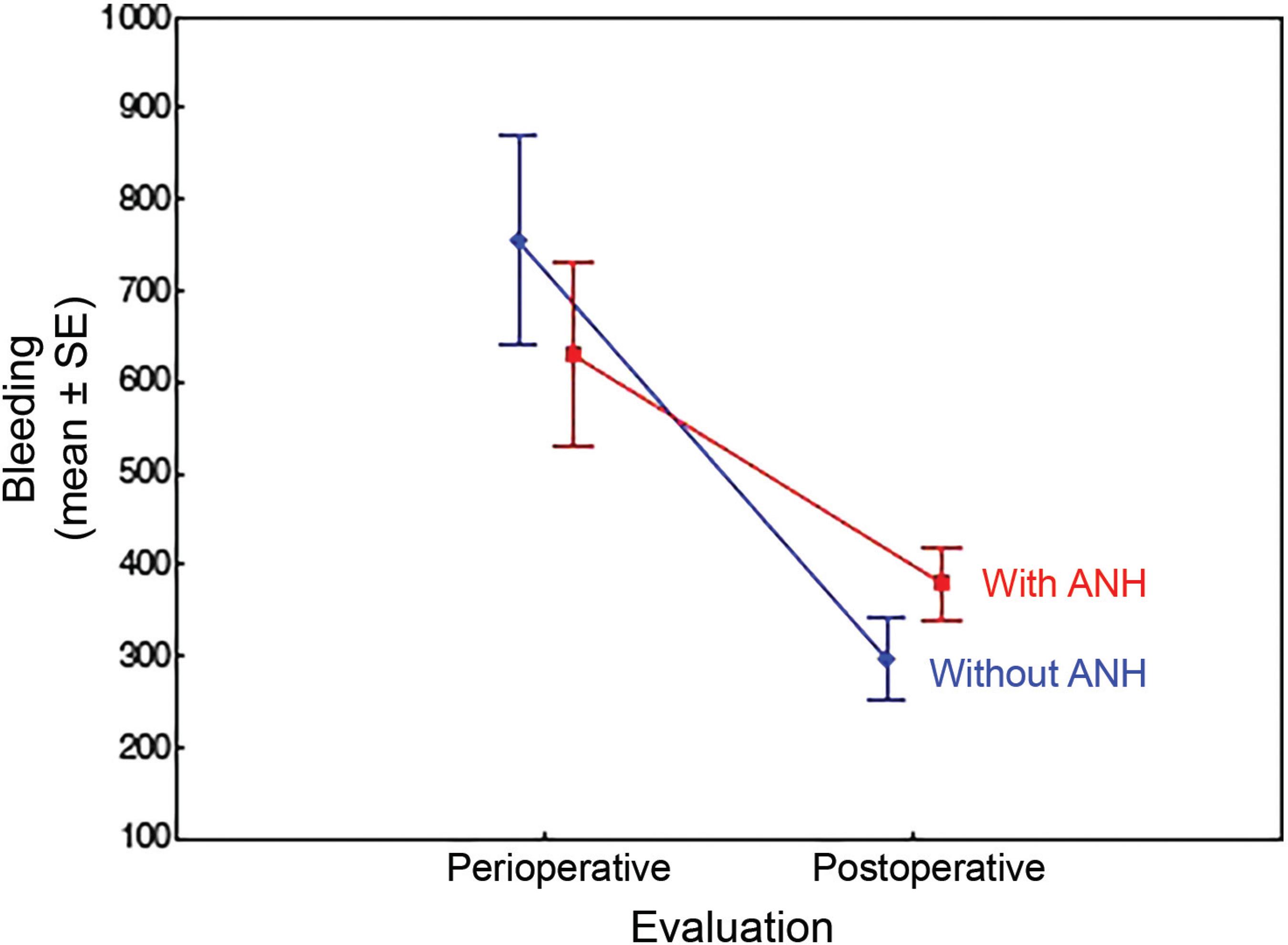
Twenty patients underwent osteotomy, as described in Table 1. For the purpose of analysis, each type of osteotomy was graded by magnitude: 0 for none; 1 point for each posterior osteotomy; 2 points for pedicle subtraction, and 3 points for each RCV, then they were divided between groups with scores ≤ 2 or > 3. In the isolated comparison between the groups, there was a greater mean of bleeding in the control group, but with greater variation, as evidenced in Figure 3. There was greater bleeding in both groups when the osteotomy was performed, with no statistical significance.
