Abstract
PURPOSE: To investigate the effects of pneumoperitoneum on colonic anastomosis healing. METHODS: Colonic anastomosis was performed in 120 rats divided into four groups: Group I - pneumoperitoneum before laparotomy, Group II - pneumoperitoneum after laparorrhaphy, Group III - pneumoperitoneum before laparotomy and after laparorrhaphy, Group IV - no pneumoperitoneum (control group). Pneumoperitoneum pressure was 5 mmHg. Animals were killed on the 3rd, 7th and 14th postoperative day. Hhistopathological features, anastomosis breaking strength, collagen histomorphometry and hydroxyproline concentration were assessed. RESULTS: Breaking strength between groups: (day 3, p=0.165; day 7, p=0.219; day 14, p=0.539). Histopathology revealed that group II had, on day 7, less infiltration of mononuclear cells (p=0.006), greater infiltration of polymorphonuclear cells (p=0.001) and greater necrosis (p=0.001); and on day 14, less fibrosis. Histomorphometry revealed a decrease in collagen in groups I and III (p<0.001) on day 7 and an increase in groups I and II on day 14 (p<0.001). Hydroxyproline concentration was similar for groups on days 3 (p=0.152), 7 (p=0.913) or 14 (p=0.981). CONCLUSION: Carbon dioxide does not impair the healing of colonic anastomosis in rats.
Pneumoperitoneum, Artificial; Carbon Dioxide; Anastomosis, Surgical; Wound Healing; Colon; Rats
8 - ORIGINAL ARTICLE
ALIMENTARY TRACT
The effect of carbon dioxide pneumoperitoneum on the healing colonic anastomosis in rats1 1 Research performed at Experimental Surgery Laboratory, School of Medicine, University of Brasilia (UnB), Brazil. Part of Master degree thesis, Postgraduate Program in Medical Sciences. Tutor: João Batista de Sousa.
Leonardo de Castro DurãesI; Igor Eduardo Caetano de FariasII; Pedro Henrique Alves de MoraisII; Paulo Gonçalves de OliveiraIII; Florêncio Figueiredo Cavalcanti NetoIV; Ruy Souza Lino JuniorV; Omar FeresVI; João Batista de SousaVII
IFellow PhD degree, Postgraduate Program in Medical Sciences, School of Medicine,, University of Brasilia (UnB), Brasilia-DF, Brazil. Intellectual and scientific content of the study, designed the protocol, involved with technical procedures, acquisition and interpretation of data, statistical analysis, manuscript writing, critical revision
IIGraduate student, School of Medicine, UnB, Brasilia-DF, Brazil. Technical procedures, acquisition and interpretation of data, statistical analysis
IIIPhD, Associate Professor, Department of Surgery, School of Medicine, UnB, Brasilia-DF, Brazil. Interpretation of data, statistical analysis, critical revision
IVPhD, Full Professor, Department of Pathology, School of Medicine, UnB, Brasilia-DF, Brazil. Macroscopic and histopathological examinations, interpretation of data, critical revision
VPhD, Associate Professor, Department of Pathology, Institute of Tropical Pathology and Public Health, Federal University of Goias (UFG), Goiania-GO, Brazil Collagen histomorphometry examinations, interpretation of data, critical revision
VIPhD, Assistant Professor, Colorectal Surgery, Department of Surgery and Anatomy, Ribeirao Preto School of Medicine, University of Sao Paulo (USP), Ribeirao Preto-SP, Brazil. Biochemical study, interpretation of data, critical revision
VIIPhD, Associate Professor, Department of Surgery, School of Medicine, UnB, Brasilia-DF, Brazil. Intellectual and scientific content of the study, designed the protocol, technical procedures, interpretation of data, manuscript writing, critical revision
Correspondence Correspondence: João Batista de Sousa Universidade de Brasília. Campus Universitário Darcy Ribeiro. Faculdade de Medicina. Laboratório de Cirurgia Experimental 70910-900 Brasília - DF Brasil Tel.: (55 61)9984-2845 sousajb@unb.br
ABSTRACT
PURPOSE: To investigate the effects of pneumoperitoneum on colonic anastomosis healing.
