Abstract
PURPOSE:
To evaluate the effects of vitamin K1 on wound healing in the left colon of rats with experimental biliary obstruction.
METHODS:
Sixteen male rats, divided into four groups of four animals each (L, M, LK, and MK), underwent colostomy followed by bowel suture in the left colon. Seven days before, animals in the L and LK groups had undergone common bile duct ligation. The animals in groups MK and LK received vitamin K1 supplementation. On day 7 after bowel suture, repeat laparotomy was performed for evaluation of colonic healing by burst pressure measurement and collection of samples for histopathological analysis. Changes in body weight were evaluated in the four groups.
RESULTS:
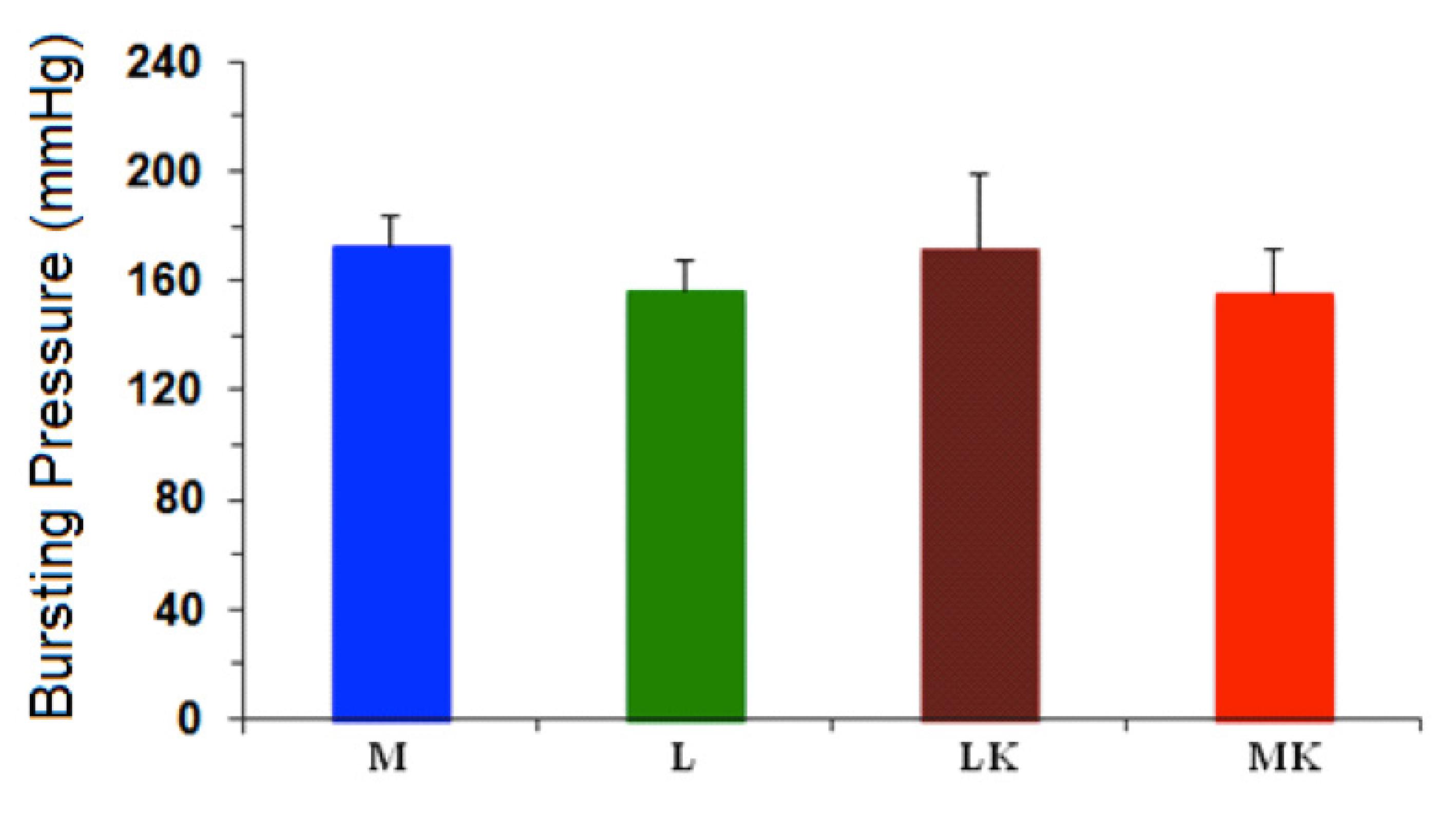
Weight loss was lower in animals supplemented with vitamin K. No significant differences were observed in burst pressure among the four groups (p>0.05). Histological analysis showed more hemorrhage and congestion in the biliary obstruction groups. Supplemented animals exhibited increased collagen formation and less edema and abscess formation.