Intraoperative bleeding between groups. Non-parametric Mann-Whitney test (p = 0.934). Abbreviation: ANH, acute normovolemic hemodilution.
Regarding the number of operated levels, it was divided between groups with a limit higher or lower than 10. More bleeding occurred in the control group, with more levels (594 × 920 mL; p = 0.095), whereas in the case of less levels, the bleeding was lower and similar between both groups, which suggests that ANH would be effective in reducing bleeding in larger surgeries. The density of the implant (number of screws per level operated) was calculated, with 1 standing for the instrumentation of all operated pedicles, and 0 representing a surgery without instrumentation (Table 2). In the control group, the patients who were submitted to posterior osteotomy, had an increased need of transfusion (p > 0.05). The analysis of the ANH group showed that most of the patients did not require transfusion even after undergoing osteotomy (p > 0.05) (Table 3). The patients who were transfused had a higher mean of operated levels, especially in the control group (p > 0.05) (Table 4).
Density of the implant (number of screws in relation to the number of levels operated); comparison between the groups (p > 0.05)
The mean value of intraoperative bleeding was of 629.4 mL, and, postoperatively, it was of 379.11 mL for the ANH group, compared to 754.2 mL and 296.2 ml respectively for the control group, but without statistical significance. There was a lower perioperative-postoperative bleeding reduction in the ANH group, with p < 0.05 (Fig. 4).
Evaluation of perioperative bleeding versus postoperative: comparison between the groups. Abbreviation: ANH, acute normovolemic hemodilution; SE, standard error.
The laboratory tests were compared before and after surgery and between the groups, as represented in Table 5.
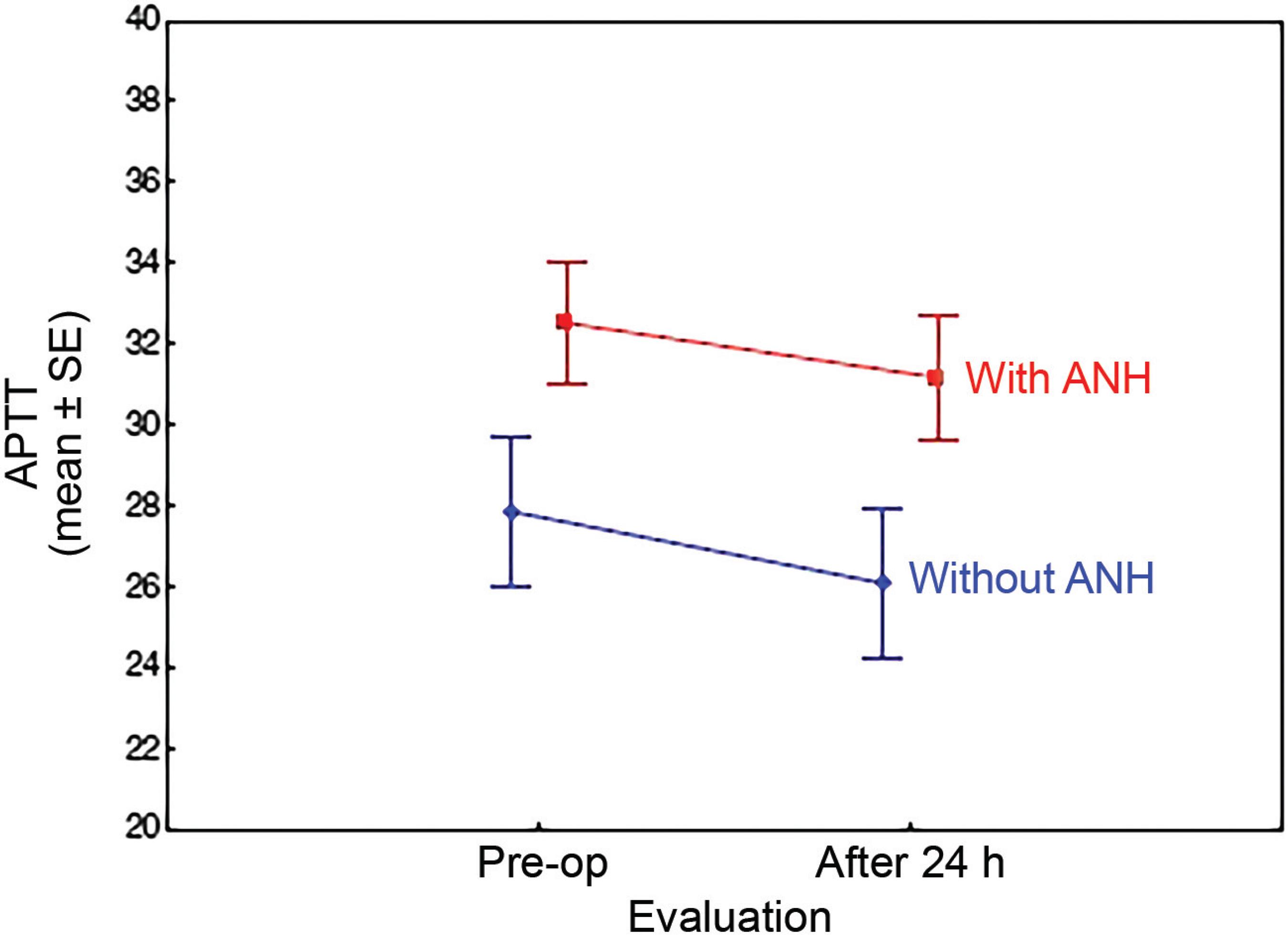
