Abstracts
PURPOSE: To compare the capsular reaction to two different coverings of silicone prosthesis through the biophysical characteristic of adherence and microscopical aspects of the inflammatory reaction and collagen formation. METHODS: Thirty two Wistar rats were used. In the dorsum of each animal a silicone elastomer with a smooth superficies and another coated with texturized silicone (Mentor) was implanted. Another one, with the same smooth superficies and other coated with silicone foam (Lifesil), making up in each side, of the dorsum, the texturized and silicone foam group respectively. The animals were split into four groups to be evaluated at 7, 14, 30 and 60 days. On the evaluation dates the implant adherence was verified witch a tensiometer and the values in kgf were obtained. The material was sent to histological analysis with hematoxilin-eosin and picrosirius colorations, to evaluate the inflammatory reaction and collagen synthesis, respectively. The obtained data were submitted to statistical treatment. RESULTS: There was more adherence of the tissue to the silicone foam (P<0,001). The inflammatory reaction was more intense in the same group, but without statistical significance. The number of giant cells and granulomas were more frequent in the silicone foam group. There was statistical significance at the 60 days for granulomas (P<0,028) and for all subgroups about number of giant cells (P< 0,012 to P<0,036). The thickness of the capsule in the silicone foam group was bigger, with statistical significance at seven days (P<0,028) and 60 days (P<0,012). The collagen deposition showed no difference in statistical analysis. CONCLUSION: The capsular reaction to the silicone foam showed stronger adherence, bigger thickness and had more number of granulomas and giant cells. No difference was observed in the intensity of inflammatory reaction in relation to type I and III collagen, when compared to the texturized cover.
Breast Implantation; Silicones; Biocompatible Materials; Contracture; Rats
OBJETIVO: Comparar a reação capsular de dois revestimentos de próteses de silicone através da característica biofísica de aderência e dos aspectos microscópicos de reação inflamatória e formação de colágeno. MÉTODOS: Implantaram-se no dorso de 32 ratos duas membranas de silicone ambas possuindo uma superfície lisa e outra diferindo em sua estrutura. Estes revestimentos foram de espuma de silicone (LifeSil) ou silicone texturizado (Mentor). Os dois grupos foram divididos em quatro sub-grupos conforme o tempo de pós-operatório avaliado: 7, 14, 30 e 60 dias. Obteve-se material para análise biofísica de aderência, a qual foi realizada com tensiômetro para obtenção de valores em kgf. O estudo microscópico da reação inflamatória e síntese de colágeno foi realizado com colorações de hematoxilina-eosina e picrosirius. Os dados foram submetidos a testes para avaliação da significância estatística. RESULTADOS: Houve maior aderência do revestimento de espuma de silicone ao tecido capsular, sendo este valor estatisticamente significativo (P<0,001). Quanto à reação inflamatória observou-se maior intensidade também neste grupo, porém sem significância estatística. Na contagem de células gigantes e granulomas os valores foram maiores para o grupo espuma de silicone com significância estatística no sub-grupo 60 dias (P<0,028) para número de granulomas; e em todos os sub-grupos (variando de P<0,012 a P<0,036) para o número de células gigantes. A reação capsular à espuma de silicone foi mais espessa, com significância estatística nos sub-grupos sete dias (P<0,028) e 60 dias (P<0,012). No estudo da síntese de colágeno, as diferenças não foram significantes estatisticamente. CONCLUSÃO: A reação capsular ao revestimento de espuma de silicone apresentou características de ter maior aderência ao tecido peri-implante, ser mais espesso, possuir maior número de granulomas e células gigantes de corpo estranho. Não demonstrou diferença quanto à intensidade da reação inflamatória em relação ao colágeno tipo I e tipo III, quando comparado ao revestimento texturizado.
