Abstracts
PURPOSE: The aim of the present study was to assess the advantages and disadvantages of liver vascular partial exclusion (LVPE) (liver dysfunction due to ischemia) during liver resection in patients submitted to partial hepatectomy. METHODS: A total of 114 patients were submitted to partial hepatectomy (minor versus major resections) with LPVE being used in 57 of them but not in the remaining 57. Patient age ranged from 35 to 73 years and 57 % were women. Mitochondrial function was assessed 30 minutes after liver resection in the remnant liver and serum aminotransferases were determined before surgery and for seven days postoperatively. LPVE time ranged from 30 to 60 minutes. Data were analyzed statistically by the Student T test (5 % level of significance). RESULTS: Mitochondrial function was similar in the minor and major liver resections. The maximum postoperative aminotransferase peak was similar in the groups with and without LPVE. CONCLUSION: LPVE did not induce mitochondrial changes in hepatic tissue in either type of surgery, and aminotransferase levels were similar for patients with and without LPVE. Thus, the results show that LPVE is a safe procedure that does not induce the significant changes typical of ischemia and reperfusion in the liver remnant.
Hepatectomy; Mitochondria; Ischemia
OBJETIVO: Avaliar as vantagens e desvantagens da oclusão vascular parcial do fígado durante ressecções hepáticas parciais. MÉTODOS: Cento e quatorze pacientes foram submetidos a hepatectomia parcial(ressecção maior versus ressecção menor) com liver partial vascular exclusion (LPVE) sendo utilizada em 57 deles. A idade dos pacientes variou entre 35 e 73 anos e 57% deles eram mulheres. A função mitocondrial foi avaliada por método polarografico avaliada 30 minutos após a ressecção hepática no fígado remanescente, e o perfil das aminotransferase foi determinado antes da cirurgia e durante sete dias de pós-operatório. A EVPH variou de 30 a 60 minutos. Dados foram analisados estatisticamente pelo teste T Student (nível de significância de 5%). RESULTADOS: Nas ressecções hepáticas maiores e menores, a função mitocondrial do fígado remanescente foi semelhante dos dois grupos. O pico máximo de aminotransferases ocorreu as 24 horas de pós-operatório e o perfil enzimático de ALT e AST foi semelhante nos grupos estudados ( minor vs major hepatectomy.) CONCLUSÃO: A EVPH não induziu alterações mitocondriais no tecido hepático em qualquer tipo de cirurgia, e os níveis de aminotransferases foram similares para pacientes hepatectomizados com e sem LPVE.Assim a LPVE foi um procedimento seguro que não induziu alterações significativas típicos de isquemia e reperfusão no fígado remanescente.
Hepatectomia; Mitocondria; Isquemia
22 - ORIGINAL ARTICLE CLINICAL RESEARCH
Biochemical liver function after partial hepatic resection with or without partial hepatic vascular exclusion1 1 Research performed at Special Liver Transplantation Unit, Departments of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo (FMRP-USP), Brazil.
Função bioquímica do fígado após ressecção hepática parcial com ou sem exclusão vascular hepática parcial
Orlando Castro e SilvaI; Enio David MenteII; Ajith Kumar SankarankuttyIII; Maria Eliza Jordani SouzaIV; Maria Cecília Jordani GomesIV; Maria Aparecida Neves Cardoso PicinatoV; Clarice Fleury FinaV; Jorge Resende Lopes JuniorVI
IChairman and head of Division of Digestive Surgery of FMRP-USP, Ribeirao Preto, Sao Paulo, Brazil. Designed the protocol, involved with technical procedures, responsible for manuscript preparation, manuscript writing, responsible for intellectual and scientific content of the study and English language
IIPhD, Assistant Professor, Division of Digestive Surgery of Department of Surgery and Anatomy of FMRP-USP, Ribeirao Preto-SP, Brazil. Helped with technical procedures, collection and processing of study and critical revision
IIIPhD, Assistant Professor, Division of Digestive Surgery of Department of Surgery and Anatomy of FMRP-USP, Ribeirao Preto-SP, Brazil. Helped with technical procedures, collection and processing of study and critical revision
IVMaster, Biochemistry, Division of Digestive Surgery, Department of Surgery and Anatomy of FMRP-USP, Ribeirao Preto-SP, Brazil. Responsible for acquisition and interpretation of data, responsible for manuscript preparation and manuscript writing
VBiochemistry, Division of Digestive Surgery, Department of Surgery and Anatomy of Faculty of FMRP-USP, Ribeirao Preto-SP, Brazil. Acquisition and interpretation of data
VIMD, Resident, Division of Digestive Surgery, Department of Surgery and Anatomy of FMRP-USP, Ribeirao Preto-SP, Brazil. Helped with technical procedures, collection and processing of study
Correspondence 1 Research performed at Special Liver Transplantation Unit, Departments of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo (FMRP-USP), Brazil.