CONCLUSION:
Vitamin K supplementation attenuated weight loss and improved colonic wound healing in rats.
Wound Healing; Tensile Strength; Vitamin K; Cholestasis; Rats
Introduction
Vitamins are organic substances found in small amounts in food. They participate in various metabolic reactions controlled by enzymes and coenzymes, usually acting as a cofactor11. Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
https://doi.org/10.1590/S0482-5004200600...
.
Vitamin K is an essential cofactor for the carboxylation of specific glutamic acid residues to form gamma-carboxyglutamic acid (Gla)11. Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
https://doi.org/10.1590/S0482-5004200600...
, 22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
. The natural forms of vitamin K include menaquinone (vitamin K2) and phylloquinone (vitamin K1), which is the predominant form found in vegetables and vegetable oils. In healthy fasting subjects, the reference range is 0.15-1.0 mg/L for phylloquinone11. Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
https://doi.org/10.1590/S0482-5004200600...
, 22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
.
The synthesis of active clotting factors II, VII, IX, X and proteins C and S is vitamin K- dependent. In addition, several other vitamin K-dependent proteins are being studied, such as the non-collagenous bone matrix protein osteocalcin11. Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
https://doi.org/10.1590/S0482-5004200600...
, 22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
.
Risk factors for vitamin K deficiency in hospitalized patients include inadequate dietary intake, malabsorption syndromes (especially due to cholestasis), antibiotic therapy, renal failure, liver dysfunction, recent major surgery, and lack of prophylactic supplementation11. Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
https://doi.org/10.1590/S0482-5004200600...
, 22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
.
A 1987 survey conducted over a period of nine years found coagulopathy due to vitamin K deficiency in 42 critically ill hospitalized patients. Of these, half had undergone major surgery 3-12 days before the diagnosis of deficiency, and 62% reported reduced intake of vitamin-containing foods before hospitalization33. Alperin JB. Coagulopathy caused by vitamin K deficiency in critically ill hospitalized patients. JAMA. 1987 Oct 9;258(14):1916-9. doi:10.1001/jama.1987.03400140078028.
https://doi.org/10.1001/jama.1987.034001...
. Standard coagulation tests such as the prothrombin time (PT) and activated partial thromboplastin time (APTT) are widely and readily available, but are insufficient to detect subclinical vitamin deficiency; measurement of the serum concentration of phylloquinone or tests for the detection of decarboxylated factor II (des-gamma carboxyprothrombin, PIVKA-II) are more accurate for this purpose22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
. A small prospective study conducted in 1994 assessed the extent of vitamin K deficiency in patients admitted to hospital with cholestatic jaundice. It was observed that 20% of patients had an increased PT and 60% had subclinical deficiency, as assessed by measurement of serum vitamin K levels44. O'Brien DP, Shearer MJ, Waldron RP, Horgan PG, Given HF. The extent of vitamin K deficiency in patients with colestatic jaundice: a preliminary communication. J R Soc Med. 1994 Jun;87(6):320-2. doi:10.1177/014107689408700607.
https://doi.org/10.1177/0141076894087006...
.
