Abstracts
OBJECTIVE: To evaluate the effects of chest physiotherapy in hospitalized patients with bronchiolitis. METHODS: The study included 29 patients younger than one year, diagnosed with acute bronchiolitis, without uncorrected congenital heart disease, neuropathy, lung pathology or need of mechanical ventilation, from March to July 2009. The opinion of the parents or guardians was evaluated using a questionnaire about the clinical condition of the patient before and after the first session of chest physiotherapy. Airway clearance techniques, such as postural drainage, manual percussion, vibration, acceleration of expiratory flow and tracheal suction were applied. The evaluation was performed daily by physical examination prior to physiotherapy and 15 to 45 minutes later, following a specific form. The outcomes observed were: changes of oxygen support, clinical signs (pulmonary auscultation, presence of retractions, oxygenation and severity classification by Downes score) and symptoms (difficulty in sleeping and in feeding, decreased activities, nasal obstruction and constant cough). RESULTS: Among the 29 patients evaluated, a significant improvement was noticed in the following signs and symptoms: pulmonary auscultation with adventitious sounds - general (p<0.001), rales (p=0.017) and wheezes (p=0.010); retractions - general (p<0.001) and intercostal retraction (p<0.001); severity of Downes Score (p<0.001). A significant improvement was also noted in all aspects evaluated in the questionnaire (p<0.001). CONCLUSIONS: Chest physiotherapy lead to a significant short term improvement in infants with bronchiolitis.
bronchiolitis; physical therapy department; hospital; pediatrics
OBJETIVO: Avaliar os efeitos da fisioterapia em pacientes pediátricos, internados com bronquiolite. MÉTODOS: O estudo incluiu 29 pacientes menores de um ano, com diagnóstico médico de bronquiolite aguda, sem cardiopatia congênita não corrigida, neuropatia, doença pulmonar de base ou que necessitassem de suporte ventilatório, no período de março a julho de 2009. Foi avaliada, por meio de questionário, a opinião dos pais ou responsáveis acerca das condições clínicas do paciente antes e após a primeira sessão de fisioterapia. Foram realizadas manobras de desobstrução brônquica, como drenagem postural, tapotagem, vibração, aceleração de fluxo expiratório e aspiração nasotraqueal. A avaliação foi realizada diariamente por meio de exame físico antes do atendimento fisioterapêutico e 15 a 45 minutos após, seguindo uma ficha específica. Os desfechos analisados foram: modificações do suporte de oxigênio, sinais clínicos (ausculta pulmonar, presença de tiragens, oxigenação e classificação da gravidade pelo escore de Downes) e sintomas (inapetência, hipoatividade, dificuldade para dormir, obstrução nasal e tosse constante). RESULTADOS: Dos 29 pacientes avaliados, houve melhora significativa nos seguintes sinais e sintomas: ausculta pulmonar com ruídos adventícios (p<0,001), estertores subcrepitantes (p=0,017) e sibilos (p=0,010), tiragens de modo geral (p<0,001), tiragem intercostal (p<0,001) e classificação da gravidade pelo escore de Downes (p<0,001). Também foi observada melhora significativa em todos os aspectos avaliados no questionário (p<0,001). CONCLUSÕES: A fisioterapia respiratória promoveu uma melhora significante em curto prazo das condições clínicas dos pacientes com bronquiolite aguda.