The coagulation profile was analyzed, and in both groups there was a widening of the PAT – with a greater difference before and after surgery in the ANH group (p = 0.014) –, and a decrease in the APTT, with a greater decrease in the control group (p = 0.793) (Figs. 5 and 6).
Prolongation of prothrombin activation time values in both groups in 24 h after surgery (p > 0.05). Abbreviations: ANH, acute normovolemic hemodilution; Pre-op, preoperative period; SE, standard error; PAT, prothrombin activation time.
Drop in the values of activated partial thromboplastin time in both groups 24 h after surgery (p > 0.05). Abbreviations: ANH, acute normovolemic hemodilution; Pre-op, preoperative period; SE, standard error; APTT, activated partial thromboplastin time.
There was a greater need for the use of local hemostatics in the control group compared to the ANH group (30.8% versus 5.9% respectively; p > 0.05). There was no statistical relevance for the need for transfusion according to the method applied, as shown in Figure 7. In general, patients requiring blood products had more severe deformities in 75% of the cases, and, consequently they had more levels to be addressed (7-14, mean: 11.1), plus osteotomies (1-9; mean: 4 versus 0-5; mean: 1.56; p < 0.05). This group also had high rates of perioperative bleeding (600-2,000 mL; mean: 1,050 mL), which was statistically significant (p = 0.007) when compared to the mean bleeding of the patients who did not receive transfusions (593.6 mL). For the purpose of comparison, the patients were divided into a group with AIS and a second group with other diagnoses. In this second group, the surgical time was longer (p <0.05), there was higher implant density (p = 0.07) and almost double the amount of posterior osteotomies performed (p > 0.05) (Table 6).
Need for transfusion compared to hemodilution (p = 0.360). Abbreviation: ANH, acute normovolemic hemodilution.