Implante Mamário; Silicones; Materiais Biocompatíveis; Contratura; Ratos
6 - ORIGINAL ARTICLE
WOUND HEALING
Healing reaction to mammary prostheses covered by textured silicone and silicone foam in rats1 1 Research performed at Principles of Surgery, Postgraduate Program, Evangelical Medical School, Curitiba-PR, Brazil.
Reação capsular aos revestimentos de próteses mamárias de silicone texturizado e espuma de silicone em ratos
Cynthia Maria S. Rojas BalderramaI; Jurandir Marcondes Ribas-FilhoII; Osvaldo MalafaiaII; Nicolau Gregori CzeczkoII; Uli Alexandre DietzII; Danielle Giacometti SakamotoIII; Leandra Pauletto Muniz BittencourtI
IMaster, Principles of Surgery Postgraduate Program, Evangelical Medical School, Curitiba-PR, Brazil
IIPhD, Full Professor, Postgraduate Program, Evangelical Medical School, Curitiba-PR, Brazil
IIIPathologist, University Evangelic Hospital of Curitiba, Curitiba-PR, Brazil
Correspondence Correspondence: Cynthia Maria S. Rojas Balderrama Al. Augusto Stellfeld, 1980 80730-150 Curitiba - PR Brazil Phone: (55 41)3240-5488 ipem@evangelico.org.br
ABSTRACT
PURPOSE: To compare the capsular reaction to two different coverings of silicone prosthesis through the biophysical characteristic of adherence and microscopical aspects of the inflammatory reaction and collagen formation.
METHODS: Thirty two Wistar rats were used. In the dorsum of each animal a silicone elastomer with a smooth superficies and another coated with texturized silicone (Mentor) was implanted. Another one, with the same smooth superficies and other coated with silicone foam (Lifesil), making up in each side, of the dorsum, the texturized and silicone foam group respectively. The animals were split into four groups to be evaluated at 7, 14, 30 and 60 days. On the evaluation dates the implant adherence was verified witch a tensiometer and the values in kgf were obtained. The material was sent to histological analysis with hematoxilin-eosin and picrosirius colorations, to evaluate the inflammatory reaction and collagen synthesis, respectively. The obtained data were submitted to statistical treatment.
RESULTS: There was more adherence of the tissue to the silicone foam (P<0,001). The inflammatory reaction was more intense in the same group, but without statistical significance. The number of giant cells and granulomas were more frequent in the silicone foam group. There was statistical significance at the 60 days for granulomas (P<0,028) and for all subgroups about number of giant cells (P< 0,012 to P<0,036). The thickness of the capsule in the silicone foam group was bigger, with statistical significance at seven days (P<0,028) and 60 days (P<0,012). The collagen deposition showed no difference in statistical analysis.
CONCLUSION: The capsular reaction to the silicone foam showed stronger adherence, bigger thickness and had more number of granulomas and giant cells. No difference was observed in the intensity of inflammatory reaction in relation to type I and III collagen, when compared to the texturized cover.
Key words: Breast Implantation. Silicones. Biocompatible Materials. Contracture. Rats.
RESUMO
OBJETIVO: Comparar a reação capsular de dois revestimentos de próteses de silicone através da característica biofísica de aderência e dos aspectos microscópicos de reação inflamatória e formação de colágeno.
MÉTODOS: Implantaram-se no dorso de 32 ratos duas membranas de silicone ambas possuindo uma superfície lisa e outra diferindo em sua estrutura. Estes revestimentos foram de espuma de silicone (LifeSil) ou silicone texturizado (Mentor). Os dois grupos foram divididos em quatro sub-grupos conforme o tempo de pós-operatório avaliado: 7, 14, 30 e 60 dias. Obteve-se material para análise biofísica de aderência, a qual foi realizada com tensiômetro para obtenção de valores em kgf. O estudo microscópico da reação inflamatória e síntese de colágeno foi realizado com colorações de hematoxilina-eosina e picrosirius. Os dados foram submetidos a testes para avaliação da significância estatística.
