Abstract
Objective:
This study aimed to compare the effects of two different perfusion techniques: conventional cardiopulmonary bypass and miniature cardiopulmonary bypass in patients undergoing cardiac surgery at the University Hospital of Santa Maria - RS.
Methods:
We perform a retrospective, cross-sectional study, based on data collected from the patients operated between 2010 and 2013. We analyzed the records of 242 patients divided into two groups: Group I: 149 patients undergoing cardiopulmonary bypass and Group II - 93 patients undergoing the miniature cardiopulmonary bypass.
Results:
The clinical profile of patients in the preoperative period was similar in the cardiopulmonary bypass and miniature cardiopulmonary bypass groups without significant differences, except in age, which was greater in the miniature cardiopulmonary bypass group. The perioperative data were significant of blood collected for autotransfusion, which were higher in the group with miniature cardiopulmonary bypass than the cardiopulmonary bypass and in transfusion of packed red blood cells, which was higher in cardiopulmonary bypass than in miniature cardiopulmonary bypass. In the immediate, first and second postoperative period the values of hematocrit and hemoglobin were higher and significant in miniature cardiopulmonary bypass than in the cardiopulmonary bypass, although the bleeding in the first and second postoperative days was higher and significant in miniature cardiopulmonary bypass than in the cardiopulmonary bypass.
Conclusion:
The present results suggest that the miniature cardiopulmonary bypass was beneficial in reducing the red blood cell transfusion during surgery and showed slight but significant increase in hematocrit and hemoglobin in the postoperative period.
Descriptores:
Cardiopulmonary Bypass; Perfusion; Postoperative Period
Resumo
Objetivo:
Este estudo teve como objetivo comparar os efeitos de duas técnicas de perfusão diferentes: convencional (CEC) e mini (MCEC) em pacientes submetidos à cirurgia cardíaca no Hospital Universitário de Santa Maria - RS.
Métodos:
Foi realizado um estudo retrospectivo, transversal, baseado em dados coletados dos pacientes operados entre 2010 e 2013. Foram analisados os registros de 242 pacientes divididos em dois grupos: Grupo I - 149 pacientes submetidos à circulação extracorpórea e Grupo II - 93 pacientes submetidos à minicirculação extracorpórea.
Resultados:
O perfil clínico dos pacientes no pré-operatório foi semelhante nos grupos circulação extracorpórea e minicirculação extracorpórea sem diferenças significativas, exceto na idade, maior no grupo minicirculação extracorpórea. Os dados perioperatórios foram significativos de sangue coletadas para autotransfusão, que foram maiores no grupo com minicirculação extracorpórea do que a circulação extracorpórea e na transfusão de concentrado de hemácias, superior em circulação extracorpórea do que em minicirculação extracorpórea. Nos valores pós-operatório imediato, primeiro e segundo, os níveis de hematócrito e da hemoglobina foram maiores e significativos na minicirculação extracorpórea que no circulação extracorpórea, embora o sangramento no primeiro e segundo dias pós-operatórios tenha sido maior e significativo no minicirculação extracorpórea que no circulação extracorpórea.
Conclusão:
Os resultados sugerem que a minicirculação extracorpórea foi benéfica em reduzir a transfusão de células vermelhas do sangue durante a cirurgia e houve discreta, mas significativa, elevação do hematócrito e hemoglobina no pós-operatório.
Descritores:
Circulação extracorpórea; Perfusão; Período pós-operatório
INTRODUCTION
Cardiac surgery had major limitations in the beginning, in the early twentieth century, for not being able to stop and open the heart to treat intracardiac lesions. However, from the development of an artificial heart-lung machine[11 Gibbon Jr. JH, Miller BJ, Feinberg C. An improved mechanical heart and lung apparatus. Med Clin N Am. 1953;1:1603-24.], showed great progress, especially with the development of cardiopulmonary bypass, progressively improved until 1954, when its use in humans has started[22 Gibbon JH Jr. Application of a mechanical heart and lung apparatus to cardiac surgery. Minn Med. 1954;37(3):171-85.]. Since that time this technique has become widespread worldwide and known as the largest contribution to cardiac surgery and cardiology for the world[33 Lillehei CW, Cohen M, Warden HE, Read RC, Aust JB, DeWall RA, et al. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot, and pulmonary atresia defects: report of first ten cases. Ann Surg. 1955;142(3):418-42.
4 Kirklin JW, Dushane JW, Patrick RT, Donald DE, Hetzel PS, Harshbarger HG, et al. Intracardiac surgery with the aid of a mechanical pump-oxygenator system (Gibbon type): report of eight cases. Proc Staff Meet Mayo Clin. 1955;30(10):201-6.-55 Dewall RA, Gott VL, Lillehei CW, Read RC, Varco RL, Warden HE, et al. A simple, expandable, artificial oxygenator for open heart surgery. Surg Clin North Am. 1956:1025-34.]. In Brazil this technique started in 1955[66 Felipozzi HJ, Santos RG, D'Oliveira LG, Perfeito JS. Cirurgia cardíaca a céu aberto com desvio extracorpóreo da circulação do coração direito. Resultados experimentais e primeiros casos clínicos. Previous note presented on the Department of Surgery at the Paulista Medical Association, on November 16, 1955.-77 Zerbini EJ, Jatene AD, Macruz R, Curi N, Verginelli G. Extracorporeal circulation in cardiac surgery. Report of first 50 cases. J Thorac Cardiovasc Surg. 1961;41:205-11.], followed by several surgeons[88 Jasbik W, Meier M, Jasbik A, Pernambuco P, Morais DJ. Modelo aperfeiçoado de coração-pulmão artificial compacto para perfusões com hemodiluição, normoterapia e hipotermia. Arq Bras Cardiol. 1967;20(suppl 1):112.