Comparison between relevant parameters of patients diagnosed with adolescent idiopathic scoliosis versus other deformities
Discussion
Bleeding control should be part of the initial surgical planning. The application of techniques can prevent the need for transfusion in patients undergoing AIS surgery.66 Verma RR, Williamson JB, Dashti H, Patel D, Oxborrow NJ. Homologous blood transfusion is not required in surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Br 2006;88 (09):1187-1191 The evolution of the surgical techniques enabled better results on terms of esthetics and function, but, the longer the procedure, the greater the perioperative bleeding77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123
8 Liu H, Yang C, Zheng Z, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. Spine 2015;40(08):570-579-99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126 and fibrinolysis, with consequent increase in hemorrhage, which generates a vicious circle that increases the morbimortality.99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126
In neuromuscular scoliosis (NMS) surgery, there is greater blood loss compared to AIS surgery,1010 Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555
11 Modi HN, Suh S-W, Hong J-Y, Song S-H, Yang J-H. Intraoperative blood loss during different stages of scoliosis surgery: A prospective study. Scoliosis 2010;5(01):16-16-1212 Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004;13(Suppl 1 ):S6-S17 mainly due to the greater extent of the arthrodesis,1111 Modi HN, Suh S-W, Hong J-Y, Song S-H, Yang J-H. Intraoperative blood loss during different stages of scoliosis surgery: A prospective study. Scoliosis 2010;5(01):16-16 with possible relation with the use of anticonvulsants and malnutrition. The estimated blood loss in the AIS surgery is of 1,300-2,200 mL, compared to 2,000-4,000 mL for the NMS surgery.1212 Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004;13(Suppl 1 ):S6-S17 In addition to hypotension, anemia and coagulopathy due to depletion, blood loss leads to an increase in the number of transfused units.1010 Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555 In the present study, patients with AIS had a mean bleeding of 561 mL, while in other deformities it was up to 2,000 mL (mean: 806 mL). Only one patient with AIS required transfusion.
Postoperative PAT and APTT prolongation is expected due to a dysfunction in platelet aggregation, which, especially in cases of NMS,1010 Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555,1313 Bosch P, Kenkre TS, Londino JA, Cassara A, Yang C, Waters JH. Coagulation Profile of Patients with Adolescent Idiopathic Scoliosis Undergoing Posterior Spinal Fusion. J Bone Joint Surg Am 2016;98 (20):e88 indicates coagulation overregulation in response to surgical stress and consumption of coagulation factors.1313 Bosch P, Kenkre TS, Londino JA, Cassara A, Yang C, Waters JH. Coagulation Profile of Patients with Adolescent Idiopathic Scoliosis Undergoing Posterior Spinal Fusion. J Bone Joint Surg Am 2016;98 (20):e88 In the present study, there was a decrease in the APTT and prolongation of the PAT in all patients, with no clinical repercussions, as verified by Oppitz and Stefani.55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724
Bleeding in deformity corrections is high because of the rich local vascularity, wide exposure and prolonged surgical time. The estimated blood loss is of 10-30 mL/kg.1111 Modi HN, Suh S-W, Hong J-Y, Song S-H, Yang J-H. Intraoperative blood loss during different stages of scoliosis surgery: A prospective study. Scoliosis 2010;5(01):16-16,1414 El-Dessouky MI, Waly SH, Nasr YM. Acute normovolemic hemodilution in spinal fusion surgery. Egypt J Anaesth 2011;31:249-254 There was a great deal of variability in the values found in the present study (200-2,000 mL), a fact that can be attributed to the etiology, the severity of the deformity, the operated levels, the osteotomies and the surgical time. Sex, advanced age, cardiovascular disease, extensive laminectomies and low Ht in the preoperative period 1515 Epstein NE. Bloodless spinal surgery: a review of the normovolemic hemodilution technique. Surg Neurol 2008;70(06):614-618,1616 Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868 did not result in increased bleeding.
Osteotomies are eventually needed to correct more severe deformities, especially in adults.1717 Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22(Suppl 2):S254-S264 Pedicle subtraction is associated with higher levels of blood loss (up to 3 L) due to the dissection of large-caliber epidural veins1818 Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239 and increased surgical time.88 Liu H, Yang C, Zheng Z, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. Spine 2015;40(08):570-579 The VCR is an option for severe and/or rigid deformities.1717 Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22(Suppl 2):S254-S264 Posterior osteotomies (also known as Smith Petersen osteotomies), which are considered easier and faster, have limited correction power (5º-20º), whereas pedicle subtraction can correct 30º-40º per level.77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123,1919 Hyun S-J, Rhim S-C. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc 2010;47(02):95-101 There are reports of higher bleeding rates with the posterior approach than with the anterior pproach.1212 Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004;13(Suppl 1 ):S6-S17 All patients in the present study had the procedure performed by the posterior approach.
