Abstract
PURPOSE: To determine the prevalence of non alcoholic fatty liver disease (NAFLD) and non alcoholic steatohepatitis (NASH) in morbidly obese patients undergoing bariatric surgery and to identify risk factors associated with the disease spectrum. METHODS: Liver biopsy was performed in 60 patients who underwent bariatric surgery, after other causes of liver disease were excluded. Clinical, biochemical and histological features were evaluated. RESULTS: NAFLD was detected in fifty-seven patients (95%) of the sample and forty patients (66.7%) of the total sample met the criteria for NASH. Perisinusoidal fibrosis was only found in three (7.5%) patients with NASH. The γGT was an independent predictive factor associated with the degree of hepatic steatosis. The variables such as dyslipidemia and ALT were independently associated with the presence of Mallory's corpuscles with the following values, respectively, OR 0, 05, 95% CI 0.002 to 0.75, P = 0.031 and OR 10, 99, 95% CI 1.44 to 83.93, P = 0.021. CONCLUSIONS: Non alcoholic fatty liver disease seems to be an obese-related condition with approximately half of asymptomatic morbidly obese patients having histological NASH. The γGT was an independent predictor of the degree of steatosis.
Fatty Liver; Obesity, Morbid; Bariatric Surgery
8 - ORIGINAL ARTICLE
CLINICAL INVESTIGATION
The spectrum of non alcoholic fatty liver disease in morbidly obese patients. Prevalence and associate risk factors1 1 Research performed at Nucleus of Obese, State of Ceara and Division of Clinical Gastroenterology, Department of Internal Medicine, Ceara Federal University (UFC), Brazil.
Suerda Guiomar FeijóI; José Milton de Castro LimaII; Maria Aparecida Alves de OliveiraIII; Régia Maria Vidal PatrocínioIV; Luis Gonzaga Moura-JuniorV; Antônio Borges CamposVI; José Wellington Oliveira LimaVII; Lúcia Libanez Bessa Campelo BragaVIII
IMD, MSc, Gastroenterologist, University Hospital Walter Cantideo, Ceara Federal University (UFC), Brazil. Conception of the study, acquisition and interpretation of data, manuscript writing
IIPhD, Associate Professor, Division of Clinical Gastroenterology, Department of Internal Medicine, UFC, Fortaleza-CE, Brazil. Acquisition of data, critical revision
IIIFellow PhD degree, Postgraduate Program in Surgery, UFC, Fortaleza-CE, Brazil. Acquisition and interpretation of data
IVMD, Department of Pathology and Legal Medicine, UFC, Fortaleza-CE, Brazil. Histological analysis, critical revision
VMD, MSc. Assistant Professor, Department of Surgery, Ceara State University, Brazil. Surgical procedures, acquisition of data
VIPhD, Associate Professor, Department of Surgery, UFC, Fortaleza-CE, Brazil. Surgical procedures, acquisition of data
VIIPhD, Department of Pathology and Legal Medicine, UFC, Fortaleza-CE, Brazil. Statistical analysis, interpretation of data
VIIIPhD, Full Professor, Department of Internal Medicine, UFC, Fortaleza-CE, Brazil. Conception and design of the study, manuscript writing, critical revision
Correspondence Correspondence: Prof. Dra Lucia L.B.C. Braga Departamento de Medicina Interna Instituto de Biomedicina - UFC Rua Nunes de Melo, 1315 60430-270 Porangabussu Fortaleza - CE Brasil Tel.: (55 85)3223-6982 Fax: (55 85)3281-5212 lucialib@terra.com.br
ABSTRACT
PURPOSE: To determine the prevalence of non alcoholic fatty liver disease (NAFLD) and non alcoholic steatohepatitis (NASH) in morbidly obese patients undergoing bariatric surgery and to identify risk factors associated with the disease spectrum.
METHODS: Liver biopsy was performed in 60 patients who underwent bariatric surgery, after other causes of liver disease were excluded. Clinical, biochemical and histological features were evaluated.
