Abstracts
PURPOSE: To analyze the usefulness of Quick Lactose Intolerance Test in relation to the genetic test based on LCT-13910C>T genotypes, previously validated for clinical practice, for primary hypolactasia/lactase-persistence diagnosis. METHODS: Thirty-two dyspeptic patients that underwent upper gastrointestinal endoscopy entered the study. Two postbulbar duodenal biopsies were taken for the Quick test, and gastric antral biopsy for DNA extraction and LCT-13910C>T polymorphism analysis. DNA was also extracted from biopsies after being used in the Quick Test that was kept frozen until extraction. RESULTS: Nine patients with lactase-persistence genotype (LCT-13910CT or LCT-13910TT) had normolactasia, eleven patients with hypolactasia genotype (LCT-13910CC) had severe hypolactasia, and among twelve with mild hypolactasia, except for one that had LCT-13910CT genotype, all the others had hypolactasia genotype. The agreement between genetic test and quick test was high (p<0.0001; Kappa Index 0.92). Most of the patients that reported symptoms with lactose-containing food ingestion had severe hypolactasia (p<0.05). Amplification with good quality PCR product was also obtained with DNA extracted from biopsies previously used in the Quick Test; thus, for the future studies antral gastric biopsies for genetic test would be unnecessary. CONCLUSION: Quick test is highly sensitive and specific for hypolactasia diagnosis and indicated those patients with symptoms of lactose intolerance.
Lactose Intolerance; Endoscopy; Biopsy; Nutrition; Public Health
OBJETIVO: Analisar a aplicabilidade do Teste Quick de Intolerância à Lactose em relação ao teste genético baseado nos genótipos LCT-13910C>T, previamente validado para a prática clínica, para diagnóstico de má digestão primária de lactose/digestão de lactose. MÉTODOS: Trinta e dois pacientes dispépticos submetidos à endoscopia digestiva entraram no estudo. Duas biópsias duodenais pós-bulbares foram empregadas no Teste Quick, e biópsia do antro gástrico para extração de DNA e análise do polimorfismo LCT-13910C>T. DNA também foi extraído de biópsias depois de terem sido usadas no teste Quick, e conservadas congeladas. RESULTADOS: Nove pacientes com genótipo de lactase persistente (LCT-13910CT ou LCT-13910TT) tinham normolactasia, onze pacientes com genótipo de hipolactasia (LCT-13910CC) tinham hipolactasia severa, e entre doze com hipolactasia leve, com exceção de uma que tinha genótipo LCT-13910CT, todos os demais tinham genótipo de hipolactasia. A concordância entre o teste genético e o Quick Teste foi alta (p<0,0001; Índice Kappa=0,92). A maioria dos pacientes que relataram sintomas com ingestão de alimentos com lactose tinham hipolactasia severa (p<0,05). Amplificação com produto de PCR foi obtido com DNA extraído das biópsias usadas no teste Quick; portanto, nos trabalhos futuros seria desnecessário coletar biópsia do antro gástrico para o teste genético. CONCLUSÃO: O Teste Quick é altamente sensível e específico para diagnóstico de hipolactasia e indicou aqueles pacientes com sintomas de intolerância à lactose.
Intolerância à Lactose; Endoscopia; Biópsia; Nutrição em Saúde Pública
14 - ORIGINAL ARTICLE
ALIMENTARY TRACT
Comparison of Quick Lactose Intolerance Test in duodenal biopsies of dyspeptic patients with single nucleotide polymorphism LCT-13910C>T associated with primary hypolactasia/lactase-persistence1 1 Research performed at Department of Surgery Riberao Preto Medical School, University of Sao Paulo (FMRP-USP) and Department of Gastroenterology, University of São Paulo School of Medicine (FM-USP), Brazil.
