Abstracts
PURPOSE: To analyze the effects of hyperbaric oxygen therapy on liver function in rats previously subjected to ischemia and reperfusion. METHODS: A randomly distribution of 23 Wistar rats was conducted into three groups: SHAM, animals subjected to surgical stress without restricting blood flow by clamping the hepatic pedicle, IR, rats underwent hepatic vascular occlusion intermittently for two complete cycles of 15 minutes of ischemia followed by 5 min of reperfusion, IR / HBO, rats underwent hepatic pedicle clamping and thereafter exposed to hyperbaric oxygen pressure of 2 absolute atmospheres for 60 minutes. We evaluated liver function through mitochondrial function, determined by the stages 3 and 4 of respiration, respiratory control ratio (RCR) and mitochondrial permeability transition (Swelling). Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were also quantified . We analyzed the results using the Mann-Whitney test and were considered significant all results with p <0.05. RESULTS: There were significant differences between the results of stage 3 in SHAM vs IR group ; of the stage 4 in the groups IR vs SHAM and SHAM vs IR /HBO; of the Respiratory Control Ratio (RCR) in the group IR vs IR / HBO ; of alanine aminotransferase in the groups IR vs SHAM , SHAM vs IR/HBO and IR vs IR / HBO; aspartate aminotransferase in the groups SHAM vs IR and SHAM vs IR / HBO. CONCLUSION: The whole analysis of the mitochondiral function indicators permits us to conclude that the hyperbaric oxygen therapy acted as a protective agent of the mitochondrial function, minimizing the ischemia-reperfusion injury of the hepatic parenchyma.
Hyperbaric Oxygen Therapy; Mitochondria; Liver Ischemia; Reperfusion
OBJETIVO: Analisar os efeitos da oxigenoterapia hiperbárica sobre a função hepática de ratos previamente submetidos à isquemia e reperfusão. MÉTODOS: Realizou-se a distribuição aleatória de 23 ratos Wistar em três grupos: SHAM, animais submetidos ao estresse cirúrgico sem restrição de fluxo sanguíneo por clampeamento do pedículo hepático; IR ratos submetidos a oclusão vascular hepática de maneira intermitente em dois ciclos completos de 15 minutos de isquemia, seguidos por 5 min de reperfusão; IR/HBO, ratos submetidos ao clampeamento do pedículo hepático e ,ulteriormente , expostos a oxigenoterapia hiperbárica a pressão de 2 atmosferas absolutas durante 60 minutos. Avaliou-se a função hepática através da função mitocondrial, determinada pelos estados 3 e 4 da respiração mitocondrial, razão de controle respiratório(RCR) e transição de permeabilidade mitocondrial (Swelling) .Quantificou-se também alanina aminotransferase e aspartato aminotransferase séricas. Analisou-se os resultados pelo teste de Mann-Whitney e foram considerados significativos os valores de p < 0,05. RESULTADOS:Houve diferença significativa nos valores do estado 3 no grupo SHAM vs IR; estado 4 nos grupos SHAM vs IR, SHAM vsIR/HBO; Razão de Controle Respiratório(RCR) no grupo IR vs IR/HBO; alanina aminotransferase nos grupos SHAM vs IR, SHAM vs IR/HBO, IR vs IR/HBO; aspartato aminotransferase nos grupos SHAM vs IR , SHAM vs IR/HBO. CONCLUSÃO: A análise dos parâmetros mitocondriais como um todo permitiu concluir que a oxigenoterapia hiperbárica atuou como agente protetor da função mitocondrial, minimizando os efeitos deletérios da lesão de isquemia e reperfusão do parênquima hepático.
Oxigenoterapia Hiperbárica; Mitocôndria; Fígado; Isquemia; Reperfusão
11 - ORIGINAL ARTICLE
ISCHEMIA-REPERFUSION
Effect of hyperbaric oxygen therapy on liver function during intermittent ischemia1 1 Research performed at Special Liver Transplant Unit, Department of Surgery and Anatomy, Medicine Faculty of Ribeirão Preto, University of São Paulo, Brazil.