Patients with cholestasis are protected from vitamin K deficiency by prophylactic administration of parenteral preparations of phylloquinone at regular intervals, as liver reserves of this compound are labile and rapidly depleted55. Usui Y, Tanimura H, Nishimura N,Kobayashi N, Okanoue T, Ozawa K. Vitamin K concentration in the plasma and liver of surgical patients. Am J Clin Nutr. 1990 May;51(5):846-52. PMID:2333843.. Vitamin K has not demonstrated toxicity, and all reported adverse reactions are due to the solubilizing vehicle or to other aspects of parenteral administration. Since 2000, the U.S. Food and Drug Administration (FDA) has instructed that adult parenteral multivitamin preparations should provide 150 μg of phylloquinone per day55. Usui Y, Tanimura H, Nishimura N,Kobayashi N, Okanoue T, Ozawa K. Vitamin K concentration in the plasma and liver of surgical patients. Am J Clin Nutr. 1990 May;51(5):846-52. PMID:2333843..
There is evidence that obstructive jaundice contributes to poor outcomes of anastomotic bowel healing66. Biondo-Simões MLP. O processo de cicatrização na icterícia obstrutiva. Icterícia obstrutiva. Medicina (Ribeirão Preto). 1997 Abr/Jun;30:192-7.
7. Arantes VN, Ozawa RY, Fagundes-Pereira WJ, Barbosa AJA, Petroianu A. Influência da icterícia obstrutiva na cicatrização da pele e de anastomose jejunal em ratos. Rev Col Bras Cir. 1999 Sept/Oct;26(5):269-73. doi.org/10.1590/S0100-69911999000500003.
https://doi.org/10.1590/S0100-6991199900...
- 88. Arnaud JP, Humbert W, Eloy MR, Adloff M. Effect of obstructive jaundice on wound healing - An experimental study in rats. Am J Surg. 1981 May;141(5):593-6. PMID:6452826.. In 1997, Brazilian investigators reviewed the literature on the subject and, after presenting data from their own experimental procedure, reported possible mechanisms responsible for failed healing in jaundiced conditions.66. Biondo-Simões MLP. O processo de cicatrização na icterícia obstrutiva. Icterícia obstrutiva. Medicina (Ribeirão Preto). 1997 Abr/Jun;30:192-7.
One hypothesis is that the lack of bile salts affect the absorption of vitamin K, leading to a deficiency in clotting factors. Consequently, there is a delay in thrombin formation, which, in turn, leads to a delay in the polymerization of fibrinogen to fibrin. This difficulty in fibrin formation may explain the delay in the arrival of fibroblasts to the site of scar formation. Thus, interference is to be expected early in the inflammatory stage of the healing process, and extending thereafter so as to delay the entire process.66. Biondo-Simões MLP. O processo de cicatrização na icterícia obstrutiva. Icterícia obstrutiva. Medicina (Ribeirão Preto). 1997 Abr/Jun;30:192-7.
There is a lack of studies confirming this hypothesis and demonstrating a role for vitamin K in the healing of colonic anastomoses in patients with obstructive jaundice.
Obstructive jaundice is often accompanied by many factors, such as malignancy, hypoproteinemia, anemia, hepatic dysfunction, and kidney failure. In addition, several of its components, such as hyperbilirubinemia and accumulation of bile salts, may also interfere with wound healing22. Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
https://doi.org/10.1053/j.gastro.2009.08...
. Experimental studies are the best option to study the influence of perioperative phylloquinone supplementation on colonic healing in the setting of obstructive jaundice, because they allow individualization of these factors. Within this context, the objective of this study is to evaluate the effects of phylloquinone supplementation on wound healing in the left colon of rats with biliary obstruction.
Methods
The research project was approved by the institutional Animal Experimentation Ethics Committee (CEUA) (protocol 42983/2012).
The study sample comprised 16 healthy male Wistar rats (Rattus norvegicus). For 10 days preoperatively, the animals were housed in cages at the UnB School of Health. Standard diet and water were provided ad libitum, and the animals were kept under a 12-hour light/dark cycle. For the purposes of the study, the 16 rats were randomly divided into four groups of four animals each.
Animals in the LK group underwent common bile duct ligation. After seven days, laparotomy was performed with exposure of the left colon and colostomy, followed by bowel suture. Vitamin K1 (0.01 mL subcutaneously once daily) was administered since the 4th day after ligation.
Animals in group L also underwent common bile duct ligation. After seven days, laparotomy was performed with exposure of the left colon and colostomy, followed by bowel suture. No supplementation was provided.