Comparação do Teste Quick de Intolerância à Lactose em biópsias duodenais de pacientes dispépticos com polimorfismo de nucleotídeo único LCT-13910C>T associado com hipolactasia primária/lactase persistente
Rejane MattarI; Anibal Basile-FilhoII; Rafael KempIII; José Sebastião dos SantosIV
IPhD, Affiliate Professor, Department of Gastroenterology, University of São Paulo School of Medicine (FM-USP), Brazil. Acquisition of data (genetic test), manuscript preparation, critical revision
IIPhD, Associate Professor, Head of Division of Intensive Care, Department of Surgery and Anatomy, Ribeirão Preto School of Medicine of the University of São Paulo (FMRP-USP), Brazil. Design, intelectual and scientific content of the study, acquisition of data (point-of-care Quict Test), manuscript writing
IIIPhD, Affiliate Professor, Division of Digestive Surgery and Endoscopy, Department of Surgery and Anatomy, Ribeirão Preto Medical School of the University of São Paulo (FMRP-USP), Brazil. Acquisition of data, involved with technical procedures of upper digestive endoscopy
IVPhD, Associate Professor, Division of Digestive Surgery and Endoscopy, Department of Surgery and Anatomy, Ribeirão Preto Medical School of the University of São Paulo (FMRP-USP), Brazil. Critical revision
Correspondence Correspondence: Anibal Basile-Filho Divisão de Terapia Intensiva, Departamento de Cirurgia e Anatomia. Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo Avenida Bandeirantes, 3900 14048-900 Ribeirão Preto - SP Brasil Tel.: (55 16) 3602-2409 abasile@fmrp.usp.br
ABSTRACT
PURPOSE: To analyze the usefulness of Quick Lactose Intolerance Test in relation to the genetic test based on LCT-13910C>T genotypes, previously validated for clinical practice, for primary hypolactasia/lactase-persistence diagnosis.
METHODS: Thirty-two dyspeptic patients that underwent upper gastrointestinal endoscopy entered the study. Two postbulbar duodenal biopsies were taken for the Quick test, and gastric antral biopsy for DNA extraction and LCT-13910C>T polymorphism analysis. DNA was also extracted from biopsies after being used in the Quick Test that was kept frozen until extraction.
RESULTS: Nine patients with lactase-persistence genotype (LCT-13910CT or LCT-13910TT) had normolactasia, eleven patients with hypolactasia genotype (LCT-13910CC) had severe hypolactasia, and among twelve with mild hypolactasia, except for one that had LCT-13910CT genotype, all the others had hypolactasia genotype. The agreement between genetic test and quick test was high (p<0.0001; Kappa Index 0.92). Most of the patients that reported symptoms with lactose-containing food ingestion had severe hypolactasia (p<0.05). Amplification with good quality PCR product was also obtained with DNA extracted from biopsies previously used in the Quick Test; thus, for the future studies antral gastric biopsies for genetic test would be unnecessary.
CONCLUSION: Quick test is highly sensitive and specific for hypolactasia diagnosis and indicated those patients with symptoms of lactose intolerance.
Key words: Lactose Intolerance. Endoscopy. Biopsy. Nutrition, Public Health.
RESUMO
OBJETIVO: Analisar a aplicabilidade do Teste Quick de Intolerância à Lactose em relação ao teste genético baseado nos genótipos LCT-13910C>T, previamente validado para a prática clínica, para diagnóstico de má digestão primária de lactose/digestão de lactose.
MÉTODOS: Trinta e dois pacientes dispépticos submetidos à endoscopia digestiva entraram no estudo. Duas biópsias duodenais pós-bulbares foram empregadas no Teste Quick, e biópsia do antro gástrico para extração de DNA e análise do polimorfismo LCT-13910C>T. DNA também foi extraído de biópsias depois de terem sido usadas no teste Quick, e conservadas congeladas.