9 Gomes OM, Conceição DS, Nogueira D Jr, Mengai A, Moraes NL, Tsuzuki S, et al. Normothermal perfusion using am membrane oxigenator. Clinical study. Rev Assoc Med Bras. 1976;22(9):353-5.
10 Jatene AD, Souza JE, Paulista PP, de Souza LC, Kormann DS, de Magalhães HM, et al. Direct surgery of coronary artery obstructions. Arq Bras Cardiol 1969;22(6):255-64.
11 Braile DM. Extracorporeal circulation. Rev Bras Cir Cardiovasc. 2010;25(4):III-V.-1212 Morais DJ, Jazbik W, Franco S. Perfusão prolongada com hemólise mínima. Uso de plasma em substituição ao sangue no oxigenador. Rev Bras Cir. 1960:42:120.], which put the country in an international leading position in cardiovascular surgery with important contributions to the development and improvement of perfusion. However, with the method came the challenges to circulate blood into metal and plastic surfaces. The contact of blood with this surfaces predisposes to changes in blood components, such as red cells, white cells, platelets, and plasma lipoproteins, that can suffer degradation and partial destruction of these elements, resulting in anemia and tissue inflammatory reactions as the systemic inflammatory response syndrome (SIRS)[1313 Vohra HA, Whistance R, Modi A, Ohri SK. The inflammatory response to miniaturized extracorporeal circulation: a review of the literature. Mediators Inflamm. 2009;2009:707042.], need for transfusion with homologous red blood cells[1414 Ferraris VA, Ferraris SP. Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J. 1995;22(3):216-30.] and increased risk of postoperative infection[1515 Banbury MK, Brizzio ME, Rajeswaran J, Lytle BW, Blackstone EH. Transfusion increases the risk of postoperative infection after cardiovascular surgery. J Am Coll Surg. 2006;202(1):131-8.]. Because of this situation, various techniques were used, such as coronary artery bypass grafting without cardiopulmonary bypass (CPB) in 1955[1616 Kolesov VI, Potashov LV. Surgery of coronary arteries [in Russian]. Eksp Khir Anesteziol. 1965;10(2):3-8.], and later with other surgeons[1717 Benetti FJ, Naselli G, Wood M, Geffner L. Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest. 1991;100(2):312-6.
18 Benetti FJ. MINI-off-pump coronary artery bypass graft: long-term results. Future Cardiol. 2010;6(6):791-5.
19 Buffolo E, Andrade JC, Succi JE, Leão LE, Cueva C, Branco JN, et al. Revascularização direta do miocárdio sem circulação extracorpórea. Descrição da técnica e resultados iniciais. Arq Bras Cardiol. 1982;38(5):365-73.-2020 Lima RC, Escobar MAS, Lobo Filho JG, Diniz R, Saraiva A, Césio A, et al. Surgical results of coronary artery bypass grafting without cardiopulmonary bypass: analysis of 3,410 patients. Rev Bras Cir Cardiovasc. 2003;18(3):261-7.], with good results in relation to the CPB. But these technical limitations were reported as difficult as revascularization of the lower wall of the left ventricle, large cardiomegaly and severe heart failure. In these situations, the technique often resulted in incomplete revascularization[2121 Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.]. Another option found to the problems of CPB was to minimize the volume of the infusion, with the miniaturization of the cardiopulmonary bypass (MCPB). Afterwards, several studies published comparing the CPB with off pump surgery and the MCPB, finding lower presence of hemodilution, coagulopathy[2121 Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.] need for transfusion of red blood cells[2222 Baikoussis NG, Papakonstantinou NA, Apostolakis E. The "benefits" of the mini- extracorporeal circulation in the minimal invasive cardiac surgery area. J Cardiol. 2014;63(6):391-6.
23 Immer FF, Ackermann A, Gygax E, Stalder M, Englberger L, Eckstein FS, et al. Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg. 2007;84(5):1515-20.
24 Puehler T, Haneya A, Philipp A, Wiebe K, Keyser A, Rupprecht L, et al. Minimal extracorporeal circulation: an alternative for on-pump and off-pump coronary revascularization. Ann Thorac Surg. 2009;87(3):766-72.
25 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.