METHODS: Colonic anastomosis was performed in 120 rats divided into four groups: Group I - pneumoperitoneum before laparotomy, Group II - pneumoperitoneum after laparorrhaphy, Group III - pneumoperitoneum before laparotomy and after laparorrhaphy, Group IV - no pneumoperitoneum (control group). Pneumoperitoneum pressure was 5 mmHg. Animals were killed on the 3rd, 7th and 14th postoperative day. Hhistopathological features, anastomosis breaking strength, collagen histomorphometry and hydroxyproline concentration were assessed.
RESULTS: Breaking strength between groups: (day 3, p=0.165; day 7, p=0.219; day 14, p=0.539). Histopathology revealed that group II had, on day 7, less infiltration of mononuclear cells (p=0.006), greater infiltration of polymorphonuclear cells (p=0.001) and greater necrosis (p=0.001); and on day 14, less fibrosis. Histomorphometry revealed a decrease in collagen in groups I and III (p<0.001) on day 7 and an increase in groups I and II on day 14 (p<0.001). Hydroxyproline concentration was similar for groups on days 3 (p=0.152), 7 (p=0.913) or 14 (p=0.981).
CONCLUSION: Carbon dioxide does not impair the healing of colonic anastomosis in rats.
Key words: Pneumoperitoneum, Artificial. Carbon Dioxide. Anastomosis, Surgical. Wound Healing. Colon. Rats.
Introduction
The ability of the human body to heal a gastrointestinal anastomosis is a fascinating event. Although many improvements have been made in colorectal surgery, anastomotic failure still occurs and has devastating consequences for patients1.
Several factors that compromise the healing of colonic anastomosis, particularly the frequency of anastomotic leakage, have been studied2-6. Tension-free anastomosis, good vascularization, and the use of appropriate sutures and staples, for example, reduce the risk of anastomotic fistulas1.
Laparoscopy is a rather new form of surgery. The first laparoscopic surgery in the gastrointestinal tract was an appendectomy in 1983, followed in 1987 by a cholecystectomy6. In 1990, Jacobs performed the first laparoscopic colectomy7. After the publication of the Clinical Outcomes of Surgical Therapy (COST) study in 2004, which demonstrated that laparoscopy had similar results to those of open surgery in the treatment of colon cancer, but better postoperative outcomes8, many surgeons were excited about the procedure. Major studies were conducted and demonstrated the safety of laparoscopic surgery in oncology9-14.
Pneumoperitoneum is used in laparoscopic surgery to provide adequate surgical exposure.
Despite the increasingly frequent use of pneumoperitoneum in colorectal surgery, few studies have evaluated its effect on the healing of intestinal anastomosis15-21.
The most commonly used gas for pneumoperitoneum is carbon dioxide (CO2). It has low toxicity and is inexpensive. However, it can cause hypercapnia, acidemia and pulmonary hypertension22-24.
Increased intra-abdominal pressure caused by pneumoperitoneum may lead to systemic effects, such as acid-base imbalance, blood gas alterations, and pulmonary, cardiovascular, and renal impairment25-28. Another important result of increased intra-abdominal pressure is a decrease in splanchnic blood flow, which may lead to ischemia of the colon during laparoscopic colectomy and increase bacterial translocation and fistulas17.
Previous studies that evaluated the use of pneumoperitoneum for intestinal anastomosis reported different and sometimes contradictory results15-21. The pressure in rats that best correspond to the pressure used in laparoscopic surgery in humans is 5mmHg20,29,30, which is the pressure we used in this study.
This study evaluated the possible effects of pneumoperitoneum with carbon dioxide in the healing of colonic anastomosis.