bronquiolite; serviço hospitalar de fisioterapia; pediatria
OBJETIVO: Evaluar los efectos de la fisioterapia en pacientes pediátricos, internados con bronquiolitis. MÉTODOS: El estudio incluyó a 29 pacientes con menos de 1 año, con el diagnóstico médico de bronquiolitis aguda, sin cardiopatía congénita no corregida, neuropatía, enfermedad pulmonar de base o que necesitaran de soporte ventilatorio en el periodo de marzo a julio de 2009. Se evaluó, mediante cuestionario, la opinión de los padres o responsables, sobre las condiciones clínicas del paciente antes y después de la primera sesión de fisioterapia. Se realizaron maniobras de desobstrucción brónquica, tales como drenaje postural, clapping, vibración, aceleración de flujo espiratorio y aspiración nasotraqueal. La evaluación fue realizada diariamente mediante examen físico antes de la atención fisioterapéutica y 15 a 45 minutos después, siguiendo una ficha específica. Los desenlaces analizados fueron: modificaciones del soporte de oxígeno, señales clínicas (ausculta pulmonar, presencia de tirajes, oxigenación y clasificación de la gravedad por el Escore de Downes) y síntomas (inapetencia, hipoactividad, dificultad en dormir, obstrucción nasal y tos constante). RESULTADOS: De los 29 pacientes evaluados, hubo mejora significativa en los signos y síntomas a continuación: ausculta pulmonar con ruidos adventicios (p<0,001), estertores subcrepitantes (p=0,017) y silbidos (p=0,010), tirajes de modo general (p<0,001), tiraje intercostal (p<0,001) y clasificación de la gravedad por el Escore de Downes (p<0,001). Se observó además mejora significativa en todos los aspectos evaluados en el cuestionario (p<0,001). CONCLUSIONES: Se concluyó que la fisioterapia respiratoria promovió una mejora significante en corto plazo de las condiciones críticas de los pacientes con bronquiolitis aguda.
Bronquiolitis; servicio hospitalar de fisioterapia; pediatría.
ORIGINAL ARTICLE
Giselle de CastroI; Renata RemondiniI; Adriana Zamprônio dos SantosIII; Cristiane do PradoIV
Instituição: Departamento Materno-Infantil do Hospital Israelita Albert Einstein (HIAE), São Paulo, SP, Brasil
IEspecialista em Fisioterapia Respiratória Pediátrica pelo Instituto da Criança do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (USP); Fisioterapeuta do Departamento Materno-Infantil do HIAE, São Paulo, SP, Brasil
IIEspecialista em Fisioterapia Cardiorrespiratória pelo Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da USP; Fisioterapeuta do Departamento Materno-Infantil do HIAE, São Paulo, SP, Brasil
IIIEspecialista em Fisioterapia Respiratória pela Universidade Adventista de São Paulo (Unasp); Fisioterapeuta do Departamento Materno-Infantil do HIAE, São Paulo, SP, Brasil
IVEspecialista em Fisioterapia Respiratória e Fisiologia do Exercício pela Universidade Federal de São Paulo (Unifesp); Coordenadora do Serviço de Fisioterapia do Departamento Materno-Infantil do HIAE, São Paulo, SP, Brasil
Endereço para correspondência
ABSTRACT
OBJECTIVE: To evaluate the effects of chest physiotherapy in hospitalized patients with bronchiolitis.
METHODS: The study included 29 patients younger than one year, diagnosed with acute bronchiolitis, without uncorrected congenital heart disease, neuropathy, lung pathology or need of mechanical ventilation, from March to July 2009. The opinion of the parents or guardians was evaluated using a questionnaire about the clinical condition of the patient before and after the first session of chest physiotherapy. Airway clearance techniques, such as postural drainage, manual percussion, vibration, acceleration of expiratory flow and tracheal suction were applied. The evaluation was performed daily by physical examination prior to physiotherapy and 15 to 45 minutes later, following a specific form. The outcomes observed were: changes of oxygen support, clinical signs (pulmonary auscultation, presence of retractions, oxygenation and severity classification by Downes score) and symptoms (difficulty in sleeping and in feeding, decreased activities, nasal obstruction and constant cough).
RESULTS: Among the 29 patients evaluated, a significant improvement was noticed in the following signs and symptoms: pulmonary auscultation with adventitious sounds - general (p<0.001), rales (p=0.017) and wheezes (p=0.010); retractions - general (p<0.001) and intercostal retraction (p<0.001); severity of Downes Score (p<0.001). A significant improvement was also noted in all aspects evaluated in the questionnaire (p<0.001).
CONCLUSIONS: Chest physiotherapy lead to a significant short term improvement in infants with bronchiolitis.
Key-words: bronchiolitis; physical therapy department, hospital; pediatrics.
RESUMEN
OBJETIVO: Evaluar los efectos de la fisioterapia en pacientes pediátricos, internados con bronquiolitis.