RESULTADOS: Houve maior aderência do revestimento de espuma de silicone ao tecido capsular, sendo este valor estatisticamente significativo (P<0,001). Quanto à reação inflamatória observou-se maior intensidade também neste grupo, porém sem significância estatística. Na contagem de células gigantes e granulomas os valores foram maiores para o grupo espuma de silicone com significância estatística no sub-grupo 60 dias (P<0,028) para número de granulomas; e em todos os sub-grupos (variando de P<0,012 a P<0,036) para o número de células gigantes. A reação capsular à espuma de silicone foi mais espessa, com significância estatística nos sub-grupos sete dias (P<0,028) e 60 dias (P<0,012). No estudo da síntese de colágeno, as diferenças não foram significantes estatisticamente.
CONCLUSÃO: A reação capsular ao revestimento de espuma de silicone apresentou características de ter maior aderência ao tecido peri-implante, ser mais espesso, possuir maior número de granulomas e células gigantes de corpo estranho. Não demonstrou diferença quanto à intensidade da reação inflamatória em relação ao colágeno tipo I e tipo III, quando comparado ao revestimento texturizado.
Descritores: Implante Mamário. Silicones. Materiais Biocompatíveis. Contratura. Ratos.
Introduction
Breast profile is of fundamental importance to women's psychological well being. Breasts are symbols not only of sexuality but also of maternity. Due to the damage caused by hypoplasia or lack of this tissue to women's self esteem, doctors have been searching for the ideal implant that would permit breast reconstitution and would be inert to the organism1.
Concern with the material to be implanted has stimulated plastic surgeons' imagination for more than one century, since Gersuny (1889), mentioned by Pitanguy1, introduced the paraffin injection technique in the mammary parenchyma.
The present beauty standard made millions of women look for the plastic surgeons' office to correct mammary volume and consistency alterations. Due to the failure of the use of autochthonous tissue such as dermal flaps, aloplastic material has been used for this purpose.
Mammary prostheses, because they are foreign elements to the body, develop multi level inflammatory silicone reactions and results in periprosthetic fibrous capsules. This reaction causes implant encapsulation and may cause capsular contraction, requiring surgical intervention to remove the implant and to treat the capsule.
Ko et al.3 remind that fibrous capsule contraction formed around the implants is the most common post-implant complication, with varying 0, 5% to 29% incidence. The clinical consequences of capsular contraction vary from globular firm breasts, discomfort, pain and the distressing extrusion of the implants. There is no medical explanation to the fact that some women develop capsular contracture and others don't and why some women develop capsular contracture on the same side of the surgical wound.
Capsule contraction etiology is uncertain and probably multifactor, and is being the subject of many human and animal studies. Some factors have been postulated in the etiology of capsule contraction such as reaction to a foreign body, hematomas, sub-clinical periprosthetic infection, mechanical irritation, reduced space for implant placement, prosthesis volume, silicone leakage, surgical trauma, thickness and material of the lining4.
In the last three decades, implants have suffered modifications in their structure in an attempt to make their material the least reactive possible, reducing capsular contraction incidence. Among other modifications, smooth implants were substituted by textured membrane linings or coated with polyurethane5.
Many studies have been made to confirm the relationship between capsular contraction and the kind of lining of silicone mammary prosthesis. Most of these studies demonstrated that textured linings presented the lowest index value of contracture.
Polyurethane linings offered the lowest index of contracture incidence due to their micro-porous structure7. An analysis with 1257 patients presented 1% incidence. However, polyurethane is responsible for intense inflammatory reaction, with relevant lining phagocytosis and lining degradation, making its removal difficult when it is necessary8.
Haddad Filho et al.9 confirm that one of the most significant modifications in silicone implants was the texture of their surfaces.
This way, an implant texture was developed, following the characteristic of polyurethane foam, aiming at less capsular contraction, less mechanical irritability which resulted from better tissue adherence, using silicone to minimize local tissue reaction10.
