Abstract
PURPOSE: To investigate the small intestinal tissue alterations in rats submitted to ischemia and tissue reperfusion using pentoxyfilline or prostaglandin E1. METHODS: Thirty five Wistar rats were used, distributed into group control (A) n=10 were submitted to intestinal ischemia and reperfusion during 60 minutes and no one drug have been utilized. In the group pentoxyfilline (B) n=10 have been utilized during tissue ischemia and reperfusion as well as prostaglandin E1 (C) n=10, but separately. In the group sham (D) n=5, the animals were submitted to surgical. After euthanasia of the animals, a segment of the small intestine was cut, stained by hematoxilin-eosin and histological analysis according to Chiu criteria. RESULTS: Histological results showed that using pentoxyflline or prostaglandin E1 the results during tissue reperfusion were better, since the levels of criteria from Chiu that predominated were level 2 and 3, indicating less tissue damage in comparison to the control group (group A) that showed levels 4 and 5, what means more severe histological tissue alterations. CONCLUSION: Use of pentoxyfilline or prostaglandin E1 promoted a beneficial effect during intestinal reperfusion, demonstrated by less severe histological lesions in the small intestine mucosa of rats submitted to ischemia and tissue reperfusion when helped by the drugs.
Ischemia; Reperfusion; Intestine, Small; Alprostadil; Rats
4 - ORIGINAL ARTICLE
ISCHEMIA-REPERFUSION
Ischemia and reperfusion of rat small intestine using pentoxyfilline and prostaglandin E11 1 Research performed at Laboratory of Experimental Surgical Technique, Federal University of Mato Grosso (UFMS), Campo Grande-MS, Brazil. Part of PhD degree thesis, Postgraduate Program in Health and Development. Tutor: Ricardo Dutra Aydos.
José Lacerda BrasileiroI; Celso Maschaschi InoyeII; Ricardo Dutra AydosIII; Iandara Schettert SilvaIV; Gustavo Ribeiro FalcãoV; Guido MarksVI; Daniel Martins PereiraVII
IFellow PhD degree, Postgraduate Program in Health and Development, Federal University of Mato Grosso do Sul (UFMS). Assistant Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Analysis and interpretation of data, manuscript writing
IIPhD, Associate Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Conception and design of study, critical revision
IIIPhD, Associate Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Guidance and experimental design
IVPhD, Associate Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Helped with technical procedures
VAssistant Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Histopathological examinations
VIPhD, Associate Professor, Department of Surgery, UFMS, Campo Grande-MS, Brazil. Critical revision, supervised all phases of the study
VIFellow PhD degree, Postgraduate Program in Health and Development, UFMS, Campo Grande-MS, Brazil. Statistical analysis, critical revision
Correspondence Correspondence: Ricardo Dutra Aydos Avenida Senador Felinto Muller, s/n 79080-190 Campo Grande - MS Brasil ricadoaydos@gmail.com
ABSTRACT
PURPOSE: To investigate the small intestinal tissue alterations in rats submitted to ischemia and tissue reperfusion using pentoxyfilline or prostaglandin E1.
METHODS: Thirty five Wistar rats were used, distributed into group control (A) n=10 were submitted to intestinal ischemia and reperfusion during 60 minutes and no one drug have been utilized. In the group pentoxyfilline (B) n=10 have been utilized during tissue ischemia and reperfusion as well as prostaglandin E1 (C) n=10, but separately. In the group sham (D) n=5, the animals were submitted to surgical. After euthanasia of the animals, a segment of the small intestine was cut, stained by hematoxilin-eosin and histological analysis according to Chiu criteria.
RESULTS: Histological results showed that using pentoxyflline or prostaglandin E1 the results during tissue reperfusion were better, since the levels of criteria from Chiu that predominated were level 2 and 3, indicating less tissue damage in comparison to the control group (group A) that showed levels 4 and 5, what means more severe histological tissue alterations.
CONCLUSION: Use of pentoxyfilline or prostaglandin E1 promoted a beneficial effect during intestinal reperfusion, demonstrated by less severe histological lesions in the small intestine mucosa of rats submitted to ischemia and tissue reperfusion when helped by the drugs.
