Abstract
PURPOSE: To assess venous hemodynamics and quality of life at lest five years after varicose vein stripping. METHODS: We conducted a prospective study with 39 patients (63 limbs) with primary lower limbs varicose veins. Preoperatively, all patients were subjected to clinical evaluation, duplex ultrassound, air plethysmography (APG), and CIVIQ questionnaire of quality of life. By APG, venous filling index (VFI), ejection fraction (EF), and residual volume fraction (RVF) were determined. CIVIQ addresses four domains in course of 20 questions, including states of physical, social, and psychological well-being, and pain level. Varicose veins were treated by standard venous stripping. At least five years after surgery (77.9 ± 10.9 months), patients were reassessed and had clinical examination, duplex ultrasound, APG, and CIVIQ repeated. No late follow-up data was available for 24 patients. RESULTS: Preoperative and late postoperative VFI levels were similar, whereas EF (P=0.05) and RVF (P=0.01), as hemodynamic variables, significantly improved following surgery. In the late postoperative period, overall CIVIQ scores were significantly lower (P=0.005), as were scores in all four domains: pain (P=0.001), physical (P=0.007), social (P=0.008), and psychological (P= 0.05). CONCLUSION: In a small prospective cohort, improvements in venous hemodynamics and in quality of life of patients submitted to standard varicose veins stripping were maintained five years after the procedure.
Varicose Veins; Stripping; Plethysmography; Quality of Life; Surgery
9 - ORIGINAL ARTICLE
CLINICAL INVESTIGATION
A prospective study of venous hemodynamics and quality of live at least five years after varicose vein stripping1 1 Research performed at Division of Vascular and Endovascular Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo (USP), Brazil.
Rogerio Takeyoshi UemaI; Nei Rodrigues Alves DezottiII; Edwaldo Edner JovilianoIII; Marcelo Bellini DalioII; Takachi MoriyaIII; Carlos Eli PiccinatoIV
IPhD, Vascular Surgeon, Division of Vascular and Endovascular Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo (USP), Brazil. Conception and design of the study; acquisition, analysis and interpretation of data; manuscript writing
IIPhD, Assistant Physician, Division of Vascular and Endovascular Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Brazil. Intellectual and scientific content of the study, manuscript writing, critical revision, final approval of the version to be published
IIIPhD, Associate Professor, Division of Vascular and Endovascular Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Brazil. Manuscript writing, critical revision
IVPhD, Chairman and Head, Division of Vascular and Endovascular Surgery, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirao Preto, USP, Brazil. CNPq reseacher. Conception and design of the study, critical revision
Correspondence Correspondence: Carlos Eli Piccinato Faculdade de Medicina de Ribeirão Preto, Campus Universitário 14049-900 Ribeirão Preto - SP Brasil Tel/Fax: (55 16)3965-2055/9119-0649 cepiccin@fmrp.usp.br
ABSTRACT
PURPOSE: To assess venous hemodynamics and quality of life at lest five years after varicose vein stripping.
METHODS: We conducted a prospective study with 39 patients (63 limbs) with primary lower limbs varicose veins. Preoperatively, all patients were subjected to clinical evaluation, duplex ultrassound, air plethysmography (APG), and CIVIQ questionnaire of quality of life. By APG, venous filling index (VFI), ejection fraction (EF), and residual volume fraction (RVF) were determined. CIVIQ addresses four domains in course of 20 questions, including states of physical, social, and psychological well-being, and pain level. Varicose veins were treated by standard venous stripping. At least five years after surgery (77.9 ± 10.9 months), patients were reassessed and had clinical examination, duplex ultrasound, APG, and CIVIQ repeated. No late follow-up data was available for 24 patients.
RESULTS: Preoperative and late postoperative VFI levels were similar, whereas EF (P=0.05) and RVF (P=0.01), as hemodynamic variables, significantly improved following surgery. In the late postoperative period, overall CIVIQ scores were significantly lower (P=0.005), as were scores in all four domains: pain (P=0.001), physical (P=0.007), social (P=0.008), and psychological (P= 0.05).
