Abstracts
PURPOSE: To evaluate the effects of fat embolism in organs such as lung and liver. METHODS: Twenty rabbits underwent autologous intramuscular fat grafting in the right thigh after liposuction. The groups were determined according to the postoperative day that occurred in euthanasia: 60, 90 and 120 day. Then, lung and liver were excised and sent to the histopathology laboratory for analysis in search of late injury secondary to a prior event of fat embolism in the tissues. RESULTS: The results showed a change in the macroscopic sample with discoloration of the liver tissue heterogeneously. There were no changes consistent with embolic effect under the microscope. CONCLUSION: The option of performing a technique of fat grafting with a less traumatic surgical procedure can be considered protective against embolic events, with no impact to late embolic events on the tissues.
Embolism, Fat; Lipectomy; Ischemia; Rabbits
OBJETIVO: Avaliar a repercussão da embolia gordurosa em órgãos como pulmão e fígado. MÉTODOS: Vinte coelhos foram submetidos à enxertia autóloga intramuscular de gordura em coxa direita após lipoaspiração. Os grupos foram determinados conforme os dias pós-operatórios (DPO) em que ocorreu a eutanásia: 60 DPO, 90DPO, 120 DPO. Em seguida, o pulmão e o fígado foram ressecados e encaminhados ao laboratório de histopatologia para análise em busca de lesão tardia secundária a evento de embolia gordurosa prévia nos tecidos. RESULTADOS: Foi evidenciada uma alteração na amostra a analise macroscópica com alteração da coloração do tecido hepático de forma heterogênea. Não houve alterações compatíveis com repercussão de processo embólico à microscopia. CONCLUSÃO: A opção pela realização de uma técnica de lipoenxertia menos traumática e com pequeno tempo cirúrgico pode ser considerada protetora para eventos embólicos, não havendo repercussão embólica a tardiamente.
Embolia Gordurosa; Lipectomia; Isquemia; Coelhos
2 - ORIGINAL ARTICLE
MODELS, BIOLOGICAL
Fat embolism in liposuction and intramuscular grafts in rabbits1 1 Research performed at the Nucleus of Experimental Surgery, Bahiana School of Medicine and Public Health (EBMSP), Salvador-BA, Brazil. Part of a project approved by FAPESB for scholarship researcher staying of the second author.
Embolia gordurosa na lipoaspiração e enxertia intramuscular em coelhos
Victor Araujo FelzemburghI; Rafaela Cavalcante das Neves BarbosaII; Victor Luiz Correia NunesIII; José Humberto Oliveira CamposIV
IMD, Volunteer Faculty, Division of Surgical Technique and Experimental Surgery I, EBMSP, Salvador-BA, Brazil. Main author. Responsible for conception, design, intellectual and scientific content of the study
IIScientific Initiation Student, Division of Surgical Technique and Experimental Surgery I, EBMSP, Foundation for Research Support of the State of Bahia (FAPESB), Salvador-BA, Brazil. Involved with technical procedures and acquisition of data
IIIMD, Associate Professor, Division of Pathology, EBMSP, Salvador-BA, Brazil. Analysis and interpretation of data
IVPhD, Full Professor, Division of Surgical Technique and Experimental Surgery I, EBMSP, Salvador-BA, Brazil. Conception, design and critical revision
Correspondence Correspondence: Victor Araujo Felzemburgh Avenida Juracy Magalhães Junior, 670 41960 060 Salvador - BA Brasil Tel.: (55 71)3346-4570 victor@ccp.med.br
ABSTRACT
PURPOSE: To evaluate the effects of fat embolism in organs such as lung and liver.
METHODS: Twenty rabbits underwent autologous intramuscular fat grafting in the right thigh after liposuction. The groups were determined according to the postoperative day that occurred in euthanasia: 60, 90 and 120 day. Then, lung and liver were excised and sent to the histopathology laboratory for analysis in search of late injury secondary to a prior event of fat embolism in the tissues.
RESULTS: The results showed a change in the macroscopic sample with discoloration of the liver tissue heterogeneously. There were no changes consistent with embolic effect under the microscope.
CONCLUSION: The option of performing a technique of fat grafting with a less traumatic surgical procedure can be considered protective against embolic events, with no impact to late embolic events on the tissues.
Key words: Embolism, Fat. Lipectomy. Ischemia. Rabbits.
RESUMO
OBJETIVO: Avaliar a repercussão da embolia gordurosa em órgãos como pulmão e fígado.