Key words: Ischemia. Reperfusion. Intestine, Small. Alprostadil. Rats.
Introduction
The subtle interruption of the arterial blood supply at any region of the human body promotes a tissue ischemia, which gives initiation of many metabolic alterations in the referred area, causing even a tissue necrosis. To repair this special area it is mandatory a tissue reperfusion. If this subtle interruption occurs partially or in the whole small intestine, with a high intensity, many times it is not possible to maintain even the basal metabolism and, consequently, there is cell death and tissue necrosis1-4. The intestinal mucosa in the small intestine, it is the first area to be severely affected in cases of ischemia. An ischemia with more than one hour duration could produce edema at submucosa, followed by loosening of the superficial mucosa and it could produce ulcers and/or bleeding in the intestinal villous3-5. When the intestinal barrier is lost, its content could go to the blood flow, with synthesis of inflammatory local factors, aggravating the lesions and mobilization of defense cells, beside to the risk of bacterial translocation. The maintenance of ischemia increases the inflammatory edema, causing derangement of the tissue microenvironment and facilitating the lesions dissemination to a more extensive area of intestinal mucosa. The involvement of the muscular layer will disturb the peristaltic movements with consequent stagnation of the intestinal content and increase of the local pressure4-9 .
It is well known that ischemia could cause tissue necrosis but if a reperfusion is done the blood flow could be reestablished, as well as recovery of tissue oxygenation in the area, bringing indispensable nutrients to tissue repair. However and paradoxally the liberation of free radicals could increase the local lesions and provoke lesions far away from the ischemic area. Therefore, the histopathological tissue alterations consequent to blood flow deprivation would be detected microscopically, by light microscopy or by imunohistochemical techniques, showing tissue alterations in the area submitted to ischemia and reperfusion3,4. At those areas the integrity of cell membrane could suffer with hypoxia and the cell itself could miss the ideal amount of energy production as well as accumulate, direct or indirectly, metabolites and inflammatory mediators causing cellular dysfunction9-15.
To minimize the ischemic effects on cells many types of drugs have been used during intestinal reperfusion as pentoxyflline16 (PTX) and prostaglandin E1 (PGE1)17, in the ischemic-reperfusion process (I/R). PTX has antioxidant action inhibiting directly the anion superoxide, which indirectly blocks the action of the enzyme xanthine-oxidase. Beside to that, it seems to diminish the intensity of inflammatory response, reduce migration of neutrophils to the area, difficult the liberation of citokynes, the tumoral necrosis factor, platellet activating factors and endothelin, a potent vasoconstrictor substance, among other factors1,13,14,16.
The PGE1 is known by its intense vasodilator effect and as a substance with intense biological activity that has been used for such a longtime in the treatment of chronic occlusive arterial disease. This substance also has capacity to avoid platellet aggregation. PGE1 has a role in the activation of fibrinolysis and/or fibrogenesis, in the modulation of cellular proliferation, in the hemorreologic activity of erithocytes, in the inhibition and activation of neutrophils capacities and also in the utilization of oxygen and glucose by the tissues. Beside to those effects there is evidence that PGE1 stimulates angiogenesis in cases of myocardic ischemia17-19.
Considering all theorical support presented above, it is our purpose to test the action of PTX and PGE1 in the appearance of histological lesions at small intestine mucosa in rats, in the process of ischemia and tissue reperfusion (I/R).
Methods
The experiments were approved and registered by Research Ethical Committee, Medical School, UFMS (protocol number 308).
Thirty five animals were utilized (Rattus norvegicus) Wistar lineage, albinic, male, adults, with approximately 260g body weight. The animals were maintained in boxes with five animals in each box, allocated in the shelves with ventilation and at animal room temperature and humidity was controlled. The light cycle was controlled with 12h lightness and 12h darkness.