Methods
This study was approved by the Ethics Committee on Animal Use of the Institute of Biological Sciences (protocol UnB doc nº 46986/2008).
This study was conducted in the Laboratory of Experimental Surgery of the School of Medicine, University of Brasilia (UnB), in collaboration with the Institute of Tropical Pathology, Federal University of Goias (UFG), and Laboratory of Biochemistry, Liver Transplantation and Experimental Surgery, School of Medicine of Ribeirao Preto (USP).
A total of 120 male Wistar rats aged about 90 days were used. After one week of acclimatization, the animals were kept in cages under a 12-h light: dark cycle with free access to a standard laboratory diet and water.
Animal weight was measured and recorded immediately before surgery and on the day that they were killed (Mars electronic scale, model AS5500 C, Mars Scales and Precision Equipment Ltd, Sao Paulo, Brazil).
The anesthetic and surgical procedures were supervised by veterinary staff, and the operations were performed by a single surgeon. The 120 rats were randomly divided into four groups of 30 animals, as follows:
Group I - 30 minutes of pneumoperitoneum before laparotomy.
Group II - 30 minutes of pneumoperitoneum after laparorrhaphy.
Group III - 30 minutes before laparotomy and 30 minutes after laparorrhaphy.
Group IV - no pneumoperitoneum (control group).
Surgical and anesthetic procedures
The animals were anesthetized with IM xylazine (10 mg/kg) and ketamine hydrochloride (75mg/kg).
In groups I and III, a Veres needle was introduced intraperitoneally in the midline 1 cm below the umbilicus. Pneumoperitoneum was established at a pressure of 5 mmHg for 30 minutes (25L Laparo Insufflator, Endoview, Recife, Brazil), and laparotomy was performed. In groups II and IV, laparotomy was performed without prior pneumoperitoneum.
A colon segment between 2.5 and 3.5 cm proximal to the peritoneal reflection was resected in all animals. An end-to-end anastomosis was performed using running 6-0 polypropylene suture (Brasuture, Sao Sebastiao da Grama, Brazil). The resected segment was washed, and the right mesenteric quadrant was isolated and frozen at -70ºC to determine hydroxyproline concentration. In groups II and III, the Veres needle was introduced into the abdominal wall under direct vision before suturing the abdominal wall. The abdominal wall was closed using a 5-0 polypropylene (Brasuture, Sao Sebastiao da Grama, Brazil) running suture.
In groups II and III, pneumoperitoneum was performed at a pressure of 5 mmHg for 30 minutes after the abdominal wall was sutured.
Postoperative procedures
After anesthetic recovery, the animals were kept in cages in groups of four (one from each experimental group). Animals that died underwent necropsy to determine the cause of death. The groups were subdivided into three subgroups of ten animals, which were killed on the 3rd, 7th or 14th postoperative day (POD). On the sacrifice day, after the induction of anesthesia, a 4 cm segment of bowel around the anastomosis was removed. The segment removed was cut in half between the mesenteric and the anti-mesenteric borders. The left segment underwent breaking strength testing. The right segment was divided in half. The mesenteric fragment was immersed in a solution of 0.9% NaCl and frozen at - 70ºC to determine the hydroxyproline concentration. The right anti-mesenteric quadrant was fixed in 10% buffered formalin for histopathological examination and quantitative analysis using collagen histomorphometry.
The animals were killed with an overdose of sodium ethyl thiobarbiturate (Thionembutal, Abbott Laboratories of Brazil Ltd., Sao Paulo, Brazil) injected into the vena cava.
Breaking strength of the anastomosis
The breaking strength of the anastomosis was tested using a Versa Test vertical test apparatus (Mecmesin Versa Test, Slinfold, West Sussex, United Kingdom) coupled to an AGF portable digital dynamometer (Panambra Industry Technical SA, Cambuci, Brazil). The rectangular fragment extracted and prepared for the test was fixed at both ends with the surgical scar at 0.5 cm between the clamps. The speed of the test was 25 mm/min, and the rupture value was expressed in Newtons (N).