MÉTODOS: Vinte coelhos foram submetidos à enxertia autóloga intramuscular de gordura em coxa direita após lipoaspiração. Os grupos foram determinados conforme os dias pós-operatórios (DPO) em que ocorreu a eutanásia: 60 DPO, 90DPO, 120 DPO. Em seguida, o pulmão e o fígado foram ressecados e encaminhados ao laboratório de histopatologia para análise em busca de lesão tardia secundária a evento de embolia gordurosa prévia nos tecidos.
RESULTADOS: Foi evidenciada uma alteração na amostra a analise macroscópica com alteração da coloração do tecido hepático de forma heterogênea. Não houve alterações compatíveis com repercussão de processo embólico à microscopia.
CONCLUSÃO: A opção pela realização de uma técnica de lipoenxertia menos traumática e com pequeno tempo cirúrgico pode ser considerada protetora para eventos embólicos, não havendo repercussão embólica a tardiamente.
Descritores: Embolia Gordurosa. Lipectomia. Isquemia. Coelhos.
Introduction
Fat embolism (FE) is defined as the mechanical blockage of the vascular lumen by circulating fat globules with diameters exceeding 8 to 10u, usually getting trapped in a capillary network1.
The mechanism of fat embolism appears to be due to neutral fat from the injured area that embolize to the pulmonary circulation2. The fat is hydrolyzed by lipase, new free fatty acids cause a toxic effect to capillary endothelium, which enhance the action of integrins, which increase the adhesiveness of neutrophils to endothelial cells, facilitating the action of proteolytic enzymes from lysosomes of neutrophils on the endothelium1.
The fat emboli, although initially spread through the venous circulation, mostly affecting the lungs, in many cases can pass to the pulmonary circulation or even the inter-atrial septum, and by arterial blood, affect any organ or structure of the organism1. The first symptoms appear between 24-72 hours3.
According to studies, adipose tissue presents itself as an ideal material for corrections that need malleable and moldable tissue4. With the advent of liposuction, fat graft has become widely used and associated with it. During the liposuction extensive trauma can happen with rupture of blood vessels and compression of the fat2.
Although most scientific studies shows the association of embolism with bone fractures, there are cases where the phenomenon was related to cosmetic procedures like liposuction and grafting.
Methods
The study protocol was analyzed and approved by the Ethic Commission on Animal Research of Bahiana School of Medicine and Public Health (EBMSP). The use of laboratory animals followed the ethical code for animal experimentation of the Council for International Organization of Medical Sciences.
It was used 20 rabbits (Oryctologus cuniculus), male, of New Zealand race, between 2 and 3 years age and weighing between 3.0 and 4.0 kg. The animals were kept in a place with an average temperature of 22 ° C, humidity between 45 - 50%, with pelleted food for 15 days before surgery.
The anesthetic protocol adopted consisted with ketamine 40mg/kg and xylazine 9mg/kg IM4. The procedure was performed at the Nucleus of Experimental Surgery of EBMSP.
Operative technique
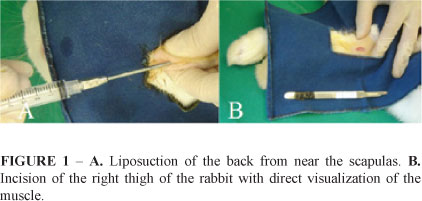
In the prone position, the trichotomy occurred on the back of the rabbit, at the shoulders, and at the lateral portion of the right thigh of the animal. After careful aseptic protocol, the incision was made on the back 2 cm from the apex of the scapula with the introduction of liposuction cannula sized 3 mm, attached to a 10 ml syringe (Figure 1). After insertion of the cannula, the aspiration of the syringe was made with a maximum pressure of 5 ml till 8 ml to aspirate adipose tissue. The time for the procedure was less than ten minutes.
Measure of 1.5 ml of fat was grafted in all rabbits at intramuscular plane in front of the right thigh muscle, over direct vision after incision of 1 cm from the skin (Figure 2). The point of infiltration of the muscle was closed with 5.0 nylon suture to prevent leakage of fat. The skin was also closed with 5.0 nylon. The animals were followed for 60, 90 and 120 days.
All animals were divided into three groups designated A, B and C containing 10, 5 and 05 animals respectively. The determination of the groups was as postoperative day in which euthanasia occurred 60, 90 and 120 days respectively.
The sacrifice consisted of application of prior anesthesia, as mentioned above, associated with a dose of 2 ml of potassium chloride intravascularly. Then the lung and the liver were ressected and sent to histopathology laboratory.
