Abstracts
BACKGROUND: Bariatric surgeries have been considered an alternative for treatment of morbid obesity. Some adverse events that people experience after the treatment frequently are the consequence of the lack of consistent knowledge associated with psychosocial factors that are related to the pre-surgery status of the patients. AIM: To evaluate psychosocial variables of 414 candidates for bariatric surgery from Clinical Hospital of Medical School at University of São Paulo, Ribeirão Preto, SP, Brazil. METHODS: Semi-structured interview, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI) and Binge Eating Scale (BES) were used. RESULTS: BMI was higher among patients who had no employment (p = 0.019). Female, patients who had a partner and patients with a BMI < 50 kg/m², all of them desired have a lower weight (p < 0.001). BAI scores were higher among patients who had no employment (p < 0.05) and higher among those with a BMI > 50 kg/m² (p < 0.05). BDI scores were higher among women (p < 0.05) and lower among those who had an employment (p < 0.01). No difference in BES was found. CONCLUSIONS: The data suggest that women showed higher indicators of anxiety and depression, suggesting that they had a more fragile psychological functioning with difficulties in coping with distress. Self-perception as well as skills and abilities, may reflect internal aspects of individual's personality. Patients who had an employment before surgery seemed have more emotional resources. So, they may feel less distress because the employment may protect them. Women and those who did not have an employment were more likely to experience depression symptoms. Furthermore, patients who did not have an employment and those with BMI> 50 kg / m² were more likely to experience anxiety symptoms.
Depression; Bariatric Surgery; Anxiety; Employment
RACIONAL: Operações bariátricas têm sido consideradas alternativa para o tratamento de obesidade mórbida. Alguns eventos adversos que as pessoas experimentam após o tratamento frequentemente são consequência da falta de conhecimento consistente associada a fatores psicossociais que estão relacionadas ao status pré-operatório dos pacientes. OBJETIVO: Avaliar as variáveis ?psicossociais de 414 candidatos ? cirurgia bari?trica do Hospital de Cl?nicas da Faculdade de Medicina da Universidade de S?o Paulo, Ribeir?o Preto, SP, Brasil. psicossociais de 414 candidatos à cirurgia bariátrica do Hospital de Clínicas da Faculdade de Medicina da Universidade de São Paulo, Ribeirão Preto, SP, Brasil. MÉTODOS: Foram utilizados entrevista semi-estruturada, Inventário de Depressão de Beck (BDI), Inventário de Ansiedade de Beck (BAI) e Binge Eating Scale (BES). RESULTADOS: IMC foi maior entre os pacientes que não tinham emprego (p = 0,019), do sexo feminino, os que tinham um parceiro e os pacientes com IMC <50 kg / m², todos eles desejando ter peso menor (p<0,001). Escores do BAI foram maiores entre os pacientes que não tinham emprego (p <0,05) e maior naqueles com IMC> 50 kg / m² (p <0,05). BDI foram mais altos entre as mulheres (p <0,05) e menores entre aqueles que tinham um emprego (p <0,01). Nenhuma diferença no BES foi encontrada. CONCLUSÕES: Os dados sugerem que as mulheres apresentaram indicadores mais elevados de ansiedade e depressão, sugerindo que elas tinham funcionamento psicológico mais frágil com dificuldades em lidar com a angústia. Auto-percepção, assim como competências e habilidades, podem refletir aspectos internos da personalidade do indivíduo. Pacientes que tiveram um emprego antes da operação parecia ter mais recursos emocionais. Assim, eles podiam sentir menos sofrimento, porque o emprego podia protegê-los. Mulheres e aqueles que não tinham emprego eram mais propensos a apresentar sintomas de depressão. Além disso, pacientes que não tinham emprego e aqueles com IMC> 50 kg / m² foram mais propensos a apresentar sintomas de ansiedade.
Depressão; Cirurgia bariátrica; Ansiedade; Emprego
ORIGINAL ARTICLE
Correspondence
ABSTRACT
BACKGROUND: Bariatric surgeries have been considered an alternative for treatment of morbid obesity. Some adverse events that people experience after the treatment frequently are the consequence of the lack of consistent knowledge associated with psychosocial factors that are related to the pre-surgery status of the patients.
