Abstracts
INTRODUCTION:
The hepatopulmonary syndrome has been acknowledged as an important vascular complication in lungs developing systemic hypoxemia in patients with cirrhosis and portal hypertension. Is formed by arterial oxygenation abnormalities induced from intrapulmonary vascular dilatations with liver disease. It is present in 4-32% of patients with cirrhosis. It increases mortality in the setting of cirrhosis and may influence the frequency and severity. Initially the hypoxemia responds to low-flow supplemental oxygen, but over time, the need for oxygen supplementation is necessary. The liver transplantation is the only effective therapeutic option for its resolution.
AIM:
To update clinical manifestation, diagnosis and treatment of this entity.
METHOD:
A literature review was performed on management of hepatopulmonary syndrome. The electronic search was held of the Medline-PubMed, in English crossing the headings "hepatopulmonary syndrome", "liver transplantation" and "surgery". The search was completed in September 2013.
RESULTS:
Hepatopulmonary syndrome is classically defined by a widened alveolar-arterial oxygen gradient (AaPO2) on room air (>15 mmHg, or >20 mmHg in patients >64 years of age) with or without hypoxemia resulting from intrapulmonary vasodilatation in the presence of hepatic dysfunction or portal hypertension. Clinical manifestation, diagnosis, classification, treatments and outcomes are varied.
CONCLUSION:
The severity of hepatopulmonary syndrome is an important survival predictor and determine the improvement, the time and risks for liver transplantation. The liver transplantation still remains the only effective therapeutic.
Hepatopulmonary syndrome; Liver transplantation; Surgery
INTRODUÇÃO:
A síndrome hepatopulmonar (SHP) tem sido reconhecida como importante complicação vascular nos pulmões desenvolvendo hipoxemia sistêmica em pacientes com cirrose e hipertensão portal. Ela é formada pela presença de anormalidade na oxigenação arterial induzida por dilatações vasculares intrapulmonares com a doença hepática e está presente em 4-32% dos pacientes com cirrose. Aumenta a mortalidade no cenário de cirrose podendo influenciar na frequência e gravidade. Inicialmente, a hipoxemia nos pacientes com esta síndrome responde à suplementação com baixo fluxo de oxigênio; mas, ao longo do tempo, há necessidade de maior suplementação de oxigênio. O transplante de fígado é a única opção terapêutica eficaz para a resolução.
OBJETIVO:
Atualizar conhecimentos sobre a síndrome hepatopulmonar, suas manifestações clínicas, diagnóstico e tratamento.
MÉTODO:
Foi realizada revisão da literatura com busca eletrônica realizada no Medline-PubMed em inglês cruzando-se os descritores "síndrome hepatopulmonar", "transplante de fígado" e "cirurgia". A pesquisa foi concluída em setembro de 2013.
RESULTADOS:
Síndrome hepatopulmonar é classicamente definida por alteração no gradiente alvéolo-arterial (AaPO2) em ar ambiente (>15 mmHg, ou >20 mmHg em pacientes >64 anos de idade) com ou sem hipoxemia resultante da vasodilatação intrapulmonar na presença de disfunção hepática ou hipertensão portal. As manifestações clínicas, diagnóstico, classificação e tratamento são variados.
CONCLUSÃO:
A avaliação da gravidade da síndrome hepatopulmonar é importante meio de predição de sobrevivência e determinação do tempo e riscos para o transplante de fígado. O tratamento consiste em oxigênio suplementar e o transplante continua sendo a única terapêutica eficaz.
