ABSTRACT
Objective:
Acute respiratory distress syndrome (ARDS) can be a devastating condition in children with cancer and alveolar recruitment maneuvers (ARMs) can theoretically improve oxygenation and survival. The study aimed to assess the feasibility of ARMs in critically ill children with cancer and ARDS.
Methods:
We retrospectively analyzed 31 maneuvers in a series of 12 patients (median age of 8.9 years) with solid tumors (n=4), lymphomas (n=2), acute lymphoblastic leukemia (n=2), and acute myeloid leukemia (n=4). Patients received positive end-expiratory pressure from 25 up to 40 cmH20, with a delta pressure of 15 cmH2O for 60 seconds. We assessed blood gases pre- and post-maneuvers, as well as ventilation parameters, vital signs, hemoglobin, clinical signs of pulmonary bleeding, and radiological signs of barotrauma. Pre- and post-values were compared by the Wilcoxon test.
Results:
Median platelet count was 53,200/mm3. Post-maneuvers, mean arterial pressure decreased more than 20% in two patients, and four needed an increase in vasoactive drugs. Hemoglobin levels remained stable 24 hours after ARMs, and signs of pneumothorax, pneumomediastinum, or subcutaneous emphysema were absent. Fraction of inspired oxygen decreased significantly after ARMs (FiO2; p=0.003). Oxygen partial pressure (PaO2)/FiO2 ratio increased significantly (p=0.0002), and the oxygenation index was reduced (p=0.01), but all these improvements were transient. Recruited patients’ 28-day mortality was 58%.
Conclusions:
ARMs, although feasible in the context of thrombocytopenia, lead only to transient improvements, and can cause significant hemodynamic instability.
Keywords:
Respiratory insufficiency; Neoplasms; Acute respiratory distress syndrome; Child
RESUMO
Objetivo:
A síndrome do desconforto respiratório agudo (SDRA) pode ser uma condição devastadora em crianças com câncer e as manobras de recrutamento alveolar (MRA) podem melhorar a oxigenação e a sobrevida. O objetivo foi avaliar a viabilidade das MRA em crianças gravemente doentes com câncer e SDRA.
Métodos:
Analisamos retrospectivamente 31 manobras em 12 pacientes (idade mediana de 8,9 anos), com tumores sólidos (n=4), linfomas (n=2) e leucemias linfoide (n=2) e mieloide agudas (n=4). Os pacientes receberam pressão expiratória final positiva de 25 a 40 cmH20, com delta de pressão de 15 cmH2O por 60 segundos. Gasometrias foram analisadas pré e pós-manobras, bem como os parâmetros de ventilação, sinais vitais, hemoglobina, sinais clínicos de sangramento pulmonar e sinais radiológicos de barotrauma. Valores foram comparados com o teste de Wilcoxon.
Resultados:
A contagem mediana de plaquetas era de 53.200/mm3. Após as manobras, em dois pacientes, a pressão arterial média declinou mais de 20%, e quatro necessitaram de aumento de drogas vasoativas. A hemoglobina permaneceu estável 24 horas após a MRA, sem sinais de pneumotórax, pneumomediastino ou enfisema subcutâneo. Houve diminuição significativa nas frações inspiradas de oxigênio (FiO2; p=0,003). A relação pressão arterial de oxigênio (PaO2)/FiO2 aumentou (p=0,002), e o índice de oxigenação caiu (p=0,01), mas essas melhoras foram transitórias. A mortalidade em 28 dias foi de 58%.
Conclusões:
As MRA, embora viáveis no contexto da trombocitopenia, levam apenas a melhorias transitórias e podem causar instabilidade hemodinâmica significativa.
Palavras-chave:
Insuficiência respiratória; Neoplasias; Síndrome do desconforto respiratório agudo; Criança
INTRODUCTION
Acute respiratory failure is a frequent condition in children with cancer admitted to the Intensive Care Unit (ICU). Those who develop acute respiratory distress syndrome (ARDS) and need mechanical ventilation (MV) have a poor prognosis.11. Ben-Abraham R, Weinbroum AA, Augerten A, Toren A, Harel R, Vardi A, et al. Acute respiratory distress syndrome in children with malignancy--can we predict outcome? J Crit Care. 2001;16:54-8. https://doi.org/10.1053/jcrc.2001.25232
https://doi.org/https://doi.org/10.1053/...