26 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.-2727 Silva LLM, Andres AJB, Senger R, Stuermer R, Godoi MCM, Correa EFM, et al. Impact of autologous blood transfusion on the use of pack red blood cells in coronary arterial bypass grafting surgery. Rev Bras Cir Cardiovasc. 2013;28(2):183-9.] and lower systemic inflammatory reaction in the surgery without CPB and MCPB in relation to the CPB[2828 Mazzei V, Nasso G, Salamone G, Castorino F, Tomasini A, Anselmi A. Prospective randomized comparison of coronary bypass with minimal extracorporeal circulation system (MECC) versus off-pump coronary surgery. Circulation. 2007;116(16):1761-7.]. It was also observed higher hemoglobin levels in MCPB than in CPB[2626 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.]. When comparing off-pump surgery and MCPB, the following effects were described: similar level of inflammatory response[2525 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.], but more controlled surgical field[2121 Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.], better coronary artery bypass grafting (CABG)[2525 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.] and higher level of hemoglobin in the MCPB than in off-pump. Other authors considered not significant the difference between CPB and the MCPB for bleeding, renal injury, length of stay[2929 Ried M, Kobuch R, Rupprecht L, Keyser A, Hilker M, Schmid C, et al. Reduced 30- day mortality in men after elective coronary artery bypass surgery with minimized extracorporeal circulation: a propensity score analysis. BMC Cardiovascular Disord. 2012;12:17.] and evolution of low-risk patients[3030 Svitek V, Lonsky V, Mandak J, Krejsek J, Kolackova M, Brzek V, et al. No clear clinical benefit of using mini-invasive extracorporeal circulation in coronary artery bypass grafting in low-risk patients. Perfusion. 2009;24(6):389-95.]. In our Service, at the University Hospital of Santa Maria, from 2010, we began using MCPB in CABG surgery. In 2011, we added to this technique an autotransfusion equipment with hemoconcentration. This year, a resident of anesthesia and Master's student, comparing patients undergoing coronary artery bypass surgery found less need and lower volume of packed red blood cells in the autotransfusion group than in those without its use[2828 Mazzei V, Nasso G, Salamone G, Castorino F, Tomasini A, Anselmi A. Prospective randomized comparison of coronary bypass with minimal extracorporeal circulation system (MECC) versus off-pump coronary surgery. Circulation. 2007;116(16):1761-7.]. Based on this initial experience, we decided to perform a retrospective analysis with a review of medical records of patients undergoing consecutive cardiac surgeries in 2010 to 2013 period, regarding the effects of two types of cardiopulmonary bypass: (with conventional CPB and MCPB) on the results of clinical and laboratory parameters of the periods before, during and after surgery. Considering the fact that this study was retrospective, we analyzed mainly the clinical aspects and changes in the hemoglobin, hematocrit, platelets, complications related to bleeding and the need of red blood pack transfusion during surgery and in the postoperative period.
METHODS
Ethical considerations
This study was reviewed and approved by the Research Ethics Committee of the Federal University of Santa Maria, RS, with number CAAE: 21598213.1.0000.5346 and order number: 434.030. Date: 08/10/2013.
Data were collected in chips (Chart 1), whose items refer to clinical, surgical and laboratory parameters of the pre-, intra- and postoperative surgery, with emphasis on hematological aspects, bleeding and transfusions, regarding the patients underwent conventional CPB and MCPB. The preoperative data refer to clinical and laboratory parameters collected before surgery; the perioperative are related to the period from the beginning to the end of surgery. The postoperative period was subdivided into three sub-periods: the early postoperative period (POI) between arrival at the Intensive Cardiology Unit (ICU) and 6:00 pm the following day, and then the first postoperative day (24 h after) and the second PO (48 h after).
In this study we analyzed the medical records of 242 patients who underwent surgery between 2010-2013, divided into two groups:
Group I (GI) - 149 patients undergoing surgery with conventional cardiopulmonary bypass (CPB).
Group II (GII) - 93 patients who underwent surgery with miniaturized cardiopulmonary bypass (MCPB).
The patients in GI underwent surgery with machine and conventional CPB circuits (Braile Biomédica®) and centrifugal pump (Maquet®). The GII, were operated circuit, centrifugal pump and MCPB Maquet® machine (Figure 1). Auto transfusion was performed by using a device named Autolog (Medtronic®) (Figure 2), when deemed necessary by the surgeon. The surgical procedures were performed by the usual techniques, corresponding to each system. Autolog® was used in both types of perfusion: 148 in the CPB group and 88 in the MCPB group. Data were tabulated in spreadsheet (Excel 2010 Windows®), and analyzed using the statistical package (SPSS 15.0)®, with test application T Student for parameters with normal distribution and Mann Whitney test for abnormal distribution, considering the significance of P<0.05. Inclusion criteria were cardiac surgeries performed sequentially in the period 2010-2013, and the exclusion were emergency surgery, reoperation and complex surgeries such as aneurysms and aortic dissection, given that our initial aim was to compare these perfusion techniques in routine surgery.
Maquet set consisting of mini bypass circuit connected to the centrifugal pump and the extracorporeal circulation machine.
RESULTS
The results were tabulated according to the analysis period: preoperative (Table 1), intraoperative (Table 2) and postoperative (Table 3). The clinical profile of patients preoperatively (Table 1) was similar in groups I (CPB) and II (mini CPB), differing only in age, the greater the mini CPB in relation to the CPB. (P<0.05). During the surgery (Table 2) there was no significant difference in duration of CPB and laboratory parameters and bleeding. There were significant differences in the collection of red blood cells for autologous transfusion (P<0.05) in the mini CPB in relation to the CPB and the volume of transfused red blood cells concentrate (Figure 3) was greater and significant in the CPB regarding the mini pump group (P<0.04).
Comparison of the type of infusion and compared to autologous transfusion concentrated red blood cell.
The immediate postoperative period (Table 3), with discrete higher values of hematocrit and hemoglobin in the mini CPB than in CPB (Figures 4 and 5), respectively, with significant differences (P<0.05). In the first and second postoperative period bleeding was also observed (Figure 6) and most significant in the mini CPB in relation to the CPB (P<0.05), however, despite this, the hematocrit and hemoglobin levels remained higher in mini CPB than in the CPB, with subtle differences, but significant (P<0.05). The complication about SIRS where referred in the Introduction, in the historic context of one important event that is related to CPB. However, in this study, we referred only the complications related to bleeding, need of RBC transfusion and change of erythrocytes, hematocrit, hemoglobin and platelets during surgery and postoperative period (Figure 7).
DISCUSSION
Cardiac surgery had major limitations in the beginning, in the early twentieth century, for not being able to stop and open the heart to treat intracardiac lesions, but with the development of an artificial heart-lung machine and extracorporeal circulation, the technique has become known and disseminated worldwide as the largest contribution to cardiac surgery and for the world cardiology.
