Abstract
Purpose:
To establish and evaluate the feasibility of continuous peritoneal lavage with vacuum peritoneostomy in an animal model.
Methods:
Eight pigs aged 3-4 months, females, were anesthetized and submitted to laparotomy and installation of a continuous peritoneal lavage with vacuum peritoneostomy. The sta-bility of the system, the physiological effects of washing with NaCl 0.9% and the sys-tem clearance were evaluated.
Results:
Stability of vacuum peritoneostomy was observed, with no catheter leaks or obstructions and the clearance proved adequate, however, the mean volume of fluids aspirated by the peritoneostomy at the end of the experiment was higher than the volume infused by the catheters (p=0.02). Besides that, the animals presented a progressive increase in heart rate (p=0.04) and serum potassium (p=0.02).
Conclusion:
The continuous peritoneal lavage technique with vacuum peritoneostomy is feasible and presents adequate clearance.
Key words:
Peritonitis; Peritoneal Lavage; Models; Animal; Swine.
Introduction
Peritoneal lavage as an adjuvant in the treatment of diffuse peritonitis has not yet been well established, however, its applicability has been discussed since the beginning of the last century. The disadvantages related to the use of this method are the dissemination of a contaminating focus throughout the cavity, the difficulty removing bacteria ad-hered to the peritoneal mesothelium and the removal of pro-inflammatory factors that would aid in the resolution of intra-abdominal infection11 Platell C, Papadimitriou JM, Hall JC. The influence of lavage on peritonitis. J Am Coll Surg. 2000;191(6):672-80. PMID: 11129818.. Clinical studies do not suggest advantages in the use of peritoneal lavage22 Whiteside OJ, Tytherleigh MG, Thrush S, Farouk R, Galland RB. Intra-operative peritoneal lavage - who does it and why? Ann R Coll Surg Engl. 2005;87:225-8. PMID: 16053685.
3 Torres OJM, Macedo EL, Melo TCM, Costa JVG, Nunes PMS, Viana RMM, Dietz UA. Fecal peritonitis in rats: efficacy of peritoneal lavage with a solution of sodium chloride 0.9%. Acta Cir Bras. 1999;14(2):65-8.
4 Schwarz A, Bölke E, Peiper M, Schulte am Esch J, Steinbach G, van Griensven M, Orth K. Inflammatory peritoneal reaction after perforated appendicitis: con-tinuous peritoneal lavage versus non lavage. Eur J Med Res. 2007;12(5):200-5. PMID: 17513191.-55 Caronna R, Benedetti M, Morelli A, Rocco M, Diana L, Prezioso G, Cardi M, Schiratti M, Martino G, Fanello G, Papini F, Farelli F, Meniconi RL, Marengo M, Dinatale G, Chirletti P. Clinical effects of laparotomy with perioperative continu-ous peritoneal lavage and postoperative hemofiltration in patients with severe acute pancreatitis. World J Emerg Surg. 2009;16;4:45. PMID: 20015376. and the results of studies using animal models are conflicting66 Brocco MC, Gomez RS, Paulo DNS, Almeida CED, Baptista JFA. Histological features of peritoneal lavage with ropivacaine in rats with fecal peritonitis. Acta Cir Bras. 2012;27(2):193-9. PMID: 22378377.
7 Camargo MG, Fagundes JJ, Leal RF, Ayrizono Mde L, Rossi DH, Oliveira Pde S, Chung WF, Lee HD, Coy CS. Influence of the peritoneal lavage with bupivacaine on the survival and resistance of colonic anastomoses performed under fecal peri-tonitis in rats. Acta Cir Bras. 2013;28(11):783-7. PMID: 24316746.-88 Qadan M, Dajani D, Dickinson A, Polk HC Jr. Meta-analysis of the effect of peri-toneal lavage on survival in experimental peritonitis. Br J Surg. 2010;97(2):151-9. PMID: 20069604..
One modality of this technique is continuous peritoneal lavage because continuous intra-abdominal irrigation would aid in the continued removal of infectious and inflammatory particles, helping to resolve peritonitis. However, when analyzing the studies conducted on the technique, it is observed that, in none of them, the lavage system studied provid-ed an adequate clearance mechanism.
Thus, it is believed that continuous peritoneal lavage may still be a solution for the treatment of severe peritonitis, since it would allow peritoneal lavage in the intensive care unit, without the burden of a new surgical procedure. Associating continuous peritoneal lavage with negative pressure peritoneostomy may be an alternative as it could keep a lavage system closed, with the possibility of more efficient infused fluid clearance.