Efeito da oxigenoterapia hiperbárica sobre a função hepática na isquemia intermitente
Leticia Botigeli BaldimI; Ricardo Nejo JrII; Maria Eliza Jordani SouzaIII; Maria Cecília Jordani GomesIII; Maria Aparecida Neves Cardoso PicinatoIII; Clarice Fleury FinaIII; Orlando Castro-e-SilvaIV
IGraduate Student of the Medicine School of Universidade Federal de São Carlos, São Carlos, SP, Brazil. Main author. Conception. Designed the protocol; Involved with technical procedures; Responsible for English language
IIGraduate Student of the medicine school at Universidade Santo Amaro, São Paulo - SP, Brazil. Involved with technical procedures
IIIMaster, Biochemistry of Division of Digestive Surgery, Department of Surgery and Anatomy of FMRPUSP, Ribeirao Preto - SP, Brazil. Involved with technical procedures
IVChairman and Head of the Department of Surgery and Anatomy of FMRP-USP, Ribeirao Preto - SP, Brazil. Conception. Responsible for intellectual and scientific content of the study; Designed the protocol; Critical Review
Correspondence Correspondence: Orlando de Castro e Silva Departamento de Cirurgia e Anatomia Av. Bandeirantes, 3900/ 9º andar 14048-900 Ribeirão Preto - SP Brasil Tel.: (55 16)3602-2242 Fax: (55 16)3602-2866 orlando@fmrp.usp.br
ABSTRACT
PURPOSE: To analyze the effects of hyperbaric oxygen therapy on liver function in rats previously subjected to ischemia and reperfusion.
METHODS: A randomly distribution of 23 Wistar rats was conducted into three groups: SHAM, animals subjected to surgical stress without restricting blood flow by clamping the hepatic pedicle, IR, rats underwent hepatic vascular occlusion intermittently for two complete cycles of 15 minutes of ischemia followed by 5 min of reperfusion, IR / HBO, rats underwent hepatic pedicle clamping and thereafter exposed to hyperbaric oxygen pressure of 2 absolute atmospheres for 60 minutes. We evaluated liver function through mitochondrial function, determined by the stages 3 and 4 of respiration, respiratory control ratio (RCR) and mitochondrial permeability transition (Swelling). Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were also quantified . We analyzed the results using the Mann-Whitney test and were considered significant all results with p <0.05.
RESULTS: There were significant differences between the results of stage 3 in SHAM vs IR group ; of the stage 4 in the groups IR vs SHAM and SHAM vs IR /HBO; of the Respiratory Control Ratio (RCR) in the group IR vs IR / HBO ; of alanine aminotransferase in the groups IR vs SHAM , SHAM vs IR/HBO and IR vs IR / HBO; aspartate aminotransferase in the groups SHAM vs IR and SHAM vs IR / HBO.
CONCLUSION: The whole analysis of the mitochondiral function indicators permits us to conclude that the hyperbaric oxygen therapy acted as a protective agent of the mitochondrial function, minimizing the ischemia-reperfusion injury of the hepatic parenchyma.
Key words: Hyperbaric Oxygen Therapy. Mitochondria. Liver Ischemia. Reperfusion.
RESUMO
OBJETIVO: Analisar os efeitos da oxigenoterapia hiperbárica sobre a função hepática de ratos previamente submetidos à isquemia e reperfusão.