This lining was labeled silicone foam and it is the focus of this study that aims at: 1. Evaluating the biophysical characteristic of lining adherence to local reacting tissue; 2. Quantifying the pre-implant inflammatory reaction; 3. Studying foreign body reaction; 4. Measuring capsule thickness; 5. Studying the relationship between mature and immature collagen.
Methods
This study was conducted at the Medical Research Institute (IPEM) of the Post-Graduate Program in Principles of Surgery of the Evangelical University Hospital of Curitiba/ Parana Evangelical Faculty and at the Parana Institute of Technology (TECPAR).
It followed the Nomina Anatomica Veterinaria and the ethical principles in animal experimentation approved by COBEA, 1991 (Brazilian College of Animal Experimentation). The study was submitted to the Ethics Committee in Research of the Curitiba Evangelical Beneficent Society, approved under no 3508/08.
Thirty two male Wistar rats (Rattus norvegicus albinus, Rodentia mammalian) were studied. The animals came from the animal colony of the Parana Institute of Technology (TECPAR) aged 100 to 120 days, weighing 200 to 300 grams. Each four animals were kept in adequate standard polypropylene boxes at the Animal House. Each box received an identification label with information on each animal. Light -dark cycle was dully observed as well as room temperature (19 and 22ºC) and adequate air humidity. The animals were fed specific animal food with free access to water and food.
The study compared two implant groups: silicone membrane and textured membrane. Each animal received both implants. The 32 animals were sub-divided in four groups of eight animals (I, II, III, IV), according to follow up time and death: 7, 14, 30 and 60 days.
Each animal received two different prostheses lining implants. Both textures were silicone membranes; however, one presented silicone foam surface and the other textured silicone.
Pieces measuring 6x2 cm were made for future extraction in 0, 5 cm monoblock to be studied microscopically and the remaining 5, 5 cm for biophysical study.
The animals were weighed and anesthetized with ketamin (50mg/kg) and xylazin (10mg/kg), on their hind legs with intramuscular injection. They were kept warm and under spontaneous ventilation until they recovered from anesthesia.
The animals' back was shaved after the area had been washed with 2/% chlorhexidine solution liquid soap and distilled water. The animals were fixed to a surgical board in ventral position with their legs fastened with rubber bands. Afterwards, two spots were marked in the shaved area with skin pens for the incision, skin removal (Figure 1A) and asepsis of the skin with 0, 5% chlorhexidine aqueous solution.
Two transversal 2 cm long incisions were made with a blade 15 scalpel on the back of the animal, 3cm above the hind legs. A distance of 1 cm between the pockets was kept. Two 2x8 subcutaneous pockets were made on the dotted lines (Figure 1B).
The implants were placed on the left side of the dorsal median line (textured membrane) and on the right side (Silicon foam). The membranes were placed at 2cm of the rim of the incision. The wound was sutured with 5-0 monofil nylon thread (Figure 2).
The animals were placed on a warm environment at 250C until they completely recovered from anesthesia and, afterwards, they were transferred to their respective boxes.
There was a daily follow up, studying the macroscopic aspects of cicatrization and the presence of complications. The wound was not dressed and the stitches were not removed.
At the 7th day for group I, 14th day for group II 30th day for group III and 60th day for group IV, the animals were euthanized with lethal inhalation of sulfuric acid.
A monoblock resection was performed considering the implant, the capsular reaction and the skin (Figure 3A). Each surgical piece was sectioned with a scalpel and 0, 5 cm of this material was sent for microscopic study (Figure 3B). The portion to be studied was that the most distant from the skin incision placed on filter paper in a flask containing 10% formaldehyde and dully identified.
The rest of the surgical piece measuring 2 x 5,5 cm was placed on filter paper inside identified flasks containing 0,9 physiological solution and sent to biophysical study.
The block containing skin, capsular reaction and the implant was sent to TECPAR laboratory for the study of adherence between the implants and capsular reaction.