Síndrome hepatopulmonar; Transplante de fígado; Cirurgia
INTRODUCTION
The hepatopulmonary syndrome (HPS) has been acknowledged as an important vascular complication in lungs due to systemic hypoxemia in patients with cirrhosis and portal hypertension. Is formed by a clinical triad of arterial oxygenation abnormalities induced by intrapulmonary vascular dilatations with liver disease. It is present in 4-32% of patients with cirrhosis1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549.. It was also seen in both genders in middle-aged patients1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880.. HPS pathogenesis is not well defined, but it is speculated that a combination of factors, such as an imbalance in the response of vascular endothelin receptors, pulmonary microvascular remodeling and genetic predisposition, leads to intrapulmonary vascular dilatation and bacterial translocation11. Fallon MB: Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol 2005, 39(4 Suppl 2):S138-142. , 1010. Luo B, Tang L, Wang Z, Zhang J, Ling Y, Feng W, Sun JZ, Stockard CR, Frost AR, Chen YF et al: Cholangiocyte endothelin 1 and transforming growth factor beta1 production in rat experimental hepatopulmonary syndrome. Gastroenterology 2005, 129(2):682-695. , 1212. Nacif LS, Andraus W, Kubrusly MS, Molan N, Chaib E, D'Albuquerque LA. Myeloperoxidase activity is increased in hepatopulmonary syndrome in rats. Arq Bras Cir Dig. 2013 Nov-Dec;26(4):293-5. , 1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549..
HPS increases mortality in the setting of cirrhosis and may influence the frequency and severity. Initially the hypoxemia responds to low-flow supplemental oxygen, but over time, the need for oxygen supplementation is necessary. Currently, no pharmacological intervention can readily improve arterial oxygenation and alter the course of HPS. Thus, liver transplantation is the only effective therapeutic option for its resolution1313. Nacif LS, Andraus W, Sartori K, Benites CM, Santos VR, Rocha-Filho JA, D'Albuquerque LC. Hypoxia among patients on the liver-transplant waiting list. Arq Bras Cir Dig. 2014 Mar;27(1):56-8. , 1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549..
The aim of this review is to update HPS on its clinical manifestation, diagnosis and treatment.
METHODS
Study identification and selection
The review was performed using electronic search on Medline-PubMed, in English. The search was performed through www.ncbi.nlm.nih.gov/pubmed and Mesh-term crossing the headings "hepatopulmonary syndrome", "liver transplantation" and "surgery". The search was completed in September 2013.
Definition
The diagnostic features of HPS include presence of liver disease or portal hypertension, an elevated age-adjusted alveolar-arterial oxygen gradient (AaPO2), and evidence of intrapulmonary vasodilatation11. Fallon MB: Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol 2005, 39(4 Suppl 2):S138-142. , 22. Fallon MB, Abrams GA: Pulmonary dysfunction in chronic liver disease. Hepatology 2000, 32(4 Pt 1):859-865. , 33. Fallon MB, Krowka MJ, Brown RS, Trotter JF, Zacks S, Roberts KE, Shah VH, Kaplowitz N, Forman L, Wille K et al: Impact of hepatopulmonary syndrome on quality of life and survival in liver transplant candidates. Gastroenterology 2008, 135(4):1168-1175. , 1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549.. It is classically defined by a widened alveolar-arterial oxygen gradient (AaPO2) on room air (>15 mmHg, or >20 mmHg in patients >64 years of age) with or without hypoxemia resulting from intrapulmonary vasodilatation in the presence of hepatic dysfunction or portal hypertension 44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262. , 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880. , 1818. Schenk P, Schöniger-Hekele M, Fuhrmann V, Madl C, Silberhumer G, Müller C: Prognostic significance of the hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology 2003, 125(4):1042-1052.. In the presence of coexisting cardiac or pulmonary disease, establishing a diagnosis of HPS can be difficult 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549..
Clinical manifestations
Involve respiratory findings associated with chronic liver disease. The insidious onset of dyspnea, particularly on exertion, is the most common complaint, but is not specific. Others symptoms may be present as platypnea and orthodeoxia55. Gómez FP, Martínez-Pallí G, Barberà JA, Roca J, Navasa M, Rodríguez-Roisin R: Gas exchange mechanism of orthodeoxia in hepatopulmonary syndrome. Hepatology 2004, 40(3):660-666. , 66. Hemprich U, Papadakos PJ, Lachmann B: Respiratory failure and hypoxemia in the cirrhotic patient including hepatopulmonary syndrome. Curr Opin Anaesthesiol 2010, 23(2):133-138.. Spider angiomata are commonly reported but are frequently seen in cirrhotic patients without HPS. Finally, clubbing and distal cyanosis, when present in the setting of liver disease or portal hypertension, should raise suspicion22. Fallon MB, Abrams GA: Pulmonary dysfunction in chronic liver disease. Hepatology 2000, 32(4 Pt 1):859-865.. The majority of patients with HPS are either asymptomatic, particularly if diagnosed during evaluation for liver transplantation. Some cases develop the insidious onset of dyspnea44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262. , 88. Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912..