RESULTS: NAFLD was detected in fifty-seven patients (95%) of the sample and forty patients (66.7%) of the total sample met the criteria for NASH. Perisinusoidal fibrosis was only found in three (7.5%) patients with NASH. The γGT was an independent predictive factor associated with the degree of hepatic steatosis. The variables such as dyslipidemia and ALT were independently associated with the presence of Mallory's corpuscles with the following values, respectively, OR 0, 05, 95% CI 0.002 to 0.75, P = 0.031 and OR 10, 99, 95% CI 1.44 to 83.93, P = 0.021.
CONCLUSIONS: Non alcoholic fatty liver disease seems to be an obese-related condition with approximately half of asymptomatic morbidly obese patients having histological NASH. The γGT was an independent predictor of the degree of steatosis.
Key words: Fatty Liver. Obesity, Morbid. Bariatric Surgery.
Introduction
Non alcoholic fatty liver disease (NAFLD) is considered one of the most common liver diseases, affecting a wide spectrum of patients worldwide. The estimated prevalence in the general population is 10 to 24% and 70% in obese patients1,2. Given the obesity epidemic, it is thought to become one of the most important liver pathology in the future. Increased levels of insulin, triglycerides, low HDL, type 2 diabetes glucose intolerance are considered important risk factors.
Approximately 60% of patients with NAFLD have metabolic syndrome3. There is a wide spectrum of liver histology in NAFLD, ranging from steatosis to steatohepatitis (NASH), advanced fibrosis and cirrhosis4. NASH is characterized by zone 3 macrovesicular steatosis, inflammatory changes, fibrosis and may ultimately lead to cirrhosis and hepatocelular carcinoma in the absence of alcohol use. NASH histological findings resolve or remit in approximately 80% of patients after bariatric surgery5. Several studies have been conducted to evaluate the real prevalence of NASH and NAFLD in severely obese patients that underwent bariatric surgery, when liver biopsy was performed. The prevalence varied from 27 to 98%, which may be explained by recent modifications in histological classification6.
It is of great importance to predict and prevent the development of advanced liver diseases in obese patients. Determining the prevalence of NASH in those patients and further understanding the role of certain predictor factors is of interest, since it would aid in identifying patients at high risk. Furthermore, patients undergoing bariatric surgery would greatly benefit from strategies to allow detection of NASH and closer follow-up given they are at increased risk for the development of cirrhosis, hepatocellular and end-stage liver disease.
Therefore, the aim of this study was to prospectively determine the prevalence of NASH in obese patients undergoing bariatric surgery from Northeastern of Brazil and to identify risk factors involved in the development of NASH.
Methods
The study was approved by the Ethics Committee for Clinical Investigation at Ceara Federal University of Brazil. Informed written consent was obtained from every patient. Seventy eight patients from the Nucleus of Obese of state of Ceara scheduled to perform gastric bypass, after consultation with the surgeon, anesthetist and dietitians, were invited to participate in the study. Eighteen failed to meet the selection criteria. The study was composed of sixty consecutive patients with obesity class II or III, defined as a BMI> 35kg/m2 that were submitted to bariatric gastric bypass surgery type. Intraoperative fine-needle liver biopsy was performed in all patients using 16 gauge biopsy needle-22mm (Bard - Max Core).
Exclusion criteria included: daily alcohol consumption > 30 g in men or > 20 g in women7 at the time of evaluation or for a period longer than two years at any time, hepatitis B or C, previous history or laboratory evidence for a specific liver disease, had undergone extensive small bowel resection or jejuno-ileal or were on parenteral nutrition. Additionally, patients were excluded if on tamoxifen, amiodarone, corticosteroids, high doses of estrogen, methotrexate and cyclins in the last six months or for a prolonged period of time.
Serology for hepatitis C (anti HCV), hepatitis B (HBsAg, anti HBc IgM, anti HBc IgG, anti HBs), autoantibodies (antinuclear antibodies, anti smooth muscle and anti mitochondrial) was performed. Iron study (ferritin and tranferrin saturation index), serum levels of AST, ALT, γGT, alkaline phosphatase, total bilirubin and fractions, protein fractions, and prothrombin time, ceruloplasmin, uric acid and TSH were evaluated. Additionally, lipid profile (HDL, LDL, VLDL and triglycerides) and glycemic profile (fasting glucose, glycated hemoglobin A1c). An assessment of past and present alcohol consumption was done.