The dissection of the rims of the piece was standardized with 0, 5 cm on each extremity, separating the implant from the capsular reaction. A tensiometer was located on one side of the implant and on the other side the capsule, the sub-cutaneous tissue and the skin and were submitted to a pulling force to induce separation among them (Figure 4). This way, a force unit in kilogram force (kgf) was obtained, sufficient to separate the capsule from the silicone implant. This unit represents the adherence produced by the tissue capsular reaction to the kinds of prosthetic surfaces: silicone, textured and foam.
The samples were fixed in 10% formaldehyde. From each surgical piece, random fragments of the capsule reaction to the silicone implant were collected.
These fragments were processed for the conventional histological technique, following the stages: Gradual dehydration, diaphanization, infiltration, paraffin blocking. From each paraffin block, two four micrometer thick glass slides with histological cuts were obtained and stained with hematoxilin-eosine (HE) and pricrosirius (sirius-red). Next, the slides' cover slips were sealed with synthetic resin and numerically identified.
HE staining offered the histological standard of capsular reaction, the kind and intensity of the inflammatory reaction, and of the foreign body reaction as well as the capsule thickness. Acute inflammatory reaction was characterized by the presence of neutrophyls, vascular congestion and diapedesis. As to the chronic inflammatory reaction, the presence of mononuclear cells (lymphocytes, plasmocytes, and monocytes) was evaluated. Inflammatory reaction was observed on the optic microscope 400x magnified in three random fields, and classified in four groups: absent (0), light (1), moderate (2) and intense (3), according to the percentage of cells in each microscopic field. For the statistical study, the sample was divided according to the inflammatory reaction: absent or discreet, moderate or intense. A study of three fields 400X magnified was used to evaluate the reaction to a foreign body using the counting of the giant cells and granulomes, and to measure the thickness of the capsule. All sections were examined by the same pathologist (Table 1) who did not know the group or the period the glass slide was made.
The proportion between type I (mature) collagen and type III (immature) collagen was studied with sirius-red staining. This technique offers information as to the density and the specific kind of collagen fibers formed in the capsule. Optic microscopy with polarized source of light, 200X magnified was used for the microscopic reading of this staining. Mature collagen fibers or type I collagen were identified, because they are thicker and present intense reddish birefringence. The immature or type III collagen fibers were thinner and dispersed with weak greenish birefringence. Microscopic images were taken with a Sony® CCD Iris camera and transmitted to a Sony® Trinitron colored monitor. The images were digitalized and analyzed with Image Pro Plus application in an Intel Pentium III® computer.
System calibration was based on the optic density of the resolution points (pixels) that form the picture. For the standardization of the reading system, all slides were evaluated at the same regulation conditions, following the instructions of the application. Three magnified fields were chosen for each slide located on the median portion, lateral right and left of the histological slides. The quantity of reddish and greenish fibers which were present on the histological cuts permitted the percent calculation of the area of the examined field occupied by these fibers. This percentage was considered proportional to the quantity of each type of fiber present in the histological cuts.
To compare evaluation timing, one factor variance analysis was used and the LSD test (least significance test) for multiple comparisons or the non-parametric Kruskal-Wallis test. For the normality condition evaluation of the variables the Shapiro-Wilks test was used. P<0,05 values indicated statistical significance.
Results
In the membrane adherence study it was observed that, for the textured surface, the results indicated the there was no significant difference between evaluation timing at 7, 14, 21, 31 and 60 days (Table 2).
For silicone foam, the results indicate that there was a significant difference in the evaluation timing 7, 14, 21, 30 and 60 days concerning adherence which increased following the post-operatory period (Table 3).
In order to evaluate these differences, timing was compared in groups of two (Table 4).
The results of the statistic tests indicated that, concerning the silicone foam surface, there was significant difference between the 7th and the 14th days, 14th and the 60th days and at 28th days and 60th day of the evaluation. There was no significant difference between the 14th and 28th days. Examining the average values, one can notice that they also increased along the evaluation days as, for example, in the case of the textured membrane (Figure 5).