Diagnosis
HPS diagnosis depends initially on the presence of liver disease or portal hypertension, an elevated age-adjusted alveolar-arterial oxygen gradient (AaPO2), and evidence of intrapulmonary vasodilatation77. Krowka MJ, Dickson ER, Wiesner RH, Krom RA, Atkinson B, Cortese DA: A prospective study of pulmonary function and gas exchange following liver transplantation. Chest 1992, 102(4):1161-1166.. It can normally be diagnosed with non-invasive tests. Its diagnosis is suspected based on history and physical exam; arterial blood gas analysis should be performed while breathing room air on pulse oximetry22. Fallon MB, Abrams GA: Pulmonary dysfunction in chronic liver disease. Hepatology 2000, 32(4 Pt 1):859-865. , 44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262.. An elevated alveolar-arterial gradient and decrease in arterial blood gas occurs due to the dilatation of pulmonary vasculature leading to shunt with ventilation-perfusion mismatch 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880..
The arterial blood gas reveals an elevated age-adjusted AaPO2 with or without hypoxemia. In detecting gas exchanges abnormalities, chest radiography and pulmonary function tests for evaluation the presence of other pulmonary abnormalities should be performed. The transthoracic microbubble contrast echocardiography is the preferred screening test for intrapulmonary vasodilatation. Pulmonary angiography, technetium-labeled macroaggregated albumin scan and chest computerized tomography could be useful in some specific situations99. Lima BL, Franca AV, Pazin-Filho A, Araujo WM, Martinez JA, Maciel BC, Simoes MV, Terra-Filho J, Martinelli AL: Frequency, clinical characteristics, and respiratory parameters of hepatopulmonary syndrome. Mayo Clin Proc 2004, 79(1):42-48. , 1111. Machicao VI, Fallon MB: Hepatopulmonary syndrome. Semin Respir Crit Care Med 2012, 33(1):11-16. , 1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1616. Rodríguez-Roisin R, Krowka MJ: Hepatopulmonary syndrome--a liver-induced lung vascular disorder. N Engl J Med 2008, 358(22):2378-2387. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549. .
Classification
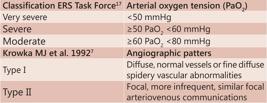
The ERS Task Force has proposed a classification using arterial oxygen tension (PaO2) to stage the severity of HPS: PaO2<50 mmHg indicates very severe; PaO250 <60 mmHg suggests severe; and a PaO2 60 and <80 mmHg corresponds with moderate stages1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880..
Krowka et al.77. Krowka MJ, Dickson ER, Wiesner RH, Krom RA, Atkinson B, Cortese DA: A prospective study of pulmonary function and gas exchange following liver transplantation. Chest 1992, 102(4):1161-1166. demonstrated two angiographic patters: type I, or diffuse, normal vessels or fine diffuse spidery arterial vascular abnormalities and type II, or focal, more infrequent, consisted of similar focal arteriovenous communications (Figure 1). Patients with advanced type I or type II, may exhibit a poor response to oxygen breathing77. Krowka MJ, Dickson ER, Wiesner RH, Krom RA, Atkinson B, Cortese DA: A prospective study of pulmonary function and gas exchange following liver transplantation. Chest 1992, 102(4):1161-1166..
Treatment
The oxygen supplementation keeps a mainstay of therapy with a PaO2<60 mmHg or with oxigen desaturation exercise-induced88. Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912. , 1616. Rodríguez-Roisin R, Krowka MJ: Hepatopulmonary syndrome--a liver-induced lung vascular disorder. N Engl J Med 2008, 358(22):2378-2387.. The transjugular intrahepatic portosystemic shunt (TIPS) had limit utility in HPS and need more clinical trials to define the efficacy1515. Paramesh AS, Husain SZ, Shneider B, Guller J, Tokat I, Gondolesi GE, Moyer S, Emre S: Improvement of hepatopulmonary syndrome after transjugular intrahepatic portasystemic shunting: case report and review of literature. Pediatr Transplant 2003, 7(2):157-162.. There are currently no effective medical therapies for HPS.
