Abstract
PURPOSE: To evaluate the effects of acute alcohol intoxication on healing of colonic anastomosis. METHODS: Thirty-six rats were allocated into two groups. Animals in the alcohol (A) were given 2 mL of ethanol diluted in 0.9% saline solution to a concentration of 40% by gavage immediately before anesthesia, whereas control (C) animals received 2 mL of 0.9% saline solution via the same route. A colonic anastomosis was then performed in all animals. On postoperative days 1, 3, and 7, anastomotic breaking strength was assessed and histopathological examination was performed. Change in body weight and mortality were also evaluated. RESULTS: The median of anastomotic tensile strength on the postoperative day 1 was 0.09 Newtons for group A and 0.13 for group C. (p>0.05). The median of anastomotic tensile strength on the postoperative day 3 was 0.13 Newtons for group A and 0.17 for group C. (p>0.05). The median of anastomotic tensile strength on the postoperative day 7 was 0.30 Newtons for group A and 0.35 for group C. (p>0.05). There was no significant difference between the groups A and C, in the first, third or seventh POD (p>0.05), in any of the analyzed parameters. There were no statistical differences between groups in the weight. Three animals died, all from the group A. CONCLUSION: Acute alcohol intoxication did not interfere with wound healing of colonic anastomoses, although it caused early postoperative mortality.
Wound Healing; Alcoholism; Ethanol; Tensile Strength; Rats
3 ORIGINAL ARTICLE
WOUND HEALING
Does acute alcohol intoxication interfere with colonic anastomosis wound healing? A rat model of nondestructive colon trauma1 1 Research performed at Experimental Surgery Laboratory, School of Medicine, Brasilia University (UnB), Brasilia-DF, Brazil.
Pedro Henrique Alves de MoraisI; Igor Eduardo Caetano de FariasI; Vinícius Lacerda RibeiroI; Luiz Eduardo Almeida SilvaI; Fabiana Pirani CarneiroII; Joel Paulo Russomano VeigaIII; João Batista de SousaIV
IGraduate students, School of Medicine, Brasilia University (UnB), Brasilia-DF, Brazil. Grants from Institutional Program for Scientific Initiation (PIBIC) of the National Council of Technological and Scientific Development (CNPq), Ministry of Science, Technology and Inovation, Brazil. Design the protocol, technical procedures, acquisition and interpretation of data, statistical analysis, manuscript writing
IIPhD, Associate Professor of Pathology, School of Medicine, UnB, Brasilia-DF, Brazil. Pathological analysis, critical revision
IIIPhD, Associate Professor, Medical Clinics, School of Medicine, UnB, Brasilia-DF, Brazil. Interpretation of data, statistical analysis, critical revision
IVPhD, Associate Professor of Surgery, School of Medicine, UnB, Brasilia-DF, Brazil. Intellectual and scientific content of the study, design the protocol, technical procedures, interpretation of data, statistical analysis, manuscript writing, critical revision
Correspondence Correspondence: João Batista de Sousa Universidade de Brasília Campus Universitário Darcy Ribeiro-Faculdade de Medicina Laboratório de Cirurgia Experimental 70910-900 Brasília DF Brasil Tel.: (55 61)9984-2845 sousajb@unb.br
ABSTRACT
PURPOSE: To evaluate the effects of acute alcohol intoxication on healing of colonic anastomosis.
METHODS: Thirty-six rats were allocated into two groups. Animals in the alcohol (A) were given 2 mL of ethanol diluted in 0.9% saline solution to a concentration of 40% by gavage immediately before anesthesia, whereas control (C) animals received 2 mL of 0.9% saline solution via the same route. A colonic anastomosis was then performed in all animals. On postoperative days 1, 3, and 7, anastomotic breaking strength was assessed and histopathological examination was performed. Change in body weight and mortality were also evaluated.
RESULTS: The median of anastomotic tensile strength on the postoperative day 1 was 0.09 Newtons for group A and 0.13 for group C. (p>0.05). The median of anastomotic tensile strength on the postoperative day 3 was 0.13 Newtons for group A and 0.17 for group C. (p>0.05). The median of anastomotic tensile strength on the postoperative day 7 was 0.30 Newtons for group A and 0.35 for group C. (p>0.05). There was no significant difference between the groups A and C, in the first, third or seventh POD (p>0.05), in any of the analyzed parameters. There were no statistical differences between groups in the weight. Three animals died, all from the group A.
CONCLUSION: Acute alcohol intoxication did not interfere with wound healing of colonic anastomoses, although it caused early postoperative mortality.
Key words: Wound Healing. Alcoholism. Ethanol. Tensile Strength. Rats.