Twenty-eight-day mortality can be as high as 58% in patients with neoplasms, septic shock, and ARDS.22. Arduini R, Araujo O, Silva D, Senerchia A, Petrilli A. Sepsis-related acute respiratory distress syndrome in children with cancer: the respiratory dynamics of a devastating condition. Rev Bras Ter Intensiva. 2016;28:436-43. https://doi.org/10.5935/0103-507x.20160077
https://doi.org/https://doi.org/10.5935/...
Studies performing lung computed tomography (CT) have shown that ARDS presents multiple gravity-dependent atelectasis areas, which are prone to opening with alveolar recruitment maneuvers (ARMs).33. Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775-86. https://doi.org/10.1056/nejmoa052052
https://doi.org/https://doi.org/10.1056/...
Extension of the recruitment area is influenced by the time elapsed since ARDS onset, and ARMs have their best efficacy the earlier they are initiated due to the development of fibrosis in the affected lung in later stages of the disease. In lungs progressing with increased resistance, high positive end-expiratory pressure (PEEP) settings during ARMs can lead to complications, particularly hemodynamic impairment.44. Godet T, Constantin JM, Jaber S, Futier E. How to monitor a recruitment maneuver at the bedside. Curr Opin Crit Care. 2015;21:253-8. https://doi.org/10.1097/mcc.0000000000000195
https://doi.org/https://doi.org/10.1097/...
Few studies have analyzed alveolar recruitment in the pediatric population and none within the cancer subpopulation. The present study aimed to evaluate the feasibility of ARMs in critically ill pediatric cancer patients who developed acute respiratory failure due to ARDS.
METHOD
This is a retrospective study approved by the Ethics Committee of Universidade Federal de São Paulo (UNIFESP) (protocol no. 12802/2009), and the informed consent form was waived. We evaluated all data on electronic medical records from patients aged 0 to 17 years, admitted to our 11-bed oncologic ICU from January 1, 2010 to December 31, 2011, with an ARDS diagnosis according to the American-European Consensus Conference.55. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Consensus Committee. J Crit Care. 1994;9:72-81. https://doi.org/10.1016/0883-9441(94)90033-7
https://doi.org/https://doi.org/10.1016/...
Exclusion criteria were: severe hemodynamic instability at the moment of ARMs (need for vasopressors - epinephrine or norepinephrine - greater than 0.05 mcg/kg/min or progressive titrating doses 2 hours prior to intervention); extreme agitation/anxiety; untreated pneumothorax; signs of alveolar or digestive hemorrhage; bronchopleural fistulae; or intracranial hypertension.66. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301-8. https://doi.org/ 10.1056/NEJM200005043421801
https://doi.org/https://doi.org/ 10.1056...
,77. Neves VC, Koliski A, Giraldi DJ. Alveolar recruitment maneuver in mechanic ventilation pediatric intensive care unit children. Rev Bras Ter Intensiva. 2009;21:453-60. https://doi.org/10.1590/S0103-507X2009000400017
https://doi.org/https://doi.org/10.1590/...
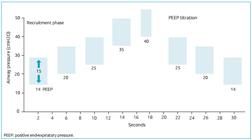
Following an institutional protocol, all patients were under continuous sedation and received neuromuscular blockade (rocuronium) before ARMs. Patients had to be at the first week of disease. ARMs were carried out in pressure-controlled ventilation mode, with a delta pressure [i.e., peak inspiratory pressure (PIP) minus PEEP] of 15 cmH2O. The initial PEEP value varied from 25 to 40 cmH2O. It was kept for 60 seconds if no hemodynamic instability (that is, bradycardia or decrease in blood pressure >20%) was observed. ARMs could be performed three times if oxygenation was not sustained. For example, children with less than 20 kg were submitted to an initial ARM at a PEEP of 25 cmH2O. ARM could be repeated at a PEEP of 30, with one last ARM at a PEEP of 35 cmH2O. Children with more than 20 kg were submitted to the first ARM at a PEEP of 30 cmH2O, the second (if necessary) at a PEEP of 35, and the last one at a PEEP of 40, always with a delta pressure of 15 cmH2O.