The animals were distributed (Figure 1) in A, B, C groups with ten animals each (n=10) and group D with five animals. The animals of the experimental groups were submitted to 60 minutes of ischemia followed by 60 minutes of tissue reperfusion. At group B the drug utilized was PTX, 40 mg.kg-1, with 20 mg.kg -1 distributed during three minutes before the initial period of ischemia and 20 mg.kg-1 during three minutes before the initial period of tissue reperfusion. PGE1 5 µg.Kg-1 was distributed with 2,5 µg.Kg-1 during three minutes before the initial period of ischemia and 2,5 µg.Kg-1 during three minutes before the initial period of tissue reperfusion. The control group did not receive any drugs for reperfusion (group A). The group D, the Sham group, all animals were submitted to analgesy, anesthesia and laparotomy without mesenteric artery occlusion (no ischemia) and no one drug have been used for reperfusion.
Procedures
The animals have been isolated in the boxes and located at one special room during three hours, with the aim to diminish the pre-operative stress an at that time they were weighted.
Dissociative anesthesia
Realized with a solution of 2:1 ketamine hydrochloride (50.mg/ml-1) and xylazine (20mg/ml-1) which dose was 0,1ml/100g-1 body weight was administered by intraperitoneal way.
Analgesy
Utilized nalbuphine (Nubain®) administered on a dose of 2mg/Kg-1 by subcutaneous way, to reduce pain during time that animals were still awaked for ischemia and reperfusion procedures and after anesthetic recovery that occurs approximately 20 minutes after the initial anesthesia.
Preoperative procedure
The animals were tricotomized in the inferior third of abdomen, the antissepsy has been done with soft brush and topical iodopirrolidin 2% and washed with saline solution 0,9%.
Surgery- (Figure 2)
The animal was positioned with the abdomen in frontal position to facilitate the incision and antissepsy was done with alcohol plus 2% iodine. The sterilized protections have been used to isolate the surgical field.
A longitudinal median incision has been done in the abdomen (median laparotomy) with 30 mm of length, sectioning the cellular subcutaneous tissue, the white line, using the blade nº 15 to expose the whole abdominal cavity and for exteriorization of the small intestine, identification and isolation of the superior mesenteric artery. This artery was occluded with an atraumatic vascular clamp during 60 minutes (ischemic phase). After this phase the intestine has been repositioned internally into the abdominal cavity by continuous sutures (with nylon monofilamentar 3-0 (mononylon®) and closed the incision.
Tissue reperfusion procedure
The animal was again anesthetized and submitted to the same anesthesia already described above, and in dorsal position the antissepsy of the skin was realized similarly. The abdomen has been opened after cutting the nylon monofilamentar 3-0 (mononylon®) sutures, the small intestine was exposed again and the vascular clamp was identified and removed. The small intestine was repositioned. The reperfusion procedures were done and a new anesthesia allowed the collection of material for histological analysis. The animals were than sacrificed by exanguination of aorta section but still under effect of anesthesia.
Material collection for histological study
After the end of the tissue reperfusion the animals of all groups were anesthetized again to remove the sutures and to ressect the fragment of approximately 2 cm at ileum, 5 cm proximal to ileocecal transition, that was washed by saline solution plus 10% formalin and fixed in 10% formalin solution.
Histological procedures
The standard histological technique has been done and the sections were stained with hematoxylin-eosin (H&E). The sections were analyzed by the pathologist using a light microscope (Microscope Nikon E 600 de x100). The professional did not have previous knowledgement about the source of each section. The tissue lesions were analyzed according Chiu et al.20 criteria and received scores as following:
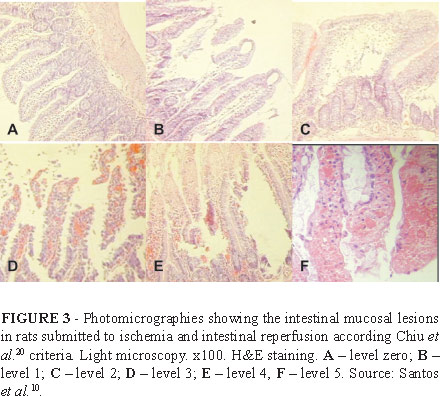
Chiu et al.20 criteria for histological analysis (Figure 3):
-
Level 0: mucosa without any histological alteration.