AIM: To evaluate psychosocial variables of 414 candidates for bariatric surgery from Clinical Hospital of Medical School at University of São Paulo, Ribeirão Preto, SP, Brazil.
METHODS: Semi-structured interview, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI) and Binge Eating Scale (BES) were used.
RESULTS: BMI was higher among patients who had no employment (p = 0.019). Female, patients who had a partner and patients with a BMI < 50 kg/m², all of them desired have a lower weight (p < 0.001). BAI scores were higher among patients who had no employment (p < 0.05) and higher among those with a BMI > 50 kg/m² (p < 0.05). BDI scores were higher among women (p < 0.05) and lower among those who had an employment (p < 0.01). No difference in BES was found.
CONCLUSIONS: The data suggest that women showed higher indicators of anxiety and depression, suggesting that they had a more fragile psychological functioning with difficulties in coping with distress. Self-perception as well as skills and abilities, may reflect internal aspects of individual's personality. Patients who had an employment before surgery seemed have more emotional resources. So, they may feel less distress because the employment may protect them. Women and those who did not have an employment were more likely to experience depression symptoms. Furthermore, patients who did not have an employment and those with BMI> 50 kg / m² were more likely to experience anxiety symptoms.
Headings: Depression. Bariatric Surgery. Anxiety. Employment.
INTRODUCTION
In the last decades obesity became a global epidemy reaching more than 900 million of overweight people and around 400 million of definitely obese people12. Recent studies in the USA showed a high prevalence of obesity among both men and women (32% and 36% respectively)7. In Brazil, data from the Brazilian Institute of Geography and Statistic11 estimated that the overweight was observed in around half of men and women. Obesity was diagnosed in 13% of the men and 17% of the women. Also, it is estimated that 3% of men and 7% of women already reached the state of obesity class III or morbid obesity18. These are alarming numbers since obesity can lead to several health problems, bringing physical and psychosocial limitations.
Bariatric surgeries have been considered an alternative for the treatment for obesity class III. It can lead people to lose a significant amount of weight and has the advantage to lead to an important improvement in quality of life related to physical and mental aspects1,15,23. Only in the USA the reports from 2006 of the American Society for Metabolic & Bariatric Surgery estimated that around 170 000 people had bariatric surgery9.
Although bariatric surgery is really important procedure for the control of obesity class III, it is relevant to point out that some adverse events that people experience after the treatment frequently are the consequence of the lack of consistent knowledge associated with psychosocial factors that are related to the pre-surgery status of the patients. So, many patients may experience failures and adverse events which are associated with undesirable psychosocial aspects that are related to the physical, mental and social functioning, as well as to the body image, behavior and cognitive aspects24.
In the context of pre-bariatric surgery psychological assessment, in general studies that use a variety of instruments, such as inventories tracking symptoms, inventories of personality, scales of assessment of quality of life and assessment of eating disorders are observed3,19.
Considering that these assessment instruments often "trap" the possibilities for different responses of patients and they limit the information to some predefined alternatives, the use of these instruments in isolation may compromise the quality and accuracy of the responses. Different studies show the usefulness of these instruments, such as Beck Depression Inventory which tracks the symptoms of depression among patients who are eligible for bariatric surgery13,17.
Others have evaluated and documented aspects related to the quality of life and mental health before and after bariatric surgery14,19. Although the use of standardized scales increases the capacity to reproduce the results, since they are isolated measures, they fail to realize how different areas interacting each other.
Within this context, despite the large number of studies that focus on trying to characterize the psychosocial profile of people who wish to undergo this surgery, there are few studies aiming to correlate different variables arising from a semi-structured interview (such as aspects related to the employment, relationships and body weight) with variables resulting from the use of scales or assessment inventories such as presence or absence of symptoms of anxiety, depression and binge eating.
The use of interviews in the context of psychosocial assessment in bariatric surgery has its relevance in providing information on specific variables related to denial of problems, difficulties in the modulation of thoughts, feelings and behaviors, and other cognitive distortions10. Most often used only as a complementary data source or a source of socio-demographic data4, the broader interviews can be very useful in the preoperative psychological evaluation, facilitating comparison and confirmation of evaluation results arising from standardized inventories.