The objectives of this study are to establish and evaluate the feasibility of continuous peritoneal lavage in a closed system using a peritoneostomy with negative pressure in an animal model.
Methods
The experiments were reviewed and approved by the Research Ethics Committee of our institution (protocol n 086/12).
It was used eight female pigs (Landrace) aged between 3-4 months weighing between 30 and 40 kg. Before the experiment, it was guaranteed that each animal had plasma hemoglobin concentration greater than or equal to 9mg / dL, normal values of blood gases and absence of clinical signs of infection.
All animals were handled per the principles of the National Institute of Health (1985) and The American Physiological Society (1995) for the care, handling and use of laboratory animals.
Anesthesia and monitoring
After fasting for 12h and with water on demand, the animals were premedicated with an intramuscular injection of ketamine (5 mg/kg) and midazolam (0.25 mg/kg). Anesthe-sia was induced with intravenous propofol (5mg/kg). They were submitted to orotrache-al intubation and ventilated (Hamilton Medical, Reno, USA) with a tidal volume of 12mL/kg and respiratory rate of 15 incursions/min. Small adjustments were made at the respiratory rate for maintenance of PaCO₂ between 35-45cmH₂O. They were kept anes-thetized with Isoflurane (1.5 vol%) and Pancuronium (5 μg/kg/min) under mechanical ventilation throughout the experiment.
The left carotid artery was catheterized for biochemical analysis, arterial gasometry (Roche Cobras b211, Roche Diagnostics USA) and invasive blood pressure monitoring (MAP). A triple lumen catheter was placed in the right internal jugular vein for infusion of anesthetics and fluids. Quantification of urinary output (UO) and indirect measure-ment of intra-abdominal pressure (IAP) was performed by an intra-bladder Foley catheter.
Continuous peritoneal lavage associated with vacuum peritoneostomy
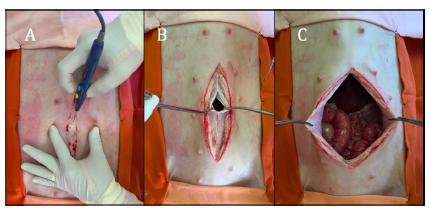
Once established anesthesia, the animals were subjected to laparotomy incision with 20cm and opening of the abdominal wall by planes with the aid of cautery to reach the abdominal cavity (Figure 1).
A. Medium incision, opening with electro-cautery; B. Opening by planes, repaired the peritoneum with Kelly’s forceps; C. Exposure of the abdominal cavity.
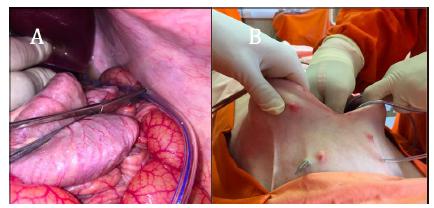
Two 4.8 mm multi-perforated polyvinyl chloride tubes were positioned within the cavi-ty, from the iliac fossa to the costophrenic recess bilaterally. Both tubes were external-ized through another openings inferior to the laparotomy (Figure 2).
A. Tube positioning on left flank; B. Outlet of the tubes by counter-opening in the right iliac fossa.
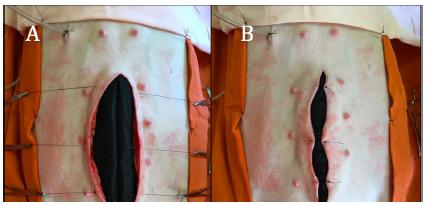
Then, the viscera were covered by a mesh of non-absorbable porous material and a sponge was placed on this screen (Figure 3). The subcutaneous tissue was removed radi-ally throughout the wound and, on the first sponge, the edges of the muscle-aponeurotic complex were approximated with three points using 2-0 mononylon thread, so that the spaces between the edges did not exceed two centimeters (Figure 4).
A. Passing through the edges of the 3-0 mononylon muscle-aponeurotic complex 2-0; B. Approaching the edges with moderate tension.
The detachment of the subcutaneous tissue allowed to accommodate another sponge on the approximate aponeurosis. The edges of the skin and subcutaneous tissue were also approximated with 3 points using 2-0 mononylon thread so the edges also did not ex-ceed two centimeters (Figure 5). The wound was covered with adhesive film and then a suction cup was placed for negative pressure maintenance through an aperture in the impermeable film (Figure 6).