-
Level 1: intestinal villous well constituted, no cellular lysis, no inflammatory process but presence of subepitelial
Grunhagen space.
-
Level 2: presence of cellular lysis, presence of subepitelial
Grunhagen space, distance among intestinal villous have been increased.
-
Level 3: destruction of free portion of villous, dilated capillaries and presence of inflammatory cells.
-
Level 4: structural destruction of intestinal villous, presence of inflammatory cells and necrotic material, hemorrhagic areas and loosening of the tip superficial intestinal mucosa villous.
-
Level 5: destruction of the whole intestinal mucosa, no glandular structures were observed anymore and amorphous substance at submucosa region.
Histological statistical analysis.
The data were analyzed by the Software Excel 2010 and statistically analyzed by Software BioEstat 5.0 and GraphPad Prism 4.0.
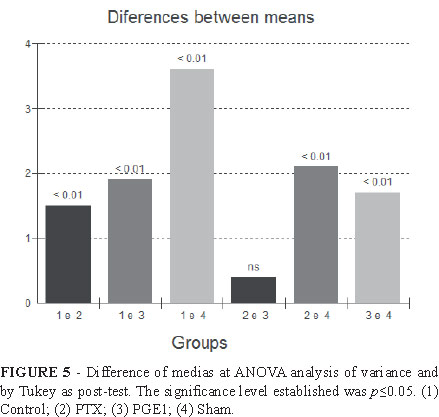
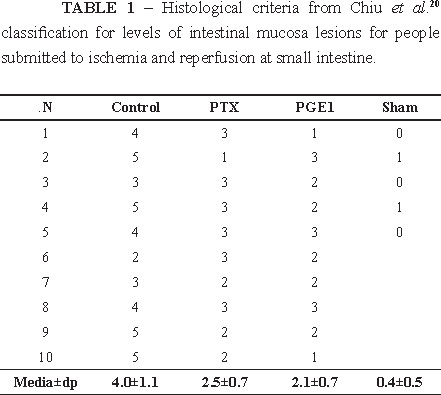
The tested hypothesis was about the differences of Chiu et al.20 classification for levels of intestinal mucosa lesions for people submitted to ischemia and small intestine reperfusion process for the control, PTX, PGE1 and Sham groups. The groups were compared by ANOVA and by Tukey as post-test. The significance level established was p<0.05.
Results
The values from above classification were statistically higher for control group (4.0±1.1) in comparison to PTX (2.5±0.7), PGE1 (2.1±0.7) and Sham group (0.4±0.5), p=0.0001. Between PTX and PGE1 groups no statistical difference was observed (p>0.05) according to the following Figures 4 and 5.
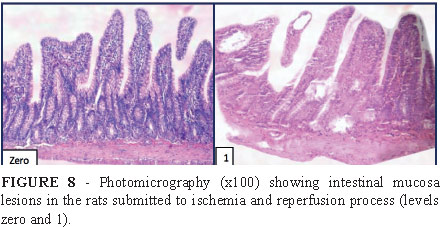
According to Table 1 it was possible to observe that without drugs PTX and PGE1 in the process of ischemia/reperfusion the media of control group were higher and the levels of lesions that predominated were 4 and 5 (Figure 6) according Chiu et al.20 criteria, indicating more severe tissue alterations. At groups PTX and PGE1 there was predominance of levels 2 and 3 (Figure 7) showing a less severe alterations during ischemia and reperfusion intestinal process (Figures 4 and 5). Sham group always showed level zero and 1, demonstrating that there was no effect from analgesy and laparotomy in those rats (Figure 8).
Discussion
After histological analysis according Chiu et al.20 it was demonstrated that without PTX1,13,14,16 and PGE117-20, in the control group, there was predominance of more severe lesions (levels 4 and 5) (Figure 8) showing villous structural destruction, presence of inflammatory cells, presence of necrotic material, hemorrhagic areas and an amorphous substance at submucosa region. However in the experimental groups, the drug utilization for reperfusion protected the intestinal mucosa and the levels of lesions that predominated were 2 and 3 de according (Chiu et al.20) criteria (Figure 7), indicating less severe lesions.