However, success was accompanied by problems such as hematological disorders[1313 Vohra HA, Whistance R, Modi A, Ohri SK. The inflammatory response to miniaturized extracorporeal circulation: a review of the literature. Mediators Inflamm. 2009;2009:707042.], cognitive, and systemic inflammatory reactions[1414 Ferraris VA, Ferraris SP. Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J. 1995;22(3):216-30.] and infections[1515 Banbury MK, Brizzio ME, Rajeswaran J, Lytle BW, Blackstone EH. Transfusion increases the risk of postoperative infection after cardiovascular surgery. J Am Coll Surg. 2006;202(1):131-8.], resulting from direct blood contact with oxygen and non-endothelial surfaces like metal and plastic. These situations led to the search for solutions to work around the problem. Then emerged coronary revascularization without cardiopulmonary bypass[1616 Kolesov VI, Potashov LV. Surgery of coronary arteries [in Russian]. Eksp Khir Anesteziol. 1965;10(2):3-8.], technique followed by other surgeons, with good results in relation to the CPB[1414 Ferraris VA, Ferraris SP. Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J. 1995;22(3):216-30.
15 Banbury MK, Brizzio ME, Rajeswaran J, Lytle BW, Blackstone EH. Transfusion increases the risk of postoperative infection after cardiovascular surgery. J Am Coll Surg. 2006;202(1):131-8.-1616 Kolesov VI, Potashov LV. Surgery of coronary arteries [in Russian]. Eksp Khir Anesteziol. 1965;10(2):3-8.].
However, other challenges have emerged, especially in CABG as the difficult access to the lower wall of the heart, great cardiomegalies and severe heart failure, making it difficult to complete revascularization[2121 Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.]. Another option was the miniaturization of cardiopulmonary bypass described as good alternative by several authors[2121 Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.
22 Baikoussis NG, Papakonstantinou NA, Apostolakis E. The "benefits" of the mini- extracorporeal circulation in the minimal invasive cardiac surgery area. J Cardiol. 2014;63(6):391-6.
23 Immer FF, Ackermann A, Gygax E, Stalder M, Englberger L, Eckstein FS, et al. Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg. 2007;84(5):1515-20.
24 Puehler T, Haneya A, Philipp A, Wiebe K, Keyser A, Rupprecht L, et al. Minimal extracorporeal circulation: an alternative for on-pump and off-pump coronary revascularization. Ann Thorac Surg. 2009;87(3):766-72.
25 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.
26 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.
27 Silva LLM, Andres AJB, Senger R, Stuermer R, Godoi MCM, Correa EFM, et al. Impact of autologous blood transfusion on the use of pack red blood cells in coronary arterial bypass grafting surgery. Rev Bras Cir Cardiovasc. 2013;28(2):183-9.-2828 Mazzei V, Nasso G, Salamone G, Castorino F, Tomasini A, Anselmi A. Prospective randomized comparison of coronary bypass with minimal extracorporeal circulation system (MECC) versus off-pump coronary surgery. Circulation. 2007;116(16):1761-7.] and restrictions by other researchers[2929 Ried M, Kobuch R, Rupprecht L, Keyser A, Hilker M, Schmid C, et al. Reduced 30- day mortality in men after elective coronary artery bypass surgery with minimized extracorporeal circulation: a propensity score analysis. BMC Cardiovascular Disord. 2012;12:17.-3030 Svitek V, Lonsky V, Mandak J, Krejsek J, Kolackova M, Brzek V, et al. No clear clinical benefit of using mini-invasive extracorporeal circulation in coronary artery bypass grafting in low-risk patients. Perfusion. 2009;24(6):389-95.].
Currently, the mini CPB is establishing itself as a suitable technique to reduce perfusion problems and the use of homologous blood. In our experience, the results for preoperative parameters (Table 1) showed no significant variation, with the exception of age, with a slight but significant increase in the group with mini CPB compared to conventional CPB (P<0.05). These findings are consistent with those of other authors[2525 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.,2626 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.]. In the perioperative period the volume of blood collected autotransfusion: 274.80 (±345.97) was 48.98% higher and significant (P<0.05) in the group with mini CPB in relation to the CPB: 184.45 (±265.88), but the average volume of transfused red blood cells was 106,37 ml (±211.97) in the pump group and 49.13 ml (±133.29) in the mini-pump group, with a difference of 57.24 ml (-53.81%) of this in relation to the CPB (P<0.04), showing a favorable effect on the mini CPB in relation to the CPB.
These findings suggest that patients of mini CPB, being autotransfused during surgery had less need for homologous blood transfusion than CPB. This result was similar to the data of other authors who found mean values of homologous blood units of 0.8 unit/patient in the groups with mini pump and off-pump, and 1.8 unit/patient in the CPB[2525 Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.]. Another study showed that there was significant reduction in the volume of blood transfusion: 0.53±0.90 CH unit in mini CPB and 1.3±1.93 units in the CPB (P<0.05)[2626 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.].
In our study the postoperative period was subdivided into three sub-periods: the early postoperative period (POI), first and second day after surgery, with the intention to better assess the effects of infusion at this stage after surgery. The results of these periods were: POI - Bleeding data, the use of concentrated red blood cells and platelets were not significant, but the hematocrit and hemoglobin had mild elevation, but significant (P<0.03). The first and second PO - bleeding was slightly more pronounced in the mini CPB in relation to the CPB (P<0.04), but despite this, hematocrit and hemoglobin remained higher in mini CPB in relation to the CPB (P<0.05). However, it is remarkable that this bleeding did not contribute to the reduction of hematocrit and hemoglobin.