The Vivano® Kit (Hartmann, Heidenheim, Germany) was used in peritoneostomy. Dur-ing washes, the infusion of fluids through the multi-perforated tubes and the aspiration performed by the peritoneostomy suction cup simultaneously (Figure 7).
A. Passing through the edges of the skin 3 wires of 2-0 mononylon; B. Approaching the edges with moderate tension in the mononylon wires.
Fluid inlets through the tubes (blue arrows). Fluid outlet through the tube with perito-neostomy suction cup (red arrow).
Clearance of the abdominal cavity
To determine the efficiency of system clearance, 4 pigs were anesthetized and submitted to the previously described technique. The animals received a solution of 17.5mL of suspension of carbon particles (nanquim) (Acrilex, Sao Bernardo do Campo, Brazil) di-luted in 1.5L of 0.9% NaCl solution.
Then the animals were submitted to negative pressure 125mmHg and peritoneal lavage with NaCl 0.9% to 15mL / min in the two multi-perforated tubes for a period of 120 minutes. Every 15 minutes, a sample of peritoneal lavage was collected. At the end of the 120 minutes, the peritoneostomy was removed and a sample of peritoneal fluid was collected in the right costophrenic recess (RCFR), left costophrenic recess (LCFR), right iliac fossa (RIF) and left iliac fossa (LIF). These samples were submitted to spectropho-tometry with a wavelength of 456nm, to determine their concentration. The absorbance curve versus concentration was calculated with the predetermined dilutions of a nan-quim solution, and the formula for calculating the sample concentrations obtained was calculated: abs = 116.9075 x con - 0.0689 (abs = absorbance, con = concentration).
System stability and physiological effects of washing with NaCl 0.9%
Four other animals were anesthetized and submitted to standard surgical technique. It was infused with NaCl 0.9%, with flow 200ml/h in the two multi-perforated tubes and alternating periods with and without the negative pressure of 125mmHg every 30 minutes, for a period of nine hours.
The peritoneostomy stability was evaluated along with continuous fluid infusion; The resistance of the system to obstructions and leaks and the water balance, as well as the physiological effects evaluated by means of recording hemodynamic parameters (mean arterial pressure, heart rate, intra-abdominal pressure and diuresis) and biochemical pa-rameters (pH, lactate, sodium, potassium and hematocrit), which were collected at the beginning of the procedure, with 3, 6 and 9 hours of follow-up.
Statistical analysis
Data are presented as mean ± standard deviation or median (interquartile range) when appropriate. Statistical analysis was performed using the program SigmaStat for Win-dows. The paired Wilcoxon test was performed for comparison between biochemical and hemodynamic variables at the beginning and at the end of the procedure.
Results
Clearance of the abdominal cavity
The analysis of the peritoneal lavage samples collected every 15 minutes showed a pro-gressive reduction in the concentration of nanquim, which was verified in all animals evaluated.
The percentage of the concentration found after 120 minutes in LIF, RCFR, LCFR, and RIF was 4.1%, 10.0%, 8.5% and 7%, 56% respectively.
System stability and physiological effects of washing with 0.9% NaCl solution
The stability of vacuum peritoneostomy, along with a continuous infusion of fluids, was maintained throughout the experiment, with no catheter leaks or obstructions. When the aspiration was interrupted, there were no significant oscillations in the intra-abdominal pressure, but it was observed that the mean volume of fluids aspirated by the peritone-ostomy at the end of the experiment was higher than the volume infused by the cathe-ters (5517.5±1052.53mL vs. 3700±200mL, p=0.02). During the 9-hour procedure, no significant oscillations were observed in MAP, however, there was a progressive in-crease in HR (Table 1). Hydroelectrolytic changes were also observed, such as progres-sive increase of serum potassium (Table 2).
Discussion
Continuous peritoneal lavage as a method of treating abdominal sepsis is technically difficult and has controversial results99 van Goor H. Interventional management of abdominal sepsis: when and how. Langenbecks Arch Surg. 2002;387(5-6):191-200. PMID: 12410353.. The concept of the technique is based on the hy-pothesis that continuous irrigation of the abdominal cavity increases the removal of con-taminants and inflammatory mediators, aiding in the Resolution of infectious disease11 Platell C, Papadimitriou JM, Hall JC. The influence of lavage on peritonitis. J Am Coll Surg. 2000;191(6):672-80. PMID: 11129818.. However, the current mechanisms used for continuous peritoneal lavage appear to be unable to exert adequate clearance of contaminants and inflammatory mediators.