ABSTRACT
PURPOSE: The aim of the present study was to assess the advantages and disadvantages of liver vascular partial exclusion (LVPE) (liver dysfunction due to ischemia) during liver resection in patients submitted to partial hepatectomy.
METHODS: A total of 114 patients were submitted to partial hepatectomy (minor versus major resections) with LPVE being used in 57 of them but not in the remaining 57. Patient age ranged from 35 to 73 years and 57 % were women. Mitochondrial function was assessed 30 minutes after liver resection in the remnant liver and serum aminotransferases were determined before surgery and for seven days postoperatively. LPVE time ranged from 30 to 60 minutes. Data were analyzed statistically by the Student T test (5 % level of significance).
RESULTS: Mitochondrial function was similar in the minor and major liver resections. The maximum postoperative aminotransferase peak was similar in the groups with and without LPVE.
CONCLUSION: LPVE did not induce mitochondrial changes in hepatic tissue in either type of surgery, and aminotransferase levels were similar for patients with and without LPVE. Thus, the results show that LPVE is a safe procedure that does not induce the significant changes typical of ischemia and reperfusion in the liver remnant.
Key words: Hepatectomy. Mitochondria. Ischemia.
RESUMO
OBJETIVO: Avaliar as vantagens e desvantagens da oclusão vascular parcial do fígado durante ressecções hepáticas parciais.
MÉTODOS: Cento e quatorze pacientes foram submetidos a hepatectomia parcial(ressecção maior versus ressecção menor) com liver partial vascular exclusion (LPVE) sendo utilizada em 57 deles. A idade dos pacientes variou entre 35 e 73 anos e 57% deles eram mulheres. A função mitocondrial foi avaliada por método polarografico avaliada 30 minutos após a ressecção hepática no fígado remanescente, e o perfil das aminotransferase foi determinado antes da cirurgia e durante sete dias de pós-operatório. A EVPH variou de 30 a 60 minutos. Dados foram analisados estatisticamente pelo teste T Student (nível de significância de 5%).
RESULTADOS: Nas ressecções hepáticas maiores e menores, a função mitocondrial do fígado remanescente foi semelhante dos dois grupos. O pico máximo de aminotransferases ocorreu as 24 horas de pós-operatório e o perfil enzimático de ALT e AST foi semelhante nos grupos estudados ( minor vs major hepatectomy.)
CONCLUSÃO: A EVPH não induziu alterações mitocondriais no tecido hepático em qualquer tipo de cirurgia, e os níveis de aminotransferases foram similares para pacientes hepatectomizados com e sem LPVE.Assim a LPVE foi um procedimento seguro que não induziu alterações significativas típicos de isquemia e reperfusão no fígado remanescente.
Descritores: Hepatectomia. Mitocondria. Isquemia.
Introduction
Partial liver resection for the treatment of malignant or benign liver tumors, may be complicated by intraoperative bleeding1,2,3,4. In particular, resection of lesions in close proximity to or infiltrating major vascular structures or an extended hepatectomy can be unpredictably complicated by life-threatening hemorrhage, even leading to rapid patient death on the operating table2,3,4,5,6. Moreover, bleeding, together with the subsequent blood transfusions, increases postoperative morbidity and mortality. Today, with the improved technical training of surgical teams and with the development of new generations of ultrasound, harmonic and water-jet scalpels and the argon cautery , the level of hemorrhage has been reduced during hepatectomy, although bleeding continues to be a factor of intra- and postoperative complications in liver resection7,8,9.