At the start of the titration phase, PEEP was reduced in decrements of 2-3 points, with less than ten seconds for each step, until oxygen saturation reached values lower than 92%. This was considered the desaturation point. The maneuver was performed again, and PEEP was set 2 cmH2O above this desaturation point (Figure 1).88. Rzezinski AF, Oliveira GP, Santiago VR, Santos RS, Ornellas DS, Morales MM, et al. Prolonged recruitment maneuver improves lung function with less ultrastructural damage in experimental mild acute lung injury. Respir Physiol Neurobiol. 2009;169:271-81. https://doi.org/10.1016/j.resp.2009.10.002
https://doi.org/https://doi.org/10.1016/...
,99. Amato MB, Carvalho CR, Isola A, Vieira S, Rotman V, Moock M, et al. Mechanical Ventilation in Acute Lung Injury (ALI)/Acute Respiratory Discomfort Syndrome (ARDS). J Bras Pneumol. 2007;33 (Suppl 2):S119-27. https://doi.org/10.1590/S1806-37132007000800007
https://doi.org/https://doi.org/10.1590/...
Positive end-expiratory pressure escalation and titration during the alveolar recruitment maneuver.
We analyzed blood gases before and after ARMs, as well as MV parameters, heart rate, mean arterial pressure (MAP), pulse oximetry, and vasopressor doses. Chest radiographs were reviewed to detect pneumothorax, pneumomediastinum, and pulmonary interstitial emphysema. Hemoglobin levels and subcutaneous emphysema were also monitored for 24 hours after ARMs. Oxygenation index (OI) was calculated according to Ortiz et al.: OI = fraction of inspired oxygen (FiO2) × mean airway pressure (mPaw) / oxygen partial pressure in arterial blood (PaO2).1010. Ortiz RM, Cilley RE, Bartlett RH. Extracorporeal membrane oxygenation in pediatric respiratory failure. Pediatr Clin North Am. 1987;34:39-46. https://doi.org/10.1016/s0031-3955(16)36179-x
https://doi.org/https://doi.org/10.1016/...
Dynamic compliance was calculated as: tidal volume / (PIP - PEEP).1111. Morrow B, Futter M, Argent A. A recruitment maneuver performed after endotracheal suction does not increase dynamic compliance in ventilated pediatric patients: a randomized controlled trial. Aust J Physiother. 2007;53:163-9. https://doi.org/10.1016/s0004-9514(07)70023-5
https://doi.org/https://doi.org/10.1016/...
We used the Wilcoxon signed-rank test to compare pre- and post-maneuver values. The Monte Carlo method determined the 99% confidence intervals, with resampling of at least 1000 tables due to the small sample size. Statistical significance was set at p<0.05. All statistical analyses were performed using the SPSS software, version 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
We analyzed 31 maneuvers performed in 12 patients, with a median age of 8.9 years (ranging from 9 months to 16 years). Table 1 presents the diagnoses: four patients had solid tumors, and eight had hematologic malignancies (one of them had undergone bone marrow transplantation). Maneuvers were performed in patients with a median of 53,200 platelets/mm3 (P25-75 = 32,200-122,530).
During ARMs, the minimum PEEP was 25 and the maximum, 40 cmH2O [interquartile range (IQR) 27-75: 35-40 cmH2O]. Maximum PIP was 55 cmH2O (IQR: 50-55 cmH2O), and the mean respiratory rate was 4.7 breaths per minute [standard deviation (SD): 3].
We found no significant changes in heart rate during ARM (mean pre-ARM: 136.7 beats per minute, SD: 26.5; post-ARM: 137.3, SD: 20.8). During seven maneuvers performed in five patients, MAP had a decline greater than 5% (12.9 mmHg on average, SD: 8.1), leading to an increase in rates of infusion of vasoactive drugs in four of them (33%). In two patients (16.6%), the reduction in MAP was greater than 20%. During six ARMs performed in two patients (16.6%), we identified a transient increase in MAP greater than 5% (mean: 23.7 mmHg, SD: 27.5). Mean MAP was 79 mmHg (SD: 16.8) before and 80.2 mmHg (SD: 18.5) after alveolar recruitment (p=0.93).