Histological evaluation
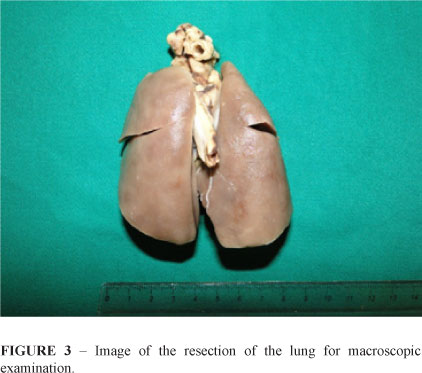
The tissues were fixed in 10% formalin and evaluated in a histopathology laboratory (Figure 3). In the laboratory, sections of the parts with alterations underwent to routine histological processing and microscopic examination. The material was analyzed to see the impact of fat embolism in organs such as lung and liver. The changes in the macroscopic samples were stained with hematoxylin-eosin in search of tissue injury or necrosis. Also assess the degree of impairment of the vascular complex by the search for microscopic fat globules. The picrosirius red staining evaluated the formation of fibrosis, allowing detailed analysis of collagen fibers.
Results
During the evaluation of lung tissue, there were not displayed macroscopic changes such as changes in color, shape or density of the tissues. There were not viewed suffering areas with tissue retraction, fibrosis or necrosis in what could be suspected previous embolic process (Figure 4). The results showed a change in the liver tissue sample analysis which it was described as macroscopic change in color but no change in shape and density (Figure 5). Histopathological examination of the organs showed no changes.
Discussion
The fat embolism syndrome (FES) typically presents between 24-72 hours, rarely in a period less than 12 hours, or greater than two weeks5. The FE is often found along the broken bones but can be associated with many other conditions such as arthroplasty, acute hepatic necrosis, delirium tremens, liposuction, pancreatitis and sickle cell anemia6. Our study there was no record of death during or after surgery.
The diagnosis of FES according to the criteria of Gurd and Wilson takes at least one major criterion and four minor or two major criterions. Among the major criterion have respiratory insufficiency, petechial rash and cerebral involvement7. As for the minor criteria: pyrexia, tachycardia, retinal changes, jaundice, renal changes, anemia, thrombocytopenia, high erythrocyte sedimentation rate and fat macroglobulinemia7. In our study none of these events were recorded however some of these clinical symptoms can be present with a difficult presentation and nonspecific diagnosis. This is also one reason that shows how difficult are the diagnosis in clinical practice.
FE is defined by the occurrence of a mechanical blockage caused by fat globules in the blood vessels, its main causes are fractures of long bones, but is also commonly occur during liposuction because of the trauma caused in fat cells and blood vessels during the procedure thus promoting inoculation of fragments of lipids in blood vessels that results in injury in the affected tissues5.
The event FE may have occurred but without impact or organ injury. Studies show that during the surgeries of knee and hip arthroplasty the occurrence of fat embolic event is 100%, however the presentation of FES is between 0.1% to 12% and 0.6% to 10% respectively. The single fracture of bones as the femur, pelvis and tibia presents fat embolism index greater than 90% however the event of FES varies from 0.05% to 3%1. Fatty embolic events in plastic surgery are a few common1-3.
Clinical complications of liposuction are rare, 5-10% of patients, being the most common complications not have systemic repercussions: seroma, edema, pigmentation, pain, and hematoma or due to the anesthetic procedure. The overall mortality from the FES after liposuction is approximately 10-15%, with higher mortality associated with fulminant FES due to severe right heart failure compared with FES in which the mortality relates largely to underlying respiratory failure (or rarely cerebral edema causing brain death)3.
It may be noted that events proven of fat embolism after liposuction with lethal outcome is infrequent, example of a study conducted at the Institute of Forensic Medicine in Belo Horizonte. During 10 years, between 60 000 autopsies, only seven events of deaths after liposuction procedures were found: one case was confirmed as fat embolism, three pulmonary thromboembolism, one hemorrhage, one perforation of a handle, one unknown cause8.
The absence of signs indicative of fat embolism among rabbits is probably due to the number of samples and the search for late effects of this type of event.
An effective way to highlight the pathology of fat embolism is by the following method: removal of the post-mortem tissue, immersion in paraffin, cut 15µm thick and impregnated with oil-red. The samples thus obtained can be frozen in formaldehyde and analyzed one month after9. The immersion in paraffin and conservation in formaldehyde was also used in our study. However, this study chose to sever the samples 4µm thick and was stained with hematoxylin and eosin. The use of picrosirius red is suitable for evidence of fibrosis.
Because it is a study with animals and the possibility of on-site assessment of the injury, the diagnosis of pulmonary embolism was adopted by the evaluation of the tissues in search of necrosis, fibrosis and fat cells in the microvasculature. Another possibility would be through the use of a marker (interleukin-6) of the material collected after surgical procedure second shown an experimental research10.