In this context, this study aimed to evaluate psychosocial variables based on standardized inventories of depression, anxiety and binge eating in relation to the characteristics derived from a semi-structured interview.
METHODS
This research was approved by the Ethics Committee of the Clinical Hospital of Medical School at University of São Paulo, Ribeirão Preto, São Paulo, Brazil, to conduct this study.
Ninety five per cent of all patients from Clinical Hospital of School of Medical School at University of São Paulo, Ribeirão Preto, SP, Brazil were evaluated corresponding to 414 participants. All of them had a clinic diagnostic of obesity class III, ie, who had Body Mass Index (BMI) > 40 kg/m². They were candidates to bariatric surgery and during this evaluation they were undergoing to the pre-surgery exams.
Among the patients, 79% were female and 22% were male. The mean age of the patients was 39 years (+ 10 years), the mean BMI was 51 kg/m² (+ 7 kg/m²) for women and 54 kg/m² (+ 7 kg/m²) for men. Sixty one per cent of the men and 49% of the women had employment. Importantly, in this case the word "employment" refers to any gainful occupation.
Instruments
The following instruments were used: a semi-structured interview that aimed not only to collect socio-demographic data but also to understand professional and relationship aspects, as well as aspects related to weight; Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI)5 which aimed to do a trace of psychological symptoms related to depression and anxiety; Binge Eating Scale (BES)8 to assess the presence of symptoms of binge eating in patients who were candidates for bariatric surgery.
Data collection
Psychological assessment was performed as soon as the patient had been considered eligible by medical staff to start pre-surgery evaluation. In general, this psychological assessment occurred around two or three months before the surgery.
Although these assessments are part of routine of center of bariatric surgery, patients were invited to participate in the research protocol that included a comprehensive assessment. So, it is important to highlight that the data presented here are part of a broader assessment.
In accepting to participate, patients were then evaluated by a psychologist from the center of bariatric surgery. These assessments occurred in one session and were individual, which lasted approximately an hour and a half to two hours.
It is important to highlight that after each assessment, codification and analysis of the results, all the patients received a brief interview which aimed to give to the patient the results from his/her evaluation.
Treatments
The interviews were read and then the responses were categorized according to themes: gender, weight, high, BMI, marital status, employment and desired weight.
In relation to the others instruments, the data were codified according to specific recommendations of each instrument, and then the analysis of them were proceeded.
Data treatments were made by using statistical package SPSS 17.0, and for different comparisons of the results the Student´s t Test was used.
RESULTS
Table 1 shows the mean values and standard deviations of the BMI according to gender, marital status and employment. BMI was significantly lower among patients who reported working at the time of evaluation than those who were not working (p = 0.019). In relation to gender and marital status no statistically significant differences were observed.
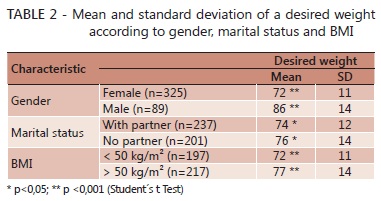
Table 2 shows that the women reported desire weight significantly less than men (p < 0.001). Patients who had a partner also reported the desire for a significantly lower weight than those who had no partner (p < 0.05). People with a BMI less than 50 kg/m² reported desire to have a significantly lower weight compared to those with a BMI greater than 50kg/m² (p < 0.001).
Table 3 shows the mean and standard deviation on the scoring of the patients in the instruments BDI, BAI and Binge Eating Scale compared to gender, marital status, employment and BMI. BAI scores were significantly higher among patients who had no employment, compared to those who worked (p < 0.05). Scores on the BAI were significantly higher among those with a BMI > 50 kg/m² (p < 0.05). There was a significant difference of BDI scores indicating higher scores among women (p < 0.05). BDI scores were significantly lower among those who were working, compared to those with not work (p < 0.01). As for the BES statistically significant differences in the comparisons were not observed.