MÉTODOS: El estudio incluyó a 29 pacientes con menos de 1 año, con el diagnóstico médico de bronquiolitis aguda, sin cardiopatía congénita no corregida, neuropatía, enfermedad pulmonar de base o que necesitaran de soporte ventilatorio en el periodo de marzo a julio de 2009. Se evaluó, mediante cuestionario, la opinión de los padres o responsables, sobre las condiciones clínicas del paciente antes y después de la primera sesión de fisioterapia. Se realizaron maniobras de desobstrucción brónquica, tales como drenaje postural, clapping, vibración, aceleración de flujo espiratorio y aspiración nasotraqueal. La evaluación fue realizada diariamente mediante examen físico antes de la atención fisioterapéutica y 15 a 45 minutos después, siguiendo una ficha específica. Los desenlaces analizados fueron: modificaciones del soporte de oxígeno, señales clínicas (ausculta pulmonar, presencia de tirajes, oxigenación y clasificación de la gravedad por el Escore de Downes) y síntomas (inapetencia, hipoactividad, dificultad en dormir, obstrucción nasal y tos constante).
RESULTADOS: De los 29 pacientes evaluados, hubo mejora significativa en los signos y síntomas a continuación: ausculta pulmonar con ruidos adventicios (p<0,001), estertores subcrepitantes (p=0,017) y silbidos (p=0,010), tirajes de modo general (p<0,001), tiraje intercostal (p<0,001) y clasificación de la gravedad por el Escore de Downes (p<0,001). Se observó además mejora significativa en todos los aspectos evaluados en el cuestionario (p<0,001).
CONCLUSIONES: Se concluyó que la fisioterapia respiratoria promovió una mejora significante en corto plazo de las condiciones críticas de los pacientes con bronquiolitis aguda.
Palabras clave: Bronquiolitis; servicio hospitalar de fisioterapia; pediatría.
Introduction
Acute bronchiolitis is one of the most common diseases of the respiratory system, affecting newborns, infants, and children up to 3 years old. This disease is more prevalent during the first six months of life, especially among preterm newborns, often leading to the need for hospitalization. Acute bronchiolitis is a seasonal disease, and it becomes an epidemic in the fall and winter months. Acute respiratory infections are important causes of morbidity and mortality, particularly in developing countries(1-3).
Acute bronchiolitis may have several different clinical manifestations, such as coryza, fever, cough, and wheezing(4). Chest X-ray usually shows hyperinflation, coarse infiltrates, and peribronchial cuffing(1). Some scales are able to assess the severity of bronchiolitis based on the analysis of clinical variables, such as the Wood-Downes-Ferres scale, which classifies the disease as mild (1-3 points), moderate (4-7 points) or severe (8 to 14 points). The items analyzed (wheezing, retraction, respiratory rate, heart rate, ventilation, and cyanosis) are scored from 0 to 3, depending on the presence and intensity of the items(5).
The treatment of acute bronchiolitis remains controversial. It includes hydration, oxygenation, respiratory physiotherapy, and medications such as bronchodilators, epinephrine, mucolytic drugs, and inhaled corticosteroids(1,6,7). Respiratory physiotherapy has been used in patients with acute bronchiolitis in order to achieve bronchial clearing, lung deflation, and alveolar recruitment by means of various techniques, such as positioning, expiratory flow acceleration, manual vibration, tapping, and aspiration of the airways(8,9). Three studies have reported beneficial effects of these techniques in patients with acute bronchiolitis(1,2).
Children hospitalized for bronchiolitis are at high risk of pulmonary sequelae, mainly characterized by cough and recurrent wheezing, which may lead to a larger number of emergency room visits and even multiple hospitalizations(4). Some authors do not recommend respiratory physiotherapy during the acute phase of bronchiolitis because bronchial hygiene techniques make children agitated, thereby increasing hypoxia and, occasionally, bronchospasm(10,11). There are even reports of rib fractures due to the intensity of bronchial hygiene techniques(12). Conversely, other authors believe that respiratory physiotherapy is beneficial in these children because it promotes decreased length of hospital stay and avoids the need for ventilatory support(2,7).