Hepatopulmonary syndrome algorithm therapeutic proposed by ERS Task Force is detailed in Figure 2.
Liver transplantation is the only effective established therapy for HPS 44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262. , 88. Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912.. The total resolution or significant improvement in gas exchange post-liver transplant is observed in more than 85% of reported patients and arterial hypoxemia normalization after transplantation is variable and may be superior to one year 44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549..
Outcomes
The causes of death in patients with HPS were mainly due to complications of hepatocellular dysfunction and portal hypertension, and correlated with the severity of hypoxemia. It has been reported that HPS can increase the mortality of patients with liver cirrhosis, especially in those with severe hypoxemia66. Hemprich U, Papadakos PJ, Lachmann B: Respiratory failure and hypoxemia in the cirrhotic patient including hepatopulmonary syndrome. Curr Opin Anaesthesiol 2010, 23(2):133-138. , 1111. Machicao VI, Fallon MB: Hepatopulmonary syndrome. Semin Respir Crit Care Med 2012, 33(1):11-16. , 1414. Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625. , 1919. Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549..
Mortality after liver transplantation also appears to be higher in patients with HPS compared to those without. The strongest predictors of post-liver transplantation mortality were the preoperative PaO2<50 mmHg alone or in combination with a macroaggregated albumin shunt fraction of 20%33. Fallon MB, Krowka MJ, Brown RS, Trotter JF, Zacks S, Roberts KE, Shah VH, Kaplowitz N, Forman L, Wille K et al: Impact of hepatopulmonary syndrome on quality of life and survival in liver transplant candidates. Gastroenterology 2008, 135(4):1168-1175. , 88. Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912.. A prospective study found that those with severe HPS (PaO2<50 mmHg) had an important increase in post-liver transplantation mortality33. Fallon MB, Krowka MJ, Brown RS, Trotter JF, Zacks S, Roberts KE, Shah VH, Kaplowitz N, Forman L, Wille K et al: Impact of hepatopulmonary syndrome on quality of life and survival in liver transplant candidates. Gastroenterology 2008, 135(4):1168-1175..
HPS increases mortality and liver transplant outcomes and may worsen in cases of advanced stages. Therefore, the worldwide centers may improve the increase priority for liver transplantation in patients with HPS and significant hypoxemia. The MELD score does not apply and reduce the survival in waiting liver transplant list patients in those patients that HPS affect decreasing quality of life33. Fallon MB, Krowka MJ, Brown RS, Trotter JF, Zacks S, Roberts KE, Shah VH, Kaplowitz N, Forman L, Wille K et al: Impact of hepatopulmonary syndrome on quality of life and survival in liver transplant candidates. Gastroenterology 2008, 135(4):1168-1175. , 44. Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262. , 66. Hemprich U, Papadakos PJ, Lachmann B: Respiratory failure and hypoxemia in the cirrhotic patient including hepatopulmonary syndrome. Curr Opin Anaesthesiol 2010, 23(2):133-138. , 88. Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912.. Liver transplantation has been considered as the only therapy established to reverse intrapulmonary vasodilation, but the postoperative mortality is still high in patients with a partial pressure of oxygen lower than 50 mmHg. A better understanding of the pathophysiological mechanism underlying HPS will help to better guide its treatment11. Fallon MB: Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol 2005, 39(4 Suppl 2):S138-142. , 22. Fallon MB, Abrams GA: Pulmonary dysfunction in chronic liver disease. Hepatology 2000, 32(4 Pt 1):859-865. , 1717. Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880. , 1818. Schenk P, Schöniger-Hekele M, Fuhrmann V, Madl C, Silberhumer G, Müller C: Prognostic significance of the hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology 2003, 125(4):1042-1052..
CONCLUSION
The severity of HPS is an important predictor to determine survival, the better moment and the risks for liver transplantation. The liver transplantation still remains the only effective therapeutic modality.