Patients were diagnosed with diabetes mellitus (DM) type 2 or impaired fasting glucose, according to previous classitication8, with hypertension when they had a resting blood pressure greater than or equal to 140/90 mmHg in two measurements. Patients were considered dyslipedemic based on the criteria of the Brazilian Society of Cardiology. The diagnosis of metabolic syndrome followed the criteria established by the International Diabetes Federation 2005 9. Alcohol consumption was classified into four categories: 0, no consumption or sporadic, 1, and 10 g / day; 2 between 10-20g/dia; 3 between 20-30g/dia.Waist circumference (WC) was considered at risk when greater than 102cm in men and> 88cm in women and waist-quandril (WHR) was assessed by measuring waist circumference divided by hip circumference10.
Histological evaluation
The material was fixed in paraffin and stained: H&E; periodic acid-Schiff after diastase (PAS-d), Perl's and Masson's trichrome, and examined by a single pathologist (RP), without prior knowledge of clinical and laboratory data of patients. All samples were deemed sufficient for the study by the pathologist. Patients were defined as having NAFLD when they had at least steatosis on biopsy, which was graded on a scale of 0 to 3 according to the criteria of Brunt et al.11. NASH diagnosis was defined as the presence of at least three of the four initial histological findings: 1) predominant macrovesicular steatosis in zone 3, 2) neutrophilic lobular inflammation 3), hepatocellular ballooning, 4) perisinusoidal fibrosis, according to the criteria of Brunt et al.11. The degree of steatosis was assessed on a scale of 0 to 3. Zero, indicating no: 1, mild (<33% of parenchyma involved) 2, moderate (33% to 66% of parenchyma involved), and 3, severe (> 66% of parenchyma involved). The degree of lobular inflammation was also graded on a scale of 0 to 3. Zero: no inflammation; 1: 1 to 2 inflammatory foci; 2: 2 to 4 inflammatory foci; 3: > 4 inflammatory foci. The stage classification required an assessment of the degree of perisinusoidal fibrosis / portal on a scale of 1 to 4. Stage 1, perisinusoidal fibrosis / pericellular in zone 3, focal or extensive; 2 fibrosis, perisinusoidal / pericellular in zone 3 and portal fibrosis, focal or extensive, 3, perisinusoidal fibrosis / pericellular fibrosis in zone 3 and portal w / fibrosis bridge, focal or extensive; 4, cirrhosis with or without perisinusoidal fibrosis. The presence of portal fibrosis in the absence of perisinusoidal fibrosis was not considered for the stage of NASH but was studied separately. Thus, histological variables described above, constitute the system of grade and stage of NASH: Grades on a scale of 1 to 3 and stage scale of 1 to 411.
Statistical analysis
Results are expressed as mean ± SD and percentages. Comparisons of quantitative variables were made using the Student's t-test. Categorical variables and proportions were tested by the qui square and Fisher exact test. Multivariate analysis was tested using logistic regression. A p-value <0.05 was considered as statistically significant All variables with a P value of 0.25 or less in univariate analyses were included in the full logistic regression model, according to recommendations of the Hosmer-Lameshow goodness-of-fit-test. Odds ratio (OR) and 95% confidence intervals (CI) were used as an estimated of the risk. Analysis was performed with SPSS computer software (version 11.5).
Results
Seventy-eight patients were invited to participate in the study, one was excluded for presenting positive marker for hepatitis C during the evaluation, four decided not to carry out with surgery, two had inadequate biopsy sample and eleven did not undergo biopsy for various technical reasons. A total of 60 patients, (73% female and 27% male) were considered for analysis.
Laboratory and demographic evaluation
Patients (mean age ± SD, 38.4 ± 11.6,) had a mean ± SD BMI of 44.2 kg/m2 ± 5.5, mean ± SD CC 125.8 ± 15.2 cm and mean ± SD of the sample WHR 0.93 ± 0.11. Thirty-four (56.6%) were hypertensive, twenty (33%) were type 2 diabetic or had changes in fasting glucose, thirty-one (51.7%) had altered lipid profile and thirty-nine (65%) fell within the metabolic syndrome. Thirty-eight (63.3%) were abstainers, and only one (1.67%) consumed between 20 - 30 g alcohol / day. The liver function tests together (AST, ALT, GGT, total bilirubin and fractions and alkaline phosphatase) were normal in twenty-seven patients (45%). γGT was raised in twenty-three (38.3%), ALT in twenty (33.3%), AST in eight (13.33%). The mean ratio of AST / ALT was 0.76 (range, 0.27 to 1.61), with the ratio AST / ALT> 1 detected in six (10%). Twenty-one (35%) had slightly elevated levels of ferritin and transferrin saturation index normal in all.