DISCUSSION
The present study aims to investigate the presence of psychological variables in candidates to bariatric surgery by comparing the results obtained with the use of standarded inventories and a semi-structured interview.
The results obtained show that women with morbid obesity had higher scores on the BDI compared to men, suggesting a greater presence of depression symptoms among women. Normative data of Cunha5 show that a score on the BDI > 12 can be an indicator suggesting the presence of mild depression.
In this case, although both men and women presenting signs suggestive of mild depression, on average, women had a significantly greater diversity of symptoms in pre-surgery period. The literature indicates the presence of depressive symptoms among people with morbid obesity in general2,16,22. However these studies do not make comparisons of results between the genders. As seen, this differentiation seems to be very important and reflect on the reasons that lead women to experience more depressive symptoms.
The present study showed that women also wanted to have a significantly lower weight than men. Considering these two aspects, one can think that these women might be experiencing internal and external pressures which are very difficult to deal. One of them refers to the demanding of having different body compared to the current one. Considering that the mean weight of these women was 138 kg, reach a weight of 71 kg (value equivalent to the weight desired by women) seems to be really very difficult to get, even through bariatric surgery. The other reason is related to the external demanding to have a body which must comply with the standards of beauty and aesthetics that are transmitted by society. If it considers that the socio-cultural parameters can influence the perception of body image and, hence the self image, appreciation of the outward appearance as well as feelings of satisfaction with body weight may go beyond the real body size, also showing association with other variables such as physical health conditions and psychosocial factors1.
It is also important the fact that it were not find statistically significant differences in results for the trace of anxiety, depression and binge eating related to the marital status.
However, the patients who had a partner in the time of evaluation wanted to reach a lower weight although they had in average a lower BMI compared to those without a partner.
The fact that these people had a partner could give them some peace of mind and even lead to some accommodation. But they seemed to feel a greater need and/or desire to decrease their body size. Perhaps because they were under pressure from their partner or by other demands inherent in marriage that could not be easily satisfied because of excess weight.
Leaving aside external issues what calls attention again is the presence of body dissatisfaction that is common among these people, regardless of their living conditions. In other words, according to, the judgment about the body of a person can go beyond physical form6. When people have more structured personality and have well-resourced mental functioning, they may experience a better understanding about their physical attractiveness. It is suggested therefore that the perception of body image seems to go beyond the perceived weight, size and shape. It also seems to reflect the internal arrangements of the individual specially related to on how the individual feels about him/herself.
Another very interesting finding refers to the fact that most patients (51.4%) were working, ie they were having some kind of paid activity before overcoming surgery. This finding opposes to what has been found in other study that relate low level of employment among bariatric surgery candidates25.
It is important to highlight that the BMI of those patients who had an employment was 61% of the men and 49% of the women and that is a far above level of what is already considered severely obese. Thus, they were severely obese people and, despite all physical limitation and different difficulties experienced by weight excess, they were still active in terms of occupational functioning. Among those patients who did not work the mean BMI was 52 kg/m², reinforcing the idea that the more obese, more difficult to work.
Moreover, they showed higher indicators of anxiety and depression compared with those who had an employment. Having an employment is considered a protective factor for the development of emotional disorders1. A person who works, in general, experiences self-esteem in a more positive way and feels more confident. For these patients who work, it can be assumed that they had emotional conditions to do it, despite the physical difficulties.
In a study that compared the emotional aspects of women in different BMI classes, the author found that women with obesity class III showed more efforts to adapt to the environment compared to women with obesity class I1. Despite the difficulty in self-acceptance and self appreciation these data suggest that people with obesity class III showed effort in search of adapting to their environment. These patients may seek recognition through other attributes, such as making better use of their cognitive resources. Thus, the supposed presence of these resources may be protecting from their experiences of distress in relation to individuals who have an employment. In this sense, these patients may feel less distress before the surgery because they have an employment which protects them.
In relation to the patients with higher levels of obesity who did not work, taking as reference the observations from Sarlio-Lahteenkorva et al.21, it is possible to raise some hypotheses.