These results are similar to those by other authors who also reported high hematocrit[2222 Baikoussis NG, Papakonstantinou NA, Apostolakis E. The "benefits" of the mini- extracorporeal circulation in the minimal invasive cardiac surgery area. J Cardiol. 2014;63(6):391-6.] and hemoglobin[2626 Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.], after the use of mini CPB in relation to the CPB. In our research, the comparison between the two perfusion techniques showed better data on mini CPB in relation to the CPB, as referred to CPB and transfusion in the perioperative period and the results of red blood cells and hemoglobin, with statistically significant values. The results suggest that the mini CPB was beneficial in reducing the transfusion of packed red blood cells and higher levels of hematocrit and hemoglobin in trans- and postoperative period as mentioned in the literature. More studies are needed on the influences of the type of cardiopulmonary bypass and the use of autotransfusion and we are now working in in this matter to include in another study.
CONCLUSION
In our study, the comparison between the two types of perfusion showed better data in the MCPB, from the first period in which the patient was referred to bleeding and transfusion in the perioperative period and the results of red blood cells and hemoglobin, with statistically significant values. The results suggest that the MCPB is beneficial for the reduction of perioperative bleeding, showing higher levels of hematocrit and hemoglobin in trans- and postoperative periods, and especially on reducing the use of concentrated homologous red blood cells, as reported in the literature. We are aware that this matter needs more studies.
-
This study was carried out at Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil, and Hospital Universitário de Santa Maria (HUSM), Santa Maria, RS, Brazil.
-
Financial Support: Hospital Universitário de Santa Maria.
REFERENCES
-
1Gibbon Jr. JH, Miller BJ, Feinberg C. An improved mechanical heart and lung apparatus. Med Clin N Am. 1953;1:1603-24.
-
2Gibbon JH Jr. Application of a mechanical heart and lung apparatus to cardiac surgery. Minn Med. 1954;37(3):171-85.
-
3Lillehei CW, Cohen M, Warden HE, Read RC, Aust JB, DeWall RA, et al. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot, and pulmonary atresia defects: report of first ten cases. Ann Surg. 1955;142(3):418-42.
-
4Kirklin JW, Dushane JW, Patrick RT, Donald DE, Hetzel PS, Harshbarger HG, et al. Intracardiac surgery with the aid of a mechanical pump-oxygenator system (Gibbon type): report of eight cases. Proc Staff Meet Mayo Clin. 1955;30(10):201-6.
-
5Dewall RA, Gott VL, Lillehei CW, Read RC, Varco RL, Warden HE, et al. A simple, expandable, artificial oxygenator for open heart surgery. Surg Clin North Am. 1956:1025-34.
-
6Felipozzi HJ, Santos RG, D'Oliveira LG, Perfeito JS. Cirurgia cardíaca a céu aberto com desvio extracorpóreo da circulação do coração direito. Resultados experimentais e primeiros casos clínicos. Previous note presented on the Department of Surgery at the Paulista Medical Association, on November 16, 1955.
-
7Zerbini EJ, Jatene AD, Macruz R, Curi N, Verginelli G. Extracorporeal circulation in cardiac surgery. Report of first 50 cases. J Thorac Cardiovasc Surg. 1961;41:205-11.
-
8Jasbik W, Meier M, Jasbik A, Pernambuco P, Morais DJ. Modelo aperfeiçoado de coração-pulmão artificial compacto para perfusões com hemodiluição, normoterapia e hipotermia. Arq Bras Cardiol. 1967;20(suppl 1):112.
-
9Gomes OM, Conceição DS, Nogueira D Jr, Mengai A, Moraes NL, Tsuzuki S, et al. Normothermal perfusion using am membrane oxigenator. Clinical study. Rev Assoc Med Bras. 1976;22(9):353-5.
-
10Jatene AD, Souza JE, Paulista PP, de Souza LC, Kormann DS, de Magalhães HM, et al. Direct surgery of coronary artery obstructions. Arq Bras Cardiol 1969;22(6):255-64.
-
11Braile DM. Extracorporeal circulation. Rev Bras Cir Cardiovasc. 2010;25(4):III-V.
-
12Morais DJ, Jazbik W, Franco S. Perfusão prolongada com hemólise mínima. Uso de plasma em substituição ao sangue no oxigenador. Rev Bras Cir. 1960:42:120.
-
13Vohra HA, Whistance R, Modi A, Ohri SK. The inflammatory response to miniaturized extracorporeal circulation: a review of the literature. Mediators Inflamm. 2009;2009:707042.
-
14Ferraris VA, Ferraris SP. Limiting excessive postoperative blood transfusion after cardiac procedures. A review. Tex Heart Inst J. 1995;22(3):216-30.
-
15Banbury MK, Brizzio ME, Rajeswaran J, Lytle BW, Blackstone EH. Transfusion increases the risk of postoperative infection after cardiovascular surgery. J Am Coll Surg. 2006;202(1):131-8.
-
16Kolesov VI, Potashov LV. Surgery of coronary arteries [in Russian]. Eksp Khir Anesteziol. 1965;10(2):3-8.
-
17Benetti FJ, Naselli G, Wood M, Geffner L. Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest. 1991;100(2):312-6.
-
18Benetti FJ. MINI-off-pump coronary artery bypass graft: long-term results. Future Cardiol. 2010;6(6):791-5.