MÉTODOS: Realizou-se a distribuição aleatória de 23 ratos Wistar em três grupos: SHAM, animais submetidos ao estresse cirúrgico sem restrição de fluxo sanguíneo por clampeamento do pedículo hepático; IR ratos submetidos a oclusão vascular hepática de maneira intermitente em dois ciclos completos de 15 minutos de isquemia, seguidos por 5 min de reperfusão; IR/HBO, ratos submetidos ao clampeamento do pedículo hepático e ,ulteriormente , expostos a oxigenoterapia hiperbárica a pressão de 2 atmosferas absolutas durante 60 minutos. Avaliou-se a função hepática através da função mitocondrial, determinada pelos estados 3 e 4 da respiração mitocondrial, razão de controle respiratório(RCR) e transição de permeabilidade mitocondrial (Swelling) .Quantificou-se também alanina aminotransferase e aspartato aminotransferase séricas. Analisou-se os resultados pelo teste de Mann-Whitney e foram considerados significativos os valores de p < 0,05.
RESULTADOS:Houve diferença significativa nos valores do estado 3 no grupo SHAM vs IR; estado 4 nos grupos SHAM vs IR, SHAM vsIR/HBO; Razão de Controle Respiratório(RCR) no grupo IR vs IR/HBO; alanina aminotransferase nos grupos SHAM vs IR, SHAM vs IR/HBO, IR vs IR/HBO; aspartato aminotransferase nos grupos SHAM vs IR , SHAM vs IR/HBO.
CONCLUSÃO: A análise dos parâmetros mitocondriais como um todo permitiu concluir que a oxigenoterapia hiperbárica atuou como agente protetor da função mitocondrial, minimizando os efeitos deletérios da lesão de isquemia e reperfusão do parênquima hepático.
Descritores: Oxigenoterapia Hiperbárica. Mitocôndria. Fígado. Isquemia. Reperfusão.
Introduction
The main concern in liver surgery consists in trying to minimize the massive bleeding and prevent blood transfusion, which proved to be deleterious agents in the post-operative period. The intraoperative hemorrhage significantly affects morbidity and mortality, and the need for blood transfusions was an important factor in postoperative complications1.Taking into consideration these challenges, some techniques are of great help in liver surgery, such as vascular occlusion by clamping the hepatic pedicle (Pringle Technique) or the total vascular exclusion of the liver. However, the main side effect of the clamping techniques consists in hepatic ischemia-reperfusion injury, which induces hepatocellular suffering and involves complex metabolic pathways2. The ischemia-reperfusion injury consists of changes observed during the reperfusion period, which are mainly related to ischemic time and it includes hepatic microcirculatory alterations, hypotension, elevated levels of serum aminotransferase and LDH , mitochondrial dysfunction and lipid peroxidation 3. These changes are the result of a complex association between ATP depletion, and leukocyte activation, Kupffer cells in the liver sinusoids, release of proteases and phospholipases, complement activation and formation of reactive oxygen species3,4.
Many strategies to mitigate the effects of ischemia-reperfusion injury have been used in animal models, mainly the surgical and pharmacological ones, and among them all some had their effects confirmed in clinical studies1,5-84 . Accordingly, the intermittent clamping of the hepatic pedicle proved to be more effective in attenuating ischemia-reperfusion injury compared to the continuous portal triad clamping7. In this context, the interest in hyperbaric oxygen therapy (HBO) has grown due to its role in ischemia and reperfusion injury therefore in the liver transplantation field9,10. HBO is the inhalation of pure oxygen at hyperbaric conditions which increases the amount of dissolved oxygen in the blood and therefore in body tissues (Henry's Law), promoting a high tissue oxygen tension that demonstrated beneficial biochemical and cellular effects to tissues11. It is known that HBO operates basically with two physical factors of hyperbaric environment: the effects of mechanical stress and increased tissue oxygenation12. However, the biochemical and cellular effects of HBO in LIR are not yet fully elucidated. First, it was thought that HBO would exacerbate the injury by increasing the supply of oxygen in the body, thus producing more free radicals. However, experimental studies in rats subjected to skin ischemia and reperfusion demonstrated the beneficial effects of HBO during reperfusion. HBO decreases endothelial cell adhesion to neutrophils, by reducing the expression of adhesion molecules on endothelial cell surface, and can increase the tissue concentration of antioxidant enzymes13.