Animals in group M underwent manipulation, but not ligation, of the common bile duct. After seven days, laparotomy was performed with exposure of the left colon and colostomy, followed by bowel suture. No supplementation was provided.
Finally, animals in the MK group underwent manipulation, but not ligation, of the common bile duct. After seven days, laparotomy was performed with exposure of the left colon and colostomy, followed by bowel suture. Vitamin K1 (0.01 mL subcutaneously once daily) was administered since the 4th day after ligation.
General anesthesia was induced with xylazine hydrochloride 14 mg/kg and ketamine 114 mg/kg intramuscularly. Once anesthesia had been achieved, the animals were placed on the operating board in the supine position, with the forelimbs and hindlimbs fixed in abduction. The anterior abdominal wall was shaved and antisepsis performed with povidone-iodine.
The abdominal cavity was accessed via a right subcostal incision 4 cm in length (Figure 1). In the L and KL groups, the common bile duct was identified and ligated with 6-0 nylon thread (Figure 2). In the M and MK groups, the common bile duct was merely manipulated. In both operations, the abdominal wall was closed with double-layer continuous 4-0 nylon sutures. Postoperative analgesia consisted of tramadol 28.5 mg/kg subcutaneously every 12 hours for 48 hours.
Markings (black dots) spaced 4 cm apart to indicate the location of the right subcostal incision.
Seven days after common bile duct ligation or manipulation, the animals were underwent a colostomy followed by bowel suture. General anesthesia was administered in identical fashion to the first operation. Laparotomy was performed via a 4-cm incision starting 1 cm above the external genitalia. After exposure of the left colon, a longitudinal colostomy, 2 cm in length, was created on the antimesenteric border, followed by continuous longitudinal bowel suture with 6-0 nylon (Figure 3).
The abdominal wall was closed in two layers of continuous sutures with 4-0 nylon. Again, postoperative analgesia consisted of tramadol 28.5 mg/kg subcutaneously every 12 hours for 48 hours, with the first dose administered 12 hours after the procedure.
All rats were weighed at two points in time: on the day of colonic surgery and on the day 7 after bowel suture. On the day of euthanasia, the animals were again subjected to general anesthesia and laparotomy for evaluation of the abdominal cavity and left colon.
Measurement of the tensile strength of the left colon wound was performed with the colon in situ as described in a previous publication by Durães at al.99. Durães LC, Durães EF, Freitas PF, Carvalho FA, Carvalho SA, Sousa JB. A new proposal for laparoscopic left colectomy in a rat model. Acta Cir Bras. 2013 Apr;28(4):239-44. doi.org/10.1590/S0102-86502013000400002.
https://doi.org/10.1590/S0102-8650201300...
by measuring the bursting pressure using a Zurich brand Z.10.B manometer on the day of euthanasia. Then, a colon segment containing the wound was resected for histopathological analysis and a blood sample was collected for determination of the serum bilirubin level. The animals were killed by overdose of thiopental.
Histological evaluation of healing was done in blind fashion by an experienced pathologist using optical microscopy after hematoxylin and eosin (H&E) staining. The following parameters were evaluated: collagen, fibroblasts, mononuclear cells, polymorphonuclear cells, hemorrhage, congestion, neovascularization, edema, ulcers, necrosis, abscess, colonies, foreign body, and fibrin crust. The findings were noted as absent or present, and the latter graded as mild (1), moderate (2), or marked (3) in intensity.
Statistical analysis was performed via one-way analysis of variance (ANOVA) to evaluate weights and the Mann-Whitney U test for tensile strength. The significance level (p) for rejecting the null hypothesis was 0.05.
Results
There was an increase in direct bilirubin compared with indirect bilirubin in groups M vs. L (p = 0.02) and KL vs. MK (p = 0.02). In addition, all animals subjected to common bile duct ligation had bilirubin levels above the reference range for Wistar rats (Figure 4).
There was no difference in tensile strength of the colonic segment that underwent bowel suture, whether on comparison of groups L vs. M or of supplemented groups (MK and LK) vs. non-supplemented groups (M and L) (Figure 5).
Histopathological evaluation showed greater collagen formation in the supplemented (LK + MK) vs. non-supplemented (L + M) groups, as well as in LK vs. L animals.