CONCLUSION: In a small prospective cohort, improvements in venous hemodynamics and in quality of life of patients submitted to standard varicose veins stripping were maintained five years after the procedure.
Key words: Varicose Veins. Stripping. Plethysmography. Quality of Life. Surgery.
Introduction
Varicose veins (VV) are a disabilitying condition, representing a critical public health problem with economic and social consequences1-4. Prevalence is high, being about 20% to 73% in females and 15% to 56% in males5-6. Elastic compression stockings are the initial treatment. Venoactive drugs can bring some relief in symptoms. Surgical stripping or endovascular ablation are typically the treatments of choice.
Once untreated, VV usually affect many aspects of daily living, harming quality of life (QOL). QOL may be defined as the patient's overall perception of his/her disease, including its functional ramifications and responses to related therapy. Launois et al.7 are credited with elaboration and validation of the Chronic Lower Limb Venous Insufficiency Questionnaire (CIVIQ), used to assess disease-specific QOL in the setting of venous disease.
Knowledge of treatment outcomes in VV is mandatory for determining the most effective therapy. Accordingly, this study was designed to assess venous hemodynamics and late QOL at least five years after varicose vein stripping.
Methods
The study was approved by the Institutional Ethics Committee and also each patient signed an informed consent (n. 13353/2008). We followed patients form a previous study at Division of Vascular and Endovascular Surgery of the University Hospital of the Faculty of Medicine of Ribeirão Preto, University of Sao Paulo17.
We selected 39 patients (63 lower limbs) with primary lower limbs VV with CEAP clinical classification8 ranging from C2 to C6 complaining of pain, discomfort and edema. Patients with prior varicose vein surgery; deep venous reflux and obstruction, confirmed by duplex ultrasound; congenital malformations; diabetes mellitus; heart disease; arterial and lymphatic vasculopathies; collagenoses; myopathies; osteopathies; arthropathies (alone or as comorbidity); and other lower limb surgeries during the study period were all excluded.
Preoperative evaluation
All patients were subjected to standard clinical examination. Duplex ultrasound was performed to rule out deep venous reflux and obstruction9, and also to diagnose superficial venous reflux (great saphenous vein, small saphenous vein or perforator insufficiency). Examinations were performed by the same independent examiner, and all results were communicated to the senior investigator. Venous hemodynamics was assessed by air plethysmography (APG). APG was performed in the Laboratory of Noninvasive Vascular Investigation during evening hours. Testing began after a procedural demonstration, assuring complete patient understanding of the process. The functionality of calf muscular pump was studied by APG, using an SDV 3000 Angiotec® device (Belo Horizonte, Brazil) with computer automated calibration. The technique described and standardized by Christopoulos et al.10 was applied to evaluate venous filling index (VFI), ejection fraction (EF), and residual volume fraction (RVF).
Disease-specific QOL was assessed by the CIVIQ questionnaire. The CIVIQ was designed expressly for evaluating QOL in patients with venous disease. This 20-question inquiry is aimed at four key areas, including states of social (three questions), physical (four questions), and psychological (nine questions) well-being and pain level (four questions). As such, it is marked by strong internal consistency and reproducibility, as well as high response capacity and longitudinal clinical validity7.
All preoperative data was defined with the prefix Pre.
Varicose veins stripping
Patients were submitted to surgical stripping in order to eliminate the VV and eliminate the superficial venous reflux. The choice of each procedure was based on findings of clinical examination and of duplex ultrasound. Ankle-to-groin great saphenous vein stripping and simultaneous phlebectomy were performed in 55 lower limbs. The same procedure with simultaneous perforating veins ligation was performed in the eight remaining. As no small saphenous vein reflux was diagnosed, no small saphenous vein stripping was performed. The same surgeon (TM) performed all operations from January 2001 to December 2004.