The aim of this study is to evaluate the effects of hyperbaric oxygen therapy (HBO) proceeded subsequently to the period of hepatocellular suffering induced by ischemia and reperfusion.
Method
Animals: A total of 23 male Wistar rats were used, weighing from 200 to 320 g, from the General Animal House of the Ribeirão Preto Campus , University of São Paulo. The animals were fed with standard laboratory diet for the species (Purina Nutromentos Ltda.) and water at will. Remained in the vivarium of the FMRP-USP at room temperature, respecting the circadian cycle of the animals as the guide of the Ethics Committee for Animal Experimentation of FMRP-USP demands.
Groups division: The animals were randomly divided into 3 groups:
I) SHAM (n = 7) rats subjected to surgical stress for 40 min without restricting blood flow by clamping the hepatic pedicle and without exposure to HBO.
II) IR (n = 7) - rats subjected to intermittent hepatic pedicle clamping in two complete cycles of 15 min of ischemia followed by 5 min of reperfusion without exposure to HBO.
III) IR / HBO (n = 9) - rats subjected to 2 cycles of occlusion of the hepatic vessels, consisting of 15 minutes of ischemia followed by 5 minutes of reperfusion and immediately exposed to HBO at 2 absolute atmospheres(ATA) for 60 min.
Surgical Procedure: Each rat was weighed and anesthetized by intramuscular application of xylazine hydrochloride (20mg/ml) solution and ketamine hydrochloride (50mg/ml) in a 1:2 ratio being administered 100mg/Kg/weigh .The evaluation of the efficiency of the anesthesia was verified by the loss of the corneal-palpebral reflex and by the lack of response when we held the rats hind paw. We Proceeded with the proper placement of the animals and performing a median incision from the xiphoid process to the pubis. After the exposure of the abdominal cavity, there was the dissection of the round ligament of the liver and identification of the triad. This was followed by clamping the portal triad a home-made clamp for 15 min, after this interval the clamp was removed and there were 5 min for reperfusion; next , the clamping and reperfusion procedure was repeated. The animal was sacrificed by total exsanguination technique by puncturing the inferior vena cava after its when the abdominal visceras were moved away.
Hyperbaric Oxygen Therapy: HBO was performed in collective camera (simultaneous exposure of 3 rats) (Sechrist, model 2500 B) directly pressurized with oxygen. The duration of each session was of 60 minutes with 15min to compression and 15 min to decompression inside the camera, thereby the exposure of the animals was continuous for 30 min to 2 ATA HBO.
Results
Regarding the parameters related to mitochondrial respiration, we found a significant difference in the rate of oxygen consumption in stage 3 of mitochondrial respiration between IR and SHAM groups (Figure 1A). The rate of oxygen consumption in stage 4 of mitochondrial respiration showed significant difference between the group and SHAM groups IR and IR / HBO (Figure 1B). The Respiratory Control Ratio (RCR) showed a significant difference between groups IR and IR / HBO (Figure 1C). No significant difference was found among the other associations.
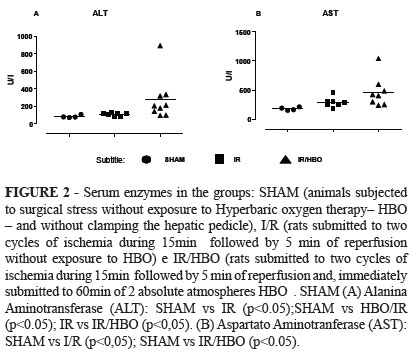
The quantification of serum enzymes showed a significant difference in the dosage of alanine aminotransferase (ALT) between the group SHAM and the groups IR and IR / HBO and between groups IR and IR / HBO (Figure 2A). There was also a significant difference in the dosage of aspartate aminotransferase (AST) between the group SHAM and groups IR and IR / HBO (Figure 2B). No significant difference was found among the other associations.