In the present study, the patients submitted to osteotomies had a higher average bleeding rate, which in line with the literature, but the only statistically relevant data was the increased need for transfusion in the control group when the osteotomies by the posterior approach were performed. The ANH was not proven effective to avoid transfusion when the osteotomy was performed, but a trend towards statistical relevance was noticed in proportion to the increase in the aggressiveness of the approach.
Identifying risk factors, discontinuing medications such as acetylsalicylic acid, anti-inflammatory drugs and anticoagulants,11 Baird EO, McAnany SJ, Lu Y, Overley SC, Qureshi SA. Hemostatic agents in spine surgery: A critical analysis review. JBJS Rev2015;3 (01):x,2020 Blanchette CM, Wang PF, Joshi AV, Asmussen M, Saunders W, Kruse P. Cost and utilization of blood transfusion associated with spinal surgeries in the United States. Eur Spine J 2007;16(03):353-363 and even preoperative embolization of the vertebral body2121 Tuchman A, Mehta VA, Mack WJ, Acosta FL Jr. Novel application of pre-operative vertebral bodyembolization to reduce intraoperative blood loss during a three-column spinal osteotomy for non-oncologic spinal deformity. JClin Neurosci 2015;22(04):765-767 reduces hospitalization time, costs and bleeding. Thorough dissection of the periosteum and the use of electrocautery and hemostatic agents11 Baird EO, McAnany SJ, Lu Y, Overley SC, Qureshi SA. Hemostatic agents in spine surgery: A critical analysis review. JBJS Rev2015;3 (01):x,66 Verma RR, Williamson JB, Dashti H, Patel D, Oxborrow NJ. Homologous blood transfusion is not required in surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Br 2006;88 (09):1187-1191 may be adjuvants of autologous donation, ANH or hypotensive anesthesia.66 Verma RR, Williamson JB, Dashti H, Patel D, Oxborrow NJ. Homologous blood transfusion is not required in surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Br 2006;88 (09):1187-1191 Although Szpalski et al2222 Szpalski M, Gunzburg R, Sztern B. An overview of blood-sparing techniques used in spine surgery during the perioperative period. Eur Spine J2004;13(Suppl 1):S18-S27 and Urban et al2323 Urban MK, Beckman J, Gordon M, Urquhart B, Boachie-Adjei O. The efficacy of antifibrinolytics in the reduction of blood loss during complex adult reconstructive spine surgery. Spine 2001; 26(10):1152-1156 have shown that adequate evidence exists for their use, controlled hypotension is controversial in spinal surgery because it does not reduce intraoperative blood loss,1414 El-Dessouky MI, Waly SH, Nasr YM. Acute normovolemic hemodilution in spinal fusion surgery. Egypt J Anaesth 2011;31:249-254 and because of the risk of spinal cord injury due to reduced flow.77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123,2424 Yagi M, Hasegawa J, Nagoshi N, et al. Does the intraoperative tranexamic acid decrease operative blood loss during posterior 30 spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 2012;37(21):E1336-E1342 They also mention that the use of systemic and local hemostatic agents would be controversial.2222 Szpalski M, Gunzburg R, Sztern B. An overview of blood-sparing techniques used in spine surgery during the perioperative period. Eur Spine J2004;13(Suppl 1):S18-S27
The use of fibrinolytics gained popularity in the 1990s.1818 Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239,2525 Tayyab NA, Marillier MM, Rivlin M, et al. Efficacy ofaprotinin as a 31 blood conservation technique for adult deformity spinal surgery: a retrospective study. Spine 2008;33(16):1775-1781 In children with NMS, their use was effective in reducing bleeding and transfusion.1010 Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555,2626 Cole JW, Murray DJ, Snider RJ, Bassett GS, Bridwell KH, Lenke LG. Aprotinin reduces blood loss during spinal surgery in children. Spine 2003;28(21):2482-2485 Aprotinin inhibits anticoagulant enzymes, as well as the intrinsic pathway of coagulation and platelet aggregation.99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126,2525 Tayyab NA, Marillier MM, Rivlin M, et al. Efficacy ofaprotinin as a 31 blood conservation technique for adult deformity spinal surgery: a retrospective study. Spine 2008;33(16):1775-1781 Its use has been discontinued99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126,1010 Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555 due to increased