The histological features that predominated with the use of drug PTX were: presence of cellular lysis, formation of subepithelial Grunhagen space, and the villous were more separated from each other with some destruction at their tips, presence of dilated capillaries and inflammatory cells. Using PGE1 the histological results were similar. Those histological features in comparison to the ones observed at control group were less severe indicating that drugs probably protected the small intestinal mucosa and our results corroborate the data of many other authors in the literature1,13,14,16-19 that also used the same drugs, that really seems to reduce the tissue lesions in the process of ischemia and reperfusion at small intestine.
The PGE117-19, is known by its intense vasodilator effect, for being a substance with intense biological activity that has been used for such a longtime to treat. the chronic arterial occlusive disease, since beside to vasodilation capacity it also inhibit platelets aggregation. PGE1 has a role at fibrinolysis and/or fibrinogenesis, as well as in cellular proliferation and modulation, in the hemorreologic activity of erythrocytes, in the activation and inhibition of neutrophils and facilitating utilization of oxygen and glucose by the tissues. There is also strong evidence that PGE1 stimulate angiogenesis in cases of em myocardic ischemia17-19,.
A PTX1,13,14,16 has an antioxidant action directly inhibiting the anion superoxide that also indirectly block xanthine-oxidase enzyme activity. Therefore, it seems to decrease intensity of inflammatory response reducing neutrophils migration to the local area, decreasing liberation of cytokines, of tumoral necrosis factor, platelet activator factor and endothelin among other factors.
The histological and statistical results obtained in this study, showed that PTX or PGE1 could reduce the lesions of small intestine mucosa in rats submitted to ischemia/reperfusion process.
Conclusions
In the experimental groups with pentoxyflline or prostaglandin E1 it was observed the reduction of small intestine mucosal lesions in rats submitted to ischemia and tissue reperfusion procedures. The histological alterations were less severe in the groups which the drugs pentoxyflline or prostaglandin E1 were used during reperfusion in comparison to the control group, showing a positive effects of the drugs.
Received: July 11, 2013
Review: Sept 10, 2013
Accepted: Oct 14, 2013
Conflict of interest: none
Financial source: none
- 1. Brasileiro JL, Fagundes DJ, Miiji LON, Oshima CTF, Teruya R, Marks G, Inouye CM, Santos MA. Ischemia and reperfusion of the soleus muscle of rats with pentoxifylline. J Vasc Bras. 2007;61(1):50-63.
- 2. Santos CHM, Pontes, JCDV, Miiji LNO, Nakamura DI, Galhardo CAV, Aguena SM. Postconditioning effect in the hepatic ischemia and reperfusion in rats. Acta Cir Bras. 2010;25;(2):63-8.
- 3. Gomes OM, Brasileiro Filho G, Salles RLA, Linhares RE, Nazar MC, Porto LAB, Paixão RM, Miranda MH. Ischemia-reperfusion histopathology alterations of the rabbit intestinal wall with and without ischemic preconditioning. Acta Cir Bras. 2011;26(4):285-8.
- 4. Bertoletto PR, Chaves JC, Fagundes ATN, Simões RS, Oshima CTF, Simões MJ, Fagundes DJ. Effect of different periods of hyperbaric oxygen on ischemia-reperfusion injury of rat small bowel. Acta Cir Bras. 2008;23(1):23-6.
- 5. Bertoletto PR, IkejiriII AT, Somaio Neto F, Chaves JC, Teruya R, Bertoletto ER, Taha MO, Fagundes DJ. Oxidative stress gene expression profile in inbred mouse after ischemia/reperfusion small bowel injury. Acta Cir Bras. 2012;27(11):773-81.
- 6. Arena EA, Longo WE, Roberts KE, Geibel P, Nateqi J, Brandstetter M, Geibel JP. Functional role of NHE4 as a pH regulator in rat and human colonic crypts. Am J Physiol Cell Physiol. 2012;302(2):412-8.