Follow-up
Postoperatively, every patient was closely followed until one year after surgery. No complications such as hematoma, wound problems, infection or nerve injuries were observed. At least five years after the procedure, patients were contacted by telephone and were asked to return to the hospital for reassessment of clinical examination, duplex ultrasound, APG, and CIVIQ. No late follow-up data was available for 24 patients. We attempted contact by telephone and mail with these patients, with no success. Postoperative data was defined with the prefix Post.
Statistical analysis
For comparing preoperative and postoperative data (APG and CIVIQ), the nonparametric two-tailed Wilcoxon test was utilized. Statistical evaluations were performed using the program Graph Pad Prism 4.0 (Graph Pad Software Inc., San Diego, CA, USA). Data was considered to be statistically significant at P values less than .05.
Results
From the 39 initial patients, 15 (22 lower limbs) were evaluated in the late postoperative period. Median age was 56 years (25 to 68 years). These patients were submitted to ankle-to-groin great saphenous vein stripping and phlebectomy (18 limbs) and the same procedure with simultaneous perforating veins ligation (four limbs). Mean follow-up was 77.9 ± 10.9 months.
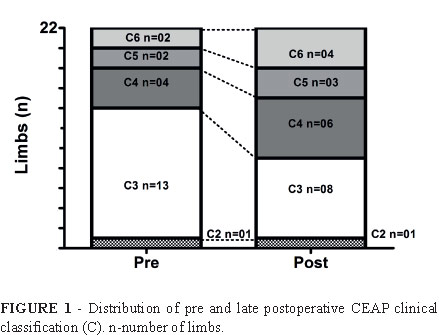
Figure 1 describes the distribution of pre and late postoperative CEAP clinical classification (C). In the long-term, clinical classification was unchanged for 59.1% (13/22 limbs), whereas 40.9% (9/22 limbs) worsened relative to preoperative CEAP status.
Late postoperative duplex ultrasound detected reflux in superficial (6/22 limbs; 27.3%) and deep (3/22 limbs; 13.6%) venous systems, as well as in perforators (4/22 limbs; 18.2%).
Regarding venous hemodynamics, VFI remained stable throughout the duration of study, showing no change from baseline to late postoperative values. On the other hand, there was a significant increase in Post EF and a fall in Post RVF, when compared with preoperative levels, representing improved venous hemodynamics in the late postoperative period (Table 1).
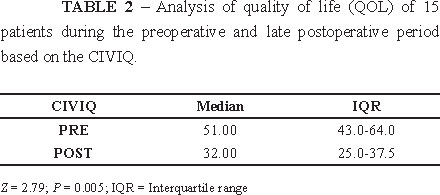
Analysis of overall CIVIQ answers indicated improved QOL in 66.7% (10/15 patients), no change in 26.7% (4/15 patients), and worsening in 6.6% (1/15 patients). These scores declined significantly in the late postoperative period, signaling enhanced QOL after surgical intervention for VV (Table 2). All four domains of the CIVIQ (pain, physical, social, and psychological) scored significantly better in late postoperative period, compared with preoperative assessments (Table 3).
The 24 patients (41 limbs) which were unavailable for late follow-up had median age of 48.5 years (40-64 years). They presented the following CEAP preoperative clinical values: C-2 (n=1); C-3 (n=12); C-4 (n=7); C-5 (n=3); and C-6 (n=1).
Discussion
This study was designed as a prospective evaluation of long-term patient outcomes following VV stripping. Both hemodynamic and QOL parameters were assessed before surgery and in the late postoperative period. Repeated attempts to quantify venous reflux based on APG have established that the results do correlate well with clinical stages of venous disease. This approach is also useful for monitoring patient status following various surgical procedures10-17. Although improved venous hemodynamics have been reported in most immediate postoperative periods10,11,16-19, few sources have documented long-term results.