Strategies to reduce intraoperative bleeding during hepatectomy include temporary occlusion of blood inflow with or without outflow control, of the whole liver or part of it during parenchymal transection, a method called hepatic vascular occlusion or control5,6,10.
The concept of hepatic vascular control is based on the proven tolerance of liver to warm ischemia and on strong evidence that liver tolerates ischemia better than bleeding5,6,10. It should also be taken into account that vascular control eliminates bleeding only during the phase of parenchymal transection and is not beneficial during the phase of liver mobilization, when bleeding may also occur. However, in this phase of liver dissection the complications have been minimized with the increasing experience gained by the surgeons, especially in liver transplantation. In addition, reasonable or minimal blood loss has been achieved during major hepatectomy performed without embarking on vascular control at all7,11. The aim of the present study was to assess the advantages and disadvantages of liver partial vascular exclusion (LPVE) (liver dysfunction due to ischemia) during liver resection in patients submitted to partial hepatectomy.
Methods
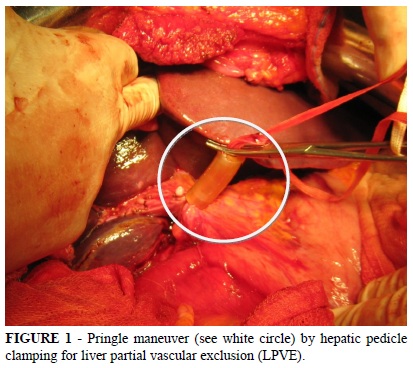
A total of 114 patients were submitted to partial hepatectomy (minor versus major resections) during the period from 1998 to 2008, with LPVE being used in 57 of them but not in the remaining 57. Patient age ranged from 35 to 73 years and 57 % were women. The surgical and laboratory team was the same throughout the study. Demographic, clinical, and biochemical data were collected using a standard form. The timing and nature of any chemotherapy were also recorded. All biochemical data obtained from laboratory assays for up to seven days postoperatively were retrieved. Liver resections were performed with or without LVPE - Pringle maneuver- as shown in Figure 11. (LPVE time changed from 30 to 60 minutes).
The operations were performed by a single team and in approximately 90 % of the cases were performed by the same surgeon (O.C.S.). Ischemic preconditioning was not used. In all cases the abdominal cavity was closed with drainage.
Preparation of mitochondria and oxygen consumption assays 12,13
Liver mitochondria were isolated by differential centrifugation. Mitochondrial oxygen consumption was analyzed polarographically with a home-made oxygraph constructed at IFSC-USP equipped with a Clarck oxygen electrode, and the respiratory parameters were determined according to an established procedure. Succinate (5 mM) was used as oxidizable substrate in 1.4 ml of medium with 125 mM sucrose, 65 mM KCl, 1 mM MgCl2, 2 mM KH2PO4, 0.1 mM EGTA, and 10 mM Hepes-KOH, pH 7.4, and 2 mg of mitochondrial protein were used. State 3 respirations were induced with 400 nmol MgADP, and state 4 respirations (basal mitochondrial respiration) were determined after phosphorylation of additional ADP.
The ratio between state 3 and state 4 (respiratory control ratio (RCR)), which represents coupling between electron transport and oxidative phosphorylation, was determined. Mitochondrial protein content was determined by the biuret method.
Mitochondrial membrane potential (MMP) 14
MMP was monitored spectrofluorimetrically using 5 M safranine-O as indicator and an SLM-Aminco, Bowman, series 2, luminescence spectrophotometer operating at 495/586 nm excitation/emission wavelength par. Assays were performed in an incubation medium containing 200 mM sucrose, 1 mM MgCl2, 2.5 mM NaH2PO4, and 10 mM Hepes-KOH, pH 7.4. Mitochondria were energized with 5 mM sodium succinate. The membrane potential variation was expressed in m, as usual.