It is important to analyze the physical therapy intervention in infants with bronchiolitis, using appropriate techniques according to patient's age and collaboration during the procedures. The guidelines are essential for proper clinical progress during the disease course in terms of appropriate positioning and stimulation of mucus clearance. Thus, further studies are necessary to assess the effects of respiratory physiotherapy in patients with acute bronchiolitis.
The objective of the present study was to evaluate the effects of respiratory physiotherapy in newborns and infants with acute bronchiolitis during hospitalization before and after physical therapy intervention using expiratory flow acceleration, tapping, manual vibration, nasotracheal aspiration, and positioning. The following outcomes were analyzed: changes in cardiorespiratory parameters (oxygen support, lung auscultation, presence of retractions, peripheral oxygen saturation, and Downes score) and parents or guardians' opinion regarding physiotherapy.
Method
The present study evaluated newborns and infants with acute bronchiolitis hospitalized at the pediatric ward, pediatric semi-intensive care unit, and pediatric intensive care unit of a private hospital from March to July 2009. We selected male and female infants up to 1 year old with acute bronchiolitis. Patients with uncorrected congenital heart disease, neuropathy, any underlying lung disease, or requiring ventilatory support were excluded.
Patients underwent daily assessment by means of physical examination before the physiotherapy session and 15 to 45 minutes after the procedure, according to a pre-defined evaluation form. The form included data on oxygen therapy, lung auscultation with adventitious sounds, subcrepitant rale, crackling, wheezing, and snoring, presence of general retractions, nasal flaring, intercostal retraction, subdiaphragmatic retraction, and sternal retraction, as well as peripheral oxygen saturation (SpO2) and classification of bronchiolitis according to Downes score. The first evaluation before the physical therapy session was conducted by the physical therapist who delivered the treatment. The second evaluation, 15 to 45 minutes after the session, was conducted by another physical therapist to avoid possible biases regarding the analysis of the response.
The physical therapy session consisted of positioning, expiratory flow acceleration, tapping, manual vibration, and nasotracheal aspiration, each procedure lasting for approximately 10 minutes each technique (duration of therapy session: 40 to 50 minutes), based on the patient's need. The number of sessions was determined according to the clinical picture of each child and the number of hospitalization days.
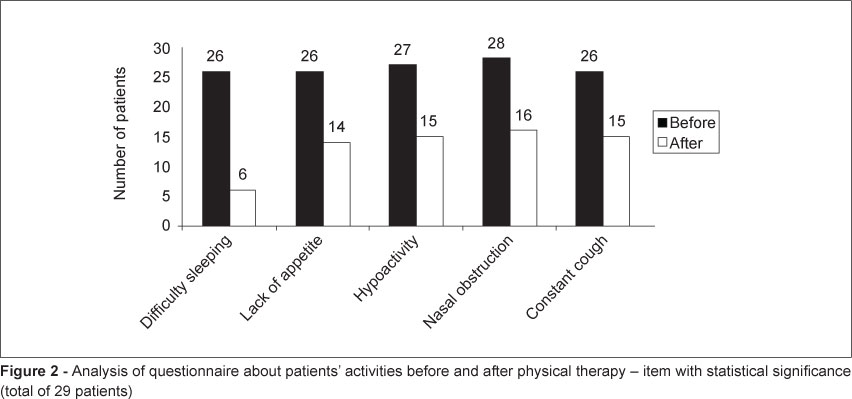
A questionnaire was administered to the children's parents and guardians before and after the first session of physiotherapy. This questionnaire evaluated the short-term effects of the therapy on the patients using the following multiple choice questions: "Does the child have trouble sleeping?" "Does the child have poor appetite?", "Is the child underactive?", "Does the child have nasal obstruction?" and "Does the child cough constantly?". Each question was answered using the "Yes" or "No" options.
Follow-up was performed after the parents or guardians provided consent by signing an informed consent form. The procedures performed in the present study were approved by the Research Ethics Committee at Hospital Israelita Albert Einstein - CEP/Einstein.