None of the children experienced a decrease in hemoglobin levels in the 24 h following ARMs. No major air leaks were detected, such as pneumothorax, pneumomediastinum, and/or subcutaneous emphysema.
FiO2 and OI significantly decreased after ARMs (p=0.003 and p=0.01, respectively); the PaO2/FiO2 ratio had a statistically significant increase (p=0.0002). These improvements in oxygenation were not sustained for more than 2 hours after ARMs, as oxygen saturation declined, and FiO2 increased again. All other blood gas parameters analyzed (pH, carbon dioxide partial pressure, bicarbonate, oxygen saturation) showed no signs of significant improvement post-maneuvers. Dynamic lung compliance was not affected either.
PEEP levels remained high after ARMs (p=0.02). Other ventilatory parameters (inspiratory pressure, mPaw, inspiratory time, and tidal volume) showed no significant differences. Table 2 describes MV parameter values and their respective p values. Figure 2 shows the boxplots of significant changes.
Boxplots of the values for the oxygen partial pressure/fraction of inspired oxygen ratio, oxygenation index, and positive end-expiratory pressure, pre- and post-recruitment maneuver.
We also analyzed the first ARM of each patient. Considering only these 12 ARMs, we found significant differences in FiO2 pre- and post-maneuvers (pre: 0.80±0.24; post: 0.58±0.22; p=0.05, according to the Wilcoxon test) and also in PaO2/FiO2 ratios pre- and post-maneuvers (pre: 95.3±49.3 and post: 158.5±72.7; p=0.03). Unfortunately, we could not perform further analyses of these first ARMs due to the small sample size.
DISCUSSION
In our small group of critically ill patients, recruitment maneuvers produced some degree of improvement in oxygenation parameters, but these improvements were evanescent. The fact that one-third of patients needed more vasoactive drugs is also concerning. The literature has no other studies on ARMs in this population, so we cannot compare results.
Pediatric cancer patients who develop ARDS are extremely ill and have high mortality rates. Ben-Abraham et al. studied 17 children with ARDS and hematologic malignancies under MV; 11 of them died (64.7%).11. Ben-Abraham R, Weinbroum AA, Augerten A, Toren A, Harel R, Vardi A, et al. Acute respiratory distress syndrome in children with malignancy--can we predict outcome? J Crit Care. 2001;16:54-8. https://doi.org/10.1053/jcrc.2001.25232
https://doi.org/https://doi.org/10.1053/...
Another study reported 29 children with cancer and sepsis-related ARDS: only 5 patients survived for more than 60 days. Among them, 31% died as a direct consequence of refractory hypoxemia, and the remaining patients died of multiple organ failure and catecholamine-refractory shock.22. Arduini R, Araujo O, Silva D, Senerchia A, Petrilli A. Sepsis-related acute respiratory distress syndrome in children with cancer: the respiratory dynamics of a devastating condition. Rev Bras Ter Intensiva. 2016;28:436-43. https://doi.org/10.5935/0103-507x.20160077
https://doi.org/https://doi.org/10.5935/...
ARDS mortality rates in this subpopulation remain unacceptably high, and no effective therapy, including pharmacological agents,1212. Fuller BM, Mohr NM, Hotchkiss RS, Kollef MH. Reducing the burden of acute respiratory distress syndrome: the case for early intervention and the potential role of the emergency department. Shock. 2014;41:378-87. https://doi.org/10.1097/shk.0000000000000142
https://doi.org/https://doi.org/10.1097/...
has been reported up to the present day.
Recruitment maneuvers can improve hypoxemia, but their use in critically ill children with cancer causes concerns due to frequent thrombocytopenia and the risk of pulmonary hemorrhage. The best method for performing ARMs is yet to be defined.1313. Rotta AT, Piva JP, Andreolio C, Carvalho WB, Garcia PC. Progress and perspectives in pediatric acute respiratory distress syndrome. Rev Bras Ter Intensiva. 2015;27:266-73. https://doi.org/10.5935/0103-507X.20150035
https://doi.org/https://doi.org/10.5935/...