Dezzotti et al.17 using APG to study changes in venous hemodynamics 30-45 days after surgery for lower limb VV, found postoperative improvement by virtue of a reduction in VFI and RVF and an increase of EF (39 patients). A decline in VFI was observed in our 39 patient 30-45 days after surgery, but the degree of change did not persist long-term (five years) after surgery in the 15 patients who completed the study. This suggests that the postsurgical VFI reverts as the disease evolves, thus explaining a worsening in clinical CEAP classification in 40.9% (9/22) of limbs. An alternate possibility is that the clinical evolution of venous disease results from local or microcirculatory factors and not from the hemodynamics of major veins20-22.
QOL analysis reflects patient perceptions of life in a number of ways, and is not merely an index of overall health23. Hence, QOL is considered a critical determinant of treatment success24, particularly in terms of disease progression. In chronic conditions such as venous disease, QOL assessments provide insight into patient complaints, which may not readily translate through traditional methods of morbidity and mortality determinations25. However, it is still unclear whether or not CEAP status, focused largely on physical changes, reflects the patient's self-perception of disease severity. Few studies have investigated this aspect26.
Kakkos et al.27 studied 45 patients (48 legs) undergoing superficial venous surgery for primary varicose veins. Venous ultrasound, clinical examination, and a QOL questionnaire were used preoperatively and at six weeks and six months postoperatively. Severity of venous symptoms was subsequently correlated with CEAP class and CEAP score (scores of disease severity standardized by means of CEAP status). The authors found that scores derived from venous symptoms rose significantly in advanced CVD, correlating with the extent of anatomic involvement. Thus, they viewed scores of clinical severity and CEAP scores as more sensitive indices of responses to surgical treatment in this setting, as opposed to CEAP classification alone.
Blomgren et al.28 assessed the impact of preoperative duplex mapping on the QOL (via SF-36 questionnaire) of patients after surgery for lower limb varicosities. Despite improving the surgical result by reducing residual veins and recurrences, at no time did the exam impact patient QOL. The follow-up period was two years and the initial patient sampling of 293 was reduced to 237 (81%) by end of study.
In an international cohort study, Kahn et al.26 evaluated 1531 patients, attempting to correlate CEAP status with severity of venous symptoms. The patients were distributed proportionately by ascending CEAP class as follows: 3.8%, 13.3%, 24.1%, 12.8%, 36.4%, 7.3% and 2.3%. Ultimately, declining QOL scores corresponded with increasing CEAP class, indicating that clinical status, based on the CEAP clinical classification, is predictive of QOL and the severity of venous disease. The generally impaired QOL of patients with chronic venous insufficiency has been further confirmed in the literature by comparative studies with other chronic disease such as rheumatoid arthritis, lumbar pain, menorrhagia, and suspected peptic ulcer29.
Much of the difficulty we encountered was in maintaining patient participation. The extended period (at least 5 years) of monitoring after surgery culminated in immense loss of follow-up. Only 38.4% of the initial patients were available for late follow-up assessment. Patients who lost follow-up were similar to those who completed the study, regarding median age and CEAP clinical classification. Baker et al.30 also faced this problem when comparing postoperative QOL (at 30 days and six months) and baseline status of treated lower limb VV using the SF-36 questionnaire. Only 59% of patients responded to the questionnaire within this brief evaluation period. Smith et al.25 managed an 80% follow-up rate within 6 months after treatment, losing 20% of patients in follow-up due to changes in address or telephone number.
In our study, overall CIVIQ scores improved significantly in the postoperative period compared with preoperative scores. Statistical analysis revealed improvement in 66.7% of the sampling, no change in 26.7%, and worsening in only 6.6%. Similar gains were noted for all four CIVIQ domains (pain, physical, social and psychological), underscoring the long-term benefits of surgical intervention in lower limb VV.
The strength of this study was limited by the number of patients enrolled, coupled with socioeconomic restrictions. Among the 39 patients agreeing to participate initially, only 15 patients completed the study, conducted during a period of at least 5 years. A lack of a non-surgical control group was also a limitation.