mortality from acute myocardial infarction99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126 and acute renal failure,2525 Tayyab NA, Marillier MM, Rivlin M, et al. Efficacy ofaprotinin as a 31 blood conservation technique for adult deformity spinal surgery: a retrospective study. Spine 2008;33(16):1775-1781 although previous studies have shown reduced transfusion in heart, knee and hip surgeries99 Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126,1818 Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239,2525 Tayyab NA, Marillier MM, Rivlin M, et al. Efficacy ofaprotinin as a 31 blood conservation technique for adult deformity spinal surgery: a retrospective study. Spine 2008;33(16):1775-1781 and also despite the fact that they have been considered superior to tranexamic acid in pedicle osteotomy.1818 Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239
Tranexamic acid was administered to all patients in this study. It acts through the reversible binding of plasminogen with lysine,2424 Yagi M, Hasegawa J, Nagoshi N, et al. Does the intraoperative tranexamic acid decrease operative blood loss during posterior 30 spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 2012;37(21):E1336-E1342 it is considered safe, and is widely used in cardiac and urogynecological surgeries. In a retrospective study,2424 Yagi M, Hasegawa J, Nagoshi N, et al. Does the intraoperative tranexamic acid decrease operative blood loss during posterior 30 spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 2012;37(21):E1336-E1342 its use in AIS resulted in less bleeding and transfusion,2424 Yagi M, Hasegawa J, Nagoshi N, et al. Does the intraoperative tranexamic acid decrease operative blood loss during posterior 30 spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 2012;37(21):E1336-E1342 but it was not effective in cases of pedicle subtraction in adults.1818 Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239 Its use does not increase the morbimortality and the incidence of thromboembolic events.2727 da Rocha VM, de Barros AGC, Naves CD, et al. Use of tranexamic acid for controlling bleeding in thoracolumbar scoliosis surgery with posterior instrumentation. Rev Bras Ortop 2015;50(02):226-231
In the present study, the rate of homologous blood transfusion was of 20%, which is within the range of 8-36% reported by Purvis et al,2828 Purvis TE, Goodwin CR, De la Garza-Ramos R, et al. Effect of liberal blood transfusion on clinical outcomes and cost in spine surgery patients. Spine J 2017;17(09):1255-1263 who described multiple possible complications (increased mortality, hospital infections, prolonged hospitalization, besides the high cost),77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123,1616 Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868,2020 Blanchette CM, Wang PF, Joshi AV, Asmussen M, Saunders W, Kruse P. Cost and utilization of blood transfusion associated with spinal surgeries in the United States. Eur Spine J 2007;16(03):353-363,2929 Fischer ST, Schuroff AA, Vialle LR. Hemodiluição isovolumétrica no tratamento cirúrgico da escoliose idiopática. Rev Bras Ortop 1994;29(03):107-110 although no complications were reported. It was not possible to isolate a factor responsible for transfusion, but a variable association between operated levels, severity of the deformity, surgical time and osteotomies.
Autologous transfusion is considered safer,33 Walunj A, Babb A, Sharpe R. Autologous blood transfusion. BJA Educ 2006;6(05):192-196 and should be performed with donation prior to surgery (3 to 5 weeks, with limitations in the case of elderly and anemic patients),77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123 normovolemic hemodilution, cell preservation (high cost),77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123,1616 Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868,2828 Purvis TE, Goodwin CR, De la Garza-Ramos R, et al. Effect of liberal blood transfusion on clinical outcomes and cost in spine surgery patients. Spine J 2017;17(09):1255-1263 or hypervolemic hemodilution, which reduces the need for allogeneic transfusion1414 El-Dessouky MI, Waly SH, Nasr YM. Acute normovolemic hemodilution in spinal fusion surgery. Egypt J Anaesth 2011;31:249-254 by dilution in plasma or in macromolecule solutions, with increasing circulating volume.44 Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274 It is considered quick, easier, more stable and cheaper than the ANH.