- 7. Xue L, Aihara E, Wang T, Montrose MH. Trefoil Factor 2 Requires Na/H exchanger 2 activity to enhance mouse gastric epithelial repair. J Biol Chem. 2011;286(44):375-82.
- 8. Loganathan A, Linley JE, Rajput I, Hunter M, Lodge JPA, Sandle GI. Induced by chemical hypoxia basolateral potassium (IKCa) channel inhibition prevents increased colonic permeability. Am J Physiol Gastrointest Liver Physiol. 2011;300(1):146-53.
- 9. Francisco Neto A, Silva JCCB, Fagundes DJ, Percário S, Novos F, Juliano Y, Moreira Neto AA. Study of oxidative changes of total antioxidant capacity of nitric oxide in rats submitted to ischemia and reperfusion of hind limbs. Acta Cir Bras. 2005;20(2):134-9.
- 10. Santos CHM, Pontes JCDV, Gomes OM, Miiji LNO, BISPO MAF. Evaluation of ischemic postconditioning effect on mesenteric ischemia treatment: experimental study in rats. Rev Bras Cir Cardiovasc. 2009;24(2):150-6.
- 11. Serpa BS, Tachibana A, Baroni RH. Acute and chronic mesenteric ischemia: MDCT findings. J Vasc Bras. 2010;9(3):156-63.
- 12. Teruya R, Fagundes DJ, Oshima CTF, Brasileiro JL, Marks G, Inouye CM, Simões MJ. The effects of pentoxifylline into the kidneys of rats in a model of unilateral hind limb ischemia/reperfusion injury. Acta Cir Bras. 2008;23(1):29-35.
- 13. Leng YF, Zhang Y, Xue X, Wang T, Kang YQ. Ischemic post-conditioning attenuates the intestinal injury induced by limb ischemia/reperfusion in rats. Braz J Med Biol Res. 2011;44(5): 411-7.
- 14. MarquiI CE, SilvaII HCA, FereziII D, CavassaniI SS, Moraes JB, Silva DAM, Simões RS, Lopes CA, Taha MO, Oliveira-Júnior IS. Pretreatment with pentoxifylline attenuates lung injury induced by intestinal ischemia/reperfusion in rats. Acta Cir Bras. 2011;26(6):438-44.
- 15. Topcua I, Vatanseverb S, Varc A, Cavusb Z, Cilakera S, Sakarya M. The effect of Misoprostol, a prostaglandin E1 analog, on apoptosis in ischemia - reperfusion-induced intestinal injury. Acta Histochem. 2007;109:322-9.
- 16. Gao F, Horie T. A synthetic analog of prostaglandin E1 prevents the production of reactive oxygen species in the intestinal mucosa of methotrexate-treated rats. Life Sci. 2002;71:1091 - 9.
- 17. Kawamura T, Nara N, Kadosaki M, Inada K, Endo S. Prostaglandin E1 reduces myocardial reperfusion injury by inhibiting pro-inflammatory cytokines production during cardiac surgery. Crit Care Med. 2004;28(7):2201-8.
- 18. Moeser AJ, Nighot PK, Ryan KA, Wooten JG, Blikslager AT. Prostaglandin-mediated inhibition of Na+/H+ exchanger isoform 2 stimulates recovery of barrier function in ischemia-injured intestine. Am J Physiol Gastrointest Liver Physiol. 2006;291:885-94.
- 19. Moreschi Júnior D, Fagundes DJ, Amado LEB, Bersani LE, Hernandes L, Moreschi HK. Effects of prostaglandin E1 (PGE1) in the genesis of blood capillaries in ischemic skeletal muscle of rats: histological. J Vasc Bras. 2007;6(4):316-24.
- 20. Chiu CJ, McArdle AH, Brown R, Scott HJ, Gurd FN. Intestinal mucosal lesion in low-flow states. Arch Surg. 1970;101:478 - 83.
Publication Dates
-
Publication in this collection
05 Dec 2013 -
Date of issue
Nov 2013
History
-
Received
11 July 2013 -
Accepted
14 Oct 2013 -
Reviewed
10 Sept 2013