Introduction
Preoperative assessment has become part of daily practice before surgery of the colon and other organs, but alcohol abuse has not received much attention1. Acute alcohol exposure represents a risk factor for increased morbidity and mortality associated with surgical or traumatic injury in human patients2. After colonic anastomosis surgery, the prognosis of the patient depends to a large extent on healing of the colonic wound.
Inappropriate wound healing of colonic anastomosis can lead to complications such as dehiscence and leakage, which can result in catastrophic consequences; the mortality rate following anastomotic leak ranges from 6.039.3%3.
The overall leakage rate after colonic anastomosis usually ranges from 3.4% to 6%3,4. In abdominal trauma, the risk of this complication after anastomosis is higher, ranging from 7% to 14% in low-risk patients up to 40% in high-risk patients5,6.
The prevalence of alcohol intoxication in trauma patients at the time of hospital admission ranges from 18% to 80%7.
Higher blood alcohol levels have been found to correlate with more severe abdominal injuries, including colonic injuries, in trauma patients8. However, the same study found that alcohol intake was not an independent risk factor for worse outcome, overall injury severity, or posttraumatic complications in patients with multiple trauma8.
Primary repair is considered the optimal technique for nondestructive colon injury at most institutions, regardless of risk factors5. We hypothesized that acute alcohol exposure shortly before surgery would be a risk factor for impaired wound healing of the colonic anastomosis, based on results from other experimental studies9-12. However, in those studies, alcohol exposure followed different patterns.
The effects of alcohol abuse on patient prognosis and on experimental wound healing are highly controversial, because they depend on the type of exposure and on the presence of associated factors such as sepsis12.
The purpose of this study was to evaluate the effects of acute alcohol intoxication on colonic anastomosis wound healing and postoperative outcomes in rats.
Methods
All procedures were performed in accordance with the ethical standards proposed by the Brazilian College of Animal Experimentation (COBEA). Approval was obtained from the Animal Research Ethics Committee of the University of Brasilia, Brazil, prior to the study.
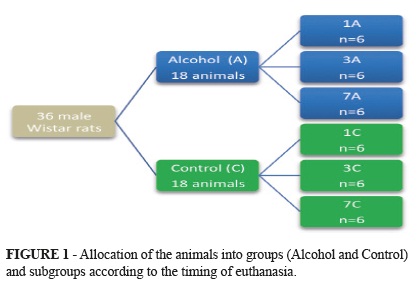
This was a randomized, single-blind experimental study. Thirty-six male Wistar rats were randomly allocated into two groups of 18 animals each: an experimental group that received alcohol (A) preoperatively and a control group (C) that did not. Each group was subdivided into three subgroups according to the timing of euthanasia (postoperative day 1, 3, or 7), yielding groups 1A, 3A, 7A and 1C, 3C, 7C (Figure 1).
On the day of surgery, rats were fasted for one hour. Animals in group A received 2 mL of ethanol diluted in 0.9% saline solution to a concentration of 40%, given by mouth using the gavage method. This dose is equivalent to an intake of 480 mL of spirits (approximately 10 shots) in a young adult man weighing 75 kg. Half of the dose (1 mL) was given at once and the remaining 1 mL was given 1 hour later, also by mouth, immediately before anesthesia. Surgeons were blinded to group allocation, and all surgeries were performed by the same team. Control group animals received 2 mL of 0.9% saline solution using the same protocol.
Anesthesia was induced by intramuscular injection of xylazine (10 mg/kg) and ketamine (75 mg/kg). After induction, the abdomen was disinfected with iodinated detergent.
A midline abdominal incision approximately 4.5 cm in length, starting 1 centimeter cranial to the symphysis pubis, was made. A 1-centimeter segment of the left colon was resected, and an end-to-end anastomosis was performed with single-layer running sutures using 6-0 polypropylene. Abdominal wall closure was performed with running sutures, in two layers, using 3-0 polypropylene. Postoperative analgesia was provided with tramadol (0.72 mg/kg every 12 hours).
On postoperative day 1, 3, or 7, according to subgroup allocation, the animals were weighed and anesthetized. Colon specimens were collected and the animals were killed with an overdose of thiopental by intravenous injection.
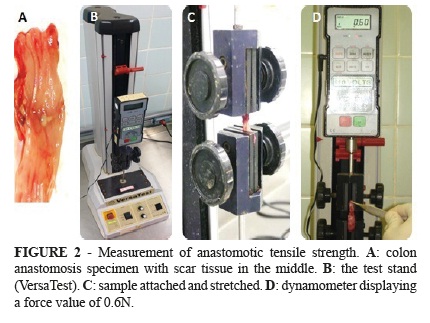
Anastomotic tensile strength (ATS) was evaluated with a VersaTest motorized test stand (Mecmesin VersaTest, United Kingdom), coupled to a digital dynamometer to which the colonic anastomosis samples were attached (Figure 2). The maximum traction force that the tissue could withstand before rupture was measured in Newtons (N).
