Abstract
The authors present a retrospective study of 60 patients with abdominal dystrophies, both with and without hernias, operated on in the period between 01 June 1994 and 30 January 1996. Their average age was 47 years. The incision at hernia itself and the dystrophic abdomen were the principal objects of the study. The authors show the importance of abdominal dermolipectomy for the complete recovery of the patient as well as demonstrate how it facilitates the technical manipulation of hernias. The technique of bilateral, longitudinal peritonio-aponeurotic transposition {the technique of Alcíno Lázaro da Silva) was used for large incisional hernias. A variation of this technique, for hernias with a hernial ring of up to 10 cm, is proposed by the authors, which consists in the closing of the ring and the reinforcement of the suture with the hernial sac. A revision is made of the results of these procedures realized in isolation and accompanied with abdominal dermolipectomy. Forty-nine recovered without complications (81.66%), three relapsed (5%), one necrosis of the midline with respiratory failure (1.67%), one little stitch gap (1,67%), two umbilical stenosis (3,33%), two wound abscess (3.33%), one cutaneous fistula (1,67%) and one death from pulmonary embolism (1.66%).
Ventral Hernia; Plastic Surgery
CASE SERIES
Dystrophies of the abdominal wall in adults. Surgical treatment1 1 Article from Dept. of "Clínica Integrada I" - Federal University of Pará - Brazil.
Jayme Fortunato AthiasI; António Carlos Bentes HortaII; Glaucilene Aragão FrancoII; Alexandre Augusto Mekdec da SilvaIII; Mauro Santos NevesIII; Sadia Martins de Paula SouzaIII; Sérgio Alexandre da Costa PereiraIII
IM.D., PhD
IIM.D.
IIIStudents
Address reprint request Address reprint request: Jaime Fortunato Athias Universidade Federal do Pará Departamento de Clínica Integrada I da UFPa. Campus Universitário Belem-Pará-Brazil
SUMMARY
The authors present a retrospective study of 60 patients with abdominal dystrophies, both with and without hernias, operated on in the period between 01 June 1994 and 30 January 1996. Their average age was 47 years. The incision at hernia itself and the dystrophic abdomen were the principal objects of the study. The authors show the importance of abdominal dermolipectomy for the complete recovery of the patient as well as demonstrate how it facilitates the technical manipulation of hernias. The technique of bilateral, longitudinal peritonio-aponeurotic transposition {the technique of Alcíno Lázaro da Silva) was used for large incisional hernias. A variation of this technique, for hernias with a hernial ring of up to 10 cm, is proposed by the authors, which consists in the closing of the ring and the reinforcement of the suture with the hernial sac. A revision is made of the results of these procedures realized in isolation and accompanied with abdominal dermolipectomy. Forty-nine recovered without complications (81.66%), three relapsed (5%), one necrosis of the midline with respiratory failure (1.67%), one little stitch gap (1,67%), two umbilical stenosis (3,33%), two wound abscess (3.33%), one cutaneous fistula (1,67%) and one death from pulmonary embolism (1.66%).
Subject headings: Ventral Hernia. Plastic Surgery.
INTRODUCTION
Abdominal dystrophy may or not be accompanied by congenital and or acquired abdominal weakness. Of these, the greatest challenge are large incisional hernias.
Acquired abdominal dystrophies, in the majority of cases, is due to obesity and in females who had many child birth. Nevertheless, it is not rare to observe important acquired abdominal dystrophies in patients with no record of childbirth, principally in those who have lost much weight as a consequence of reducing diets14
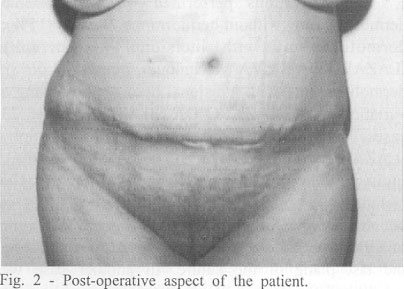
Another group of patients is found among the thin, but who as a result of multiple childbirths have an anesthetic aspect leading to a decline in self- esteem. As a result of these situations, dermolipectomy is mandatory for the surgical cure of abdominal dystrophy, known clinically as abdominal apron (Figs. 1 e 2) In addition, abdominal plastic surgery makes other surgical intervention easier, especially pelvic. The procedure does not increase post-operatory complications.