Considering the psychosocial damages that these people experience, as the association between overweight and negative features, it can be supposed that the lack of an employment does not happen only by physical limitations, but also by internal constraints. In other words, these people did not have cognitive resources that are enough to contain the experiences of anxiety, as well as to counteract the attitudes of discrimination and prejudice that overweight people are exposed to. In general, people with morbid obesity are seen as lazy, sloppy, disgusting and few believe in their cognitive, physical, social and psychological conditions1,20,21.
Thus, the emotional condition of the patients who did not work is of utmost importance. As previously referred, self-perception as well as skills and abilities, may reflect the internal aspects of individual's personality. Considering that these people showed higher levels of anxiety and depression, it can be infered that they had a more fragile psychological functioning with difficulties in coping with distress. In a study that was conducted only with women who were submitted to bariatric surgery, the author observed that these women showed indicators of difficulty to deal with distress prior the surgery, despite the presence of positive resources of personality organization1.
The data found show that people who were working before surgery seemed to have more emotional resources, since they were significantly better than the group of people who did not have an employment. It is questionable if these people were better just because they had an employment or if the work itself was serving as a protective factor.
Moreover, there is a question whether it could also be considered a protective factor for a faster and effective recovery of surgery, the fact that these patients are better psychological point of view and they have an employment. To answer these questions further research should be conducted to try finding positive correlations between these variables. It would also be of great importance to conduct studies seeking to characterize the role of the occupation (employment / work) in the recovery of the patient who overcame bariatric surgery. Further studies in this area will be necessary so that they can investigate issues relating to work and emotional aspects within a longitudinal methodology in order to seek to understand them within a continuous time.
This study used not only inventories but also a semi-structured interview which gave important information about the patients. This study characterized the relation between emotional aspects, relationships, body weight and employment or occupation which was important to understand some limitations of these patients and their emotional resources and difficulties. However this interview is not validated yet. So, it is suggested a need to have a tool which is going to be a specific and validated instrument to assess candidates to bariatric surgery and that it will give information about some areas related to the bariatric surgery which need to be evaluated.
CONCLUSIONS
Female patients and those who did not have an employment are more likely to present depression symptoms. Moreover, patients who did not have an employment and those who have BMI > 50 kg/m² are more predisposed to present anxiety symptoms and more likely to have higher BMI. Patients who had a partner desired a lower weight than those patients who did not have a partner. Both female patients and patients with BMI < 50 kg/m² also desired lower weight. This is expected considering that men, in general, have already a BMI greater than women. Moreover, when considering the expected weight loss after surgery, it is more likely to suppose that patients with lower BMI are more likely to want a smaller weight.
REFERENCES
- 1. Almeida GAN. A imagem corporal los Mulheres: Aspectos psicossociais eA Cirurgia de restrição gástrica. Ribeirão Preto, São Paulo, 2003.
- 2. Baptista MN, Vargas JF, Baptista ASD. Depressão e Qualidade de Vida los UMA maostra brasileira de obesos mórbidos. Avaliação Psicológica de 2008, 7 (2): 235-247.
- 3. Bauchowitz UA, Gonder-Frederick LA, Olbrisch ME et al. Avaliação psicossocial dos candidatos à cirurgia bariátrica: Um levantamento das práticas atuais. Psicossoma Med. 2005, 67:825-32.
- 4. Canetti L, Berry EM, Elizur Y. preditores psicossociais da perda de peso e ajustamento psicológico após a cirurgia bariátrica e um programa de perda de peso: o papel mediador de comer emocional. International Journal of Eating Disorders 2009, 42 (2): 109-17.
- 5. Cunha JA. Manual da english version das Escalas Beck. São Paulo, SP: Casa do Psicólogo, 2001.
- 6. Fisak-Jr B, Tantleff-Dunn b S, Petersonb RD. Informações personalidade: Será que a influência avaliações atratividade de tamanhos diferentes do corpo? Corpo Imagem de 2007, 4 (2): 213-7.
- 7. Flegal KM , Carroll MD , Ogden CL et al. Prevalência e tendências na obesidade entre os adultos dos EUA, 1999-2008. JAMA 2010; 303 (3): 235-41.