Biochemical study
The concentration of hydroxyproline was measured for each animal during the operation (pretest sample) and the reoperation (posttest sample). Hydroxyproline concentration was determined in standardized anastomosis samples using the method described by Segemann and Stalder and modified by Medugorac4,5,31,32. The concentration of hydroxyproline was expressed in milligrams of hydroxyproline per gram of tissue.
Collagen histomorphometry
Histomorphometry of collagen in the perianastomotic regions was qualitatively evaluated using slides stained with picrosirius and imaged digitally. Images were captured using a Sony S85 digital camera (Sony Corporation, Tokyo, Japan) coupled to a Zeiss light microscope Axion Star (Carl Zeiss Vision, Ulm, Germany). Resolution was 1280 x 960 pixels, and all images were analyzed using the ImageJ software (Wayne Rasband, Research Services Branch, National Institute of Mental Health, Bethesda, MD, USA).
Histopathological study
After fixation in 10% buffered formalin, the specimens were prepared for paraffin blocks. Sections perpendicular to the anastomosis were stained with hematoxylin and eosin. An experienced pathologist blinded to animal group assessed healing using light microscopy.
The following characteristics were evaluated in each specimen: congestion, edema, hemorrhage, focal necrosis, mononuclear infiltration, polymorphonuclear infiltrate, neovascularization, granulation, fibrosis, abscess and ulceration.
Statistical analysis
Results were analyzed using SPSS 13.0, SigmaStat 2.0 and Microsoft Excel. Statistical analysis of deaths was performed using a chi-square test. To compare weights, we used analysis of variance (ANOVA). The Kruskal-Wallis test was used to compare breaking strength values. The Fisher exact test was used to compare histopathological findings. To test the deposition of hydroxyproline and collagen histomorphometry, the Kruskal-Wallis test and the Dunn procedure for multiple comparisons were used. The level of significance was set at 5% (p<0.05).
Results
Clinical progression
Of the 120 animals, six died during the experiment: four in Group I (one evisceration, one blocked fistula and two unknown causes), one in Group II (unknown cause) and one in Group IV (unknown cause). Although deaths were more frequent in group I, this difference was not statistically significant (p=0.097).
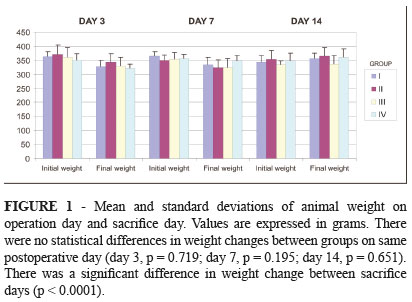
Animal weight
Baseline animal weight ranged from 312 g to 430 g (mean: 353.9 g), and final weight, from 273 g to 429 g (mean: 335.6 g). ANOVA revealed that there were no statistical differences between weights in the different groups on the same postoperative day (3rd POD, p=0.719; 7th POD, p=0.195; 14th POD, p=0.651), but the difference between the three days was statistically significant (p<0.0001) (Figure 1).
Breaking strength of the anastomosis
There were no statistically significant differences between groups on the 3rd POD (p=0.165), 7th POD (p=0.219), or the 14th POD (p=0.539). However, there was a significant difference when comparing the three days (p<0.0001) (Figure 2).
Hydroxyproline levels
Hydroxyproline levels were measured in samples obtained during the first operation (pretest) and at the time of reoperation (posttest). The pretest samples had no significant differences between Groups I and III (pneumoperitoneum before sample collection; 1.09 mg/g±0.24 mg/g) and Groups II and IV (no pneumoperitoneum before sample collection; 1.14 mg/g±0.32 mg/g; p=0.699).
There was a decrease in the mean value of hydroxyproline on sacrifice day (posttest) for all final time points compared with the day of operation (pretest).