Incisional hernias are more frequently located in the median infra-umbilical region2,3,11,12. Other locations, in order of frequency, are: right iliac cavity; left iliac cavity; and right hypochondrium. With the advent of esternotomies and the extension of the incision to the upper third of the abdomen, we have various cases of supra-umbilical hernias, below the xiphoid process, the place of the drain of the operation.
The incidence11,12 may vary from 47.14% to60.42% in gynecological and obstetric surgery. Among other factors which influence the etiology of incisional hernias are: infection of the operatory wound; thick drains exposed by the incision itself; and imperfect closing of the muscles and aponeurosis layers1,11,12. Continual peritoneal dialyses are also cited as causes of abdominal hérnias6,22. Cases have been related of incisional hernias at the places of penetration of instruments for video-laparoscopic surgery, including the incarceration of triem8,10,17. Pre-pubic hernias have also been described15.
Among the best known procedures are those of CATTEL1, LEX11,12, LÁZARO DA SILVA9,16, and SLIM et al.18.
Over time, various materials have been employed to reinforce large, incisional hernias. Thus, total grafts of skin, autogenoic dermal grafts4, transplant of dermal corion5, fascia lata and hard polypropylene mesh. The latter, when placed in contact with subcutaneous cellular tissue, runs the risk of producing fistulas and rejections. In direct contact with the intestinal loops, may cause digestive fistulas5.
The objective of this study is to evaluate bilateral, longitudinal peritoneum-aponeurotic transposition technique and a variation of this technique for small and medium hernias, and to demonstrate that the execution of abdominal dermolipectomy associated with the cure of abdominal weakness is very important to give the patients back the quality of life compromised by abdominal dystrophies.
METHOD
In the period between 01 June 1994 and 30 January 1996, sixty patients referred from the Brazilian National Health Service (Sistema Único de Saúde -SUS) were operated on at São Marcos, Clínica dos Acidentados, and Sírio-Libanês Hospitais with support from the Division of Research and Post-Graduation at the Federal University of Para. Of the 60 patients, 52 were female (86.66%) and 8 male (13.34%). Their ages ranged from 26 to 70 years, with an average of 47 years.
Before surgery, the patients were submitted to rigorous routine clinical and laboratory examinations. When we suspected other pathologies, we requested other exams, such as ultrasonography of the upper abdomen and pelvis. For those patients that were to be submitted to simultaneous vaginal surgery, exams for prevention cancer of the uterine colon and direct examination and culture and antibiotic-sensibility of vaginal secretion were realized. For those patients that would have dermolipectomy, we recommended three baths daily for three days before the operation with tensoactive substances to wash the head and abdomen.
We carried out the dermolipectomy using the technique of Grazer. In 2 cases, of obese patients, we used the technique of Pitanguy to avoid "pig's car" at the extremities of the incision by which the skin and subcutaneous cellular tissue are moved until the borderline on the ribs and the xiphoid process. During the operation, we sprayed Rifampicine over the fat-cutaneous retails and the lifted surface which is drained with a vacuum system. The bandage used was compressive with the belt itself sterilized.
a) Surgical technique used were of incisional herniorraphy with bilateral median longitudinal peritoneum-aponeurotic transposition (technique of LÁZARO DA SILVAV6): 1) Incision over the previous scar without affecting the herniary sac; 2) Careful dissection of the same; 3) Opening of the sac and freeing of adherences, when they exist; 4) Longitudinal incisions (both 1.5 cm from the edge of the muscle) one on the posterior sheath and peritoneum of the abdominal rectus muscle and the other on the anterior surface of the sheath of the abdominal rectus muscle; 5) Continuous suture on the edge of the herniary sac on the posterior surface of the lateral edge of the abdominal rectus muscle. This suture closes the abdominal cavity and covers the blood thirsty posterior surface of the abdominal rectus; 6) Suture of the median edges of the abdominal rectus muscles, thus remaking the midline; 7) The third plane, anterior and on the surface, is formed by the long edge of the remaining herniary sac on the lateral edge of the anterior face of the abdominal rectus muscle, thus reconstituting the anterior sheath of the muscle and recovering the bloodthirsty area of the same (Figs. 3 and 8) Draining by vacuum and application of compressive bandages.
b) Variation on the technique of LÁZARO DA SILVAV6: 1) Careful dissection of the herniary sac; 2) Incision of the herniary sac and freeing of adherences; 3) Suture of the edged of the herniary ring with stitches; 4) Reinforcement of the previous suture using herniary sac performed with an overlapped suture or even an edge to edge one, depending on the case.