RESULTADOS: Nove pacientes com genótipo de lactase persistente (LCT-13910CT ou LCT-13910TT) tinham normolactasia, onze pacientes com genótipo de hipolactasia (LCT-13910CC) tinham hipolactasia severa, e entre doze com hipolactasia leve, com exceção de uma que tinha genótipo LCT-13910CT, todos os demais tinham genótipo de hipolactasia. A concordância entre o teste genético e o Quick Teste foi alta (p<0,0001; Índice Kappa=0,92). A maioria dos pacientes que relataram sintomas com ingestão de alimentos com lactose tinham hipolactasia severa (p<0,05). Amplificação com produto de PCR foi obtido com DNA extraído das biópsias usadas no teste Quick; portanto, nos trabalhos futuros seria desnecessário coletar biópsia do antro gástrico para o teste genético.
CONCLUSÃO: O Teste Quick é altamente sensível e específico para diagnóstico de hipolactasia e indicou aqueles pacientes com sintomas de intolerância à lactose.
Descritores: Intolerância à Lactose. Endoscopia. Biópsia. Nutrição em Saúde Pública.
Introduction
Lactase or lactase-phlorizin hydrolase, located in the brush border of intestinal mucosa, is responsible for the hydrolysis of lactose, the major carbohydrate present in milk, into galactose and glucose. The maximal activity of lactase is during perinatal period; however, in most humans of different ethnic groups, it declines at some point during life, emerging two groups: lactase-persistence (normolactasia, lactose digestion) and lactase non-persistence (hypolactasia, lactose maldigestion). Undigested lactose is fermented by the intestinal flora, producing hydrogen, methane, carbon dioxide and short-chain fatty acids, which cause symptoms of lactose intolerance, flatulence, bloating, abdominal pain and diarrhea, depending on the amount of ingested lactose1.
Symptoms suggestive of lactose intolerance are unspecific and may be related to other causes such as irritable bowel syndrome, cow's milk protein allergy, bacterial overgrowth, celiac disease, and inflammatory bowel disease, or other dietary sources of intestinal gas, such as beans, which contain two indigestible sugars, stachyose and raffinose1. Self-perceived lactose intolerance may lead to unnecessary avoidance of milk and dairy products, the main source of calcium in the diet, with future consequences on bone health1, hypertension, and diabetes2. Thus, diagnosis of lactose maldigestion imposes for adequate clinical management and correct lactose-restriction diet.
The diagnosis of lactose maldigestion was initially performed by lactase activity in jejunal biopsies3, being replaced by duodenal biopsies; nonetheless, the mean lactase activity in the duodenum is lower than in the jejunum, being less reliable4. Quick Lactose Intolerance Test in postbulbar duodenum samples showed sensitivity and specificity of 95% and 100%, respectively5, being more sensitive than lactose breath test6,7, and highly sensitive in a pediatric population8.
Lactose tolerance test, based on blood glucose levels measured before and after an oral load of lactose, indicates lactose tolerance when the rise of serum glucose is >20 mg/dL, although widely performed is less sensitive than the lactose tolerance hydrogen breath test, considered the gold standard. Both tests provoke symptoms in those with lactose maldigestion, are long-standing, and cumbersome; the hydrogen breath test depends on the activity of the intestinal flora to ferment undigested lactose9.
In a Brazilian population, using the single nucleotide LCT-13910C>T polymorphism of lactase-persistence, only 24.7% of Europeans descent and 18.3% of African origin subjects had lactase-persistence genotype1, and showed an excellent correlation with lactose tolerance test results10. Thus, the purpose of this study was to compare the results of Quick Lactose Intolerance Test with LCT-13910C>T genotypes to achieve its clinical application for hypolactasia diagnosis.
Methods
This prospective research protocol was approved by the Research Ethics Committee of the Clinics Hospital of Ribeirão Preto Medical School of the University of São Paulo (Protocol 8171/2012). Subjects that were routinely enrolled to perform the upper digestive endoscopy for some clinical investigation were invited to participate, and gave written informed consent. Exclusion criteria were signs of bleeding, fistulas, or recent high digestive sutures (<7 days), and celiac disease.