-
19Buffolo E, Andrade JC, Succi JE, Leão LE, Cueva C, Branco JN, et al. Revascularização direta do miocárdio sem circulação extracorpórea. Descrição da técnica e resultados iniciais. Arq Bras Cardiol. 1982;38(5):365-73.
-
20Lima RC, Escobar MAS, Lobo Filho JG, Diniz R, Saraiva A, Césio A, et al. Surgical results of coronary artery bypass grafting without cardiopulmonary bypass: analysis of 3,410 patients. Rev Bras Cir Cardiovasc. 2003;18(3):261-7.
-
21Harling L, Punjabi PP, Athanasiou T. Miniaturized extracorporeal circulation vs. off- pump coronary artery bypass grafting: what the evidence shows? Perfusion. 2011;26(Suppl 1):40-7.
-
22Baikoussis NG, Papakonstantinou NA, Apostolakis E. The "benefits" of the mini- extracorporeal circulation in the minimal invasive cardiac surgery area. J Cardiol. 2014;63(6):391-6.
-
23Immer FF, Ackermann A, Gygax E, Stalder M, Englberger L, Eckstein FS, et al. Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg. 2007;84(5):1515-20.
-
24Puehler T, Haneya A, Philipp A, Wiebe K, Keyser A, Rupprecht L, et al. Minimal extracorporeal circulation: an alternative for on-pump and off-pump coronary revascularization. Ann Thorac Surg. 2009;87(3):766-72.
-
25Panday GF, Fischer S, Bauer A, Metz D, Schubel J, El Shouki N, et al. Minimal extracorporeal circulation and off-pump compared to conventional cardiopulmonary bypass in coronary surgery. Interact Cardiovasc Thorac Surg. 2009;9(5):832-6.
-
26Perthel M, Klingbeil A, El-Ayoubi L, Gerick M, Laas J. Reduction in blood product usage associated with routine use of mini bypass systems in extracorporeal circulation. Perfusion. 2007;22(1):9-14.
-
27Silva LLM, Andres AJB, Senger R, Stuermer R, Godoi MCM, Correa EFM, et al. Impact of autologous blood transfusion on the use of pack red blood cells in coronary arterial bypass grafting surgery. Rev Bras Cir Cardiovasc. 2013;28(2):183-9.
-
28Mazzei V, Nasso G, Salamone G, Castorino F, Tomasini A, Anselmi A. Prospective randomized comparison of coronary bypass with minimal extracorporeal circulation system (MECC) versus off-pump coronary surgery. Circulation. 2007;116(16):1761-7.