There was a clear difference between the adherence values when the two membranes were compared, being the averages higher in the silicone foam implants (Table 5).
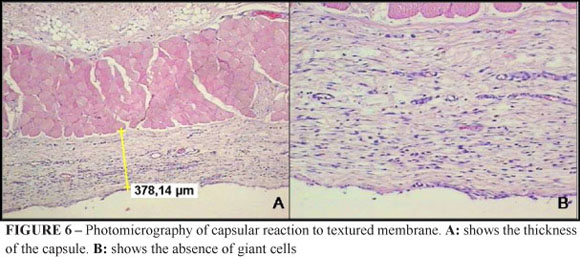
The histological study of the interface with the textured coating showed neo-vascularization with some ectasic blood vessels and a discreet or absent number of multinuclear giant cells (Figure 6).
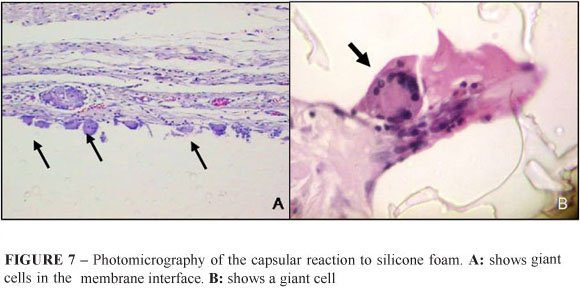
Acute inflammatory reaction was discreet or absent in all studied animals. The intensity of the chronic inflammatory reaction is registered in Figure 7 and Table 6, showing the predominance of absent and discreet acute inflammatory reaction in both groups.
Many nuclear cells were present in the interface of the tissue with the silicone foam coating, indicating foreign body reaction (Figure 7).
The quantitative analysis showed a greater number of statistically significant giant cells in the foam group, in all studied sub-groups (Table 8).
The measures of silicone foam coating were superior as regards the thickness of the capsules (Table 9).
There was a decrease in the percentage of type III immature collagen in both groups. These values are statistically significant when comparing sub-groups. There was no statistic significance when average values were compared between the groups (Figure 8).
In the initial phase of the capsular reaction the presence of type III collagen (greenish) and type I (reddish) were almost the same. Proportionally, with the evolution of the post-operatory period, type I collagen increased, and was present in both groups (Figure 9). The highest proportion of type I collagen was of no significance when both groups were compared; however, it was significant in the sub-group comparison.
Discussion
Many different textures have been developed aiming at the ideal breast implant and many studies try to define the advantages of each of them. At present, the utilized coatings are made of silicone elastomers with smooth surface, many kinds and forms of textured surfaces and surfaces covered with polyurethane foam.
Polyurethane causes intense foreign body reaction, stronger than that caused by silicone coatings1. Many studies have certified that polyurethane coated prostheses present less incidence of capsular contracture. This is due to capsule formation inside the spongy structure of polyurethane which results in non-continuous tissue reaction, hindering contraction11. The encapsulation of polyurethane fragments helps the formation of a discontinuous capsule. However, the use of polyurethane in humans was questioned after it proved carcinogenic in rats due to its degradation product, 2, 4- toluenodiamine12. This evidence was not significant enough to prevent its use in humans. Polyurethane coverings decompose with the passing of time, exposing a smooth coating which hinders capsule contraction.
Silicone has been amply used in different kinds of medical prostheses because it has been considered an inert and less reactive material, although one cannot believe that it is pure, inactive and eternal. There are collateral effects associated with implants because they stimulate the defense mechanism to eliminate it as a foreign body. Among the materials used in implants, silicone is one of the most inactive materials, due partly to its hydrophobic characteristic that impedes chemical and enzymatic agents to affect the material2.
Many studies attested to the superiority of textured membranes over the smooth ones in capsular reduction13,14. This textured quality is directly related to the degree of discontinuity of the capsule and the consequent reduction of its contracture.