The patients' age was expressed as mean, standard deviation (minimum and maximum), while sex was expressed as absolute frequencies. The signs and symptoms evaluated before and after the physical therapy sessions and the questionnaire items were expressed as absolute frequencies and percentages. The comparison between the signs and symptoms before and after the sessions was performed using generalized estimating equation - GEE models(13) in order to consider the dependence between the therapy sessions provided to the same patient. In relation to the questionnaire items, the comparison was made using the McNemar's test. All analyses were performed considering a significance level of 5% and using the statistical computer program SPSS (version 17.0, SPSS Inc, Chicago, Ill).
Results
Of the 29 patients, 16 were female and 13 were male. Only four had a history of morbidity (1 bronchospasm, 1 bronchiolitis, 1 meningitis, and 1 preterm birth). Their mean age was 4.6 months (SD=3 months), ranging from 16 days to 9 months.
In the comparisons related to the signs and symptoms observed during 97 physical therapy sessions, there was significant improvement in six out of the 13 items evaluated. These items were: lung auscultation with adventitious sounds (subcrepitant rale and wheezes), intercostal retractions, and Downes score (Figure 1).
In the evaluation of lung auscultation, in the 92 sessions during which there was adventitious sounds, 13 patients did not present with such symptom after physiotherapy. Among the five patients who did not have adventitious sounds, two showed worsening regarding this symptom. Of the 47 patients who had retractions, 26 did not present with this symptom after therapy. However, of the 50 patients who did not have retraction, eight had this symptom after treatment. In relation to Downes score, of the 56 patients who had a mild score, four increased to a moderate score. A moderate score was found in 40 patients, and 20 of them reached a mild score. The only patient who had a severe score before the therapy achieved a mild score after the treatment (Table 1).
On one hand, of the 21 patients who were treated with oxygen therapy, seven had this therapy discontinued. On the other hand, of the 76 who did not receive oxygen therapy, three needed O2 support after the respiratory physiotherapy. Of the 9 patients with poor oxygenation (considering optimal SpO2 ³93%), six showed improvement. However, of the 88 who had optimal SpO2, nine showed worsening. In spite of the changes we found, there was no statistically significant difference in relation to oxygen therapy and SpO2.
The five symptoms assessed in the questionnaire were present in most patients. Figure 2 shows that there was improvement in all items with a significant reduction in the number of patients with symptoms. "Difficulty sleeping" showed the highest significance (of the 26 patients who had this symptom before the therapy, only six still had this difficulty after the physical therapy sessions). It is noteworthy to mention that the item "constant cough" was the only one showing worsening (Table 2) even though it had the second highest percentage of patients who improved. However, this occurred only in two patients.
Discussion
The pathophysiological characteristics of acute bronchiolitis are accumulation of mucus in the airways, obstruction and collapse of alveoli, and lung hyperinflation(1). Infants with acute viral bronchiolitis have adventitious sounds on lung auscultation due to inflammation in the lower airways, as well as accumulation of mucus and material detached from the respiratory mucosa(14). Clinical manifestations such as tachypnea, mild and moderate hypoxia, and signs of respiratory discomfort (nasal flaring and retractions of accessory muscles of respiration - intercostal and subcostal) are common in patients with acute viral bronchiolitis. Patients may also have cough, fever, coryza, adventitious sounds on lung auscultation (wheezes, crackles or snoring), decreased chest expansion and prolonged expiratory phase(1,15,16). Based on this context, we decided to conduct a study regarding the treatment with respiratory physiotherapy in order to confirm or refute the findings from the literature.
In the present study, we found significant improvement in terms of the presence of retractions after respiratory physiotherapy, especially regarding intercostal retractions. In relation to subdiaphragmatic retraction, two patients did not have it before the physical therapy sessions, but showed this type of retraction after the therapy. The American Academy of Pediatrics, in a review of randomized clinical trials involving cohorts and case-controls found in the literature, designed levels of recommendation for the therapeutic resources used in bronchiolitis and concluded that the respiratory physiotherapy should not be used as a routine treatment because it increases the level of stress in children. However, it has been suggested that physical therapy in children with bronchiolitis is able to open the airways, removing mucus and preventing atelectasis(16-18). According to Carvalho et al, respiratory physiotherapy may be indicated throughout the course of bronchiolitis because it provided bronchial clearing, lung deflation, and alveolar recruitment(1).