There were no statistically significant differences in the hydroxyproline concentration between groups on the day the animals were killed (posttest; 3rd POD, p=0.152; 7th POD, p=0.913; 14th POD, p=0.981).
There was a gradual and significant increase in the amount of hydroxyproline according to sacrifice day (p<0.001; Figure 3).
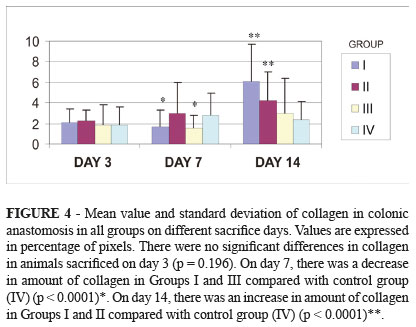
Histomorphometric study of collagen
There were no statistically significant differences in collagen between groups sacrificed on the 3rd POD (p=0.196). Among the animals sacrificed on the 7th POD, there was a significant decrease in the amount of collagen in Groups I and III compared with Group IV (control) (p<0.0001). Among the animals sacrificed on the 14th POD, there was a significant increase of collagen in Groups I and II compared with the control Group (IV) (p<0.0001) (Figure 4).
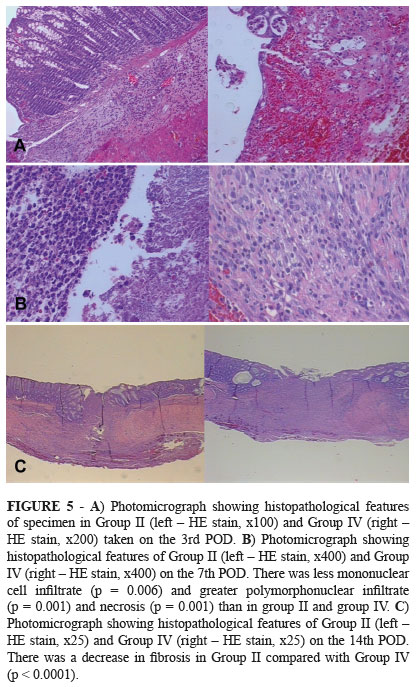
Histopathology
The histopathological examination of specimens from animals sacrificed on the 3rd POD showed a predominance of acute phenomena characterized by congestion, edema, hemorrhage, polymorphonuclear infiltrate and focal necrosis (Figure 5).
In animals sacrificed on the 7th POD, there were simultaneous acute and chronic phenomena characterized by polymorphonuclear infiltrate, increased mononuclear infiltrate, fibrosis, neovascularization and granulation. There was less mononuclear cell infiltration (p=0.006), greater polymorphonuclear infiltrate (p=0.001) and more necrosis (p=0.001) in group II compared with group IV (Table 1) (Figure 5).
In animals sacrificed on the 14th day, acute inflammation had disappeared and intense fibrosis was seen. There was a statistically significant decrease in fibrosis in Group II compared with Group IV (p<0.0001) (Figure 5) (Table 2).
Discussion
Laparoscopy has become increasingly more frequent in the practice of colorectal surgeons. The benefits of this procedure to patients, such as shorter hospitalization, less postoperative pain, and earlier return of bowel function, are indisputable. Oncological results similar to those of open surgery have also been reported by several studies, leading to an increasing demand for this type of surgery9-14.
Colonic anastomosis leakages are complications associated with high morbidity and mortality rates. Despite the increasingly frequent use of pneumoperitoneum in surgical procedures, especially in colorectal surgery, its effect on the healing of colonic anastomosis is controversial, which motivated this present study.
The animal chosen for the study was the Wistar rat, which has been used in several studies to evaluate healing of intestinal anastomosis5,15,17-21. The time points scheduled for reoperation and animal sacrifice represent three stages of healing: exudative or acute inflammatory response, proliferative fibroplasia and remodeling of mature collagen33.