A sample of the anastomotic scar tissue was collected for histopathological analysis, fixed in formalin, and stained with hematoxylin and eosin. The amount of collagen, fibroblast, mononuclear and polymorphonuclear infiltration and neovascularization was graded qualitatively on a scale of 0 to 3, where 0 = absent and 3 = marked. Abscess, bacterial colonization, foreign body, crust, and fibrin formation were scored dichotomously as 0 or 1, meaning absent or present, respectively.
Results were analyzed in SPSS (Statistical Package for the Social Sciences) 18.0. Parametric and nonparametric tests were used as appropriate according to the nature of the variables. The paired-samples t-test was used for comparison of body mass, and the KruskalWallis test for anastomotic tensile strength. Fisher's exact test was used for statistical analysis of all histopathological variables. Significance was set at p<0.05.
Results
Anastomotic tensile strength (ATS)
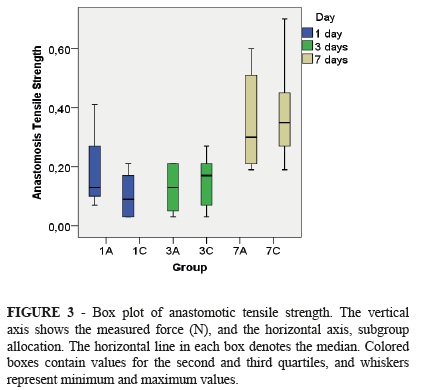
Among animals killed on postoperative day 1 (blue boxes, Figure 3), group 1C (controls) had a median ATS of 0.09 N (interquartile range 0.15 N), whereas group 1A had a median ATS of 0.13 N and an undetermined interquartile range. There were no significant difference between these groups (p>0.05).
Among animals killed on postoperative day 3 (green boxes, Figure 3), group 3C had a median ATS of 0.17 N (interquartile range 0.17 N), and group 3A, a median ATS of 0.13 N (interquartile range 0.16 N). Again, there was no significant difference between these groups (p>0.05).
Among animals killed on postoperative day 7 (beige boxes, Figure 3), group 7C had a median ATS of 0.35 N (interquartile range 0.26 N), and group 7A, a median ATS of 0.3 N (interquartile range 0.33 N). There was no significant between-group difference (p>0.05).
Histopathology
There were no significant differences in any of the analyzed parameters between groups C and A, whether on postoperative days 1, 3, or 7 (p>0.05) (Table 1).
Body weight
Overall, the mean preoperative body weight was 310 ± 7.85 g, and the mean postoperative body weight, 291 ± 7 g. The only animals that did not lose weight postoperatively were those in group 1A. All other subgroups lost weight between postoperative day 0 and the time of euthanasia (Table 2).
Mortality rate
There were three deaths, all in group 1A, which corresponds to a 50% mortality rate in this subgroup and 16.6% if all alcohol-exposed animals are considered.
Discussion
Studies evaluating the effects of alcohol on trauma, colon surgery, and wound healing have reported conflicting findings, because the effects of alcohol intake depend on the pattern of exposure (chronic or acute), the amount ingested, the duration of intake, the time since alcohol exposure, the presence of alcohol withdrawal, and other associated factors11. Epidemiological studies usually include patients with all types of exposures, and the outcome may depend on the prevailing type.
In this study, we analyzed the effects of acute alcohol intoxication on colon wound healing and prognosis in healthy rats, with no comorbidities, given a large amount of alcohol (in terms of ethanol intake per kg body weight) over a short time just before surgery. This model is representative of a substantial portion of human patients with colonic trauma, as alcohol is involved in up to 80% of incidents causing trauma and most of those patients are not chronic abusers, but rather were binge drinking7. In the present study, this type of alcohol exposure did not affect colonic anastomosis healing.
Alcohol is one of most important risk factors for fatal injuries in trauma, contributing to one-third of all deaths from accidents. In traffic incidents, it is responsible for a twofold mortality rate, higher impact speed, greater injury severity, and higher preclinical mortality7. In our sample, the mortality rate was 50% in group 1Awhich corresponds to early and even preclinical deathversus zero in the control animals.