- 8. Freitas S, Lopes CS, Coutinho W et al. Tradução e Adaptação para o inglês da Escala de Compulsão Alimentar Periódica. Revista Brasileira de Psiquiatria 2001, 23 (4): 215-20.
- 9. Gainesville, FL. Cirurgia metabólica deve desempenhar papel mais importante no tratamento da diabetes tipo 2 e outras doenças metabólicas. Sociedade Americana de Cirurgia Metabólica e Bariátrica 2007.
- 10. Glinski J, S Wetzler, Goodman E. A Psicologia da cirurgia bypass gástrico. Cirurgia de Obesidade de 2001, 5: 581-8.
-
11Instituto Brasileiro de Geografia e Estatística, 2008-2009. Antropometria e Estado nutricional de Crianças, adolescentes e Adultos no Brasil.
- 12. Kelly T, W Yang, Chen CS et al. Carga global de obesidade em 2005 e projeções para 2030. International Journal of Obesity 2008; 32: 1431-7.
- 13. Krukowski RA, Friedman KE, Applegate KL. O Utilitário do Inventário de Depressão de Beck em uma População Cirurgia Bariátrica. Cirurgia da obesidade 2010, 20 (4): 426-31.
- 14. Malone M, Alger-Mayer Estado Binge S. e Qualidade de vida após a cirurgia de bypass gástrico: Um Estudo de um ano. Obesidade Research 2004, 12: 473-81.
- 15. Mamplekou E, Komesidou V, Bissias C et al. Condição psicológica e Qualidade de Vida em Pacientes com Obesidade Mórbida Antes e Depois da perda de peso Cirúrgica. Cirurgia de Obesidade de 2005; 15 (8): 1177-1184.
- 16. Matos MI, Aranha LS, NA Faria et al. Binge eating disorder, ansiedade, depressão e imagem corporal em pacientes de obesidade grau III. Revista Brasileira de Psiquiatria 2002, 24 (4): 165-9.
- 17. Munoz DJ, Chen E, Fischer S et al. Considerações para o uso do Inventário de Depressão de Beck na avaliação do peso losssurgery-pacientes que procuram. Cirurgia da obesidade 2007, 17 (8): 1097-1101.
- 18. Ogden CL, Carroll MD, Curtin LR et al. Prevalência de excesso de peso e obesidade em o Unido . Estados, 1999-2004 JAMA 2006; 295 (13): 1549-55.
- 19. Oliveira JAI, Yoshida EMP. Avaliação psicológica de obesos Grau III os antes e depois de Cirurgia Bariátrica. Psicologia Reflexão e Crítica 2009, 22 (1): 12-19.
- 20. Paulo R, Brownell KD. Preconceito, discriminação e obesidade. Obesidade Research 2001, 9 (12): 788-805.
- 21. Sarlio Lahteenkorva-S, Stunkard A, fatores Rissanen A. Psicossocial e qualidade de vida na obesidade. International Journal of Obesity e Distúrbios Metabólicos 1995, 19: S1-S5.
- 22. Segal A, Fandino J. Indicações e contra-indicações parágrafo Realização das Operações bariátricas. Revista Brasileira de Psiquiatria 2002, 24 (suppl.3): 68-72.
- 23. van Hout GCM, Boekestein P, Fortuin FAM et al. Funcionamento psicossocial após Cirurgia Bariátrica. Cirurgia de Obesidade de 2006, 16 (6): 787-94.
- 24. van Hout GCM, van Oudheusden I, van Heck GL.Psychological Perfil da obesidade mórbida. Cirurgia de Obesidade de 2004, 14: 579-88.
- 25. Velcu LM, Adolphine R, R Mourelo et al. Perda de peso, qualidade de vida e situação de emprego após Roux-en-Y bypass gástrico: 5 anos de análise. Surg Obes Relat Dis 2005, 1:413-6;
Psychosocial aspects in bariatric surgery: the association among emotional variables, job, relationships and body weight
Publication Dates
-
Publication in this collection
15 Dec 2011 -
Date of issue
Sept 2011
History
-
Accepted
26 Apr 2011 -
Received
14 Dec 2011