Three mechanisms may affect intestinal healing in laparoscopic surgery: increased intra-abdominal pressure, the type of gas used and the time of exposure to the pneumoperitoneum.
Increased abdominal pressure occurs in various clinical situations, such as ascites, abdominal distension, ileus, mechanical obstruction, reduced hernia, pancreatitis, sepsis and trauma. Pressures above 20 mmHg indicate intra-abdominal hypertension, which is accompanied by significant deleterious abdominal and systemic effects25. Laparoscopic surgery uses carbon dioxide (CO2) to visualize the abdominal cavity, leading to increased abdominal pressure. The pressure used in laparoscopic surgery in humans is 12-15 mmHg. This pressure allows for good visualization of the peritoneal cavity with few metabolic and cardiovascular effects. In this study, the pneumoperitoneum in rats was achieved at a pressure of 5 mmHg, as several studies have shown that this pressure in rats corresponds to the pressure used in laparoscopic surgery in humans20,29,30. To our knowledge, there is no other study about the healing of the colon using this pressure in different times of the operation.
The length of exposure to pneumoperitoneum may affect the healing process, but in a study by Ozer et al.19the duration of pneumoperitoneum did not change histopathological parameters or hydroxyproline concentrations.
CO2is used by plastic surgeons, dermatologists and angiologists to increase circulation and tissue perfusion34. In laparoscopy, the hypercapnia induced by CO2 may lead to peripheral vasodilation, which may increase oxygenation in the anastomotic region and improve healing20. The overall mortality in our study was 5%, which is consistent with the rates between 0 and 11% reported in previous studies about anastomotic healing in rats5,15,17-21,35. There were no significant differences in number of deaths according to group.
The animals initially lost weight, but recovered their initial weight between the 7th POD and 14th POD, which is consistent with the literature35. There were no significant differences in the weight of animals killed on the same POD, which suggests that pneumoperitoneum performed with CO2 does not produce the metabolic changes that are followed by weight loss.
The breaking strength of the anastomosis provides rapid, accurate and reproducible results36. In this study, no significant differences between groups were found, but the values in group III (pneumoperitoneum before laparotomy and after laparorrhaphy) were higher than in the other groups at all postoperative days. Group III best represents laparoscopic colectomy, during which pneumoperitoneum is performed for the dissection, paused to remove the specimen and perform the surgical anastomosis or place the staples, and then restored to review the abdomen and the anastomosis. Our findings, therefore, suggest that laparoscopic surgery is safe for colonic anastomosis.
We found no significant differences in hydroxyproline concentration between groups, but the mean and median concentrations were higher in all treated groups than in the control group, which suggests that the pneumoperitoneum does not affect the formation of collagen.
No significant differences were found in collagen deposition on the 3rd POD. On the 7th POD, the amount of collagen was lower in groups I and III than in the control group. However, on the 14th POD, there was an increase in the amount of collagen in groups I and II, which may indicate that there is a delay in the healing process on the 7th POD, but a recovery and improvement by the 14th POD.
Histopathological examinations found acute phenomena on the 3rd POD, which progressively changed to chronic phenomena on the 7th and 14th POD. The significant differences between group II and the control group suggest that healing is delayed in this group. In rats that received pneumoperitoneum after suture, Kologlu et al.18 found delayed healing up to the 4th POD, when the animals were killed.
Our review of studies in the literature revealed that anastomotic healing was worse when rats were exposed to high intra-abdominal pressures that corresponded to human intra-abdominal hypertension15,17 or to prolonged pneumoperitoneum18. Studies with rats that used pressures corresponding to those used in laparoscopic surgery in humans found no worsening of healing20-21.
Theoretically, the increased abdominal pressure inherent to laparoscopic surgery might cause transient ischemia, healing impairment and a consequent increase of anastomotic fistula. Other studies demonstrated that reduced intestinal oxygenation worsened healing37-39. In this study, healing was not impaired, which demonstrates that there are no effects of ischemia at a pressure of 5mmHg.