The fixed delta pressure method used here seems to allow more hemodynamic stability compared with the sequential method.88. Rzezinski AF, Oliveira GP, Santiago VR, Santos RS, Ornellas DS, Morales MM, et al. Prolonged recruitment maneuver improves lung function with less ultrastructural damage in experimental mild acute lung injury. Respir Physiol Neurobiol. 2009;169:271-81. https://doi.org/10.1016/j.resp.2009.10.002
https://doi.org/https://doi.org/10.1016/...
,1414. Iannuzzi M, Sio A, De Robertis E, Piazza O, Servillo G, Tufano R. Different patterns of lung recruitment maneuvers in primary acute respiratory distress syndrome: effects on oxygenation and central hemodynamics. Minerva Anestesiol. 2010;76:692-8. Slowly decreasing PEEP also seems to maintain alveolar stability for longer.1515. Girgis K, Hamed H, Khater Y, Kacmarek RM. A decremental PEEP trial identifies the PEEP level that maintains oxygenation after lung recruitment. Respir Care. 2006;51:1132-9.,1616. Lim CM, Jung H, Koh Y, Lee JS, Shim TS, Lee SD, et al. Effects of alveolar recruitment maneuver in early acute respiratory distress syndrome according to antiderecruitment strategy, etiological category of diffuse lung injury, and body position of the patient. Crit Care Med. 2003;31:411-8. https://doi.org/10.1097/01.ccm.0000048631.88155.39
https://doi.org/https://doi.org/10.1097/...
Studies on adults have demonstrated that optimizing PEEP after ARMs is essential to improve oxygenation,1616. Lim CM, Jung H, Koh Y, Lee JS, Shim TS, Lee SD, et al. Effects of alveolar recruitment maneuver in early acute respiratory distress syndrome according to antiderecruitment strategy, etiological category of diffuse lung injury, and body position of the patient. Crit Care Med. 2003;31:411-8. https://doi.org/10.1097/01.ccm.0000048631.88155.39
https://doi.org/https://doi.org/10.1097/...
which was achieved in our subjects by setting PEEP above the desaturation point, presupposing that this point would correspond to the partial alveolar collapse. Boriosi et al.1717. Boriosi JP, Sapru A, Hanson JH, Asselin J, Gildegorin G, Newman V, et al. Efficacy and safety of lung recruitment in pediatric patients with acute lung injury. Pediatr Crit Care Med. 2011;12:431-6. https://doi.org/10.1097/pcc.0b013e3181fe329d
https://doi.org/https://doi.org/10.1097/...
identified an improvement in the PaO2/FiO2 ratio that could last up to 12 hours after the maneuvers. In our study, however, improvement lasted for no more than 2 hours, showing the transient efficacy of ARMs, also registered by Kheir et al.1818. Kheir JN, Walsh BK, Smallwood CD, Retting JS, Thompson JE, Gómez-Laberge C, et al. Comparison of 2 lung recruitment strategies in children with acute lung injury. Respir Care. 2013;58:1280-90. https://doi.org/10.4187/respcare.01808
https://doi.org/https://doi.org/10.4187/...
No significant changes were found regarding the patients’ heart rates. Cruces et al. pointed out hypotension as a common side effect of ARM, detecting MAP reductions of 9.2%.1919. Cruces P, Donoso A, Valenzuela J, Díaz F. Respiratory and hemodynamic effects of a stepwise lung recruitment maneuver in pediatric ARDS: a feasibility study. Pediatr Pulmonol. 2013;48:1135-43. https://doi.org/10.1002/ppul.22729
https://doi.org/https://doi.org/10.1002/...
In our study, MAP declines led to increased infusion of vasopressors in four patients (33.3%), highlighting the extreme care needed when performing ARMs. No bleeding or airway complications were noted in the subsequent 24-hour period.
As ARMs improve oxygen saturation during a short period, healthcare providers might feel tempted to perform them frequently, but no data available from controlled studies allow strong conclusions on their efficacy, safety, and long-term consequences in children.2020. Arun TB. Alveolar recruitment maneuvers in ventilated children: caution required. Indian J Crit Care Med. 2011;15:141. https://doi.org/10.4103/0972-5229.83005
https://doi.org/https://doi.org/10.4103/...