In a study with rats undergoing liposuction, embolic event occurred in blood samples of experimental groups intraoperatively at 30 end 60 minutes11. It was observed that increasing the number of fat globules is directly related to the time of liposuction11. In our study, the liposuction procedure was performed on all animals at time of less than 10 minutes with removal of 8 ml of adipose tissue per animal, contrasting with the 60 minutes cited in other studies11,12. The lack of finding may also be attributed to the minimally invasive nature of the technique and choice for reduced surgical time.
The tumescent technique compared with dry technique for liposuction is less associates with FE event, however with the diffusion of the tumescent technique, it reflected in an increase in event of death due to anesthetics toxicity8.
Comparative experimental study in rats, embolic event in the blood and organs occurred for both tumescent technique and the dry technique12. In both groups were found FE with the exception of control group12. The use of tumescent technique involves the use of higher anesthetic infiltration and thus increases the risk of complications related to anesthesia. Our study chose a not tumescent technique. There was no infiltration of any solution before liposuction.
In our study the choice of aspiration with 10 ml syringe and 3 mm cannula was made, the use of this less traumatic technique compared to the use of vacuum suction unit produce less damage of adipocytes during aspiration5,13,14. Experimental studies involving liposuction procedures shows techniques more harmful and long duration11-13. This difference may interfere considerably in the outcome.
The methodology of this study precludes the visualization of lipid deposits in acute fase in organs because the euthanasia was made late, at 60, 90 and 120 days. There wasn't any repercussions of embolic event in the long term of all animals. However, fat embolism finding alone is not sufficient to prove an event of death, provided that there are other phenomena that may be involved and are more frequent causes of complications.
Conclusion
The option of performing a technique of fat grafting with a less traumatic surgical procedure can be considered to be protective against embolic events, with no impact to late embolic events on the tissues.
Received: December 20, 2011
Review: February 21, 2012
Accepted: March 19, 2012
Conflict of interest: none
Financial source: none
- 1. Filomeno LTB, Carelli CR, Silva NCLF, Barros TEPF, Amatuzzi MM. Fat embolism: a review for current orthopaedics pratice. Acta Ortop Bras. 2005;13(4):196-208.
- 2. Folador JC. Síndrome de embolia gordurosa: relato de caso associado à lipoaspiração. J Pneumol. 1999;25(2):114-7.
- 3. Wang HD, Zheng JH, Deng CL, Yang SL. Fat embolism syndromes following liposuction. Aesthetic Plast Surg. 2008;32:731-6.
- 4. Aygit AC, Sarikaya A, Doganay L, Top H, Cakir B, Firat MF. The fate of intramuscularly injected fat autografts: an experimental study in rabbits. Aesthetic Plast Surg. 2004;28(5):334-9.
- 5. Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56:145-54.
- 6. Gupta A, Reilly CS. Fat embolism. Contin Educ Anaesth Crit Care Pain. 2007;7(5):148-51.
- 7. Taviloglu K, Yanar H. Fat embolism syndrome. Surg Today. 2007;37:5-8.
- 8. Avelar LET, Lapertosa L, Versiane TM. Óbitos pós-lipoaspiração. Rev Bras Cir Plást. 2010; 25(Supl):60.
- 9. Sevitt S. Fat embolism in patients with fractured hips. Br Med J. 1972;2:262-4.
- 10. Yoga R, Theis JC, Walton M, Sutherland W. Interleukin-6 as an early marker for fat embolism. J Orthop Surg Res. 2009;4:18.
- 11. El-Ali KM, Gourly T. Assessment of the risk of systemic fat mobilization and fat embolism as consequence of liposuction: ex vivo study. Plast Reconstr Surg. 2006;117(7):2269-76.
- 12. Senen D, Atakul D, Erten G, Erdogan B, Lortlar N. Evaluation of the risk of systemic fat mobilization and fat embolus following liposuction with dry and tumescent technique: an experimental study on rats. Aesthetic Plast Surg. 2009;33:730-7.
- 13. Erdim M, Tezel E, Numanoglu A, Sav A. The effects of the size of liposuction cannula on adipocyte survival and the optimum temperature for fat graft storage: an experimental study. J Plast Reconstr Aesthet Surg. 2008;62(9):1210-4.
- 14. Shiffman MA, Mirrafati S. Fat transfer technique: the effects of harvest and transfer methods on adipocyte viability and review of the literature. Dermatol Surg. 2001;27(9):819-26.
Publication Dates
-
Publication in this collection
01 June 2012 -
Date of issue
May 2012
History
-
Received
20 Dec 2011 -
Accepted
19 Mar 2012 -
Reviewed
21 Feb 2012