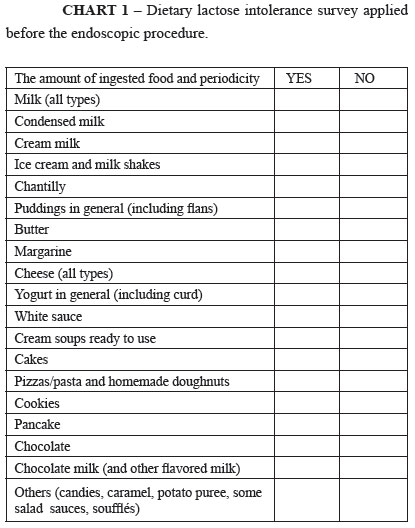
A questionnaire of dietary lactose containing food ingestion and related symptoms was applied (Chart 1).
Thirty-two dyspeptic patients (mean age 50.2±17.5 years, 59.4% females), submitted to routine upper digestive endoscopy in the Digestive Endoscopy Center of Clinics Hospital of Ribeirão Preto Medical School of the University of São Paulo, entered the study. Twenty-three (72%) subjects were Caucasian and 9 were African-Brazilians.
Quick lactose intolerance test
Two specimens of biopsy of the postbulbar region (2 mm each) were taken to perform the Quick Test (Biohit, Helsinki, Finland) for lactase activity assay, according to the manufacturer instruction. The specimens were placed into the well of the test plate immediately after its collection; two drops (80 µl) of a substrate solution were added and incubated for 15 minutes. After this step 2 drops of chromogen solution (10 µl) in acetic acid and 1 drop (80 µl) of signaling enzymatic solution were added with incubation time of 5 minutes. The total reaction time was 20 minutes. The test result was colorimetric: a dark blue coloring, indicating normolactasia (lactase activity), light blue color mild hypolactasia and colorless severe hypolactasia.
LCT-13910C>T single nucleotide polymorphism analysis
DNA was extracted by salting out from specimens of the antrum11, and used in the polymerase chain reaction and restriction fragment length polymorphism analysis, as was previously described10. Two biopsies after being used in the Quick Test were frozen for DNA extraction in order to see viability to avoid collection of biopsies from the gastric antrum for the genetic test. Digested PCR products with HinfI were visualized on a 3% low melting point agarose gel stained by ethidium bromide. Samples showing a single band of 201 bp were classified as the LCT-13910CC genotype (hypolactasia or lactase non-persistence), a single band of 177 bp as the LCT-13910TT genotype (normolactasia, lactase-persistence), and two bands of 201 bp and 177 bp the LCT-13910CT genotype (normolactasia, lactase-persistence).
Statistical analysis
Statistical analysis was performed by Kappa index measure of agreement of diagnostic tests, and Chi-square or Likelihood ratio using SPSS version 15.0 for Windows (Chicago, Illinois, USA). A p value of <0.05 was considered statistically significant.
Results
There was no significant association of ethnicity and gender with LCT-13910C>T genotypes, the Quick Test results, and the presence of symptoms with milk and/or dairy products consumption, despite Caucasians being less symptomatic (Chart 2).
Nine patients (41%) with hypolactasia genotype and one (10%) with lactase-persistence genotype reported symptoms with milk and/or dairy products consumption, p>0.05 (Table 1).
The association of symptoms with the distribution of the patients according to the Quick Test results was significant (p<0.05), showed that 8 (72.7%) of the patients with severe hypolactasia, one with mild hypolactasia and one with normolactasia had symptoms with lactose-containing food ingestion (p<0.05). One Caucasian woman 46 years old with lactase-persistence and normolactasia had symptoms with milk ingestion (Chart 2).
Nine patients with LCT-13910CT or LCT-13910TT genotypes had normolactasia, eleven patients with LCT-13910CC genotype had severe hypolactasia and among twelve with mild hypolactasia, except for one that had LCT-13910CT genotype, all the others were LCT-13910CC (Table 2). Agreement between the Quick Test and the genetic test was high (p<0.0001; Kappa index 0.92), considering LCT-13910CC as hypolactasia genotype, and LCT-13910CT or LCT-13910TT as lactase-persistence genotype, the sensitivity and the negative predictive value of the Quick Test were 100%, and the specificity and the positive predictive value were 90% and 95.6%, respectively.