REFERENCES
-
1Fallon MB: Mechanisms of pulmonary vascular complications of liver disease: hepatopulmonary syndrome. J Clin Gastroenterol 2005, 39(4 Suppl 2):S138-142.
-
2Fallon MB, Abrams GA: Pulmonary dysfunction in chronic liver disease. Hepatology 2000, 32(4 Pt 1):859-865.
-
3Fallon MB, Krowka MJ, Brown RS, Trotter JF, Zacks S, Roberts KE, Shah VH, Kaplowitz N, Forman L, Wille K et al: Impact of hepatopulmonary syndrome on quality of life and survival in liver transplant candidates. Gastroenterology 2008, 135(4):1168-1175.
-
4Fallon MB, Zhang J: The lung in liver disease: old problem, new concepts. Trans Am Clin Climatol Assoc 2013, 124:250-262.
-
5Gómez FP, Martínez-Pallí G, Barberà JA, Roca J, Navasa M, Rodríguez-Roisin R: Gas exchange mechanism of orthodeoxia in hepatopulmonary syndrome. Hepatology 2004, 40(3):660-666.
-
6Hemprich U, Papadakos PJ, Lachmann B: Respiratory failure and hypoxemia in the cirrhotic patient including hepatopulmonary syndrome. Curr Opin Anaesthesiol 2010, 23(2):133-138.
-
7Krowka MJ, Dickson ER, Wiesner RH, Krom RA, Atkinson B, Cortese DA: A prospective study of pulmonary function and gas exchange following liver transplantation. Chest 1992, 102(4):1161-1166.
-
8Krowka MJ, Fallon MB: Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? Am J Transplant 2008, 8(5):911-912.
-
9Lima BL, Franca AV, Pazin-Filho A, Araujo WM, Martinez JA, Maciel BC, Simoes MV, Terra-Filho J, Martinelli AL: Frequency, clinical characteristics, and respiratory parameters of hepatopulmonary syndrome. Mayo Clin Proc 2004, 79(1):42-48.
-
10Luo B, Tang L, Wang Z, Zhang J, Ling Y, Feng W, Sun JZ, Stockard CR, Frost AR, Chen YF et al: Cholangiocyte endothelin 1 and transforming growth factor beta1 production in rat experimental hepatopulmonary syndrome. Gastroenterology 2005, 129(2):682-695.
-
11Machicao VI, Fallon MB: Hepatopulmonary syndrome. Semin Respir Crit Care Med 2012, 33(1):11-16.
-
12Nacif LS, Andraus W, Kubrusly MS, Molan N, Chaib E, D'Albuquerque LA. Myeloperoxidase activity is increased in hepatopulmonary syndrome in rats. Arq Bras Cir Dig. 2013 Nov-Dec;26(4):293-5.
-
13Nacif LS, Andraus W, Sartori K, Benites CM, Santos VR, Rocha-Filho JA, D'Albuquerque LC. Hypoxia among patients on the liver-transplant waiting list. Arq Bras Cir Dig. 2014 Mar;27(1):56-8.
-
14Palma DT, Fallon MB: The hepatopulmonary syndrome. J Hepatol 2006, 45(4):617-625.
-
15Paramesh AS, Husain SZ, Shneider B, Guller J, Tokat I, Gondolesi GE, Moyer S, Emre S: Improvement of hepatopulmonary syndrome after transjugular intrahepatic portasystemic shunting: case report and review of literature. Pediatr Transplant 2003, 7(2):157-162.
-
16Rodríguez-Roisin R, Krowka MJ: Hepatopulmonary syndrome--a liver-induced lung vascular disorder. N Engl J Med 2008, 358(22):2378-2387.
-
17Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB, Committee ETFP-HVDPS: Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J 2004, 24(5):861-880.
-
18Schenk P, Schöniger-Hekele M, Fuhrmann V, Madl C, Silberhumer G, Müller C: Prognostic significance of the hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology 2003, 125(4):1042-1052.
-
19Zhang J, Fallon MB: Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol 2012, 9(9):539-549.
Publication Dates
-
Publication in this collection
Jul-Sep 2014
History
-
Received
10 Sept 2013 -
Accepted
25 Feb 2014