Experimental and epidemiological studies of chronic alcohol abusers have found alcohol to be deleterious to many aspects of the postoperative period, such as wound healing, reoperation rate, leakage, weight loss, and the metabolic response to trauma and surgery1,11. Although this patient population clearly suffers the effects of alcohol abuse on wound healing, with higher mortality and morbidity rates, these effects are reversible after two weeks to three months1.
Pereira et al.9 has shown that a model of chronic alcohol abuse in rats is associated with lower weight gain, impaired intestinal healing (as demonstrated by significantly lower bowel anastomosis breaking strength), and higher postoperative complication rates.
We did not find a higher risk of colon dehiscence in the treated group. Therefore, emergent primary repair of nondestructive colon injuries in patients with acute alcohol intoxication seems to be safe, corroborating the current practice of most hospitals5.
Nevertheless, a previous study by our research group found that colonic anastomosis wound healing is impaired in rats with peritoneal sepsis and acute alcohol intake with the same alcohol exposure pattern used in the current study12. This suggests that diversion may be required if the intoxicated patient has fecal contamination and sepsis, as occurs in destructive colon trauma, for instance12. In our previous study, which included two groups (sepsis + alcohol and sepsis alone), the sepsis group exposed to alcohol exhibited poorer wound healing. Therefore, this type of alcohol exposure may act not as an independent risk factor, but as a cofactor.
Conclusion
In the exposure pattern used experimentally in this study, acute alcohol intoxication did not interfere with wound healing of colonic anastomoses, although it did increase early postoperative mortality.
Acknowledgements
To UnB Academic League for Emergency and Trauma (LETUnB) for its support and for stimulating our curiosity in the fields of trauma surgery and emergency medicine.
Received: June 05, 2013
Review: Aug 07, 2013
Accepted: Sept 09, 2013
Conflict of interest: none
Financial source: none
- 1. Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86(7):869-74.
- 2. Radek KA, Mathies A M, Burns AL, Heinrich SA, Kovacs EJ, Dipietro LA. Acute ethanol exposure impairs angiogenesis and the proliferative phase of wound healing. Am J Physiol Heart Circ Physiol. 2005;289(3): H1084-90.
- 3. Chambers WM, Mortensen NJ. Postoperative leakage and abscess formation after colorectal surgery. Best Pract Res Clin Gastroenterol. 2004;18(5):865-80.
- 4. Buchs NC, Gervaz P,Secic M , Bucher P, Mugnier-Konrad B, Morel P. Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis. 2008;23(3):26570.
- 5. Miller PR, Fabian TC, Croce MA, Magnotti LJ, Pritchard FE, Minard G, Stewart RM. Improving outcomes following penetrating colon wounds: application of a clinical pathway. Ann Surg. 2002;235(6):775-81.
- 6. Ott MM, Norris PR, Diaz JJ, Collier BR, Jenkins JM, Gunter OL, Morris JA. Colon anastomosis after damage control laparotomy: recommendations from 174 trauma colectomies. J Trauma. 2011;70 (3):595-602.
- 7. Stübig T, Petri M, Zeckey C, Brand S, Müller C, Otte D, Krettek C, Haasper C. Alcohol intoxication in road traffic accidents leads to higher impact speed difference, higher ISS and MAIS, and higher preclinical mortality. Alcohol. 2012;46(7):681-6.
- 8. Zeckey C, Danneckera S, Hildebrand F, Mommsen P, Scherer R, Probst C, Krettek C, Frink M. Alcohol and multiple trauma: is there an influence on the outcome? Alcohol. 2011;45(3):245-51.
- 9. Pereira RSC, Hasimoto CN, Pelafsky L, Llanos JC, Cataneo DC, Spadella CT, Minossi JG. Intestinal healing in rats submitted to ethanol ingestion. Acta Cir Bras. 2012;27(3):236-43.
- 10. Molina PE, Zambell KL, Noremberg K, Eason J, Phelan H, Zhang P, Stouwe CV, Carnal JW, Porreta C. Consequences of alcohol-induced early dysregulation of responses to trauma/hemorrhage. Alcohol. 2004;33(3):217-27.
- 11. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219-29.
- 12. Morais PH, Ribeiro VL, Caetano de Farias IE, Almeida Silva LE, Carneiro FP, Russomano Veiga JP, Sousa JB. Alcohol acute intoxication before sepsis impairs the wound healing of intestinal anastomosis: rat model of the abdominal trauma patient. World J Emerg Surg. 2012;7(Suppl 1):S10.
Correspondence:
Publication Dates
-
Publication in this collection
07 Oct 2013 -
Date of issue
Oct 2013
History
-
Received
05 June 2013 -
Accepted
09 Sept 2013 -
Reviewed
07 Aug 2013