Histological data
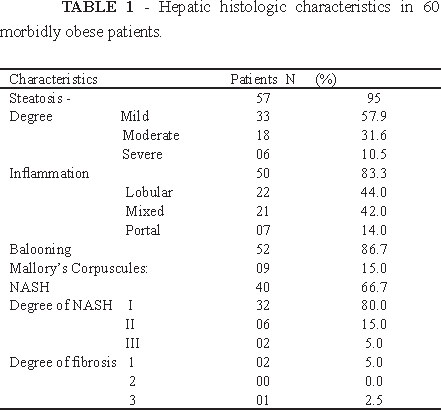
Liver biopsy results are summarized in Table 1. Fifty-seven patients (95%) had hepatic steatosis. Twenty-four (42.1%) had moderate to severe steatosis. Forty (66.6%) met all histologic criteria for NASH as described by Brunt et al.11
Factors associated with the degree of hepatic steatosis
Table 2 shows the association of demographic, anthropometric and laboratory variables with the degree of hepatic steatosis (I versus II and III degree of hepatic steatosis). γGT was the only variable significantly and independently associated with the degree of steatosis ( OR 0.04, 95% CI 0.003 to 0.63, P = 0.022)
Factors associated with histological features present in NAFLD
In univariable analysis Mallory corpuscles were significantly associated with type 2 diabetes (p = 0.036), dyslipidemia (p = 0.017), glucose (p = 0.008), HbA1c (p = 0.027), ALT (p = 0.004) and ferritin (p = 0.040). After subjecting these values to the logistic regression variables dyslipidemia and ALT were confirmed as factors independently associated with presence of Mallory's corpuscles with the following values, respectively, OR 0.05, 95% CI 0.002 to 0.75, P = 0.031 and OR 10.99, 95% CI 1.44 to 83.93, P = 0.021. Age was the only variable that was independently associated with the presence of ballooning, OR 0.89, 95% CI 0.79 to 0.99, P = 0.029.
Factors associated with NASH
In the univariable analysis, the factors that were significantly associated with NAFLD were: triglycerides (P = 0.029); group consisting of type 2 diabetes and those with impaired fasting glucose (P = 0.044), fasting glucose greater than 110mg/dL (p = 0.034), ALT changes (p = 0.044). The logistic regression analysis identified no factor independently associated with NASH.
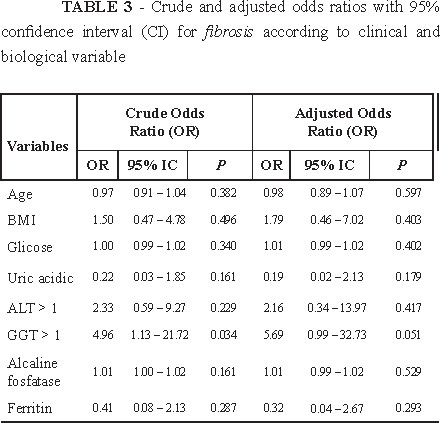
Factors associated with fibrosis
Zone 3 perisinusoidal fibrosis was detected in three cases (7.5%) while the isolated portal fibrosis was seen in seven (11.6%). Figure 1 The univariable analysis for factors associated with perisinusoidal fibrosis was compromised by the low prevalence of perisinusoidal fibrosis in the sample. However, taking into account that in morbid obesity, portal fibrosis alone has received attention12, all type of fibrosis (perisinusoidal, portal, perisinusoidal and portal) were analyzed as a group, and portal fibrosis also been analyzed separately. Only the elevation of γ GT showed a significant association with the first group (p = 0.035). After logistic regression analysis, γ GT did not remain as a significant independent factor. However, there was a trend towards significancy (OR 5.69, 95% CI 0.99 to 32.73, P = 0.051) Table 3.