-
29Ried M, Kobuch R, Rupprecht L, Keyser A, Hilker M, Schmid C, et al. Reduced 30- day mortality in men after elective coronary artery bypass surgery with minimized extracorporeal circulation: a propensity score analysis. BMC Cardiovascular Disord. 2012;12:17.
-
30Svitek V, Lonsky V, Mandak J, Krejsek J, Kolackova M, Brzek V, et al. No clear clinical benefit of using mini-invasive extracorporeal circulation in coronary artery bypass grafting in low-risk patients. Perfusion. 2009;24(6):389-95.
Publication Dates
-
Publication in this collection
Jul-Aug 2015
History
-
Received
17 Feb 2015 -
Accepted
23 June 2015



 *P<0.05; mini CPB=miniaturized cardiopulmonary bypass.
*P<0.05; mini CPB=miniaturized cardiopulmonary bypass.
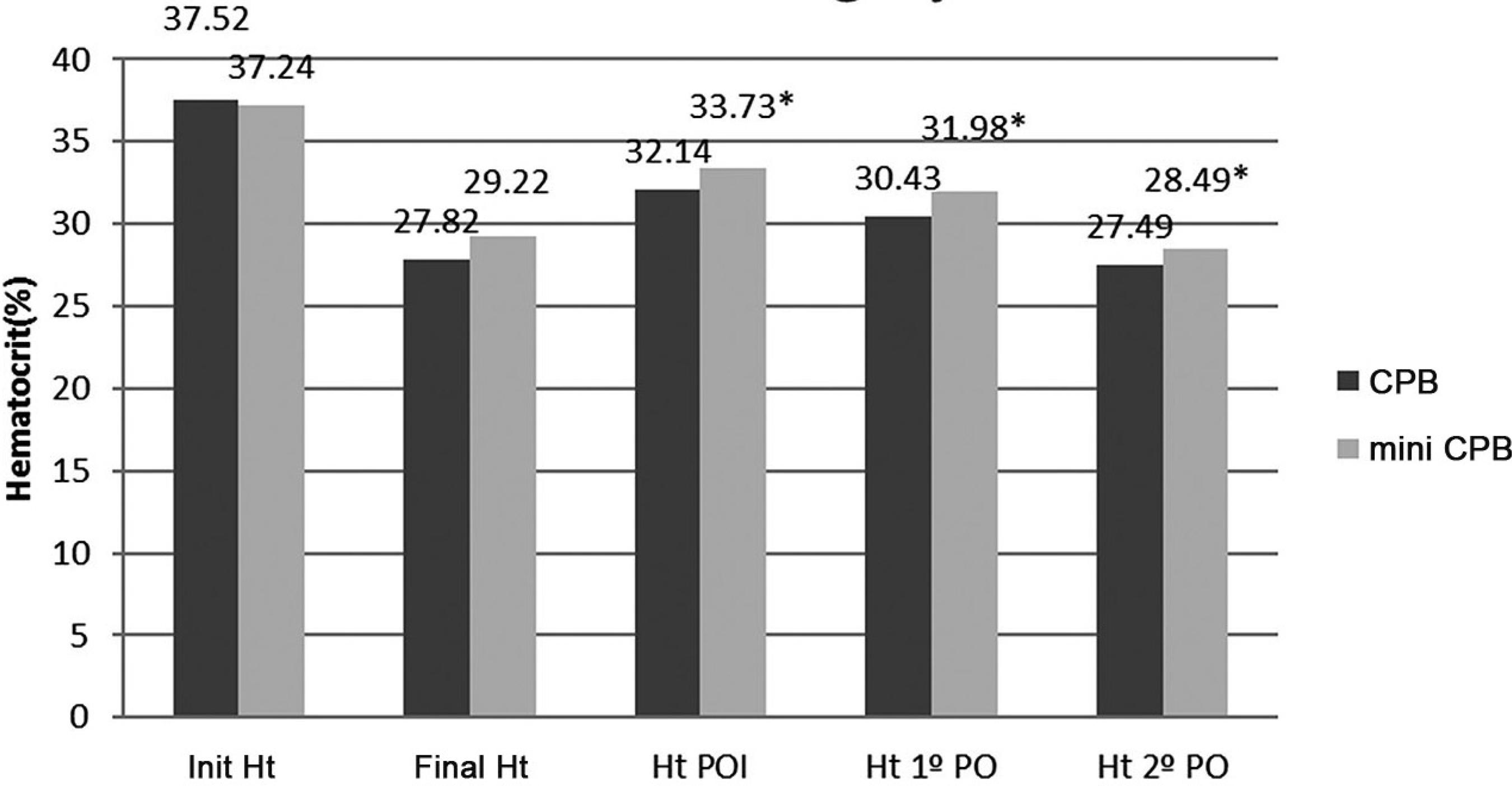 *P<0.05; Init Ht=initial hematocrit; Final Ht=final hematocrit; Ht POI=hematocrit on the immediate postoperative period; Ht 1 PO= hematocrit on the first day after surgery; Ht 2 PO= hematocrit on the second day after surgery.
*P<0.05; Init Ht=initial hematocrit; Final Ht=final hematocrit; Ht POI=hematocrit on the immediate postoperative period; Ht 1 PO= hematocrit on the first day after surgery; Ht 2 PO= hematocrit on the second day after surgery.
 *P<0.05; Init Heb=initial hemoglobin; Final Hb=final hemoglobin; Hb POI=hemoglobin on the immediate postoperative period; Heb 1 PO=hemoglobin on the first day after surgery; Heb 2 PO=hemoglobin on the second day after surgery.
*P<0.05; Init Heb=initial hemoglobin; Final Hb=final hemoglobin; Hb POI=hemoglobin on the immediate postoperative period; Heb 1 PO=hemoglobin on the first day after surgery; Heb 2 PO=hemoglobin on the second day after surgery.
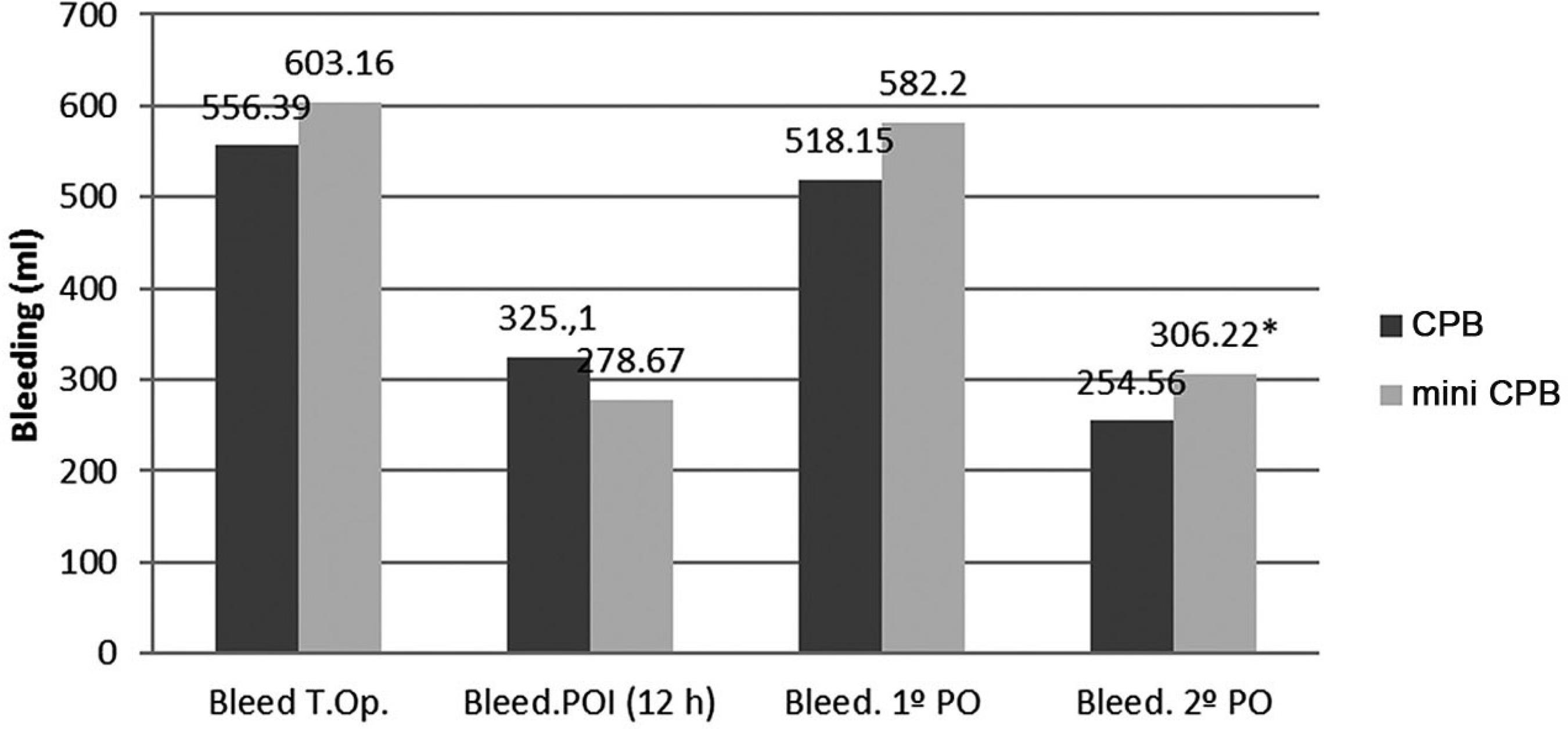 *P<0.05; Bleed T.Op=postoperative bleeding; Bleed POI=bleeding on the immediate postoperative period; Bleed. 1º PO=bleeding on the first day after surgery; Bleed. 2º PO=bleeding on the second day after surgery.