In the present study, there was improvement of lung auscultation after physiotherapy in most patients, especially in relation to subcrepitant rale and wheezing. In 2008, Lanza et al found that the use of respiratory physiotherapy in patients hospitalized for bronchiolitis caused a reduction in respiratory distress, greater amount of aspirated mucus, and qualitative improvement in lung auscultation after vibrocompression and tapping(14). In a study involving 12 infants with obstructive breathing pattern, Postiaux also reported a significant reduction in wheezing after inhalation of bronchodilators, especially when combined with physical therapy maneuvers, since wheezing was caused by excessive mucus(16,19). In the studies by Webb et al, Nicholas et al and Bohe et al, patients with bronchiolitis did not benefit from the physical therapy techniques used (postural drainage, tapping, and vibration). Conversely, in French studies, in addition to the techniques of percussion and vibration, expiratory flow acceleration, in particular, proved to be effective for removing mucus. Therefore, respiratory physiotherapy was recommended in a consensus for the management and treatment of bronchiolitis(15,20-22).
Luisi demonstrated that although there is no direct evidence demonstrating the benefits of respiratory physiotherapy in patients with bronchiolitis, bronchial hygiene and alveolar recruitment techniques are used to treat this disease in health care facilities around the world. Respiratory physiotherapy has been used for bronchial clearance and hygiene, prevention of atelectasis and alveolar recruitment, since it provides reduced airway resistance, promoting better ventilation-perfusion and, consequently, diminishing the respiratory work by removing excessive mucus from the airways(15).
Perrotta et al mentioned the study by Postiaux (2006), which showed that there is no scientific evidence confirming the efficacy of respiratory physiotherapy in neonates and infants with bronchiolitis; however, the use of a score based on clinical signs could help to support the clearance techniques in these patients(9,23). In the present study, we used the Wood-Downes-Ferres(5) scale, which classifies the disease as mild, moderate or severe. We found clear evidence of the clinical improvement after physiotherapy in the patients who had moderate and severe Downes score.
In the analysis of the questionnaire, there was significant improvement in various items, including "difficulty sleeping", "lack of appetite", "hypoactivity," "nasal obstruction", and "constant cough" after the physical therapy session, because pulmonary hypersecretion directly affects the items assessed. Currently there are not many studies in the literature demonstrating the qualitative benefit of respiratory physiotherapy in patients with bronchiolitis. In contrast, in the clinical practice, there is an increasing number of prescriptions of respiratory physiotherapy for infants with bronchiolitis, mainly to reduce pulmonary complications(16). Some authors have suggested that children with mild respiratory distress and who have normal appetite should only be observed. However, those who have significant respiratory distress with feeding difficulties, risk of reflux and bronchoaspiration, and increased upper airway edema should be treated with hydration and oral nasal aspiration(17,18). Based on our findings, we conclude that respiratory physiotherapy promoted a significant short-term improvement of many signs and symptoms in patients with bronchiolitis.
The present study has some limitations such as absence of sample power calculation. Thus, our study has a greater descriptive than inferential value. Our intention was not to extrapolate results, but to generate hypotheses. The absence of a control group makes the results less reliable; however, we had difficulties to obtain a control group because the study was conducted at a hospital where most doctors prescribe respiratory physiotherapy for patients with bronchiolitis. We believe that further studies should be conducted to provide scientific evidence to the discussion of the benefits of physical therapy in children hospitalized for bronchiolitis.
Acknowledgements
We are thankful to the physical therapists of the Maternal and Child Department of Hospital Israelita Albert Einstein and to those who significantly helped to conduct this study.
References
- 1. Carvalho WB, Johnston C, Fonseca MC. Bronquiolite aguda, uma revisão atualizada. Rev Assoc Med Bras 2007;53:182-8.
- 2. Lourenção LG, Salomão Junior JB, Rahal P, Souza FP, Zanetta DM. Infecções pelo vírus sincicial respiratório em crianças. Pulmão RJ 2005; 14:59-68.