Taking these evidences into consideration, in this present study, we chose to compare two coatings made of the same material, silicone, because it presents less foreign body reaction and two different kinds of rugosities: textured and microporous membrane or foam, in order to obtain a greater discontinuity of the peri-implant reaction.
Brohim14 used fragments of the surface of prostheses in order to obtain microscopic data on peri-implant reaction to different coating textures. Following the same procedure, the authors of this study used coating fragments of silicone prostheses. The necessity to use a 5, 5cm x 2cm membrane, after sample collection for histological study was due to the dimension of the tensiometer available for the study. Kafejian et al.15 pointed out the necessity to keep a 2cm distance from the incision for the placement of the materials. This is to minimize the action of operative manipulation on the inflammatory reaction. In this study it was agreed that 1cm was enough.
Some authors mention the mechanic friction between the implant and the peri-implant tissue reaction as the cause of capsular contraction. This study suggests the hypothesis that there might be less contraction in the textured prostheses due to the decrease of adhesive capsular characteristic, thus decreasing the mechanical friction previously mentioned9,14.
The necessary force to loosen the membrane´s peri-implant tissue indirectly demonstrated the invasion of this tissue inside the coating's texture. This force was directly proportional to the porosity of the membrane.
Contrary to Lyras5 study that detected intense acute inflammatory reaction in the analysis of the reaction to textured coatings, in this study this reaction was absent or discreet in all groups. As to chronic inflammatory reaction, the absent and discreet types predominated in both groups, certifying the findings already described16,17 that detected discreet reaction to textured implants, with intense reaction to silicone foam.
Escudero et al.2 affirmed that there is a more intense chronic inflammatory reaction with macrophages and giant cells in textured prostheses due to tissue growth inside the coating.
Corroborating this affirmation, there was a larger number of giant cells in all sub-groups of silicone foam which presented greater tissue growth inside the coating. A greater number of granulomes in the foam group was also evident, with significant difference at 60 days. This may be due to tissue growth inside a microporous structure with greater contact of the peri-implant surface with the silicone coating.
The greater contact between adjacent tissues and the microporous surface of the foam coating made evident, in this study, by tissue growth inside the membrane, favors the stimulus of monocytes in multinuclear giant cell differentiation in face of foreign and non digestible material.
In a comparative study between silicone foam coatings and textured coatings, Batra et al.17 found a thicker capsule in the foam group, similar to the one found in this study. However, the methodology differed from the present study in that they counted the cellular layers.
As to the thickness of the capsules, silicone coatings were superior. This superiority cannot be related to a greater probability of contracture occurrence, because there is no consensus in the literature and the studies on the subject use different methodologies and present controversial results.
In this study it was observed that, along the post-operatory period, collagen type I increased in both groups. As to immature collagen type III, there was a decrease in its percentage in both groups. This information was similar to the results already found in rabbits, in other words, a progressive decrease in immature collagen. Collagen type I presented a progressive increase in all sub-groups. The comparison of both coatings showed no evidence of significant difference in the proportion of Type I and III collagen. An expected substitution of type III collagen for collagen type I in the process of tissue remodeling occurred, with no difference between both kinds of coatings.
As to the collagen fibers disposition, a specific study is necessary determine the parallel or discontinuous structure, once the authors2 related this characteristic to the capsule contractive capacity.
Conclusions
1. There was greater adherence between capsular reaction to silicone foam coating; 2. There was no difference between acute inflammatory reactions and chronic reactions between the membranes; 3. Silicone foam membrane presents greater reaction to foreign bodies than the textured one; 4. The thickness of the capsular reaction was significantly more intense in the silicone foam coating; 5. There is a progressive increase of type I collagen in both coatings, with no difference whatsoever.