In the ANH, the collected blood is diluted with acellular fluid in the ratio of 2-4:1,77 Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123,1616 Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868 leading to a reduction in perioperative blood loss with maintenance of the flow.33 Walunj A, Babb A, Sharpe R. Autologous blood transfusion. BJA Educ 2006;6(05):192-196
4 Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274-55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724 Many studies show that ANH reduces the need for homologous transfusion between 18% and 90%;55 Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724,2929 Fischer ST, Schuroff AA, Vialle LR. Hemodiluição isovolumétrica no tratamento cirúrgico da escoliose idiopática. Rev Bras Ortop 1994;29(03):107-110 however, in the present study, there was no statistical significance regarding this, perhaps due to the number of cases. The ANH is considered safe and effective in spinal surgery when there is an estimated loss higher than 1 L or 20% of blood volume.1616 Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868,2929 Fischer ST, Schuroff AA, Vialle LR. Hemodiluição isovolumétrica no tratamento cirúrgico da escoliose idiopática. Rev Bras Ortop 1994;29(03):107-110 There is a risk of extreme hemodilution (Ht < 20%), with risk of tissue ischemia, which is reversed with infusion of fresh plasma, according to McLaughlin.1414 El-Dessouky MI, Waly SH, Nasr YM. Acute normovolemic hemodilution in spinal fusion surgery. Egypt J Anaesth 2011;31:249-254 Its use in the pediatric population was tested in a 2004 prospective randomized study3030 Oliveira GS, Tenório SB, Cumino DO, et al. Acute normovolemic hemodilution in children submitted to posterior spinal fusion. Rev Bras Anestesiol 2004;54(01):84-90 with children undergoing posterior arthrodesis, which proved that the ANH is safe and able to reduce the need for transfusion without the complications related to anemia.3030 Oliveira GS, Tenório SB, Cumino DO, et al. Acute normovolemic hemodilution in children submitted to posterior spinal fusion. Rev Bras Anestesiol 2004;54(01):84-90 Tse et al3131 Tse EY, Cheung WY, Ng KF, Luk KD. Reducing perioperative blood loss and allogeneic blood transfusion in patients undergoing major spine surgery. J Bone Joint Surg Am 2011;93(13):1268-1277 have shown in their review that ANH, tranexamic acid, intrathecal morphine and modification of the operative techniques seem to be the best options to reduce perioperative bleeding and allogeneic blood transfusion. The use of ANH in this study aided in the control of bleeding, but not to the point of avoiding transfusion in an isolated manner.
Conclusion
The ANH technique associated with tranexamic acid has not been proven effective in reducing the need for homologous blood transfusion in corrective surgeries of spinal deformities, despite its tendency to reduce intraoperative bleeding, especially in cases that are considered more complex. The combined effect of the severity of the deformity, the osteotomies, and the number of operated/instrumented levels is a determinant for the need for transfusion, and the association of preoperative and intraoperative measures to control the bleeding should be considered in these cases. It is believed that a larger casuistry could prove its efficacy in comparison with isolated fibrinolytics.
-
*
Originally Published by Elsevier Editora Ltda.
References
-
1Baird EO, McAnany SJ, Lu Y, Overley SC, Qureshi SA. Hemostatic agents in spine surgery: A critical analysis review. JBJS Rev2015;3 (01):x
-
2Maxwell MJ, Wilson MJA. Complications of blood transfusion. BJA Educ 2006;6(06):225-229
-
3Walunj A, Babb A, Sharpe R. Autologous blood transfusion. BJA Educ 2006;6(05):192-196
-
4Oriani G, Pavesi M, Oriani A, Bollina I. Acute normovolemic hemodilution. Transfus Apheresis Sci 2011;45(03):269-274
-
5Oppitz PP, Stefani MA. Acute normovolemic hemodilution is safe in neurosurgery. World Neurosurg 2013;79(5-6):719-724
-
6Verma RR, Williamson JB, Dashti H, Patel D, Oxborrow NJ. Homologous blood transfusion is not required in surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Br 2006;88 (09):1187-1191