- 3. Miyao CR, Gilio AE, Vieira S, Hein N, Pahl MM, Betta SL et al Infecções virais em crianças internadas por doença aguda no trato respiratório inferior. J Pediatr (Rio J) 1999;75:334-44.
- 4. Albernaz EP, Menezes AM, César JA, Victora CG, Barros FC. Hospitalização por bronquiolite aguda como fator de risco para sibilância recorrente. Cad Saude Publica 2000;16:1049-57.
- 5. Ferrés J. Comparison of two nebulized treatments in wheezing infants. Eur Respir J 1988; 1 (Suppl):306.
- 6. Rozov T. Doenças pulmonares em pediatria: diagnóstico e tratamento. São Paulo: Atheneu; 2005.
- 7. Sarmento GJ. Fisioterapia respiratória no paciente crítico - rotinas clínicas. Barueri: Manole; 2005.
- 8. Balachandran A, Shivbalan S, Thangavelu S. Chest physiotherapy in pediatric practice. Indian Pediatr 2005;42:559-68.
- 9. Perrotta C, Ortiz Z, Roqué i Figuls M. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database Syst Rev 2005:CD004873.
- 10. Chalumeau M, Foix-L'Helias L, Scheinmann P, Zuani P, Gendrel D, Ducou-le-Pointe HD. Rib fractures after chest physiotherapy for bronchiolitis or pneumonia in infants. Pediatr Radiol 2002;32:644-7.
- 11. Presto BL, Presto LD. Fisioterapia respiratória, uma nova visão. Rio de Janeiro: Loyola; 2003.
- 12. Wallis C, Prasad A. Who needs chest physiotherapy? Moving from anecdote to evidence. Arch Dis Child 1999;80:393-7.
- 13. Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika 1986;73:13-22.
- 14. Lanza FC, Cadrobbi C, Gazzotti MR, Faria R, Luque A, Solé D. Fisioterapia respiratória em lactentes com bronquiolite: realizar ou não? Mundo Saude 2008;32:183-8.
- 15. Luisi F. O papel da fisioterapia respiratória na bronquiolite viral aguda. Sci Med 2008;18:39-44.
- 16. Mucciollo MH, Simionato NA, Paula LC, Feola AI, Monteiro VC, Ceccon ME. Fisioterapia respiratória nas crianças com bronquiolite viral aguda: visão crítica. Pediatria (São Paulo) 2008;30:257-64.
- 17. American Academy of Pediatrics. Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics 2006;118:1774-93.
- 18. Clover RD. Clinical practice guideline for bronchiolitis: key recommendations. Am Fam Physician 2007;75:171.
- 19. Postiaux G. Auscultation pulmonaire et kinésithérapie en pédiatre. Rev Mal Respir 1999;16 (Suppl 3):206-7.
- 20. Webb MS, Martin JA, Cartlidge PH, Ng YK, Wright NA. Chest physiotherapy in acute bronchiolitis. Arch Dis Child 1985;60:1078-9.
- 21. Nicholas KJ, Dhouieb MO, Marshall TG, Edmunds AT, Grant MB. An evaluation of chest physiotherapy in the management of acute bronchiolitis: changing clinical practice. Physiotherapy 1999;85:669-74.
- 22. Bohé L, Ferrero ME, Cuestas E, Polliotto L, Genoff M. Indicación de la fisioterapia respiratoria convencional en la bronchiolitis aguda. Medicina (B. Aires) 2004;64:198-200.
- 23. Postiaux G, Dubois R, Marchand E, Demay M, Jacquy J, Mangiaracina M. Effets de la kinésithérapie respiratoire associant Expiration Lente Prolongée et Toux Provoquée dans la bronchiolite du nourrisson. Kinésither Rev 2006; 6:35-41.
Analysis of symptoms, clinical signs and oxygen support in patients with bronchiolitis before and after chest physiotherapy during hospitalization
Publication Dates
-
Publication in this collection
17 Feb 2012 -
Date of issue
Dec 2011
History
-
Received
28 Sept 2010 -
Accepted
04 Apr 2011