*P<0.05; Bleed T.Op=postoperative bleeding; Bleed POI=bleeding on the immediate postoperative period; Bleed. 1º PO=bleeding on the first day after surgery; Bleed. 2º PO=bleeding on the second day after surgery.
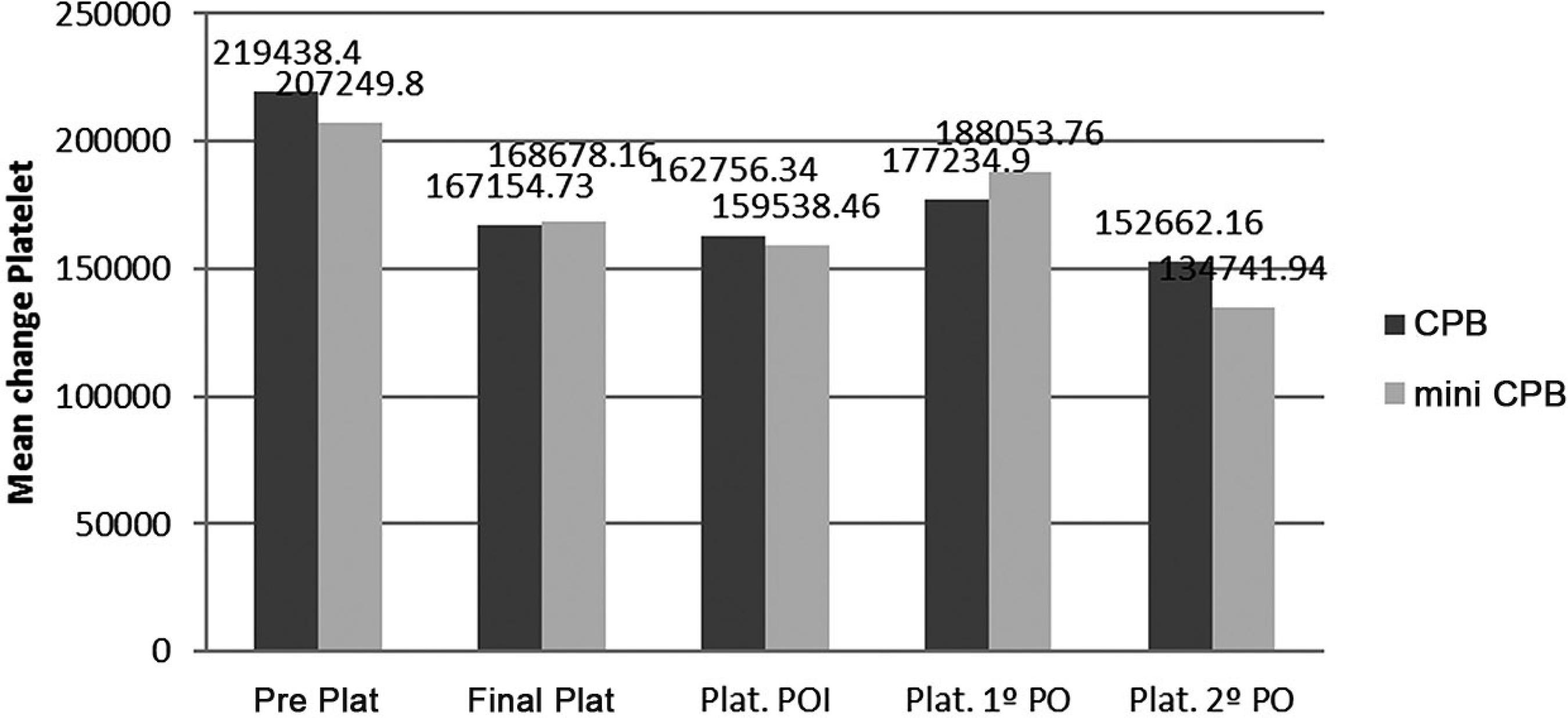 *P>0.05; Pre Plat=previous platelets; Final Plat=final platelets; Plat POI=platelets on the postoperative period; Plat. 1º PO=platelets on the first day after surgery; Plat. 2º PO =platelets on the second day after surgery.
*P>0.05; Pre Plat=previous platelets; Final Plat=final platelets; Plat POI=platelets on the postoperative period; Plat. 1º PO=platelets on the first day after surgery; Plat. 2º PO =platelets on the second day after surgery.