The incidence of hemorrhage and congestion was higher in the groups that underwent common bile duct ligation as compared with groups undergoing manipulation alone, both when analyzing MK vs. LK and M vs. L separately and when pooling groups and comparing LK + L vs. MK + M.
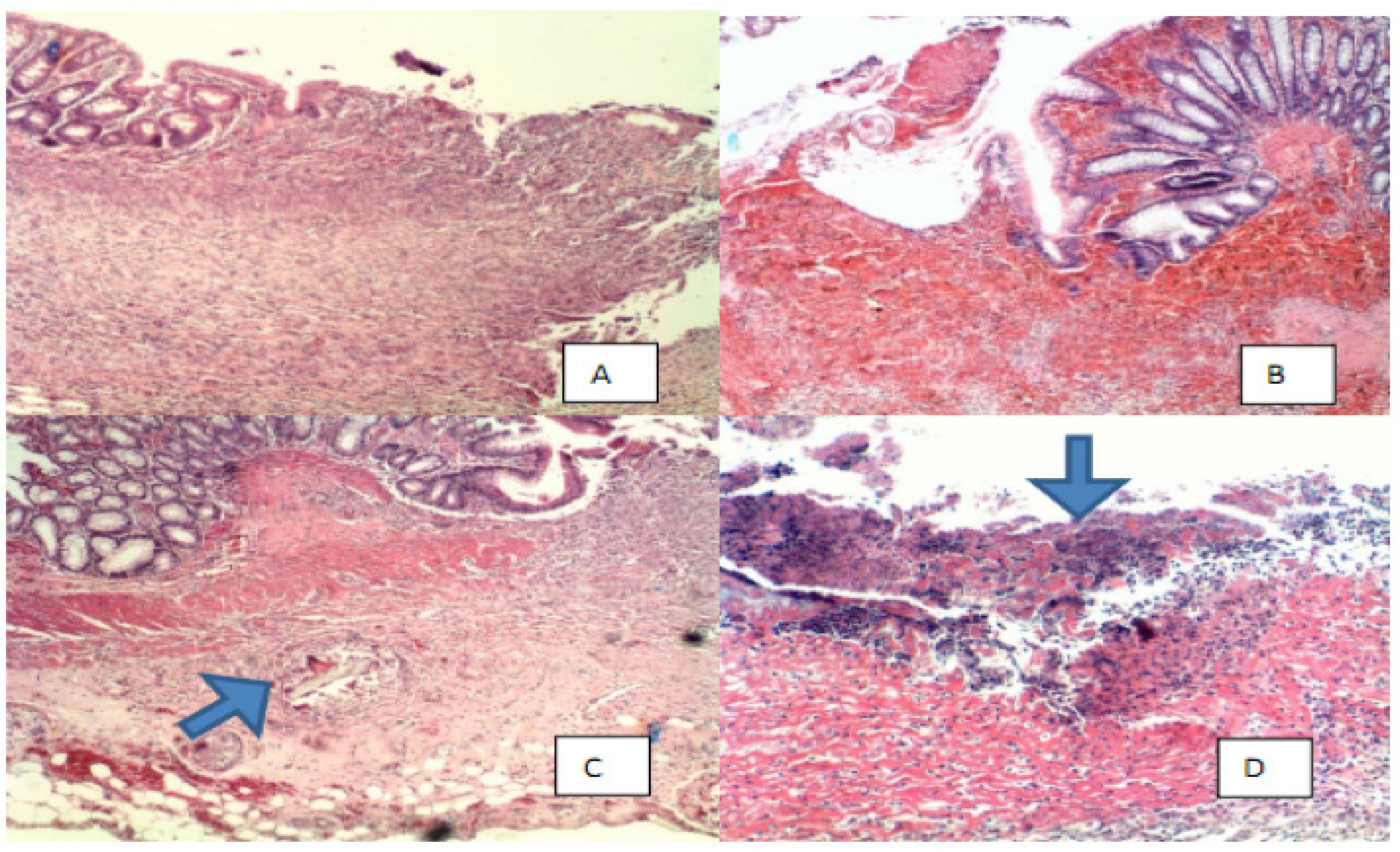
Abscess formation was noticed in all except one animal in the non-supplemented groups, whereas in the supplemented groups, only two rats developed this complication. In the supplemented groups, foreign body formation was observed in all rats, something which was seldom seen in non-supplemented rats (Figure 6).