-
7Kim KT, Park KJ, Lee JH. Osteotomy of the spine to correct the spinal deformity. Asian Spine J 2009;3(02):113-123
-
8Liu H, Yang C, Zheng Z, et al. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. Spine 2015;40(08):570-579
-
9Khurana A, Guha A, Saxena N, Pugh S, Ahuja S. Comparison of aprotinin and tranexamic acid in adult scoliosis correction surgery. Eur Spine J 2012;21(06):1121 -1126
-
10Dhawale AA, Shah SA, Sponseller PD, et al. Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine 2012;37(09):E549-E555
-
11Modi HN, Suh S-W, Hong J-Y, Song S-H, Yang J-H. Intraoperative blood loss during different stages of scoliosis surgery: A prospective study. Scoliosis 2010;5(01):16-16
-
12Shapiro F, Sethna N. Blood loss in pediatric spine surgery. Eur Spine J 2004;13(Suppl 1 ):S6-S17
-
13Bosch P, Kenkre TS, Londino JA, Cassara A, Yang C, Waters JH. Coagulation Profile of Patients with Adolescent Idiopathic Scoliosis Undergoing Posterior Spinal Fusion. J Bone Joint Surg Am 2016;98 (20):e88
-
14El-Dessouky MI, Waly SH, Nasr YM. Acute normovolemic hemodilution in spinal fusion surgery. Egypt J Anaesth 2011;31:249-254
-
15Epstein NE. Bloodless spinal surgery: a review of the normovolemic hemodilution technique. Surg Neurol 2008;70(06):614-618
-
16Stehling L, Zauder HL. Acute normovolemic hemodilution. Transfusion 1991;31(09):857-868
-
17Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22(Suppl 2):S254-S264
-
18Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO. Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 2010;35(02):235-239
-
19Hyun S-J, Rhim S-C. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc 2010;47(02):95-101
-
20Blanchette CM, Wang PF, Joshi AV, Asmussen M, Saunders W, Kruse P. Cost and utilization of blood transfusion associated with spinal surgeries in the United States. Eur Spine J 2007;16(03):353-363
-
21Tuchman A, Mehta VA, Mack WJ, Acosta FL Jr. Novel application of pre-operative vertebral bodyembolization to reduce intraoperative blood loss during a three-column spinal osteotomy for non-oncologic spinal deformity. JClin Neurosci 2015;22(04):765-767
-
22Szpalski M, Gunzburg R, Sztern B. An overview of blood-sparing techniques used in spine surgery during the perioperative period. Eur Spine J2004;13(Suppl 1):S18-S27
-
23Urban MK, Beckman J, Gordon M, Urquhart B, Boachie-Adjei O. The efficacy of antifibrinolytics in the reduction of blood loss during complex adult reconstructive spine surgery. Spine 2001; 26(10):1152-1156
-
24Yagi M, Hasegawa J, Nagoshi N, et al. Does the intraoperative tranexamic acid decrease operative blood loss during posterior 30 spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 2012;37(21):E1336-E1342
-
25Tayyab NA, Marillier MM, Rivlin M, et al. Efficacy ofaprotinin as a 31 blood conservation technique for adult deformity spinal surgery: a retrospective study. Spine 2008;33(16):1775-1781
-
26Cole JW, Murray DJ, Snider RJ, Bassett GS, Bridwell KH, Lenke LG. Aprotinin reduces blood loss during spinal surgery in children. Spine 2003;28(21):2482-2485
-
27da Rocha VM, de Barros AGC, Naves CD, et al. Use of tranexamic acid for controlling bleeding in thoracolumbar scoliosis surgery with posterior instrumentation. Rev Bras Ortop 2015;50(02):226-231
-
28Purvis TE, Goodwin CR, De la Garza-Ramos R, et al. Effect of liberal blood transfusion on clinical outcomes and cost in spine surgery patients. Spine J 2017;17(09):1255-1263
-
29Fischer ST, Schuroff AA, Vialle LR. Hemodiluição isovolumétrica no tratamento cirúrgico da escoliose idiopática. Rev Bras Ortop 1994;29(03):107-110
-
30Oliveira GS, Tenório SB, Cumino DO, et al. Acute normovolemic hemodilution in children submitted to posterior spinal fusion. Rev Bras Anestesiol 2004;54(01):84-90
-
31Tse EY, Cheung WY, Ng KF, Luk KD. Reducing perioperative blood loss and allogeneic blood transfusion in patients undergoing major spine surgery. J Bone Joint Surg Am 2011;93(13):1268-1277
Publication Dates
-
Publication in this collection
14 Nov 2019 -
Date of issue
Sep-Oct 2019
History
-
Received
10 Dec 2017 -
Accepted
21 Feb 2018