The main limitation of our study is having a sample too small to determine all aspects of ARM safety. Nonetheless, it was performed as a pilot study to assess the feasibility of ARMs in these extremely ill patients.
A recent large, well-designed, adult clinical trial resulted not only in limited success but in higher 28-day mortality in the ARM group;2121. Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs Low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335-45. https://doi.org/10.1001/jama.2017.14171
https://doi.org/https://doi.org/10.1001/...
maximum ARM could even be associated with cardiac arrest. Interestingly, 28-day mortality was higher in this group than in the control group (55.3% vs. 49.3%), but still lower than in the cancer and ARDS population.2121. Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs Low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335-45. https://doi.org/10.1001/jama.2017.14171
https://doi.org/https://doi.org/10.1001/...
Therefore, assessing actual evidence, ARM should be reserved for patients suffering from refractory hypoxemia, already under potentially non-protective high inspiratory or peak pressures and FiO2, and not as a routine therapy in ICUs.
In conclusion, ARMs, although viable, have restrictions regarding their effectiveness in children with cancer and ARDS, with transient improvements in oxygenation, but no improvements in lung compliance. Despite the lack of bleeding-related complications, even in the context of thrombocytopenia, hemodynamic instability seems to be a major concern.
REFERENCES
-
1Ben-Abraham R, Weinbroum AA, Augerten A, Toren A, Harel R, Vardi A, et al. Acute respiratory distress syndrome in children with malignancy--can we predict outcome? J Crit Care. 2001;16:54-8. https://doi.org/10.1053/jcrc.2001.25232
» https://doi.org/https://doi.org/10.1053/jcrc.2001.25232 -
2Arduini R, Araujo O, Silva D, Senerchia A, Petrilli A. Sepsis-related acute respiratory distress syndrome in children with cancer: the respiratory dynamics of a devastating condition. Rev Bras Ter Intensiva. 2016;28:436-43. https://doi.org/10.5935/0103-507x.20160077
» https://doi.org/https://doi.org/10.5935/0103-507x.20160077 -
3Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775-86. https://doi.org/10.1056/nejmoa052052
» https://doi.org/https://doi.org/10.1056/nejmoa052052 -
4Godet T, Constantin JM, Jaber S, Futier E. How to monitor a recruitment maneuver at the bedside. Curr Opin Crit Care. 2015;21:253-8. https://doi.org/10.1097/mcc.0000000000000195
» https://doi.org/https://doi.org/10.1097/mcc.0000000000000195 -
5Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Consensus Committee. J Crit Care. 1994;9:72-81. https://doi.org/10.1016/0883-9441(94)90033-7
» https://doi.org/https://doi.org/10.1016/0883-9441(94)90033-7 -
6Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301-8. https://doi.org/ 10.1056/NEJM200005043421801
» https://doi.org/https://doi.org/ 10.1056/NEJM200005043421801 -
7Neves VC, Koliski A, Giraldi DJ. Alveolar recruitment maneuver in mechanic ventilation pediatric intensive care unit children. Rev Bras Ter Intensiva. 2009;21:453-60. https://doi.org/10.1590/S0103-507X2009000400017
» https://doi.org/https://doi.org/10.1590/S0103-507X2009000400017 -
8Rzezinski AF, Oliveira GP, Santiago VR, Santos RS, Ornellas DS, Morales MM, et al. Prolonged recruitment maneuver improves lung function with less ultrastructural damage in experimental mild acute lung injury. Respir Physiol Neurobiol. 2009;169:271-81. https://doi.org/10.1016/j.resp.2009.10.002
» https://doi.org/https://doi.org/10.1016/j.resp.2009.10.002 -
9Amato MB, Carvalho CR, Isola A, Vieira S, Rotman V, Moock M, et al. Mechanical Ventilation in Acute Lung Injury (ALI)/Acute Respiratory Discomfort Syndrome (ARDS). J Bras Pneumol. 2007;33 (Suppl 2):S119-27. https://doi.org/10.1590/S1806-37132007000800007