Conclusion
In a small prospective cohort, improvements in venous hemodynamics and in quality of life of patients submitted to standard varicose veins stripping were maintained five years after the procedure.
Received: July 24, 2013
Review: Sept 23, 2013
Accepted: Oct 22, 2013
Conflict of interest: none
Financial sources: Teaching, Research and Assistance Foundation, Clinics Hospital, Ribeirao Preto Faculty of Medicine, Sao Paulo University-USP(FAEPA-HC/FMRP-USPNational) and Council of Technological and Scientific Development (CNPq).
- 1. De Backer G. Epidemiology of chronic venous insufficiency. Angiology. 1997;48(7):569-76.
- 2. Carpentier P, Priollet P. Epidemiology of chronic venous insufficiency. Presse Med. 1994;23(5):197-201.
- 3. Fowkes FG, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology. 2001;52 Suppl 1:S5-15.
- 4. Cesarone MR, Belcaro G, Nicolaides AN, Geroulakos G, Griffin M, Incandela L, De SM, Sabetai M, Agus G, Bavera P, Ippolito E, Leng G, Di RA, Cazaubon M, Vasdekis S, Christopoulos D, Veller M. 'Real' epidemiology of varicose veins and chronic venous diseases: the San Valentino Vascular Screening Project. Angiology. 2002;53(2):119-30.
- 5. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175-84.
- 6. Maffei FH, Magaldi C, Pinho SZ, Lastoria S, Pinho W, Yoshida WB, Rollo HA. Varicose veins and chronic venous insufficiency in Brazil: prevalence among 1755 inhabitants of a country town. Int J Epidemiol. 1986;15(2):210-7.
- 7. Launois R, Reboul-Marty J, Henry B. Construction and validation of a quality of life questionnaire in chronic lower limb venous insufficiency (CIVIQ). Qual Life Res. 1996;5(6):539-54.
- 8. Eklof B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, Meissner MH, Moneta GL, Myers K, Padberg FT, Perrin M, Ruckley CV, Smith PC, Wakefield TW, American Venous Forum International Ad Hoc Committee for Revision of the CC. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(6):1248-52.
- 9. Coleridge-Smith P, Labropoulos N, Partsch H, Myers K, Nicolaides A, Cavezzi A. Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs--UIP consensus document. Part I. Basic principles. Eur J Vasc Endovasc Surg. 2006;31(1):83-92.
- 10. Christopoulos D, Nicolaides AN, Galloway JM, Wilkinson A. Objective noninvasive evaluation of venous surgical results. J Vasc Surg. 1988;8(6):683-7.
- 11. Gillespie DL, Cordts PR, Hartono C, Woodson J, Obi-Tabot E, LaMorte WW, Menzoian JO. The role of air plethysmography in monitoring results of venous surgery. J Vasc Surg. 1992;16(5):674-8.
- 12. Jiang P, van Rij AM, Christie RA, Hill GB, Thomson IA. Venous physiology in the different patterns of recurrent varicose veins and the relationship to clinical severity. Cardiovasc Surg. 2000;8(2):130-6.
- 13. Owens LV, Farber MA, Young ML, Carlin RE, Criado-Pallares E, Passman MA, Keagy BA, Marston WA. The value of air plethysmography in predicting clinical outcome after surgical treatment of chronic venous insufficiency. J Vasc Surg. 2000;32(5):961-8.
- 14. Nishibe T, Nishibe M, Kudo F, Flores J, Miyazaki K, Yasuda K. Stripping operation with preservation of the calf saphenous veins for primary varicose veins: hemodynamic evaluation. Cardiovasc Surg. 2003;11(5):341-5.
- 15. van Rij AM, Jiang P, Solomon C, Christie RA, Hill GB. Recurrence after varicose vein surgery: a prospective long-term clinical study with duplex ultrasound scanning and air plethysmography. J Vasc Surg. 2003;38(5):935-43.
- 16. Kim IH, Joh JH, Kim DI. Venous hemodynamic changes in the surgical treatment of primary varicose vein of the lower limbs. Yonsei Med J. 2004;45(4):577-83.