Discussion
The present prospective study evaluated liver biopsies of patients that underwent bariatric surgery. The prevalence of NAFLD in the sample in this study was 95%, and among patients with NAFLD, twenty-four (42.1%) scored higher (Grade II and III).
The γGT was the only laboratory parameter that showed independent association with the degree of liver steatosis after logistic regression analysis. Interestingly. AST did not correlate with the degree of steatosis even in the univariate analysis and an AST / ALT ratio below 1 was found in 90% of cases. These findings suggest that increased levels of γ GT are not associated with alcohol consumption. Recent studies have demonstrated an association of GT levels with NAFLD. However, few studies have evaluated the frequency of such findings13. Additionally, increased levels of γ GT have been associated with oxidative stress14 and insulin resistance syndrome15. Our findings highlight the importance of monitoring γ GT levels in patients with NAFLD.
Among the histological findings in NAFLD, the presence of corpuscles Mallory was independently associated with dyslipidemia and ALT changes. Free fatty acids, acting at the intracellular level may result in the formation of corpuscles underlying Mallory16. The hepatocyte ballooning showed an independent association with age and a trend towards statistical significance with type 2 diabetes. The trend towards an independent association of type 2 diabetes with hepatocyte ballooning as well as and dyslipidemia and ALT in the presence of Mallory's corpuscles may support the idea of type 2 diabetes, dyslipidemia and ALT as factors associated with NAFLD. The ballooning of hepatocytes and presence of Mallory's corpuscles are now crucial for the framework of NASH in the spectrum of NAFLD13. It has been suggested that the mechanisms of pathogenesis of steatosis and ballooning are closely linked to insulin resistence, and their long-term evolution may be predicted by early improvement in insulin resistence17.
The prevalence of NASH in this study was 66.7%, similarly with what was reported from Belo Horizonte Southeastern of Brazil 57%18, lower than found in Ribeirao Preto also in Southeastern of Brazil 89%19 and in Greek 98%20, however it is higher than that reported from Dixon et al. 25% 5 and Beymer et al. 33%21 in the USA. In this study we did not find any significant association between NASH and gender unlike others studies that found higher prevalence of NASH in men22,23.
In the univariable analysis, diabetes mellitus and changes in fasting glucose were significantly associated with NASH, as well as laboratory variables ALT, triglyceride and glucose levels >110mg/dL. However, none of these variables remained significant after the adjusted analysis. The BMI, WHR and waist circumference did not show statistical significance as factors associated with NASH in our study, in accordance with several studies2,5.
We found a lower rate of fibrosis in this asymptomatic population (12%) than is commonly identified and no evidence of cirrhosis. One explanation may include referral bias in other published reports, but the exclusion criteria that applied to preexisting liver disease may also be related. Another possibility could be due to the fact that the mean age of the patient is lower than the one reported from the studies that found higher fibrosis rates since it has been reported that age could be a predictive factor for fibrosis in several studies2.
The role of isolated portal fibrosis, despite being reported in patients with NAFLD, has not been fully understood. Abrams et al.12 found isolated portal fibrosis in 30.3% of 195 liver biopsies in obese morbid patients and hyperglycemia. Our findings in the isolated portal fibrosis highlight the importance of this type of in the group of morbidly obese patients13. The two groups of fibrosis studied were not associated with any of the variables evaluated. It has been described a significant association between AST, ALT and γ GT elevation and NASH/fibrosis. However, high proportion of patients with NASH (and even severe NASH and hepatic cirrhosis) may present with normal serum concentrations of hepatic enzymes20.
Conclusions
Non alcoholic fatty liver disease seems to be an obese-related condition with approximately half of asymptomatic morbidly obese patients having histological NASH. The γGT was an independent predictor of the degree of steatosis.
Received: July 11, 2013
Review: Sept 10, 2013
Accepted: Oct 14, 2013
Conflict of interest: none
Financial source: none
- 1. Angulo P. GI epidemiology: nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2007;25:883-9.
- 2. Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40(3 Suppl 1):S5-10.