Biopsies that were previously used in the Quick Test and used for DNA extraction, gave good quality PCR products; thus, gastric antrum biopsies could be avoid for the genetic test.
Discussion
The most important finding of this study is that comparing the genetic test with Quick lactose intolerance test, the latter indicates individuals with severe hypolactasia that are more prone to present symptoms of lactose intolerance, agreeing with previous report5, rather than those with mild hypolactasia, even both presenting primary hypolactasia genotype. Another finding was that mild hypolactasia was associated with hypolactasia genotype rather than with lactase-persistence genotype, as was previously described by Kuokkanen et al.5, although they showed that these individuals had intermediate levels of duodenal lactase activity, between those levels detected in the normolactasia group and in the severe hypolactasia group. This finding may explain the fact that some individuals with hypolactasia genotype are asymptomatic even ingesting a great amount of milk, suggesting that the levels of the physiological decline of lactase vary among different populations12.
The association of primary hypolactasia genotype with symptoms after lactose-containing food ingestion was not significant, in contrast to previously reported in 1900 Finnish adults that showed a significant association of hypolactasia genotype, less milk intake, and the presence of gastrointestinal symptoms13, the explanation for that is 50% of patients with hypolactasia genotype had mild hypolactasia. One Caucasian woman 46 years old with lactase-persistence and normolactasia, unexpectedly reported symptoms with milk ingestion that may be caused by irritable bowel syndrome (IBS), as was suggested there may be other components of milk besides lactose that cause symptoms among subjects with IBS14.
Even though the number of the patients analyzed in this study is lower than previous reported by other authors that compared the Quick Test with the genetic test, the results of sensitivity (100%) was similar5. Although presenting a high sensitivity the Quick Test has limitations, one is the size of the biopsies that if larger or shorter than 2 mm may give false negative or false positive results of hypolactasia, respectively. Another is the dependence on an invasive exam for collection of samples that not always is accepted by the patients that prefer a blood collection test. A biopsy-based gastrointestinal endoscopy exam is limited by the coagulation status, bleeding risks, and clinical conditions of the patient. Another point to consider is the Quick Test has to be performed immediately after collection of duodenum samples, requiring a laboratory technician in the endoscopy suite, as the incubation times have to be rigorously followed, and even being a very simple device, skillful in laboratory handling is necessary to perform the Quick Test.
The Quick Test is expensive (USD 30/individual test) for the Public Health Service compared to the genetic test, being more suitable for dyspeptic patients already undergoing endoscopy examination in private clinics for some clinical investigation. Additionally, the genetic test indicates primary hypolactasia and lactase-persistence8. However, those with lactase-persistence genotype may also present transitory hypolactasia along with celiac disease, Crohn's disease, or infectious enteritis diagnosis 1.
Outside the setting of tertiary referral centers genetic test may be considered more cumbersome than a gastrointestinal endoscopy with duodenal biopsy for the Quick Test analysis. Nonetheless, blood samples may be shipped to this referral centers for DNA-based genetic tests that have advantages: absence of lactose intolerance symptoms, single testing, non-invasive, and low cost8.
In these case series an association of hypolactasia genotype with ethnic groups was not observed in contrast with our report in 567 brazilians8, maybe the effect of the low number of patients.
Conclusions
Quick test is highly sensitive and specific to indicate subjects with hypolactasia and lactase persistence, and those more prone to present lactose intolerance symptoms. The genetic test is simple, non invasive, highly sensitive, and has a low cost.
Acknowledgments
To Ronaldo Vicente Martins for his precious patients records acquisition and Endoscopy Personnel Staffing for technical procedures of duodenal biopsy specimen acquisition for Lactose Intolerance Quick Test. Maria do Socorro Monteiro for technical assistance of the genetic test. The financial support for the kit purchasing was received from the Hospital das Clínicas (FAEPA) of Ribeirão Preto Medical School of the University of São Paulo (FMRP-USP), and for the genetic tests from the Hospital das Clinicas of FMUSP and Fundação Faculdade de Medicina.