- 17. Dezotti NRA, Joviliano EE, Toma MK, Moriya T, Piccinato CE. Venous hemodynamic study by air plethysmography in the pre and postoperative period of lower limb varicose veins. J Vasc Bras. 2009;8(1):21-8.
- 18. Sakuda H, Nakaema M, Matsubara S, Higa N, Kamada Y, Kuniyoshi Y, Koja K. Air plethysmographic assessment of external valvuloplasty in patients with valvular incompetence of the saphenous and deep veins. J Vasc Surg. 2002;36(5):922-7.
- 19. Park UJ, Yun WS, Lee KB, Rho YN, Kim YW, Joh JH, Kim DI. Analysis of the postoperative hemodynamic changes in varicose vein surgery using air plethysmography. J Vasc Surg. 2010;51(3):634-8.
- 20. van Bemmelen PS, Mattos MA, Hodgson KJ, Barkmeier LD, Ramsey DE, Faught WE, Sumner DS. Does air plethysmography correlate with duplex scanning in patients with chronic venous insufficiency? J Vasc Surg. 1993;18(5):796-807.
- 21. Iafrati MD, Welch H, O'Donnell TF, Belkin M, Umphrey S, McLaughlin R. Correlation of venous noninvasive tests with the Society for Vascular Surgery/International Society for Cardiovascular Surgery clinical classification of chronic venous insufficiency. J Vasc Surg. 1994;19(6):1001-7.
- 22. Labropoulos N, Delis K, Nicolaides AN, Leon M, Ramaswami G. The role of the distribution and anatomic extent of reflux in the development of signs and symptoms in chronic venous insufficiency. J Vasc Surg. 1996;23(3):504-10.
- 23. van Korlaar I, Vossen C, Rosendaal F, Cameron L, Bovill E, Kaptein A. Quality of life in venous disease. Thromb Haemost. 2003 Jul;90(1):27-35.
- 24. Rass K, Frings N, Glowacki P, Hamsch C, Graber S, Vogt T, Tilgen W. Comparable effectiveness of endovenous laser ablation and high ligation with stripping of the great saphenous vein: two-year results of a randomized clinical trial (RELACS study). Arch Dermatol. 2012;148(1):49-58.
- 25. Smith JJ, Guest MG, Greenhalgh RM, Davies AH. Measuring the quality of life in patients with venous ulcers. J Vasc Surg. 2000;31(4):642-9.
- 26. Kahn SR, M'Lan C E, Lamping DL, Kurz X, Berard A, Abenhaim LA, Group VS. Relationship between clinical classification of chronic venous disease and patient-reported quality of life: results from an international cohort study. J Vasc Surg. 2004;39(4):823-8.
- 27. Kakkos SK, Rivera MA, Matsagas MI, Lazarides MK, Robless P, Belcaro G, Geroulakos G. Validation of the new venous severity scoring system in varicose vein surgery. J Vasc Surg. 2003;38(2):224-8.
- 28. Blomgren L, Johansson G, Bergqvist D. Quality of life after surgery for varicose veins and the impact of preoperative duplex: results based on a randomized trial. Ann Vasc Surg. 2006;20(1):30-4.
- 29. Garratt AM, Macdonald LM, Ruta DA, Russell IT, Buckingham JK, Krukowski ZH. Towards measurement of outcome for patients with varicose veins. Qual Health Care. 1993;2(1):5-10.
- 30. Baker DM, Turnbull NB, Pearson JC, Makin GS. How successful is varicose vein surgery? A patient outcome study following varicose vein surgery using the SF-36 Health Assessment Questionnaire. Eur J Vasc Endovasc Surg. 1995;9(3):299-304.
Publication Dates
-
Publication in this collection
05 Dec 2013 -
Date of issue
Nov 2013
History
-
Received
24 July 2013 -
Accepted
22 Oct 2013 -
Reviewed
23 Sept 2013