Received: March 17, 2009
Review: May 12, 2009
Accepted: June 16, 2009
Conflict of interest: none
Financial source: none
How to cite this article
Balderrama CMSR, Ribas-Filho JM, Malafaia O, Czeczko NG, Dietz UA, Sakamoto DG, Bittencourt LP. Healing reaction to mammary prostheses covered by textured silicone and silicone foam in rats. Acta Cir Bras. [serial on the Internet] 2009 Sept-Oct;24(5). Available from URL: http://www.scielo.br/acb
* Color figures available from www.scielo.br/acb
- 1. Pitanguy I, Salgado F, Radwanski H, Stersa R. Estágio atual dos implantes mamários. Rev Bras Cir. 1992;82(1):41-9.
- 2. Escudero FJ, Guarch R, Lozano JA. Reacción tisular a las prótesis mamarias. Contractura capsular periprotésica. An Sist Sanit Navar. 2005;28(2):41-53.
- 3. Ko CY, Ahn CY, Ko J, Chopra W, Shaw WW. Capsular synovial metaplasia as a common response to both textured and smooth implants. Plast Reconstr Surg. 1996;97(7):1427-35.
- 4. Asplund O, Gylbert L, Jurell G, Ward C. Textured or smooth implants for submuscular breast augmentation: a controlled study. Plast Reconstr Surg. 1996;97(6):1200-6.
- 5. Lyras I. Tissue reaction to rough and smooth silicone implants (A comparative and analytical experimental study in rats). Rev Soc Bras Cir Plast. 1993;8(1):131-41.
- 6. Barnsley GP, Sigurdson LJ, Barnsley SE. Textured surface breast implants in the prevention of capsular contracture among breast augmentation patients: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2006;117(7):2182-90.
- 7. Vázquez G, Pellón A. Polyurethane-coated silicone gel breast implants used for 18 years. Aesthetic Plast Surg. 2007;31(4):330-6.
- 8. Dini GM, Ferreira LM. Early complication with the use of polyurethane-covered breast implants. Plast Reconstr Surg. 2006;117(6):2098-100.
- 9. Haddad Filho D, Zveibel DK, Alonso N, Gemperli R. Comparison between textured silicone implants and those bonded with expanded polytetrafluoroethylene in rats. Acta Cir Bras. 2007;22(3):187-94.
- 10. Wagenführ Jr J. Análise histológica comparativa das cápsulas dos implantes de espumas de silicone em ratos. Rev Soc Bras Cir Plast. 2007;22(1):19-23.
- 11. Brand KG. Polyurethane-coated silicone implants and the question of capsular contracture. Plast Reconstr Surg. 1984;73(3):498.
- 12. Sepai O, Henschler D, Czech S, Eckert P, Sabbioni G. Exposure to toluenediamines from polyurethane-covered breast implants. Toxicol Lett. 1995;77(1-3):371-8.
- 13. Zimman OA, Toblli J, Stella I, Ferder M, Ferder L, Inserra F. The effects of angiotensin-converting-enzyme inhibitors on the fibrous envelope around mammary implants. Plast Reconstr Surg. 2007;120(7):2025-33.
- 14. Brohim RM, Foresman PA, Hildebrandt PK, Rodeheaver GT. Early tissue reaction to textured breast implant surfaces. Ann Plast Surg. 1992;28(4):354-62.
- 15. Kafejian AP, Haddad-Filho D, Guidugli-Neto J, Goldenberg S. Estudo comparativo das reaçòes teciduais à implantação de silicone e politetrafluoroetileno expandido no dorso de ratos. Acta Cir Bras.1997;12(3):182-8.
- 16. Lesesne CB. Textured surface silicone breast implants: histology in the human. Aesthetic Plast Surg. 1997;21(2):93-6.
- 17. Batra M, Bernard S, Picha G. Histologic comparison of breast implant shells with smooth, foam, and pillar microstructuring in a rat model from 1 day to 6 months. Plast Reconstr Surg. 1995;95(2):354-63.
Publication Dates
-
Publication in this collection
15 Oct 2009 -
Date of issue
Oct 2009
History
-
Reviewed
12 May 2009 -
Received
17 Mar 2009 -
Accepted
16 June 2009