Healing is complex and depends not only on the amount of collagen, but also on the type and structure of collagen. The best way to assess the anastomosis healing would be the leakage; however, such an occurrence is small, what made us to use other parameters: clinical outcome, anastomotic breaking strength, hydroxyproline, collagen histomorphometry and histopathological evaluation.
Conclusion
Although some changes were seen in collagen histomorphometry and histopathology in this study, analyzing all the parameters together, the use of pneumoperitoneum with CO2 at a pressure of 5mmHg in different periods of the operation did not impair the healing of colonic anastomosis in rats.
Received: May 14, 2013
Review: July 15, 2013
Accepted: Aug 16, 2013
Conflict of interest: none
Financial source: none
- 1. Abbas MA. Anastomotic leak: should we continue to accept the risks? Dis Colon Rectum. 2010;53(6):859-60.
- 2. Ravo B. Colorectal anastomotic healing and intracolonic bypass procedure. Surg Clin North Am. 1988;68(6):1267-94.
- 3. Koruda MJ, Rolandelli RH. Experimental studies on the healing of colonic anastomoses. J Surg Res. 1990;48(5):504-15.
- 4. de Sousa JB, Soares EG, Aprilli F. Effects of diclofenac sodium on intestinal anastomotic healing. Experimental study on the small intestine of rabbits. Dis Colon Rectum. 1991;34(7):613-7.
- 5. de Oliveira PG, Soars' EG, Arielle F. Influence of misoprostol, a synthetic prostaglandin E1 analog, on the healing of colonic anastomoses in rats. Dis Colon Rectum. 1994;37(7):660-3.
- 6. Dubois F, Berthelot G, Levard H. Laparoscopic cholecystectomy: historic perspective and personal experience. Surg Laparosc Endosc. 1991;1(1):52-7.
- 7. Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1(3):144-50.
- 8. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050-9
- 9. Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10(1):44-52.
- 10. Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248(1):1-7.
- 11. Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J. Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev. 2008;34(6):498-504.
- 12. Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25(21):3061-8.
- 13. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477-84.
- 14. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718-26.
- 15. Ozgun H, Boylu S, Cevikel MH, Yenisey C, Erpek H, Culhaci N, Demirkiran AE. Effects of pneumoperitoneum with or without colostomy on rat colonic anastomotic healing. ANZ J Surg. 2004;74(3):158-63.
- 16. Olson KH, Balcos EG, Lowe MC, Bubrick MP. A comparative study of open, laparoscopic intracorporeal, and laparoscopic assisted low anterior resection and anastomosis in pigs. Am Surg. 1995;61(3):197-201.
- 17. Polat C, Arikan Y, Vatansev C, Akbulut G, Yilmaz S, Dilek FH, Gokce O. The effects of increased intraabdominal pressure on colonic anastomoses. Surg Endosc. 2002;16(9):1314-9.
- 18. Kologlu M, Sayek I, Kologlu LB, Onat D. Effect of persistently elevated intraabdominal pressure on healing of colonic anastomoses. Am J Surg. 1999;178(4):293-7.
- 19. Ozer I, Ulas M, Ercan M, Ozogul YB, Zengin N, Bostanci EB, Ozel U, Bilgihan A, Akoglu M. The effects of duration of CO2 pneumoperitoneum on colonic anastomosis. J Invest Surg. 2008;21(4):177-81.
- 20. Rosch R, Stumpf M, Junge K, Drinjakovic D, Schachtrupp A, Afify M, Schumpelick V. Influence of pneumoperitoneum on small bowel anastomoses: a histological analysis in the rat model. J Invest Surg. 2005;18(2):63-9.
- 21. Tytgat SH, Rijkers GT, van Der Zee DC. The influence of the CO2 pneumoperitoneum on a rat model of intestinal anastomosis healing. Surg Endosc. 2012;26(6):1642-7.