Photomicrograph of ulcerated mucosa in the area of the scar in A, with hemorrhage in B, granuloma with foreign body (arrow) in C and fibrin crust and bacterial colonies (arrow) in D. HE x100.
Edema was more severe in mice that had not received supplementation than in supplemented ones. The other parameters analyzed (fibroblasts, agranulocytes, granulocytes, neovascularization, ulcers, necrosis, foreign body reaction, fibrin crust, and bacterial colonies) showed no substantial differences between groups (Table 1).
Body weight analysis was performed using measurements acquired at the time of colon surgery and at the time of euthanasia. The ANOVA test for repeated measures was used for analysis of the following values: P group, P effect-time, and P interaction.
The P group determines whether the two variables are significantly different, "P effect-time" determines whether there was a change in variable over time, and the P interaction finds correlation between variables, whether direct or indirect. The variables of interest were body weight in groups L, M, KL, and MK, compared one by one (Table 2).
The LK group and the L group showed significant variation in weight over time (P effect-time); P interaction shows that the supplemented animals experienced less weight loss than non-supplemented animals (Figure 7).
Discussion
There is evidence in the literature that jaundice interferes negatively with the healing process66. Biondo-Simões MLP. O processo de cicatrização na icterícia obstrutiva. Icterícia obstrutiva. Medicina (Ribeirão Preto). 1997 Abr/Jun;30:192-7.
7. Arantes VN, Ozawa RY, Fagundes-Pereira WJ, Barbosa AJA, Petroianu A. Influência da icterícia obstrutiva na cicatrização da pele e de anastomose jejunal em ratos. Rev Col Bras Cir. 1999 Sept/Oct;26(5):269-73. doi.org/10.1590/S0100-69911999000500003.
https://doi.org/10.1590/S0100-6991199900...
- 88. Arnaud JP, Humbert W, Eloy MR, Adloff M. Effect of obstructive jaundice on wound healing - An experimental study in rats. Am J Surg. 1981 May;141(5):593-6. PMID:6452826.. However, this was not evident in the present study when comparing groups L vs. M and LK vs. M, whether on histological analysis or tensile strength analysis of the sutured bowel segment.
Our results did not demonstrate any differences between the jaundiced and non-jaundiced groups, although they do point to a yet-understudied role of vitamin K in the wound healing process. Animals with obstructive jaundice that received vitamin K supplementation exhibited higher collagen formation than animals in the non-supplemented jaundice group, which confirms our initial hypothesis.
Animals in the common bile duct ligation groups had hemorrhage and congestion to a more marked degree than rats that underwent manipulation alone. This evidence suggests that there was in fact a vitamin K deficiency leading to coagulopathy in animals with ligated common bile ducts, causing an increase in the incidence of bleeding and altering the first phase of healing, which is dependent on the proper functioning of hemostatic mechanisms.
Better healing was observed in the supplemented groups (LK and MK) in comparison with the non-supplemented control groups (L and M), as indicated by increased presence of collagen and less abscess and edema formation on histopathological evaluation.
The greater weight gain observed in the supplemented animals suggests a possible interference of vitamin K deficiency on the metabolic response to trauma. Bleeding due to induced coagulopathy may lead to increased catabolism, resulting in weight loss and poor nutritional status. Studies have shown that weight loss and poor nutritional status interfere with colon healing1010. Mäkelä JT, Kiviniemi H, Laitinen S. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003 May;46(5):653-60. doi: 10.1007/s10350-004-6627-9.
https://doi.org/10.1007/s10350-004-6627-...
. Furthermore, weight gain as a marker of improvement in nutritional status is itself a good prognostic factor, associated with low morbidity and mortality and decreased length of stay1111. Windsor JA, Hill GL. Weight loss with physiologic impairment. A basic indicator of surgical risk. Ann Surg. 1988 Mar;207(3):290-6. PMID:3345115..