In cases of dermolipectomy, in addition to routine procedures, the patients remained for three days in the Fowley position, after which the drains were removed and the patient released. The stitches were removed gradually over a period of 15 days.
Follow-up was done by means of mailed reminders.
RESULTS
The operations performed were: abdominal dermolipectomy without herniorraphy, 9 cases (15%); dermolipectomy with incisional herniorraphy (LÁZARO DA SILVA's technique), 7 cases (11,66%); dermolipectomy with incisional herniorraphy using a variation on the LÁZARO DA SiLVA technique, 23 cases (38.33%); isolated incisional herniorraphy (LÁZARO DA SlLVA's technique), 4 cases (6.66%); incisional herniorraphy (with variation of the technique), 6 cases (10%); and 1 case (1.66%) in which there was no herniary sac using the technique of Cattle modified with propylene mesh substituting the last plane of the suture. In another case we substituted the second plane of the transposition for a prosthesis, which was placed between the two peritoneal sheaths (Table I).
When the umbilical hernia is small an dor is not compromised by an incisional hernia, we correct it in order to use the umbilical scar to improve esthetic appearance. When that is not possible, we build a neo-umbilicus which does not usually give good results.
As to the location of incisional hernias, there were: 30 cases (50%) in the median infra-umbilical region; 6 cases (10%) in the median supra-umbilical region; 5 cases (8.33%) in the right para-retal; and 1 case (1.67%) in the lumbar region. The average birthrate was 5.7 births. There were 31 cases (51.66%) of patients with a pervious history of suppuration. The simultaneous operations were: cholecystistectomies, 2 cases (3.33%); perineoplasties 6 cases (10%); and hysterectomy, 2 cases (3.33%).
Other hernias were operated on associated with dermolipectomies with or without incisional herniorraphy (Table II).
Of the 60 patients operated on, 49 (81.66%) did not present complications. Those that did occur are shown on table III.
DISCUSSION
Abdominal hernias, mainly incisional, when they occur in "normal" abdomens may at times be corrected easily and others with difficulty, depending on their size and local conditions. However, when they occur in deformed abdomens, principally because of obesity or childbirths, their treatment is more complex and requires dermolipectomy as mandatory for the success of surgical therapy, since it facilitates the manipulation of the herniary sac as well as forming a real belt of skin that becomes an aid to hernia! correction14.
The patient will only reach full quality of life if the plastic surgery of the abdomen is carried out as well. Some patients require correction of perineal lacerations and urinary incontinence which are also consequences of a badly conducted deliveries. In this cases the gynecologist performed the surgery. As a result of these factors we are of the opinion that dermolipectomy should be a technique of the general surgeon, since it is a procedure simple to execute and results in enormous benefits for the patient
The LÁZARO DA SILVA's technique avoids the use of prostheses and their complications. We have had cases of persistent fistulas, and even with the screen being exposed. His technique is easy to carry out, produces few complications, and very low indices of relapse9. In our experience, the case of relapse that we had with a very large infra-umbilica! para-retal right-side incisional hernia was a consequence of a vary large abscess. The size of the relapsed is that of a hernial ring of approximately 1.5 cm and does not interfere in the quality of life of the patient.
The variation on the LÁZARO DA SILVA's technique is used in incisional hernias with up to 10 cm of hernial ring which have been closed without tension. It has the advantage of avoiding aponeurotic displacements, at times extensive, and it is of simpler execution than transposition, which is used for rings larger than 10 cm. Our two relapses (one right para-retal and the other median infra-umbilical) occurred in a patient submitted to physical exertion shortly after surgery and another that had a cough in the same period. One of there has already been operated on (the one with the right para-retal hernia) using approach of the aponeurosis without opening the herniary sac.
Progressive pneumoperitoneum, used as an auxiliary procedure in large incisional hérnias7 presents risks such as haemorrhage and peritonitis and may lead to death9. On the LÁZARO DA SILVA's technique is not required.
CONCLUSION
Dermolipectomy is mandatory for the cure of abdominal dystrophies, and in addition, facilitates the treatment of hernias because of the better exposure of them. It should be carried out for the success of the surgical treatment of abdominal dystrophies whether or not they are accompanied by hernias.
The technique of bilateral longitudinal peritoneum-aponeurotic transposition gives results that qualify it as a procedure of first choice for large incisional hernias.
The variation on the LÁZARO DA SILVA's technique is effective in addition to easy execution, with a low rate of relapse.
Accepted for publication on february, 1996.