It is believed that most previously used peritoneal lavage methods use the same lavage infusion route to aspirate the lavage, causing technical problems such as leakage, early clogging of the catheters, contamination, and infection of the undrained volume. More-over, in these techniques, the abdominal wall is kept closed, which induces an increase in intra-abdominal pressure and, consequently, hemodynamic changes. The unfavorable results ended up indicating the abandonment of the technique in the treatment of dif-fuse peritonitis.
Still in the 1990s, some authors10,11 proposed peritoneal lavage techniques that used dif-ferent infusion and aspiration routes, but due to the complexity of both, were not men-tioned in other studies or protocols and were probably abandoned.
Continuous peritoneal lavage presents several technical difficulties, including mainte-nance of system integrity, maintenance of the abdominal cavity isolated from the exter-nal environment, and efficient aspiration of the infused lavage fluids.
Peritoneostomy, using abdominal wall retention techniques, avoids abdominal wall retraction1212 Pliakos I, Papavramidis TS, Mihalopoulos N, Koulouris H, Kesisoglou I, Sapalidis K, Deligiannidis N, Papavramidis S. Vacuum-assisted closure in severe abdominal sepsis with or without retention sutured sequential fascial closure: a clinical trial. Surgery. 2010;148(5):947-53. PMID: 20227097.. This technique, applied to continuous peritoneal lavage, promotes greater stability of the system, avoiding leaks that may lead to discontinuity of the whole.
Another important aspect is the lavage associated with the peritoneostomy. This ap-proach increases the compliance of the abdominal cavity, maintaining normal values of intra-abdominal pressure, despite the volume added to the cavity with the lavage. Previ-ously used washing methods maintain the closed cavity with the suture of the aponeuro-sis, contributing to increase intra-abdominal pressure and development of abdominal compartment syndrome99 van Goor H. Interventional management of abdominal sepsis: when and how. Langenbecks Arch Surg. 2002;387(5-6):191-200. PMID: 12410353..
The clearance developed by the system is another interesting aspect of this model. Pre-vious studies have reported that inefficiency in aspirating lavage fluid is one of the main problems of continuous peritoneal lavage in previous techniques and is a reason for not recommending the method99 van Goor H. Interventional management of abdominal sepsis: when and how. Langenbecks Arch Surg. 2002;387(5-6):191-200. PMID: 12410353.. The continuous peritoneal lavage model associated with vacuum peritoneostomy is efficient in performing abdominal fluid clearance. The results of the evaluation with suspended carbon particles demonstrate the ability of the system to remove such particles dispersed by the abdominal cavity, such that in 120 minutes of washing it was possible to reduce the concentration of nanquim in the cavity recesses by approximately 90%.
The fluid used seems to be another important factor. The 0.9% NaCl solution was cho-sen based on the usual practice of surgeons washing the abdominal cavity with large volumes of saline to remove contaminating particles. However, studies suggest that the use of saline may be harmful to the peritoneal mesothelium1313 Breborowicz A, Oreopoulos DG. Is normal saline harmful to the peritoneum? Perit Dial Int. 2005;25 Suppl 4:S67-70. PMID: 16300274.,1414 Polubinska A, Winckiewicz M, Staniszewski R, Breborowicz A, Oreopoulos DG. Time to reconsider saline as the ideal rinsing solution during abdominal surgery. Am J Surg. 2006;192(3):281-5. PMID: 16920418., may promote the for-mation of peritoneal adhesions1515 Cwalinski J, Staniszewski R, Baum E, Jasinski T, Mackowiak B, Breborowicz A. Normal saline may promote formation of peritoneal adhesions. Int J Clin Exp Med. 2015 Jun 15;8(6):8828-34. PMID: 26309535., as well causing electrolyte disturbances99 van Goor H. Interventional management of abdominal sepsis: when and how. Langenbecks Arch Surg. 2002;387(5-6):191-200. PMID: 12410353.. In this study, it was also observed negative water balance, hemodynamic changes, progressive increase in HR and biochemical changes such as the progressive increase of serum potassium.
This study demonstrates how the continuous peritoneal lavage model associated with vacuum peritoneostomy solves the problems encountered in previous peritoneal lavage attempts. This model can keep the lavage system stable for nine hours without clogging or leaking. However, further studies should be conducted with additional wash fluid options aimed at maintaining homeostasis during the wash period before using in clinical studies as a therapeutic option for diffuse peritonitis.