- 3. Blackburn GL, Mun EC. Effects of weight loss surgeries on liver disease. Semin Liver Dis. 2004;24(4):371-9.
- 4. Wang JT, Liu YL. Non-alcoholic fatty liver disease: the problems we are facing. Hepatobiliary Pancreat Dis Int. 2003;2(3):334-7.
- 5. Dixon JB, Bhatal PS, Obrien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in severely obese. Gastroenterology. 2001;121:91-100.
- 6. Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients under going bariatric surgery. J Hepatol. 2006;45(4):600-6.
- 7. Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR. Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPARγ ligand rosiglitazone. Hepatology. 2003;38:1008-17.
-
8. Report of the expert committee on the diagnosis and classification of diabetes mellitus.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003;26 Suppl 1:S5-20.
- 9. Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28(11):2745-9.
- 10. Cronk C, Roche AF. Race and soc-specific reference data for triceps and subcapsular skinfolds and weight/stature. Am J Clin Nutr. 1998;35:347-54.
- 11. Brunt EM, Janney CJ, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Non-alcoholic steatohepatitis: a proposal for grading and staging the histologic lesions. Am J Gastroenterol. 1999;94:2467-74.
- 12. Abrams GA, Kunde SS, Lazenby AJ, Clements RH. Portal fibrosis and hepatic steatosis in morbidly obese subjects: spectrum of nonalcoholic fatty liver disease. Hepatology. 2004;40:475-83.
- 13. Sanyal AJ. Aga: technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1705-25.
- 14. Lee DH, Ha MH, Kim JH, Christiani DC, Gross MD, Steffes M, Blomhoff R, Jacobs DR Jr. Gamma-glutamyltransferase and diabetes a 4 year follow-up study. Diabetologia. 2003;46:359-64.
- 15. Yokoyama H, Moriya S, Homma Y, Ogawa T. Association between gamma-glutamyl transpeptidase activity and status of disorders constituting insulin resistance syndrome. Alcohol Clin Exp Res. 2003;27:225-55.
- 16. Wanless IR, Bargman JM, Oreopoulus DG, Vas SI. Subcapsular steatonecrosis in response to peritoneal insuline delivery: a clue to the pathogenesis of steatonecrosis in obesity. Mod Pathol. 1989;2:69-74.
- 17. Mathurin P, Hollebecque A, Arnalsteen L, Buob D, Leteurtre E, Caiazzo R, Pigeyre M, Verkindt H, Dharancy S, Louvet A, Romon M, Pattou F. Prospective study of the long-term effects of bariatric surgery on liver injury in patients without advanced disease. Gastroenterology. 2009;137(2):532-40.
- 18. Lima ML, Mourão SC, Diniz MT, Leite VH. Hepatic histopathology of patients with morbid obesity submitted to gastric bypass. Obes Surg. 2005;15(5):661-9.
- 19. Júnior WS, Nonino-Borges CB. Clinical predictors of different grades of nonalcoholic fatty liver disease. Obes Surg. 2012;22(2):248-52.
- 20. Stratopoulos C, Papakonstantinou A, Terzis I, Spiliadi C, Dimitriades G, Komesidou V, Kitsanta P, Argyrakos T, Hadjiyannakis E. Changes in liver histology accompanying massive weight loss after gastroplasty for morbid obesity. Obes Surg. 2005;15(8):1154-60.
- 21. Beymer C, Kowdley KV, Larson A, Edmonson P, Dellinger EP, Flum DR. Prevalence and predictors of asymptomatic liver disease in patients undergoing gastric bypass surgery. Arch Surg. 2003;138:1240-44.
- 22. Zelber-Sagi S, Nitzan-Kaluski D, Halpern Z, Oren R. Prevalence of primary non-alcoholic fatty liver disease in a population-based study and its association with biochemical and anthropometric measures. Liver Int. 2006;26:856 - 63.
- 23. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387-95.
- 24. Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, Sterling RK, Shiffman ML, Stravitz RT, Sanyal AJ. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-92.
Publication Dates
-
Publication in this collection
05 Dec 2013 -
Date of issue
Nov 2013
History
-
Received
11 July 2013 -
Accepted
14 Oct 2013 -
Reviewed
10 Sept 2013