- 1. BEVILACQUA, R.G. & MELO Jr., F.F. - Cirurgia das hernias umbilicais e incisionais. In; GOFFI, F.S. Técnica Cirúrgica, Rio de Janeiro: Atheneu, 1978, p. 585-8.
- 2. CATALDO, M.L.S. - Emprego do saco herniário na correção cirúrgica das hernias logitudinais - aspectos experimentais. Belo Horizonte. 1977. [Tese-Mestrado-Universidade Federal de Minas Gerais]
- 3. CAVALCANTI, M.A. - Tratamento cirúrgico das grandes eventrações e lipodistrofias abdominais. Rev. Col. Bros. Cir., 9:291-4, 1982.
- 4. CHARETOM. B., LANDREN. S., BARDAXOGLOU, E., TERBLANCHE, J., LAUNOIS, B. - Lasing tecnique using derma! autografts for the management of large incisional hernias. Acta Chir. Belg., 94:291-4, 1994.
- 5. HU, TAM M, SALAPA, M., JAMRI, S. J. - Corion transplantation in reconstruction of ventral hernias. Bratisl Lek listy, 95:228-31, 1994.
- 6. IMVRIOS, G., TSAKIRIS, D., GAKIS, D., TAKOUDAS, D., KOUKOUDÍS, P., PAPAD1MÍTRIOU, M., ANTONIADIS, A. - A prostetic mesh repair of multiple recurrent and large abdominal hernias in continuous ambulatory peritoneal dialysis patients Perit Dial Int, 14: 338-43, 1994.
- 7. KAKHNOVSKI, I.M., ANTROPOVA, N.V., SOLOMATIN, A.S., MARKOVA, Z.S., VDONIVA, T.I. - Hemodinamyc changes in patients with large postoperative ventral hernias Klin Med (Mosk), 72:50-2, 1994.
- 8. KANAMARU, H., ODAKA, A., HORIE, Y., MAKITA,Y.A. - Case of external supravesical hernia repair with laparoscopic surgery Nippon Geka Gakai Zasshi, 96:121-4, 1995.
- 9. KATER, N. & MIGUEL, J. - Análise de 90 pacientes portadores de hernia incisional operados pela técnica de Lázaro da Silva.- Rev. Col Brás. Cir., 20:251-5, 1993.
- 10. KOPELMAM, D., SCFIEIN, M. ASSALIA, A., HASHMONAI, M. - Small bowel obstruction following laparoscopic cholecystectomy diagnosis of incisional hernia by computed tomography Surg. Laporosc. Endosc, 4:325-6, 1994.
- 11. LEX, A.; RAIA, A.A. - Hernia Incisional In. Zerbini, E.J. Clínica Cirúrgica Alípio Corrêa Netto, São Paulo: Sarvier, 1974. p. 100-107.
- 12. LEX, A. - Tratamento cirúrgico das hernias incisionais. In. Atualização cirúrgica. São Paulo. Manole, 1975, p.195-213.
- 13. PITANGY, I. - Abdosninoplasticas. O Hospital, 171:1541- 56, 1967.
- 14. PONTES, R. - Plástica abdominal: importância de sua associação à correção das hernias incisionais. Rev. Brás. de Cir., 52:85-92, 1966.
- 15. NORRIS, J.P., FLANINGAN, R.C., PICKLEMAN, J. - Parapubic hernia following radical retropubic prostatectomy. Urology, 44:922-3, 1994.
- 16. SILVA, A.L. - Bilateral surgical correction of longitudinal median, paramedian internal and eternal pararectal incisional hernias and diastasis. Arq. Brás. Cir. Dig., 2:50-63, 1987.
- 17. STORMS, P., STUYVEM, G., VANHEMELEN, G., SEBRECHTS, R. - Incarcerated troccar-wound hernia after laparoscopic hystereclomy. Is closure of farge trocar fascia defects after laparoscopy necessary? Surg Endosc, 5:901-2, 1994.
- 18. SLIM, K., PEZET, D., CHIPPONI, J. - Les grande eventracion de Ia paroi abdominale. Une technique de plastie aponevrotique associe a une prothesc. Press Med, 23:1815-6, 1994.
- 19. SUH, H., WADHWA., N.K., CABRALDA, T, SOKUMBI,D.; PINARD, B. - Abdominal wall hernias in ESRD patients receiving peritoneal dyalisis. Adv. Perit. Dial., v. 10, p. 85-8, 1994.
Publication Dates
-
Publication in this collection
01 Dec 2010 -
Date of issue
Mar 1997