- 22. Gerges FJ, Kanazi GE, Jabbour-Khoury SI. Anesthesia for laparoscopy: a review. J Clin Anesth. 2006;18(1):67-78.
- 23. Fernandez-Cruz L, Saenz A, Taura P, Sabater L, Astudillo E, Fontanals J. Helium and carbon dioxide pneumoperitoneum in patients with pheochromocytoma undergoing laparoscopic adrenalectomy. World J Surg. 1998;22(12):1250-5.
- 24. Neuberger TJ, Andrus CH, Wittgen CM, Wade TP, Kaminski DL. Prospective comparison of helium versus carbon dioxide pneumoperitoneum. Gastrointest Endosc. 1996;43(1):38-41.
- 25. Ivatury RR, Diebel L, Porter JM, Simon RJ. Intra-abdominal hypertension and the abdominal compartment syndrome. Surg Clin North Am. 1997;77(4):783-800.
- 26. Safran DB, Orlando R3rd Physiologic effects of pneumoperitoneum. Am J Surg. 1994;167(2):281-6.
- 27. Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110(3):810-5.
- 28. Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, Buchler MW. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg. 2004;21(2):95-105.
- 29. Avital S, Itah R, Szomstein S, Rosenthal R, Inbar R, Sckornik Y, Weinbroum A. Correlation of CO2 pneumoperitoneal pressures between rodents and humans. Surg Endosc. 2009;23(1):50-4.
- 30. Berguer R, Cornelius T, Dalton M. The optimum pneumoperitoneum pressure for laparoscopic surgery in the rat model. A detailed cardiorespiratory study. Surg Endosc. 1997;11(9):915-8.
- 31. Stegemann H, Stalder K. Determination of hydroxyproline. Clin Chim Acta. 1967;18(2):267-73.
- 32. Medugorac I. Collagen content in different areas of normal and hypertrophied rat myocardium. Cardiovasc Res. 1980;14(9):551-4.
- 33. Herrmann JB, Woodward SC, Pulaski EJ. Healing of colonic anastomoses in the rat. Surg Gynecol Obstet. 1964;119:269-75
- 34. Brandi C, D'Aniello C, Grimaldi L, Bosi B, Dei I, Lattarulo P, Alessandrini C. Carbon dioxide therapy in the treatment of localized adiposities: clinical study and histopathological correlations. Aesthetic Plast Surg. 2001;25(3):170-4.
- 35. Mastboom WJ, Hendriks T, de Man BM, de Boer HH. Influence of methylprednisolone on the healing of intestinal anastomoses in rats. Br J Surg. 1991;78(1):54-6.
- 36. Rossi LF, Ramos RR, Ely JB, Kestering DM, Soldi MS, Brum SPB, d'Acampora AJ. Considerations that may influence the result of trials assessing tensile strength in experimental surgery. Acta Cir Bras. 2007;22(6):499-502.
- 37. Posma LA, Bleichrodt RP, van Goor H, Hendriks T. Transient profound mesenteric ischemia strongly affects the strength of intestinal anastomoses in the rat. Dis Colon Rectum. 2007;50(7):1070-9.
- 38. Posma LA, Bleichrodt RP, Lomme RM, de Man BM, van Goor H, Hendriks T. Early anastomotic repair in the rat intestine is affected by transient preoperative mesenteric ischemia. J Gastrointest Surg. 2009;13(6):1099-106.
- 39. Posma LA, Hendriks T, Verhofstad AA, de Man BM, Lomme RM, Bleichrodt RP. Reduction of oxygenation and blood flow in pedicled bowel segments in the rat and its consequences for anastomotic healing. Dis Colon Rectum. 2010;53(1):93-100.
Publication Dates
-
Publication in this collection
29 Aug 2013 -
Date of issue
Sept 2013
History
-
Received
14 May 2013 -
Accepted
16 Aug 2013 -
Reviewed
15 July 2013