» https://doi.org/https://doi.org/10.1590/S1806-37132007000800007 -
10Ortiz RM, Cilley RE, Bartlett RH. Extracorporeal membrane oxygenation in pediatric respiratory failure. Pediatr Clin North Am. 1987;34:39-46. https://doi.org/10.1016/s0031-3955(16)36179-x
» https://doi.org/https://doi.org/10.1016/s0031-3955(16)36179-x -
11Morrow B, Futter M, Argent A. A recruitment maneuver performed after endotracheal suction does not increase dynamic compliance in ventilated pediatric patients: a randomized controlled trial. Aust J Physiother. 2007;53:163-9. https://doi.org/10.1016/s0004-9514(07)70023-5
» https://doi.org/https://doi.org/10.1016/s0004-9514(07)70023-5 -
12Fuller BM, Mohr NM, Hotchkiss RS, Kollef MH. Reducing the burden of acute respiratory distress syndrome: the case for early intervention and the potential role of the emergency department. Shock. 2014;41:378-87. https://doi.org/10.1097/shk.0000000000000142
» https://doi.org/https://doi.org/10.1097/shk.0000000000000142 -
13Rotta AT, Piva JP, Andreolio C, Carvalho WB, Garcia PC. Progress and perspectives in pediatric acute respiratory distress syndrome. Rev Bras Ter Intensiva. 2015;27:266-73. https://doi.org/10.5935/0103-507X.20150035
» https://doi.org/https://doi.org/10.5935/0103-507X.20150035 -
14Iannuzzi M, Sio A, De Robertis E, Piazza O, Servillo G, Tufano R. Different patterns of lung recruitment maneuvers in primary acute respiratory distress syndrome: effects on oxygenation and central hemodynamics. Minerva Anestesiol. 2010;76:692-8.
-
15Girgis K, Hamed H, Khater Y, Kacmarek RM. A decremental PEEP trial identifies the PEEP level that maintains oxygenation after lung recruitment. Respir Care. 2006;51:1132-9.
-
16Lim CM, Jung H, Koh Y, Lee JS, Shim TS, Lee SD, et al. Effects of alveolar recruitment maneuver in early acute respiratory distress syndrome according to antiderecruitment strategy, etiological category of diffuse lung injury, and body position of the patient. Crit Care Med. 2003;31:411-8. https://doi.org/10.1097/01.ccm.0000048631.88155.39
» https://doi.org/https://doi.org/10.1097/01.ccm.0000048631.88155.39 -
17Boriosi JP, Sapru A, Hanson JH, Asselin J, Gildegorin G, Newman V, et al. Efficacy and safety of lung recruitment in pediatric patients with acute lung injury. Pediatr Crit Care Med. 2011;12:431-6. https://doi.org/10.1097/pcc.0b013e3181fe329d
» https://doi.org/https://doi.org/10.1097/pcc.0b013e3181fe329d -
18Kheir JN, Walsh BK, Smallwood CD, Retting JS, Thompson JE, Gómez-Laberge C, et al. Comparison of 2 lung recruitment strategies in children with acute lung injury. Respir Care. 2013;58:1280-90. https://doi.org/10.4187/respcare.01808
» https://doi.org/https://doi.org/10.4187/respcare.01808 -
19Cruces P, Donoso A, Valenzuela J, Díaz F. Respiratory and hemodynamic effects of a stepwise lung recruitment maneuver in pediatric ARDS: a feasibility study. Pediatr Pulmonol. 2013;48:1135-43. https://doi.org/10.1002/ppul.22729
» https://doi.org/https://doi.org/10.1002/ppul.22729 -
20Arun TB. Alveolar recruitment maneuvers in ventilated children: caution required. Indian J Crit Care Med. 2011;15:141. https://doi.org/10.4103/0972-5229.83005
» https://doi.org/https://doi.org/10.4103/0972-5229.83005 -
21Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs Low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335-45. https://doi.org/10.1001/jama.2017.14171
» https://doi.org/https://doi.org/10.1001/jama.2017.14171
Funding
-
This study did not receive any funding.
Publication Dates
-
Publication in this collection
11 Jan 2021 -
Date of issue
2021
History
-
Received
13 Aug 2019 -
Accepted
19 Jan 2020 -
Published
04 Jan 2021