Conflict of interest: none
Financial source: FAEPA
- 1. Mattar R, Mazo DFC, Carrilho FJ. Lactose intolerance: diagnosis, genetic, and clinical factors. Clin Exp Gastroenterol. 2012;5:113-21.
- 2. Nicklas TA, Qu H, Hughes SO, He M, Wagner SE, Foushee HR, Shewchuk RM. Self-perceived lactose intolerance results in lower intakes of calcium and dairy foods and is associated with hypertension and diabetes in adults. Am J Clin Nutr. 2011;94:191-8.
- 3. Dahlqvist A. Assay of intestinal disaccharidases. Anal Biochem. 1968;22:99-107.
- 4. Lagman JM, Rowland R. Activity of duodenal disaccharidases in relation to normal and abnormal mucosal morphology. J Clin Pathol. 1990;43:537-40.
- 5. Kuokkanen M, Myllyniemi M, Vauhkonen M, Helske T, Kääriäinen I, Karesvuori S, Linnala A, Härkönen M, Järvelä I, Sipponen P. A biopsy-based quick test in the diagnosis of duodenal hypolactasia in upper gastrointestinal endoscopy. Endoscopy. 2006;38:708-12.
- 6. Ojetti V, La Mura R, Zocco MA, Cesaro P, De Masi E, La Mazza A, Cammarota G, Gasbarrini G, Gasbarrini A. Quick Test: a new test for the diagnosis of duodenal hypolactasia. Dig Dis Sci. 2008;53:1589-92.
- 7. Rao P, Rao N, Jordinson M, Scott C, Hinchcliffe C, Campbell D. Comparison of Quick Point-of-Care Test for small-bowel hypolactasia with biochemical lactase assay in children. JPGN. 2012;54:401-3.
- 8. Mattar R, Monteiro MS, Villares CA, Santos AF, Silva JMK, Carrilho FJ. Frequency of LCT -13910C>T single nucleotide polymorphism associated with adult-type hypolactasia/lactase persistence among Brazilians of different ethnic groups. Nutr J. 2009;8:46.
- 9. Law D, Conklin J, Pimentel M. Lactose Intolerance and the role of the lactose breath test. Am J Gastroenterol. 2010;105:1726-8.
- 10. Mattar R, Monteiro MS, Villares CA, Santos AF, Carrilho FJ. Single nucleotide polymorphism C/T-13910, located upstream of the lactase gene, associated with adult-type hypolactasia: validation for clinical practice. Clin Biochem. 2008;41:628-30.
- 11. Mattar R, Santos AF, Eisig JN, Rodrigues TN, Silva FM, Lupinacci RM, Iriya K, Carrilho FJ. No correlation of babA2 with vacA and cagA genotypes of Helicobacter pylori and grading of gastritis from peptic ulcer disease patients in Brazil. Helicobacter. 2005;10:601-8.
- 12. Ingram CJE, Raga TO, Tarekegn A, Browning SL, Elamin MF, Bekele E, Thomas MG, Weale ME, Bradman N, Swallow DM. Multiple rare variants as a cause of a common phenotype: several different lactase persistence associated alleles in a single ethnic group. J Mol Evol. 2009;69:579-588.
- 13. Anthoni SR, Rasinperä HA, Kotamies AJ, Komu HA, Pihlajamäki HK, Kolho K-L, Järvelä IE. Molecularly defined adult-type hypolactasia among working age people with reference to milk consumption and gastrointestinal symptoms. World J Gastroenterol. 2007;13:1230-5.
- 14. Ligaarden SC, Lydersen S, Farup PG. Diet in subjects with irritable bowel syndrome: a cross-sectional study in the general population BMC Gastroenterol. 2012,12:61.
Publication Dates
-
Publication in this collection
01 Feb 2013 -
Date of issue
2013