Discussion
The ischemia-reperfusion injury seriously affects the process of oxidative phosphorylation. Since the mitochondrial membrane are localization sites of the respiratory chain and, and cell membranes are target of the free radicals generated during reperfusion, it is supposed that the destruction of the membranes will result in impairment of oxidative phosphorylation. Thus, the mitochondrial changes are associated with liver microcirculation injury and are good indicators of ischemia and reperfusion8,13-15.
Likewise, serum transaminases quantifications are classic parameters of hepatocellular injury, indicating changes in mitochondrial membrane permeability, and being widely used in studies regarding the ischemia and reperfusion injury5,13,16,17.
In our study we evaluated mitochondrial respiration by oxygen consumption rate in stage 4 (resting respiration) ,rate of oxygen consumption in stage 3 (active respiration) and respiratory control ratio (RCR), which indicates the coupling between electrons transfer through the respiratory chain and oxidative phosphorylation. Additionally, we evaluated the permeability of the inner mitochondrial membrane by osmotic swelling of mitochondria, related to Ca + homeostasis .
Ss for the stage 3 of mitochondrial respiration (Figure 1A) there was a decrease in the oxygen consumption rate in the IR group compared with the SHAM group (p <0.05) indicating impaired mitochondrial energy production, which indicates a deleterious effect of ischemia / reperfusion in this group. This result is found by other authors15, but in different models of ischemia-reperfusion. Taking into consideration the oxygen consumption in stage 3 it was not found in our study significant difference between the group that underwent ischemia and reperfusion with or without exposure to HBO, demonstrating that HBO was not harmful when this parameter was evaluated.
Relative the stage 4 of mitochondrial respiration (Figure 1B ), it was observed a decrease in the rate of oxygen consumption by the mitochondria in group IR compared to SHAM group (p <0.05), indicating a change in permeability of the mitochondrial inner membrane, responsible for maintaining the proton gradient when the membrane is energized 13. When the group IR /HBO was evaluated in contrast to SHAM group it was also observed that there was a decrease in the rate of oxygen consumption in stage 4. Curiously, this decrease in stage 4 in IR and IR / HBO groups compared to SHAM group indicates a stability of the inner mitochondrial membrane. These results suggest a cellular mechanism that compensates a possible functional deficiency caused by ischemia. This result is not found in the literature. Thus, we also conclude that HBO was not detrimental to stage 4 of mitochondrial respiration comparing the ischemic groups submitted or not to this procedure.
By analyzing the RCR (Figure 1C) there was not found difference between the SHAM group and the ischemic groups with or without exposure to HBO. Significant difference was found between groups IR and IR / HBO groups, demonstrating increased results of RCR in IR / HBO group. This result suggests that HBO was effective in accelerating the respiration under energy demand conditions , with preserved free energy of oxidation-reduction reactions in the form of ATP.
The osmotic mitochondrial swelling induced by Ca +2 and phosphate (Figure 1D) showed no significant difference between groups.
With regard to serum levels of ALT (Figure 2A) there was an increase in the results obtained in the IR group compared to SHAM group (p <0.05), which is in agreement with other studies in the literature5,13. We also found increased levels of ALT in group IR / HBO compared to SHAM group and in the group IR/HBO compared to the IR group. These facts suggest that HBO increased the hepatocellular injury.
There was a significant increase of AST in IR group compared to the SHAM group, as demonstrated by other authors 15. The group IR / HBO also showed an increase compared to the SHAM group, corroborating the results obtained with ALT levels. However, the same was not observed in groups IR and IR / HBO results that showed no significant difference, indicating that HBO was effective in containing the damage of hepatocytes when comparing the ischemic groups.
Conclusion
The analysis of the mitochondrial function indicators as a whole allows us to conclude that the hyperbaric oxygen therapy acted as a protective agent of the mitochondrial function, minimizing the ischemia-reperfusion injury of the hepatic parenchyma.
References
1. Kapoor S. Hepatic ischaemia-reperfusion injury from bench to bedside (Br J Surg 2010;97:1461-1475). Br J Surg. 2011;98(3):459.