Serum aminotransferases 15
Blood samples (4 ml) were placed in a container without previous anticoagulant treatment. Serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) activities were determined by standard procedures using a commercial spectrophotometer (Model E2250-CELM).
Statistical analysis
Data were analyzed statistically by the Student T test (5 % level of significance).
Results
The serum aminotransferase profile was similar (p>0.05) in all groups studied, with or without LPVE (Figures 2 and 3). The maximum peaks of both enzymes occurred 24 hours after surgery and were similar in patients subjected to minor and major hepatectomies with and without LPVE (p>0.05) (Figures 2 and 3).
The respiratory control ratio (RCR) and mitochondrial membrane potential (MMP) of the remnant liver of patients subjected to minor and major partial hepatectomy were similar in all groups studies as show the Figure 4.
Discussion
The better knowledge of the topohraphic and systemic anatomy of the liver, together with great scientific and technological advances, has given the surgeon greater security in performing increasingly larger liver resections. This greater detachment has facilitated the technical domination of liver transplantation, and vice versa1,5,11. Several measures have been adopted over the years in order to minimize intraoperative bleeding and the hepatic insufficiency usually due to small liver remnants or to the hepatocellular suffering of livers previously involved by changes that worsen during partial liver resection5,7,9,10.
Regarding intraoperative bleeding, hepatic pedicle clamping for LPVE is the oldest method of hepatic vascular control in order to avoid or minimize bleeding originating from the liver parenchyma, especially during liver resection. LPVE is performed by encircling the hepatoduodenal ligament with tape and then applying a tourniquet or a vascular clamp until the pulse in the hepatic artery disappears distally1,5,6,11. Prior to placing the occluding clamp or tourniquet, careful dissection of the hepatic pedicle is needed to leave it free of adhesions, because if these adhesions are left intact there is a serious risk of injuring the inferior vena cava or the duodenum when placing the clamp. After pedicle clamping, a sympathetic reflex produced by clamping causes a 40% increase in systemic vascular resistance and a 40% increase in mean arterial pressure1,5,6,11.
LPVE is generally well tolerated because caval flow is not interrupted and specific anesthetic management is not required. The anesthesiologist should also be alerted to the possibility of intraoperative air embolism, as with any kind of inflow vascular occlusion where the major hepatic veins are left open. The consequences of air embolism can be minimized by placing the patient in a 15 degree Trendelenburg position. A number of clinical studies have established 60 minutes as the safe duration of partial exclusion under normothermic conditions for normal livers1,5,6,11. In the present study we used vascular exclusion for 25 up to 90 minutes and none of the patients had liver or systemic complications. Longer LPVE periods have been reported in normal livers with favorable clinical outcomes.
The effectiveness of LPVE in reducing bleeding during major hepatectomies has been shown in historical controls and also in several clinical studies. LPVE cannot prevent bleeding from hepatic veins and should be used with caution or even avoided for lesions close to or involving the cavohepatic junction1,5. Hemorrhage from hepatic veins can be minimized by operating under low flow and by complete devascularization of the resected segments16,17. On the other hand, retrograde flow from hepatic veins during the Pringle maneuver seems to contribute to attenuation of hepatic I/R injury, as was demonstrated in the literature. In the present study the levels of aminotransferases were the same in the groups studied (with and without LPVE). Similarly, the energy capacity of the liver remnant was similar in all groups studied. The liver mitochondrial function was similar in the livers with and without LPVE in the minor and major hepatectomies1,5,11.
Conclusion
Because of its effectiveness and simplicity, LPVE remains the most popular method of vascular control. In our patients, periods of LPVE of up to 90 minutes in normal livers in minor and major hepatectomies had favorable clinical outcomes.