The vitamins with a classically defined role in healing are vitamins A and C; a possible role of vitamin E in this process is currently being studied1212. Thomas DR. Specific nutritional factors in wound healing. Adv Wound Care. 1997 Jul-Aug;10(4):40-3. PMID: 9306784.. To better define the role of vitamin K in wound healing and metabolic response to trauma, it is desirable that coagulation be evaluated in future studies. This could be done even with simple tests such as the prothrombin time (PT) and serum levels of vitamin K-dependent clotting factors, or by more complex methods such as molecular and immunohistochemical assays.
Conclusion
Vitamin K supplementation attenuated weight loss and improved colonic healing on histopathological evaluation, but had no effects on the tensile strength of the anastomosis.
References
-
1Klack K, Carvalho JF. Vitamina K: metabolismo, fontes e interação com o anticoagulante Varfarina. Rev Bras Reumatol. 2006 Nov/Dez 46(6):398-406. doi.org/10.1590/S0482-50042006000600007.
» https://doi.org/10.1590/S0482-50042006000600007 -
2Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009 Nov;137(5 Suppl):S105-18. doi: 10.1053/j.gastro.2009.08.046.
» https://doi.org/10.1053/j.gastro.2009.08.046 -
3Alperin JB. Coagulopathy caused by vitamin K deficiency in critically ill hospitalized patients. JAMA. 1987 Oct 9;258(14):1916-9. doi:10.1001/jama.1987.03400140078028.
» https://doi.org/10.1001/jama.1987.03400140078028 -
4O'Brien DP, Shearer MJ, Waldron RP, Horgan PG, Given HF. The extent of vitamin K deficiency in patients with colestatic jaundice: a preliminary communication. J R Soc Med. 1994 Jun;87(6):320-2. doi:10.1177/014107689408700607.
» https://doi.org/10.1177/014107689408700607 -
5Usui Y, Tanimura H, Nishimura N,Kobayashi N, Okanoue T, Ozawa K. Vitamin K concentration in the plasma and liver of surgical patients. Am J Clin Nutr. 1990 May;51(5):846-52. PMID:2333843.
-
6Biondo-Simões MLP. O processo de cicatrização na icterícia obstrutiva. Icterícia obstrutiva. Medicina (Ribeirão Preto). 1997 Abr/Jun;30:192-7.
-
7Arantes VN, Ozawa RY, Fagundes-Pereira WJ, Barbosa AJA, Petroianu A. Influência da icterícia obstrutiva na cicatrização da pele e de anastomose jejunal em ratos. Rev Col Bras Cir. 1999 Sept/Oct;26(5):269-73. doi.org/10.1590/S0100-69911999000500003.
» https://doi.org/10.1590/S0100-69911999000500003 -
8Arnaud JP, Humbert W, Eloy MR, Adloff M. Effect of obstructive jaundice on wound healing - An experimental study in rats. Am J Surg. 1981 May;141(5):593-6. PMID:6452826.
-
9Durães LC, Durães EF, Freitas PF, Carvalho FA, Carvalho SA, Sousa JB. A new proposal for laparoscopic left colectomy in a rat model. Acta Cir Bras. 2013 Apr;28(4):239-44. doi.org/10.1590/S0102-86502013000400002.
» https://doi.org/10.1590/S0102-86502013000400002 -
10Mäkelä JT, Kiviniemi H, Laitinen S. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003 May;46(5):653-60. doi: 10.1007/s10350-004-6627-9.
» https://doi.org/10.1007/s10350-004-6627-9 -
11Windsor JA, Hill GL. Weight loss with physiologic impairment. A basic indicator of surgical risk. Ann Surg. 1988 Mar;207(3):290-6. PMID:3345115.
-
12Thomas DR. Specific nutritional factors in wound healing. Adv Wound Care. 1997 Jul-Aug;10(4):40-3. PMID: 9306784.
-
Financial source: National Council for Scientific and Technological Development (CNPq)
-
1
Research performed at Experimental Surgery Laboratory, School of Medicine, University of Brasilia (UnB), Brazil.
Publication Dates
-
Publication in this collection
Aug 2014
History
-
Received
10 Mar 2014 -
Reviewed
12 May 2014 -
Accepted
11 June 2014