2. Castro-Silva O, Centurion S, Pacheco EG, Brisotti JL, Oliveira AF, Sasso KD. Aspectos básicos da lesão de isquemia e reperfusão e do pré-condicionamento isquêmico. Acta Cir Bras. 2002;17:96-100.
3. Miranda L, Viaro F, Ceneviva R, Evora P. As bases experimentais da lesão por isquemia e reperfusão do fígado.Revisão. Acta Cir Bras. 2004;19(1):3-12.
4. Collard CD, Gelman S. Pathophysiology, clinical manifestations, and prevention of ischemia-reperfusion injury. Anesthesiology. 2001;94(6):1133-8.
5. Helewski K, Kowalczyk-Ziomek G, Czecior E, Wyrobiec G, Harabin-Slowinska M, Juszko-Piekut M, et al. Protective effect of intermittent clamping of the portal triad in the rat liver on liver ischemia-reperfusion injury. Hepat Mon. 2011;11(6):445-51.
6. Lesurtel M, Lehmann K, de Rougemont O, Clavien PA. Clamping techniques and protecting strategies in liver surgery. HPB (Oxford). 2009;11(4):290-5.
7. Petrowsky H, McCormack L, Trujillo M, Selzner M, Jochum W, Clavien PA. A prospective, randomized, controlled trial comparing intermittent portal triad clamping versus ischemic preconditioning with continuous clamping for major liver resection. Ann Surg. 2006;244(6):921-8.
8. Miranda LEC, Viaro F, Ceneviva R, Evora, PRB. A atividade respiratória mitocondrial é um bom parâmetro para a lesão por isquemia e reperfusão hepática?. Arq. Gastroenterol.2005;42:89-94 .
9. Kihara K, Ueno S, Sakoda M, Aikou T. Effects of hyperbaric oxygen exposure on experimental hepatic ischemia reperfusion injury: relationship between its timing and neutrophil sequestration. Liver Transpl. 2005;11(12):1574-80.
10. Muralidharan V, Christophi C. Hyperbaric oxygen therapy and liver transplantation. HPB (Oxford). 2007;9(3):174-82.
11. Tibbles PM, Edelsberg JS. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334(25):1642-8.
12. Tolentino EC, Ferez, O, Oliveira GR, Ramalho FS, Ramalho LNZ, Zucoloto S, Et al. Oxigenoterapia hiperbárica e regeneração hepática. Acta Cir Bras. 2003;8:4-5.
13. Lima CX, Sanches MD, Rezende Neto JB, Silva RC, Teixeira MM, Souza DaG, et al. Hyperbaric oxygen therapy aggravates liver reperfusion injury in rats. Acta Cir Bras. 2008;23(4):315-21.
14. Tolentino EC, Castro-Silva O, Zucoloto S, Souza ME, Gomes MC, Sankarankutty AK, et al. Effect of hyperbaric oxygen on liver regeneration in a rat model. Transplant Proc. 2006;38:1947-52.
15. Castro-Silva O, Sankarankutty AK, Correa RB, Ferreira J, Vollet Filho JD, Kurachi C, et al. Autofluorescence spectroscopy in liver transplantation: preliminary results from a pilot clinical study. Transplant Proc. 2008;40:722-5.
16. Silva, FN. Isquemia hepática normotérmica em ratos: estudo da lesão celular através do uso de clampeamento pedicular contínuo e intermitente. Rev Col Bras Cir. 2002;29:342-8.
17. Seyama Y, Imamura H, Inagaki Y, Matsuyama Y, Tang W, Makuuchi M, Kokudo N. Intermittent clamping is superior to ischemic preconditioning and its effect is more marked with shorter clamping cycles in the rat liver. J Gastroenterol. 2013;48(1):115-24.
Conflict of interest: none
Financial source: none
- 1. Kapoor S. Hepatic ischaemia-reperfusion injury from bench to bedside (Br J Surg 2010;97:1461-1475).