Correspondence:
Orlando de Castro e Silva
Departamento de Cirurgia e Anatomia - HCFMRP
Av. Bandeirantes, 3900/9° andar
14048-900 Ribeirão Preto - SP Brasil
Tel.: (55 16)3602-2242
Conflict of interest: none
Financial sources: CNPq, FAPESP and SUS
Present at the XII National Congress on Experimental Surgery of the Brazilian Society for the Development of Research in Surgery-SOBRADPEC, 2011 October 26-29, Ribeirao Preto-SP, Brazil.
- 1. Bismuth H. Major hepatic resection under total vascular exclusion. Ann Surg. 1989;210:13-19
- 2. Curley SA, Izzo F, Ellis LM, Nicolas Vauthey J, Vallone P. Radiofrequency abalation of hepatocelular cancer in 110 patients with cirrhosis. Ann Surg. 2000;232:381- 91
- 3. Fasculo F, Giori A, Fissi S, Bozzetti F, Doci R, Gennari L. Cavitron Ultrasonic Surgical Aspirator (CUSA) in liver resection. Int Surg. 1993;77:64-6
- 4. Hansen PD, Isla AM, Habid NA. Liver resection using total vascular exclusion, scapel divion of the parenchyma and a simple compression technique for haemostasis and biliary control. J Gastrointest Surg. 1993;3:537-42
- 5. Elijah Dixon, Charles M. Vollmer, Jr.,Oliver F. Bathe, Francis Sutherland. Vascular occlusion to decrease blood loss during hepatic resection. Am J Surg. 2005;190:75-86
- 6. W. Zhou, A. Li, Z. Pan, S. Fu, Y. Yang, L. Tang, Z. Hou, M. Wu. Selective hepatic vascular exclusion and Pringle maneuver: A comparative study in liver resection. Journal of cancer Surgery. EJSO 2008;34:49-54
- 7. Wrightson WR, Edwards MJ, McMasters KM. The role of the ultrasonically activated shears and vascular cutting stapler in hepatic resection. Am Surg. 2000;66:1037- 40
- 8. Weber JC, Navarra G, Jiao LR, Nicholls JP, Jensen SL, Habid NA. New technique for liver resection using heat coagulative necrosis. Ann Surg. 2002;236:560-3
- 9. Wolf RF, Xie H, Petty J, Teach JS, Prahl SA. Argon ion beam hemostasis with albumin after resection. Am J Surg. 2002;183:584-7
- 10. Zacharoulis D, Asopa V, Navarra G, Nicholls JP, Jensen SL, Habib NA. Hepatectomy using intraoperative ultrasound-guided radiofrequency ablation. Int Surg. 2003;88:80-2
- 11. Paul Needhama, Dowmitra Dasguptaa, John Daviesa, Mark D. Stringerb. Postoperative biochemical liver function after major hepatic resection in children. J Pediatr Surg. 2008;43:1610-18
- 12. Pedersen PL, Greenawalt JW, Soper JW, Bustamente E. Preparation and characterization of mitochondria and submitochondrial particles of rat liver and liver-derived tissues. Methods Cell Biol. 1978;20:411-81.
- 13. Souza MEJ, Polizello ACM, Uyemura SA, Castro-E-Silva O Jr, Curti C. Effect of fluoxetine on rat liver mitochondria. Biochem Pharmacol. 1994;48:535-41.
- 14. Jordani MC, Santos AC, Prado IMR, Uyemura SA, Curti C. Flufenamic acid as an inducer of mitochondrial permeability transition. Mol Cell Biochem. 2000;210:153-8.
- 15. Henry JR, Chiamori N, Golub OJ, Berkman S. Revised spetrophotometric methods for the determination of glutamic oxalacetic transaminase, glutamic pyrivuc transaminase, and lactic acid dehydrogenase. Am J Clin Pathol. 1960;34:381-90.
- 16. Nakayama H, Massuda H, Shibata M, Amano S, Fukuzawa M. Incidence of bile leakage after three types of hepatic parenchymal transaction. Hepatogastroenterology. 2003;1517-20
- 17. Wang WX, Fan ST. Use of the Endo-GIA vascular stapler for hepatic resection. Asian J Surg. 2003;26:193-6
Publication Dates
-
Publication in this collection
24 Oct 2011 -
Date of issue
2011