Conclusions
The continuous peritoneal lavage technique with vacuum peritoneostomy is feasible and presents adequate clearance.
References
-
1Platell C, Papadimitriou JM, Hall JC. The influence of lavage on peritonitis. J Am Coll Surg. 2000;191(6):672-80. PMID: 11129818.
-
2Whiteside OJ, Tytherleigh MG, Thrush S, Farouk R, Galland RB. Intra-operative peritoneal lavage - who does it and why? Ann R Coll Surg Engl. 2005;87:225-8. PMID: 16053685.
-
3Torres OJM, Macedo EL, Melo TCM, Costa JVG, Nunes PMS, Viana RMM, Dietz UA. Fecal peritonitis in rats: efficacy of peritoneal lavage with a solution of sodium chloride 0.9%. Acta Cir Bras. 1999;14(2):65-8.
-
4Schwarz A, Bölke E, Peiper M, Schulte am Esch J, Steinbach G, van Griensven M, Orth K. Inflammatory peritoneal reaction after perforated appendicitis: con-tinuous peritoneal lavage versus non lavage. Eur J Med Res. 2007;12(5):200-5. PMID: 17513191.
-
5Caronna R, Benedetti M, Morelli A, Rocco M, Diana L, Prezioso G, Cardi M, Schiratti M, Martino G, Fanello G, Papini F, Farelli F, Meniconi RL, Marengo M, Dinatale G, Chirletti P. Clinical effects of laparotomy with perioperative continu-ous peritoneal lavage and postoperative hemofiltration in patients with severe acute pancreatitis. World J Emerg Surg. 2009;16;4:45. PMID: 20015376.
-
6Brocco MC, Gomez RS, Paulo DNS, Almeida CED, Baptista JFA. Histological features of peritoneal lavage with ropivacaine in rats with fecal peritonitis. Acta Cir Bras. 2012;27(2):193-9. PMID: 22378377.
-
7Camargo MG, Fagundes JJ, Leal RF, Ayrizono Mde L, Rossi DH, Oliveira Pde S, Chung WF, Lee HD, Coy CS. Influence of the peritoneal lavage with bupivacaine on the survival and resistance of colonic anastomoses performed under fecal peri-tonitis in rats. Acta Cir Bras. 2013;28(11):783-7. PMID: 24316746.
-
8Qadan M, Dajani D, Dickinson A, Polk HC Jr. Meta-analysis of the effect of peri-toneal lavage on survival in experimental peritonitis. Br J Surg. 2010;97(2):151-9. PMID: 20069604.
-
9van Goor H. Interventional management of abdominal sepsis: when and how. Langenbecks Arch Surg. 2002;387(5-6):191-200. PMID: 12410353.
-
10Dittrich K, Kriwanek S, Armbruster C. Dorso-ventral continuous irrigation using the Incise Pouch. Langenbecks Arch Chir. 1993;378(3):185-7. PMID: 8326812.
-
11Losanoff J, Kjossev K. Palisade dorsoventral lavage for neglected Peritonitis. Am J Surg 1997;173:134-5. PMID: 9074380.
-
12Pliakos I, Papavramidis TS, Mihalopoulos N, Koulouris H, Kesisoglou I, Sapalidis K, Deligiannidis N, Papavramidis S. Vacuum-assisted closure in severe abdominal sepsis with or without retention sutured sequential fascial closure: a clinical trial. Surgery. 2010;148(5):947-53. PMID: 20227097.
-
13Breborowicz A, Oreopoulos DG. Is normal saline harmful to the peritoneum? Perit Dial Int. 2005;25 Suppl 4:S67-70. PMID: 16300274.
-
14Polubinska A, Winckiewicz M, Staniszewski R, Breborowicz A, Oreopoulos DG. Time to reconsider saline as the ideal rinsing solution during abdominal surgery. Am J Surg. 2006;192(3):281-5. PMID: 16920418.
-
15Cwalinski J, Staniszewski R, Baum E, Jasinski T, Mackowiak B, Breborowicz A. Normal saline may promote formation of peritoneal adhesions. Int J Clin Exp Med. 2015 Jun 15;8(6):8828-34. PMID: 26309535.
-
Financial source:
none
-
1
Research performed at Laboratory of Surgical Physiopathology (LIM-62), School of Medicine, Universidade de São Paulo (USP), Brazil.
Publication Dates
-
Publication in this collection
June 2017
History
-
Received
14 Feb 2017 -
Reviewed
15 Apr 2017 -
Accepted
18 May 2017