- Br J Surg. 2011;98(3):459.
- 2. Castro-Silva O, Centurion S, Pacheco EG, Brisotti JL, Oliveira AF, Sasso KD. Aspectos básicos da lesão de isquemia e reperfusão e do pré-condicionamento isquêmico. Acta Cir Bras. 2002;17:96-100.
- 3. Miranda L, Viaro F, Ceneviva R, Evora P. As bases experimentais da lesão por isquemia e reperfusão do fígado.Revisão. Acta Cir Bras. 2004;19(1):3-12.
- 4. Collard CD, Gelman S. Pathophysiology, clinical manifestations, and prevention of ischemia-reperfusion injury. Anesthesiology. 2001;94(6):1133-8.
- 5. Helewski K, Kowalczyk-Ziomek G, Czecior E, Wyrobiec G, Harabin-Slowinska M, Juszko-Piekut M, et al. Protective effect of intermittent clamping of the portal triad in the rat liver on liver ischemia-reperfusion injury. Hepat Mon. 2011;11(6):445-51.
- 6. Lesurtel M, Lehmann K, de Rougemont O, Clavien PA. Clamping techniques and protecting strategies in liver surgery. HPB (Oxford). 2009;11(4):290-5.
- 7. Petrowsky H, McCormack L, Trujillo M, Selzner M, Jochum W, Clavien PA. A prospective, randomized, controlled trial comparing intermittent portal triad clamping versus ischemic preconditioning with continuous clamping for major liver resection. Ann Surg. 2006;244(6):921-8.
- 8. Miranda LEC, Viaro F, Ceneviva R, Evora, PRB. A atividade respiratória mitocondrial é um bom parâmetro para a lesão por isquemia e reperfusão hepática?. Arq. Gastroenterol.2005;42:89-94 .
- 9. Kihara K, Ueno S, Sakoda M, Aikou T. Effects of hyperbaric oxygen exposure on experimental hepatic ischemia reperfusion injury: relationship between its timing and neutrophil sequestration. Liver Transpl. 2005;11(12):1574-80.
- 10. Muralidharan V, Christophi C. Hyperbaric oxygen therapy and liver transplantation. HPB (Oxford). 2007;9(3):174-82.
- 11. Tibbles PM, Edelsberg JS. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334(25):1642-8.
- 12. Tolentino EC, Ferez, O, Oliveira GR, Ramalho FS, Ramalho LNZ, Zucoloto S, Et al. Oxigenoterapia hiperbárica e regeneração hepática. Acta Cir Bras. 2003;8:4-5.
- 13. Lima CX, Sanches MD, Rezende Neto JB, Silva RC, Teixeira MM, Souza DaG, et al. Hyperbaric oxygen therapy aggravates liver reperfusion injury in rats. Acta Cir Bras. 2008;23(4):315-21.
- 14. Tolentino EC, Castro-Silva O, Zucoloto S, Souza ME, Gomes MC, Sankarankutty AK, et al. Effect of hyperbaric oxygen on liver regeneration in a rat model. Transplant Proc. 2006;38:1947-52.
- 15. Castro-Silva O, Sankarankutty AK, Correa RB, Ferreira J, Vollet Filho JD, Kurachi C, et al. Autofluorescence spectroscopy in liver transplantation: preliminary results from a pilot clinical study. Transplant Proc. 2008;40:722-5.
- 16. Silva, FN. Isquemia hepática normotérmica em ratos: estudo da lesão celular através do uso de clampeamento pedicular contínuo e intermitente. Rev Col Bras Cir. 2002;29:342-8.
- 17. Seyama Y, Imamura H, Inagaki Y, Matsuyama Y, Tang W, Makuuchi M, Kokudo N. Intermittent clamping is superior to ischemic preconditioning and its effect is more marked with shorter clamping cycles in the rat liver. J Gastroenterol. 2013;48(1):115-24.
Publication Dates
-
Publication in this collection
01 Feb 2013 -
Date of issue
2013